Abstract
The purpose of the study was to investigate the influence of multiple factors on the survival of tooth‐supported single crowns and assess the biological and technical complications. This retrospective study included patients rehabilitated with single crowns with a minimum follow‐up time of 6 months after delivery. The cumulative survival rate was calculated over the maximum period of follow‐up time and reported in a life‐table survival analysis. Univariate and multivariate Cox regression was used to evaluate the associations between clinical covariates and crown failure. The included cohort group consisted of 1037 single crowns delivered in 401 patients and followed for a mean of 134.8 ± 80.2 months. Cumulative survival rate was 89.9% and 80.9% after 5 and 10 years and 70.5% and 61.8% after 15 and 20 years, respectively. The main reasons for single crown failure were loss of retention, tooth loss, and fracture. Anterior placement, non‐vital abutments, and bruxism significantly influenced the survival of single crowns. The survival of single crowns was not influenced by patient's age and sex, location of the crowns in relation to the jaws, type of tooth, presence of post and core, and type of crown material, treatment providers, or smoking. Anterior placement, non‐vital abutments, and bruxism are factors suggested to increase the risk of single crown failure and the prevalence of technical and biological complications.
Keywords: post and core, single crown, survival rate, technical and biological complications, tooth vitality
INTRODUCTION
Missing coronal tooth structure due to caries and/or trauma can be restored by dental restorations [1]. The amount of remaining tooth structure is the main factor determining the type of coronal restoration, that is, whether to use full or partial coverage restorations, and also influences the type of material to be used, for example, amalgam, composite, glass ionomer, ceramic, or metal [2]. Short‐ and long‐term clinical performance of tooth‐supported single crowns have been reported by several studies. The estimated survival rates at short‐ to medium‐term follow‐up, up to 5 years, have been reported to range between 93.3%–96.6% [3, 4] and 85.4% after a period of 25 years of function [5]. Failures do occur and it is important to investigate the cause of failures in order to improve the prognosis.
Single crowns are subjected to several clinical circumstances which could influence the survival and complication rates. One such variable is tooth vitality. Interdental receptors in the dental pulp have a protective role against harmful overloading force and this could be reduced or lost in non‐vital teeth [6]. Furthermore, loss of tooth structure following endodontic and subsequent restorative treatments could weaken the tooth and increase susceptibility of fracture [7, 8]. When the remaining coronal tooth structure is insufficient to retain a restoration, a post is needed [1, 9]. Presence of a post could increase the stress on the root surface and subsequently increase the risk of tooth fracture [10, 11]. Another variable that could affect the survival of single crowns is the magnitude of biting force which is affected by several factors such as patient's age, sex, tooth location, status of the dentition, opposing arch, and bruxism [11, 12, 13, 14, 15, 16, 17, 18].
Single crowns may be fabricated from several materials such as metals, metal‐ceramics, or all‐ceramics. The type of restorative material may affect the clinical outcome of single crowns [19]. Metal and zirconia frameworks are generally covered by a porcelain veneer [5, 20]. Porcelain chipping has been reported as one of the most frequent technical complications for veneered single crowns [3]. To overcome the problem of chipping, all‐ceramic single crowns can be made without a veneer. However, these restorations have sometimes showed a risk of complete fracture [21]. Many studies have compared the survival of different types of single crown materials [3] but few have included type of material among other clinical variables in multifactorial analyses.
Treatment plan and decision‐making should rely on several general and local factors. Recognizing these factors during treatment planning may reduce the risk of complications and failures. Therefore, the aim of the present retrospective study was to investigate the survival rates and technical and biological complications of tooth‐supported single crowns with respect to several aforementioned variables.
MATERIAL AND METHODS
Study design
The dental records archive and the digital journals of all patients (a total number of approximately 4000 records) at the Faculty of Odontology, Malmö University, Sweden were reviewed by one investigator (MH) to identify patients rehabilitated with tooth‐supported full coverage single crowns. The study protocol was approved by the Regional Ethical Committee in Lund, Sweden (Dnr 4,3‐2018/422; Dnr 2018/856) and followed the STROBE guidelines [22].
Definitions
Survival was defined as the prosthesis remaining in situ and in function, even though complications might have occurred. A prosthesis that had been removed or replaced was considered a failed prosthesis. Chipping was defined as loss of veneer substance with or without metal exposure, being classified as minor (managed chair‐side) or major (sent to the dental lab for reparation). A tooth was considered as a failure if exhibiting extensive alveolar bone loss and/or excessive tooth mobility, extensive caries, or any other complication that would make the tooth unsuitable to remain as retainer for single crown and therefore lead to tooth loss. Crowns on incisors and canines were classified as anterior crowns, while crowns on premolars and molars were classified as posterior crowns.
All patients included in the present study had undergone clinical examination including an anamnestic part and self‐report questionnaire to identify bruxism. In the present study, a distinction between “possible” and “probable” sleep or awake bruxism was made. A recording of “possible” sleep or awake bruxism was based on self‐report using questionnaires and/or the anamnestic part of a clinical examination. A recording of “probable” bruxism was based on self‐report together with clinical examination [23]. The information on the self‐report and clinical examination was verified from annotations in the dental records of each eligible patient. Patients were thus classified as “probable” bruxers if such findings were identified.
Inclusion and exclusion criteria
All patients treated with full coverage tooth‐supported single crowns at the aforementioned faculty who had a minimum follow‐up time of 6 months after delivery of the prosthetic work and an available dental record at the clinic's archive were included. The exclusion criteria consisted of conventional full‐coverage fixed dental prostheses, resin‐bonded and cantilever fixed dental prostheses, partial‐coverage crowns, and cases with lack of information regarding the outcome measures.
Data collection
The patient data were collected and entered directly into a database in a SPSS file (SPSS version 27; SPSS) by one investigator (MH). The following data were collected: patient's age and sex, location of the crowns in relation to the jaws (maxilla, mandible), area of crown placement (anterior, posterior), type of tooth (incisor, canine, premolar, molar), tooth vitality, presence of post and core, type of crown material, type of cement, situation of the opposing arch (natural dentition, fixed or removable denture), treatment provider (dental student, general or specialist dentist), smoking habits, bruxism, and complications after delivery of the single crowns including the date when they occurred. Information on types of materials used in the single crowns were obtained from the dental lab order. Technical and biological complications were evaluated radiographically and through the patients’ records. Biological complications included caries, loss of tooth vitality, periapical infection, mobility, and tooth loss. Technical complications included tooth fracture, loss of retention, framework fracture, and minor and major porcelain chipping.
Statistical analysis
The data were described using mean values, standard deviations (SD), and percentages. The interval survival rate of the single crowns was calculated using the information of the period of failure, and the cumulative survival rate was calculated over the maximal period of follow‐up reported, in a life‐table survival analysis.
Univariate and multivariate Cox regression was used to evaluate the associations between clinical covariates and crown failure. Hazard ratio (HR) and 95% confidence intervals (95% CI) were estimated from Cox proportional hazard models. In order to verify multicollinearity, a correlation matrix of all the predictor variables with a significant odds ratio (p value cut‐off point of 0.1) identified in the univariate models was examined, to see whether there were some high correlations among the predictors. Collinearity statistics obtaining variance inflation factor (VIF) and tolerance statistic were also performed to detect more subtle forms of multicollinearity. For the final multivariable Cox regression model, all variables that were univariably moderately associated (p < 0.10) with single crown failure were included. For this crown‐level analysis, clustering of multiple single crowns within each patient was accounted for in the Cox models using the methods outlined by Lee et al. [24] and Lin [25]. Data were statistically analyzed using the SPSS software. Cox models were performed using the Stata software version 15 (StataCorp). The command mestreg was used for the Cox models, in order to take into account clustering of observations in patients. The statistical significance level was set at p < 0.05.
RESULTS
A total of 1050 single crowns were executed by dental students, general practitioners, or specialists at a prosthodontic and general adult dental care department during the period between 1981 and 2018 and had complete information on outcomes. The data of 13 single crowns were excluded from the analyses as they had a minimum follow‐up time of less than 6 months (Figure 1).
FIGURE 1.
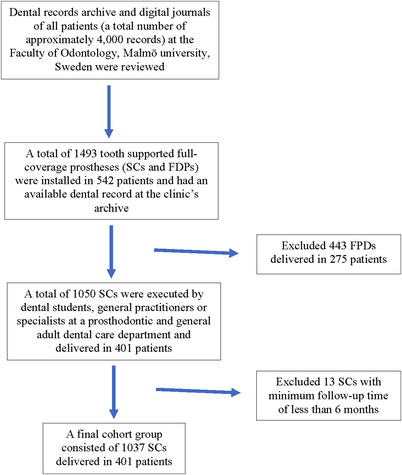
Flow‐chart describing the selection of participants/crowns. SC, single crown; FDP, fixed dental prosthesis
The final sample consisted of 1037 single crowns, 47.5% of which were supported by vital abutments and 52.5% by non‐vital abutments. These single crowns were installed in 401 patients, 195 men and 206 women, who had a mean age of 56.8 years (± 12.9 SD, min–max 21.0–86.6) and 57.7 years (± 12.5 SD, min–max 28.1–85.6), respectively, at the day of crown delivery. Most patients attended regular follow‐up visits during the first year but not all continued regular annual follow‐ups. The 1037 single crowns were followed for a mean of 134.8 ± 80.2 months, SD (min–max, 6.0–360.7).
Table 1 presents the descriptive characteristics of the single crowns included in the study, with number of failed crowns and follow‐up time according to the different factors analyzed. Tables 2 and 3 show the different types of all‐ceramic single crown materials and the veneering status, respectively. Veneered oxide ceramics, zirconia (27.8%) and alumina (24.9%), were the most common material used for all‐ceramic single crowns. Partial veneering was used in most veneered zirconia single crowns. Table 4 presents the results for the life‐table survival analysis. The cumulative survival rates for all single crowns were 89.9% and 80.9% after 5 and 10 years, respectively. After 15 and 20 years of function, the cumulative survival rates for 284 and 111 single crowns were 70.5% and 61.8%, respectively. A total of 230 single crowns were considered failures (Table 4). Failures occurred in 149 patients, after a mean follow‐up time of 114.5 ± 70.4 months ± SD (min–max, 7.3–293.6). Loss of retention, tooth loss, and tooth fracture were the most common reasons for single crown failures (Table 5).
TABLE 1.
Descriptive data of the single crowns included in the study, with follow‐up time according to the different factors. The descriptive unit is the crown, not the patient
| Factor | Number of single crowns (%) | Number of failed single crowns | Follow‐up time (months) Mean ± SD (min–max) |
|---|---|---|---|
| Sex | |||
| Male | 506 (48.8) | 114 | 129.0 ± 83.0 (6.2–360.7) |
| Female | 531 (51.2) | 116 | 140.3 ± 77.1 (6.0–355.4) |
| Age | |||
| <50 years | 309 (29.8) | 86 | 159.2 ± 79.6 (6.2–333.6) |
| ≥50 years | 728 (70.2) | 144 | 124.4 ± 78.3 (6.0–360.7) |
| Jaw | |||
| Maxilla | 605 (58.3) | 150 | 128.9 ± 80.4 (6.0–355.4) |
| Mandible | 432 (41.7) | 80 | 143.1 ± 79.3 (6.9–360.7) |
| Crown region | |||
| Anterior | 282 (27.2) | 70 | 115.4 ± 74.1 (6.0–335.1) |
| Posterior | 755 (72.8) | 160 | 142.0 ± 81.3 (6.2–360.7) |
| Tooth type | |||
| Incisor | 217 (20.9) | 56 | 117.6 ± 73.6 (6.0–335.1) |
| Canine | 65 (6.3) | 14 | 108.0 ± 75.8 (9.2–298.9) |
| Premolar | 391 (37.7) | 83 | 138.6 ± 81.5 (6.8–360.7) |
| Molar | 364 (35.1) | 77 | 145.8 ± 80.9 (6.2–316.0) |
| Tooth vitality | |||
| Non‐vital | 544 (52.5) | 149 | 136.6 ± 79.7 (6.2–360.7) |
| Vital | 493 (47.5) | 81 | 132.8 ± 80.8 (6.0–132.8) |
| Post and core a | |||
| No | 71 (13.1) | 18 | 112.1 ± 71.7 (7.0–290.5) |
| Yes | 472 (86.9) | 131 | 140.0 ± 80.2 (6.2–360.7) |
| Material | |||
| All‐ceramic | 169 (16.3) | 26 | 81.5 ± 65.4 (6.3–234.8) |
| High‐noble gold ceramic | 678 (65.4) | 171 | 158.1 ± 72.6 (7.3–360.7) |
| Full gold | 68 (6.5) | 14 | 143.1 ± 81.9 (8.4–143.1) |
| CoCr ceramic | 122 (11.8) | 19 | 74.3 ± 72.3 (6.0–262.5) |
| Crown occluding to b | |||
| Natural teeth | 591 (59.8) | 131 | 138.3 ± 79.4 (6.0–355.4) |
| Fixed prosthesis | 398 (40.2) | 99 | 127.8 ± 80.2 (6.2–360.7) |
| Treatment provider | |||
| Dental student | 836 (80.6) | 197 | 140.0 ± 77.3 (6.0–303.1) |
| General or specialist dentist | 201 (19.4) | 33 | 113.1 ± 88.2 (7.6–360.7) |
| Bruxism | |||
| No | 696 (67.1) | 141 | 141.9 ± 77.4 (6.0–360.7) |
| Yes | 341 (32.9) | 89 | 120.3 ± 83.9 (8.5–333.6) |
| Smoking c | |||
| No | 283 (50.6) | 61 | 135.5 ± 78.3 (6.8–316.0) |
| Yes | 191 (34.2) | 50 | 123.0 ± 82.9 (6.2–329.5) |
| Ex‐smoker | 85 (15.2) | 17 | 145.6 ± 80.2 (11.3–298.9) |
Abbreviation: SD, standard deviation.
Only for non‐vital teeth.
Few cases were not considered her: crowns opposed removable partial denture (n = 26), and not occluding to anything (n = 22).
For the cases in which information on smoking habits was available.
TABLE 2.
Types of all‐ceramic materials used for the single crowns
| Types of all‐ceramic material | Frequency | (%) |
|---|---|---|
| Zirconia with porcelain veneer | 47 | 27.8 |
| Alumina with porcelain veneer | 42 | 24.9 |
| Lithium disilicate glass‐ceramic (e.max) | 29 | 17.2 |
| Monolithic zirconia | 23 | 13.6 |
| Leucite‐reinforced glass‐ceramic (Empress) | 21 | 12.4 |
| Lithium disilicate glass‐ceramic (Empress 2) | 4 | 2.4 |
| Feldspathic porcelain | 3 | 1.8 |
| Total | 169 | 100.0 |
TABLE 3.
Veneering status of all‐ceramic single crowns
| Type of ceramic material | Complete veneer | Partial veneer | Total |
|---|---|---|---|
| Zirconia | 17 | 30 | 47 |
| Alumina | 42 | 0 | 42 |
| Total | 59 | 30 | 89 |
TABLE 4.
Life‐table survival analysis showing the cumulative survival rate of the single crowns
| Interval start time (years) | Number entering interval | Number withdrawing during interval | Number exposed to risk | Single crown failures | Survival rate within each interval (%) | Cumulative proportion surviving at end of interval (%) | Standard error (%) |
|---|---|---|---|---|---|---|---|
| 0 | 1037 | 26 | 1024.0 | 10 | 99.0 | 99.0 | 0.3 |
| 1 | 1001 | 43 | 979.5 | 18 | 98.2 | 97.2 | 0.5 |
| 2 | 940 | 47 | 916.5 | 14 | 98.5 | 95.7 | 0.6 |
| 3 | 879 | 29 | 864.5 | 17 | 98.0 | 93.8 | 0.8 |
| 4 | 833 | 21 | 822.5 | 16 | 98.1 | 92.0 | 0.9 |
| 5 | 796 | 58 | 767.0 | 18 | 97.7 | 89.9 | 1.0 |
| 6 | 720 | 33 | 703.5 | 12 | 98.3 | 88.3 | 1.1 |
| 7 | 675 | 33 | 658.5 | 12 | 98.2 | 86.7 | 1.2 |
| 8 | 630 | 44 | 608.0 | 13 | 97.9 | 84.9 | 1.2 |
| 9 | 573 | 39 | 553.5 | 15 | 97.3 | 82.6 | 1.3 |
| 10 | 519 | 44 | 497.0 | 10 | 98.0 | 80.9 | 1.4 |
| 11 | 465 | 27 | 451.5 | 9 | 98.0 | 79.3 | 1.5 |
| 12 | 429 | 35 | 411.5 | 13 | 96.8 | 76.8 | 1.6 |
| 13 | 381 | 42 | 360.0 | 10 | 97.2 | 74.6 | 1.7 |
| 14 | 329 | 38 | 310.0 | 7 | 97.7 | 73.0 | 1.8 |
| 15 | 284 | 29 | 269.5 | 9 | 96.7 | 70.5 | 1.9 |
| 16 | 246 | 30 | 231.0 | 11 | 95.2 | 67.2 | 2.0 |
| 17 | 205 | 20 | 195.0 | 3 | 98.5 | 66.1 | 2.1 |
| 18 | 182 | 39 | 162.5 | 2 | 98.8 | 65.3 | 2.2 |
| 19 | 141 | 27 | 127.5 | 3 | 97.6 | 63.8 | 2.3 |
| 20 | 111 | 26 | 98.0 | 3 | 96.9 | 61.8 | 2.5 |
| 21 | 82 | 33 | 65.5 | 0 | 100 | 61.8 | 2.5 |
| 22 | 49 | 9 | 44.5 | 2 | 95.5 | 59.0 | 3.0 |
| 23 | 38 | 16 | 30.0 | 2 | 93.3 | 55.1 | 3.9 |
| 24 | 20 | 9 | 15.5 | 1 | 93.5 | 51.6 | 5.0 |
| 25 | 10 | 3 | 8.5 | 0 | 100 | 51.6 | 5.0 |
| 26 | 7 | 2 | 6.0 | 0 | 100 | 51.6 | 5.0 |
| 27 | 5 | 3 | 3.5 | 0 | 100 | 51.6 | 5.0 |
| 28 | 2 | 0 | 2.0 | 0 | 100 | 51.6 | 5.0 |
| 29 | 2 | 1 | 1.5 | 0 | 100 | 51.6 | 5.0 |
| 30 | 1 | 1 | 0.5 | 0 | 100 | 51.6 | 5.0 |
TABLE 5.
Reasons for the single crown failures
| Failure | Frequency | (%) |
|---|---|---|
| Loss of retention | 61 | 26.5 |
| Tooth loss | 31 | 13.5 |
| Tooth fracture | 29 | 12.6 |
| Replace old crown by new one due to change situation | 25 | 10.9 |
| Recurrent caries | 20 | 8.7 |
| Periapical destruction | 17 | 7.4 |
| Excessive bone loss | 11 | 4.8 |
| Major chipping | 8 | 3.5 |
| Mobility | 8 | 3.5 |
| Loss of tooth vitality | 7 | 3.0 |
| Esthetic dysfunction | 6 | 2.6 |
| Framework fracture | 4 | 1.7 |
| Tooth loss unknown reason | 2 | 0.9 |
| Poor fitting | 1 | 0.4 |
| Total | 230 | 100 |
Tables 6 and 7 present the results for the univariate and multivariate Cox proportional hazard models. Multicollinearity was observed between the factors “crown region” and “tooth type.” Therefore, the factor “tooth type”, which was moderately associated with crown failure in the univariate model, was excluded from the multivariate model. The estimated hazard ratio (HR) indicated that the following factors were influential for single crown survival: single crowns in posterior teeth had a lower HR than anterior teeth, crowns in vital teeth showed a lower HR than non‐vital teeth, and crowns in bruxers showed a higher HR than in non‐bruxers. Table 8 shows the biological and technical complications recorded for the single crowns. Loss of retention and recurrent caries were the most common complications. All‐ceramic and cobalt‐chromium based metal‐ceramic single crowns cemented with resin cement showed a lower occurrence of loss of retention than other types of single crown materials and cements (Table 9).
TABLE 6.
Univariate Cox proportional hazard models for single crown failure
| Factor | Hazard ratio (95% CI) | p value |
|---|---|---|
| Sex | ||
| Male | 1 | |
| Female | 0.88 (0.68, 1.14) | 0.33 |
| Age | ||
| <50 years | 1 | |
| ≥50 years | 0.94 (0.72, 1.23) | 0.65 |
| Jaw | ||
| Maxilla | 1 | |
| Mandible | 0.67 (0.51, 0.88) | 0.004 |
| Crown region | ||
| Anterior | 1 | |
| Posterior | 0.66 (0.50, 0.88) | 0.004 |
| Tooth type | ||
| Incisor | 1 | |
| Canine | 0.94 (0.52, 1.69) | 0.84 |
| Premolar | 0.66 (0.47, 0.93) | 0.017 |
| Molar | 0.65 (0.46, 0.91) | 0.013 |
| Tooth vitality | ||
| Non‐vital | 1 | |
| Vital | 0.61 (0.47, 0.80) | <0.001 |
| Post and core a | ||
| No | 1 | |
| Yes | 0.82 (0.50, 1.35) | 0.44 |
| Material | ||
| All‐ceramic | 1 | |
| Gold ceramic | 0.75 (0.49, 1.14) | 0.17 |
| Full gold | 0.71 (0.37, 1.37) | 0.31 |
| CoCr ceramic | 1.11 (0.61, 2.01) | 0.73 |
| Crown occluding to | ||
| Natural teeth | 1 | |
| Fixed prosthesis | 1.19 (0.91, 1.55) | 0.21 |
| Treatment provider | ||
| Dental student | 1 | |
| General or specialist dentist | 0.89 (0.61, 1.29) | 0.53 |
| Bruxism | ||
| No | 1 | |
| Yes | 1.55 (1.88, 2.02) | 0.001 |
| Smoking | ||
| No | 1 | |
| Yes | 1.37 (0.94, 1.99) | 0.10 |
| Ex‐smoker | 0.85 (0.50, 1.46) | 0.56 |
Abbreviation: 95% CI, 95% confidence interval.
Only for non‐vital teeth.
TABLE 7.
Multivariate Cox proportional hazard regression analysis of single crown failure
| Factor | Hazard ratio (95% CI) | p value |
|---|---|---|
| Jaw | ||
| Maxilla | 1 | |
| Mandible | 0.77 (0.58, 1.03) | 0.073 |
| Crown region | ||
| Anterior | 1 | |
| Posterior | 0.73 (0.55, 0.99) | 0.04 |
| Tooth vitality | ||
| Non‐vital | 1 | |
| Vital | 0.64 (0.49, 0.84) | 0.001 |
| Bruxism | ||
| No | 1 | |
| Yes | 1.52 (1.17, 1.98) | 0.002 |
Abbreviation: 95% CI, 95% confidence interval.
TABLE 8.
Biological and technical complications for single crowns
| Complication | Frequency | (%) |
|---|---|---|
| Loss of retention | 103 | 9.9 |
| Recurrent caries | 89 | 8.6 |
| Tooth loss | 75 | 7.2 |
| Periapical destruction | 61 | 5.9 |
| Loss of vitality | 48 | 4.6 |
| Tooth fracture | 29 | 2.8 |
| Mobility | 28 | 2.7 |
| Bone loss | 19 | 1.8 |
| Chipping | 19 | 1.8 |
| Framework fracture | 5 | 0.5 |
TABLE 9.
Occurrence of single crown loss of retention, according to the type of crown material and type of cement
| Types of cement | |||||
|---|---|---|---|---|---|
| Zinc phosphate cement | Resin cement | Glass ionomer cement | Resin modified glass‐ionomer cement | Total | |
| Material | n/N (%) | n/N (%) | n/N (%) | n/N (%) | n/N (%) |
| All‐ceramic | 6/55 (10.9) | 7/110 (6.4) | 1/4 (25.0) | 0/0 (0) | 14/169 (8.3) |
| Gold ceramic | 68/657 (10.4) | 1/4 (25.0) | 1/8 (12.5) | 1/4 (25.0) | 71/673 (10.5) |
| Gold | 6/66 (9.1) | 0/1 (0) | 0/1 (0) | 0/0 (0) | 6/68 (8.8) |
| CoCr ceramic | 11/116 (9.5) | 0/6 (0) | 0/0 (0) | 0/0 (0) | 11/122 (9.0) |
| Total | 91/894 (10.2) | 8/121 (6.6) | 2/13 (15.4) | 1/4 (25.0) | 102/1032 (9.9) |
A crosstabulation was performed for two variables (presence of post and core and area of crown placement) in order to explore the reason for the higher HR in anterior than in posterior teeth. The analysis showed that 89.9% of non‐vital anterior teeth had post and core (Table 10).
TABLE 10.
Tooth vitality, presence of post and core and area of crown placement
| Anterior | Posterior | Total | |
|---|---|---|---|
| Tooth vitality | n/N (%) | n/N (%) | n/N (%) |
| Vital tooth | 144/282 (51.1) | 350/755 (46.4) | 494/1037 (47.6) |
| Nonvital tooth without post and core | 14/282 (4.9) | 57/755 (7.5) | 71/1037 (6.9) |
| Nonvital tooth with post and core | 124/282 (44.0) | 348/755 (46.1) | 472/1037 (45.5) |
DISCUSSION
Based on the results of the present study, the survival rates of single crowns are influenced by area of crown placement (anterior, posterior), tooth vitality, and bruxism. The cumulative survival rate of single crowns after 5 and 10 years of function were lower than reported by previous reviews and a retrospective study [3, 4, 26]. Reviews have reported the 5‐year survival rates of metal‐ceramic and all‐ceramic single crowns to be between 90.7% and 96.6%, respectively [3, 4]. A retrospective study reported 10‐year survival rate of anterior and posterior metal‐ceramic single crowns to be 92.3% and 95.9%, respectively [26]. Studies with even longer follow‐up, reported the survival rates of single crowns after 18 and 25 years of function to be between 74.9% and 85.4%, respectively [1, 5] which also were higher compared to the present study. In one of mentioned studies, all treatment was performed by one prosthodontic specialist in a private prosthodontic clinic [5]. This is in contrast to the present study, where treatment was performed in a dental school by several treatment providers with different clinical experience, including general practitioners and dental students as well as specialists. The varying degree of experience could have negatively influenced the treatment outcome. However, our study may be more representative as the results obtained at a specialist clinic may perhaps not be expected to be obtained by general practitioners [27]. Additionally, patients seeking treatment at specialists' private clinics are perhaps not representative of a general population of dental patients and this might also influence results. A factor with expected positive influence on the survival rate of single crowns is a regular follow‐up [1]. Regular follow‐up visits, including professional oral prophylaxis every 6 months, has been shown to have a positive influence on the prognosis of fixed prosthetic treatment [28]. This factor was however limited in the present study as few patients attended regular annual follow‐up visits past the first year.
The area of crown placement showed a significant influence on the survival of single crowns. Anterior single crowns showed a higher HR in relation to posterior ones. This may be surprising considering the generally lower loads expected in the anterior area [14, 15]. However, the high frequency of post and core in the anterior teeth could be the reason behind the higher rate of failure in anterior teeth. It has been reported that anterior teeth with post and core showed a higher risk of failure than posterior teeth with post and core [29]. Furthermore, the occlusal load of anterior teeth is often not parallel to the long axis of the tooth which results in an unfavorable load distribution [29] that might increase the micromotion of the crown and post if present, which subsequently increases the stress on the root surface, leading to tooth fracture, which was one of the most common reasons for single crown failures in the present study [10, 11]. Generating an appropriate ferrule in the remaining tooth structure during post fabrication could increase the fracture resistance and reduce the risk of tooth fracture [30, 31, 32]. Clinical examination was not performed in the present study however, which precludes any assessment of the presence or not of an appropriate ferrule in the included cases. Moreover, a limited amount of remaining tooth structure in the non‐vital anterior teeth compared to the posterior teeth could increase the incidence of loss of retention for post and core and lead to crown failure [29]. Loss of single crown retention has been reported to occur 2.66 times more frequently in the anterior than in posterior teeth [26]. While no explanations were offered for these findings [26], the result is in agreement with our findings.
Tooth vitality had a significant influence on the survival of single crowns in the present study. Dental pulp has interdental receptors which protect the tooth from overloading force [6]. These receptors are lost in non‐vital teeth which tends to increase the threshold for the maximum biting force [6, 33] and thereby contribute to increased risk of tooth damage and fracture [6]. Additionally, loss of tooth structure during endodontic and restorative procedures may reduce the biomechanical properties and fracture resistance and increase the susceptibility to tooth fracture [7, 8, 34]. The result is in agreement with a previous study, where single crowns on non‐vital teeth with/without post showed a high rate of failure compared to single crowns on vital teeth [35]. Higher failure rate of single crowns on non‐vital teeth than on vital ones was also reported by another previous study [36]. In the present study, the majority of single crowns supported by non‐vital teeth had post and core, which could also increase the risk of single crowns failures [10, 11]. single crowns on non‐vital teeth with post and core have showed a higher failure rate compared to single crowns on non‐vital teeth without post and core [35]. On the other hand, the result of the present study was in contrast to a previous paper, where the survival rates were not statistically significant different between single crowns on vital and non‐vital teeth with post and core [1]. The latter lack of difference was mainly attributed to the fact that there was no additional removal of tooth substance for the root canals that received post and core [1].
In the present study, bruxism showed a significant influence on the occurrence of single crown failure. Bruxism has been defined as a repetitive jaw‐muscle activity represented by clenching and grinding of the teeth and/or by bracing or thrusting of the mandible during wakefulness and sleep [23]. Diagnosis of bruxism based on diagnostic grading system of “possible,” “probable,” and “definite” sleep or awake bruxism has been suggested for both clinical and research situations [23]. Self‐report questionnaire, a clinical examination, in combination with a polysomnographic recording are used for “definite” diagnosis of sleep bruxism [23]. Electromyography recording of the masseter muscles is also one of the methods for grading “definite” awake bruxism. However, the polysomnographic and electromyographic diagnostic options are not commonly used in the clinic due to high cost and limited availability [23, 37]. Instead, self‐report questionnaires are commonly used for both clinical and research purposes and can be applied for a large population [38]. In the present study, information from anamnesis, self‐report questionnaire and clinical examination was used, and patients were thus classified as “probable” bruxers if such findings were identified.
Bruxism could increase the incidence of loss of retention which was the most common complication and the main reason for single crown failures in the present study. Loss of retention has been reported to occur more frequently in bruxers as there is often limited clinical crowns height as a result of tooth wear, combined with excessive occlusal forces [18]. Loss of retention was reported in a previous study as one of the most common complications for single crowns [39]. The longevity of single crowns is closely related to the marginal seal between abutment and crown [40]. Resin cement has an excellent ability to minimize the marginal discrepancy and leakage of all‐ceramic single crowns [41]. In the present study, all‐ceramic single crowns cemented with resin cement revealed better clinical performance compared to single crowns bonded with other cements such as zinc phosphate, as also observed in other studies [42, 43, 44]. The possible reason is the limited tensile strength of zinc phosphate cement which could increase the possibility of retention loss [42]. In addition to providing sealing, resin cements can form a chemical bond to ceramics after proper conditioning [45]. However, the groups are imbalanced as few metal‐based crowns were cemented using resin cement.
Bruxism could also increase the risk of tooth loss. In the present study, tooth loss occurred as a consequence of extensive alveolar bone loss and/or excessive tooth mobility. In periodontally compromised patients, excessive overload by bruxism could enhance periodontal breakdown and negatively influence the alveolar bone density and create a bony defect which leads to pathological tooth mobility and tooth loss [46, 47, 48]. The risk of porcelain chipping of single crowns has been reported to be three times higher in bruxers compared to non‐bruxers [49]. In the present study however, porcelain chipping was reported as one of the less frequent complications. The reason for this observation could be the high number of single crowns made of precious alloy as framework (high‐noble gold‐based ceramic). The bond strength of porcelain to precious alloy is significantly higher compared to bonding to non‐precious alloy frameworks which reduces the tendency for adhesive veneering ceramic fracture for the precious alloy single crowns [26, 50, 51]. This was also found in a previous paper where only 1.7% of single crowns made of precious alloy framework had porcelain chipping [26].
Recurrent caries was reported as the second most common complication in the present paper. Recurrent marginal caries could be a consequence of ill‐fitting margin or could follow the loss of single crown retention [52]. Ill‐fitting crown margins accumulate more plaque which could increase the incidence of the recurrent marginal caries [28, 53]. As a clinical examination was not performed in the present study, the precise primary cause of the recurrent caries could not be ascertained.
The types of crown material had no significant influence on the survival of the single crowns. These results are in agreement with a previous review where most types of all‐ceramic single crowns showed similar survival rates to those reported for metal ceramic ones [3]. The type of material may influence the outcome of single crown less than in fixed dental prostheses due to the difference in biomechanics between single crowns and fixed dental prostheses as single crowns are less complicated in their design having no connector and splinting areas [49].
Patient's age and sex had no significant influence on the survival of single crowns. The magnitude of the biting force is higher in men than women [12, 13, 14, 54] and decreases significantly after 50 years of age [13]. However, number of teeth has been reported as the most important factor affecting the magnitude of the biting force rather than patient's age and sex [13]. This factor was not controlled among included patients and could have influenced the results.
The status of the opposing arch was included as a variable in the multifactor analysis. However, as the dentition may have changed at subsequent follow‐ups, it is difficult to judge if complications occurred when the single crowns were opposed by natural dentition or fixed or removable prosthesis.
There are limitations with retrospective studies based on patient records. Treatment providers were not calibrated, and the clinical procedures were not standardized and controlled as it could be in a prospective study. Moreover, some data may not have been completely recorded in the patients journals at each follow‐up appointment. The present study emanated from a teaching institution. The patients that were not treated by students and specialists are probably representative of general dental practice. While patients seeking treatment at a low‐cost student clinic could have lower socio‐economic status and poorer general and oral health, this was not analyzed. This may limit the generalizability of the results. Nevertheless, record‐based retrospective studies involving several variables and treatment providers are valuable as they provide information about risks and complications which can help the practitioner in everyday treatment planning.
Within the limitations of this retrospective study, we conclude that anterior placement, non‐vital abutments, and bruxism are factors increasing the rate of single crown failure.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Mohammed Hawthan, Bruno Chrcanovic, Christel Larsson Larsson; Methodology: Mohammed Hawthan, Bruno Chrcanovic; Software: Mohammed Hawthan, Bruno Chrcanovic; Validation: Mohammed Hawthan, Bruno Chrcanovic, Christel Larsson; Formal analysis: Mohammed Hawthan, Bruno Chrcanovic; Investigation: Mohammed Hawthan, Bruno Chrcanovic; Resources: Christel Larsson; Data curation: Mohammed Hawthan; Writing‐original draft preparation: Mohammed Hawthan; Writing – review and editing: Bruno Chrcanovic, Christel Larsson; Visualization:Mohammed Hawthan, Bruno Chrcanovic, Christel Larsson; Supervision: Bruno Chrcanovic, Christel Larsson; Project administration: Mohammed Hawthan; Funding acquisition: Mohammed Hawthan.
ACKNOWLEDGEMENT
The authors would like to thank Umm Al‐Qura University, Makkah, Saudi Arabia, for funding this study.
Hawthan M, Chrcanovic BR, Larsson C. Retrospective clinical study of tooth‐supported single crowns: A multifactor analysis. Eur J Oral Sci. 2022;130:e12871. 10.1111/eos.12871
REFERENCES
- 1. De Backer H, Van Maele G, Decock V, Van den Berghe L. Long‐term survival of complete crowns, fixed dental prostheses, and cantilever fixed dental prostheses with posts and cores on root canal‐treated teeth. Int J Prosthodont. 2007;20:229‐34. [PubMed] [Google Scholar]
- 2. Sequeira‐Byron P, Fedorowicz Z, Carter B, Nasser M, Alrowaili EF. Single crowns versus conventional fillings for the restoration of root‐filled teeth. Cochrane Database Syst Rev. 2015:CD009109. 10.1002/14651858.CD009109.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All‐ceramic or metal‐ceramic tooth‐supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: single crowns (SCs). Dent Mater. 2015;31:603‐23. [DOI] [PubMed] [Google Scholar]
- 4. Pjetursson BE, Sailer I, Zwahlen M, Hämmerle CH. A systematic review of the survival and complication rates of all‐ceramic and metal‐ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res. 2007;18(Suppl 3):73‐85. [DOI] [PubMed] [Google Scholar]
- 5. Walton TR. The up to 25‐year survival and clinical performance of 2340 high gold‐based metal‐ceramic single crowns. Int J Prosthodont. 2013;26:151‐60. [DOI] [PubMed] [Google Scholar]
- 6. Awawdeh L, Hemaidat K, Al‐Omari W. Higher maximal occlusal bite force in endodontically treated teeth versus vital contralateral counterparts. J Endod. 2017;43:871‐5. [DOI] [PubMed] [Google Scholar]
- 7. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989;15:512‐6. [DOI] [PubMed] [Google Scholar]
- 8. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18:332‐5. [DOI] [PubMed] [Google Scholar]
- 9. Baba NZ, Goodacre CJ, Daher T. Restoration of endodontically treated teeth: the seven keys to success. Gen Dent. 2009;57:596‐603. [PubMed] [Google Scholar]
- 10. Peters MC, Poort HW, Farah JW, Craig RG. Stress analysis of a tooth restored with a post and core. J Dent Res. 1983;62:760‐3. [DOI] [PubMed] [Google Scholar]
- 11. Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post‐core reconstructed teeth: a review. Int J Prosthodont. 2001;14:355‐63. [PubMed] [Google Scholar]
- 12. Bakke M, Holm B, Jensen BL, Michler L, Möller E. Unilateral, isometric bite force in 8‐68‐year‐old women and men related to occlusal factors. Scand J Dent Res. 1990;98:149‐58. [DOI] [PubMed] [Google Scholar]
- 13. Miyaura K, Matsuka Y, Morita M, Yamashita A, Watanabe T. Comparison of biting forces in different age and sex groups: a study of biting efficiency with mobile and non‐mobile teeth. J Oral Rehabil. 1999;26:223‐7. [DOI] [PubMed] [Google Scholar]
- 14. Shinogaya T, Bakke M, Thomsen CE, Vilmann A, Sodeyama A, Matsumoto M. Effects of ethnicity, gender and age on clenching force and load distribution. Clin Oral Investig. 2001;5:63‐8. [DOI] [PubMed] [Google Scholar]
- 15. Kumagai H, Suzuki T, Hamada T, Sondang P, Fujitani M, Nikawa H. Occlusal force distribution on the dental arch during various levels of clenching. J Oral Rehabil. 1999;26:932‐5. [DOI] [PubMed] [Google Scholar]
- 16. Gibbs CH, Anusavice KJ, Young HM, Jones JS, Esquivel‐Upshaw JF. Maximum clenching force of patients with moderate loss of posterior tooth support: a pilot study. J Prosthet Dent. 2002;88:498‐502. [DOI] [PubMed] [Google Scholar]
- 17. Miyaura K, Morita M, Matsuka Y, Yamashita A, Watanabe T. Rehabilitation of biting abilities in patients with different types of dental prostheses. J Oral Rehabil. 2000;27:1073‐6. [DOI] [PubMed] [Google Scholar]
- 18. Johansson A, Omar R, Carlsson GE. Bruxism and prosthetic treatment: a critical review. J Prosthodont Res. 2011;55:127‐36. [DOI] [PubMed] [Google Scholar]
- 19. Lazarski MP, Walker WA, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J Endod. 2001;27:791‐6. [DOI] [PubMed] [Google Scholar]
- 20. Rauch A, Schrock A, Schierz O, Hahnel S. Material selection for tooth‐supported single crowns‐a survey among dentists in Germany. Clin Oral Investig. 2021;25:283‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Della Bona A, Kelly JR. The clinical success of all‐ceramic restorations. J Am Dent Assoc. 2008;139:8S‐13S. [DOI] [PubMed] [Google Scholar]
- 22. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495‐9.25046131 [Google Scholar]
- 23. Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40:2‐4. [DOI] [PubMed] [Google Scholar]
- 24. Lee EW, Wei L, Amato DA, Leurgans S. Cox‐type regression analysis for large numbers of small groups of correlated failure time observations. Survival analysis: state of the art. Springer; 1992. pp. 237‐47. [Google Scholar]
- 25. Lin DY. Cox regression analysis of multivariate failure time data: the marginal approach. Stat Med. 1994;13:2233‐47. [DOI] [PubMed] [Google Scholar]
- 26. Behr M, Zeman F, Baitinger T, Galler J, Koller M, Handel G, et al. The clinical performance of porcelain‐fused‐to‐metal precious alloy single crowns: chipping, recurrent caries, periodontitis, and loss of retention. Int J Prosthodont. 2014;27:153‐60. [DOI] [PubMed] [Google Scholar]
- 27. Karlsson S, Nilner K, Dahl B. A textbook of fixed prosthodontics. Scand Approach Stockholm: FoÈ rlagshuset Gothia. 2000:337‐56. [Google Scholar]
- 28. Valderhaug J, Ellingsen JE, Jokstad A. Oral hygiene, periodontal conditions and carious lesions in patients treated with dental bridges. A 15‐year clinical and radiographic follow‐up study. J Clin Periodontol. 1993;20:482‐489. [DOI] [PubMed] [Google Scholar]
- 29. Mentink AG, Meeuwissen R, Käyser AF, Mulder J. Survival rate and failure characteristics of the all metal post and core restoration. J Oral Rehabil. 1993;20:455‐461. [DOI] [PubMed] [Google Scholar]
- 30. Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: a literature review. J Endod. 2012;38:11‐9. [DOI] [PubMed] [Google Scholar]
- 31. Stankiewicz NR, Wilson PR. The ferrule effect: a literature review. Int Endod J. 2002;35:575‐81. [DOI] [PubMed] [Google Scholar]
- 32. Tan PL, Aquilino SA, Gratton DG, Stanford CM, Tan SC, Johnson WT, et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent. 2005;93:331‐6. [DOI] [PubMed] [Google Scholar]
- 33. Loewenstein WR, Rathkamp R. A study on the pressoreceptive sensibility of the tooth. J Dent Res. 1955;34:287‐94. [DOI] [PubMed] [Google Scholar]
- 34. Dimitriu B, Vârlan C, Suciu I, Vârlan V, Bodnar D. Current considerations concerning endodontically treated teeth: alteration of hard dental tissues and biomechanical properties following endodontic therapy. J Med Life. 2009;2:60‐5. [PMC free article] [PubMed] [Google Scholar]
- 35. Schmidlin K, Schnell N, Steiner S, Salvi GE, Pjetursson B, Matuliene G, et al. Complication and failure rates in patients treated for chronic periodontitis and restored with single crowns on teeth and/or implants. Clin Oral Implants Res. 2010;21:550‐7. [DOI] [PubMed] [Google Scholar]
- 36. Walton TR. A 10‐year longitudinal study of fixed prosthodontics: clinical characteristics and outcome of single‐unit metal‐ceramic crowns. Int J Prosthodont. 1999;12:519‐26. [PubMed] [Google Scholar]
- 37. Manfredini D, Bucci MB, Sabattini VB, Lobbezoo F. Bruxism: overview of current knowledge and suggestions for dental implants planning. Cranio. 2011;29:304‐12. [DOI] [PubMed] [Google Scholar]
- 38. Koyano K, Tsukiyama Y, Ichiki R, Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil. 2008;35:495‐508. [DOI] [PubMed] [Google Scholar]
- 39. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications in fixed prosthodontics. J Prosthet Dent. 2003;90:31‐41. [DOI] [PubMed] [Google Scholar]
- 40. Diaz‐Arnold AM, Vargas MA, Haselton DR. Current status of luting agents for fixed prosthodontics. J Prosthet Dent. 1999;81:135‐41. [DOI] [PubMed] [Google Scholar]
- 41. Gu XH, Kern M. Marginal discrepancies and leakage of all‐ceramic crowns: influence of luting agents and aging conditions. Int J Prosthodont. 2003;16:109‐16. [PubMed] [Google Scholar]
- 42. Sorrentino R, Galasso L, Tetè S, De Simone G, Zarone F. Clinical evaluation of 209 all‐ceramic single crowns cemented on natural and implant‐supported abutments with different luting agents: a 6‐year retrospective study. Clin Implant Dent Relat Res. 2012;14:184‐97. [DOI] [PubMed] [Google Scholar]
- 43. Ortorp A, Kihl ML, Carlsson GE. A 5‐year retrospective study of survival of zirconia single crowns fitted in a private clinical setting J Dent. 2012;40:527‐30. [DOI] [PubMed] [Google Scholar]
- 44. van den Breemer CR, Gresnigt MM, Cune MS. Cementation of glass‐ceramic posterior restorations: a systematic review. Biomed Res Int. 2015;2015:148954. 10.1155/2015/148954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tian T, Tsoi JK, Matinlinna JP, Burrow MF. Aspects of bonding between resin luting cements and glass ceramic materials. Dent Mater. 2014;30:e147‐62. [DOI] [PubMed] [Google Scholar]
- 46. Weston P, Yaziz YA, Moles DR, Needleman I. Occlusal interventions for periodontitis in adults. Cochrane Database Syst Rev. 2008:CD004968. 10.1002/14651858.CD004968.pub2 [DOI] [PubMed] [Google Scholar]
- 47. Ericsson I, Lindhe J. Effect of longstanding jiggling on experimental marginal periodontitis in the beagle dog. J Clin Periodontol. 1982;9:497‐503. [DOI] [PubMed] [Google Scholar]
- 48. Glickman I. Inflammation and trauma from occlusion, co‐destructive factors in chronic periodontal disease. J Periodontol. 1963;34:5‐10. [Google Scholar]
- 49. Reitemeier B, Hansel K, Kastner C, Weber A, Walter MH. A prospective 10‐year study of metal ceramic single crowns and fixed dental prosthesis retainers in private practice settings. J Prosth Dent. 2013;109:149‐55. [DOI] [PubMed] [Google Scholar]
- 50. Mikeli A, Boening KW, Lißke B. Ceramic defects in metal‐ceramic fixed dental prostheses made from Co‐Cr and Au‐Pt alloys: a retrospective study. Int J Prosthodont. 2015;28:487‐9. [DOI] [PubMed] [Google Scholar]
- 51. Drummond JL, Randolph RG, Jekkals VJ, Lenke JW. Shear testing of the porcelain‐metal bond. J Dent Res. 1984;63:1400‐01. [DOI] [PubMed] [Google Scholar]
- 52. Hämmerle CH. Success and failure of fixed bridgework. Periodontol 2000. 1994;4:41‐51. [DOI] [PubMed] [Google Scholar]
- 53. Karlsson S. A clinical evaluation of fixed bridges, 10 years following insertion. J Oral Rehabil. 1986;13:423‐32. [DOI] [PubMed] [Google Scholar]
- 54. Bakke M. Bite force and occlusion. Semin Orthodont. 2006;12:120‐6. [Google Scholar]


