Abstract
Introduction
Effective teamwork in paediatric cardiac surgery is known to improve team performance and surgical outcomes. However, teamwork in low‐ and middle‐income countries (LMICs), including Mongolia, is understudied. We examined multiple dimensions of teamwork to inform a team‐based training programme to strengthen paediatric cardiac surgical care in Mongolia.
Methods
We used a mixed‐methods approach, combining social network analysis and in‐depth interviews with medical staff, to explore the structure, process, quality, and context of teamwork at a single medical centre. We conceptualised the team's structure based on communication frequency among the members (n = 24) and explored the process, quality, and context of teamwork via in‐depth interviews with select medical staff (n = 9).
Results
The team structure was highly dense and decentralised, but the intensive care unit nurses showed high betweenness‐centrality. In the quality and process domain of teamwork, we did not find a regular joint decision‐making process, leading to the absence of common goals among the team members. Although role assignment among the medical staff was explicit, those strictly defined roles hindered active communication about patient information and responsibility‐sharing. Most interviewees did not agree with the organisational policies that limited discussions among team members; therefore, medical staff continued to share training and work experiences with each other, leading to strong and trustworthy relationships.
Conclusion
The findings of this study underscore the importance of well‐structured and goal‐oriented communication between medical staff, as well as the management of the quality of collaboration within a team to increase teamwork effectiveness in paediatric cardiac surgery teams in LMICs.
Keywords: cardiovascular disease, child health, ICU nurses, LMICs, social network analysis, team‐based training
Highlights
Team‐based training interventions have been feasible and effective in low‐ and middle‐income countries.
Although ICU nurses are a central part of the paediatric cardiac surgery care team, there are no formal post‐operative or training activities that can facilitate the joint decision‐making and common goal‐sharing process.
Resource sharing, clear role assignment, and conflict resolution rules are lacking and organisational support is key to improving teamwork.
Building trust between hospital administrators and team leadership is needed.
1. INTRODUCTION
Congenital heart disease (CHD), the most common type of congenital defect, accounts for a substantial burden of child mortality in low‐ and middle‐income countries (LMICs). 1 , 2 In LMICs, more than 90% of congenital anomalies are considered to be acute, 2 and most cases require surgery at short notice. However, paediatric patients in LMICs still lack adequate cardiac surgical care. 3 A significant barrier to increasing access and improving treatment quality for CHD in LMICs is the inadequate surgical workforce, which has limited skills and competencies to deliver perioperative, intraoperative, and postoperative services. 4
Increasing the quality of teamwork within a cohesive multidisciplinary surgical team is known to result in successful patient and surgical outcomes. 5 , 6 , 7 , 8 A team is defined as ‘two or more individuals with specific tasks working together to achieve common goals through sharing information, resources, and mutual trust’. 9 Promoting effective teamwork among local medical staff has been shown to improve surgical outcomes for children with CHD in LMICs. 9 By implementing training that emphasises collaborative team‐building within the medical staff of an LMIC team in partnership with a high‐income country (HIC) team, local medical staff can strengthen their capacities in communicating about patient information and surgical procedures with diverse professionals within the team, including cardiac surgeons, perfusionists, paediatric cardiologists, intensive care unit (ICU) nurses, ward nurses, and scrub nurses. 6 , 9
Teamwork has been operationalised as having three dimensions that can facilitate or hinder effective collaboration: social network structure, quality and process, and context. First, studies exploring teamwork structure have examined team size, density, and centrality. 10 , 11 , 12 , 13 , 14 , 15 , 16 Teamwork structure can be identified by the patterns of interconnected communication or information‐sharing behaviours among team members. 17 Structure has important implications for the quality of personal relationships, communication, communication‐related roles, and power dynamics among team members. 18 For example, network size is an important indicator measuring the extent to which the communication within a team is efficient, since a large network size makes communication among stakeholders more complex. 13 , 19 Additionally, the measure of betweenness‐centrality makes it possible to identify gatekeepers of communication within subsets of the team. Network members with a high betweenness‐centrality score tend to control information flow between other network members, thereby coordinating or leading teamwork. 13 , 20
Second, the process and quality of teamwork have been investigated in terms of diverse factors, including shared goals, role assignments, the balance between common goals and individual autonomy, shared knowledge, and trust among team members. 21 , 22 , 23 Joint decision‐making processes facilitate shared goals and understanding of other team members' opinions and behaviours and promote team members' commitment to and satisfaction with their work. 19 , 21 , 24 Additionally, explicit role assignments prevent role conflict among team members, facilitating holistic trust within a team. 25 Since the aim of teamwork is to achieve common goals, it is important to maintain a balance between the individual opinions, goals, and autonomy of each team member and those of the team or hospital. If the team's mission extensively constrains a team member, the team member's commitment to the team can diminish. 25 , 26 , 27 , 28 Actively sharing information and knowledge allows team members to effectively reduce the ambiguity of their tasks and adjust their roles and activities to achieve better team performance. 10 , 21 , 29 , 30 , 31 Moreover, when team members are trustworthy and have good interpersonal relationships, the communication process becomes more effective as communication costs are reduced, and team members can fully understand each other's behaviours. 24 , 25 , 30 , 32 , 33 Highly cohesive relationships among team members motivate them to be more supportive, making working conditions more productive. 31 , 34
Finally, another group of studies has explored how the environmental context, such as the working conditions in a hospital 8 , 11 , 12 , 21 , 29 , 35 , 36 or the organisation's culture for teamwork, can stimulate or hinder effective teamwork. 37 An organisational culture that values and encourages teamwork and participation in a team can facilitate effective teamwork. 37
Although earlier studies have contributed to understanding the multiple dimensions of teamwork including structure, process and quality, and context, those studies lack an integrated perspective on these dimensions, particularly in LMICs. Some studies have explored teamwork between medical staff, especially within HICs 19 , 24 , 25 ; however, only a few studies have explored teamwork beyond the operating room. 11 , 35 , 38
In light of the above considerations, this study aimed to explore the following aspects of a paediatric cardiac surgery team in a tertiary‐level general hospital of Mongolia using a mixed‐methods approach, combining social network analysis (SNA) and in‐depth interviews with medical staff: (1) structure: network density, degree, and betweenness‐centrality of the team through an analysis of network data measured by communication frequency among medical staff, (2) teamwork quality and process: joint decision‐making and goal‐sharing processes; explicit role assignments and conflict resolution; respecting each member's autonomy; information and resource sharing; and trustworthy relationships among the medical staff, and (3) context: facilitators or barriers of effective teamwork in the hospital or in the local context. We provide practical recommendations on how to improve teamwork in LMIC contexts, and believe that our findings can serve as a foundation for implementing future interventions or training programs in LMICs where scarce resources are dedicated to promoting team building.
2. METHODS
2.1. Conceptual framework
To understand the integrated dimensions of teamwork, we operationalised the structure (network size, density, degree‐centrality, and betweenness‐centrality), process and quality (governance, administration, autonomy, resource sharing, and trustworthy relationships), and context (culture and provision of resources) of teamwork (Table 1).
TABLE 1.
Conceptual framework of collaborative teamwork
| Conceptual dimensions of teamwork | Sub‐dimensions | Description | Source |
|---|---|---|---|
| Structure | Network size | Total number of team members in a network | 13 , 19 , 39 , 40 |
| Network density | Total number of relational ties divided by the total possible number of relational ties | 41 , 42 | |
| Network degree‐centrality | Number of ties incident to a network member | 41 , 42 | |
| Network betweenness‐centrality | Total number of shortest paths between every possible pair of nodes in a graph that pass through a given node | 13 , 20 | |
| Process & quality | Governance | How to jointly make decisions about rules that will govern behaviour and relationships | 19 , 22 , 23 , 24 , 43 |
| Administration | Establishing an effective operating system for collaboration that includes clarity of roles and responsibilities, communication channels, and processes for conflict resolution | 19 , 22 , 23 , 24 , 25 , 43 | |
| Autonomy | Balancing organisational identity and autonomy with team members | 22 , 23 , 25 , 26 , 27 , 28 , 43 | |
| Resource sharing | Mutually beneficial interdependencies based either on differing interests or shared interest | 10 , 21 , 22 , 23 , 29 , 30 , 31 , 43 | |
| Trustworthy relationship | Trustworthy relationships between team members | 22 , 23 , 24 , 25 , 30 , 31 , 32 , 33 , 34 , 43 | |
| Context | Culture or climate for teamwork | The extent to which organisations value and encourage teamwork and participation | 37 |
| Provision of resources for teamwork | Provision of recognition, information systems, rewards, and time | 37 |
2.2. Study setting
The study was carried out in the department of cardiovascular surgery of a tertiary‐level general hospital, the Third State Central Hospital of Mongolia, located in Ulaanbaatar, Mongolia. Paediatric cardiac surgery was first performed at the hospital in 2005 (Shastin hospital 44 ). According to the annual hospital report, the hospital received an average of approximately 8100 inpatients and 24,500 outpatient visits for cardiovascular disease each year from 2017 to 2019 (Shastin hospital 45 ). Since 2013, the Third State Central Hospital of Mongolia, the JW LEE Cent, and Seoul National University Hospital of South Korea have been collaborating on a project to build team‐based paediatric cardiac surgical care. The project aims to increase the safety of surgery and surgical capacity through enhanced knowledge and skills, and to improve the quality of care for children with CHD via team‐based multi‐professional hands‐on training. Mongolian trainees and Korean trainers perform their clinical duties together or in parallel, depending on what is considered more efficient. More details on the training can be found elsewhere. 9 , 46
2.3. Data collection and measures
Data collection took place during the annual visits. Both quantitative and qualitative data were collected during the week of training from October 6–12, 2019, and the follow‐up qualitative data were collected from June 23 to 31 July 2020. We applied a mixed‐methods approach combining SNA and in‐depth interviews to investigate the characteristics of the teamwork structure, process, and context. The Mongolian staff provided a roster of the paediatric cardiac surgery team upon request, which is different from the roster of the adult cardiac surgery team. Twenty‐eight Mongolian medical staff were listed as members of the paediatric cardiac surgery team at the hospital; the team included surgeons, perfusionists, ICU nurses, ward nurses, and scrub nurses. Of these, two cardiac surgeons, one scrub nurse, and one cardiologist were excluded from the survey because they were on vacation and were not available. Therefore, our final study participants included 24 clinical staff (Table 2). Survey questionnaires were provided in Appendix A.
TABLE 2.
Study participants (N = 24)
| Professions | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cardiac surgeon | General surgeon | Anaesthesiologist | Anaesthesiology nurse | ICU nurse | Wound dressing nurse | Scrub nurse | Assistant nurse | |
| Survey (n = 24) | 4 | 1 | 5 | 2 | 7 | 1 | 3 | 1 |
| Interview (n = 9) | 3 | 1 | 1 | 0 | 4 | 0 | 0 | 0 |
Note: A total of four medical staffs indicated dual positions: two were cardiac surgeon and general surgeon, one was anaesthesiologist and wound dressing nurse, and one was ICU nurse and scrub nurse. The main profession of the two was identified through additional interviews, and classified as those professions. Interview participants were included in the whole study participants.
To collect network data for visualising and measuring the network structure (i.e., density and centrality), we surveyed the paediatric cardiac surgery team (n = 24). We measured communication frequency between medical staff on a range from ‘not at all’ (1) to ‘most frequently’ (5). We guided each medical staff member to select one option for the frequency of interactions with each other member. We provided the list of medical staff members using the paediatric cardiac surgery team roster that was provided. Network density was measured by how diffuse or dense the connections between network members were across the entire network, based on the number of actually connected nodes compared to all possible connected nodes among network members. In contrast, individual medical staff member degree‐centrality was calculated by summing the total number of connections for each individual, and individual betweenness‐centrality was calculated by measuring the total number of shortest paths between every possible pair of nodes for each individual. 41
Qualitative data were collected via individual in‐depth interviews of the Mongolian medical staff (n = 9), chosen based on their professional background and career experience, to further explore the communication and collaboration processes. Since the interview participants were part of the team, they participated in both the SNA surveys and the in‐depth interviews. We conducted the first interview session alongside the SNA survey from October 6–12, 2019 in Mongolia (n = 5). For both the quantitative and qualitative data analysis, we needed more extensive contextual information related to the network structure and context to understand and interpret the results appropriately (e.g., why were the highest betweenness‐centrality scores found for some ICU nurses). The second‐round interviews were additionally conducted from June 23 to 31 July 2020, virtually due to COVID‐19 (n = 4). Bilingual interviewers (Mongolian‐Korean) used a semi‐structured guide to conduct the interviews. All surveys and interviews were conducted after receiving written consent for participation.
2.4. Data analysis
The network density, degree‐centrality, and betweenness‐centrality scores were calculated using UCINET version 6.0. 47 Centrality scores were calculated based on Freeman's degree of centrality. 48 We transformed the 5‐point scale for communication frequency (1–5) into a two‐scaled (0–1) edge, recoding scores of 1–2 as 0, and scores of 3–5 as 1. As most frequency scores were high, weighting the edges would not have been meaningful.
The network structure was visualised using Gephi software 49 version 0.9.2. Gephi splits data into ‘nodes,’ consisting of individuals, and ‘edges,’ which are the connections between two nodes. Data generated by Gephi software were provided in Appendix B.
Qualitative data were analysed through a thematic analysis of qualitative data focussing on the themes of the collaboration process. We used open coding of transcripts to identify keywords, phrases, and statements. All researchers read each transcript and identified meaningful words, phrases, and patterns from the participant's responses through selective coding. Finally, responses were categorised into themes related to the five dimensions of collaboration. All quotes were extracted from individual interviews, and names are not shown to protect confidentiality.
2.5. Ethics statement
The study protocol was approved by institutional review boards at Seoul National University College of Medicine (IRB 1807‐177‐963). Study participation was voluntary and written informed consent in the local language (Mongolian) was obtained from all participants. Surveyors and interviewers trained in ethical matters collected all data.
3. RESULTS
3.1. Sample characteristics
Among the 28 medical staff who were listed in the team roster, 24 were available to participate in the study (85.7%). All available staff participated in the study (100%). Six respondents were men (five surgeons and an anaesthesiologist), and the rest were women, who were mostly nurses. The respondents' average age was 36 years at the time of the survey (n = 19, 5 of 24 were missing answers). The respondents were mostly married (66.7%) regardless of age. The average length of professional experience was 10.3 years, and approximately 40% had worked for more than 10 years (n = 23, 1 of 24 was missing an answer). The average length of experience in paediatric cardiac surgery and care was 8.3 years (n = 21, 3 of 24 were missing answers), and the average length of experience practicing in the current hospital was 11.5 years (n = 22, 2 of 24 were missing answers). All respondents indicated that they participated in at least one paediatric cardiac surgery‐related training programme. Roughly 41% of respondents had participated in a paediatric cardiac surgery‐related training programme at least three times. The average monthly salary of the respondents was about 670,000 MNT (equivalent to 236.06 USD) (Table 3).
TABLE 3.
Sample characteristics
| Demographic and professional characteristics (n = 24) | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 6 | 25.0 |
| Female | 18 | 75.0 |
| Age a | ||
| 25–35 | 8 | 42.1 |
| 35–50 | 11 | 57.9 |
| Marital status | ||
| Married | 16 | 66.7 |
| Single | 5 | 20.8 |
| Divorced | 3 | 12.5 |
| Years of experience in current profession a | ||
| < 5 years | 5 | 21.8 |
| 5–10 years | 9 | 39.1 |
| >10 years | 9 | 39.1 |
| Years of experience in paediatric cardiac surgery and care a | ||
| < 5 years | 8 | 38.1 |
| 5–10 years | 7 | 33.3 |
| >10 years | 6 | 28.6 |
| Years of experience in current hospital a | ||
| < 5 years | 3 | 13.6 |
| 5–10 years | 9 | 40.9 |
| >10 years | 10 | 45.5 |
| Number of trainings completed in paediatric cardiac surgery and care a | ||
| < 3 | 13 | 59.1 |
| 3–5 | 9 | 40.9 |
| Monthly salary a | ||
| < 600,000 MNT (equivalent to 211.39 USD) | 5 | 22.7 |
| 600,000–800,000 MNT | 11 | 50.0 |
| >800,000 MNT (equivalent to 281.86 USD) | 6 | 27.3 |
Due to missing answers, n size varies.
3.2. Structure
Figure 1 illustrates the overall network structure among Mongolian medical staff attending paediatric cardiac surgery.
FIGURE 1.
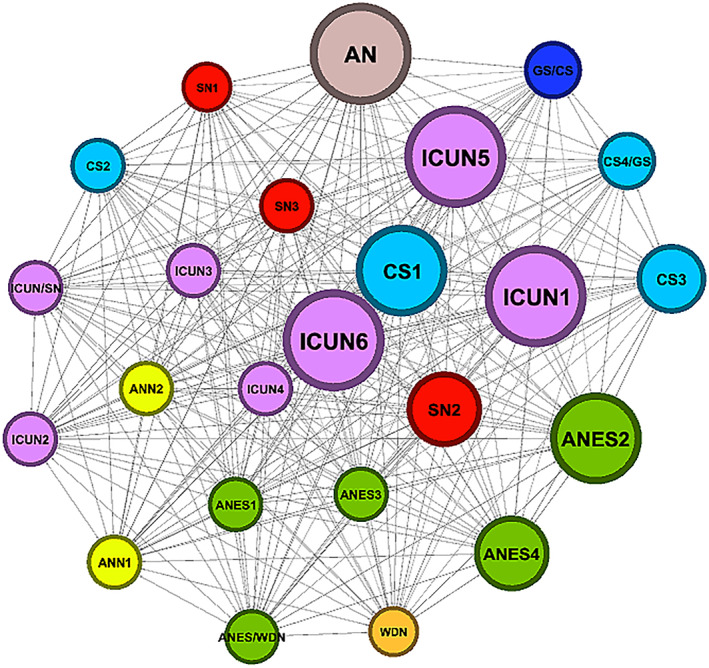
Sociogram of social network among Mongolian medical staff attending paediatric cardiac surgery in 2019 (n = 24). CS, cardiovascular surgeon; GS, general surgeon; ANES, anaesthesiologist; SN, scrub nurse; ICUN, ICU nurse; ANN, anaesthesiologist nurse; WDN, wounded dressing nurse; AN, assistant nurse; C, cardiologist. Note: The larger size of the circle denotes higher betweenness centrality, and the colour of the nodes are labelled according to the profession; We randomly assigned a number to an individual for distinction; The node labelled two professions by a slash mark indicates the person who dual positions, and the main profession is mentioned first
The total number of individuals in the network (nodes) was 24, and the number of the relationships between individuals (edges) was 506. The network density of the graph was high (0.917); since this value ranges from 0 to 1, a density of 0.917 means that most individuals reported communication with most others. Degree‐centrality was very low (8.7), as this measure ranges from 0 to 100 (Table 4). Betweenness‐centrality ranged from 0 to 7.83. Specifically, three ICU nurses (ICU 1,5,6) and the assistant nurse (AN1) had the highest betweenness‐centrality scores (7.83), whereas a wound dressing nurse (WDN) and a scrub nurse (SN1 presented the lowest scores (0) (Figure 2).
TABLE 4.
Characteristics of network structure (n = 24)
| Network structure | |
|---|---|
| Size | |
| Node | 24 |
| Edge | 506 |
| Density (0–1) | 0.917 |
| Degree‐centrality (0%–100%) | 8.7 |
FIGURE 2.
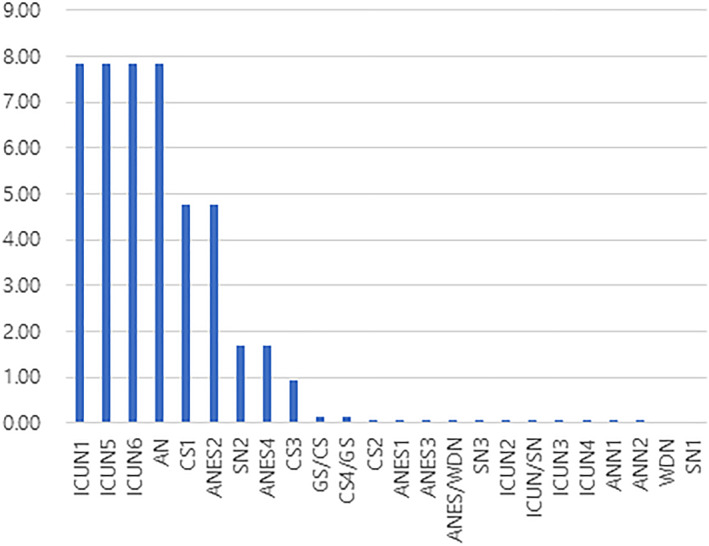
Betweenness‐centrality among Mongolian medical staff attending paediatric cardiac surgery in 2019 (n = 24). CS, cardiovascular surgeon; GS, general surgeon; ANES, anaesthesiologist; SN, scrub nurse; ICUN, ICU nurse; ANN, anaesthesiologist nurse; WDN, wounded dressing nurse; AN = assistant nurse
The interviews revealed that the ICU nurses often asked the surgeons, anaesthesiologists, or scrub nurses about patients because the surgeons did not provide information about patients' surgical outcomes, and the surgeons frequently asked the ICU nurses about patients' conditions.
It is rare for surgeons to talk to ICU nurses about the procedure after surgery. Instead, we get that information from the scrub nurse or the anaesthesiologists. (ICUN4)
In my case, I often communicate with nurses. Basically, in the morning, I ask nurses to get information about patients. Because nurses spend the most time in the hospital, they have a lot of information about patients. Sometimes, doctors often communicate through nurses when they cannot directly communicate due to their busy work. (CS4/GS)
3.3. Quality and process
3.3.1. Conceptual understanding of the ‘team’ and ‘teamwork’
Most medical staff recognised the importance of having a team for paediatric cardiac surgery and establishing good teamwork to have successful surgical outcomes. However, when we asked the respondents to indicate the team member(s) with whom they worked to achieve successful surgical outcomes, the answers varied significantly. For example, some participants were very inclusive, with responses encompassing non‐clinical staff such as cleaners or hospital administrators. Some had a narrower perception of the team according to their own professions and main tasks, and some did not perceive themselves as paediatric cardiac team members. Overall, one staff member mentioned that the staff were at the initial stage of understanding the concept of a paediatric cardiac surgery team and teamwork.
In Mongolia, the concept of teamwork is not established among medical staff. There are heart surgeons in this hospital, but neither anaesthesiologists, cardiopulmonary surgeons, nor ICU nurses know what a heart surgeon does. Everyone else doesn't know how he works. (CS1)
Next, we explored the medical staff's experiences and understanding of the team and teamwork according to the five dimensions of the collaboration process: governance, administration, autonomy, resource sharing, and trust‐building.
3.3.2. Governance: Joint decision‐making and common goal‐sharing process
The interviews revealed that, due to the lack of formal arenas for decision‐making and goal‐sharing processes, the medical staff did not have opportunities to discuss and share common visions, goals, and commitment to successful surgical outcomes. While regular meetings were held once a week, only doctors participated, and nurses had separate meetings once a week. These meetings did not function for joint decision‐making and discussions to share information on patients' conditions. Instead, these meetings were held to share superficial information on the patients and to receive last‐minute instructions from the team leader. Moreover, there was a lack of informal channels to communicate and share between medical staff.
The surgery team gathers every week and holds a meeting, but we superficially report on the number of operations performed and how many people have been treated. I want to share and discuss team members' experiences and opinions, but it is impossible. (ANES4)
Only on Tuesday, the ICU nurses, surgeons, and hospital managers can get together to talk. (ICUN/SN)
3.3.3. Administration: Clear role assignment and conflict resolution rules
Although the roles among the medical staff were obvious based on their assigned tasks, the explicit role assignment hindered close collaboration for successful surgical outcomes. For example, the medical staff tended to focus on their roles, not recognising other team members' tasks from a holistic perspective. For surgeons, surgery was their main and sole task; thus, they rarely engaged in postoperative tasks. For example, surgeons rarely provided information to the ICU nurses about the results of operations or patients' conditions. For this reason, some ICU nurses individually tried to obtain patients' information from scrub nurses or anaesthesiologists to provide more appropriate treatment.
As long as patients stay in the ICU, surgeons believe that caring for these patients is the sole responsibility of the ICU staff. (ICUN/SN)
In the ICU, […] the nurses provide all the care. Thus, we [ICU nurses] need more information about the patient's surgery to provide better care for the patient. For this reason, the nurses individually ask surgeons about the patient's surgical procedure and results, and try to get information about them. (ICUN4)
Another explanation for the lack of postoperative information‐sharing might be the lack of shared responsibility among medical staff regarding the surgical results. Still, only the surgeon who conducted surgery had final responsibility for the results due to their professions' articulated role assignments. Thus, the quality of care in the ICU depended on individuals' efforts and communication capacity.
Additionally, while working together in a team, there are inevitable conflicts, but there are few opportunities to have a conversation to resolve conflicts.
When we work together, conflicts are inevitable, I think. Thus, there needs to be an opportunity for us to understand each other, correct misunderstandings, and resolve conflicts through formal or informal meetings or communication channels. (CS2)
3.3.4. Autonomy: The balance between the goals of individuals and the hospital
Maintaining a balance between individuals' goals and the hospital's goals related to paediatric cardiac surgery was hard to achieve due to hospital‐imposed restrictions on decision‐making and team composition for surgery. For example, while some of the medical staff emphasised that the team should accumulate diverse experiences through performing complex surgical cases, the hospital forbade doing so due to concerns regarding surgical failures.
There is a lot of pressure [about surgery] from the hospital. For example, if we continue surgery, of course, there will be mistakes, risks, and many things can happen. If the patient dies, the hospital puts pressure on the surgeon to quit the hospital. (ANES4)
Other medical staff advised the hospital to restrict rotations of the staff, such as ICU nurses, who needed to continually collaborate as surgical team members for paediatric cardiac surgery, but this proposal was not accepted by the leadership of the hospital.
3.3.5. Sharing resources: Sharing information, advice, and knowledge among team members
Among the medical staff, timely and concrete information about the patients was commonly perceived as the most necessary and important knowledge to be shared. Most of the ICU nurses experienced substantial difficulties in effectively caring for patients due to their lack of knowledge about the patients' health conditions. Although some ICU nurses individually tried to acquire information about patients from the surgeons, the nurses emphasised the need to share more extensive information about patients postoperatively to provide appropriate care through an established system such as regular meetings.
It is hard to access information on how the operation went and the patient's condition. Yesterday, I just guessed the condition of a patient who moved into the ICU without knowing what kind of disease he was suffering from or how the operation was conducted. In this situation, it is challenging to determine how to care for the patient. (ICUN6)
3.3.6. Trust‐building: Mutual trust and respect among team members
Overall, the medical staff seemed to have strong mutual trust because most of them had worked together in this hospital for a long period. Some medical staff mentioned that participating in a team‐based fellowship abroad, in Korea, helped them understand and experience the concept of teamwork. Notably, the relationship between ICU nurses and anaesthesiologists was firmly based on established trust. This relationship was possible through the efforts of anaesthesiologists and nurses to regularly share and discuss patients' conditions.
We have been working together in the same operating room since 2013, so we have a good relationship. […] When I participated in training at Seoul National University Hospital and Yonsei University in the past, all four of my colleagues learnt the Korean team‐based surgical system just like learning the letters A, B, and C. Since we shared training experiences and learnt the Korean system together, we can collaborate based on mutual trust. (ANES4)
However, the medical staff of the paediatric cardiac surgery team tended to distrust the hospital administrators or leaders due to disagreements about teamwork issues and hospital management. As mentioned earlier, the study participants reported that while most cardiac surgery team members wanted to share their vision, goals, knowledge, and skills related to surgery with all members (including nurses) through the formal or informal channels, the leaders of the hospital refused to change the existing governance system. Currently, the paediatric cardiac surgery team exists without a formal structure.
3.4. Context
The interviewees emphasised a lack of support from the hospital for establishing and strengthening teamwork. As discussed earlier, regular meetings for discussions and joint decision‐making were not held by the hospital. Moreover, the hospital considered meetings to strengthen teamwork a waste of time.
The hospital can organise the schedule of team members. However, when I suggested times for team members to participate in a team meeting, the hospital administrator said, “Didn't you sign the labour contract? Keep working the proper hours.” (CS2)
4. DISCUSSION
This study provides insights into the structure, process, quality, and context of teamwork among the paediatric cardiac surgery team at a tertiary hospital in Mongolia. To our knowledge, this is the first investigation of a communication and collaboration network of a paediatric cardiac surgery team in an LMIC.
Using SNA, we found that the overall network size was 28; the density was high, but the degree‐centrality was low. This suggests that the network's structure cohesion is high, and individuals who are central to the structure tend to have little capacity to influence others. This can be explained by the inverse relationship between network density and degree‐centrality. 50 In addition, the ICU nurses had the highest betweenness‐centrality among all team members. This can be interpreted as showing that the ICU nurses played a crucial role in communicating to connect medical staff. This is not surprising, since prior research has indicated that nurses can play the roles of critical communicators in multidisciplinary teams in addition to communicating with patients and families. 51 The analysis of the teamwork process and quality showed that the team did not have opportunities to participate in joint decision‐making, share common goals or visions, or understand other members' tasks. While each members' role and task assignment were very explicit, there was no conflict resolution arrangement or rules in the team. The balance between each medical staff member's autonomy and the hospital's goals was not achieved due to the hospital's coercive control over when to perform surgery. Information about patients' health conditions or surgical outcomes was not shared between surgeons and ICU nurses due to their explicit role assignments. There were differences in perceived responsibility felt for patient outcomes among surgeons and nurses. While the medical staff's interpersonal relationships were generally intimate and trustworthy based on their common experiences and long‐term working periods, the relationship between the medical staff and the hospital administrators was conflicted.
Although the medical staff agreed with the importance of teamwork for successful surgical outcomes, during the interviews, we found that they did not have an established concept of a paediatric cardiac surgery team and teamwork. Nonetheless, we found that most of the respondents embraced the multidisciplinary nature of a team. Most of the respondents in our study perceived themselves as playing an important role in the team. The size of this paediatric cardiac surgery team was larger than the ideal number of 5 to 15 members that has been stated in the conceptual framework on medical team. 13 , 23 , 37 This may be why some nurses did not recognise themselves as team players. Therefore, providing education to share teamwork values and reducing the size of the team may increase the awareness of the team and improve the functionality of the team.
The survey results showed that the communication patterns of the team members were decentralised. Participants in the interviews elucidated that they yearned for a centralised network. This is in line with a recently published article demonstrating that surgical team members who were strategically core to the task achieved better goal attainment. 52 Although our SNA analysis revealed that the betweenness‐centrality was high among ICU nurses, which indicates that they seemed to be in control of communication within the team, the qualitative interviews explicated that the frequency of communication through the ICU nurses did not necessarily reflect high‐quality communication since inconsequential information was delivered to them.
The strong trust among team members seemed positive at the surface; however, the lack of a governance structure for the paediatric cardiac surgery team demonstrated the need for a structural and tangible organization of the team. Additionally, barriers to teamwork and communication included a lack of formal and informal communication channels, as well as a lack of open and joint decision‐making and goal‐sharing among the staff. The main communication channel was during formal meetings where the medical staff shared superficial information about patients. Additionally, due to the highly explicit role assignment among the medical staff, most were indifferent to each other's work. For example, surgeons rarely shared information about patients' conditions after surgery, and the ICU nurses felt that they were not fully informed to provide optimal care. The interviews also showed that physicians' satisfaction with teamwork was higher than nurses', which may be due to the hierarchical nature of the structures. 53 , 54 These results suggest that there is room for growth in multi‐professional teamwork and collaboration. Nevertheless, the results of this study document the need for a team‐based approach when building paediatric cardiac surgical capacity.
Since team‐based practice is a factor contributing to success in the improvement of paediatric cardiac surgical care and cardiac intensive programs, increased research focussing on improving teamwork for high‐quality care is needed. 55 Since perceived interdependence or teamwork can impact knowledge‐sharing and performance, 56 , 57 future interventions should reinforce the current structure of the team and improve communication practices with the local context in mind. For example, a 10‐year team‐based training programme in Uzbekistan to build paediatric cardiac surgical capacity among medical staff found that the training programme significantly increased team members' sharing goals for patients' health outcomes, as well as improved surgical outcomes. 9 Without comprehensive and sustainable training programs, paediatric cardiac surgery teams in LMICs will forgo opportunities to improve their engagement and efficiency.
This study has limitations. First, we inquired about the overall communication among the team members; however, this does not reflect communication during specific circumstances, such as when the team may work on challenging versus simpler cases. We were not able to survey and interview all members of the team, although we were able to recruit 24 out of the 28 team members. Additionally, our analysis did not include ward nurses, as they were not perceived as part of the paediatric cardiac surgery team; however, a future analysis should also explore relationships with other clinicians who may be part of patient's follow‐up after surgery. Finally, our analysis was confined to one team in Mongolia, and since there is considerable variation in organisational structure and staffing across hospitals, our results are not generalisable and should be interpreted with caution.
5. CONCLUSION
The findings revealed the importance of a holistic and in‐depth understanding of the communication structure, process and quality of collaboration, and hospital's organisational culture related to teamwork in order to increase teamwork effectiveness in paediatric cardiac surgery teams in LMICs. This study sheds light on how to make teamwork more effective for patient health outcomes. Future programme implementations and evaluations should take into account that teamwork‐building is not an easy process, and it is cyclical. It requires time, patience, resilience, and sustainability. 25 We recommend that future studies should establish a baseline network model and track the process longitudinally, using both quantitative and qualitative methods.
CONFLICT OF INTEREST
All authors have no conflicts of interest to declare.
ETHICAL APPROVAL
The study protocol was approved by institutional review boards at Seoul National University College of Medicine (IRB 1807‐177‐963). Study participation was voluntary and written informed consent in the local language (Mongolian) was obtained from all participants. Surveyors and interviewers trained in ethical matters collected all data.
AUTHOR CONTRIBUTIONS
Seungheon Han conceptualised and designed the study, and Woong‐Han Kim led programme management and supervision of field data collection. Seungheon Han, Jongho Heo and Jayoung Park contributed to field data collection, and Seoah Kweon analysed quantitative data and Seungheon Han analysed qualitative data. Seungheon Han, Sugy Choi, Jayoung Park, and Seoah Kweon wrote the initial draft. Seungheon Han and Sugy Choi were the major contributors in writing the manuscript. Jongho Heo, Woong‐Han Kim, Se Jin Oh, Holly B. Shakya provided critical comments. All authors provided revisions to the draft and approved the final manuscript.
Supporting information
Supporting Information S1
Table S1
ACKNOWLEDGEMENTS
We gratefully acknowledge the assistance of all research participants and colleagues involved in the pediatric cardiac surgery capacity‐building training program in Mongolia. The JW LEE Center for Global Medicine, Seoul National University College of Medicine, Seoul National University Boramae Medical Center funded the study.
Han S, Choi S, Park J, et al. The teamwork structure, process, and context of a paediatric cardiac surgery team in Mongolia: a mixed‐methods approach. Int J Health Plann Mgmt. 2022;37(4):2224‐2239. 10.1002/hpm.3463
Jongho Heo and Woong‐Han Kim contributed equally.
Contributor Information
Jongho Heo, Email: joheo@nafi.re.kr.
Woong‐Han Kim, Email: woonghan@snu.ac.kr.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta‐analysis. J Am Coll Cardiol. 2011;58(21):2241‐2247. [DOI] [PubMed] [Google Scholar]
- 2. Sitkin NA, Ozgediz D, Donkor P, Farmer DL. Congenital anomalies in low‐and middle‐income countries: the unborn child of global surgery. World J Surg. 2015;39(1):36‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Murala JS, Karl TR, Pezzella AT. Pediatric cardiac surgery in low and middle‐income countries: present status and need for a paradigm shift. Front pediatr. 2019;7:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vervoort D, Meuris B, Meyns B, Verbrugghe P. Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2020;159(3):987‐996. e6. [DOI] [PubMed] [Google Scholar]
- 5. Lingard L, Reznick R, Espin S, Regehr G, DeVito I. Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Acad Med. 2002;77(3):232‐237. [DOI] [PubMed] [Google Scholar]
- 6. Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiol Scand. 2009;53(2):143‐151. [DOI] [PubMed] [Google Scholar]
- 7. Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM. Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery. 2007;142(5):658‐665. [DOI] [PubMed] [Google Scholar]
- 8. Mundt MP, Agneessens F, Tuan W‐J, Zakletskaia LI, Kamnetz SA, Gilchrist VJ. Primary care team communication networks, team climate, quality of care, and medical costs for patients with diabetes: a cross‐sectional study. Int J Nurs Stud. 2016;58:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Han S, Choi S, Heo J, et al. Evaluation of a ten‐year team‐based collaborative capacity‐building program for pediatric cardiac surgery in Uzbekistan: lessons and implications. Annals of Global Health. 2020;86(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Creswick N, Westbrook JI. Who do hospital physicians and nurses go to for advice about medications? a social network analysis and examination of prescribing error rates. J patient Saf. 2015;11(3):152‐159. [DOI] [PubMed] [Google Scholar]
- 11. Grant MC, Hanna A, Benson A, et al. Dedicated operating room teams and clinical outcomes in an enhanced recovery after surgery pathway for colorectal surgery. J Am Coll Surg. 2018;226(3):267‐276. [DOI] [PubMed] [Google Scholar]
- 12. Siantz E, Rice E, Henwood B, Palinkas L. Where do peer providers fit into newly integrated mental health and primary care teams? A mixed method study. Adm Policy Ment Health Ment Health Serv Res. 2018;45(4):538‐549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meltzer D, Chung J, Khalili P, et al. Exploring the use of social network methods in designing healthcare quality improvement teams. Soc Sci Med. 2010;71(6):1119‐1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anderson C, Talsma A. Characterizing the structure of operating room staffing using social network analysis. Nurs Res. 2011;60(6):378‐385. [DOI] [PubMed] [Google Scholar]
- 15. Pinelli VA, Papp KK, Gonzalo JD. Interprofessional communication patterns during patient discharges: a social network analysis. J general Intern Med. 2015;30(9):1299‐1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Palazzolo M, Grippa F, Booth A, Rechner S, Bucuvalas J, Gloor P. Measuring social network structure of clinical teams caring for patients with complex conditions. Proc‐Soc Behav Sci. 2011;26(0):17‐29. [Google Scholar]
- 17. McGuire M, Silvia C. Does leadership in networks matter? Examining the effect of leadership behaviors on managers' perceptions of network effectiveness. Publ Perform Manag Rev. 2009;33(1):34‐62. [Google Scholar]
- 18. Newman ME. The structure of scientific collaboration networks. Proc Natl Acad Sci. 2001;98(2):404‐409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? Jama. 2004;291(10):1246‐1251. [DOI] [PubMed] [Google Scholar]
- 20. Hossian L, Wu A, Chung K. Actor centrality correlates to project based coordination. Paper presented at: Proceedings of the 2006 20th anniversary conference on Computer supported cooperative work. 4 November 2006. [Google Scholar]
- 21. Patel H, Pettitt M, Wilson JR. Factors of collaborative working: a framework for a collaboration model. Appl Ergon. 2012;43(1):1‐26. [DOI] [PubMed] [Google Scholar]
- 22. Thomson AM, Perry JL. Collaboration processes: inside the black box. Publ Adm Rev. 2006;66(s1):20‐32. [Google Scholar]
- 23. Thomson AM, Perry JL, Miller TK. Conceptualizing and measuring collaboration. J Public Adm Res Theory. 2009;19(1):23‐56. [Google Scholar]
- 24. Mickan SM, Rodger SA. Effective health care teams: a model of six characteristics developed from shared perceptions. J Interprofessional care. 2005;19(4):358‐370. [DOI] [PubMed] [Google Scholar]
- 25. Jünger S, Pestinger M, Elsner F, Krumm N, Radbruch L. Criteria for successful multiprofessional cooperation in palliative care teams. Palliat Med. 2007;21(4):347‐354. [DOI] [PubMed] [Google Scholar]
- 26. Bryson JM, Crosby BC, Stone MM. The design and implementation of Cross‐Sector collaborations: propositions from the literature. Publ Adm Rev. 2006;66(s1):44‐55. [Google Scholar]
- 27. Huxham C. Theorizing collaboration practice. Publ Manag Rev. 2003;5(3):401‐423. 10.1080/1471903032000146964 [DOI] [Google Scholar]
- 28. Huxham C, Vangen S. Managing to Collaborate: The Theory and Practice of Collaborative Advantage. Routledge; 2013. [Google Scholar]
- 29. Sabot K, Blanchet K, Berhanu D, et al. Professional advice for primary healthcare workers in Ethiopia: a social network analysis. BMC Health Serv Res. 2020;20(551):1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Salas E, Sims DE, Burke CS. Is there a “big five” in teamwork? Small Group Res. 2005;36(5):555‐599. [Google Scholar]
- 31. Estryn‐Béhar M, Van der Heijden BI, Ogińska H, et al. The impact of social work environment, teamwork characteristics, burnout, and personal factors upon intent to leave among European nurses. Med Care. 2007;45(10):939‐950. [DOI] [PubMed] [Google Scholar]
- 32. Chen B. Assesing interorganizational networks for public service delivery: a process‐perceived effectiveness framework. Publ Perform Manag Rev. 2008;31(3):348‐363. [Google Scholar]
- 33. Ostrom E. Governing the Commons: The Evolution of Institutions for Collective Action. Cambridge University Press; 1990. [Google Scholar]
- 34. Kalisch BJ, Lee H. Nursing teamwork, staff characteristics, work schedules, and staffing. Health Care Manag Rev. 2009;34(4):323‐333. [DOI] [PubMed] [Google Scholar]
- 35. Dahl AB, Abdallah AB, Maniar H, et al. Building a collaborative culture in cardiothoracic operating rooms: pre and postintervention study protocol for evaluation of the implementation of teamSTEPPS training and the impact on perceived psychological safety. BMJ open. 2017;7(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chan BC, Perkins D, Wan Q, et al. Finding common ground? Evaluating an intervention to improve teamwork among primary health‐care professionals. Int J Qual Health Care. 2010;22(6):519‐524. [DOI] [PubMed] [Google Scholar]
- 37. Deneckere S, Robyns N, Vanhaecht K, et al. Indicators for follow‐up of multidisciplinary teamwork in care processes: results of an international expert panel. Eval health Prof. 2011;34(3):258‐277. [DOI] [PubMed] [Google Scholar]
- 38. Sexton JB, Makary MA, Tersigni AR, et al. Teamwork in the operating roomfrontline perspectives among hospitals and operating room personnel. Anesthesiol J Am Soc Anesthesiol. 2006;105(5):877‐884. [DOI] [PubMed] [Google Scholar]
- 39. Provan KG, Kenis P. Modes of network governance: structure, management, and effectiveness. J public Adm Res theory. 2008;18(2):229‐252. [Google Scholar]
- 40. Graddy EA, Chen B. Influences on the size and scope of networks for social service delivery. J Public Adm Res Theory. 2006;16(4):533‐552. [Google Scholar]
- 41. Scott J. Social Network Analysis: A Handbook. 2nd ed. SAGE Publications; 2000. [Google Scholar]
- 42. Provan KG, Milward HB. A preliminary theory of interorganizational network effectiveness: a comparative study of four community mental health systems. Adm Sci Q. 1995;40(1):1‐33. [Google Scholar]
- 43. Thomson AM. Collaboration: Meaning and Measurement. Indiana University; 2002. [Google Scholar]
- 44. Shastin Hospital Mongolia. Accessed July 21, 2021. www.shastinhospital.mn. http://www.shastinhospital.mn/home/show/3/10/1 [Google Scholar]
- 45. Ulaanbaatar. Shastin Hospital. Statistics for; 2019. Accessed July, 2021. http://www.shastinhospital.mn/home/show/2289 [Google Scholar]
- 46. Choi S, Vervoort D, Kim W‐H. The role of cardiac surgery in global surgery and global health: a case study from Tashkent. J Global Health Reports. 2019;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for Social Network Analysis; 2002. [Google Scholar]
- 48. Freeman LC. Centrality in social networks conceptual clarification. Soc Netw. 1978;1(3):215‐239. [Google Scholar]
- 49. Bastian M, Heymann S, Jacomy M. Gephi: an open source software for exploring and manipulating networks. Icwsm. 2009;8:361‐362. [Google Scholar]
- 50. Wasserman S, Faust K. Social Network Analysis: Methods and Applications. Cambridge University Press; 1994. [Google Scholar]
- 51. Apker J, Propp KM, Ford WSZ, Hofmeister N. Collaboration, credibility, compassion, and coordination: professional nurse communication skill sets in health care team interactions. J Prof Nurs. 2006;22(3):180‐189. [DOI] [PubMed] [Google Scholar]
- 52. Pasarakonda S, Grote G, Schmutz JB, et al. A strategic core role perspective on team coordination: benefits of centralized leadership for managing task complexity in the operating room. Human Factors. 2020.0018720820906041. [DOI] [PubMed] [Google Scholar]
- 53. Alexanian JA, Kitto S, Rak KJ, Reeves S. Beyond the team: understanding interprofessional work in two North American ICUs. Crit Care Med. 2015;43(9):1880‐1886. [DOI] [PubMed] [Google Scholar]
- 54. Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav Int J Ind, Occup Organ Psychol Behav. 2006;27(7):941‐966. [Google Scholar]
- 55. Bastero P, Staveski SL, Zheleva B, et al. Partnership models for the establishment of sustainable paediatric cardiac surgical and cardiac intensive care programmes in low‐and middle‐income countries. Cardiol Young. 2017;27(S6):S55‐S60. [DOI] [PubMed] [Google Scholar]
- 56. Markon M‐P, Chiocchio F, Fleury M‐J. Modelling the effect of perceived interdependence among mental healthcare professionals on their work role performance. J Interprofessional Care. 2017;31(4):520‐528. [DOI] [PubMed] [Google Scholar]
- 57. Brown JB, Mulder C, Clark RE, Belsito L, Thorpe C. It starts with a strong foundation: constructing collaborative interprofessional teams in primary health care. J Interprofessional Care. 2021;35(4):514‐520. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Table S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


