Abstract
The pediatric population seems to be at a lower risk of developing severe clinical symptoms of COVID‐19. However, the clinical and epidemiological characteristics of COVID‐19 in children are yet to be fully clarified. This retrospective observational study aimed to evaluate the frequency of pediatric laboratory‐confirmed COVID‐19 patients from February 2020 to April 2021. A total of 740 (5.1% of total) pediatric COVID‐19 cases were observed during the study period. The peak of pediatric cases was observed in November 2020, with 239 cases. During the first wave of pandemics, the frequency of pediatric cases was 0.89% (49/5877 cases), ranging from 0.6% in February 2020 to 1.3% in April 2020. On the contrary, after the beginning of the second wave, the frequency of pediatric cases raised from 5.3% in September 2020 to 9.4%in February 2021, with an overall frequency of 8.2% (690/8416 cases). A different rate of SARS‐CoV‐2 circulation was observed among the pediatric population between the pandemic waves. During the second wave, two peaks of cases were observed. The last peak was associated with the spread of a more transmissive SARS‐CoV‐2 strain (VOC 202012/01).
Keywords: COVID‐19, epidemiology, pandemic, pediatric infection, SARS‐CoV‐2
Key message.
Overall, only 5% of COVID‐19 cases accounted for patients <15 years. Two different rates of SARS‐CoV‐2 circulation were observed among the pediatric population between the pandemic waves. During the second wave, two peaks of cases were observed. The last peak was associated with the spread of a more transmissive SARS‐CoV‐2 strain (VOC 202012/01).
1. INTRODUCTION
Since coronavirus disease 2019 (COVID‐19) was initially reported in China on December 30, 2019, SARS‐CoV‐2 spread worldwide.1, 2 As of April 12, 2021, 135 million confirmed infections and near to 3 million deaths have been reported worldwide. 3 At the beginning of the Pandemic, Lombardy was the Italian region most affected by the SARS‐CoV‐2 virus. 4 Generally, viral respiratory infections are primarily concentrated in the pediatric population. However, as early observed during the first pandemic wave, the pediatric population has not been mainly involved, and data on the effective burden of the pandemic in the pediatric population are very limited. Compared to adults, there are relatively few studies on pediatric COVID‐19.5, 6, 7 In particular, the clinical and epidemiological characteristics of COVID‐19 in children aged 0–16 years are yet to be fully clarified. In the scenario of the rapid worldwide spread of SARS‐CoV‐2 infection, the rising number of pediatric cases is to be expected. This retrospective analysis aimed to evaluate the frequency of pediatric infection among COVID‐19 cases diagnosed in our center, since the beginning of the Pandemic.
A total of 14353 COVID‐19 cases have been detected at our Regional Reference Laboratory (Molecular Virology Unit, Fondazione IRCCS Policlinico San Matteo Pavia, Italy) between February 20, 2020 and April 12, 2021. The presence of SARS‐CoV‐2 RNA was assessed using specific real‐time RT‐PCR as previously described. 8 Among COVID‐19 cases, 740 (5.1% of total) were observed in patients <15 years, with 397 (53.6%) male and 343 (46.4%) female. As showed in Figure 1A, the peak of pediatric cases was observed in November 2020 with 239 cases. After December 2020, an overall decrease of cases was observed until a second peak observed in March 2021 with 138 cases. On the contrary, during the first wave of pandemic (February‐June 2020), the peak of pediatric cases was observed in March 2020, with 28 cases corresponding to the month with the most significant number of cases (n = 3960) observed in our hospital (Figure 1A). Between May 2020 and September 2020, less than 10 cases/month were observed, according to the reduced circulation of SARS‐CoV‐2 in Lombardy. During the first wave of pandemics, the frequency of pediatric cases was 0.89% (49/5877 cases), ranging from 0.6% in February 2020 to 1.3% in April 2020 (Figure 1B). On the contrary, after the beginning of the second wave, the frequency of pediatric cases raised from 5.3% in September 2020 to 9.4%in February 2021, with an overall frequency of 8.2% (690/8416 cases) (Figure 1B).
FIGURE 1.
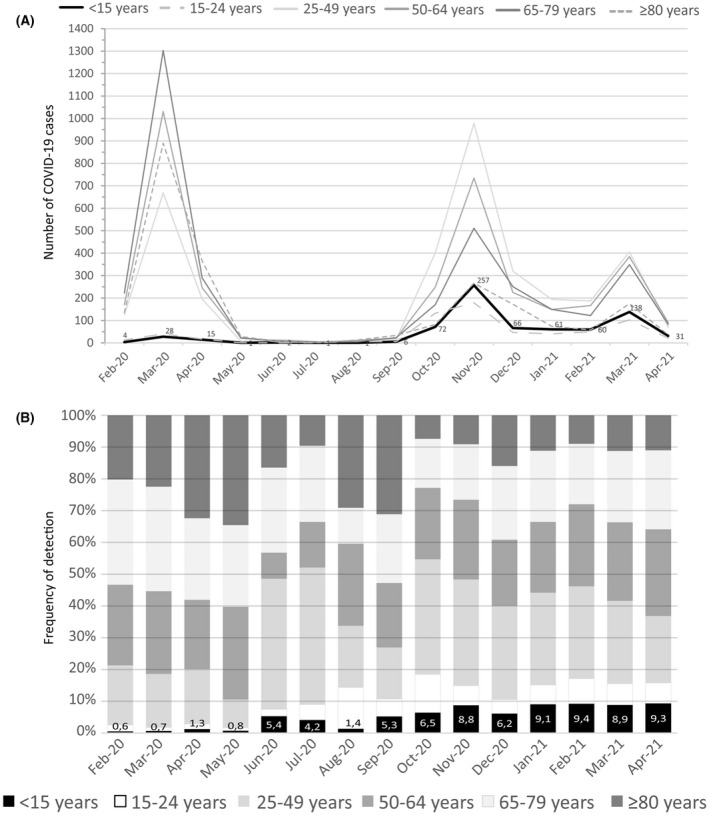
The number of COVID‐19 cases according to age category between February 2020 and April 2021 (A). The number of pediatric cases (<15 years) is reported near the peak for each month. Frequency of SARS‐CoV‐2 cases detection according to age category (B). The percentage of pediatric cases (<15 years) is reported within the bars for each month
Despite the evidence of the wide circulation of other respiratory viruses (eg, influenza and respiratory syncytial virus) among the pediatric population in our study, only 5% of COVID‐19 cases accounted for patients <15 years. In addition, two different rates of circulation were observed comparing first and second pandemic waves (<1% vs. 8.2%). This difference could be explained by the changing containing measures implemented during the lockdown on March‐May 2020 compared to the second wave (September 2020 – April 2021). As previously observed, most pediatric patients were asymptomatic and can spread the infection to their family members, some of whom develop severe symptoms. 9 Thus, in this context, it is expected that the rates of circulation observed have been different.
In our analysis, three peaks of cases were observed. The first on March 2020 was supported by the uncontrolled circulation of SARS‐CoV‐2 probably present in our Region since January 2020. 10 The second peak was observed during the second wave started in September 2020, where a global increase in the number of newly reported cases was seen in the European and Eastern countries. 3 Lastly, after introducing the SARS‐CoV‐2 variant of concern (VOC) 202012/01 (alpha, lineage B.1.1.7) in January 2020 in Italy, a third peak of cases on March 2021 was observed. The occurrence of a third peak was supported by the circulation of VOC 202012/01 associated with an increased rate of transmission. 11
In conclusion, different rates of SARS‐CoV‐2 circulation were observed among the pediatric population between the pandemic waves. During the second wave, two peaks of cases were observed. The last peak was associated with the spread of a more transmissive SARS‐CoV‐2 strain (VOC 202012/01).
CONFLICT OF INTEREST
All authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Francesca Rovida: Conceptualization (equal); Supervision (lead); Writing‐review & editing (equal). Federica Giardina: Methodology (equal), Writing‐review & editing (equal). Guglielmo Ferrari: Methodology (equal), Writing‐review & editing (equal). Federica Novazzi: Methodology (equal), Writing‐review & editing (equal). Stefania Paolucci: Methodology (equal), Writing‐review & editing (equal). Antonio Piralla: Conceptualization (equal); Supervision (lead); Writing‐review & editing (equal). Fausto Baldanti: Conceptualization (equal); Supervision (equal); Writing‐review & editing (equal).
ACKNOWLEDGMENTS
We thank Daniela Sartori for manuscript editing.
Rovida F, Giardina F, Ferrari G, Paolucci S, Piralla A, Baldanti F. SARS‐CoV‐2 infections in pediatric patients: A comparison of three pandemic waves. Pediatr Allergy Immunol. 2022;33 (Suppl. 27):93–95. 10.1111/pai.13642
Funding information
This study was supported by “Ricerca Finalizzata” from the Ministry of Health, Italy (grant COVID‐2020‐12371817).
Editor: Elena Chiappini
REFERENCES
- 1. Dong E, Du H, Gardner L. An interactive web‐based dashboard to track COVID‐19 in real time. Lancet Infect Dis. 2020;20:533‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO Coronavirus (COVID‐19) Dashboard (Accessed 15th April 2021). https://covid19.who.int
- 4. Riccardo F, Ajelli M, Andrianou XD, et al. Epidemiological characteristics of COVID‐19 cases and estimates of the reproductive numbers 1 month into the epidemic, Italy, 28th January to 31st March 2020. Euro Surveill. 2020;25:2000790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wei M, Yuan J, Liu Y, et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020;323:1313‐1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID‐19 among children in China. Pediatrics. 2020;145:e20200702. [DOI] [PubMed] [Google Scholar]
- 7. Ma H, Hu J, Tian J, et al. A single‐center, retrospective study of COVID‐19 features in children: a descriptive investigation. BMC Med. 2020;18:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rovida F, Cereda D, Novati S, et al. Low risk for SARS‐CoV2 symptomatic infection and early complications in paediatric patients during the ongoing CoVID19 epidemics in Lombardy. Clin Microbiol Infect. 2020;26:1569‐1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castagnoli R, Votto M, Licari A, et al. Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020;174:882‐889. [DOI] [PubMed] [Google Scholar]
- 10. Alteri C, Cento V, Piralla A, et al. Genomic epidemiology of SARS‐CoV‐2 reveals multiple lineages and early spread of SARS‐CoV‐2 infections in Lombardy. Italy. Nat Commun. 2021;12:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS‐CoV‐2 lineage B.1.1.7 in England. Science. 2021;372. [DOI] [PMC free article] [PubMed] [Google Scholar]


