Abstract
Aim
To analyze and examine the concept of exclusive breast pumping (EP).
Background
Breastmilk is the ideal nutrition for infants, yet when breastfeeding is unsuccessful, parents resort to informal breastmilk sharing, artificial formula feeding, or EP. A growing proportion of families exclusively pump yet they often receive guidance from social media rather than healthcare providers because healthcare providers are uninformed about this feeding method.
Data Source
Cumulative Index of Nursing and Allied Health Literature, PubMed, and Google Scholar databases were searched using the following keywords: human milk express*, breast express*, breast milk express, breastmilk express*, exclusive pump, exclusive breast pumping, and exclusive expression.
Review Methods
Concept analysis design using Walker and Avant's method.
Results
Three defining attributes of (1) absence of direct breastfeeding, (2) breastmilk expression, (3) and an enduring infant feeding pattern of feeding expressed breastmilk only via a bottle were identified. All three attributes are required to confirm the presence of the concept of exclusive pumping. Definitions, antecedents, consequences, and empirical referents are described. Model and contrary cases are discussed.
Conclusion
This exclusive pumping concept analysis allows for consistency in terminology in practice and research. EP is a feeding method which can increase the proportion of infants who are fed breastmilk and may reduce the risks that arise from artificial formula feeding.
Keywords: concept analysis, family nursing, maternal‐child health, perinatal, women's health
1. INTRODUCTION
Infant feeding is usually described as breastfeeding (i.e., direct feeding at the breast), formula feeding, or combination feeding which includes both approaches. There is a new approach to infant feeding called exclusive breastmilk expression, which is when a person pumps breastmilk and the infant consumes breastmilk only from a bottle. In the last 10 years, there has been a growing proportion of families who feed their infants by exclusive breastmilk expression. These families, commonly known as exclusive pumpers (EPers) or parents exclusively pumping (EP), have different concerns, information needs, and outcomes compared to families who formula feed or directly breastfeed. Among American families who feed their infants breastmilk, between 5.6% and 14.3% were EP within the first 6 months. 1 , 2 , 3 The prevalence of EP was higher in Asian countries among families choosing to breastfeed, with such regional variations as 5.1%–19.8% in Hong Kong, 22.6% in China, and 26.5% in Singapore. 4 , 5 , 6 In this concept analysis, EP will be defined as an infant only receiving expressed breastmilk via a bottle. The infant may be solely breastmilk fed or may receive both breastmilk and artificial formula. Direct breastfeeding will be defined as an infant receiving breastmilk from directly latching onto a person's breast with or without supplementation of pumped breastmilk.
There are many reasons that may lead parents to consider EP. For example, pumping may have started when an infant was hospitalized in the neonatal intensive care unit and the parents are encouraged to provide breastmilk. 1 , 7 , 8 Or pumping may have been proposed as a possible short‐term solution following problems with direct breastfeeding, such as the infant's inability to latch, transfer milk effectively, accept the breast, or parents needing/wanting to monitor intake. 5 , 9 , 10 Over 89% of EP parents chose to exclusively pump only after unsuccessful attempts at direct breastfeeding. 10 A case report of an EP family showed a client who attempted to directly breastfeed before every pumping session for 2 months before deciding to exclusively pump. 11 Parents reported feeling “heartbroken” or needing to cope with the grief of being unable to directly breastfeed or transition to direct breastfeeding. 7 , 9 For whatever reason, when their original plan of direct breastfeeding was unsuccessful, they adapt and decide to exclusively pump to help the infant receive the benefits of breastmilk. 9 There are parents whose first choice was EP, but they are in the minority. 10 , 12 However, EP, as a relatively new concept, may have been influenced by the availability of high‐quality breast pumps, families returning to work before the breastfeeding relationship was established, and the availability of social media to gain social support for EP and a source for EP strategies. 10 , 13
Regardless of how it is delivered, providing breastmilk has numerous benefits for both the birthing parent and the infant. Parents who lactate had lower risks of breast carcinoma, ovarian carcinoma, and type 2 diabetes. 14 Children who received the optimal duration of breastmilk feedings had a lower risk of otitis media, asthma, infection related mortality, and all‐cause mortality. 15 , 16 , 17 Most recommendations do not distinguish between breastmilk feeding delivery methods, which could include direct breastfeeding and EP. The World Health Organization (WHO), The United Nations Children's Fund (UNICEF), and the American Academy of Pediatrics recommend exclusive breastfeeding for 6 months followed by the addition of complementary foods and continued breastfeeding for at least 2 years. 18 , 19 , 20 Although 84.1% of American families initiated breastfeeding, only 58.3% provided any breastmilk at 6 months and only 25.6% reported that they were exclusively breastfeeding at 6 months of age. 21 Although these resources state breastfeeding, WHO also adds that no bottles, pacifiers, or teats should be used, and the infants should breastfeed on demand. 22 The Association of Women's Health, Obstetric, and Neonatal Nurses, The American College of Obstetricians and Gynecologists, and The American Academy of Family Physicians also concur that breastmilk is the ideal and normative nutrition for infants. 23 , 24 , 25 While EP is not specifically addressed in these recommendations, more must be known about EP to help those unable to directly breastfeed to offer their infants the benefits of breastmilk and avoid risks from artificial formula feeding. Research that can distinguish between direct breastfeeding, EP, artificial formula feeding, and their combinations can help facilitate understanding of infant outcomes and progress. 26 Understanding EP is necessary to engage these families in research and practice so that their specific needs can be identified, and outcomes addressed effectively. A concept analysis following the Walker and Avant method is the first step in deepening this understanding. 27 This concept analysis includes the defining attributes, antecedents, consequences, and empirical referents for EP, along with model and contrary cases.
1.1. Data sources
A comprehensive search was completed using the Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed, and Google Scholar using the search terms human milk express*, breast express*, breast milk express, and breastmilk express* in June‐September 2021. Additional searches were completed for exclusive pump, exclusive breast pumping, and exclusive expression. Reference lists from EP studies were reviewed to find additional research. Eligibility criteria included English language and published between 2000 and 2021. This study adheres to all ethical standards for research that does not involve human or animal subjects in the United States. Data sharing not applicable to this article as no datasets were generated or analyzed during the current study. See Figure 1 for PRISMA diagram.
Figure 1.
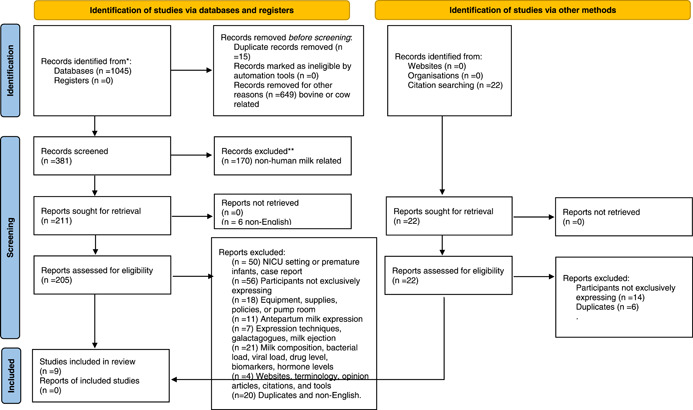
Exclusive breast pumping PRISMA flow diagram for concept analysis [Color figure can be viewed at wileyonlinelibrary.com]
1.2. Concept identification
The term breastfeeding typically includes direct breastfeeding with infant's mouth on the breast extracting milk, feeding the infant a parent's pumped milk, feeding the infant donor breastmilk, feeding frozen breastmilk after the parent has stopped lactating, or any combination of the above. 28 This broad definition and the differing understandings of the term breastfeeding can be problematic in research and clinical practice. Distinguishing between the mode of delivery (feeding at the breast, feeding from a bottle or cup) and the substance given (parent's breastmilk, artificial formula, donor breastmilk) will help providers more accurately capture the characteristics of their patients, as well as help with representative subgroups within study samples to help understand the contributions to maternal and infant outcomes. 29 , 30 , 31
There is no definition for EP outside the human lactation arena and it has only recently been seen in literature. Exclusive is an adjective defined as (1) excluding, (2) accepting only restricted patronage, or (3) single or sole. 32 The noun breast is defined as (1) either of the mammary glands extending from the front of the chest in humans and some other mammals, (2) the body's ventral surface between the neck and abdomen or part of the clothing the covers the breast, (3) “seat of emotion and thought,” or (4) something resembling a breast. 33 A breast pump is defined as “a device for extracting and collecting milk from the breast during lactation.” 34 Breast pumping is not a dictionary term but generally is used to describe the process of using the breast pump to extract breastmilk. With researchers and practitioners who work with these families, the term, exclusive breast pumping was commonly shortened to exclusive pumping. It may also be labeled exclusive breastmilk expression. The definition of exclusive pumping then is providing breastmilk only by use of the breast pump and excluding other avenues of providing breastmilk, which is consistent with how EP was used in the literature.
1.3. Defining attributes
Defining attributes of a concept are the characteristics “most frequently associated with the concept.” 27 The body of evidence exploring EP was composed of few studies with small sample sizes ranging from 10 to 83 with the exception of one large sample of 2005. 1 , 5 , 6 , 9 , 10 , 26 , 35 This does not allow for easily representing the EP population. However, the three attributes most common across studies with samples or subsamples of parents who choose EP are: (1) absence of direct breastfeeding, (2) breastmilk expression, (3) and an enduring infant feeding pattern of feeding expressed breastmilk only via a bottle. For a family to be exclusively pumping, all three attributes must be present. Though families may initially only exclusively pump, families often transition to bottle feeding both breastmilk and artificial formula. 1 , 5 This shift may or may not be considered EP, depending on the study.
1.4. Absence of direct breastfeeding
Absence of direct breastfeeding is the infant not extracting milk from the breast and usually was not the parent's preference or due to circumstances beyond the parent's control. 9 , 10 Among the studies that include families exclusively pumping, the distinguishing markers of this subgroup were (a) consistently did not directly breastfeed, (b) utilized an electric breast pump to provide breastmilk, and (c) possibly used manual expression to express breastmilk. 1 , 3 , 5 , 9 , 10 , 36 , 37 , 38 The unifying theme was the lack of direct breastfeeding while still providing breastmilk.
1.5. Breastmilk expression
While breastmilk can be expressed by hand, a manual pump, or an electric pump, for parents whose infant is not latching on at all, an effective double, electric breast pump or possibly a hospital‐grade electric double pump is an essential tool to empty the breasts effectively and efficiently. 39 Parents are commonly told to pump at the same frequency as their infant would feed at the breast. In the newborn stage, a parent exclusively pumping would expect to pump 8–12 times daily. 40 Without emptying the breasts, the levels of feedback inhibitor of lactation increase, and the parent's milk supply would decrease. 41 For a pumping parent to maintain their milk supply, regular milk removal is essential to maintain breastmilk supply. When an infant's breastmilk demands exceed the supply in a mother who is directly breastfeeding, the infant can increase their frequency of feeding and provide manual stimulation to increase the supply. It may be more challenging to increase the breastmilk supply in EP families, especially if they do not have an effective breast pump.
The value of having a high‐quality double‐electric pump was even more important to parents who are reliant upon the breast pump. 12 Parents often asked healthcare personnel and other mothers for advice on purchasing a pump. 42 In this author's experience, EP parents are proficient at combining equipment from different manufacturers to create the most effective breast pump for them. For EP parents to continue to provide breastmilk in the absence of direct breastfeeding, efficient and effective breastmilk expression was necessary.
1.6. Enduring infant feeding pattern
An enduring infant feeding pattern of feeding expressed breastmilk only via a bottle without direct breastfeeding is descriptive in itself. Infants unable to use a bottle, especially those in the NICU, may receive all of their breastmilk from a nasogastric, orogastric, or gastrostomy tube. There can be confusion; however, as most families who are characterized as breastfeeding families actually use a combination of direct breastfeeding and feeding pumped breastmilk. 5 , 38 Therefore, this combination feeding was not characterized as EP since they are also directly breastfeeding. Though no minimum time for this pattern has been defined, the key was that it was consistent, there was no variation in other delivery methods for breastmilk, and there was not a plan for direct breastfeeding in the future. Studies that included a sample or subsample of persons exclusively pumping did not have a minimum time to establish an enduring pattern in the inclusion criteria. 1 , 3 , 5 , 9 , 10 , 36 , 37 , 38 Notably, self‐identification of EP often coincided with the discontinuation of attempts to direct breastfeed, which can further blur the identification of an enduring infant feeding pattern. This may be a period of weeks to months. In the studies, the average EP duration ranged from 1.5 to 12 months. 1 , 5 , 6 , 9 , 10
For those exclusively pumping, they must learn how to maintain a milk supply with only EP. Milk supply is established in the first few weeks of lactation and peaks at 900 ml/day around 40 days postpartum. 43 Milk supply can decrease within a few days with incomplete breast emptying and nipple stimulation. Therefore, approximately 1 week of EP and maintaining their milk supply would be an estimated minimum amount of time to establish a pattern.
2. ANTECEDENTS OF EXCLUSIVE PUMPING
Antecedents are events that must occur before the existence of the concept. 27 Antecedents for EP include (a) the onset of Stage 2 lactogenesis, (b) a parent that values the benefits of breastmilk, and (c) an understanding that breast milk can be separated from breastfeeding.
2.1. Onset of Stage 2 lactogenesis
To exclusively pump, the person needs to have achieved Stage 2 lactogenesis. The person exclusively pumping may not be the person who gave birth (e.g., induced lactation [i.e., Stage 2 lactogenesis] in an adoptive parent) or the person parenting the child (e.g., surrogate pregnancy). There are many physiological changes and body systems that must perform within normal limits to have stage 2 lactogenesis. These include normal breast development, normal endocrine function, and normal nerve innervation. 44 To maintain milk production, one must regularly remove the milk and stimulate the nipple. 45 With breast stimulation from a breast pump or infant, the posterior lobe of the pituitary gland releases oxytocin to activate the milk ejection reflex and the anterior lobe of the pituitary gland releases prolactin to promote milk synthesis for the next feeding. 41
2.2. Value the benefits of breastmilk
Before EP was possible, parents must have valued the benefits of breastmilk and intended to feed the infant breastmilk. 9 , 10 , 12 , 35 Infant feeding education and breastfeeding promotion are a routine part of antepartum care. 46 Most parents made their infant feeding decision before pregnancy or early pregnancy. 47 When new parents who intended to direct breastfeed encounter barriers, pumping may be the initial method used to feed their infant. When these difficulties did not resolve, some parents choose to exclusively pump to ensure their infant still received some of the benefits of breastmilk. 9 Parents value the health benefits of breastmilk and 98.2% of persons who exclusively pumped stated they exclusively pumped instead of using formula or donor breast milk due to the health benefits to the baby. 10 Pasteurized donor breastmilk availability is limited and rarely available following the initial hospitalization. Informal breastmilk sharing may be an option but may be costly and present additional risks.
2.3. Separating breastmilk from breastfeeding
The improvements in quality and efficiency of available breast pumps, along with mandated insurance reimbursement, have influenced the ease of separating breastfeeding from the provision of breastmilk. 12 , 13 , 48 Furthermore, with such improvements, many more women had access to breast pumps when facing breastfeeding difficulties. 2 The availability of high‐quality pumps enable parents to actualize breastmilk feeding that does not only come at the breast. Families educated on the benefits of breastmilk and EP can realize those benefits may remain when feeding expressed breastmilk.
3. CONSEQUENCES OF EXCLUSIVE PUMPING
The consequences of the concept of EP include seeking EP relevant information and strategies, a focus on breastmilk supply or breastmilk “stash,” and an altered duration of breastmilk feeding.
3.1. Seeking EP information
Information on EP was often missing from prenatal classes, and there were no formal EP support programs, therefore, persons who exclusively pumped seeked information support, and guidance by doing their own research online and asking other parents on social media. 9 , 35 , 37 , 42 , 49 , 50 , 51 Healthcare providers often miss opportunities to give education and support on exclusive pumping. 35 , 49 Education and support can help parents increase their knowledge and self‐efficacy around infant feeding and reinforce that breastmilk successfully can be fed in the absence of direct breastfeeding.
3.2. Breastmilk stash
Many breastmilk feeding families are astutely aware of their breastmilk supply (i.e., milk volume obtained from the breast) or breastmilk stash (i.e., stored breastmilk). Insufficient milk supply was a common reason for premature breastfeeding cessation and having an adequate milk supply and a breastmilk stash provide flexibility if they encounter temporary problems with supply, illnesses, or separation. 52 , 53 Often, breastfeeding families seeked information on managing their breastmilk supply. 9 , 49 , 51 Parents may interpret the volume of breastmilk produced by pumping to indicate their supply, with those who perceived they had a low milk supply more likely to stop feeding breastmilk. 12 , 13 , 42 In addition, women may tie their self‐worth to the volume of milk produced. 12 Furthermore, EP families more likely had breastmilk supply problems, which may foster further inquiries on how to maintain their milk supply and further put pressure on themselves to have a full milk supply. 1 , 7 , 37 In studies of women who both pumped and directly breastfed, when the infants consumed more than they pumped, women reported feelings of personal failure. 13 Challenges with breastmilk supply affects breastmilk stashes. Exclusive pumping families, similarly, to other breastfeeding families, strived to plan and achieve a sufficient breastmilk supply and breastmilk stash so that they can use the breastmilk carefully and strategically to meet their breastfeeding goals. 2
3.3. Altered duration of breastmilk feeding
Exclusive pumping families, when compared to other breastmilk feeding families, generally had a decreased breastmilk feeding duration. EP families produced breastmilk for a shorter period of time, stopped pumping sooner, and had a higher likelihood of early weaning compared to families who fed by a mix of direct breastfeeding and pumped breastmilk. 1 , 4 , 5 , 6 The context for these altered durations of breastmilk feeding needs to be other families who planned to directly breastfeed, so they are interpreted accurately. As such, what may appear to be a decreased duration when compared to breastfeeding families, could actually be an increased duration for EP families who otherwise may have opted to use artificial formula even earlier due to obstacles with direct breastfeeding. Therefore, a likely consequence of EP was altered duration of breastmilk feeding.
4. EMPIRICAL REFERENTS
Exclusive pumping lacks an operational definition, and a relevant measurement tool does not exist. In three small studies, the prevalence of EP was between 5.1% and 19.8%. 1 , 3 , 4 To determine the presence of EP, researchers would look for the presence of all three attributes (a) absence of direct breastfeeding, (b) breastmilk expression, (c) and enduring infant feeding pattern of feeding expressed breastmilk without directly breastfeeding from the breast. Observation of the presence of all three attributes would constitute EP.
To facilitate measurement of EP, clinicians and researchers can first determine the presence of EP and then the duration of EP. As with breastfeeding, there may be a dose‐dependent relationship that is guided by recommendations from health organizations such as UNICEF, which may lead to additional benefits with extended duration or increased exclusivity. Three parameters of duration for all breastmilk feeding families may provide value, (a) the duration the lactating adult expressed breastmilk, (b) the duration the infant received only breastmilk for nutrition, and (c) the total duration the infant received any breastmilk feedings. If the research is examining the outcomes for the lactating person, they would look at the presence or absence of EP, presence or absence of direct breastfeeding, and the total duration the adult expressed breastmilk. If clinicians or researchers are looking for infant outcomes associated with substance fed and mode of delivery, they may look for the duration of time the infant received only breastmilk, duration of time the infant received any breastmilk and the mode of delivery throughout the infant's lifetime. Future infant feeding studies should clearly differentiate the substance fed and the mode of delivery to clearly see associations between substance, delivery method, and the outcomes of interest. 2 , 28
4.1. Model case
Maria, a primigravida with gestational diabetes, gave birth to José at 36 weeks gestation. José was hypoglycemic and would not breastfeed, therefore 30 ml of artificial formula was given. Maria wanted to directly breastfeed José, but he was too sleepy and would not latch onto her breast (no direct breastfeeding), so Maria called the nurse, requesting help. The nurse attempted to stimulate José to wake up and effectively latch, but he would not latch. The nurse brought Maria a breast pump and Maria used the breast pump to extract breastmilk (breastmilk expression) and bottle‐fed it to Jose. Over the following weeks, José continued to have problems latching onto the breast effectively and transferring breastmilk. He would often just latch onto the nipple, which caused tissue damage for Maria and frustration for José. Maria continued pumping breastmilk and bottle feeding it to José. After 4 weeks, Maria eventually stopped trying to directly breastfeed (no direct BF), continued to use the breast pump to extract breastmilk (breastmilk expression), and bottle‐fed José pumped breastmilk. They continued this infant feeding pattern (infant feeding pattern formed and enduring) until they met their feeding goals at 12 months old. There can be many reasons why a family may exclusively pump, but all will have the attributes of an absence of direct breastfeeding, breastmilk expression, and an enduring infant feeding pattern of feeding expressed breastmilk without directly breastfeeding. Figure 2 displays the relationship between the attributes, antecedents, consequences, and empirical referents of EP.
Figure 2.
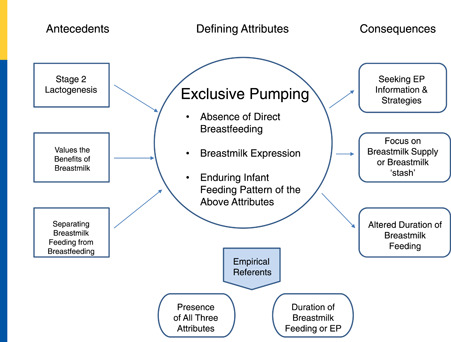
Relationship among the antecedents, defining attributes, consequences, and empirical referents associated with exclusive pumping [Color figure can be viewed at wileyonlinelibrary.com]
4.2. Contrary case
Katie's parents, Jessica and Terry, alternated between directly breastfeeding (presence of direct breastfeeding) and formula feeding Katie. Jessica did not pump or hand express breastmilk (no breastmilk expression). Jessica had 6 months of maternity leave and could directly breastfeed for most feedings. Exclusive pumping was not performed; therefore, an enduring pattern of EP cannot persist over time. This case does not have the core attributes necessary for EP. In the contrary case, direct breastfeeding was present, the parent was not expressing breastmilk manually or with a breast pump, and no pattern of exclusive pumping was established.
5. CONCLUSION AND RECOMMENDATION
Exclusive pumping is a relatively new concept in the literature but appears to be a helpful practice for those who want to feed their infants breastmilk and do not desire or cannot directly breastfeed. To foster future research, a well‐defined EP concept can be incorporated into larger quantitative and qualitative studies about infant feeding practices. Understanding the true prevalence of EP and its associated maternal and infant outcomes will foster better understanding of these families and infants' unique needs. This concept analysis affirms consideration of the language around infant feeding must change, and the broad term of breastfeeding may not be the most accurate and consistent descriptor of all breastmilk feeding families. Lacking a verified measurement tool, providers can confirm that EP is present by observation of the three attributes of (a) absence of direct breastfeeding, (b) breastmilk expression, and (c) an enduring infant feeding pattern of feeding expressed breastmilk only via a bottle. For families encountering difficulties with direct breastfeeding, providers who are aware of and knowledgeable can offer the option to exclusively pump.
This concept analysis also can provide the groundwork for future research about how to best support and help these families achieve the positive health outcomes associated with breastmilk feeding. Studies exploring EP families' equipment needs, the number of daily pumps needed, the volume of milk pumped daily at different ages, and the percentage of the infant's diet that is fulfilled by pumped breast milk would help providers better understand EP and its impact. Finally, future research focusing on helping EP families reach their infant feeding goals may facilitate an increase in the number of babies being fed breastmilk.
CONFLICT OF INTEREST
The author declares no conflict of interest.
Rosenbaum KA. Exclusive Breastmilk Pumping: A Concept Analysis. Nurs Forum. 2022;57:946‐953. 10.1111/nuf.12766
REFERENCES
- 1. Keim SA, Boone KM, Oza‐Frank R, Geraghty SR. Pumping milk without ever feeding at the breast in the moms2moms study. Breastfeed Med. 2017;12(7):422‐429. 10.1089/bfm.2017.0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O'Sullivan EJ, Geraghty SR, Rasmussen KM. Human milk expression as a sole or ancillary strategy for infant feeding: a qualitative study. Matern Child Nutr. 2017;13(3):e12332. 10.1111/mcn.12332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shealy KR, Scanlon KS, Labiner‐Wolfe J, Fein SB, Grummer‐Strawn LM. Characteristics of breastfeeding practices among US mothers. Pediatrics. 2008;122(Suppl 2):S50‐S55. 10.1542/peds.2008-1315f [DOI] [PubMed] [Google Scholar]
- 4. Bai DL, Fong DYT, Lok KYW, Wong JYH, Tarrant M. Practices, predictors and consequences of expressed breast‐milk feeding in healthy full‐term infants. Public Health Nutr. 2017;20(3):492‐503. 10.1017/S136898001600241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jiang B, Hua J, Wang Y, Fu Y, Zhuang Z, Zhu L. Evaluation of the impact of breast milk expression in early postpartum period on breastfeeding duration: a prospective cohort study. BMC Pregnancy Childbirth. 2015;15:268. 10.1186/s12884-015-0698-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pang W, Bernard J, Thavamani G, et al. Direct vs. expressed breast milk feeding: relation to duration of breastfeeding. Nutrients. 2017;9(6):547. 10.3390/nu9060547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bower K, Burnette T, Lewis D, Wright C, Kavanagh K. “I had one job and that was to make milk”. J Hum Lact. 2017;33(1):188‐194. 10.1177/0890334416679382 [DOI] [PubMed] [Google Scholar]
- 8. Froh EB, Deatrick JA, Curley MAQ, Spatz DL. Making meaning of pumping for mothers of infants with congenital diaphragmatic hernia. J Obstet Gynecol Neonatal Nurs. 2015;44(3):439‐449. 10.1111/1552-6909.12564 [DOI] [PubMed] [Google Scholar]
- 9. Clapton‐Caputo E, Sweet L, Muller A. A qualitative study of expectations and experiences of women using a social media support group when exclusively expressing breastmilk to feed their infant. Women Birth. 2021;34(4):370‐380. 10.1016/j.wombi.2020.06.010 [DOI] [PubMed] [Google Scholar]
- 10. Jardine FM. Breastfeeding Without Nursing: The Lived Experiences of Exclusive Pumpers. Digital Repository at the University of Maryland. Published online 2020. 10.13016/bzw3-sp5r [DOI]
- 11. McGuire E. Exclusive expression: a woman who achieved an abundant milk supply. Breastfeed Rev. 2021;29(2):7‐13. [Google Scholar]
- 12. Felice JP, Geraghty SR, Quaglieri CW, Yamada R, Wong AJ, Rasmussen KM. “Breastfeeding” without baby: A longitudinal, qualitative investigation of how mothers perceive, feel about, and practice human milk expression. Matern Child Nutr. 2017;13(3):e12426. 10.1111/mcn.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Felice JP, Geraghty SR, Quaglieri CW, Yamada R, Wong AJ, Rasmussen KM. “Breastfeeding” but not at the breast: mothers' descriptions of providing pumped human milk to their infants via other containers and caregivers. Matern Child Nutr. 2017;13(3):e12425. 10.1111/mcn.12425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chowdhury R, Sinha B, Sankar MJ, et al. Breastfeeding and maternal health outcomes: a systematic review and meta‐analysis. Acta Paediatr. 2015;104(467):96‐113. 10.1111/apa.13102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bowatte G, Tham R, Allen K, et al. Breastfeeding and childhood acute otitis media: a systematic review and meta‐analysis. Acta Paediatr. 2015;104(467):85‐95. 10.1111/apa.13151 [DOI] [PubMed] [Google Scholar]
- 16. Lodge C, Tan D, Lau M, et al. Breastfeeding and asthma and allergies: a systematic review and meta‐analysis. Acta Paediatr. 2015;104(467):38‐53. 10.1111/apa.13132 [DOI] [PubMed] [Google Scholar]
- 17. Sankar MJ, Sinha B, Chowdhury R, et al. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta‐analysis. Acta Paediatr. 2015;104(467):3‐13. 10.1111/apa.13147 [DOI] [PubMed] [Google Scholar]
- 18. World Health Organization 2021. Exclusive breastfeeding for six months best for babies everywhere. January 15, 2011. Accessed November 9. https://www.who.int/news/item/15-01-2011-exclusive-breastfeeding-for-six-months-best-for-babies-everywhere
- 19. World Health Organization . Infant and Young Child Feeding. World Health Organization. June 9, 2021. Accessed November 13, 2021. https://www.who.int/en/news-room/fact-sheets/detail/infant-and-young-child-feeding
- 20. Eidelman AI, Schanler RJ. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827‐e841. 10.1542/peds.2011-3552 [DOI] [PubMed] [Google Scholar]
- 21. Centers for Disease Control and Prevention 2021. Breastfeeding Report Card: United States, 2020. Breastfeeding. September 17, 2020. Accessed November 10. https://www.cdc.gov/breastfeeding/data/reportcard.htm
- 22. World Health Organization 2021. Breastfeeding: Recommendations. Accessed November 9, 2021. https://www.who.int/health-topics/breastfeeding#tab=tab_2
- 23.American Academy of Family Physicians. Breastfeeding, Family Physicians Supporting (Position Paper). April 2021. Accessed October 22, 2021. https://www.aafp.org/about/policies/all/breastfeeding-position-paper.html
- 24. Crow SD, Hanley LE, American College of Obstetricians and Gynecologists' Breastfeeding Expert Work Group . Optimizing support for breastfeeding as part of obstetric practice. Obstet Gynecol. 2018;132(4):e187‐e196. [DOI] [PubMed] [Google Scholar]
- 25. Association of Women's Health . Obstetric, and neonatal nurses. breastfeeding and the use of human milk. JOGNN. 2021;50(5):E1‐E5. [DOI] [PubMed] [Google Scholar]
- 26. Keim SA, Sullivan JA, Sheppard K, et al. Feeding infants at the breast or feeding expressed human milk: long‐term cognitive, executive function, and eating behavior outcomes at age 6 years. J Pediatr. 2021;233:66‐73. 10.1016/j.jpeds.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Walker LO, Avant KC. Strategies for Theory Construction in Nursing. 6th ed. Pearson; 2019. [Google Scholar]
- 28. Rasmussen KM, Felice JP, O'Sullivan EJ, Garner CD, Geraghty SR. The meaning of “breastfeeding” is changing and so must our language about it. Breastfeed Med. 2017;12(9):510‐514. 10.1089/bfm.2017.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boone KM, Geraghty SR, Keim SA. Feeding at the breast and expressed milk feeding: associations with otitis media and diarrhea in infants. J Pediatr. 2016;174:118‐125. 10.1016/j.jpeds.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Noel‐Weiss J, Boersma S, Kujawa‐Myles S. Questioning current definitions for breastfeeding research. Int Breastfeed J. 2012;7(1):9. 10.1186/1746-4358-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Geraghty SR, Rasmussen KM. Redefining “breastfeeding” initiation and duration in the age of breastmilk pumping. Breastfeed Med. 2010;5(3):135‐137. 10.1089/bfm.2009.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. 2021. Merriam‐Webster Dictionary. Exclusive | Definition of Exclusive by Merriam‐Webster. Accessed November 9. https://www.merriam-webster.com/dictionary/exclusive
- 33. 2021. Merriam‐Webster Dictionary. Breast | Definition of Breast by Merriam‐Webster. Accessed November 9. https://www.merriam-webster.com/dictionary/breast
- 34. 2021. Collins English Dictionary. Breast Pump. Accessed February 7. https://www.thefreedictionary.com/breast%2Bpump
- 35. Anders L 2021. Experiences of Exclusively Expressing Breast Milk for TermInfants: A Qualitative Analysis. Published online. [DOI] [PMC free article] [PubMed]
- 36. Coffey‐Glover L. The boob diaries: discourses of breastfeeding in ‘exclusive pumping’ blogs. Discourse Context & Media. 2020;38:100446. 10.1016/j.dcm.2020.100446 [DOI] [Google Scholar]
- 37. Jardine FM. Breastfeeding without nursing: “if only I'd known more about exclusively pumping before giving birth”. J Hum Lact. 2019;35(2):272‐283. 10.1177/0890334418784562 [DOI] [PubMed] [Google Scholar]
- 38. O'Sullivan EJ, Geraghty SR, Cassano PA, Rasmussen KM. Comparing alternative breast milk feeding questions to U.S. breastfeeding surveillance questions. Breastfeed Med. 2019;14(5):347‐353. 10.1089/bfm.2018.0256 [DOI] [PubMed] [Google Scholar]
- 39. Porta R, Miralles N, Paltrinieri A, et al. A breast milk pump at the bedside: a project to increase milk production in mothers of very low birth weight infants. Breastfeed Med. 2021;16(4):309‐312. 10.1089/bfm.2020.0122 [DOI] [PubMed] [Google Scholar]
- 40. 2021. Texas Health and Human Services Commission. Pumping at Work. Breastmilk: Every Ounce Counts. Accessed November 9. https://www.breastmilkcounts.com/working-moms/pumping-at-work/
- 41. World Health Organization 2021. The physiological basis of breastfeeding ‐ Infant and Young Child Feeding ‐ NCBI Bookshelf. Model chapter for textbooks for medical students and allied health professionals. 2009. Accessed November 9. https://www-ncbi-nlm-nih-gov.ezproxy.uttyler.edu/books/NBK148970/ [PubMed]
- 42. Yamada R, Rasmussen KM, Felice JP. “What is ‘enough,’ and how do I make it?”: a qualitative examination of questions mothers ask on social media about pumping and providing an adequate amount of milk for their infants. Breastfeed Med. 2019;14(1):17‐21. 10.1089/bfm.2018.0154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mohrbacher N 2021. How Much Milk Should You Expect to Pump? Nancy Mohrbacher. November 27, 2012. Accessed November 3. http://www.nancymohrbacher.com/articles/2012/11/27/how-much-milk-should-you-expect-to-pump.html
- 44. Mulder PJ. A concept analysis of effective breastfeeding. J Obstet Gynecol Neonatal Nurs. 2006;35(3):332‐339. [DOI] [PubMed] [Google Scholar]
- 45. Pillay J, Davis TJ. Physiology, Lactation. In: StatPearls. StatPearls Publishing; 2021. [PubMed]
- 46. American Academy of Pediatrics (AAP) . American College of Obstetricians and Gynecologists (ACOG). Guidelines for Perinatal Care. 8th ed. American Academy of Pediatrics; 2017. [Google Scholar]
- 47. Kjelland K, Corley D, Slusher I, Moe K, Brockopp D. The best for baby card: an evaluation of factors that influence women's decisions to breastfeed. Newborn and Infant Nursing Reviews. 2014;14(1):23‐27. 10.1053/j.nainr.2013.12.007 [DOI] [Google Scholar]
- 48. Geraghty SR, Sucharew H, Rasmussen KM. Trends in breastfeeding: it is not only at the breast anymore. Matern Child Nutr. 2013;9(2):180‐187. 10.1111/j.1740-8709.2012.00416.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Dietrich Leurer M, McCabe J, Bigalky J, Mackey A, Laczko D, Deobald V. “We just kind of had to figure it out”: a qualitative exploration of the information needs of mothers who express human milk. J Hum Lact. 2020;36(2):273‐282. 10.1177/0890334419883203 [DOI] [PubMed] [Google Scholar]
- 50. Strauch L, Sweet L, Scott H, Müller A. Mechanisms of support for exclusive breastmilk expressers in the community: a scoping review. BMC Pregnancy Childbirth. 2019;19(1):511. 10.1186/s12884-019-2667-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lebron CN, St , George SM, Eckembrecher DG, Alvarez LM. “Am I doing this wrong?” breastfeeding mothers' use of an online forum. Matern Child Nutr. 2020;16(1):e12890. 10.1111/mcn.12890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hornsby PP, Gurka KK, Conaway MR, Kellams AL. Reasons for early cessation of breastfeeding among women with low income. Breastfeed Med. 2019;14(6):375‐381. 10.1089/bfm.2018.0206 [DOI] [PubMed] [Google Scholar]
- 53. Gatti L. Maternal perceptions of insufficient milk supply in breastfeeding. J Nurs Scholarsh. 2008;40(4):355‐363. 10.1111/j.1547-5069.2008.00234.x [DOI] [PMC free article] [PubMed] [Google Scholar]


