Abstract
Aim
To evaluate the effectiveness of cardiovascular risk communication strategies to improve understanding and promote risk factor modification.
Design
Systematic review with narrative synthesis.
Data sources
A comprehensive database search for quantitative and qualitative studies was conducted in five databases, Cumulative Index to Nursing and Allied health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), EMBASE, Applied Social Sciences Index and Abstracts (ASSIA) and Web of Science. The searches were conducted between 1980 and July 2019.
Review methods
The systematic review was conducted in accordance with Cochrane review methods. Data were extracted and a narrative synthesis of quantitative and qualitative results was undertaken.
Results
The abstracts of 16,613 articles were assessed and 210 underwent in‐depth review, with 31 fulfilling the inclusion criteria. We observed significant heterogeneity across study designs and outcomes. Nine communication strategies were identified including numerical formats, graphical formats, qualitative information, infographics, avatars, game interactions, timeframes, genetic risk scores and cardiovascular imaging. Strategies that used cardiovascular imaging had the biggest impact on health behaviour change and risk factor modification. Improvements were seen in diet, exercise, smoking, risk scores, cholesterol and intentions to take preventive medication.
Conclusion
A wide range of cardiovascular risk communication strategies has been evaluated, with those that employ personalized and visual evidence of current cardiovascular health status more likely to promote action to reduce risk.
Impact
Future risk communication strategies should incorporate methods to provide individuals with evidence of their current cardiovascular health status.
Keywords: cardiovascular diseases, communication, heart disease risk factors, literature review, nursing, primary prevention, systematic review
1. INTRODUCTION
Cardiovascular disease is the leading cause of death and disability globally (World Health Organisation, 2017). An ageing population and increases in cardiovascular risk factors, such as obesity, are exacerbating the problem (Timmis et al., 2018). It is estimated that as many as 80% of these deaths are preventable (World Health Organisation, 2017), highlighting the importance of prevention in reducing the number of unnecessary deaths and the burden of cardiovascular disease. Nurses form the largest health professional group managing cardiovascular risk factors (Hayman et al., 2015) and thus have a key role to play in the prevention of cardiovascular disease. Identifying individuals who would benefit from risk factor management is challenging due to the insidious nature of atherosclerosis, which is often advanced before symptoms develop (Cooney et al., 2009). Cardiovascular risk prediction assessments aid health professionals in clinical decision‐making about preventative treatment and are also used to inform individuals about their risks (Rossello et al., 2019). An abundance of research exists on how to accurately predict cardiovascular risk, but attention is needed on how best to inform individuals of that risk (Ahmed et al., 2012). Individuals can only make informed decisions around risk reduction if they fully comprehend their risk.
1.1. Background
Risk communication is the open, real‐time exchange of information, advice and opinion between experts and those at risk to improve understanding and facilitate informed decisions about clinical management (Thomson et al., 2015). It is a cornerstone of cardiovascular screening and should enhance a person’s knowledge and perception of risk, allowing them to make informed decisions (Ahmed et al., 2012). Individuals who are better informed about their cardiovascular health are more likely to adhere to preventative measures and may have better outcomes (Thomson et al., 2015). Information must be credible, clear and easy to understand (Ahmed et al., 2012) to avoid potential misinterpretation of risk and suboptimal choices about treatment. Furthermore, poor communication can also reduce confidence in health professionals and lead to anxiety and other adverse outcomes.
Many different strategies exist to communicate cardiovascular risk to individuals including numerical formats, qualitative information, visual representation or a combination. Recently, health professionals have been providing feedback from medical imaging to communicate risk information to individuals (Hollands et al., 2010). With such a pivotal role in managing risk factors, nurses involved need to be confident and skilled communicators. Understanding the effectiveness of available strategies will enable nurses to select the best approach for cardiovascular risk discussions.
2. THE REVIEW
2.1. Aims
The aim of this systematic review was to identify existing cardiovascular risk communication strategies and to evaluate their acceptability and effectiveness to improve understanding and promote risk factor modification in asymptomatic individuals without known cardiovascular disease.
2.2. Design
A systematic review of quantitative and qualitative studies was chosen to permit a more complete analysis and maximize findings. The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis (PRISMA) (Moher et al., 2009) and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTEREQ) (Tong et al., 2012) guidelines (Appendix S2). The review protocol was registered with an international register of systematic reviews (PROSPERO ID: CRD42020204797).
2.3. Search methods
The systematic review search was guided by the population, intervention, comparison and study design (PICOS) criteria (Appendix S3). A comprehensive search was conducted in five online databases (CINAHL, Medline, EMBASE, ASSIA and web of science) using the following terms: risk communication, risk communication tools and risk messages, cardiovascular disease, ischaemic heart disease, atherosclerosis and risk presentation. Search terms were adapted to each database and are detailed in Appendix S1. The searches were conducted between 1980 and July 2019 and no language exclusions were applied. Relevant studies were sought from trial registries (clinical.gov) and reference lists of included studies were searched to identify additional studies. The titles and abstracts of all potentially eligible studies identified from the search were reviewed against pre‐determined inclusion and exclusion criteria by one reviewer (SS). The full texts of all potential studies were then independently screened by two reviewers (SS, AF and FS) and disagreements were resolved through discussion with a third reviewer (SS, AF and FS). Outcomes of interest were those associated with behaviour change, risk factor modification, risk knowledge and understanding, increased intentions and acceptability of the approach.
2.3.1. Inclusion and exclusion criteria
Randomized trials, cohort studies and observational and qualitative studies were all eligible for inclusion. Only published research studies were sought and conference abstracts were excluded. Only primary prevention studies were eligible and studies of secondary prevention or in populations with established cardiovascular disease were excluded. Studies which communicated risks associated with cardiovascular treatments were also excluded. The target population was adults eligible for cardiovascular screening and thus studies with younger cohorts, such as college students were excluded. Studies which assessed the performance of cardiovascular risk scores and did not communicate risk to individuals were also excluded. Moreover, studies which evaluated behaviour change interventions, for example tailored smoking cessation interventions, were excluded as it cannot be ascertained if changes in outcomes were a result of the risk communication strategy or another component of the intervention.
2.4. Search outcome
After duplicates were removed, a total of 16,613 titles and abstracts were identified and screened. The full‐text manuscripts for 210 studies were reviewed and a total of 31 (20 quantitative and 11 qualitative) met the inclusion criteria (Figure 1). The included studies were conducted across eight different countries from 2004 to 2019 (Table 1). A total of 20,618 (n = 20,256 quantitative and n = 362 qualitative) participants were included across the 31 studies, including patients, members of the public and general practitioners. Two studies did not report the sex of the participants, but the proportion of male participants across the remaining studies was 59%. Most of the studies provided individuals with their personal risks, but some provided hypothetical risk scenarios. Significant heterogeneity in study outcomes was observed across the quantitative studies. The outcomes assessed included acceptability of the communication strategy, emotional responses, knowledge and understanding of risk, intentions and changes in health behaviours or risk factors (Table 2). The quantitative studies evaluated the performance of the risk communication strategy against the outcomes chosen (Table 3), whereas the qualitative studies provided an exploration of the participant's perceptions of the strategy (Table 4).
FIGURE 1.
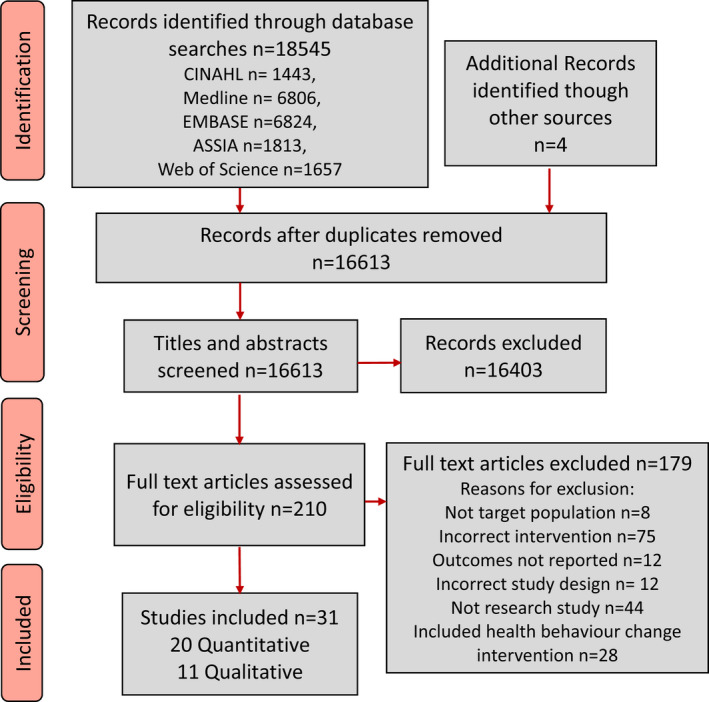
PRISMA diagram of study flow.
TABLE 1.
Study characteristics
| Study | Author (year), Country | Study aims | Design | Sample size and context | Mean age and range | Sex (% male) | CVD risk assessment | Risk communication strategy | Variables of strategy | Professional communicating risk (or mode of delivery) | Main outcome measures |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quantitative studies | Adarkwah et al. (2019), Germany | Compare the effects of presenting a cardiovascular risk to patients and their subsequent adherence to intervention using 10‐year risk illustration in the decision aide software Arriba (emoticons) and newly developed time to event illustration | Prospective randomized trial | n = 294 patients who GPs wanted to discuss behaviour change with |
58 30–80 |
42.1% | Personal risk. Absolute, Framingham risk equations | Graphical format | Coloured time to event bar graph and icon arrays (emoticons) | General physician | Adherence to behavioural change intervention patient agreed on |
| Bonner et al. (2015), Australia | Test the effect of heart age on psychological and behavioural outcomes compared with 5‐year absolute risk is low‐ (i.e., 5‐year absolute risk of a CVD event <10%) to moderate‐risk (10%–15% absolute risk) patients | Randomized 2 × 3 factorial design | n = 469, non‐diabetic, not known to be high risk of CVD, no anti‐hypertensives or lipid lowering medication |
54 45–64 |
50% | Personal risk. Absolute, Framingham risk equation | Numerical and graphical formats | Percentage, heart age and bar graph | Online | Intention to change lifestyle (improve diet, increase physical activity and stop smoking | |
| Damman et al. (2018), Netherlands | (1) Evaluate the effects of infographics about qualitative risk dimensions either with or without risk numbers on risk comprehension (2) Investigate what type of qualitative risk dimension (causes, timeline or consequences) can be best emphasized in infographics. (3) Test effects of heart age compared with traditional risk number on risk comprehension | Controlled experimental 2 × 2 | n = 727, target population of cardiovascular risk calculators |
Mean not reported 45–65 |
51.7% | Hypothetical scenarios. Absolute, Dutch calculator (modified version of SCORE) | Infographics, numerical formats and qualitative information | Infographics, heart age, percentages and text information | n/a hypothetical scenario | Information recall, cognitive‐risk appraisal, risk comprehension, affective risk appraisal and worry | |
| Domenech et al. (2016), Spain | Test the hypothesis that knowledge of the genetic risk score (GRS) in uncontrolled hypertensive patients would improve BP control | A randomized, single‐blind cohort study in two parallel groups | n = 67 patients with uncontrolled ambulatory BP (24 h‐ABPM >130/80) | 54.5 (9.3) range not reported | 74.3% | Personal risk. Genetic risk, based on Cardio in Code & SCORE | Genetic risk score | Verbal risk categories | Clinician | Improved blood pressure control | |
| Fair et al. (2008), UK | Test the hypothesis that responses to coronary heart disease (CHD) risk estimates are heightened by the use of ratio formats, peer group risk information and long time frames. | Cross‐sectional, between factors design | n = 1480, general population |
Mean not reported 30–70 |
50% | Hypothetical scenarios. Absolute, Framingham | Numerical formats | Percentages, risk ratios and peer‐group comparators | n/a hypothetical scenario | Risk perception, emotional response and intention to change lifestyle | |
| French et al. (2004), UK | Examine the emotional and cognitive impact of personal and social comparison information about health risk | Observational factorial design | n = 970, 40–60 years with no history of heart disease | 49 (6.7) range not reported | 48% | Hypothetical Scenarios, Absolute risk (calculator/cohort not reported) | Numerical formats | Social comparisons, frequencies, percentages, bar graphs and icon arrays | n/a hypothetical scenario | Worry, reassurance, the likelihood of event, confidence in understanding, familiarity with cardiac events and comparison with others | |
| Frileux et al. (2004), France | Explore the impact of the preventive medical message on the intention to change behaviour. | Observational factorial design | n = 150 unpaid volunteers with no history of heart disease |
Mean not reported 20–80 |
40.67% | Hypothetical scenarios. Absolute (calculator not defined) | Numerical formats and timeframes | Percentages and 5, 10, 15 and 20 year timeframe | n/a hypothetical scenarios | Intention to adopt a specific behaviour. | |
| Johnson et al. (2015), USA | Examine how knowledge of the CAC score affects risk perception, the likelihood of taking action and health‐promoting behaviour change in persons at high risk for cardiovascular disease | Observational pre‐and post‐design | n = 174 undergoing CAC scan with ≥3 risk factors |
58.5 40–79 |
62% | Personal risk. Coronary calcium scoring (CAC) | Cardiovascular imaging | Coronary artery calcium scores and verbal risk category | Nurse over the telephone | Risk perceptions, the likelihood of action, worry, behaviour change and risk modification | |
| Kalia et al. (2006), USA | Evaluate whether visualization of coronary calcium would positively affect patients’ adherence rates | Observational pre‐ and post‐design | n = 505, asymptomatic patients on statin therapy referred for EBT risk assessment |
61 (10) range not reported |
82% | Personal risk. Electron Beam Tomography (TBT) coronary calcium scoring | Cardiovascular imaging | Coronary artery calcium scores, visualization and verbal risk categories | Research Team | Adherence to lipid‐lowering therapy and lifestyle modification | |
| Knowles et al. (2017), USA | Test whether providing a genetic risk score (GRS) for coronary artery disease (CAD) would serve as a motivator to improve adherence to risk‐reducing strategies | Pilot randomized control trial | n = 65 participants seeking cardiovascular risk evaluation with >6% risk of CAD over the next 10 years or >20% over the next 30 years |
57.5 (10)* range not reported *at randomization |
57% | Personal risk. Framingham risk score multiplied by genetic risk score (evaluated in ARIC cohort). | Genetic risk score | Percentage, individual percentiles on distribution graph and an absolute number of risk alleles. | Physician | Change in LDL cholesterol | |
| Korcarz et al. (2008), USA | Determine if identifying increased carotid intima‐media thickness (CIMT) or carotid plaque during office‐based ultrasound screening examinations could alter physicians' treatment plans and patients' motivation about health‐related behaviours | Observational pre‐and post‐design | n = 263 men ≥45 years or women ≥55 years with ≥1 CVD risk factor or women 45–54 with family history and ≥1 additional risk factor |
58.1 45–70 |
48.7% | Personal risk. Ultrasound, images of the distal wall of each carotid. Plaque is defined as a thickening of intimal reflection on the arterial lumen. | Cardiovascular imaging | Carotid ultrasounds and verbal information about plaque or increased carotid intima‐media thickness | Not documented | Patient motivation and physician treatment plans | |
| Lopez‐Gonzalez et al. (2015), Spain | Test whether communicating cardiovascular diseases risk using the Heart Age risk assessment tool will be able to motivate a population to adopt healthier lifestyles and improve CVD risk profile over the use of a traditional percentage‐based tool | Randomized controlled trial | n = 2844 public sector workers |
46.1 (7.1) range not reported |
47.7% | Personal risk. Absolute Framingham REGICOR | Numerical formats | Percentage or heart age | Research team & clinical assistants | Framingham REGICOR score | |
| Naslund et al. (2019), Sweden | Investigate the impact of pictorial information about an individual’s atherosclerosis, as demonstrated by carotid ultrasound, in comparison with traditional risk factor‐based risk communication | Randomized controlled trial | n = 3175, aged 40 with first degree relative with CVD or aged 50 with ≥1 risk factor or aged 60. | Not reported | 52.6% | Personal risk. Ultrasound of carotid intima‐media wall thickness. ARIC cohort reference for vascular age | Cardiovascular imaging | Vascular age and stylised picture of the ultrasound image. Plaque formation is shown as traffic light | Written information and images. Telephone follow‐up with a nurse. | Changes in Framingham risk score and SCORE risk score at 1 year | |
| Navar et al. (2018), USA | Determine how the ASCVD risk time horizon, outcome and presentation format influence risk perceptions and treatment preferences | Randomized survey study | n = 2708, from patient and Provider Assessment of Lipid Management (PALM) registry | Median 67 (interquartile range 61–76) | 55% | Hypothesized risk scenario. The absolute risk, SCORE and ASCVD risk calculator | Numerical formats, graphical formats and timeframe icons | Lifetime or 10‐year risk timeframes, percentage, bar graph and icons. | n/a hypothetical scenarios | Perceived risk and willingness to take medication | |
| Orakzai et al. (2008), USA | Assess whether higher coronary artery calcium (CAC) scores determined by electron beam computed tomography (EBCT) are associated with beneficial lifestyle behaviours in asymptomatic individuals. | Observational pre‐and postdesign | n = 980, asymptomatic patients referred for EBCT risk assessment by GP |
60 (8) range not reported |
78% | Personal risk. Electron Beam Tomography (TBT) coronary calcium scoring | Cardiovascular imaging | Coronary artery calcium scores, visualization of scan and verbal risk categories | Physician and technologist | Aspirin initiation, diet changes and increased exercise | |
| Powers et al. (2011), USA | Evaluate the impact of personalized coronary heart disease and stroke risk communication on patients’ knowledge, beliefs and health behaviour. | Randomized controlled trial | n = 89, ≥55 years, diagnosis of hypertension |
67 (8) range not reported |
98% | Personal risk. The absolute risk, Framingham or risk factor education material | Numerical and graphical formats | Percentage, a vertical bar graph with comparison information | Not documented | Exercise, knowledge of risk factors, locus of control, medication adherence, risk estimate, worry, B.P., preferred means of reducing risk, decisional conflict and acceptability | |
| Ruiz et al. (2013), USA | Investigate whether icon arrays increase understanding, recall, perception of CVR and behavioural intent compared with numerical information. | Randomized controlled trial | n = 121 male veterans >20 years at intermediate/high risk but unaware of risk |
61 (7.61) range not reported |
100% | Personal risk. Absolute risk based on National Cholesterol Education Programme | Numerical and graphical formats | Frequencies, icon arrays (stick figures) and percentages | Online | Risk recall, risk change, confidence, risk perceptions, modification intentions and adherence, self‐efficacy, accessibility of information and attitudes | |
| Ruiz et al. (2016), USA | Compare the efficacy of a computer‐based aid communicating global CVR with or without animated avatars for improving patients, risk perception, emotional response and intention to make lifestyle changes and follow medical treatments to reduce CVR. | Randomized controlled trial | n = 41, male veterans >20 years at intermediate/high risk but unaware of risk. |
64 (7) 49–77 |
100% | Personal risk. Absolute, National Cholesterol Education Programme | Avatars | Lip‐synching avatar with text or recorded voice and text | Online | Risk understanding, risk recall, risk perceptions, emotional reaction, intent to adhere to modification, self‐efficacy and attitudes towards computer aid. | |
| Witteman et al. (2014), USA | Test whether four icon array design factors (animated random dispersal of risk events, avatars to represent an individual, personalisation of avatar, that is choosing a colour and moving avatars) help convey randomness and how risk applies to an individual, thereby better aligning risk perceptions with risk estimates | Randomized controlled trial (2 x 2 factorial design) | n = 3630 of Internet users, aged 35–74, with no cardiovascular disease or previous stroke |
53 (10) range not reported |
45% | Personal risk. Absolute, Framingham | Avatars, graphical formats and numerical formats | Online calculator. Verbal labels, icons, avatars and frequencies. | Online | Risk perception | |
| Zikmund‐Fisher et al. (2014), USA | Assess whether varying the icon used in the icon arrays would alter people's risk perceptions, their recall of risk info, preferences about these graphics and assess if numeracy or graphical literacy influenced the results | Prospective randomized trial | n = 1504, internet users, with no known history of heart disease or stroke |
53.8 (9.7) range not reported |
45.7% | Personal risk. Absolute, D'Agostino model developed from Framingham | Graphical formats | Icon arrays—ovals, blocks, restroom icons, faces (smiley and frowns), head outlines and head and shoulder photographs | Online | Risk recall, risk perceptions and graph preferences | |
| Qualitative Studies | Ancker et al. (2009), USA | Explore consumer preferences for different interactive graphics, basic usability and consumer interpretations of what they were seeing. | Focus groups | n = 16 members of the general public aged 20–65+ | Not reported | 18.75% | Hypothesized scenarios. Absolute, calculator based on the National Cholesterol Education Programme guidelines | Graphical formats and numerical formats | Online interactive calculator with bar graphs, icon arrays and frequencies | n/a hypothetical scenarios | N/A |
| Bonner, Jansen, McKinn, et al. (2014); Bonner, Jansen, Newell, et al. (2014), Australia | Investigate patient experiences and understanding of online heart age calculators that use different verbal, numerical and graphical formats based on 5‐ and 10‐year Framingham risk equations used in clinical practice guidelines around the world | Semi‐structured interviews | n = 26 ≥ 1 CVD risk factor, not taking anti‐hypertensives or lipid lowering medication |
54 40–70 |
38.46% | Personal risk. Absolute, Framingham risk equations | Numerical formats & timeframes | Online, heart age, absolute risk with 5 and 10 year timeline | Online | N/A | |
| Bonner, Jansen, McKinn, et al. (2014); Bonner, Jansen, Newell, et al. (2014), Australia | Explore GPs' descriptions of their communication strategies in CVD risk management, and investigate the reasons why they do or do not communicate quantitative absolute risk guidelines to patients. | Semi‐structured interviews | n = 25, GPs with varying levels of experience (<10–>30 years) |
Mean not reported <40–>60 |
28.57% | N/A communication styles | N/A | Positive, scare tactic and indirect | n/a | N/A | |
| Damman et al. (2016), Netherlands | Identify the barriers from the perspective of consumers with low health literacy in using risk information as provided in cardiometabolic risk assessments | Cognitive interviews | n = 23, low health literacy/numeracy |
52.6 40–66 |
45% | Actual, personal risk. Absolute, Dutch national cardiometabolic risk assessment | Numerical formats | Online, self‐assessment, percentage | Online | N/A | |
| Damman et al. (2017), Netherlands | Examine how lay people understand the result derived from an online cardiometabolic risk calculator. | Eye tracker and semi‐structured interviews | n = 16, target population of the prevention programme (no history of type 2 diabetes, CVD and CKD) |
Mean not reported 45–60 |
19% | personal risk. Absolute, National Prevention programme for CVD, type 2 diabetes and CKD calculator | Numerical and graphical formats | Risk percentage, natural frequency, bar graph, categorical verbal label and comparative information | Online | N/A | |
| Goldman et al. (2006), USA | Explore patients’ perceptions of cholesterol and cardiovascular disease risk and their reactions to three strategies for communicating CVD risk | Focus groups | n = 50, aged 20–<70. Recruited from primary care | Not reported | 57.9% | Hypothetical scenarios. Absolute, Framingham | Numerical and graphical formats | Icon arrays, bar graph, percentage and heart age | Research team | N/A | |
| Hill et al. (2010), Australia | Explore consumer and GP views and preferences about the most suitable formats for the representation and discussion of absolute risk for CVD. | Focus groups | n = 37 (19 consumers without CVD and 18 GPs) |
Mean not reported 40–60 |
Not reported | Hypothetical scenarios. Absolute, Framingham | Numerical formats, qualitative information and graphical formats | Statements, icons, percentages, timeframes, risk ratios and frequencies | Research team | N/A | |
| Middlemass et al. (2014), UK | Explore how patients who have had a recent conventional cardiovascular risk assessment, perceive additional information from genetic testing for CHD | Interviews | n = 29, patients undergoing CVD risk assessment who wanted genetic test |
Median—59 53.5–62 |
74.4% | Personal risk. Genetic risk, commercial test using panel of nine risk alleles | Genetic risk scores | Verbal risk category | Written | N/A | |
| Shefer et al. (2016), UK | Explore the short term response to receiving different forms of CHD risk information and lifestyle advice for risk reduction. | Interviews & focus groups (embedded in RCT) | n = 54 (interviews n = 41), blood donor study participants with no history of CVD |
Mean not reported 40–80 |
59.3% | Personal risk. Genetic risk & phenotypic (absolute risk based on Framingham) | Numerical formats | Percentage, natural frequency, heart age, visual & peer comparative risk | Online | N/A | |
| Sheridan et al. (2009), USA | Explore how individuals respond to global coronary heart disease (CHD) risk and use it in combination with treatment information to make decisions to initiate and maintain risk‐reducing strategies | Focus groups | n = 29, known risk but no CVD |
62.7 52–75 |
72% | Personal risk (mock risk if unable to calculate). Absolute risk, calculator not reported | Numerical and graphical formats | Percentage, coloured bar chart and comparative information | Research team | N/A | |
| Wan et al. (2008), Australia | Develop a model for a joint approach to its implementation based on an exploration of the views of patients, general practitioners (GPs) and key informants (KIs) | Focus groups and interviews | n = 57, (22 GPs, 26 patients and 9 Key informants) |
Patients: 63.5 42–81 |
Not reported for all | Risk not provided. Absolute Risk, New Zealand CVAR calculator | N/a | Online (self‐assessment) and paper calculator | n/a | N/A |
TABLE 2.
Overview of outcomes and results
| Strategy | Study | Outcomes | ||||||
|---|---|---|---|---|---|---|---|---|
| Acceptability | Emotional response | Risk knowledge and understanding | Intentions | Changes in health behaviours or risk factors | ||||
| Numerical format | ||||||||
| Percentage | Powers et al. (2011) | + | + | − | o | |||
| Risk ratios | Fair et al. (2008) | − | + | + | ||||
| Heart age | Bonner et al. (2015) | − | − | + | − | |||
| Lopez‐Gonzalez et al. (2015) | + | |||||||
| Damman et al. (2018) | + | + | ||||||
| Graphical format | ||||||||
| Icon arrays | Ruiz et al. (2013) | − | − | |||||
| Zikmund‐Fisher et al. (2014) | Rest rooms and photos | + | ||||||
| Blocks and faces | − | |||||||
| Witteman et al. (2014) | + | − | ||||||
| French et al. (2004) | + | |||||||
| Bar graphs | French et al. (2004) | + | ||||||
| Adarkwah et al. (2019) | + | |||||||
| Navar et al. (2018) | + | + | ||||||
| Avatars | Witteman et al. (2014) | + | + | |||||
| Ruiz et al. (2016) | o | + | ||||||
| Qualitative information | Damman et al. (2018) | + | ||||||
| Infographics | Damman et al. (2018) | − | ||||||
| Timeframe | ||||||||
| Lifetime | Fair et al. (2008) | − | ||||||
| Shorter timeframe (5–10 years) | Frileux et al. (2004) | + | ||||||
| Genetic risk score | Domenech et al. (2016) | + | ||||||
| Knowles et al. (2017) | + | + | o a | |||||
| Cardiovascular imaging | ||||||||
| Coronary artery calcium scoring | Johnson et al. (2015) | + | ||||||
| Orakzai et al. (2008) | + | |||||||
| Kalia et al. (2015) | + | |||||||
| Ultrasound carotid | Näslund et al. (2019) | + | ||||||
| Korcarz et al. (2008) | + | + | ||||||
Positive effect on weight but negative effect on LDL cholesterol.  ;
;  ;
;  .
.
TABLE 3.
Quantitative results
| Strategy | Study | Comparators | Results |
|---|---|---|---|
| Numerical formats | |||
| Percentages | Powers et al. (2011) | Risk factor education |
*1 conditional logistic regression (Fisher exact test when data sparse) *2 t test |
| Risk ratios | Fair et al. (2008) | Percentages |
*1 logistic regression *2 ANOVA |
| Heart age | Bonner et al. (2015) | Percentages |
*Mann‐Whitney test |
| Lopez‐Gonzalez et al. (2015) | Percentages and control (no risk score) |
|
|
| Damman et al. (2018) | Percentages and risk ratios |
*ANOVA |
|
| Graphical displays | |||
| Icon arrays | Ruiz et al. (2013) | Percentages |
|
| Zikmund‐Fisher et al. (2014) | Comparison of icons |
|
|
| Witteman et al. (2014) | Random sequencing |
*ANOVA |
|
| Icon arrays and bar graphs | French et al. (2004) | Numbers |
*ANOVA |
| Adarkwah et al. (2019) | N/A each other |
*Student’s t test |
|
| Navar et al. (2018) | N/A each other |
*Two‐tailed test |
|
| Avatars | Witteman et al. (2014) | Icons and frequencies |
*nested factorial ANOVA |
| Ruiz et al. (2016) | Voice and text |
*ANOVA |
|
| Qualitative information | Damman et al. (2018) | Infographics |
|
| Infographics | Damman et al. (2018) | Qualitative information |
|
| Timeframes | |||
| Lifetime risk | Fair et al. (2008) | 10 year risk |
*ANOVA |
| 5, 10, 15 & 20 year risk | Frileux et al. (2004) | N/A each other |
*ANOVA with repeated measures |
| Genetic Risk Scores | Domenech et al. (2016) | No risk score |
*Pearson chi‐square test |
| Knowles et al. (2017) | Framingham risk score |
*Hodges‐Lehmann statistic |
|
| Cardiovascular imaging | |||
| Coronary artery calcium scores | Johnson et al. (2015) | No comparison |
*ANOVA |
| Orakzai et al. (2008) | No comparison |
*t test and Mann‐Whitney rank‐sum test |
|
| Kalia et al. (2006) | No comparison |
|
|
| Carotid ultrasounds | Näslund et al. (2019) | Percentages |
|
| Korcarz et al. (2008) | No comparison |
*multiple linear regression model |
|
TABLE 4.
Perceptions of risk communication strategy
| Risk communication strategy | Participant quotes |
|---|---|
| Numerical formats | |
| Numbers | ‘Going to make me go online or make an appointment with a doctor who can make it clearer’ (Ancker et al., 2009) |
| Percentages |
‘oh that’s only half of the risk! Let’s take a look…your risk is 42%. Then it could have been worse’ (Damman et al., 2016) ‘I have 2%...what does that mean…does that mean 2 days out of 100 I'm at risk?’ (Bonner et al., 2014) |
| Heart age |
‘I hate this 74 and 72, that's not real… The only one who can say what my heart age would be is the cardiologist when he goes in and has a look at my heart’ (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014) ‘I mean, I already feel that I am healthy‐ish for my age.. to me that says yeah you’re ok’ (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014) ‘Wow this is very good…It's an eye‐opener… oh yeah I'm overweight and this and that but never thinking that it (would) have such an impact on my heart’ (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014) ‘I'm thinking that it's kind of overwhelming. It's intimidating for a man to come in who is 52 and find out he's got a heart age of 79. I think it's going to be very upsetting. He’s gonna be really shaken’ (Goldman et al., 2006) ‘I think the idea of [cardiovascular risk‐adjusted age] made it personal. Because this is your age. It brought you into it’ (Goldman et al., 2006) |
| Graphical formats | |
| Bar graphs | ‘well I’m not above the 50%, I'm in the red zone but the lower part of it’ (Damman et al., 2016) |
| Icon arrays |
‘It's a lot to look at’ (Ancker et al., 2009) ‘clearer that you’re talking about human beings and not statistics’ (Ancker et al., 2009) ‘It can give a false reading’ (participant talking about random sequencing) (Ancker et al., 2009) |
| Game interaction | ‘It's like a game because you’re playing around with it. That's what I like about it because you learn too’ (Ancker et al., 2009) |
| Genetic Risk Score |
‘if you have a high genetic risk it's in your genes… deprived yourself of all your nice treats but you’ve had the same end result, you might as well have enjoyed it and gone!’ (Shefer et al., 2016) ‘If it's going to run in the family you’ve got to accept it haven'’t you? If it's your turn to, if your number comes up you can’t do nothing about it’ (Middlemass et al., 2014) ‘I was sure there was something in the family make up but it's nice to know that's not the case’ (Middlemass et al., 2014) ‘The lifestyle I have led puts me at a greater risk than the person who didn’t live my lifestyle’ (Middlemass et al., 2014) |
2.5. Quality appraisal
A quality assessment was undertaken for included studies by one reviewer (SS) and a second reviewer (AF) appraised 30% of the studies to ensure consistency (supplementary material online). The quality appraisal was based on criteria from the Critical Appraisal Skills Programme (CASP) tools for qualitative, randomized controlled trials, case‐controlled studies and cohort studies.
2.6. Data abstraction
Separate quantitative and qualitative data extraction forms were developed to collect data from eligible studies and included: location, study design, participant characteristics, data collection methods, risk communication strategy and outcome data. The data were then visually presented in a table.
2.7. Data synthesis
Due to the heterogeneity in study designs and outcomes, a meta‐analysis was not feasible. A narrative synthesis, which adopts a textual approach to summarize the findings of systematic reviews, was performed for the quantitative studies in accordance with the Economic and Social Research Council (ESRC) methods programme guidance on narrative synthesis in systematic reviews (Popay et al., 2006). The data extraction forms were used to produce a descriptive summary, organizing data by communication strategy. The study outcomes and results were then tabulated (Table 2). A narrative summary (Dixon‐Woods et al., 2004) was undertaken for the qualitative studies, and the data were summarized under the same categories. The quantitative and qualitative results were integrated and the reviewers used concept mapping to explore relationships by producing a commentary of the data.
3. RESULTS
3.1. Summary of findings
Nine different categories of cardiovascular risk communication strategies were identified and summarized under the following headings: numerical formats, graphical formats, qualitative information, infographics, avatars, game interactions, timeframes, genetic risk scores and cardiovascular imaging. In addition to these, the analysis of the qualitative studies identified multiple factors which may also influence risk communication. These have been categorized into pre‐assessment factors, mode of assessment, risk communication and post‐assessment (Figure 2 and Table S4).
FIGURE 2.
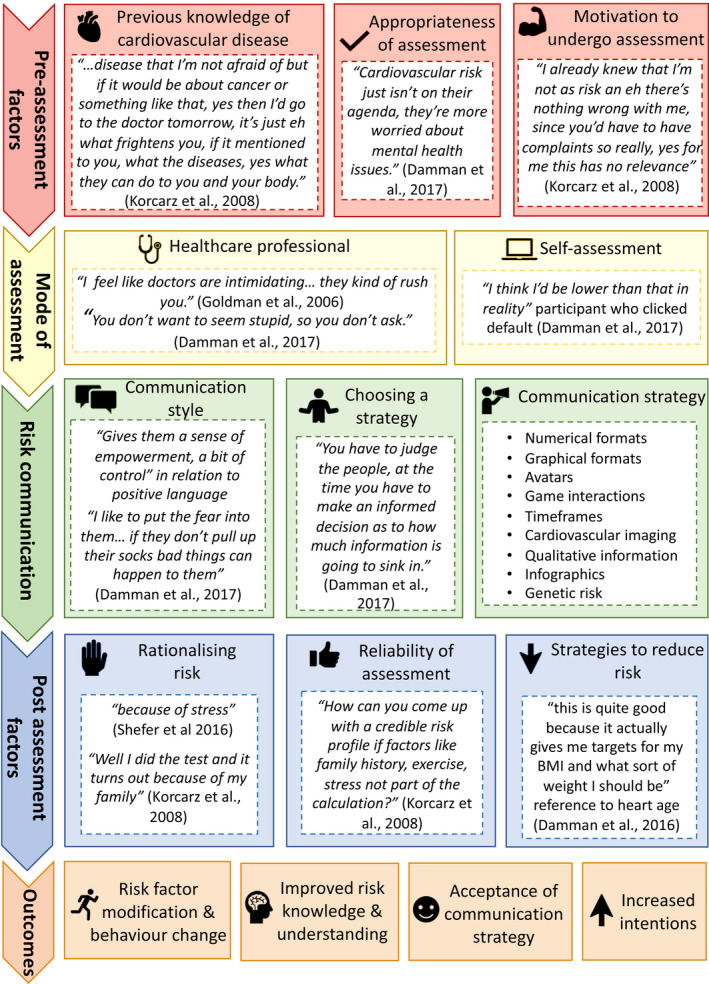
Factors during cardiovascular assessment that influence risk communication.
3.2. Study quality
Two of the qualitative studies scored low overall using the CASP risk appraisal tool and the remaining studies were of medium quality. The components with the poorest scores were rigour of data analysis, clarity of statement of findings and design. Two of the studies (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014; Hill et al., 2010) failed to describe the qualitative approach taken. Overall, most of the quantitative studies addressed a clearly focussed issue, considered all important outcomes and had results in keeping with existing evidence. Studies scored lower in recruitment strategies and generalizability of the results. This was attributable to several biases including recruitment of a majority or all‐male sample (Powers et al., 2011; Ruiz et al., 2013, 2016) and participants at low cardiovascular risk (Bonner et al., 2015; Lopez‐Gonzalez et al., 2015). A small proportion of studies scored low in minimizing bias while measuring outcomes (French et al., 2004) and reasons include using research‐developed tools as opposed to validated ones (Adarkwah et al., 2019).
3.3. Risk communication strategies
3.3.1. Numerical formats
This describes quantitative risk information provided as percentages, risk ratios or heart age scores and was investigated in eight studies (five quantitative and three qualitative). In a randomized trial, participants were more likely to agree that risk information was presented clearly and more helpful and reported less decisional conflict in choosing their preferred risk reduction method when presented with their Framingham risk score as opposed to risk factor education only (Powers et al., 2011). There were no differences in health behaviours, blood pressure or medication adherence and perceived risk declined in both groups at 3 months.
Damman et al. (2016) identified that providing estimates of the percentage of similar individuals who will have a cardiovascular event at a given time period failed to heighten risk perception as some participants believed a risk score below 50% implied low risk. Participants also had problems recalling percentages, especially when provided with multiple numbers from their assessment. This was reiterated in a second qualitative study (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014), where participants had difficulties remembering and understanding their risk percentage.
Only one quantitative study (Fair et al., 2008) investigated risk ratios by comparing them to percentages. Risk ratios increased risk perceptions and intentions to make lifestyle changes, however, also increased levels of worry.
The final numerical strategy evaluated was the use of an estimated heart age, which calculates an individual's heart age based on their risk profile, and was investigated in three quantitative studies. Bonner et al. (2015) compared the effect of providing individuals with their heart age against a percentage event rate at 5 years on behavioural and psychological outcomes. There was no significant difference in intention to change lifestyle or in risk perceptions. At 2 weeks, recall was highest in the heart age group but had significantly decreased since the intervention. Those with a younger heart age were more likely to recall their risk than those in the percentage group, however, there was no difference in recall between groups in participants with an older heart age. Participants in the heart age group, however, perceived the results to be less credible and had less of a positive emotional response.
Another study (Lopez‐Gonzalez et al., 2015) compared the effect of the heart age on modifiable cardiovascular risk factors against a percentage event rate and a control group, who received conventional medical advice only. At 12 weeks, there was a significant decrease in weight and smoking in both experimental groups compared with the control group but was accentuated in the heart age group. At 12 months, Framingham risk scores had increased in the control group but decreased in the heart age and percentage groups. When the heart age was compared with either a percentage or natural frequency, the heart age improved intentions to become more physically active and to visit a general practitioner (Damman et al., 2018).
Two qualitative studies addressed the acceptability of the heart age. High‐risk participants were less accepting of their results and questioned their credibility (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014). Those with a heart age that closely reflected their own age were also more reassured. In the study by Goldman et al. (2006), participants felt that the heart age score would be more memorable, but warned that receiving an older heart age may increase anxiety in individuals. A further qualitative study (Ancker et al., 2009) revealed that although some individuals were accepting numerical risk information, others found it too impersonal.
3.3.2. Graphical formats
The risk was visually represented in graphical formats in eight studies (six quantitative and two qualitative) including bar graphs and icon arrays. Risk recall was lower when presented as an icon array compared with a numerical format immediately post‐intervention, with no differences between the groups at 2–3 weeks on recall or understanding of risk (Ruiz et al., 2013). There were also no significant differences in perceptions of seriousness, intentions to change lifestyle, follow medical treatment or overall satisfaction. Moreover, there were no differences in clarity or helpfulness of the information between the groups. Additionally, participants who received their risk in a graphical format (bar graph or icon array) compared with a numerical format (percentage and risk ratio) reported lower levels of worry but were not more reassured (French et al., 2004).
In a randomized trial, where icon arrays were compared directly with bar graphs (Adarkwah et al., 2019), no differences were observed in the recall of interventions agreed on with a general practitioner at 3 months. Risk perceptions were highest in the bar graph group at 3 months but decreased in comparison with baseline, whereas it remained consistent in the icon array group. Additionally, in a second study, participants who were shown their risk as a bar graph had a higher perceived risk and were more likely to take preventative treatment than those who received an icon array (Navar et al., 2018). Conversely, a qualitative study (Damman et al., 2016) highlighted individuals may misinterpret the severity of their results when using bar graphs because high scores such as 20% appear to be in the lower portion of the graph.
The type of icon used also influenced perceptions and risk recall. The icons which performed better in risk recall were restroom icons and photographs with blocks and faces performing the worst (Zikmund‐Fisher et al., 2014). Mean perceived cardiovascular risk perceptions did not significantly differ and were moderately correlated with the actual risk information that was presented. Random rather than sequential positioning of negative icons to portray the chance of suffering a cardiovascular event was associated with better alignment between risk estimates and perceptions but reduced lifestyle intention scores (Witteman et al., 2014). Random dispersal was also reported as more realistic in a qualitative study. (Ancker et al., 2009). Participants found icon arrays with stick icons more personal and relatable than those which use shapes.
3.3.3. Avatars
Avatars are digital representations of people used to promote social interaction (Ruiz et al., 2016) and were addressed in two quantitative studies. Avatars improved overall risk perceptions among participants and alignments between risk estimates and intentions to see a doctor (Witteman et al., 2014). Conversely, no differences in risk recall or understanding were found when avatars were compared against voice and text alone (Ruiz et al., 2016). There were no significant differences in worry, disturbance or confidence to follow medical treatments, however, the avatar was favoured in intentions to make lifestyle changes.
3.3.4. Qualitative information
Qualitative information can be provided to individuals to help structure how a lay person thinks about risk. Qualitative information was investigated in one quantitative study. Participants were more likely to provide correct answers for risk recall and subjective risk comprehension questions when qualitative information was used to communicate risk compared with infographics.
3.3.5. Infographics
Infographics are sophisticated visualizations compromised of imagery, charts and text to provide an overview of a topic. They also provide additional narratives such as information about risk factors. One quantitative study investigated the use of infographics and found that infographics negatively influenced the recall of risk causes and subjective risk comprehension and more correct answers were given when qualitative information was used (Damman et al., 2018). Health literacy also influenced results as participants with adequate health literacy were more likely to consider infographic information useful.
3.3.6. Game interactions
Game‐like interactions are those which permit individuals to interact with the information provided to them (Ancker et al., 2009). Only one qualitative study (Ancker et al., 2009) investigated the use of an interactive game format to portray cardiovascular risk and involved clicking different icons to reveal which individuals would be affected by cardiovascular disease. Some participants enjoyed the interactive component which made it more like a game, whereas others found the process time‐consuming.
3.3.7. Timeframes
Time‐based risk formats allow for timeframe manipulations and can portray the accrual of risk over time. Timeframes were addressed in two quantitative studies. Participants who were shown their lifetime cardiovascular risk reported higher incidences of worry and were less reassured than participants who received a 10‐year cardiovascular risk (Fair et al., 2008). Similarly, in a study (Frileux et al., 2004), where five different timeframes (ranging from 5 to 20 years) were investigated, the shorter timeframes performed better. Higher intentions to adopt preventative behaviour were also reported when shorter timeframes were used.
3.3.8. Genetic risk scores
Genetic risk scores use statistical measures of genome variations that increase an individual’s probability of developing cardiovascular disease (Shefer et al., 2016). Four studies (two quantitative and two qualitative) investigated the use of providing individuals with feedback from a genetic risk score to communicate cardiovascular risk. Receiving a genetic risk score was associated with improved hypertension control at 16 weeks compared with participants who received no risk information in a randomized controlled trial. (Domenech et al., 2016). When comparing the Framingham risk score only to the Framingham risk score plus genetic risk score, there was no effect on low‐density lipoprotein cholesterol at 3 or 6 months. High‐risk participants in the genetic risk score group did, however, report a moderate loss in weight (Knowles et al., 2017).
Shefer et al. (2016) identified that when participants were provided with both their Framingham risk score and genetic risk score, they often only remembered one score and were unable to recall which one it was. Furthermore, participants often misunderstood their genetic risk score, believing if their risk was ‘in their genes’ it could not be modified. This misconception was also highlighted in a second qualitative study (Middlemass et al., 2014). One participant, however, recognized the importance of the gene and environment interaction and that lifestyle modification could reduce an increased genetic risk. Participants with a low genetic risk score felt reassured by their results, particularly those with a family history of cardiovascular disease (Middlemass et al., 2014).
3.3.9. Cardiovascular imaging
The results from cardiovascular imaging, including coronary artery calcium scoring and carotid ultrasound measurements, can be used to provide feedback to individuals about their current cardiovascular health and risk of a future event. Cardiovascular imaging was addressed in five quantitative studies. Three quantitative studies investigated the use of coronary artery calcium scores. The first (Johnson et al., 2015) provided participants with their coronary artery calcium score and verbal risk category. Overall, over two‐thirds of the participants could accurately identify their risk category based on their coronary artery calcium score. A significantly lower proportion of high‐risk participants identified that their score placed them in the high‐risk category. All five risk groups showed improvements in health‐promoting behaviour; however, there were no changes in risk perceptions over time. Worry was highest in the low‐risk group at baseline but highest in the moderate‐ and high‐risk groups at 3 months. In the other two studies, participants were provided with verbal information about their coronary artery calcium scores. The studies were similar in design and may include the same participants but reported different outcomes. Orakzai et al. (2008) determined that the number of participants who reported initiating aspirin therapy, increasing exercise and modifying their diet increased with increasing coronary artery calcium scores. Over half of the participants in the highest risk category reported modifying their diet and increasing exercise. In the second study (Kalia et al., 2006), statin compliance at 3 years was highest in participants with high coronary artery calcium scores and lowest in those with low‐risk scores. Overall, a large proportion of participants reported increasing exercise levels, stopping smoking and making dietary modifications.
In two studies, participants were provided with the results of their carotid ultrasound scan. In a randomized controlled trial, Framingham risk scores decreased at 1 year among participants who received a visualization of their scan result and increased in the group who received a risk score only (Näslund et al., 2019). Additionally, there was a greater reduction in low‐density lipoprotein cholesterol concentrations and smoking rates in the group who received a visualization of their carotid ultrasound. Korcarz et al. (2008) provided participants with verbal information about their carotid ultrasound. Participants with increased levels of plaque reported increased perceptions of having or developing heart disease and intentions to take cholesterol‐lowering medication.
3.4. Factors that impact on cardiovascular risk communication
3.4.1. Pre‐assessment factors
Three pre‐assessment factors were identified from the review including previous knowledge of cardiovascular disease. Some participants did not understand what cardiovascular disease encompassed and it was perceived as less frightening than cancer (Damman et al., 2017). Some believed that they had adequate knowledge of cardiovascular disease and risk factors, deeming themselves not at risk. This links to the second factor, which is motivation to undergo cardiovascular risk assessment. Some participants who believed that they were of low risk were unlikely to undergo screening, particularly when they had no physical complaints (Damman et al., 2017). The appropriateness of a cardiovascular assessment was also highlighted by healthcare professionals. They believed that if patients had more pressing health concerns, discussing their cardiovascular risk would place an additional burden on them (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014).
3.4.2. Mode of assessment
Self‐assessment and assessment by healthcare professionals were the two modes of cardiovascular assessment identified. Some participants felt that their doctor was too busy or intimidating to conduct an assessment (Ancker et al., 2009). They were also too embarrassed to request clarification if they did not comprehend their risk (Ancker et al., 2009). Online calculators allowed individuals to conduct their own assessment, but many underestimated their risk factor values and entered incorrect data (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014). Furthermore, if they did not understand their risk, they were unable to seek clarification from a healthcare professional.
3.4.3. Communication of risk
As well as choosing which communication strategy to use, healthcare professionals highlighted that they also use different communication styles. Some opt for paternalistic communication styles promoting fear, whereas others prefer to empower patients (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014). Furthermore, they identified that they chose which strategy to use based on how much information they believed patients could process. For example, they believed that colourful charts were most beneficial in patients with low health literacy (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014).
3.4.4. Post‐assessment
Three post‐assessment factors were identified including perceived reliability of assessment, rationalizing risk and reducing risk. Participants questioned the reliability of some probabilistic risk scores because they expected to provide more information about their health and behaviour (Damman et al., 2016). Many went on to rationalize their risk, blaming factors out of their control including stress or family history (Damman et al., 2016). One participant felt that the heart age score encouraged risk reduction as it provided a target to work towards (Bonner, Jansen, McKinn, et al., 2014; Bonner, Jansen, Newell, et al., 2014). Another participant identified that they would be more willing to take risk reduction measures if they had decided on them in partnership with their doctor (Sheridan et al., 2009).
4. DISCUSSION
This is the first systematic review of both quantitative and qualitative studies into cardiovascular risk communication strategies. Nine different categories of cardiovascular risk communication strategies were identified. The results reveal that multiple factors are involved in communicating cardiovascular risk which influence acceptance, risk understanding and health factor modification. We report that strategies providing the results of cardiovascular imaging and an estimation of heart age were the most effective at communicating cardiovascular risk. Conversely, those attempting to represent risk using bar charts, percentages and infographics were less successful.
Cardiovascular imaging feedback and estimates of heart health are both methods of portraying personalized risk information. This is more relatable and therefore enhances risk perceptions and drives behaviour change. This aligns with research conducted by Lawton (2002) which proposes that health behaviour change is reactive and not proactive. Providing individuals with physical evidence of cardiovascular diseases, such as is demonstrated on the scan or with a heart age above that of the actual age, may provide a cue to action. The heart age is more memorable and understandable because it conveys to individuals how suboptimal their heart is.
Individuals are less engaged in risk discussions when physical symptoms are absent, with many unaware symptoms of cardiovascular disease are not present until the cardiovascular disease is advanced. Cardiovascular imaging removes any uncertainties with the notion of risk by providing direct evidence of cardiovascular disease. This is in keeping with previous research where strategies which employed imaging or visual techniques were the most effective at communicating personalized risk (French et al., 2017). It is also important to consider the limitations associated with using cardiovascular imaging to communicate cardiovascular risk. Imaging is more time‐consuming and expensive than traditional methods and imaging technologies may not be readily available or accessible in developing countries. Moreover, it may provide false reassurance as normal scans in young individuals with unhealthy lifestyles may incorrectly suggest that they can continue with their current lifestyle.
Several risk communication strategies, such as percentages, bar graphs and icon arrays, which provide patients with a probability, fail to heighten risk perceptions (Damman et al., 2016). Many of the most commonly used cardiovascular risk scores, such as the Framingham score, classify a 20% risk of developing cardiovascular disease over the next 10 years as high. As 20% appears in the lower portion of the graphs, these scores can be interpreted as low risk. The same is true for icon arrays as a large number of positive icons makes it easy for participants to believe that they would be one of the individuals not affected (Ancker et al., 2009).
The genetic risk score also provides individuals with a probabilistic risk score. One study claimed that providing a genetic risk score improved blood pressure control (Domenech et al., 2016). It is difficult to establish if this was the result of receiving a genetic risk score or an improved awareness of risk because the control group received no risk information. Participants believed that their genetic risk could not be modified and consequently were less motivated to make lifestyle improvements. The genetic risk assessment and gene and lifestyle interaction require more explanation to individuals.
In addition to the communication strategy, it was identified that a wider range of factors can influence the success of cardiovascular risk communication. These factors may affect how well a particular strategy works and highlights individuals may perceive risk differently based on their values, environment and relationship with a health professional. This is in keeping with the first two components of de Haes and Bensing’s medical communication model (de Haes & Bensing, 2009). The first element involves fostering a relationship with patients. Healthcare professionals must ensure an open and transparent relationship, where patients feel empowered to ask questions. Second, before providing risk information professionals should gather information from patients, enabling them to understand patient beliefs and values and choose the best communication strategy. The other components of the model include decision‐making, enabling disease and treatment‐related behaviour and responding to emotions.
Responding to emotions is also crucial and those involved in risk discussions must recognize the potential negative impact of being identified as high risk. Those designated as being at risk who previously viewed themselves as healthy are now faced with a revised health status despite lacking the associated symptoms (Gillespie, 2015). This may bring new social manifestations and health regimes similar to those who are ill. Care must be taken when broaching high‐risk discussions and professionals must offer suitable support.
4.1. Strengths and limitations
This is the first systematic review of quantitative and qualitative studies into cardiovascular risk communication strategies and included a large number of studies from a range of countries. The narrative synthesis approach enabled an overview of the large and diverse evidence base. As this review involved both quantitative and qualitative studies, we were able to expand on the quantitative results by identifying other factors which influence the success of cardiovascular risk communication.
It is, however, important to address the limitations associated with this review. First, narrative synthesis analysis is open to subjective interpretation. However, the inclusion of tabulated data helps ensure transparency. The studies were conducted in high‐income western countries and the cultural bias of the investigators may have influenced their lens of inquiry and analysis. In addition, despite no language restrictions, all studies were published in English, which may have excluded important cultural contexts. This may affect the generalizability of the results, as individuals’ cultural backgrounds and beliefs impact their perceptions of healthcare and lifestyle practices. Another limiting factor is that some of the studies provided participants with hypothetical risk scenarios, which may not have elicited true emotional responses. In addition, some of the studies included participants with low cardiovascular risk or those interested in their health. It is also possible that partaking in research led to participants overestimating health behaviours particularly in the self‐reported data. Some of the included risk communication strategies could be considered complex interventions and it can be difficult to unpick the active ingredient with the success dependent on many factors. Healthcare professionals must consider the optimization of the communication strategy in their setting.
5. CONCLUSION
The cardiovascular risk communication strategy which had the most significant impact on cardiovascular health behaviours and risk factors were those which used cardiovascular imaging. More high‐quality randomized controlled trials are required to confirm these findings and determine the effect of these strategies on long‐term behaviour change and other important clinical outcomes such as reduced cardiovascular mortality. Qualitative studies into individuals’ perceptions of cardiovascular imaging risk communication strategies would also help to identify the key components contributing to its benefits as a risk communication strategy. Our findings, however, suggest that future risk communication strategies would be more successful if they incorporated methods to provide individuals with evidence of their current cardiovascular health status.
AUTHORS’ CONTRIBUTION
SS, NLM, FS and LN conceived the study and its design. SS, FS, KJ and AF conducted the searches and performed the screening. SS and AF performed the quality assessment for included studies. SS acquired and interpreted the data. AF, FS and LM provided feedback on the qualitative analysis. SS, NLM, LN and FS drafted the manuscript. All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE: http://www.icmje.org/recommendations/):
substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
drafting the article or revising it critically for important intellectual content.
FUNDING INFORMATION
This study was funded by a British Heart Foundation Research Training Fellowship for Nurses and Healthcare Professionals Clinical (FS/RTF/21/30028) awarded to SS. NLM is supported by a Chair Award, Programme Grant and Research Excellence Award (CH/F/21/90010, RG/20/10/34966 and RE/18/5/34216) from the British Heart Foundation.
CONFLICT OF INTEREST
No conflict of interest has been declared by the author(s).
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15327.
Supporting information
Appendix S1. Xxxx
Appendix S2. Xxxx
Appendix S3. Xxxx
ACKNOWLEDGEMENTS
Marshall Dozier, Academic Support Librarian, for providing assistance and advice during the preparation of the search strategy. PROSPERO Registration Number: CRD42020204797.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Adarkwah, C. C. , Jegan, N. , Heinzel‐Gutenbrunner, M. , Kühne, F. , Siebert, U. , Popert, U. , Donner‐Banzhoff, N. , & Kürwitz, S. (2019). The Optimizing‐Risk‐Communication (OptRisk) randomized trial ‐ impact of decision‐aid‐based consultation on adherence and perception of cardiovascular risk. Patient Preference and Adherence, 13, 441–452. 10.2147/PPA.S197545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed, H. , Naik, G. , Willoughby, H. , & Edwards, A. G. K. (2012). Communicating risk. BMJ, 344, e3996. 10.1136/bmj.e3996 [DOI] [PubMed] [Google Scholar]
- Ancker, J. S. , Chan, C. , & Kukafka, R. (2009). Interactive graphics for expressing health risks: Development and qualitative evaluation. Journal of Health Communication, 14(5), 461–475. 10.1080/10810730903032960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner, C. , Jansen, J. , McKinn, S. , Irwig, L. , Doust, J. , Glasziou, P. , & McCaffery, K. (2014). Communicating cardiovascular disease risk: An interview study of General Practitioners' use of absolute risk within tailored communication strategies. BMC Family Practice, 15(100967792), 106. 10.1186/1471-2296-15-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner, C. , Jansen, J. , Newell, B. , Irwig, L. , Glasziou, P. , Doust, J. , Dhillon, H. , & McCaffery, K. (2014). I don't believe it, but i'd better do something about it: Patient experiences of online heart age risk calculators. Journal of Medical Internet Research, 16(5), 118–129. 10.2196/jmir.3190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner, C. , Jansen, J. , Newell, B. R. , Irwig, L. , Teixeira‐Pinto, A. , Glasziou, P. , Doust, J. , McKinn, S. , & McCaffery, K. (2015). Is the "Heart Age" concept helpful or harmful compared to absolute cardiovascular disease risk? An experimental study. Medical Decision Making, 35(8), 967–978. 10.1177/0272989X15597224 [DOI] [PubMed] [Google Scholar]
- Cooney, M. T. , Dudina, A. L. , & Graham, I. M. (2009). Value and limitations of existing scores for the assessment of cardiovascular risk: A review for clinicians. Journal of the American College of Cardiology (JACC), 54(14), 1209–1227. 10.1016/j.jacc.2009.07.020 [DOI] [PubMed] [Google Scholar]
- Damman, O. C. , Bogaerts, N. M. M. , van den Haak, M. J. , & Timmermans, D. R. M. (2017). How lay people understand and make sense of personalized disease risk information. Health Expectations, 20(5), 973–983. 10.1111/hex.12538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damman, O. C. , Bogaerts, N. M. M. , van Dongen, D. , & Timmermans, D. R. M. (2016). Barriers in using cardiometabolic risk information among consumers with low health literacy. British Journal of Health Psychology, 21(1), 135–156. 10.1111/bjhp.12149 [DOI] [PubMed] [Google Scholar]
- Damman, O. C. , Vonk, S. I. , van den Haak, M. J. , van Hooijdonk, C. M. J. , & Timmermans, D. R. M. (2018). The effects of infographics and several quantitative versus qualitative formats for cardiovascular disease risk, including heart age, on people's risk understanding. Patient Education and Counseling, 101(8), 1410–1418. 10.1016/j.pec.2018.03.015 [DOI] [PubMed] [Google Scholar]
- de Haes, H. , & Bensing, J. (2009). Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Education and Counseling, 74(3), 287–294. 10.1016/j.pec.2008.12.006 [DOI] [PubMed] [Google Scholar]
- Dixon‐Woods, M. , Agarwal, S. , Young, B. , Jones, D. , & Sutton, A. (2004). Integrative approaches to qualitative and quantitative evidence. NHS Health Development Agency. [Google Scholar]
- Domenech, M. , Elosua, R. , Salas, E. , Sierra, C. , Marrugat, J. , & Coca, A. (2016). Awareness of genetic coronary risk score improves blood pressure control in hypertensive patients. Revista espanola de cardiologia (English ed.), 69(12), 1226–1227. 10.1016/j.rec.2016.06.017 [DOI] [PubMed] [Google Scholar]
- Fair, A. K. I. , Murray, P. G. , Thomas, A. , & Cobain, M. R. (2008). Using hypothetical data to assess the effect of numerical format and context on the perception of coronary heart disease risk. American Journal of Health Promotion, 22(4), 291–296. 10.4278/061030140R2.1 [DOI] [PubMed] [Google Scholar]
- French, D. , Cameron, E. , Benton, J. , Deaton, C. , Harvie, M. , French, D. P. , & Benton, J. S. (2017). Can communicating personalised disease risk promote healthy behaviour change? A systematic review of systematic reviews. Annals of Behavioral Medicine, 51(5), 718–729. 10.1007/s12160-017-9895-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- French, D. P. , Kinmonth, A. L. , Marteau, T. M. , & Sutton, S. R. (2004). The impact of personal and social comparison information about health risk. British Journal of Health Psychology, 9(2), 187–200. https://search.proquest.com/docview/57225568?accountid=10673 [DOI] [PubMed] [Google Scholar]
- Frileux, S. , Munoz Sastre, M. T. , Mullet, E. , & Sorum, P. C. (2004). The impact of the preventive medical message on intention to change behavior. Patient Education and Counseling, 52(1), 79–88. [DOI] [PubMed] [Google Scholar]
- Gillespie, C. (2015). The risk experience: The social effects of health screening and the emergence of a proto‐illness. (1467‐9566 [Electronic]). [DOI] [PubMed]
- Goldman, R. E. , Parker, D. R. , Eaton, C. B. , Borkan, J. M. , Gramling, R. , Cover, R. T. , & Ahern, D. K. (2006). Patients' perceptions of cholesterol, cardiovascular disease risk, and risk communication strategies. Annals of Family Medicine, 4(3), 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayman, L. L. , Berra, K. , Fletcher, B. J. , & Houston Miller, N. (2015). The role of nurses in promoting cardiovascular health worldwide: The Global Cardiovascular Nursing Leadership Forum. (1558‐3597 [Electronic]). [DOI] [PubMed]
- Hill, S. , Spink, J. , Cadilhac, D. , Edwards, A. , Kaufman, C. , Rogers, S. , Ryan, R. , & Tonkin, A. (2010). Absolute risk representation in cardiovascular disease prevention: Comprehension and preferences of health care consumers and general practitioners involved in a focus group study. BMC Public Health, 10(100968562), 108. 10.1186/1471-2458-10-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollands, G. J. , Hankins M Fau ‐ Marteau, T. M. , & Marteau, T. M. (2010). Visual feedback of individuals' medical imaging results for changing health behaviour. (1469‐493X [Electronic]). [DOI] [PubMed]
- Johnson, J. E. , Gulanick, M. , Penckofer, S. , & Kouba, J. (2015). Does knowledge of coronary artery calcium affect cardiovascular risk perception, likelihood of taking action, and health‐promoting behavior change? The Journal of Cardiovascular Nursing, 30(1), 15–25. 10.1097/JCN.0000000000000103 [DOI] [PubMed] [Google Scholar]
- Kalia, N. K. , Miller, L. G. , Nasir, K. , Blumenthal, R. S. , Agrawal, N. , & Budoff, M. J. (2006). Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis, 185(2), 394–399. 10.1016/j.atherosclerosis.2005.06.018 [DOI] [PubMed] [Google Scholar]
- Knowles, J. W. , Zarafshar, S. , Pavlovic, A. , Goldstein, B. A. , Tsai, S. , Li, J. , McConnell, M. V. , Absher, D. , Ashley, E. A. , Kiernan, M. , Ioannidis, J. P. A. , & Assimes, T. L. (2017). Impact of a genetic risk score for coronary artery disease on reducing cardiovascular risk: A pilot randomized controlled study. Frontiers in Cardiovascular Medicine, 4. 10.3389/fcvm.2017.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korcarz, C. E. , Decara, J. M. , Hirsch, A. T. , Mohler, E. R. , Pogue, B. , Postley, J. , Tzou, W. S. , Stein, J. H. , Korcarz, C. E. , DeCara, J. M. , Hirsch, A. T. , Mohler, E. R. , Pogue, B. , Postley, J. , Tzou, W. S. , & Stein, J. H. (2008). Ultrasound detection of increased carotid intima‐media thickness and carotid plaque in an office practice setting: Does it affect physician behavior or patient motivation? Journal of the American Society of Echocardiography, 21(10), 1156–1162. 10.1016/j.echo.2008.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton, J. (2002). Colonising the future: Temporal perceptions and health‐relevant behaviours across the adult lifecourse. Sociology of Health & Illness, 24(6), 714–733. 10.1111/1467-9566.00315 [DOI] [Google Scholar]
- Lopez‐Gonzalez, A. A. , Aguilo, A. , Frontera, M. , Bennasar‐Veny, M. , Campos, I. , Vicente‐Herrero, T. , Tomas‐Salva, M. , De Pedro‐Gomez, J. , & Tauler, P. (2015). Effectiveness of the Heart Age tool for improving modifiable cardiovascular risk factors in a Southern European population: A randomized trial. European Journal of Preventive Cardiology, 22(3), 389–396. 10.1177/2047487313518479 [DOI] [PubMed] [Google Scholar]
- Middlemass, J. B. , Yazdani, M. F. , Kai, J. , Standen, P. J. , & Qureshi, N. (2014). Introducing genetic testing for cardiovascular disease in primary care: A qualitative study. The British Journal of General Practice, 64(622), e282–e289. 10.3399/bjgp14X679714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. BMJ, 339, b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Näslund, U. , Ng, N. , Lundgren, A. , Fhärm, E. , Grönlund, C. , Johansson, H. , Lindahl, B. , Lindahl, B. , Lindvall, K. , Nilsson, S. K. , Nordin, M. , Nordin, S. , Nyman, E. , Rocklöv, J. , Vanoli, D. , Weinehall, L. , Wennberg, P. , Wester, P. , & Norberg, M. (2019). Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): A pragmatic, open‐label, randomised controlled trial. Lancet, 393, 133–142. 10.1016/S0140-6736(18)32818-6 [DOI] [PubMed] [Google Scholar]
- Navar, A. M. , Wang, T. Y. , Mi, X. J. , Robinson, J. G. , Virani, S. S. , Roger, V. L. , Wilson, P. W. F. , Goldberg, A. C. , & Peterson, E. D. (2018). Influence of cardiovascular risk communication tools and presentation formats on patient perceptions and preferences. JAMA Cardiology, 3(12), 1192–1199. 10.1001/jamacardio.2018.3680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orakzai, R. H. , Nasir, K. , Orakzai, S. H. , Kalia, N. , Gopal, A. , Musunuru, K. , Blumenthal, R. S. , & Budoff, M. J. (2008). Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. The American Journal of Cardiology, 101(7), 999–1002. 10.1016/j.amjcard.2007.11.059 [DOI] [PubMed] [Google Scholar]
- Popay, J. , Roberts, H. , Sowden, A. , Petticrew, M. , Arai, L. , Rodgers, M. , Britten, N. , Roen, K. , & Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC Methods Programme. 10.13140/2.1.1018.4643 [DOI]
- Powers, B. J. , Danus, S. , Grubber, J. M. , Olsen, M. K. , Oddone, E. Z. , & Bosworth, H. B. (2011). The effectiveness of personalized coronary heart disease and stroke risk communication. American Heart Journal, 161(4), 673–680. [DOI] [PubMed] [Google Scholar]
- Rossello, X. , Dorresteijn, J. A. , Janssen, A. , Lambrinou, E. , Sherrenberg, M. , Bonnefoy‐Cudraz, E. , Cobain, M. , Piepoli, M. F. , Visseren, F. L. , & Dendale, P. (2019). Risk Prediction Tools in Cardiovascular Disease Prevention: A Report From the ESC Prevention of CVD Programme Led by the European Association of Preventive Cardiology (EAPC) in Collaboration With the Acute Cardiovascular Care Association (ACCA) and the Association of Cardiovascular Nursing and Allied Professionals (ACNAP). European Journal of Preventive Cardiology, 26(14), 1534–1544. 10.1177/2047487319846715 [DOI] [PubMed] [Google Scholar]
- Ruiz, J. G. , Andrade, A. D. , Garcia‐Retamero, R. , Anam, R. , Rodriguez, R. , & Sharit, J. (2013). Communicating global cardiovascular risk: Are icon arrays better than numerical estimates in improving understanding, recall and perception of risk? Patient Education and Counseling, 93(3), 394–402. 10.1016/j.pec.2013.06.026 [DOI] [PubMed] [Google Scholar]
- Ruiz, J. G. , Andrade, A. D. , Karanam, C. , Krishnamurthy, D. , Nino, L. , Anam, R. , & Sharit, J. (2016). The communication of global cardiovascular risk by avatars. Studies in Health Technology and Informatics, 220(ck1, 9214582), 341–344. [PubMed] [Google Scholar]
- Shefer, G. , Silarova, B. , Usher‐Smith, J. , & Griffin, S. (2016). The response to receiving phenotypic and genetic coronary heart disease risk scores and lifestyle advice ‐ A qualitative study. BMC Public Health, 16(1), 1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan, S. L. , Behrend, L. , Vu, M. B. , Meier, A. , Griffith, J. M. , & Pignone, M. P. (2009). Individuals' responses to global CHD risk: A focus group study. Patient Education and Counseling, 76(2), 233–239. 10.1016/j.pec.2009.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson, R. , Edwards A., Grey J. (2015). Risk communication in the clinical consultation. (1470‐2118 (Print; )). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmis, A. , Townsend, N. , Gale, C. , Grobbee, R. , Maniadakis, N. , Flather, M. , Wilkins, E. , Wright, L. , Vos, R. , Bax, J. , Blum, M. , Pinto, F. , Vardas, P. , & Group, E. S. D . (2018). European Society of Cardiology: Cardiovascular Disease Statistics 2017. European Heart Journal, 39(7), 508–579. 10.1093/eurheartj/ehx628 [DOI] [PubMed] [Google Scholar]
- Tong, A. , Flemming, K. , McInnes, E. , Oliver, S. , & Craig, J. (2012). Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology, 12(1), 181. 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witteman, H. O. , Fuhrel‐Forbis, A. , Wijeysundera, H. C. , Exe, N. , Dickson, M. , Holtzman, L. , Kahn, V. C. , & Zikmund‐Fisher, B. J. (2014). Animated randomness, avatars, movement, and personalization in risk graphics. Journal of Medical Internet Research, 16(3), e80. 10.2196/jmir.2895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . (2017). Fact Sheets: Cardiovascular diseases (CVD). https://www.who.int/en/news‐room/fact‐sheets/detail/cardiovascular‐diseases‐(cvds)
- Zikmund‐Fisher, B. J. , Witteman, H. O. , Dickson, M. , Fuhrel‐Forbis, A. , Kahn, V. C. , Exe, N. L. , Valerio, M. , Holtzman, L. G. , Scherer, L. D. , & Fagerlin, A. (2014). Blocks, ovals, or people? Icon type affects risk perceptions and recall of pictographs. Medical Decision Making, 34(4), 443–453. 10.1177/0272989X13511706 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Xxxx
Appendix S2. Xxxx
Appendix S3. Xxxx
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


