Abstract
Objective
To assess the effect of vocal cordectomy on airflow across equine larynges at different Rakestraw grades of arytenoid abduction using a unidirectional airflow model.
Study design
Ex vivo, repeated measures.
Sample population
Twenty cadaveric equine larynges.
Methods
The right arytenoid cartilage was maximally abducted in all larynges. Each larynx was assigned a Rakestraw grade A or B, and the left arytenoid was abducted accordingly. Each larynx was tested under 3 conditions: intact, left vocal cordectomy (LVC), and bilateral vocal cordectomy (BVC). Translaryngeal pressure and airflow were measured, and digital video footage was obtained. Translaryngeal impedance (TLI) was calculated, and the arytenoid left‐to‐right quotient angle (LRQ) and rima glottis cross‐sectional area (CSA) were measured from standardized still images.
Results
Vocal cordectomy reduced TLI by 14.5% in LVC in comparison with intact larynges at Rakestraw grade B (P = .014). In Rakestraw grade A position, neither unilateral nor bilateral vocal cordectomy had any effect on TLI. Regardless of Rakestraw allocation, both LVC and BVC increased CSA in comparison with intact larynges (P < .005), with BVC larynges experiencing a greater effect than LVC (P < .0001).
Conclusion
Using a unilateral airflow model, LVC improved TLI in larynges where arytenoid position approximated Rakestraw grade B. However, when the arytenoid position approximated Rakestraw grade A, there was no effect on TLI following LVC or BVC.
Clinical significance
Surgeons considering a vocal cordectomy should take into account the degree of arytenoid abduction before performing the procedure, as it may not be warranted from a TLI point of view.
1. INTRODUCTION
Recurrent laryngeal neuropathy is a common, widespread, performance‐limiting peripheral nerve disease of horses. Degeneration of the recurrent laryngeal nerve (RLN) 1 causes neurogenic atrophy of the only intrinsic laryngeal abductor muscle, the cricoarytenoideus dorsalis (CAD) muscle. 2 The resultant arytenoid cartilage collapse (ACC) reduces airflow by a reduction in the rima glottis cross‐sectional area (CSA) and an increase in translaryngeal impedance (TLI). This is exacerbated most during exercise due to the high negative pressures present within the upper respiratory tract. 3 , 4 The condition is variable in prevalence among breeds with prior studies reporting 10% of thoroughbreds and up to 40% of draft horses affected. 5 , 6 , 7
Dynamic or exercising laryngeal function is evaluated using the Rakestraw grading system. 8 Horses with exercising Rakestraw grade A and most with grade B are not generally considered candidates for a laryngoplasty surgery. However, in some of these cases, one or both vocal cords can be noted to collapse independently of the corniculate process position. Horses with partial collapse (Rakestraw grade B) or horses with vocal cord collapse alone can be treated with ventriculocordectomy or vocal cordectomy. Tan et al. (2005) reported vocal cord collapse in conjunction with ACC in 22% of cases undergoing high‐speed treadmill evaluation. The same study also reported vocal‐cord collapse as the only upper respiratory tract (URT) abnormality in 5% of cases 9
Ventriculectomy, vocal cordectomy, or ventriculocordectomy are all commonly performed in clinical practice to improve airway function and may be performed either unilaterally or bilaterally. 10 , 11 , 12 Surgical removal of the vocal cord with or without the laryngeal saccule is reported to widen the ventral aspect of the rima glottis and decrease respiratory noise during exercise. 13 Although ventriculectomy improves respiratory noise, it is less effective at improving airway function than the ventriculocordectomy procedure. 12 , 14
It is well accepted that laryngoplasty is superior to ventriculocordectomy at improving airflow function in horses with ACC. 15 , 16 , 17 On the other hand, ventriculocordectomy reduces respiratory noise more effectively, is cheaper and less invasive to perform, and has a lower incidence of postoperative complications. 3 , 18 As such, in populations that perform at submaximal intensities (nonracing disciplines), removal of the vocal fold with or without the ventricle may be preferable to laryngoplasty.
In horses that have undergone a laryngoplasty, the decision to perform a unilateral or bilateral vocal cordectomy or a similar procedure is very common and has been performed historically under the same general anesthesia as the laryngoplasty. Recently, a treatment for post laryngoplasty dysphagia has been reported that bulks the remnant vocal cord following ventriculocordectomy or vocal cordectomy. 19 A less aggressive vocal cordectomy, preserving more tissue in the vocal cord region, or not performing a vocal cordectomy, has been considered by some surgeons as a method to reduce postoperative dysphagia. As a result, the benefit of performing a vocal cordectomy on CSA and TLI at different degrees of arytenoid position (Rakestraw grades) is an important factor to consider when deciding whether to perform a vocal cordectomy postoperatively. Furthermore, with the advent of standing laryngoplasty procedures, the degree of arytenoid abduction post laryngoplasty can be considered readily prior to performing vocal cordectomy. An understanding of the effect of a vocal cordectomy on airflow across larynges at different degrees of arytenoid abduction would enable surgeons to make a more objective decision regarding whether vocal cordectomy will be of clinical benefit.
Previous studies have demonstrated how both ventriculectomy and ventriculocordectomy alter respiratory noise. 3 , 4 , 14 , 20 However, there is currently no information on how airflow across the larynx is altered by vocal cordectomy (VC) (unilateral or bilateral) as a sole treatment. As such, this study attempts to quantify the effect on airway mechanics following unilateral and bilateral VC at 2 different Rakestraw grades (A and B).
We hypothesized that (1) compared to baseline, left vocal cordectomy (LVC) will reduce TLI; (2) a bilateral VC (BVC) will decrease TLI greater than a unilateral one (LVC), and (3) the effects of VC on TLI will be greater at Rakestraw B than A.
2. MATERIALS AND METHODS
2.1. Specimen preparation
Twenty grossly normal equine cadaveric larynges were collected from an abattoir, wrapped in 0.9% saline‐soaked gauze, and frozen at −20 °C. Larynges were thawed at 20 °C for 24 h before testing. Thawed larynges were wrapped again in saline‐soaked gauze to prevent drying of the tissues prior to testing. Soft‐tissue dissection was performed as previously described maintaining the intrinsic laryngeal musculature. 21 The cricoid length of each larynx was measured at the dorsal midline from cranial to caudal using calipers, and subsequently, the left CAD muscle was sharply transected caudal to its insertion on the muscular process of the arytenoid cartilage. Testing was performed on a single day in a temperature‐controlled laboratory.
2.2. Flow chamber
The larynx was mounted in a unidirectional vacuum system as described by Ahern et al. (2019) for testing. 21 Two vacuum/blowers (2400 W 230‐240 V 50 Hz, Ryobi, Japan), set on vacuum mode, controlled using a variable autotransformer (Powertech SRV‐5, Variac, Australia), and attached to an ergospirometer (Quadflow Equine Spirometry, QF, RobacScience Pty Ltd, Australia) were connected via a 50 mm PVC pipe to the testing chamber. Catheters, connected to a differential pressure transducer (Differential Pressure Transducer, Digitron, Rototherm Australia Pty Ltd, Australia), were positioned through airtight holes cranial to the larynx in the flow chamber (representative of pharyngeal pressure) and in the 50 mm PCV pipe immediately caudal to the flow chamber, level with the first tracheal ring (representative of tracheal pressure). Larynges were mounted in a uniform position within the flow chamber and affixed to the PVC pipe using cable ties, ensuring an airtight seal. The epiglottis was secured to the bottom of the flow chamber using an 18 gauge needle to prevent retroversion. A high‐definition digital camera (HC‐V250; Panasonic, Australia) was mounted above the inlet valve and focused on the rima glottidis.
2.3. Suture placement
Prior to testing, both the left and the right arytenoid cartilage were maximally abducted and fixed with Vicryl (Coated Vicryl 2 TP‐1 65 mm 1/2c, Ethicon, Summerville, NJ) using a standardized laryngoplasty technique. In brief, a #2 Vicryl suture on a trocar point ½ circle needle was passed through the right cricoid cartilage 0.5 cm lateral to the midline and 1 cm from the caudal edge without penetrating the laryngeal mucosa. The needle was subsequently passed through the muscular process of the right arytenoid cartilage in a caudodorsal‐to‐cranioventral direction approximately 30° from the frontal plane. The needle was removed, and the suture ends were tightened to maximal abduction and tied with 5 throws. The procedure was repeated on the left side but, rather than being tied, the suture ends were clamped using a Kelly hemostat to allow repositioning of the arytenoid cartilage following calibration. During calibration, the inlet valve and voltage regulator were adjusted such that a flow rate of 55 L/s and a prelaryngeal pressure of 12 mmHg was achieved, similar to previous studies. 21 , 22 , 23 , 24
Subsequently, the left prosthesis was loosened. Larynges were randomly assigned to either Rakestraw grade A or B and the left arytenoid was abducted accordingly. Random allocation was performed using a coin toss and the degree of adduction was standardized as much as possible. In the first instance, the suture ends were clamped using a Kelly hemostat. The left‐to‐right quotient angle ratio (LRQ) was calculated from a digital photograph, and once an adequate value was confirmed, the suture ends were tied for the remainder of testing. A target LRQ for Rakestraw A and Rakestraw B larynges was 0.88 and 0.65 respectively; 8 however, values of 0.85‐0.95 and 0.6‐0.7 were considered acceptable. Photographic control was used to obtain LRQ ratios and position the left arytenoid cartilage. A Vicryl prosthesis (Coated Vicryl 2 TP‐1 65 mm 1/2c; Ethicon) was used throughout the study.
Each larynx underwent sequential testing of 3 states: intact, unilateral (LVC), and bilateral (BVC) vocal cordectomy under static (inspiratory) airflow conditions at 55 L/s. 25 During airflow testing, data, including airflow and translaryngeal pressure, were collected, and a high‐definition digital video using a high‐definition digital camera (HC‐V250; Panasonic) was obtained simultaneously over a standardized 5 s period. A still image was obtained at 2.5 s and the data averaged for analysis. All data collection and calculations were performed using Microsoft Excel.
2.4. Vocal cordectomy
The vocal cord was grasped using Kelly hemostatic forceps parallel and abaxial to the leading edge and a crescent‐shaped wedge of tissue excised using curved Metzenbaum scissors in a ventral to dorsal direction. For consistency, the entire vocal cord was excised. Care was taken not to perforate the laryngeal mucosa during the procedure (Figure 1). All VC procedures were performed by a single investigator (NL).
FIGURE 1.
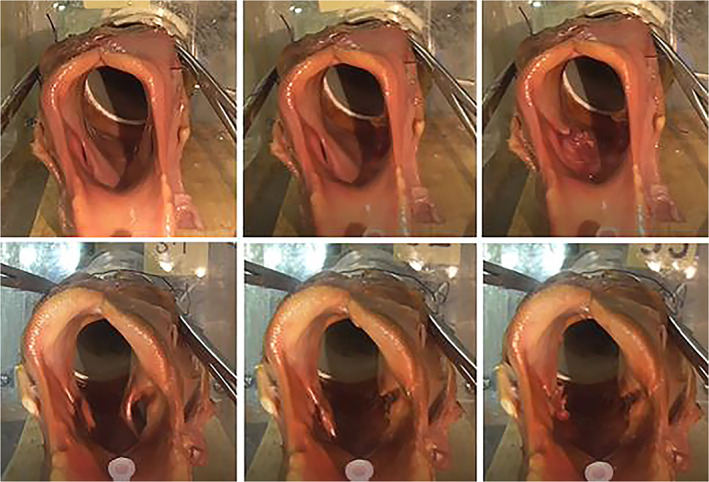
Digital images of the 3 examined states during flow testing: intact (left), unilateral vocal cordectomy (center), and bilateral vocal cordectomy (right) of a representative Rakestraw grade A (top) and grade B (bottom) larynx.
2.5. Measured variables
2.6. Translaryngeal impedance
An ergospirometer (RobacScience Pty Ltd) positioned between the larynx and the vacuum was used to measure airflow (L/s). Calibration was performed as previously described. 26 Calibrations were performed at 0 L/s and 55 L/s flow using an orifice plate. Barometric pressure, relative humidity, and ambient temperature were also calibrated as per Quadflow requirements (Testo 06362135 humidity/temperature probe; Testo Pty Ltd, Australia). Prelaryngeal and tracheal catheters (positioned immediately cranial to the larynx and at the first tracheal ring respectively) were connected to a differential pressure transducer (Digitron) and calibrated to a prelaryngeal pressure of 12 mmHg using a handheld manometer. Translaryngeal pressure readings were recorded every second during testing. Translaryngeal impedance (mmHg/L/s) was calculated by dividing the mean translaryngeal differential pressure by the mean airflow.
2.7. Left to right quotient angle
The arytenoid left‐to‐right quotient angle (LRQ) ratio was measured and calculated using a software package (Image J) as previously validated. 25 , 27 In short, a line was drawn from the ventral to dorsal aspect of the rima glottidis and extended by a third to give a point that was used to measure the left (L°) and right (R°) arytenoid angles. The LRQ was then calculated by dividing L° by R°.
2.8. Cross‐sectional area
Using the Image J freehand draw icon, the circumference of the rima glottidis was measured and the cross‐sectional area calculated. The left to right quotient angle ratio and cross‐sectional area (CSA) measurements were obtained for each state using still video images obtained during testing. All measurements were performed by a single investigator (NL).
2.9. Statistical analysis
Data distribution was assessed by a Shapiro‐Wilk test. Normally distributed data are reported as mean ± standard deviation (SD) and data that were not normally distributed are reported as median and range. The effects of Rakestraw grade (grade A or grade B) and the effect of VC (intact, LVC and BVC) on TLI, LRQ, and CSA were assessed by a 2‐way‐repeated measures factorial analysis of variance with post hoc Tukey tests performed when appropriate. Statistical analysis was performed using commercially available software (GraphPad Prism 9, GraphPad Software, Inc, San Diego, California; MedCalc Software bvba, Belgium) and P ≤ .05 was considered statistically significant. Pearson correlation matrices were also created for Rakestraw grades A and B under the 3 different states (intact, left, and bilateral VC) to detect clinically relevant correlations between continuous variables (cricoid length, flow, translaryngeal pressure, pharyngeal pressure, tracheal pressure, impedance, LRQ, and CSA).
3. RESULTS
All specimens completed testing between 24 and 32 h after removal from the freezer. Subjectively, tissue pliability was effectively maintained following thawing and all testing and data collection was performed without complication. All data were normally distributed and, as expected, for all comparisons, there was an effect of subject (P < .0001). There was an effect of Rakestraw grade (P < .0001) on LRQ; however, there was no effect of VC (P = .168) nor was there a Rakestraw grade × VC effect (P = .8) on LRQ.
There was a effect of both Rakestraw grade (P = .0055) and VC (P < .001) on CSA, but no Rakestraw grade × VC effect (P = .56), with lower CSA in Rakestraw grade B larynges in comparison with Rakestraw grade A larynges in all 3 states; intact (Rakestraw A; 54.94 mm2 ± 11.21 mm2, Rakestraw B; 42.61 mm2 ± 8.90 mm2, P = .05), LVC (Rakestraw A; 59.27 mm2 ± 10.36 mm2, Rakestraw B; 45.90 mm2 ± 8.21 mm2, P = .02), and BVC (Rakestraw A; 64.35 mm2 ± 10.80 mm2, Rakestraw B; 50.58 mm2 ± 7.45 mm2, P = .018); however, all coefficients of variation were similar. Regardless of Rakestraw grade, VC increased the CSA of LVC larynges in comparison with intact (7.8%, P = .005), BVC larynges in comparison with intact (17.9%, P < .001) and BVC larynges in comparison with LVC larynges (10.1%, P < .001) (Figure 2).
FIGURE 2.
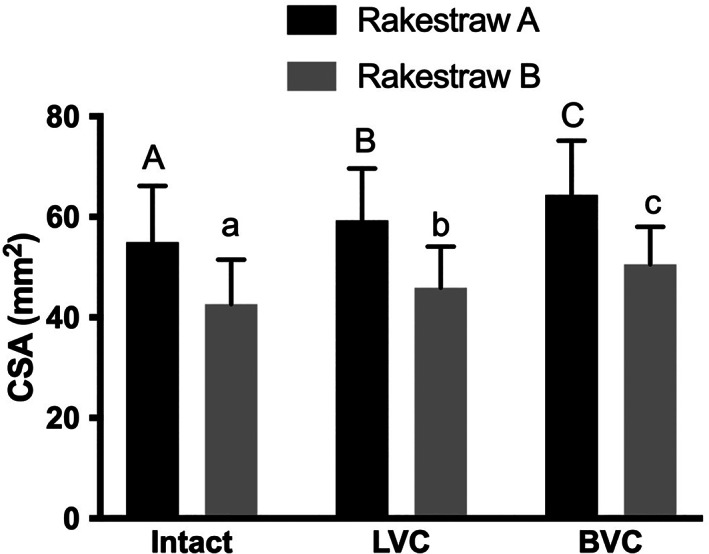
Cross‐sectional area (CSA) (mean ± standard deviation) of Rakestraw grade A and grade B larynges for intact, left ventriculocordectomy (LVC), and bilateral ventriculocordectomy (BVC) states. Regardless of Rakestraw allocation, both LVC and BVC increased CSA in comparison with intact larynges, with BVC larynges having a greater effect than LVC. Capitalized letters denote differences between Rakestraw grade A larynges, and uncapitalized letters denote differences between Rakestraw grade B larynges. Different letters indicate P < .05.
There was no effect of Rakestraw grade on TLI (P = .24); however, an effect of VC was detected (P = .032) with a reduction in TLI only detected in Rakestraw grade B larynges, with an LVC reduced TLI by 14.5% in comparison with intact larynges (intact; 0.12 mmHg/L/s ± 0.04 mmHg/L/s LVC; 0.1 mmHg/L/s ± 0.02 mmHg/L/s; P = .014). Bilateral VC did not result in a difference for TLI in comparison with intact (P = .08) (Figure 3). There was no Rakestraw grade × VC effect (P = .37) on TLI.
FIGURE 3.
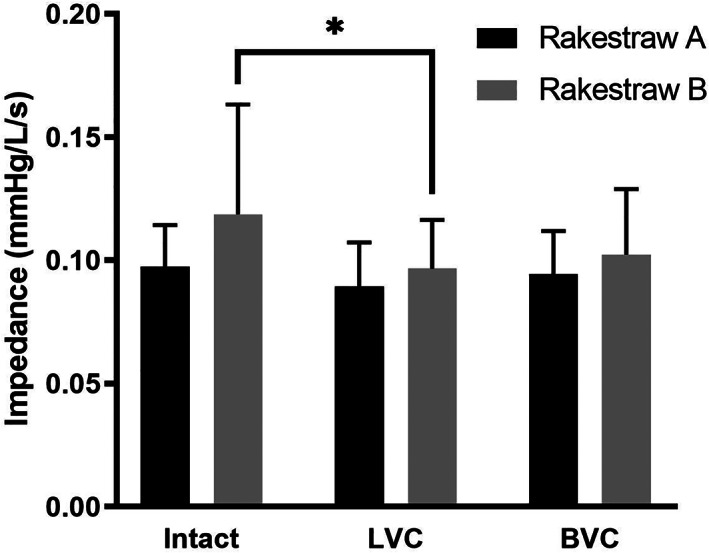
Translaryngeal impedance (TLI) (mean ± standard deviation) of Rakestraw grade A and grade B larynges for each of the 3 intervention states: intact, left ventriculocordectomy (LVC), and bilateral ventriculocordectomy (BVC). In grade A larynges, compared to intact there was no difference in TLI following either LVC or BVC. In grade B larynges, compared to intact, TLI was reduced following LVC but not BVC. Asterisk (*) indicates P < .05.
Pearson correlations confirmed associations between flow, pharyngeal pressure, tracheal pressure, TLI, and CSA (data provided in Table S1).
4. DISCUSSION
Regardless of Rakestraw grade, a unilateral (left) vocal cordectomy increased the rima glottis cross‐sectional area as compared with that of intact larynges, and a bilateral vocal cordectomy further increased the cross‐sectional area as compared with unilateral vocal cordectomy. Nevertheless, translaryngeal impedance was only reduced following a unilateral vocal cordectomy in Rakestraw grade B larynges. As hypothesized, the effects of vocal cordectomy on translaryngeal impedance were greater in Rakestraw grade B larynges as compared with Rakestraw grade A larynges. However, in contrast to our hypothesis, a bilateral vocal cordectomy did not decrease translaryngeal impedance to a greater extent than a unilateral vocal cordectomy. In fact, no difference in TLI was demonstrated between intact larynges and those that had undergone bilateral vocal cordectomy (Figure 3). The reason for this is unclear. The authors speculate that the handling and replacement of specimens between tests, and the previous airflow testing, may be responsible for the increased impedance through tissue relaxation or increased variance, which is evidenced by the higher standard deviation following laryngeal repositioning for BVC testing. Potentially at higher airflow rates where there is increased vocal fold collapse, a BVC may be beneficial compared to an LVC alone. However this is speculation and requires further investigation. Based on our results and assuming a power of 0.8, a sample of 8 larynges per group was required to detect a significant difference, suggesting that, at n = 10/group, the experiment was adequately powered. However, the nature of the study, being ex vivo, might have limited our ability to detect a significant difference warranting additional studies to further investigate the effects of performing a unilateral or bilateral vocal cordectomy.
At Rakestraw grade A, TLI did not change following either LVC or BVC. A likely explanation for this is that, at full abduction, the first tracheal ring is the most influential site of impedance to airflow and not the rima glottis. 28 Another possible factor may be the variations in tension on the vocal cord at different Rakestraw grades of arytenoid cartilage abduction. Perkins et al. (2011) demonstrated that, as arytenoid abduction increases, the counter tension on the vocal cord also increases. As such, the vocal cords of grade A larynges may have more resistance to collapse during exercise, leading to less impedance at grade A than grade B. 25 These results suggest that performing a vocal cordectomy may be of no additional benefit in horses with arytenoid positioning approximating Rakestraw grade A post prosthetic laryngoplasty, as impedance and therefore airflow will not be further improved. Moreover, retaining the vocal fold may reduce tracheal aspiration if postoperative dysphagia occurs.
Nonetheless, the improvement in TLI in Rakestraw grade B larynges following LVC and not BVC suggests that a bilateral VC may not be warranted over unilateral to improve airflow based on the airflow conditions of this model. One reason to avoid performing a bilateral VC is the risk of cicatrix formation or “laryngeal webbing” at the ventral aspect of the rima glottis. Some surgeons elect to perform a bilateral cordectomy but retain the ventral aspect of the vocal cord. By not excising the ventral portion, laryngeal webbing can be avoided, 14 and there is some protection against dysphagia, which can occur following an aggressive VC. 19 However, the retained vocal cord tissue will not be under tension and will likely cause turbulent airflow during exercise. From a clinical standpoint, it is also worth considering that a unilateral VC can be readily performed using a laser during a standing endoscopic procedure. Conversely, bilateral VC is more commonly performed via a more invasive laryngotomy approach. It is important to acknowledge that the effects of VC may differ when performed using laser versus sharp dissection.
Jansson et al. (2000) reported on the effects of left cordopexy, laryngoplasty, and laryngoplasty with left cordopexy in an ex vivo laryngeal hemiplegic model. 24 They found that both CSA and TLI were not different in larynges that had undergone both laryngoplasty and cordopexy in comparison with just a laryngoplasty. Even though cordopexy, not cordectomy, was performed, this agrees with the findings of the present study, where LVC did not improve TLI of Rakestraw grade A larynges.
In the present study, VC had no effect on LRQ for either Rakestraw grade. However, the lack of muscular function in cadaver larynges may produce results different from those found in vivo. In horses with low‐grade RLN that have not undergone laryngoplasty, neuromuscular fatigue during exercise can cause progressive loss of abduction without the prosthesis to maintain the cartilage's position. As such, the effect of VC in exercising horses who have undergone laryngoplasty but have either Rakestraw grade B arytenoid abduction, or vocal fold collapse, despite Rakestraw grade A arytenoid abduction, requires additional investigation.
A major limitation of ex vivo airflow testing models is that the flow conditions that are used often do not directly correlate with in vivo conditions, which can vary widely. The flow rate of 55 L/s used in this study is similar to that of previous publications that used unidirectional airflow models. 21 , 22 This is approximately 75% of the VO2max and greater than 75% but less than 100% HRmax in an exercising horse. 22 , 26 However, respiratory airflows of 75 L/s have been recorded in maximally exercising populations. 22 It is currently unknown if, at higher flow rates, bilateral VC will reduce TLI more effectively than unilateral VC. Furthermore, while this and similar airflow models have been used extensively in ex vivo airflow studies, they provide only a crude replication of the dynamic turbulent airflow in exercising horses and simulate only inspiration. Using a computational flow model, Rakesh and colleagues demonstrated that larynges with greater than or equal to 25% left ACC also experience concurrent right aryepiglottic fold and bilateral vocal fold collapse. 28 In horses with grade B ACC, it is therefore possible that a right AEF resection could be beneficial in addition to a VC resection, although our model did not demonstrate any obvious right AEF collapse.
Vocal cordectomy was used in this study because of its frequent use in practice and relative ease of performance. However, the effect of ventriculocordectomy relative to vocal cordectomy in a clinical setting is unknown. Anecdotally, vocal cordectomy appears to have a comparable effect to ventriculocordectomy but this may be due to tissue retraction and the formation of scar tissue. Scar tissue is more fibrous and less elastic, and thus less susceptible to collapse. The process of healing may also obliterate the opening to the ventricle. The ventricles were not sealed following VC in this study, which more closely replicates the short‐term postoperative period. It is possible that, in vivo, a further small reduction in TLI compared to that demonstrated here may occur following healing due to the elimination of airflow into the saccule of the ventricle and remodeling of the mucosa.
Consideration was given to the small sample size and inherent ex vivo limitations of the study. Although attempts were made to reduce the loss of moisture from the tissues during testing, a degree of drying may have occurred. The larynges used in the study were obtained from an abattoir postslaughter. Although no antemortem information on signalment or respiratory function was available, the muscle and cartilaginous structures were all deemed to be grossly normal before inclusion. In addition, all larynges were required to fit the construct (5 cm tracheal attachment) without adaptation and therefore were likely to have been derived from adult horses. As there was no association of cricoid cartilage length with any of the measured variables we can rationalize that the laryngeal size was appropriate to allow effective airtight instrumentation without the interference of the soft tissues.
The results demonstrated that using an ex vivo unilateral airflow model, unilateral LVC improves inspiratory TLI in larynges with arytenoid cartilage positioning equivalent of a Rakestraw grade B. Vocal cordectomy appears to provide no additional benefit to airflow in cases with Rakestraw grade A arytenoid positioning. Based on these findings, clinicians may consider performing a unilateral left vocal cordectomy in cases with Rakestraw grade B arytenoid abduction, or after partial loss of abduction following prosthetic laryngoplasty. Further research at higher flow rates, in more severe ACC grades (Rakestraw grade C or D) and in vivo are required to determine the clinical effect of VC on airflow mechanics in maximally exercising horses.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this report.
Supporting information
Appendix S1 Supporting Information
ACKNOWLEDGMENTS
Author Contributions:Lean NE, DVM, DVClinSci, DACVS: Obtained specimens, performed testing, managed the data and prepared the manuscript. Bertin FR, DVM, MS, Ph.D., DACVIM (LAIM): Performed all statistical analysis, prepared figures for the manuscript and reviewed the manuscript. Ahern BJ, BVSc, Ph.D., DACVS, DACVSMR: Conceived and designed the study, performed testing, and reviewed the manuscript.
Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Lean NE, Bertin FR, Ahern BJ. Influence of unilateral and bilateral vocal cordectomy on airflow across cadaveric equine larynges at different Rakestraw grades of arytenoid abduction. Veterinary Surgery. 2022;51(6):974‐981. doi: 10.1111/vsu.13823
The preliminary results of this work were presented as a poster at the ACVS Surgery Summit, October 11‐14, 2017, Indianapolis, USA.
Funding informationNo financial support was received.
REFERENCES
- 1. Hahn C, Matiasek K, Dixon P, Molony V, Rodenacker K, Mayhew I. Histological and ultrastructural evidence that recurrent laryngeal neuropathy is a bilateral mononeuropathy limited to recurrent laryngeal nerves. Equine Vet J. 2008;40:666‐672. [DOI] [PubMed] [Google Scholar]
- 2. Cahill JI, Goulden BE. The pathogenesis of equine laryngeal hemiplegia‐a review. N Z Vet J. 1987;35:82‐90. [DOI] [PubMed] [Google Scholar]
- 3. Brown JA, Derksen FJ, Stick JA, Hartmann WM, Robinson NE. Ventriculocordectomy reduces respiratory noise in horses with laryngeal hemiplegia. Equine Vet J. 2003;35:570‐574. [DOI] [PubMed] [Google Scholar]
- 4. Robinson P, Derksen FJ, Stick JA, Sullins KE, DeTolve PG, Robinson NE. Effects of unilateral laser‐assisted ventriculocordectomy in horses with laryngeal hemiplegia. Equine Vet J. 2006;38:491‐496. [DOI] [PubMed] [Google Scholar]
- 5. Dixon PM, McGorum BC, Railton DI, et al. Laryngeal paralysis: a study of 375 cases in a mixed‐breed population of horses. Equine Vet J. 2001;33:452‐458. [DOI] [PubMed] [Google Scholar]
- 6. Brakenhoff JE, Holcombe SJ, Hauptman JG, Smith HK, Nickels FA, Caron JP. The prevalence of laryngeal disease in a large population of competition draft horses. Vet Surg. 2006;35:579‐583. [DOI] [PubMed] [Google Scholar]
- 7. McClellan NR, Santschi EM, Hurcombe SD, Litsky AS. An ex vivo model to evaluate the effect of cyclical adductory forces on maintenance of arytenoid abduction after prosthetic laryngoplasty performed with and without mechanical arytenoid abduction. Vet Surg. 2014;43:598‐605. [DOI] [PubMed] [Google Scholar]
- 8. Rakestraw PC, Hackett RP, Ducharme NG, Nielan GJ, Erb HN. Arytenoid cartilage movement in resting and exercising horses. Vet Surg. 1991;20:122‐127. [DOI] [PubMed] [Google Scholar]
- 9. Tan RH, Dowling BA, Dart AJ. High‐speed treadmill videoendoscopic examination of the upper respiratory tract in the horse: the results of 291 clinical cases. Vet J. 2005;170:243‐248. [DOI] [PubMed] [Google Scholar]
- 10. Dixon RM, McGorum BC, Railton DI, et al. Long‐term survey of laryngoplasty and ventriculocordectomy in an older, mixed‐breed population of 200 horses. Part 1: maintenance of surgical arytenoid abduction and complications of surgery. Equine Vet J. 2003;35:389‐396. [DOI] [PubMed] [Google Scholar]
- 11. Tetens J, Derksen FJ, Stick JA, Lloyd JW, Robinson NE. Efficacy of prosthetic laryngoplasty with and without bilateral ventriculocordectomy as treatments for laryngeal hemiplegia in horses. Am J Vet Res. 1996;57:1668‐1673. [PubMed] [Google Scholar]
- 12. Kraus BM, Parente EJ, Tulleners EP. Laryngoplasty with ventriculectomy or ventriculocordectomy in 104 draft horses (1992‐2000). Vet Surg. 2003;32:530‐538. [DOI] [PubMed] [Google Scholar]
- 13. Hawkins J. Laser Ventriculocordectomy. Hawkins J, Advances in Equine Upper Respiratory Surgery. ACVS Foundation; 2015:21‐27. [Google Scholar]
- 14. Cramp P, Derksen FJ, Stick JA, et al. Effect of ventriculectomy versus ventriculocordectomy on upper airway noise in draught horses with recurrent laryngeal neuropathy. Equine Vet J. 2009;41:729‐734. [DOI] [PubMed] [Google Scholar]
- 15. Derksen FJ, Stick JA, Scott EA, Robinson NE, Slocombe RF. Effect of laryngeal hemiplegia and laryngoplasty on airway flow mechanics in exercising horses. Am J Vet Res. 1986;47:16‐20. [PubMed] [Google Scholar]
- 16. Shappell KK, Derksen FJ, Stick JA, Robinson NE. Effects of ventriculectomy, prosthetic laryngoplasty, and exercise on upper airway function in horses with induced left laryngeal hemiplegia. Am J Vet Res. 1988;49:1760‐1765. [PubMed] [Google Scholar]
- 17. Williams JW, Pascoe JR, Meagher DM, Hornof WJ. Effects of left recurrent laryngeal neurectomy, prosthetic laryngoplasty, and subtotal arytenoidectomy on upper airway pressure during maximal exertion. Vet Surg. 1990;19:136‐141. [DOI] [PubMed] [Google Scholar]
- 18. Brown JA, Derksen FJ, Stick JA, Hartmann WM, Robinson NE. Effect of laryngoplasty on respiratory noise reduction in horses with laryngeal hemiplegia. Equine Vet J. 2004;36:420‐425. [DOI] [PubMed] [Google Scholar]
- 19. Luedke LK, Cheetham J, Mohammed HO, Ducharme NG. Management of postoperative dysphagia after prosthetic laryngoplasty or arytenoidectomy. Vet Surg. 2020;49:529‐539. [DOI] [PubMed] [Google Scholar]
- 20. Barnett TP, O'Leary JM, Parkin TD, Dixon PM, Barakzai SZ. Long‐term exercising video‐endoscopic examination of the upper airway following laryngoplasty surgery: a prospective cross‐sectional study of 41 horses. Equine Vet J. 2013;45:593‐597. [DOI] [PubMed] [Google Scholar]
- 21. Ahern BJ, Lukas E, Lam K, et al. Evaluation of a prototype dynamic laryngoplasty system in vitro with an equine vacuum airflow system. Vet Surg. 2019;48:173‐179. [DOI] [PubMed] [Google Scholar]
- 22. Cheetham J, Witte T, Soderholm L, Hermanson J, Ducharme N. In vitro model for testing novel implants for equine laryngoplasty. Vet Surg. 2008;37:588‐593. [DOI] [PubMed] [Google Scholar]
- 23. Hawkins JF, Couetil L, Miller MA. Maintenance of arytenoid abduction following carbon dioxide laser debridement of the articular cartilage and joint capsule of the cricoarytenoid joint combined with prosthetic laryngoplasty in horses: an in vivo and in vitro study. Vet J. 2014;199:275‐280. [DOI] [PubMed] [Google Scholar]
- 24. Jansson N, Ducharme NG, Hackett RP, Mohammed HO. An in vitro comparison of cordopexy, cordopexy and laryngoplasty, and laryngoplasty for treatment of equine laryngeal hemiplegia. Vet Surg. 2000;29:326‐334. [DOI] [PubMed] [Google Scholar]
- 25. Perkins JD, Meighan H, Windley Z, Troester S, Piercy R, Schumacher J. In vitro effect of ventriculocordectomy before laryngoplasty on abduction of the equine arytenoid cartilage. Vet Surg. 2011;40:305‐310. [DOI] [PubMed] [Google Scholar]
- 26. Curtis RA, Kusano K, Evans DL, Lovell NH, Hodgson DR. Reliability of cardiorespiratory measurements with a new ergospirometer during intense treadmill exercise in thoroughbred horses. Vet J. 2005;169:223‐231. [DOI] [PubMed] [Google Scholar]
- 27. Leutton JL, Lumsden JM. Dynamic respiratory endoscopic findings pre‐ and post laryngoplasty in thoroughbred racehorses. Equine Vet J. 2015;47:531‐536. [DOI] [PubMed] [Google Scholar]
- 28. Rakesh V, Ducharme NG, Cheetham J, Datta AK, Pease AP. Implications of different degrees of arytenoid cartilage abduction on equine upper airway characteristics. Equine Vet J. 2008;40:629‐635. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information


