RANZCR needs to stay modern and allow candidates the opportunity to subspecialise and move their careers forward. – Clinical Radiology Trainee Oct 2020.
Background
There is a growing demand for subspecialty training in radiology, as demonstrated by the 46.0%/67.9% (Australia/New Zealand) of radiologists and 55.9% of new fellows who have previously or are currently undertaking subspecialty fellowship training beyond attainment of Fellowship of the Royal Australian and New Zealand College of Radiologists (FRANZCR). 1 , 2 The clinical radiologist plays a key role in patient care and multidisciplinary discussions and access to accredited subspecialty training is of utmost importance to remain at the peak of current knowledge and beyond.
Having said that, however, a trainee cannot train forever. Such is the complexity of modern radiology work that it is unfeasible to attain and maintain subspecialist level knowledge in all areas, and unreasonable to continuously add further training years beyond attainment of FRANZCR. In addition to this, there are currently fewer overall training years after medical school graduation required for areas including nuclear medicine and cardiac imaging via the Royal Australasian College of Physicians (RACP) 3 training pathways than RANZCR.
Furthermore, several areas of radiology practice have become microcredentialled after strong influence from nonradiologists, including cardiac CT and colonography, as well as a recent near‐miss with prostate MRI. Moving forward, it is essential for the radiology community to govern and credential our own subspecialty training. The longer we delay this body of work, the higher the risk it will be done by practitioners external to us, without our best interests foremost.
Overseas models
Radiology colleges around the world, including the United Kingdom and North American colleges, have moved to models of integrated subspecialty training. In the United Kingdom, trainees follow a 3 + 2 model, whereby the first 3 years are for general ‘Clinical Radiology Training’ followed by 2 years of ‘Special Interest Training with maintenance and development of general radiology skills’. 4 Areas of special interest include paediatric, musculoskeletal, neurological, thoracic and breast radiology. Interventional radiology (IR) in the UK follows a 3 + 3 model. 4 Further, specific curricula with learning objectives have been defined for breast, neurological and interventional radiology.
In North America, the percentage of radiologists practising as subspecialists, defined as 50% or more of work in a given subspecialty area, has risen from 37.1% in 2012 to 44.6% in 2017. 5 The US training model reflects this, with 4 years of general radiology training followed by an optional fifth ‘subspecialty fellowship’ year, which is undertaken by approximately 90% of trainees. There is also a 5 year ‘integrated IR residency’ training programme comprising 3 years of diagnostic radiology and 2 years of IR. 6
Artificial intelligence
The era of artificial intelligence (AI) in radiology has arrived, and it is likely that the first areas of radiology to be automated are high volume and low complexity tasks, such as
Detection of haemorrhage on CT Brain
Detection of pulmonary embolism on CTPA
Chest x‐ray critical findings and alerts (e.g. pneumothorax)
Detection of fracture on x‐ray.
In fact, AI products for these applications and more already exist. 7
As AI technologies improve, further areas of diagnostic work will become at least partly automated, and areas where radiologist input may be of highest value include:
Complex diagnostic interpretation (multimodality, evolution of findings over time, multisystem disease and troubleshooting of AI findings)
Multidisciplinary meetings
Procedural work.
These areas are at the peak of subspecialty knowledge, and it is vital that radiologists have subspecialty training to add value. This requires a strong framework of accredited and integrated subspecialty training by RANZCR.
Comparable specialty college in Australia and New Zealand
While RANZCR is a small college in comparison to larger subspecialised colleges such as RACP, RANZCR is comparable in size to the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG);
RANZCR: 1801 specialists, 486 trainees (2016 & 2018 Aust. Dept of Health data)
RANZCOG: 1742 specialists, 552 trainees (2016 & 2018 Aust. Dept of Health data).
RANZCOG has 4 years of core training followed by 2 years of advanced training, 8 with five subspecialty areas:
Gynaecological Oncology
Maternal Foetal Medicine
Obstetrical and Gynaecological Ultrasound
Reproductive Endocrinology and Infertility
Urogynaecology.
This comparator addresses the common misconception that radiology in Australia and New Zealand is too small for subspecialisation. The end goal is not siloed and fragmented subspecialisation, but rather upskilling in key areas to add value to robust general skills. A further advantage is that radiologists could demonstrate their advanced training credentials in areas of shared practice with other specialities (e.g. obstetric ultrasound and endovascular surgery).
Survey of clinical radiology trainees
Given that the current clinical radiology training programme commencing in 2022 does not allow for subspecialty training with the exception of nuclear medicine, 9 a short survey was designed using Google forms to determine the sentiment of clinical radiology trainees in Australia and New Zealand. The survey provided background information and invited trainees to indicate their relative support on a Likert scale for each of the following three models:
5 year model of general radiology training with subspecialty fellowships commencing after FRANZCR
4 + 1 or 4 + 2 model. Fifth (and sixth if desired) year trainees can focus on one (or more) specific subspecialty areas after completion of examinations in fourth year, as dual training Australian nuclear medicine trainees currently do. Trainees would still spend a portion of time (20–30%) in general radiology, with the remaining time in the subspecialty
3 + 2 or 3 + 3 model. Fourth and fifth (and sixth if desired) year trainees can focus on one (or more) subspecialty areas of radiology, as FRCR interventional radiology trainees currently do. Trainees would still spend a portion of time (20–30%) in general radiology, with the remaining time in the subspecialty.
The survey was emailed to all clinical radiology trainees by the chair of the clinical radiology trainees committee, with approval from RANZCR. Guidance was provided by the author's local institutional ethics committee that this represented a quality improvement and evaluation activity.
A total of 50 anonymised responses were received, representing over 10% of the total trainee cohort (Fig. 1). The most preferred model was a 4 + 1 or 4 + 2 model (with accredited subspecialty certification), indicating a clear preference for integrated subspecialty training in the FRANZCR programme.
Fig. 1.
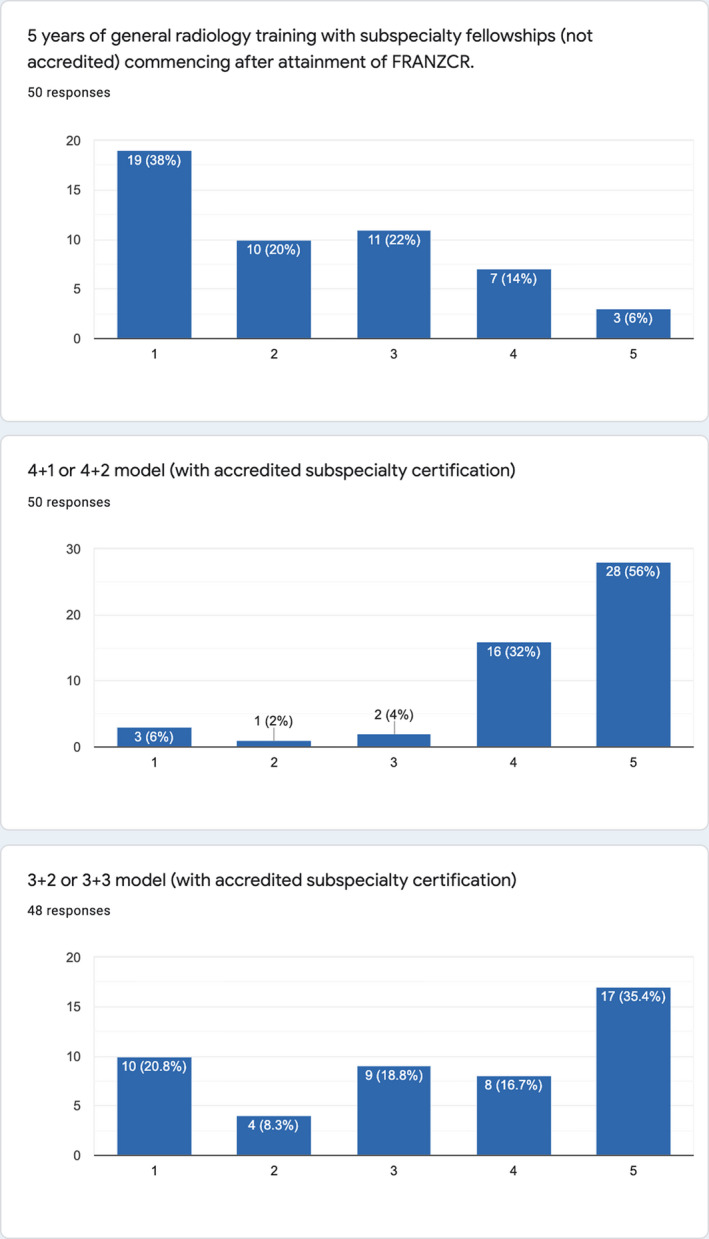
Survey results. Y axis: Number of responses. X axis: Rated from 1 (weakest support) to 5 (strongest support).
Suggested model for FRANZCR integrated subspecialty training and discussion
A suggested model of integrated FRANZCR subspecialty training based on results received is as follows.
Phase 1 and 2 of training would include completion of all examinations (part 1 and part 2) over 4 years. Phase 3 of training would be dedicated subspecialty training in areas of the trainee's choosing. Trainees would retain the ability to attain FRANZCR after the fifth year, with an optional sixth year for trainees wanting to complete further subspecialty training.
A reasonable breakdown of work during subspecialty training is at least 3.5 days in the subspecialty. This, in addition to continual contribution to the after‐hours roster, will ensure that trainees continue to develop general radiology proficiency.
The amount of time required for training in each subspecialty will be a decision for that particular craft group. For example, Nuclear Medicine is prescribed as 2 years of training by the Committee for Joint College Training in Nuclear Medicine. 10 Other currently informal fellowships in diagnostic neurological, thoracic and breast radiology are generally undertaken as programmes of 1 year or 6 months. As systems develop, the subspecialty leadership groups can determine the duration, learning objectives and assessments required for achievement of credentialed subspecialty training in that area, as seen in the UK and USA. The interventional radiology training programmes at RANZCR currently under development would likely align well with this proposed model.
There are a number of key advantages of integrated subspecialty training:
Subspecialty training to prepare trainees for the future of radiology practice
Credentialled subspecialty learning objectives and assessments, with key competencies that can be shown to relevant employers and regulatory bodies (e.g. hospitals and governments)
Control of subspecialisation in our profession, by our profession. We can determine how to define a subspecialist radiologist and govern the training credential
Defined and reasonable length of training, rather than informal fellowships added onto 5 years of general training.
Conclusion
Integrating subspecialty training into the curriculum and broader college structure requires immense work, but it is vital for the future of our profession. This is not simply the opinion of a few, it is the demonstrated preference of current clinical radiology trainees, the future of our profession. As radiology continues to evolve towards subspecialisation, let us define what this means ourselves as a profession and ensure that it is developed in the best possible way for our colleagues.
Acknowledgement
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
M Lukies MBBS (Hons), FRANZCR, MMed (Radiology).
Conflict of interest: None.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. The Royal Australian and New Zealand College of Radiologists 2016 Workforce survey report. [Cited 02 Mar 2021.] Available from URL: www.ranzcr.com
- 2. The Royal Australian and New Zealand College of Radiologists 2017 Clinical radiology new fellows survey report. [Cited 02 Mar 2021.] Available from URL: www.ranzcr.com
- 3.The Royal Australasian College of Physicians training curricula, 2021. [Cited 02 Mar 2021.] Available from URL: https://www.racp.edu.au/trainees
- 4. The Royal College of Radiologists Radiology curricula, 2021. [Cited 02 Mar 2021.] Available from URL: https://www.rcr.ac.uk/clinical‐radiology/specialty‐training/radiology‐curricula
- 5. Rosenkrantz AB, Hughes DR, Duszak R Jr. Increasing subspecialization of the National Radiologist Workforce. J Am Coll Radiol 2020; 17: 812–8. [DOI] [PubMed] [Google Scholar]
- 6.The American Board of Radiology Diagnostic and Interventional Radiology training pathways, 2021. [Cited 02 Mar 2021.] Available from URL: https://www.theabr.org/
- 7. Aidoc homepage, 2021. [Cited 02 Mar 2021.] Available from URL: https://www.aidoc.com/
- 8. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists Specialist Training, FRANZCOG Training Program, 2021. [Cited 02 Mar 2021.] Available from URL: https://ranzcog.edu.au/training/specialist‐training
- 9. The Royal Australian and New Zealand College of Radiologists Clinical Radiology Handbook, 2021. [Cited 02 Mar 2021.] Available from URL: www.ranzcr.com
- 10.The Australasian Association of Nuclear Medicine Specialists, Education and Training, 2021. AANMS website. [Cited 01 Dec 2021.] Available from URL: https://aanms.org.au/education‐and‐training/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


