Abstract
Background
Interest in the use of yoga to enhance engagement with and augment the benefits of psychological treatment has grown. However, a systematic approach to reviewing existing research examining the use of yoga with psychological treatment is lacking.
Materials and Methods
This mapping review identified and synthesised research trialling yoga as an integrated or adjunct therapy with evidence‐based psychological interventions for the treatment of anxiety, depression, PTSD, and eating disorders.
Results
Overall, the review identified ten published and three unpublished studies, representing either single group or small quasi‐experimental research designs.
Discussion
Limited but promising findings were shown for yoga with CBT for anxiety and depression, and the integration of yoga within intensive treatment models for PTSD.
Conclusions
Future research is encouraged to focus on controlled trials that enable examination of the component effect of yoga when applied with evidence‐based psychological treatment and acceptability and feasibility data to further knowledge regarding a role for yoga in clinical practice.
Keywords: anxiety, complementary therapy, depression, eating disorders, evidence‐based psychological treatment, mapping review, posttraumatic stress disorder, yoga
1. INTRODUCTION
1.1. Background
Disease burden attributable to common mental disorders is well documented, identifying mental illness as a significant global health concern. In Australia, for example, anxiety and depression represent the leading causes of nonfatal disease burden, with mental disorders collectively representing the third highest‐burden disease group across fatal and nonfatal conditions (Australian Institute of Health and Welfare [AIHW], 2018). Conservatively, prevalence data indicate that approximately 45% of adult Australians experience a mental illness in their lifetime (AIHW, 2018), with similar prevalence rates in other developed nations (Kessler et al., 2009; Steel et al., 2014). The high frequency and substantial disease burden of mental disorders demonstrate the need for acceptable, effective, and accessible intervention efforts.
Psychological therapies represent first‐line treatments across multiple mental disorder groups (National Institute of Care Excellence [NICE], 2011a). There is good quality evidence for the acceptability and clinical efficacy of cognitive behavior therapy (CBT) and its third wave adaptions such as mindfulness‐based cognitive therapy (MCBT), acceptance and commitment therapy (ACT), and dialectical behavior therapy (DBT) in treating common mental disorders, including depression and anxiety (Bai et al., 2020; Ghahari et al., 2020; Goldberg et al., 2019; Hofmann et al., 2012; Panos et al., 2014). Despite the strong evidence base for psychological therapies, and CBT in particular, it is acknowledged that these treatments fail to fully resolve symptoms of mental disorder for a significant proportion of affected individuals (Huhn et al., 2014). Sizeable drop‐out rates are also observed across a number of disorders, including posttraumatic stress disorder (PTSD) (Gutner et al., 2016), depression (Hans & Hiller, 2013), eating disorders (Linardon et al., 2018), and panic disorder (Keijsers et al., 2001). Equally, patterns of treatment access indicate that many adults do not access psychological therapies to begin with (Burges et al., 2009; Wang et al., 2007), with particularly low rates of treatment engagement observed for PTSD (Strecker & Fortney, 2011).
As such, adults suffering from mental disorders are increasingly seeking Complementary and Integrative Health (CIH) approaches as substitutes to psychological treatment (Hansen & Kristoffersen, 2016; Spinks & Hollingsworth, 2012) or alongside it (de Jonge et al., 2018; Elkins et al., 2005; Unützer et al., 2000). CIH approaches refer to nonmainstream health care practices that are used either together with, or in place of, conventional health practices (National Centre for Complementary and Integrative Health [NCCIH], 2008). Approaches that integrate CIH with psychotherapies, such as CBT, have been shown to reduce premature treatment termination for depression, PTSD, and eating disorders (Swift & Greenberg, 2014).
Amongst these CIH practices, yoga has grown in popularity. Referred to as a mind‐body practice, yoga typically integrates physical movement and postures (asana), with breath control practices (pranayama), and relaxation or meditation (dhyana), with the aim of supporting health and well‐being (Kraftsow, 1999). Over and above the physical benefits of yoga, the research findings highlight that many people attribute their motivation to engage with the practice for stress relief purposes and to manage mental health conditions (Park et al., 2016; Penman et al., 2012). Anecdotal evidence also suggests that acceptance has grown for recommending the use of yoga alongside psychological therapy in clinical practice (Eliot, 2008; Ware, 2007; Weintraub, 2012; West et al., 2017).
1.2. Yoga and mental health
The growing interest in yoga as a complementary approach to improving mental health is synonymous with a rapid rise in research examining its potential as an intervention for treating mental illness (Bussing et al., 2012; Gupta et al., 2018; Jeter et al., 2015). Recent systematic reviews have identified that yoga may be beneficial in reducing symptoms of depressive disorders (Cramer et al., 2017; Cramer, Lauche, Langhorst, et al., 2013) and depressive symptoms associated with other mental disorders (Brinsley et al., 2020), as well as anxiety disorder symptoms (Cramer, Lauche, et al., 2018; Zoogman et al., 2019), symptoms of PTSD (Cramer, Anheyer, et al., 2018), and eating disorders (Borden & Cook‐Cottone, 2020; Ostermann et al., 2019). Overall, these reviews conclude that yoga merits preliminary consideration as a standalone treatment for these conditions but caution that the available evidence is limited and typically of low to moderate quality, pointing instead to a role for yoga as a safe adjunct to other forms of treatment. Evidence for the use of yoga in treating other mental health conditions, such as schizophrenia, is limited, leaving recommendations unclear (Cramer, Lauche, Klose, et al., 2013).
Importantly, a number of psychological factors are implicated in the therapeutic effects of yoga (Butterfield et al., 2017), with research demonstrating positive effects for yoga on self‐regulation (Dick et al., 2014), self‐efficacy (Franzblau et al., 2006; Martin et al., 2015), interoception and embodiment (Neukirch et al., 2019; Rivest‐Gadbois & Boudrias, 2019), motivation (Martin et al., 2015), connection (Kishida et al., 2018), self‐compassion (Crews et al., 2016; Gard et al., 2012; Snaith et al., 2018), psychological flexibility (Dick et al., 2014), positive affect (Park et al., 2020), and mindfulness (Tellhed et al., 2019; Tihanyi et al., 2016). Given these psychological factors are also the targets of psychological treatments for common mental disorders, including anxiety and depression, it is of interest to consider the various ways yoga might enhance or reinforce the benefits of psychological interventions.
Emerging evidence examining the capacity of yoga to significantly increase mindfulness highlights a potential key pathway for yoga to improve psychological wellbeing (Boni et al., 2018; Carmody & Baer, 2008). Commonly described as the cultivation of deliberate and nonjudgmental attention to the present moment (Kabat‐Zinn, 1994), mindfulness‐based practices are incorporated into MBCT (Segal et al., 2013), DBT (Linehan, 2014), and ACT (Hayes, 2011), highlighting the positive benefits of combining mindfulness with established cognitive and behavioral strategies (Hofmann et al., 2010; Lang, 2013). As a specific body‐based mindfulness approach, yoga (especially hatha‐yoga) offers similar and potentially additional benefits to current therapies through the cultivation of mindful attention to physical movement, the breath, and meditative self‐enquiry (Desikachar, 1995; Uebelacker & Broughton, 2016). It may possibly be a more accessible mindfulness practice than seated meditations (Carmody & Baer, 2008; Dick et al., 2014). Additionally, there is emerging evidence suggesting that yoga might enhance engagement in current psychological therapies (Uebelacker et al., 2010), as well as provide an experiential platform to facilitate the psychotherapeutic process (Valente & Marotta, 2011). Subsequently, as a complement to recent systematic reviews of yoga as a standalone treatment for common mental disorders (Cramer et al., 2017; Cramer, Anheyer, et al., 2018; Cramer, Lauche, et al., 2018), it is of interest to examine how yoga might be usefully adopted as an adjunct to or integrated into current psychological treatments.
1.3. The current study
Despite growing interest in yoga to support psychological treatment of mental health conditions, to our knowledge, there has been no comprehensive review of research examining yoga as an adjunct to or integrated with, standard psychological treatments for mental disorders. Examining this knowledge gap is necessary to examine the evidence base for integrated yoga and psychological treatment (Nauphal et al., 2019; Patwardhan, 2016) and to highlight key areas for future research relevant to clinical practice. Understandably, health practitioners will be reticent to prescribe yoga alongside psychological treatment for mental disorders without a complete understanding of the current evidence base, whilst psychologists interested in integrating yoga with evidence‐based psychological approaches have a responsibility as scientist‐practitioners to critically appraise relevant intervention research as well as the practical and ethical issues arising from the use of yoga as a complementary therapy (Kamradt, 2017; Park, 2013).
Accordingly, this study utilizes evidence mapping to report on interventions where yoga and evidence‐based psychological treatment are integrated (i.e., combined in a single intervention protocol) or where yoga serves as an adjunct therapy (i.e., delivered alongside) to psychological treatment as usual for common mental health conditions in adulthood. In doing so, it aims to synthesize the current knowledge base and identify relevant knowledge gaps for future research. As noted by Callahan et al. (2012), a broad appraisal of an evidence base represents a key first step when examining new intervention approaches, before moving to a systematic exploration of effectiveness.
Specifically, it aims to answer the following research questions:
-
a)
What is the scope, type, and extent of the evidence base for the adoption of yoga as an adjunct to, or integrated within the protocol of adapted forms of evidence‐based psychological therapies, for anxiety, depression, PTSD, and eating disorders?
-
b)
What are the key knowledge gaps that should direct future research in using yoga alongside psychological treatments?
2. METHODS
This study used evidence mapping methodology to systematically identify, organize and summarize available research related to yoga as a complementary approach to psychological treatment. While specific methods and reporting guidelines are not yet established for evidence mapping, there is growing consensus as to what constitutes an evidence map and how it complements more generic scoping approaches (Miake‐Lye et al., 2016). Specifically, this approach involves the engagement of experts early in the process to elaborate the aims and scope of the mapped research field, a systematic search of this field, and the production of a user‐friendly format in which to display the findings to meet the needs of an end‐user, in this case, clinicians and clinical researchers (Miake‐Lye et al., 2016). We adapted evidence mapping procedures used by Katz et al. (2003) and Callahan et al. (2012) as the aims of these studies aligned with the current study. These are summarized in Table 1 and described below following the Preferred Reporting items for Systematic Review and Meta‐Analysis (PRISMA) guidelines (Moher et al., 2015).
Table 1.
Steps in process of evidence map generation
| Step | Task |
|---|---|
| 1 | Apply expert opinion to develop research questions |
| 2 | Develop the region of evidence to be mapped (hatha yoga; specific disorders; published and protocols) |
| 3 | Apply mapping coordinates and developing search strategy |
| 4 | Search the evidence bounded by map |
| 5 | Screen and plot the distribution of studies retrieved (“drawing the map”) |
| 6 | Summarize and assess mapped studies for the generation of knowledge gaps and priority future research |
| 7 | Quality appraisal |
2.1. Step 1. Apply expert opinion to develop research questions
The aims of this study relate to the fields of clinical psychology and yoga. As such, consultation was necessary with practitioners and researchers with knowledge across these two domains, including in the delivery of evidence‐based psychological treatment to a range of mental disorders, as well as applied yoga research in mental health. Subsequently, a small panel was established with those having clinical experience in the delivery of psychological treatment as well as an understanding of evidence‐based clinical research, in addition to training and experience in yoga and published research on yoga and mental health. This panel included experts in Australia (Authors MOS [Clinical Psychologist and clinical researcher in yoga and mental health, Yoga Teacher], SE [Clinical researcher in yoga and other mind‐body modalities for health including mental health and women's health], and SM [Researcher in yoga and other mindfulness‐based practices for health and mental health, Yoga Teacher]) and India (Author JA [Clinical Psychologist and Researcher with focus on yoga and psychology research]) along with a Clinical Psychologist and academic (Author GM) outside the field to promote a balanced view to the mapped evidence.
The panel, informed by their respective knowledge (of each research domain) and clinical experience, engaged in an iterative process of scoping and refinement through virtual (email) debate and dialog. This led to the finalization of key areas of focus for the mapping review and established the research questions.
2.2. Step 2. Develop the region of evidence to be mapped
Although the panel noted the broad application of yoga in the treatment of mental disorders, there were agreement that the strongest evidence for the therapeutic application of yoga currently exists for depression (Cramer et al., 2017; Cramer, Lauche, Langhorst, et al., 2013), anxiety (Cramer, Lauche, et al., 2018; Zoogman et al., 2019), PTSD (Cramer, Anheyer, et al., 2018) and eating disorders (Borden & Cook‐Cottone, 2020; Ostermann et al., 2019). Thus, studies that included samples with these disorders were targeted. In parallel, the research field of focussed psychological interventions for mental disorders is vast. Accordingly, the panel stipulated that only those studies where the type of psychological intervention examined was considered “evidence–based” should be included. Whilst the terminology of “evidence‐based” is not precisely defined, the panel agreed to adopt Australia's current published best practice guidelines for the application of psychological interventions to mental disorders (Australian Psychological Society [APS], 2018). Upon guidance from the panel, Level I and II evidenced interventions when applied to a specific clinical disorder were denoted as “evidence‐based.” These were cross‐referenced with the NICE guidelines (NICE, 2005, 2009, 2011b, 2011c, 2013, 2014, 2017, 2018) for best practice mental health treatments, and inconsistencies were addressed by the panel via consensus. Based on this analysis, Table 2 specifies the psychological interventions with Level I and Level II evidence for treating the defined mental disorders for the purposes of this review. The evidence map was limited to intervention studies with samples of adults aged 18 or over, noting that the evidence base for yoga and psychological interventions for adults and children is not completely overlapping.
Table 2.
Evidence‐based psychological interventions (Level I and Level II) for common mental disorders in adulthood
| Mental disorder | Level I* | Level II* |
|---|---|---|
| Depression | CBT, IPT, MBCT, PST, psychodynamic therapy, psychoeducation | ACT, DBT, EFT, EMDR, FI, Schema therapy, SFT |
| Anxiety disorders | ||
| Generalized anxiety disorder | CBT | ACT, MCT, MBCT, MBSR, psychodynamic therapy, psychoeducation |
| Specific phobia | CBT | – |
| Social anxiety disorder | CBT | ACT, IPT, MBSR, psychodynamic therapy |
| Obsessive‐compulsive disorder | CBT | ACT, FI, MBCT, MCT |
| Posttraumatic stress disorder (PTSD) | CBT, EMDR | DBT, EFT, MCT, MBSR |
| Eating disorders | ||
| Anorexia nervosa | – | CBT, FI, psychodynamic therapy |
| Bulimia nervosa | CBT | DBT |
| Binge eating disorder | CBT | DBT, IPT, MBSR, psychoeducation |
Abbreviations: ACT, acceptance and commitment therapy; CBT, cognitive behavior therapy; DBT, dialectical behavior therapy; EFT, emotion focussed therapy; EMDR, eye movement desensitization and reprocessing; FI, family (based) interventions; IPT, interpersonal psychotherapy; MBCT, mindfulness‐based cognitive therapy; MBSR, mindfulness‐based stress reduction; MCT, metacognitive therapy; PST, problem solving therapy; SFT, solution focussed therapy.
Adapted from Australian Psychological Society (2018).
Given the heterogeneity within yoga approaches (Cramer, Lauche, et al., 2018; Cramer, Lauche, Langhorst, et al., 2013; Field, 2016) and this being a known limitation to furthering the evidence for yoga for mental health disorders (Nauphal et al., 2019), it was necessary to define what comprised a yoga intervention for the purposes of this review. As hatha yoga represents the most practiced style in western countries, and includes such schools as Iyengar, Kundalini, Ashtanga, Yin, and Viniyoga (De Michelis, 2004; Singleton, 2010), it was determined to be an operationally useful definition of yoga. Accordingly, only those studies that described the following components of hatha yoga (herein referred to as yoga) were included within the evidence map: physical postures (asana), breath regulation/exercises (pranayama), and relaxation or meditation (Dhyana). Moreover, whilst dosage requirements for yoga are not precisely defined, the panel agreed that single session hatha yoga was insufficient as a yoga exposure, rather the yoga intervention must occur over more than one session.
Trials were included if they either: (a) delivered yoga alongside an evidence‐based psychological intervention (adjunct) for the purpose of relieving symptomatology or improving functioning for participants diagnosed with anxiety, depression, PTSD, or eating disorders (including by an auxiliary yoga teacher or therapist outside the team responsible for the psychological intervention); or (b) incorporated yoga into an evidenced‐based psychological treatment approach (integrated) for these participant groups.
Noting the infancy of this study field and the research questions of interest, the panel agreed not to exclude any mapped evidence because of quality at this step (for quality appraisal method, see Step 5).
2.3. Step 3. Apply mapping coordinates and developing search strategy
Search strategies were devised separately for (i) databases and (ii) clinical trial registries to establish the breadth of registered yoga studies and identify published and in progress trials relevant to the research questions.
-
(i)
The overall search structure for relevant databases was established using Boolean logic (AND/OR) to identify studies examining a combination of yoga and evidence‐based psychological interventions (e.g., CBT and ACT) relevant to the target mental disorders (“Anxiety,” “Depression,” “PTSD,” and “Eating Disorders”). See Table 3 for the specific search strategy and defined search parameters.
-
(ii)
The Australian and New Zealand Clinical Trials Registry (ANZCTR), International Standard Randomized Controlled Trial Number Registry (ISRCTN), and ClinicalTrials.gov clinical trial registries were also searched. Given the relatively small number of yoga‐based trials arising in ANZCTR and ISRCTN (81 and 43, respectively) when searched using the broad term of “yoga,” all were reviewed by two authors against the search parameters. However, using this broad search term in ClinicalTrials.gov derived a very large number of yoga‐based trials (n = 887). As such, the search was refined using the search terms detailed in Table 3, representing the target mental disorders, resulting in 243 trials. Again, each was reviewed by two authors against the search parameters. Studies were included that used a cohort trial design, such as a cohort trial or randomized controlled trial (RCT), to examine yoga and evidence‐based psychological intervention(s) for adults affected by the targeted mental disorders, with no restrictions of outcome variables. Other types of trials, such as case studies, or review papers were excluded.
Table 3.
Search parameters
Databases searched via EBSCO host 1900–2021:
|
Search terms:
|
Clinical trials registries searched:
|
| Limits: No limits implemented in search strategy. |
| PICOS: |
|
|
|
|
|
Exclusion:
|
Efforts were made to contact authors of all studies published in languages other than English to request translated versions.
To optimize the breadth of findings, dissertations were included, however other types of gray literature, such as news reports, were excluded on the basis that they are not scientific studies. Finally, only retrieved studies published in English were included unless correctly translated versions could be sourced.
2.4. Step 4. Search the evidence bounded by map
Searches were conducted in May 2020 and updated in May 2021. Retrieved citations were collated into Endnote software, where duplicates were deleted, then uploaded to Covidence (Veritas Health Innovation, 2021). Titles and abstracts of all retrieved studies were independently screened by two authors for potential inclusion in the agreed evidence map, with inconsistencies resolved by discussion with a third author. Full‐text articles for all potentially eligible studies were then read and assessed against the inclusion and exclusion criteria until agreement was reached. Where necessary, the authors of relevant identified studies were contacted to clarify aspects of the trial that related to specific inclusion and exclusion criteria. For example, the authors of research examining a culturally adapted CBT protocol were contacted to clarify the type of yoga “stretching” used in their intervention, confirming that it did not include all components of a hatha yoga intervention (Kananian et al., 2017). Reference lists of included studies were also reviewed to retrieve additional trials not identified through the search strategy.
2.5. Step 5. Screen and plot the distribution of studies retrieved (“drawing the map”)
Trials were coded according to the mental disorder of interest followed by which evidenced‐based intervention was evaluated. Trials were further classified according to how yoga was incorporated into the psychological intervention. That is, whether yoga was: (a) applied as an adjunct to the standard evidence‐based psychological treatment or, (b) integrated with an evidence‐based psychological approach in an adapted form of the treatment. In circumstances where multiple papers were published against a single trial, the primary reference was determined and then subsequent publications and outcomes arising from the same trial were noted to avoid multiple publication bias. Using this categorization, the evidence map was developed with studies distributed by a mental disorder of interest, psychological intervention, and the yoga approach.
2.6. Step 6. Summarize and assess mapped studies for the generation of knowledge gaps and priority future research
Relevant data were extracted and coded by three authors from the mapped evidence and cross‐checked by a fourth. Data of interest included mental disorder, study design, psychological intervention, yoga intervention, participant details (including number, mental health diagnoses, attrition rates, age, and sex ratio), outcome measures, and results. Intervention descriptions focussed on whether yoga was an adjunct to another evidence‐based psychological intervention or integrated within a combined intervention protocol. Following the aims of evidence mapping, the conclusions and future directions elaborated by the authors of each included study were also extracted and summarized. The overall map of evidence and summary data, along with the full text for all included studies, were then circulated to all members of the expert panel. In turn, the panel determined areas of priority for the field and key considerations for the use of yoga as a complementary approach to evidence‐based psychological treatments for the mental disorders of interest. Key future directions were selected with consideration to the extent and quality of the current evidence. Next steps were also defined as well as issues of feasibility and acceptability to clinical psychology.
2.7. Step 7. Quality appraisal
The Oxford Centre for Evidence‐based Medicine (OCEBM) Levels of Evidence was used to critically appraise the mapped evidence (OCEBM, 2011). Whilst quality appraisal is typically beyond the scope of evidence mapping, the OCEBM approach is designed to assist clinicians and clinician‐researchers evaluating the evidence related to clinical questions (Howick et al., 2011) and as such, was deemed appropriate to the present review's research questions. It also allowed for the appraisal of a broad range of methodological approaches including qualitative and mixed methods, enabling a single appraisal method across all included studies. Based on the OCEBM method, studies are provided with a score between 1 (highest) and 5 (lowest) according to the study design with RCTs typically ranked high and poorly designed case–control studies ranked low. These scores are then typically synthesized to make recommendations regarding the strength of evidence for a particular intervention. Two authors independently appraised each study with discrepancies resolved by discussion. The outcome of this quality appraisal was factored into decisions made by the panel about priority research directions, whilst acknowledging that a lack of rigorous studies does not equate to a lack of being able to identify useful patterns and trends in a field important but limited such as this one.
3. RESULTS
The search strategy yielded 238 articles from the selected databases, of which 21 were identified as relevant after screening titles and abstracts (see Figure 1). Of the 21 reviewed in full‐text, 9 were excluded based on the predefined criteria, including three that did not examine a yoga intervention involving all components of hatha yoga. An additional published study was retrieved via reference mining of included articles (Cook‐Cottone et al., 2008). For the clinical trials registries, a total of 376 studies were retrieved, with eight identified as relevant based on screening of titles and abstracts. Following full‐text review, six were excluded, including two that did not examine a hatha yoga intervention. Of the two studies that met the inclusion criteria (O'Shea, 2020; Staples, 2018) the trial conducted by O'Shea (2020) was completed, with qualitative findings published and retrieved elsewhere (O'Shea et al. 2021). To our knowledge, the findings of the second retrieved trial are currently unpublished (Staples, 2018).
Figure 1.
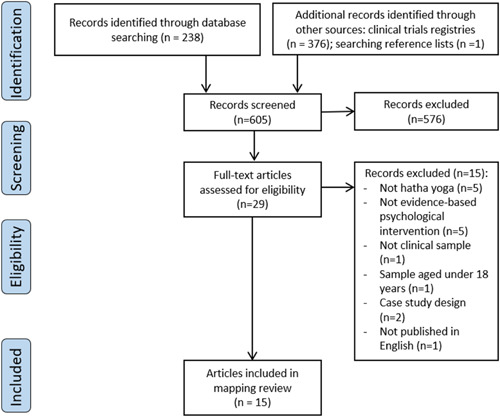
PRISMA flow diagram
A total of 15 studies were included for the mapping review and categorized according to the selection criteria, noting where studies arose from the same trial (Beck, 2008; O'Shea et al. 2021; Cook‐Cottone et al., 2008; O'Shea, 2020). This represented 13 unique studies meeting the criteria for the evidence map. Two of these were unpublished dissertations (Briggs, 2017; Zuehlke, 2008), and two were treatment protocols which, to the authors' knowledge, remain untested or unpublished (Staples, 2018; Zuehlke, 2008). Details of included studies are summarized in Table 4 according to key characteristics relevant to the mapping review.
Table 4.
Summary of studies examining yoga as an adjunct to or integrated within evidence‐based psychological treatments for common mental disorders
| Mental disorder | Author(s) year country | Interventions (adjunct or integrated) | Aims | Sample | Study design | Outcome measures | Results | Conclusions and future directions | Quality appraisala |
|---|---|---|---|---|---|---|---|---|---|
| Depressive Disorders | |||||||||
| Major and persistent depressive disorders |
Butler et al. (2008) USA |
Adjunct Hypnosis: 10 weekly group sessions of 1.5 h. 2‐h booster session in Week 12. Yoga Intervention: 8 weekly group sessions of 2 h each, one 4‐h retreat and one booster session in Week 12. Psychoeducation: Readings, internet resources, and the self‐help book Feeling Good (Burns, 1999) |
To examine the effects of three interventions on diagnostic status and symptom levels for depressive disorders: 1) Hypnosis and psychoeducation 2) Yoga and psychoeducation 3) Psychoeducation only. |
46 adults (74% women) diagnosed with a depressive disorder: − 50% (n = 23) dysthymia − 28% (n = 13) dysthymia + major depressive episoder (MDE) − 15.2% (n = 7) MDE in partial remission − 6.5% (n = 3) chronic major depression of two+ years. Yoga + psychoeducation group (n = 17) Hypnosis + psychoeducation group (n = 17) Psychoeducation (control group; n = 18) Aged: 22–80 years. Attrition rate: 6/46 (13%). |
RCT pilot with follow‐up |
Hamilton Rating Scale for Depression (HRSD) (Hamilton, 1960) Cornell Dysthymia Rating Scale‐Self Report (CDRS‐SR) (Mason et al., 1995) |
Significantly more participants in the yoga group experienced remission (n = 10; 77%) than those in the control group (n = 5; 36%) (p < 0.03) at follow‐up, but not compared to the hypnosis group (n = 8; 62%). No participants in the intervention groups developed a new MDE at follow‐up compared with the control group (n = 3). |
Preliminary support for the use of group hypnosis or yoga in conjunction with psychoeducation to improve depressive diagnostic status and prevent development of further MDEs. The impact on remission rates indicates potential for hypnosis or yoga as treatments for long‐term depressed mood, in conjunction with psychoeducation. Findings warrant the conduct of larger, more controlled studies examining the separate interventions of yoga, meditation and hypnosis to identify individual treatment effects. |
Level 2 Randomized trial or observational study with dramatic effect |
| Moderate depressive symptoms |
USA |
Adjunct psychological intervention: Manualized individual Acceptance and Commitment Therapy delivered across 6 weekly sessions, approximately 50–60 min each, by graduate therapists. Yoga intervention: Six weekly group sessions of yoga, approximately 60 min each, including practices of mindful awareness via deep breathing, connection to body, breath, and movement, mindful body scan and brief relaxation. Group classes also included nonparticipants. |
To examine whether an adjunct yoga program further reduces depressive symptoms when provided alongside ACT compared to ACT as a standalone treatment. |
24 college students (75% women) with moderate depressive symptoms (as measured by the BDI‐II) ACT + Yoga (n = 12) ACT (control group; n = 12) Aged: 18–25 years (Mean = 20.17 years). Comorbidity: Not specifically reported, 33.3% self‐reported previous mental health diagnoses. Attrition rate: 9/35 (26%) |
RCT |
Beck Depression Inventory‐II (BDI‐II) (A. Beck et al., 2000) Mindfulness Attention Awareness Scale (MAAS) (Brown & Ryan, 2003) Acceptance and Action Questionnaire‐II (AAQ‐II) (Bond et al., 2011) World Health Organization Quality of Life – short form (WHOQOL‐BREF) (The WHOQoL Group, 1998) |
No significant differences observed on outcomes between groups. Significant improvements were observed pre‐post analyses for mindfulness, overall quality of life, psychological quality of life and physical. Nonsignificant improvements observed on pre‐post analyses for depression, acceptance, and environment quality of life. |
Findings suggest that an adjunct yoga program to ACT does not enhance reductions to depressive symptoms compared to ACT as standalone treatment. ACT and yoga resulted in significant improvements to mindfulness, but not depression. Future research with larger samples is needed to replicate findings and review potential confounding variables. |
Level 2 Randomized trial or observational study with dramatic effect |
| Pre or postpartum depression |
Zuehlke USA |
Integrated Psychological Intervention: Eight manualized group sessions of two hours each, combining CBT and Interpersonal Psychotherapy with psychoeducation and yoga. Yoga Intervention: Low impact 20‐minute yoga sessions via a video following psychological aspects of the intervention, tailored to postnatal women, incorporating relaxation training and physical activity. |
To develop an integrative group therapy manual for decreasing depressive symptoms and increasing overall wellbeing in women with postnatal depression. | Designed for adult women within six months of their first childbirth diagnosed with MDD, prepartum or postpartum depression. | Protocol Only | Not available due to study design. | Not available due to study design. | Not available due to study design. |
Level 5 Mechanism‐based reasoning |
| Perinatal depression and bipolar spectrum disorder |
Miklowitz et al. (2015) USA |
Integrated psychological intervention: Eight weekly 2‐h group mindfulness‐based cognitive therapy (MBCT) sessions facilitated by trained clinicians based on a standardized manual (Segal et al., 2013). Yoga intervention: Mindful yoga, body scan, and sitting meditations included in sessions. |
To examine the feasibility, acceptability, and benefits of an eight‐session MBCT program incorporating yoga for women with perinatal depression (MDD) or bipolar spectrum disorder (BSD); and to secondarily compare findings across MDD and BSD participants. |
39 pregnant women with a lifetime diagnosis of a mood disorder and current subthreshold symptoms (break down of diagnoses not reported). Aged: Over 18 years (mean = 33.7 years for group with bipolar disorder; 35.2 years for group with depression). Attrition rate: 7/39 (18%) |
Quasi‐experimental with follow‐up |
Client satisfaction questionnaire (CSQ‐8) (Larsen et al., 1979) BDI‐II (Beck et al., 2000) HRSD (Hamilton, 1960) Young Mania Rating Scale (YMRS) (Young et al., 1978) State‐Trait Anxiety Inventory‐Current Status Scale (STAI‐C) (Spielberger, 1983) Longitudinal Interval Follow‐Up Evaluation (LIFE) (Keller et al., 1987) Five Facet Mindfulness Questionnaire (FFMQ) (Baer et al., 2008) |
32 participants completed the program and reported high levels of satisfaction. BDI‐II scores decreased significantly across both groups over time, from a mildly to a minimally depressed state. Participants with depression showed greater reductions in depression and increases in mindfulness than participants with bipolar disorder. No significant changes were observed in anxiety or mania scores. |
Preliminary findings in support of MBCT as a promising treatment for both pregnant and postnatal women with depression, with high levels of treatment satisfaction, completion rates and reductions in depressive symptoms that maintain over time. Future research is needed to focus specifically on pregnant women with bipolar disorder and incorporate larger more rigorous research designs. |
Level 3 Non‐randomized controlled cohort/follow‐up study |
| Major depressive disorder (MDD) |
Niemi et al. (2016) Vietnam |
Adjunct Eight weekly group sessions including: Psychoeducation: Based on standardized manual (Patel et al., 2010) including information about symptoms, effects on interpersonal difficulties, support to engage in treatment and strategies to alleviate symptoms. Yoga Intervention: Including slow movements and breathing exercises, with some components of Qigong for cultural relevance. |
To evaluate the effectiveness of a collaborative stepped‐care community‐based intervention including psychoeducation and yoga for depression management in primary healthcare. |
56 adults with moderate level depression (42.9% women) Psychoeducation + Yoga (n = 34) Treatment as usual (Control group; n = 22) Aged: 17–96 years (mean 64.5) Comorbidity: Not reported. Attrition rate: 0/56 (0%) although 11/56 (20%) were lost to follow‐up. |
Cluster RCT | Patient Health Questionnaire‐9 (PHQ‐9) (Kroenke et al., 2001) |
Statistically significant reductions in the post‐intervention depression scores reported for the intervention group compared to treatment as usual. 42.9% of participants in the intervention group recovered from depression after 8‐weeks, while none did in the treatment as usual group. |
Findings suggest that the combined intervention of yoga and psychoeducation was more effective for treating moderate depression than standard care. Future research with larger sample sizes is needed to examine the cross‐cultural generalizability of these findings and feasibility of integrating such a combined program into primary care, along with long‐term follow up outcomes. |
Level 2 Randomized trial or observational study with dramatic effect |
| Anxiety disorders | |||||||||
| Generalized Anxiety Disorder (GAD) |
Khalsa et al. (2015) USA |
Integrated Six weekly one and a half hour sessions applying the group treatment of Yoga‐enhanced CBT (Y‐CBT) including: Psychological Intervention: instruction and experiential cognitive restructuring using both traditional and alternative CBT interventions Yoga Intervention: 30 min of Kundalini Yoga (Shannahoff‐Khalsa, 2006) in each session, including breathing practices, (long slow abdominal breathing), loosening warm‐up exercises (particularly for spinal flexibility), physical postures and movements, yoga meditations incorporating mindfulness, awareness, breath regulation, and deep relaxation practices. |
To evaluate the preliminary efficacy of Y‐CBT in relation to reducing anxiety and depression in a treatment‐resistant population. |
32 adult participants (81% female) diagnosed with “treatment resistant” GAD and at least one comorbid mental disorder in a community‐based mental health service. Aged: 23–62 years (Mean = 43.21 years). Comorbidity: ‐ Additional mood disorder (n = 24) ‐ MDD (n = 18) ‐ Substance use disorder (n = 4) ‐ ADHD (n = 2) ‐ PTSD (n = 4) ‐ Panic disorder (n = 3) ‐ Schizophrenia (n = 3) Attrition rate: 10/32 (31%). |
Single group pre‐post |
The State Trait Anxiety Inventory (STAI) (Spielberger, 1983) The Treatment Outcome Package (TOP) (Kraus et al., 2005) |
Statistically significant improvements reported for state and trait anxiety, as well as measures of depression, panic, suicidality, sleep disturbance, sexual function, and quality of life. |
Provides preliminary support for efficacy of the integrated Y‐CBT program for ‘treatment resistant’ presentations of GAD. Future research is needed in the form of a larger randomized control study incorporating qualitative data to supplement quantitative data as well as confirm and better understand the potential accessibility, adherence, and feasibility of Y‐CBT for GAD. |
Level 3 Nonrandomized controlled cohort/follow‐up study |
| Panic Disorder |
Vorkapic and Range (2014) Brazil |
Adjunct psychological intervention: Eight weekly group CBT sessions of 50 min. Yoga intervention: Group yoga sessions (for control group, once weekly sessions for group combined with CBT), of 50 min, over 8 weeks, involving physical postures (asana), breathing techniques (pranayama), relaxation (yoga nidra), and meditation (mindfulness). Participants completing yoga only received biweekly sessions and participants completing yoga and CBT received yoga sessions once per week. |
To investigate the efficacy of yoga in reducing symptoms of panic disorder compared to yoga combined with CBT. |
20 participants (99% female) were diagnosed with panic disorder. Yoga group (n = 10) Yoga + CBT (n = 10). Aged: Mean = 42.3 years (Yoga group); 40.9 years (Yoga + CBT group) Comorbidity: Not reported. Attrition: Not reported. |
Quasi‐experimental |
Beck Anxiety Inventory (BAI) (A. T. Beck & Steer, 1993) Hamilton Anxiety Rating Scale (HAM‐A) (Hamilton, 1959) The Panic Beliefs Inventory and Body Sensations Questionnaire (Chambless et al., 1984) Body Sensations Questionnaire (BSQ; Chambless et al., 1984) |
Significant reductions in anxiety and panic levels were reported across both groups. Greater nonsignificant reductions in panic related symptoms were reported in the yoga and CBT treatment group compared to the yoga only group. |
Improvements in mental health symptoms can be observed after the practice of contemplative techniques including yoga alone or when applied as an ancillary approach to CBT. Future research should focus on the mechanisms by which mind‐body therapies complement each other to potentially improve clinical outcomes for patients with panic disorder. |
Level 2 Randomized trial or observational study with dramatic effect |
| Transdiagnostic | |||||||||
| Depression and Anxiety |
O'Sheac (2020) Australia |
Adjunct Psychological Intervention: Eight weekly group CBT sessions of two hours each, adapted from The Mood Management Group (Nathan et al., 2004), representing treatment as usual (TAU). Yoga Intervention: In addition to TAU, therapeutic yoga program including eight weekly group sessions of one‐hour and individualized home practice. |
To assess the feasibility and acceptability of therapeutic yoga as an adjunct to CBT in a primary mental health setting. To explore whether an adjunctive therapeutic yoga program yields additional clinical benefits alongside standardized group CBT. |
Recruiting adults diagnosed with mild to moderate depression or anxiety attending a primary mental health clinic. | Pilot feasibility and acceptability mixed‐methods study with pre/post and follow up data |
Qualitative: Semi‐structured interviews with participants and stakeholders. Primary quantitative outcome: Depression Anxiety Stress Scales (DASS) (Lovibond & Lovibond, 1996) |
Not available | Not available |
Level 2 Randomized trial or observational study with dramatic effect |
| Depression and Anxiety |
O'Shea et al. (2021) Australia |
As above | To examine whether a personalized therapeutic yoga program was experienced by adults with anxiety and depression as an acceptable or complementary adjunct to group‐based CBT. |
Of the 32 participants who entered the adjunct yoga program, 27 (78% female) provided qualitative data, who were diagnosed with anxiety and/or depression. Aged: 19–66 years (mean = 41.2). Comorbidity: ‐ PTSD (n = 1) ‐ Eating disorder (n = 1). Attrition (of broader study): 7/32 (22%). |
Qualitative arm of above‐mixed methods study As above |
In‐depth semi‐structured interviews at post‐intervention and three‐month follow up timepoints |
Three primary themes with nine subthemes reflecting lived experiences of: 1. The combined therapies: − 1.1. Intuitively appealing, − 1.2. Enhanced therapeutic outcomes, − 1.3. The dance between yoga and CBT. 2. Complementary elements: − 2.1. Moving the body with the breath, − 2.2. Yoga is an embodied routine, − 2.3. A practice for me, and then others, − 2.4 A shared healing journey. 3. Engagement over time: − 3.1. The process of struggle and growth, − 3.2. Yoga as a self‐management tool. |
Adults with anxiety and depression described therapeutic yoga as a highly acceptable adjunct to CBT, that can enhance engagement and clinical outcomes from psychological treatment. Yoga seems to offer an accessible and sustainable practice for adults to self‐manage their mental health. Future research is needed to examine lived experiences of yoga for men, as well as longer‐term outcomes to further determine sustainability. |
As above |
| Posttraumatic stress disorder (PTSD) | |||||||||
| PTSD (caused by combat and military sexual trauma) |
Zalta et al., (2018) USA |
Integrated Three‐week intensive outpatient program including: Psychological Intervention: Cognitive Processing Therapy (CPT) and psychoeducation, delivered across 15 individual sessions and 13 group sessions. 13 group sessions of mindfulness‐based stress reduction (MBSR). Yoga Intervention: 12 group yoga sessions. |
To examine the effects of an intensive outpatient program on symptoms of PTSD and compare difference to those participants with PTSD caused by combat to those caused by military sexual trauma. |
191 veterans and service members diagnosed with PTSD (11.5% women). Sample was represented by 19 program cohorts including 12 combat veteran focussed cohorts and 7 encompassing veterans with military sexual trauma Comorbidity: Not reported. Attrition rate: 15/191 (8%). |
Non‐randomized cohort study |
PTSD checklist for DSM‐5 (PCL‐5) (Weathers et al., 2013) PHQ‐9 (Kroenke et al., 2001) Posttraumatic Cognitions Inventory (PTCI) (Foa et al., 1999) |
Clinically meaningful reductions across all measures of PTSD symptoms from pre‐ to post‐intervention for both groups of veterans with combat and military‐sexual trauma. Improvements observed as greater for combat veterans, although difference was nonsignificant. |
Intensive and multicomponent interventions including yoga show promise for reducing symptoms of PTSD in veterans, alongside or over longer‐term interventions. Future researching is needed to examine level of variance and clinical change caused by each components of treatment (CPT, MBSR and yoga). |
Level 3 Non‐randomized controlled cohort/follow‐up study |
| Combat‐related PTSD |
Steele et al. (2018) USA |
Integrated Warrior Camp 7‐day treatment program: Psychological interventions: EMDR, equine‐assisted psychotherapy and narrative writing. Yoga Intervention: Seven daily sessions of yoga. No further information provided regarding protocol. |
To investigate the efficacy of the Warrior Camp (WC) treatment program for combat related PTSD. |
85 returned service members (29% women) diagnosed with PTSD who had served in the military and reported having been deployed to a combat zone. Aged: 22–72 years (Mean = 42.94) Comorbidity: Not reported. Attrition rate: Not reported. |
Single group pilot study with pre‐ post data |
Mississippi Scale for Combat‐related PTSD (Keane et al., 1988) PHQ‐9 (Kroenke & Spitzer, 2002) Revised Adult Attachment Scales (RAAS) (Collins, 1996) Moral Injury Events Scale (MIES) (Nash et al., 2013) Davidson Trauma Scale (Davidson et al., 1997) Dissociative Experiences Scale (Frischholz et al., 1990) |
Statistically significant improvements reported in symptoms of PTSD, depression, moral injury, dissociation, and adult attachment measures over time, with effect sizes ranging from small to large. |
Preliminary evidence to support the use of intensive integrative treatment approaches that include yoga alongside evidence‐based psychotherapy for PTSD. Future research is needed to examine the integrative treatment model in comparison to treatment as usual for PTSD and to determine the extent to which each individual modality affects positive change. |
Level 3 Nonrandomized controlled cohort/follow‐up study |
| PTSD |
Zepeda Medez et al. (2018) Netherlands |
Integrated Five‐day intensive inpatient program including: Psychological Intervention: Two 90‐minute individual EMDR sessions each day, with an additional session provided one week after treatment, aimed at reducing emotional distress associated with the most upsetting traumatic memories, based on the Dutch version of the EMDR protocol (Beer et al., 2015). Yoga Intervention: One hour of trauma‐informed yoga at the end of each day, consisting of postures, breathing exercises, guided meditation on body awareness and relaxation. |
To investigate the feasibility and preliminary effectiveness of an intensive five‐day inpatient treatment program incorporating EMDR and trauma‐informed yoga for PTSD. |
12 adults (25% women) diagnosed with PTSD. Aged: Mean = 44.2 years. Comorbidity: ‐ MDD (n = 7) ‐ Panic disorder with agoraphobia (n = 3) ‐ OCD (n = 2) ‐ Alcohol dependence disorder (n = 2) Attrition rate: 1/12 (8%). |
Single group pilot study with pre‐post and follow up data | PTSD checklist for DSM‐5 (PCL‐5) (Weathers et al., 2013) |
Almost all (11/12) participants completed the treatment program. Noting lack of statistical power, treatment outcomes were based on criteria of clinically significant change and the Reliable Change Index. PTSD symptoms improved over time for majority (n = 9) of participants, with a moderate effect size identified at follow up. Two participants no longer met criteria for PTSD after the program. |
A 5‐day intensive inpatient EMDR and yoga treatment appears acceptable for adults with PTSD and effective for reducing PTSD symptoms. Future research is warranted to examine optimal treatment format and duration, to examine the relative contribution to clinical change for EMDR compared to yoga, and to determine the long‐term effects of intensive integrative treatments. |
Level 3 Nonrandomized controlled cohort/follow‐up study |
| PTSD |
Staples c (2018) USA |
Integrated Eight weekly three‐hour treatment sessions including: Psychological Intervention: 1.5 h of group CBT Yoga Intervention: 1.5 h of (Kundalini) yoga |
To evaluate the effectiveness of a CBT and yoga program for improving PTSD symptoms and sleep quality in people who have experienced a traumatic event. | 45 participants (no further details available) | Single group with pre‐post and 2‐ month follow‐up data |
PTSD checklist for DSM‐5 (PCL‐5) (Weathers et al., 2013) Pittsburgh Sleep Quality Index (PSQI) (Smyth, 1999) |
Not available | Not available |
Level 3 Nonrandomized controlled cohort/follow‐up study |
| Eating disorders | |||||||||
| Anorexia or bulimia nervosa |
Cook‐Cottone et al. (2008) USA |
Integrated Eight weekly two‐hour group sessions of the attunement in mind, body, and relationship (AMBR) program including: Psychological Intervention: Cognitive behavioral and dialectic behavioral theory (DBT) with dissonance‐induction content. Yoga Intervention: 50 min of body‐focused yoga, including instructions on breathing and self‐talk, and 15 min of meditation/relaxation practices. |
To examine preliminary outcomes for treating eating disorders with the AMBR program. |
29 women diagnosed with anorexia or bulimia nervosa engaged in an eating disorder treatment clinic Aged: 14–30 years (Mean = 20). Comorbidity: Not reported. Attrition rate: 5/29 (17%). |
Single group pilot study with pre‐ post data |
Three subscales from the Eating Disorder Inventory‐2 (EDI‐2) (Garner, 1991) ‐ Drive for Thinness, ‐ Body Dissatisfaction, ‐ Bulimia. |
Significant reductions were reported in participants’ desires for thinness and body dissatisfaction scores after the program. No significant differences were reported in bulimia scores. |
Preliminary positive findings for an integrative mind body treatment encompassing aspects of CBT, DBT and relational theory in the treatment of eating disorders. Further research is warranted for empirical validation of such findings using more robust RCT design, as well as qualitative data collection to assess acceptability and feasibility through examination of participant experiences and feedback. |
Level 3 Nonrandomized controlled cohort/follow‐up study |
|
Beck b (2008) USA |
Published above | ||||||||
Abbreviations: ACT, acceptance and commitment therapy; ADHD, attention deficit hyperactivity disorder; AMBSR, attunement in mind, body, and relationship program; BSD, bipolar spectrum disorder; CBT, cognitive behavioral therapy; CPT, cognitive processing therapy; DBT, Dialectical behavior therapy; EMDR, eye movement desensitization reprocessing therapy; GAD, generalized anxiety disorder; MBCT, mindfulness‐based cognitive therapy; MBSR, mindfulness‐based stress reduction; MDD, major depressive disorder; MDE, major depressive episode; OCD, obsessive‐compulsive disorder; PTSD, posttraumatic stress disorder; RCT, randomized controlled trial; TAU, treatment as usual; USA, United States of America; WC, warrior camp; Y‐CBT, yoga enhanced cognitive behavioral therapy.
Quality appraisal based on Oxford Centre for Evidence‐based Medicine (OCEBM, 2011).
Unpublished dissertations.
Retrieved from clinical trials registry (trial in progress).
3.1. Evidence map
Figure 2 is an evidence map for all included studies according to: (1) the mental disorder of interest, (2) type of evidence‐based psychological intervention, and (3), whether yoga was (a) applied as an adjunct to standard evidence‐based psychological intervention, or (b) integrated with an evidence‐based psychological intervention in an adapted treatment protocol.
Figure 2.
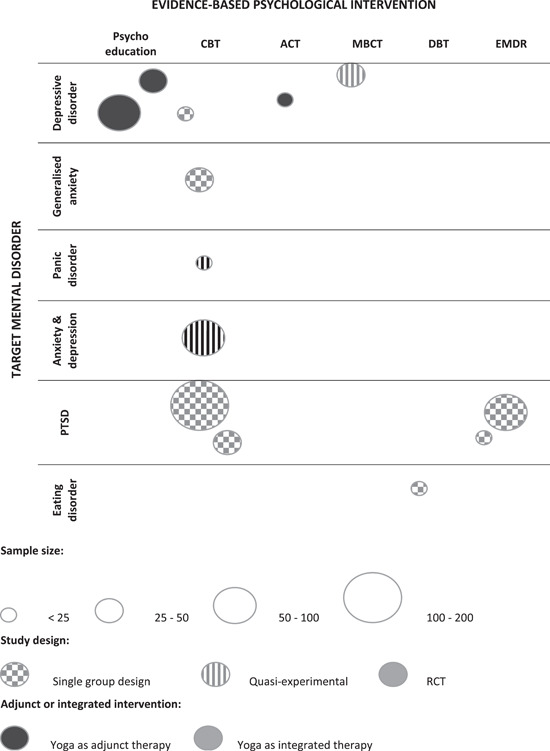
Evidence map
3.2. Summary of trials by condition
Most studies (n = 8) examined yoga in conjunction with evidence‐based psychological interventions for the treatment of anxiety and depression. Of these, two considered yoga as a means to augment evidence‐based psychological treatments for participants with chronic or treatment‐resistant forms of these conditions (Butler et al., 2008; Khalsa et al., 2015), and two for peri and post‐natal women (Miklowitz et al., 2015; Zuehlke, 2008). One study applied yoga and CBT trans‐diagnostically for anxiety and depression (O'Shea, 2020). Notably, high rates of comorbidity was a recurring pattern across studies. For example, most participants (81%) in M. K. Khalsa et al. (2015) yoga‐enhanced CBT study had a diagnosis in addition to GAD, which was predominantly depression. Three studies reported findings for yoga with evidence‐based psychological treatments for PTSD in intensive integrated treatment models (Steele et al., 2018; Zalta et al., 2018; Zepeda Méndez et al., 2018) with a fourth representing an unpublished trial of integrated yoga and CBT treatment protocol for the condition (Staples, 2018). One trial examined yoga alongside components of CBT and DBT for eating disorders (Cook‐Cottone et al., 2008).
3.3. Evidence‐based psychological interventions examined alongside yoga
When considering which psychological interventions were implemented in conjunction with yoga, CBT was the most commonly studied (n = 9), including one study that assessed MBCT (Miklowitz et al., 2015), an adapted CBT protocol incorporating yoga as a mindfulness exercise. Two studies evaluated psychoeducation based on CBT principles alongside yoga (Butler et al., 2008; Niemi et al., 2016) and another explored ACT supplemented by group yoga (Briggs, 2017). A single study, retrieved through both peer‐review publication and dissertation format, reported findings from an integrated treatment model incorporating CBT and DBT with yoga (Beck, 2008; Cook‐Cottone et al., 2008). The remaining two studies examined EMDR with yoga for PTSD (Steele et al., 2018; Zepeda Méndez et al., 2018).
3.4. Studies examining yoga as an adjunct therapy to standard evidence‐based psychological interventions
Just below half of the reviewed studies (n = 5) investigated yoga as an adjunct to standard evidence‐based psychological treatment. Niemi et al. (2016) examined weekly group yoga as an adjunct to weekly psychoeducation for the treatment of depressive symptoms in adults in Vietnam being treated for moderate depression within primary care (n = 34), compared with treatment as usual (TAU) (n = 22). Applying intention to treat analyses and a cutoff point of 4 on the Patient Health Questionnaire (PHQ‐9; Kroenke et al., 2001), which represents at least mild levels of depressive symptoms, around 40% of participants in the yoga and psychoeducation group were categorized as no longer depressed after the eight weeks, compared with no participants in the TAU group (Fisher's exact test, p < 0.001). Whilst studies incorporating long‐term follow‐up were pending, it was concluded that the combination of psychoeducation and yoga shows promise as an effective, culturally appropriate, and scalable approach for treating depression in Vietnam. It was further noted that pragmatic concerns rather than an a priori power calculation determined the sample size for the study, tempering these conclusions.
Butler et al. (2008) examined whether yoga or hypnosis augmented the effects of psychoeducation for adults with long‐term depressive disorders. χ 2 analyses were used to compare changes in depressive symptoms and diagnostic status between participants who completed treatment incorporating meditation and yoga in adjunct to psychoeducation (n = 13/17) versus those completing group therapy with hypnosis in adjunct to psychoeducation (n = 13/17) versus those who completed psychoeducation alone (n = 14/18). Results revealed that significantly more participants in the meditation/yoga and psychoeducational group (n = 10; 77%), but not the hypnosis group (n = 5, 47%), achieved a remission compared with those participants in the control group (n = 5; 36%), however small sample size tempers confidence in these findings. Authors concluded that these findings provided cautious support for the role of meditative practices including yoga to overcome some of the current clinical limits to psychoeducation for sufferers of long‐term depressed mood.
Briggs (2017) compared ACT alone (n = 12) to ACT plus yoga (n = 12) for college students experiencing low to moderate depression, using a single‐blind, randomized, active control design, to determine if the addition of yoga to ACT helps to relieve depressive symptoms. Outcome measures included the Beck Depression Inventory‐II (BDI‐II) (A. Beck et al., 2000), the Mindfulness Attention Awareness Scale (MAAS) (Brown & Ryan, 2003), and the World Health Organization Quality of Life–short form (WHOQOL‐BREF) (The WHOQoL Group, 1998). Findings indicated that participants undertaking a 6‐week course of ACT alone demonstrated similarly small improvements on measures of depression, mindfulness, and quality of life, compared to those engaged in weekly group yoga as an ancillary treatment to ACT. Noting that the study was not sufficiently powered to detect a treatment difference, changes from pre‐ to posttreatment were not statistically significant for either group. Nevertheless, a trend was observed for the adjunct treatment group, suggesting slightly greater improvements on most measures. However, the clinical relevance of this trend is unclear. Considering the incorporation of mindfulness practices in ACT, these findings suggest that yoga may not afford greater benefits than other mindfulness practices already integrated into the intervention.
Vorkapic and Rangé (2014) compared the clinical benefits of an 8‐week yoga intervention with the clinical benefits of the same yoga intervention supplemented with group CBT for 20 adults with panic disorder. Based on pre‐post within‐group analyses, statistically significant improvements in anxiety and panic symptoms were reported for both groups. The authors also reported trends in the data indicating greater improvements for the yoga and CBT group and the possibility that combining the techniques of yoga and CBT might augment the benefits of yoga alone, however, these differences were not statistically significant. Unfortunately, like other studies reviewed, interpretation of the results of this study is limited by the small sample size and lack of power analysis.
Finally, O'Shea (2020) and O'Shea et al. (2021) applied a mixed‐methods pragmatic pilot design to assess the acceptability and feasibility of implementing a therapeutic yoga program (group yoga combined with individual home practice) as an adjunct to group CBT for anxiety and depression, when compared to standard psychological care (group CBT alone), in a primary mental health setting. The study sought the perspectives of participants and key stakeholders such as referring clinicians and facilitators of CBT as to the acceptability and feasibility of the combined program. The Depression, Anxiety and Stress Scale (DASS) (Lovibond & Lovibond, 1996) was also used to compare preliminary rates of efficacy. While the main outcomes of the study are yet to be published, qualitative findings suggest that participants (n = 27) who self‐selected into the therapeutic yoga program as an adjunct to CBT found it highly acceptable and attributed many of the benefits to the unique combination of yoga and CBT elements. For example, participants noted that yoga represented an accessible form of behavioral activation as well as providing a means to reduce arousal and engage more effectively in group processes and CBT skills, such as thought disputation. Follow up interviews conducted three‐months after the intervention further highlighted how participants utilized yoga practices alongside CBT tools to sustain these benefits and prevent relapse. Based on these qualitative findings, the authors concluded that therapeutic yoga represents an accessible and acceptable adjunct to CBT, with the potential to enhance rates of engagement and clinical outcomes for adults with anxiety and depression.
3.5. Studies examining integrated evidenced‐based psychological interventions with yoga
Over half (n = 8) studies were reviewed that examined adapted forms of treatment where yoga was integrated with evidence‐based psychological interventions. M. K. Khalsa et al. (2015) designed and examined the potential benefits of a 6‐week integrated CBT and (kundalini) yoga intervention (Y‐CBT) incorporating yoga and meditation with CBT for GAD. In a single group pre‐post design, 32 participants suffering from GAD were enrolled to participate in the yoga‐enhanced CBT program. Having been in treatment as usual for an average of 2.79 years whilst remaining symptomatic, participants were categorized as treatment resistant. Twenty‐two of the participants (69%) completed the 6‐week intervention. Paired t tests were used to analyse mean changes from pre‐test to posttest on the State and Trait Inventory (STAI) (Spielberger, 1983) and outcomes measured via the Treatment Outcome Package (Kraus et al., 2005) including depression, panic and suicidality but no power analysis was reported. Statistically significant improvements were described on state and trait anxiety (p < 0.01), depression (p < 0.01), panic (p < 0.001), and sleep (p < 0.01). The authors noted that the effect size estimates of the study (e.g., a Hedge's g effect size of 0.97 for the combined treatment for GAD) compared favorably to studies examining CBT treatment alone. Given that the majority of participants were suffering from chronic rather than episodic anxiety, they proposed that the yoga enhanced CBT intervention might offer additional benefits to this cohort. Nevertheless, similar to most of the mapped evidence, the lack of a control group did not allow this hypothesis to be tested. As such, the authors identified the need for controlled studies incorporating qualitative data to better understand the possible additional benefits of yoga to CBT and how these benefits might be acquired.
Of the two adapted forms of MBCT for perinatal depression incorporating yoga identified in the review (Miklowitz et al., 2015; Zuehlke, 2008), only one has been published to our knowledge (Miklowitz et al., 2015). In an open trial, this study sought to examine the feasibility, acceptability, and benefits of an eight‐session MBCT program incorporating yoga for women with perinatal depression (MDD) or bipolar spectrum disorder (BSD) (n = 39), and to secondarily compare findings between MDD and BSD participants. Other meditation‐based elements were also included, such as mindfulness practices, body scans, and sitting meditations. Depression scores decreased significantly pre to posttreatment, with a mean depression score change of 12.2–7.4 (p = 0.08), measured by the BDI‐II (A. Beck et al., 2000), suggesting a shift from a mild to a minimally depressed state. Women in the study reported high levels of treatment satisfaction, with low rates of attrition observed, suggesting that the combination of MBCT with yoga might enhance engagement in treatment for peri‐natal depression. Notably, in sub‐group analyses, mood improvement was not observed among those with BSD.
Only one trial investigated an integrated treatment approach for anorexia and bulimia nervosa in a pilot study of a manualized group treatment approach incorporating yoga with DBT and cognitive therapy (Cook‐Cottone et al., 2008). The central aim was to examine changes in symptoms of anorexia nervosa and bulimia nervosa in a pre‐post pilot study design using paired sample t tests to compare pre‐ and posttest ratings of drive for thinness, (DT), body dissatisfaction (BD), and bulimia (BU) using the Eating Disorder Inventory‐2 (EDI‐2) (Garner, 1991). Twenty‐four of the commencing 29 (83%) female participants completed the treatment, suggesting good acceptability of the intervention, with significant reductions observed at posttreatment for BD (p < 0.01) and DT (p < 0.01) but not for BU. The authors concluded that incorporating yoga with existing evidence‐based psychological treatments had the potential to further relieve eating disorder symptoms through the provision of an experiential platform to practice mind and body skills and develop a more authentic connection with the body. They noted the need for controlled studies of larger samples to understand which of the components of the study contributed to the outcomes.
All four studies examining yoga and evidence‐based psychological interventions for PTSD adopted integrated treatment protocols, whereby yoga was included as a component of an adapted form of evidence‐based psychological treatment, with one an unpublished treatment protocol combining group CBT and yoga (Staples, 2018). Steele et al. (2018) assessed treatment effects of an intensive 1‐week (7 day) integrated treatment program of EMDR, yoga, equine‐assisted psychotherapy, and narrative writing for returned service personnel diagnosed with PTSD (n = 85) in a single‐group pilot study. Noting the study did not report a power analysis, statistically significant improvements were reported for distress across all measures, including for PTSD (p < 0.001) and depression (p < 0.001), measured by the Mississippi Scale for Combat‐related PTSD (Keane et al., 1988), and the PHQ‐9, respectively. The authors concluded the addition of the daily yoga program complemented EMDR by reducing symptoms of PTSD, whilst also supporting returned service personnel to regain physical and mental balance and purpose. However, the lack of a control group meant that treatment effects could not be specifically attributed to yoga or other aspects of the combined program. Similar promising findings were reported for a 5‐day intensive outpatient treatment program incorporating EMDR and daily yoga (Zepeda Méndez et al., 2018), where PTSD symptoms were assessed pre‐post and at 3‐week follow‐up in a single‐group pilot study design. Applying reliable change indexes and clinically significant change analyses, nine of 11 participants experienced significant reductions in PTSD symptoms, with two no longer meeting diagnostic criteria for PTSD at follow‐up. Only one participant did not complete the treatment program. Even though these findings provided further support for the benefits of incorporating yoga with EMDR for the treatment of PTSD, as per Steele et al. (2018), the single‐group pilot design did not allow for separately assessing the benefits of either component.
Similarly, Zalta et al. (2018) examined changes in symptoms of depression and PTSD in a group of military personnel (n = 176) undertaking a 3‐week intensive treatment program incorporating CBT, yoga, and other components, such as art therapy, nutrition advice, and psychoeducation. Symptoms of PTSD were measured by the PTSD Checklist for DSM‐5 (PCL‐5) (Weathers et al., 2013) and symptoms of depression were measured by the PHQ‐5 and assessed before, during, and after the intervention. The study found high levels of engagement with the program, and large and significant treatment effect sizes for both PTSD symptomatology and depression (Cohen's d = 1.40; 1.04, p < 0.001, respectively). The authors concluded that intensive outpatient programs incorporating a mixture of psychological and lifestyle modalities, including yoga, show promise for therapeutic gains for this group in shorter timeframes. Again, the uncontrolled nature of the study limits further understanding of the component elements of these intensive interventions for PTSD, specifically yoga.
3.6. Study design and quality appraisal
Each mapped study was appraised based on the OCEBM levels of evidence (see Table 4). Noting the small size of mapped evidence overall, problems with lack of statistical power and the exclusion of case studies, no studies represented Level 1 quality of evidence. Only five studies were RCTs or other forms of controlled studies incorporating a control group, representing Level 2 evidence, and the majority (n = 6) were nonrandomized studies with a single group, pre‐post intervention design (Level 3). One trial was yet to publish findings to our knowledge and could not be assessed, and one study was an unpublished protocol aimed at expanding treatment options for postpartum depression (Level 5). Overall, based on our assessment of these evidence levels, Grade B evidence exists for the incorporation of yoga into evidence‐based psychological treatments for anxiety and depression indicating such combined treatment protocols can be suggested for these conditions. Based on the four studies of PTSD each representing Level 3 evidence, a Level C recommendation level is identified for the benefits of intensive integrated treatments incorporating yoga denoting they may be considered for this condition. The single identified study that examined an integrated treatment model for eating disorders, utilizing DBT, cognitive therapy, and yoga, is insufficient to make a recommendation.
4. DISCUSSION
This review has identified and appraised current published and unpublished research on evidence‐based psychological interventions which has incorporated yoga, for a range of common mental disorders, to understand the extent and distribution of such research. It also identified research gaps and key future directions. Findings are considered amid emerging discourses examining the complementarity of yoga and Western psychological approaches (Caplan et al., 2013; Forfylow, 2011; Patwardhan, 2016; Uebelacker et al., 2010) and the potential for yoga to augment established psychological treatments (Nauphal et al., 2019; Park, 2013), extending on the extant research examining yoga as a standalone treatment for mental disorders.
4.1. Key findings
Despite growing interest in the integration of yoga with psychological interventions, only a small body of evidence was identified, revealing several important opportunities to move the field forward. The evidence map included 13 unique studies, four of which were unpublished, with almost half of these focussed on the treatment of depression (noting that one study included participants with bipolar spectrum disorders and subclinical symptoms of depression (Miklowitz et al., 2015)) and the others on anxiety (n = 2), PTSD (n = 4) and EDs (n = 1). Only four of the studies reported follow‐up data (Butler et al., 2008; Miklowitz et al., 2015; O'Shea et al., 2021; Zepeda Méndez et al., 2018). Notably, two were focussed on more chronic and long‐term presentations (of depression [Butler et al., 2008] and anxiety [M. K. Khalsa et al., 2015]), highlighting an interest in how yoga might enhance engagement and outcomes in cohorts with high levels of morbidity and poor engagement in treatment. Although yoga was used alongside a range of evidence‐based psychological interventions, CBT was used most frequently. This finding aligns with the prominence of CBT as an evidence‐based treatment for a range of common mental disorders (APS, 2018), recent adaptations of CBT incorporating mindfulness practices, such as MBCT (Segal et al., 2013), and the potential theoretical alignment between CBT and yoga (such as that proposed by M. K. Khalsa et al., 2015).
Of the completed studies identified in this review (n = 11), all but one (Briggs, 2017) reported symptom improvements, with no adverse events, for treatment approaches that incorporated yoga either as an adjunct to, or integrated with, evidence‐based psychological treatments, across all mental health disorders of interest. Where reported (n = 9, 81%), attrition rates were typically lower than for trials of standalone psychological interventions, particularly for PTSD, suggesting that yoga might enhance engagement in current evidence‐based psychological treatments. Moderate to strong effects were found for integrated treatment approaches that incorporated yoga for depression (Niemi et al., 2016), panic disorder (Vorkapic & Rangé, 2014), GAD (M. K. Khalsa et al., 2015), PTSD (Steele et al., 2018; Zepeda Méndez et al., 2018), and EDs (Cook‐Cottone et al., 2008), comparing favorably to effect size estimates concerning standalone psychological treatments for these disorders.
Critically, the findings from the quality appraisal highlighted a predominance of single group pre‐post study designs in the mapped evidence, which precludes conclusions regarding the potential additional benefit of yoga to current evidence‐based psychological interventions. For example, four of the identified studies examined interventions with a mix of evidence‐based psychological components, yoga, and other potentially therapeutic components (e.g., equine‐assisted therapy and narrative writing), utilizing a single group design (Butler et al., 2008; Steele et al., 2018; Zalta et al., 2018). This prevents analysis of their relative contributions to the outcomes and calls for simpler interventions and/or component analyses. M. K. Khalsa et al. (2015) examined a combined yoga and CBT protocol (Y‐CBT) for sufferers of treatment‐resistant GAD. Although effect sizes for anxiety and related symptoms were favorable to those found for CBT alone in other trials, the authors acknowledged the uncontrolled nature of the study design was not equipped to test the hypothesis that yoga augments the benefits of CBT for the condition. A single study identified in this review has investigated the effects of yoga in comparison to a treatment protocol applying yoga as an adjunct to CBT for panic disorder (Vorkapic & Rangé, 2014). Utilizing an RCT design, the study established that both CBT and a combination of CBT and yoga led to significant reductions in panic and panic related symptoms. Despite a trend for greater reductions in symptomatology for the combined treatment, the small sample size limited the potential to examine whether this finding could be attributed to an augmenting effect of yoga. Taken together, this analysis identified cautious support for yoga to augment CBT, particularly for anxiety disorders. A strength of the current study was the application of the evidence levels specified by the OCEBM (2011) for all included studies and the ascribing of recommendation categories for combined protocols for each condition of interest. Specifically, this analysis identified that the inclusion of yoga is suggested to augment CBT for anxiety and depression. Combined protocols for PTSD where current evidence is limited to low grade data, merits consideration only.
Only one of the mapped studies included qualitative methods to investigate the experiences of participants of a combined treatment, specifically incorporating a therapeutic yoga program as an adjunct to CBT (O'Shea et al., 2021; O'Shea, 2020). Findings of this study indicate that adults with anxiety and depression experience therapeutic yoga as an acceptable and suitable adjunct to CBT, and attribute many of the clinical benefits of the treatment to the combined approach. The primary quantitative outcomes of this pragmatic mixed‐methods study are yet to be published.
4.2. Future research directions
How yoga‐based interventions interact with established treatments for depression has been identified as a key question that requires answering to move the evidence for yoga as a potential treatment forward (Nauphal et al., 2019). Despite the recent growth of yoga research in the mental health field, this review illustrates a paucity of studies addressing the question of whether yoga has the potential to improve outcomes for people with depression as well as the other common mental disorders, when used with evidence‐based psychological therapies. Rather, most reviewed studies were small underpowered pilot studies of adapted treatment protocols whereby yoga was integrated or used as an adjunct with an evidence‐based psychological intervention, and any additional effects of yoga could not be dismantled. Self‐selection of participants into most included studies also limits a full understanding of the clinical impacts of these new interventions for participants assigned to them in usual practice. Nevertheless, conducting small open or pilot trials of a single intervention are generally accepted as building blocks, before an RCT can be justified, and do not typically include primary aims regarding efficacy (Freedland, 2020). Given the positive preliminary findings identified in the uncontrolled trials reviewed here, future research is encouraged to focus on adequately powered and designed trials, such as RCTs, to determine the relative effects of evidence‐based psychological interventions with and without yoga.
Current evidence also demonstrates a preponderance of quantitative enquiry. Only one study included qualitative data as part of a mixed‐methods design (O'Shea et al., 2021). An expansion of research to include individual perspectives from those participating in yoga alongside standard psychological care will deepen our understanding of the barriers and enablers to these integrative approaches, as well as any possible mechanisms driving change over time (Barkham et al., 2010; Capon et al., 2019). Given yoga yields some clinical benefit on psychological variables, such as self‐regulation (Dick et al., 2014), mindfulness (Tellhed et al., 2019; Tihanyi et al., 2016), and self‐efficacy (Franzblau et al., 2006; Martin et al., 2015), which are also the targets of psychological interventions, qualititative enquiries could contribute important findings for the development of new integrated treatments.
With such a focus on quantitative research designs, the acceptability and feasibility of yoga used alongside evidence‐based psychological treatments have also not been sufficiently examined, with only two studies adopting measures relevant to these two aspects (O'Shea, 2020; Zepeda Méndez et al., 2018). Considering the costs of larger controlled studies, an understanding of the acceptability and feasibility of implementing yoga alongside psychological treatments via the collection of data such as recruitment, retention, tolerability, and treatment safety (Thabane et al., 2010) is critical. Similarly, gathering the perspectives of health practitioners such as clinical psychologists regarding the inclusion of yoga with current therapeutic approaches is necessary (Liem, 2020), including due regard to the potential ethical issues that arise when combining yoga with evidence‐based treatments (Kamradt, 2017).
4.3. Clinical implications
The findings of this review provide cautious and preliminary support for applying yoga to the current evidenced psychological interventions for mental disorders. This aligns with the emerging dialog between the schools of yoga and psychology regarding the potential benefits of including yoga in psychological treatment plans (Caplan et al., 2013; Forfylow, 2011; Patwardhan, 2016; Valente & Marotta, 2011). Further, given the substantial burden for adults who do not engage with recommended treatment, such as CBT, or prematurely terminate it, the potential for yoga to safely support engagement and retention holds important promise and is worthy of further exploration. Importantly, many adults with mental disorder seek CIH approaches, such as yoga, on the premise that they reduce the stigma of treatment or because they hold a preference for mind‐body approaches (de Jonge et al., 2018; Gureje et al., 2015; Simon et al., 2020).
Research on the use of yoga as a complement to CBT is the most advanced, with numerous hypotheses proposing how yoga might augment the benefits of CBT. For example, by describing the impacts of yoga on the default mode network (Hasenkamp et al., 2012) and the autonomic nervous system, M. K. Khalsa et al. (2015) hypothesized that yoga facilitates positive changes in both the relaxation response of the parasympathetic nervous system, as well as cognitive processes that enhance engagement with CBT techniques. The authors suggest that CBT and yoga are complementary in the way that yoga induces states of relaxation, which in turn reduces negative cognitive patterns such as rumination, while CBT promotes disputing and challenging negative thoughts when they arise. Similarly, Vorkapic and Rangé (2014) concluded that yoga and other mindfulness practices share similar concepts allowing for a reinforcing and complementary effect when used together. They noted that both CBT and yoga encourage awareness of negative thinking and that yoga supported the capacity for practitioners to decentralize and detach from these cognitive experiences in such a way that more flexible and helpful cognitive responses were possible. Indeed, the lived experiences examined by O'Shea et al. (2021) of adults with anxiety and depression engaged in therapeutic yoga alongside CBT indicated that yoga reinforced and built upon such aspects of CBT, such as cognitive restructuring and behavioral activation. Although the current evidence limits the extent to which these hypotheses can be examined, they hold promise for the ways in which yoga and CBT might be mutually beneficial and encourage further examination of integration points between yoga and other psychological treatments.
The increasing prominence of yoga in more condensed and intensive treatment programs for PTSD was also notable. Poor engagement, high rates of drop‐out and nonresponse are typically problematic for current evidence‐based treatments for PTSD, including CBT and EMDR (Kehle‐Forbes et al., 2016). Findings reported here suggest that yoga might be an important component to such emerging treatment models through its effects on reducing arousal and other symptoms of PTSD and increasing commitment to treatment interventions. Similarly, treatment of EDs has similarly shown only moderate effects, with mixed compliance and high relapse rates (Bandini et al., 2006; Borden & Cook‐Cottone, 2020; Grenon et al., 2019; Khalsa et al., 2017; Solmi et al., 2021; van den Berg et al., 2019). Research using yoga in combination with standard treatments for EDs is new and developing [for a review, see Borden and Cook‐Cottone (2020)], with small to moderate effects reported across ED symptoms for yoga‐based interventions. The single trial examining a combined approach of CBT, DBT and yoga for treating EDs identified here is the start of an evidence base for incorporating yoga when treating EDs and suggests embodied approaches including yoga warrant further attention.
Finally, the role for yoga as a method to support cross‐cultural adaptation of evidence‐based psychological treatments in clinical practice is worthy of further consideration. Important conclusions were drawn by Niemi et al. (2016) that combining yoga with psychoeducation to treat depression in community primary care in Vietnam, was culturally relevant and scalable. Other researchers have also found that incorporating components of yoga with CBT among diverse cultural and ethnic minority groups promotes treatment adherence and positive expectations regarding outcomes for these groups (Hinton & Jalal, 2019; Hinton et al., 2009; Hinton et al., 2012; Kananian et al., 2017). Whilst these studies were not included in the current review as yoga protocols did not meet the criteria for hatha yoga, (with ‘yoga‐like stretches’ instead), they support a role for yoga to overcome barriers to treatment for groups underrepresented in psychological care and CBT in particular. Conversely, despite it being nondenominational, the possibility that yoga may be an unacceptable adjunct for some cultural groups must also be considered.
4.4. Limitations
Although the current study applied a robust methodology for identifying and synthesizing available evidence through the emergent review approach of evidence mapping, the following methodological limitations are noted. First, considering the relatively early stage of this study area, the review took an inclusive approach to the search strategy. Thus, the review appraised evidence of relatively lower quality when compared to “gold‐standard” approaches, such as RCTs. Whilst the quality appraisal approach utilized was an attempt to weight outcomes relative to the standard of the study designs employed, the application of a different approach to the appraisal of the evidence might have yielded different conclusions. Furthermore, the exclusion criteria for the review meant that trials of lower quality, such as case studies, were omitted, yielding the potential for the quality appraisal to be artificially inflated. Nevertheless, only studies representing unpublished dissertations were omitted because they did not meet the selection criteria (Golfinopoulos, 2015; Miller, 2005).
Similarly, a mapping review is primarily focussed on mapping existing evidence in a particular domain to direct future research in areas where evidence is limited (Miake‐Lye et al., 2016). As such, unlike other forms of review, such as systematic reviews and meta‐analytic studies, mapping reviews do not aim to assess efficacy of any intervention under examination. When and if the research field matures and a broader range of studies are available, the application of these review approaches will enable more robust conclusions regarding the effectiveness of yoga when used alongside evidence‐based psychological treatments. Finally, the review was focussed on yoga incorporated with evidence‐based psychological treatments in line with its interest in the relevance of yoga to clinical psychology. Accordingly, research relating to the practice of yoga when combined with psychological therapies with a less established evidence base was excluded, such as emotion‐focused psychoeducation and compassion‐focused therapy (Jonsson et al., 2020). Nevertheless, it is acknowledged that a broader lens may yield important observations to the area of integrative approaches in psychology. Similarly, the review was limited to evidence examining hatha‐yoga. Overall, a lack of consistency when reporting yoga intervention content, dosage and frequency of practice continues to hamper yoga research (Jeter et al., 2015). Even with the focus on hatha‐yoga, the mapped evidence identified that yoga interventions demonstrated considerable heterogeneity. Nevertheless, it is possible that a broader definition of yoga beyond hatha may have yielded different findings. For example, a small body of evidence combining yoga‐based breath practices alone (pranayama) with evidenced‐based psychological interventions was not reviewed here but shows promise (Descilo et al., 2010). The development and documentation of agreed elements of and dosage information regarding yoga interventions for mental disorders, for adoption in future research is broadly encouraged (de Manincor et al., 2015).
5. CONCLUSIONS
This review was the first to systematically represent the nature and extent of evidence for yoga as a complementary or adjunct treatment in clinical psychology practice. Findings gave rise to parallel narratives concerning positive trends for the useful application of yoga with current evidence‐based psychological therapies, along with necessary future research directions. Conclusions are limited by the small number of identified studies, so only cautious support can be offered for yoga as a complementary approach to psychological treatments for anxiety, depression, and PTSD. Overall, the research has lagged behind practice and efforts to now move the evidence forward are encouraged.
1. PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/jclp.23338.
6. ACKNOWLEDGMENTS
Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
O'Shea, M. , Capon, H. , Evans, S. , Agrawal, J. , Melvin, G. , O'Brien, J. , & McIver, S. (2022). Integration of hatha yoga and evidence‐based psychological treatments for common mental disorders: An evidence map. Journal of Clinical Psychology, 78, 1671–1711. 10.1002/jclp.23338
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Th e WHOQoL Group . (1998). Development of the World Health Organization WHOQOL‐BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. 10.1017/s0033291798006667 [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (AIHW) . (2018). Australia's health 2018. Australia's health series no. 16. https://www.aihw.gov.au/getmedia/7c42913d-295f-4bc9-9c24-4e44eff4a04a/aihw-aus-221.pdf.aspx?inline=true
- Australian Psychological Society (APS) . (2018). Evidence‐based psychological interventions in the treatment of mental disorders: A review of the literature. Australian Psychological Society. [Google Scholar]
- Baer, R. A. , Smith, G. T. , Lykins, E. , Button, D. , Krietemeyer, J. , & Sauer, S. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342. 10.1177/1073191107313003 [DOI] [PubMed] [Google Scholar]
- Bai, Z. , Luo, S. , Zhang, L. , Wu, S. , & Chi, I. (2020). Acceptance and Commitment Therapy (ACT) to reduce depression: A systematic review and meta‐analysis. Journal of Affective Disorders, 260, 728–737. 10.1016/j.jad.2019.09.040 [DOI] [PubMed] [Google Scholar]
- Bandini, S. , Antonelli, G. , Moretti, P. , Pampanelli, S. , Quartesan, R. , & Perriello, G. (2006). Factors affecting dropout in outpatient eating disorder treatment. Eating and Weight Disorders ‐ Studies on Anorexia, Bulimia and Obesity, 11(4), 179–184. 10.1007/BF03327569 [DOI] [PubMed] [Google Scholar]
- Barkham, M. , Hardy, G. E. , & Mellor‐Clark, J. (2010). Developing and delivering practice‐based evidence: A guide for the psychological therapies. Wiley‐Blackwell. [Google Scholar]
- Beck, A. , Steer, R. , & Brown, G. (2000). BDI‐II Beck depression inventory manual (2nd ed.). The Psychological Corporation. [Google Scholar]
- Beck, A. T. , & Steer, R. A. (1993). Beck anxiety inventory manual. The Psychological Corporation. [Google Scholar]
- Beck, M. (2008). Manual‐based group intervention for disordered eating: The innovative practice of integrating dbt, positive psychology, and yoga. (69). ProQuest Information & Learning. Available from EBSCO psyhdatabase.
- Beer, B. , Groote, F. , Oppenheim, H. J. , & Ten Broeke, E. (2015). Protocol Format casusconceptualisatie emdr [Protocol format case conceptualization EMDR]. www.emdr.nl
- van den Berg, E. , Houtzager, L. , de Vos, J. , Daemen, I. , Katsaragaki, G. , Karyotaki, E. , Dekker, J. , Cuijpers, P. , & Dekker, J. (2019). Meta‐analysis on the efficacy of psychological treatments for anorexia nervosa. European Eating Disorders Review, 27(4), 331–351. 10.1002/erv.2683 [DOI] [PubMed] [Google Scholar]
- Bond, F. W. , Hayes, S. C. , Baer, R. A. , Carpenter, K. M. , Guenole, N. , Orcutt, H. K. , Zettle, R. D. , Waltz, T. , & Zettle, R. D. (2011). Preliminary psychometric properties of the acceptance and action questionnaire‐II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Boni, M. , Schutze, R. , Kane, R. T. , Morgan‐Lowes, K. L. , Byrne, J. , & Egan, S. J. (2018). Mindfulness and avoidance mediate the relationship between yoga practice and anxiety. Complementary Therapies in Medicine, 40, 89–94. 10.1016/j.ctim.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Borden, A. , & Cook‐Cottone, C. (2020). Yoga and eating disorder prevention and treatment: A comprehensive review and meta‐analysis. Eating disorders, 28(4), 400–437. 10.1080/10640266.2020.1798172 [DOI] [PubMed] [Google Scholar]
- Briggs, J. M. (2017). Yoga as an ancillary treatment to acceptance and commitment therapy for depression. (78). ProQuest Information & Learning. EBSCOhost psyh database.
- Brinsley, J. , Schuch, F. , Lederman, O. , Girard, D. , Smout, M. , Immink, M. A. , Rosenbaum, S. , Stubbs, B. , Firth, J. , Davison, K. , & Rosenbaum, S. (2020). Effects of yoga on depressive symptoms in people with mental disorders: A systematic review and meta‐analysis. British Journal of Sports Medicine, 55, 992–1000. 10.1136/bjsports-2019-101242 [DOI] [PubMed] [Google Scholar]
- Brown, K. W. , & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well‐being. Journal of Personality and Social Psychology, 84(4), 822–848. [DOI] [PubMed] [Google Scholar]
- Burges, P. , Pirkis, J. E. , Slade, T. N. , Johnston, A. K. , Meadows, G. N. , & Gunn, J. M. (2009). Service use for mental health problems: Findings from the 2007 National Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry, 43(7), 615–623. 10.1080/00048670902970858 [DOI] [PubMed] [Google Scholar]
- Burns, D. D. (1999). The feeling good handbook. Penguin Books. [Google Scholar]
- Bussing, A. , Michalsen, A. , Khalsa, S. B. , Telles, S. , & Sherman, K. J. (2012). Effects of yoga on mental and physical health: A short summary of reviews. Evidence Based Complementary and Alternative Medicine, 2012, 165410. 10.1155/2012/165410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler, L. D. , Waelde, L. C. , Hastings, T. A. , Chen, X. ‐H. , Symons, B. , Marshall, J. , Spiegel, D. , Kaufman, A. , Nagy, T. F. , Blasey, C. M. , Seibert, E. O. , & Spiegel, D. (2008). Meditation with yoga, group therapy with hypnosis, and psychoeducation for long‐term depressed mood: A randomized pilot trial. Journal of Clinical Psychology, 64(7), 806–820. 10.1002/jclp.20496 [DOI] [PubMed] [Google Scholar]
- Butterfield, N. , Schultz, T. , Rasmussen, P. , & Proeve, M. (2017). Yoga and mindfulness for anxiety and depression and the role of mental health professionals: A literature review. The Journal of Mental Health Training, Education and Practice, 12(1), 44–54. 10.1108/JMHTEP-01-2016-0002 [DOI] [Google Scholar]
- Callahan, P. , Liu, P. , Purcell, R. , Parker, A. G. , & Hetrick, S. E. (2012). Evidence map of prevention and treatment interventions for depression in young people. Depression Research & Treatment, 2012, 820735. 10.1155/2012/820735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplan, M. , Portillo, A. , & Seely, L. (2013). Yoga psychotherapy: The integration of western psychological theory and ancient yogic wisdom. Journal of Transpersonal Psychology, 45(2). [Google Scholar]
- Capon, H. , O'Shea, M. , & McIver, S. (2019). Yoga and mental health: A synthesis of qualitative findings. Complementary therapies in Clinical Practice, 37, 122–132. 10.1016/j.ctcp.2019.101063 [DOI] [PubMed] [Google Scholar]
- Carmody, J. , & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well‐being in a mindfulness‐based stress reduction program. Journal of Behavioural Medicine, 31(1), 23–33. 10.1007/s10865-007-9130-7 [DOI] [PubMed] [Google Scholar]
- Chambless, D. L. , Caputo, G. C. , Bright, P. , & Gallagher, R. (1984). Assessment of fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. Journal of Consulting and Clinical Psychology, 52(6), 1090–1097. 10.1037/0022-006X.52.6.1090 [DOI] [PubMed] [Google Scholar]
- Collins, N. L. (1996). Working models of attachment: Implications for explanation, emotion and behavior. Journal of Personality and Social Psychology, 71(4), 810–832. 10.1037//0022-3514.71.4.810 [DOI] [PubMed] [Google Scholar]
- Cook‐Cottone, C. , Beck, M. , & Kane, L. (2008). Manualized‐group treatment of eating disorders: Attunement in mind, body, and relationship (AMBR). The Journal for Specialists in Group Work, 33(1), 61–83. 10.1080/01933920701798570 [DOI] [Google Scholar]
- Cramer, H. , Lauche, R. , Langhorst, J. , & Dobos, G. (2013). Yoga for depression: A systematic review and meta‐analysis. Depression and Anxiety, 30(11), 1068–1083. 10.1002/da.22166 [DOI] [PubMed] [Google Scholar]
- Cramer, H. , Anheyer, D. , Lauche, R. , & Dobos, G. (2017). A systematic review of yoga for major depressive disorder. Journal of Affective Disorders, 213, 70–77. 10.1016/j.jad.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Cramer, H. , Anheyer, D. , Saha, F. J. , & Dobos, G. (2018). Yoga for posttraumatic stress disorder: A systematic review and meta‐analysis. BMC Psychiatry, 18(1), 72. 10.1186/s12888-018-1650-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer, H. , Lauche, R. , Klose, P. , Langhorst, J. , & Dobos, G. (2013). Yoga for schizophrenia: A systematic review and meta‐analysis. BMC Psychiatry, 13, 32. 10.1186/1471-244X-13-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer, H. , Lauche, R. , Anheyer, D. , Pilkington, K. , de Manincor, M. , Dobos, G. , & Ward, L. (2018). Yoga for anxiety: A systematic review and meta‐analysis of randomized controlled trials. Depression and Anxiety, 35(9), 830–843. 10.1002/da.22762 [DOI] [PubMed] [Google Scholar]
- Crews, D. A. , Stolz‐Newton, M. , & Grant, N. S. (2016). The use of yoga to build self‐compassion as a healing method for survivors of sexual violence. Journal of Religion & Spirituality in Social Work: Social Thought, 35(3), 139–156. 10.1080/15426432.2015.1067583 [DOI] [Google Scholar]
- Davidson, J. R. , Book, S. W. , Colket, J. T. , Tupler, L. A. , Roth, S. , David, D. , Smith, R. D. , Hertzberg, M. , Mellman, T. , Beckham, J. C. , Smith, R. D. , Davison, R. M. , Katz, R. , & Feldman, M. E. (1997). Assessment of a new self‐rating scale for post‐traumatic stress disorder. Psychological Medicine, 27(1), 153–160. [DOI] [PubMed] [Google Scholar]
- De Michelis, E. (2004). A history of modern yoga: Patanjali and western esotericism. Bloomsbury Publishing PLC. [Google Scholar]
- Descilo, T. , Vedamurtachar, A. , Gerbarg, P. L. , Nagaraja, D. , Gangadhar, B. N. , Damodaran, B. , Brown, R. P. , Adelson, B. , Braslow, L. H. , Marcus, S. , & Brown, R. P. (2010). Effects of a yoga breath intervention alone and in combination with an exposure therapy for post‐traumatic stress disorder and depression in survivors of the 2004 South‐East Asia tsunami. Acta Psychiatrica Scandinavica, 121(4), 289–300. 10.1111/j.1600-0447.2009.01466.x [DOI] [PubMed] [Google Scholar]
- Desikachar, T. K. V. (1995). The heart of yoga: Developing a personal practice. Inner Traditions International. [Google Scholar]
- Dick, A. M. , Niles, B. L. , Street, A. E. , DiMartino, D. M. , & Mitchell, K. S. (2014). Examining mechanisms of change in a yoga intervention for women: The influence of mindfulness, psychological flexibility, and emotion regulation on PTSD symptoms. Journal of Clinical Psychology, 70(12), 1170–1182. 10.1002/jclp.22104 [DOI] [PubMed] [Google Scholar]
- Eliot, E. (2008). Yoga off the mat: Motivating clients to surrender to discomfort. Annals of the American Psychotherapy, 11, 18–25. [Google Scholar]
- Elkins, G. , Marcus, J. , Rajab, M. H. , & Durgam, S. (2005). Complementary and alternative therapy use by psychotherapy clients. Psychotherapy: Theory, Research, Practice, Training, 42(2), 232–235. 10.1037/0033-3204.42.2.232 [DOI] [Google Scholar]
- Field, T. (2016). Yoga research review. Complementary Therapies in Clinical Practice, 24, 145–161. 10.1016/j.ctcp.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Foa, E. B. , Ehlers, A. , Clark, D. M. , Tolin, D. F. , & Orsillo, S. M. (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. [Google Scholar]
- Forfylow, A. (2011). Integrating yoga with psychotherapy: A complementary treatment for anxiety and depression. Canadian Journal of Counselling and Psychotherapy, 45(2), 132–150. [Google Scholar]
- Franzblau, S. H. , Smith, M. , Echevarria, S. , & Van Cantfort, T. E. (2006). Take a breath, break the silence: The effects of yogic breathing and testimony about batterying on feelings of self‐efficacy in battered women. International Journal Of Yoga Therapy, 16, 49–57. [Google Scholar]
- Freedland, K. E. (2020). Pilot trials in health‐related behavioral intervention research: Problems, solutions, and recommendations. Health Psychology, 39(10), 851–862. 10.1037/hea0000946 [DOI] [PubMed] [Google Scholar]
- Frischholz, E. J. , Braun, B. G. , Sachs, R. G. , & Hopkins, L. (1990). The Dissociative Experiences Scale: Further replication and validation. Dissociation: Progress in the Dissociative Disorders, 3(3), 151–153. [Google Scholar]
- Gard, T. , Brach, N. , Hölzel, B. , Noggle, J. J. , Conboy, L. A. , & Lazar, S. W. (2012). Effects of a yoga‐based intervention for young adults on quality of life and perceived stress: The potential mediating roles of mindfulness and self‐compassion. The Journal of Positive Psychology, 7(3), 165–175. 10.1080/17439760.2012.667144 [DOI] [Google Scholar]
- Garner, D. (1991). Eating disorder inventory‐2 professional manual. Psychological Assessment Resources, Inc. [Google Scholar]
- Ghahari, S. , Mohammadi‐Hasel, K. , Malakouti, S. K. , & Roshanpajouh, M. (2020). Mindfulness‐based cognitive therapy for generalised anxiety disorder: A systematic review and meta‐analysis. East Asian Archives of Psychiatry, 30(2), 52–56. 10.12809/eaap1885 [DOI] [PubMed] [Google Scholar]
- Goldberg, S. B. , Tucker, R. P. , Greene, P. A. , Davidson, R. J. , Kearney, D. J. , & Simpson, T. L. (2019). Mindfulness‐based cognitive therapy for the treatment of current depressive symptoms: A meta‐analysis. Cognitive Behaviour Therapy, 48(6), 445–462. 10.1080/16506073.2018.1556330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golfinopoulos, C. (2015). A qualitative study of women diagnosed with generalized anxiety disorder utilizing complementary medicine in conjunction with psychotherapy. (75). ProQuest Information & Learning. EBSCOhost psych database.
- Grenon, R. , Carlucci, S. , Brugnera, A. , Schwartze, D. , Hammond, N. , Ivanova, I. , Tasca, G. A. , Mcquaid, N. , Proulx, G. , & Tasca, G. A. (2019). Psychotherapy for eating disorders: A meta‐analysis of direct comparisons. Psychotherapy Research, 29(7), 833–845. 10.1080/10503307.2018.1489162 [DOI] [PubMed] [Google Scholar]
- Gupta, B. , Ahmed, K. M. , Dhawan, S. , & Gupta, R. (2018). Yoga research a scientometric assessment of global publications output during 2007‐16. Pharmacognosy Journal, 10(3), 394–402. 10.5530/pj.2018.3.65 [DOI] [Google Scholar]
- Gureje, O. , Nortje, G. , Makanjuola, V. , Oladeji, B. , Seedat, S. , & Jenkins, R. (2015). The role of global traditional and complementary systems of medicine in treating mental health problems. Lancet Psychiatry, 2(2), 168–177. 10.1016/s2215-0366(15)00013-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutner, C. A. , Gallagher, M. W. , Baker, A. S. , Sloan, D. M. , & Resick, P. A. (2016). Time course of treatment dropout in cognitive‐behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice and Policy, 8(1), 115–121. 10.1037/tra0000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton, M. (1959). The assessment of anxiety states by rating. British Journal of Medical Psychology, 32, 50–55. [DOI] [PubMed] [Google Scholar]
- Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 25, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hans, E. , & Hiller, W. (2013). Effectiveness of and dropout from outpatient cognitive behavioral therapy for adult unipolar depression: A meta‐analysis of nonrandomized effectiveness studies. Journal of Consulting & Clinical Psychology, 81(1), 75–88. 10.1037/a0031080 [DOI] [PubMed] [Google Scholar]
- Hansen, A. H. , & Kristoffersen, A. E. (2016). The use of CAM providers and psychiatric outpatient services in people with anxiety/depression: A cross‐sectional survey. BMC Complementary and Alternative Medicine, 16(1), 461. 10.1186/s12906-016-1446-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasenkamp, W. , Wilson‐Mendenhall, C. D. , Duncan, E. , & Barsalou, L. W. (2012). Mind wandering and attention during focused meditation: A fine‐grained temporal analysis of fluctuating cognitive states. NeuroImage, 59(1), 750–760. 10.1016/j.neuroimage.2011.07.008 [DOI] [PubMed] [Google Scholar]
- Hayes, S. C. (2011). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). Guilford Publications. [Google Scholar]
- Hinton, D. E. , & Jalal, B. (2019). Dimensions of culturally sensitive CBT: Application to Southeast Asian populations. American Journal of Orthopsychiatry, 89(4), 493–507. [DOI] [PubMed] [Google Scholar]
- Hinton, D. E. , Hofmann, S. G. , Pollack, M. H. , & Otto, M. W. (2009). Mechanisms of efficacy of CBT for Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure response. CNS Neuroscience & Therapeutics, 15(3), 255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton, D. E. , Rivera, E. I. , Hofmann, S. G. , Barlow, D. H. , & Otto, M. W. (2012). Adapting CBT for traumatized refugees and ethnic minority patients: Examples from culturally adapted CBT (CA‐CBT). Transcultural Psychiatry, 49(2), 340–365. 10.1177/1363461512441595 [DOI] [PubMed] [Google Scholar]
- Hofmann, S. G. , Sawyer, A. T. , & Fang, A. (2010). The empirical status of the "new wave" of CBT. Psychiatric Clinics of North America, 33(3), 701–710. 10.1016/j.psc.2010.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann, S. G. , Asnaani, A. , Vonk, I. J. J. , Sawyer, A. T. , & Fang, A. (2012). The efficacy of cognitive behavioral therapy: Aa review of meta‐analyses. Cognitive Therapy and Research, 36(5), 427–440. 10.1007/s10608-012-9476-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howick, J. , Chalmers, I. , Glasziou, P. , Greenhalgh, T. , Heneghan, C. , Liberati, A. , & Thornton, H. (2011). Explanation of the 2011 Oxford Centre for Evidence‐Based Medicine (OCEBM) levels of evidence (Background Document). https://www.cebm.ox.ac.uk/resources/levels-of-evidence/explanation-of-the-2011-ocebm-levels-of-evidence/
- Huhn, M. , Tardy, M. , Spineli, L. M. , Kissling, W. , Förstl, H. , Pitschel‐Walz, G. , Leucht, S. , Leucht, C. , Samara, M. , Dold, M. , Davis, J. M. , & Leucht, S. (2014). Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders. JAMA Psychiatry, 71(6), 706–715. [DOI] [PubMed] [Google Scholar]
- Jeter, P. E. , Slutsky, J. , Singh, N. , & Khalsa, S. B. (2015). Yoga as a therapeutic intervention: A bibliometric analysis of published research studies from 1967 to 2013. Journal of Alternative and Complementary Medicine, 21(10), 586–592. 10.1089/acm.2015.0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jonge, P. , Wardenaar, K. J. , Hoenders, H. R. , Evans‐Lacko, S. , Kovess‐Masfety, V. , Aguilar‐Gaxiola, S. , Thornicroft, G. , Al‐Hamzawi, A. , Alonso, J. , Andrade, L. H. , Benjet, C. , Bromet, E. J. , Bruffaerts, R. , Bunting, B. , Caldas‐de‐Almeida, J. M. , Dinolova, R. V. , Florescu, S. , de Girolamo, G. , Gureje, O. , … Thornicroft, G. (2018). Complementary and alternative medicine contacts by persons with mental disorders in 25 countries: Results from the World Mental Health Surveys. Epidemiology and Psychiatric Sciences, 27(6), 552–567. 10.1017/S2045796017000774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonsson, G. , Franzén, L. , Nyström, M. B. T. , & Davis, P. A. (2020). Integrating yoga with psychological group‐treatment for mixed depression and anxiety in primary healthcare: An explorative pilot study. Complementary Therapies in Clinical Practice, 41, 101250. 10.1016/j.ctcp.2020.101250 [DOI] [PubMed] [Google Scholar]
- Kabat‐Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. Hyperion. [Google Scholar]
- Kamradt, J. M. (2017). Integrating yoga into psychotherapy: The ethics of moving from the mind to the mat. Complementary Therapies in Clinical Practice, 27, 27–30. 10.1016/j.ctcp.2017.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kananian, S. , Ayoughi, S. , Farugie, A. , Hinton, D. , & Stangier, U. (2017). Transdiagnostic culturally adapted CBT with Farsi‐speaking refugees: A pilot study. European Journal of Psychotraumatology, 8(Suppl 2), 1–10. 10.1080/20008198.2017.1390362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz, D. L. , Williams, A. ‐l , Girard, C. , Goodman, J. , Comerford, B. , Behrman, A. , & Bracken, M. B. (2003). The evidence base for complementary and alternative medicine: Methods of evidence mapping with application to CAM. Alternative Therapies in Health and Medicine, 9(4), 22–37. [PubMed] [Google Scholar]
- Keane, T. M. , Caddell, J. M. , & Taylor, K. L. (1988). Mississippi scale for combat‐related posttraumatic stress disorder: Three studies in reliability and validity. Journal of Consulting and Clinical Psychology, 56(1), 85–90. [DOI] [PubMed] [Google Scholar]
- Kehle‐Forbes, S. M. , Meis, L. A. , Spoont, M. R. , & Polusny, M. A. (2016). Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological Trauma, 8(1), 107–114. 10.1037/tra0000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keijsers, G. , Kampman, M. , & Hoogduin, C. (2001). Dropout prediction in cognitive behavior therapy for panic disorder. Behavior Therapy, 32(4), 739–749. 10.1016/S0005-7894(01)80018-6 [DOI] [Google Scholar]
- Keller, M. B. , Lavori, P. W. , Friedman, B. , Nielsen, E. , Endicott, J. , McDonald‐Scott, P. , & Andreasen, N. C. (1987). The longitudinal interval follow‐up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44(6), 540–548. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Aguilar‐Gaxiola, S. , Alonso, J. , Chatterji, S. , Lee, S. , Ormel, J. , Wang, P. S. , Ustün, T. B. , & Wang, P. S. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiologia e Psichiatria Sociale, 18(1), 23–33. 10.1017/s1121189x00001421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa, M. K. , Greiner‐Ferris, J. M. , Hofmann, S. G. , & Khalsa, S. B. S. (2015). Yoga‐enhanced cognitive behavioural therapy (Y‐CBT) for anxiety management: A pilot study. Clinical Psychology and Psychotherapy, 22(4), 364–371. 10.1002/cpp.1902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa, S. S. , Portnoff, L. C. , McCurdy‐McKinnon, D. , & Feusner, J. D. (2017). What happens after treatment? A systematic review of relapse, remission, and recovery in anorexia nervosa. Journal of Eating Disorders, 5, 20. 10.1186/s40337-017-0145-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kishida, M. , Mama, S. K. , Larkey, L. K. , & Elavsky, S. (2018). "Yoga resets my inner peace barometer": A qualitative study illuminating the pathways of how yoga impacts one's relationship to oneself and to others. Complementary Therapy Medicine, 40, 215–221. 10.1016/j.ctim.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Kraftsow, G. (1999). Yoga for wellness. Penguin Books. [Google Scholar]
- Kraus, D. R. , Seligman, D. A. , & Jordan, J. R. (2005). Validation of a behavioral health treatment outcome and assessment tool designed for naturalistic settings: The Treatment Outcome Package. Journal of Clinical Psychology, 61(3), 285–314. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. W. (2001). The PHQ‐9. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang, A. J. (2013). What mindfulness brings to psychotherapy for anxiety and depression. Depression and Anxiety. [DOI] [PubMed]
- Larsen, D. L. , Attkisson, C. C. , Hargreaves, W. A. , & Nguyen, T. D. (1979). Client satisfaction questionnaire. [DOI] [PubMed]
- Liem, A. (2020). The possibilities and challenges of integrative medicine implementation in clinical psychology: A qualitative study in Indonesia. BMC Complementary Medicine and Therapies, 20(1), 223. 10.1186/s12906-020-03019-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon, J. , Hindle, A. , & Brennan, L. (2018). Dropout from cognitive‐behavioral therapy for eating disorders: A meta‐analysis of randomized, controlled trials. International Journal of Eating Disorders, 51(5), 381–391. 10.1002/eat.22850 [DOI] [PubMed] [Google Scholar]
- Linehan, M. (2014). DBT skills training manual. The Guilford Press. [Google Scholar]
- Lovibond, S. , & Lovibond, P. (1996). Manual for the Depression Anxiety Stress Scales. Psychology Foundation of Australia. [Google Scholar]
- de Manincor, M. , Bensoussan, A. , Smith, C. , Fahey, P. , & Bourchier, S. (2015). Establishing key components of yoga interventions for reducing depression and anxiety, and improving well‐being: A Delphi method study. BMC Complementary and Alternative Medicine, 15, 85. 10.1186/s12906-015-0614-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin, E. C. , Dick, A. M. , Scioli‐Salter, E. R. , & Mitchell, K. S. (2015). Impact of a yoga intervention on physical activity, self‐efficacy, and motivation in women with PTSD symptoms. Journal of Alternative and Complementary Medicine, 21(6), 327–332. 10.1089/acm.2014.0389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, B. J. , Kocsis, J. H. , Leon, A. C. , Thompson, S. , Frances, A. J. , & Morgan, R. O. (1995). Assessment of symptoms and change in dysthymic disorder. In Kocsis J. H., & Klein D. N. (Eds.), Diagnosis and treatment of chronic depression (pp. 73–88). Guildford Press. [Google Scholar]
- Miake‐Lye, I. M. , Hempel, S. , Shanman, R. , & Shekelle, P. G. (2016). What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Systematic Reviews, 5, 28. 10.1186/s13643-016-0204-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz, D. , Semple, R. , Hauser, M. , Elkun, D. , Weintraub, M. , & Dimidjian, S. (2015). Mindfulness‐based cognitive therapy for perinatal women with depression or bipolar spectrum disorder. Cognitive Therapy & Research, 39(5), 590–600. 10.1007/s10608-015-9681-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, T. M. (2005). The integration of short‐term dynamic therapy and yoga in the treatment of generalized anxiety disorder and depression. (66). ProQuest Information & Learning. EBSCOhost psyh database.
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , Petticrew, M. , Stewart, L. A. , Shekelle, P. , Stewart, L. A. , & PRISMA‐P, G. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Systematic Reviews, 4, 1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash, W. P. , Marino Carper, T. L. , Mills, M. A. , Au, T. , Goldsmith, A. , & Litz, B. T. (2013). Psychometric evaluation of the moral injury events scale. Military Medicine, 178(6), 646–652. [DOI] [PubMed] [Google Scholar]
- Nathan, P. , Smith, L. , Rees, C. , Correia, H. , Juniper, U. , Kingsep, P. , & Lim, L. (2004). Mood management course: A cognitive behavioural group treatment programme for anxiety disorders and depression (2nd ed.). Centre for Clinical Interventions. [Google Scholar]
- National Centre for Complementary and Integrative Health (NCCIH) . (2008). Complementary, alternative, or integrative health: What's in a name? https://nccih.nih.gov/health/integrative-health#term http://nccam.nih.gov/sites/nccam.nih.gov/files/%20D347_05-25-2012.pdf
- National Institute of Care Excellence (NICE) . (2005). Obsessive‐compulsive disorder and body dysmorphic disorder: treatment: Clinical guideline [CG31]. https://www.nice.org.uk/guidance/cg31 [PubMed]
- Nauphal, M. , Mischoulon, D. , Uebelacker, L. , Streeter, C. , & Nyer, M. (2019). Yoga for the treatment of depression: Five questions to move the evidence‐base forward. Complementary Therapies in Medicine, 46, 153–157. 10.1016/j.ctim.2019.08.012 [DOI] [PubMed] [Google Scholar]
- Neukirch, N. , Reid, S. , & Shires, A. (2019). Yoga for PTSD and the role of interoceptive awareness: A preliminary mixed‐methods case series study. European Journal of Trauma and Dissociation, 3(1), 7–15. 10.1016/j.ejtd.2018.10.003 [DOI] [Google Scholar]
- NICE . (2009). Depression in adults: recognition and management: Clinical guideline [CG90]. https://www.nice.org.uk/guidance/cg90
- NICE . (2011a). Common mental health problems: identification and pathways to care: Clinical guideline [CG123]. https://www.nice.org.uk/guidance/cg123
- NICE . (2011b). Depression in adults. https://www.nice.org.uk/guidance/qs8/resources/depression-in-adults-pdf-58302785221
- NICE . (2011c). Generalised anxiety disorder and panic disorder in adults: management: Clinical guideline [CG113]. https://www.nice.org.uk/guidance/cg113 [PubMed]
- NICE . (2013). Social anxiety disorder: recognition, assessment and treatment: Clinical guideline [CG159]. https://www.nice.org.uk/guidance/cg159
- NICE . (2014). Anxiety disorders: Quality standard [QS53]. https://www.nice.org.uk/guidance/qs53
- NICE . (2017). Eating disorders: recognition and treatment: Clinical guideline [NG69]. https://www.nice.org.uk/guidance/ng69
- NICE . (2018). Post‐traumatic stress disorder: Clinical guideline [NG116]. https://www.nice.org.uk/guidance/ng116
- Niemi, M. , Kiel, S. , Allebeck, P. , & Hoan, L. T. (2016). Community‐based intervention for depression management at the primary care level in Ha Nam Province, Vietnam: A cluster‐randomised controlled trial. Tropical Medicine & International Health, 21(5), 654–661. 10.1111/tmi.12674 [DOI] [PubMed] [Google Scholar]
- O'Shea, M. (2020). Examining yoga as an adjunct treatment to CBT for adults with anxiety and depression. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=375465%26isReview=true
- O'Shea, M. , Capon, H. , Evans, S. , & McIver, S. (2021). Yoga complements cognitive behaviour therapy as an adjunct treatment for anxiety and depression: Qualitative findings from a mixed‐methods study. Psychology and Psychotherapy: Theory, Research and Practice, 94, 1015–1035. 10.1111/papt.12343 [DOI] [PubMed] [Google Scholar]
- Ostermann, T. , Vogel, H. , Boehm, K. , & Cramer, H. (2019). Effects of yoga on eating disorders: A systematic review. Complementary Therapies in Medicine, 46, 73–80. 10.1016/j.ctim.2019.07.021 [DOI] [PubMed] [Google Scholar]
- Oxford Centre for Evidence‐Based Medicine (OCEBM) . (2011). The Oxford 2011 levels of evidence. http://www.cebm.net/index.aspx?o=5653
- Panos, P. T. , Jackson, J. W. , Hasan, O. , & Panos, A. (2014). Meta‐analysis and systematic review assessing the efficacy of dialectical behavior therapy (DBT). Research on Social Work Practice, 24(2), 213–223. 10.1177/1049731513503047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, C. (2013). Mind‐body CAM interventions: Current status and considerations for integration into clinical health psychology. Journal of Clinical Psychology, 69(1), 45–63. 10.1002/jclp.21910 [DOI] [PubMed] [Google Scholar]
- Park, C. , Riley, K. , Bedesin, E. , & Stewart, V. (2016). Why practice yoga? Practitioners' motivations for adopting and maintaining yoga practice. Journal of Health Psychology, 21(6), 887–896. 10.1177/1359105314541314 [DOI] [PubMed] [Google Scholar]
- Park, C. , Finkelstein‐Fox, L. , Groessl, E. J. , Elwy, A. R. , & Lee, S. Y. (2020). Exploring how different types of yoga change psychological resources and emotional well‐being across a single session. Complementary Therapies in Medicine, 49, 102354. 10.1016/j.ctim.2020.102354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, V. , Weiss, H. A. , Chowdhary, N. , Naik, S. , Pednekar, S. , Chatterjee, S. , De Silva, M. J. , Bhat, B. , Araya, R. , King, M. , Simon, G. , Verdeli, H. , & Kirkwood, B. R. (2010). Effectiveness of an inter[1]vention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet, 376, 2086–2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patwardhan, A. (2016). Is the integration of yoga with psychotherapy compatible? What are the risks? Journal of Psychology & Psychotherapy, 6(261), 2161. [Google Scholar]
- Penman, S. , Cohen, M. , Stevens, P. , & Jackson, S. (2012). Yoga in Australia: Results of a national survey. International Journal of Yoga, 5(2), 92–101. 10.4103/0973-6131.98217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivest‐Gadbois, E. , & Boudrias, M. H. (2019). What are the known effects of yoga on the brain in relation to motor performances, body awareness and pain? A narrative review. Complementary Therapies in Medicine, 44, 129–142. 10.1016/j.ctim.2019.03.021 [DOI] [PubMed] [Google Scholar]
- Segal, Z. V. , Williams, J. M. G. , & Teasdale, J. D. (2013). Mindfulness‐based cognitive therapy for depression (2nd ed.). The Guilford Press. [Google Scholar]
- Shannahoff‐Khalsa, D. S. (2006). Kundalini yoga meditation: Techniques specific for psychiatric disorders, couples therapy, and personal growth. W W Norton & Co. [Google Scholar]
- Simon, N. M. , Hofmann, S. G. , Rosenfield, D. , Hoeppner, S. S. , Hoge, E. A. , Bui, E. , & Khalsa, S. B. S. (2020). Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder. JAMA Psychiatry, 78, 13. 10.1001/jamapsychiatry.2020.2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton, M. (2010). Yoga body: The origins of modern posture practice. Oxford University Press. [Google Scholar]
- Smyth, C. (1999). The Pittsburgh Sleep Quality Index (PSQI). Journal of Gerontological Nursing, 25(12), 10–11. [DOI] [PubMed] [Google Scholar]
- Snaith, N. , Schultz, T. , Proeve, M. , & Rasmussen, P. (2018). Mindfulness, self‐compassion, anxiety and depression measures in South Australian yoga participants: Implications for designing a yoga intervention. Complementary Therapies in Clinical Practice, 32, 92–99. 10.1016/j.ctcp.2018.05.009 [DOI] [PubMed] [Google Scholar]
- Solmi, M. , Wade, T. D. , Byrne, S. , Del Giovane, C. , Fairburn, C. G. , Ostinelli, E. G. , Cipriani, A. , De Crescenzo, F. , Johnson, C. , Schmidt, U. , Treasure, J. , Favaro, A. , Zipfel, S. , & Cipriani, A. (2021). Comparative efficacy and acceptability of psychological interventions for the treatment of adult outpatients with anorexia nervosa: A systematic review and network meta‐analysis. Lancet Psychiatry, 8(3), 215–224. 10.1016/s2215-0366(20)30566-6 [DOI] [PubMed] [Google Scholar]
- Spielberger, C. D. (1983). State‐trait anxiety inventory for adults.
- Spinks, J. , & Hollingsworth, B. (2012). Policy implications of complementary and alternative medicine use in Australia: Data from the National Health Survey. Journal of Alternative & Complementary Medicine, 18(4), 371–378. 10.1089/acm.2010.0817 [DOI] [PubMed] [Google Scholar]
- Staples, J. (2018). A cognitive behavioral therapy and yoga program for trauma symptoms. Georgetown University. Clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT02368444
- Steel, Z. , Marnane, C. , Iranpour, C. , Chey, T. , Jackson, J. W. , Patel, V. , & Silove, D. (2014). The global prevalence of common mental disorders: A systematic review and meta‐analysis 1980‐2013. International Journal of Epidemiology (London), 43(2), 476–493. 10.1093/ije/dyu038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele, E. , Wood, D. S. , Usadi, E. J. , & Applegarth, D. M. (2018). TRR's warrior camp: An intensive treatment program for combat trauma in active military and veterans of all eras. Military Medicine, 183, 403–407. 10.1093/milmed/usx153 [DOI] [PubMed] [Google Scholar]
- Strecker, T. , & Fortney, J. (2011). Barriers to mental health treatment among veterans. In Ruzek J. I., Schnurr P. P., Vasterling J. J., & Freidman M. (Eds.), Caring for veterans with deployment‐related stress disorders. American Psychological Association. [Google Scholar]
- Swift, J. K. , & Greenberg, R. P. (2014). A treatment by disorder meta‐analysis of dropout from psychotherapy. Journal of Psychotherapy Integration, 24(3), 193–207. 10.1037/a0037512 [DOI] [Google Scholar]
- Tellhed, U. , Daukantaitė, D. , Maddux, R. E. , Svensson, T. , & Melander, O. (2019). Yogic breathing and mindfulness as stress coping mediate positive health outcomes of yoga. Mindfulness, 10(12), 2703–2715. 10.1007/s12671-019-01225-4 [DOI] [Google Scholar]
- Thabane, L. , Ma, J. , Chu, R. , Cheng, J. , Ismaila, A. , Rios, L. P. , Goldsmith, C. H. , Robson, R. , Thabane, M. , Giangregorio, L. , & Goldsmith, C. H. (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10(1), 1. 10.1186/1471-2288-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tihanyi, B. T. , Boor, P. , Emanuelsen, L. , & Koteles, F. (2016). Mediators between yoga practice and psychological well‐being: mindfulness, body awareness and satisfaction with body image. European Journal of Mental Health, 11(1‐2), 1121–1127. [Google Scholar]
- Uebelacker, L. A. , & Broughton, M. K. (2016). Yoga for depression and anxiety: A review of published research and implications for healthcare providers. Rhode Island Medical Journal, 99(3), 20–22. [PubMed] [Google Scholar]
- Uebelacker, L. A. , Epstein‐Lubow, G. , Gaudiano, B. A. , Tremont, G. , Battle, C. L. , & Miller, I. W. (2010). Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. Journal of Psychiatric Practice, 16(1), 22–33. 10.1097/01.pra.0000367775.88388.96 [DOI] [PubMed] [Google Scholar]
- Unützer, J. , Klap, R. , Sturm, R. , Young, A. S. , Marmon, T. , Shatkin, J. , & Wells, K. B. (2000). Mental disorders and the use of alternative medicine: Tesults from a national survey. American Journal of Psychiatry, 157(11), 1851–1857. 10.1176/appi.ajp.157.11.1851 [DOI] [PubMed] [Google Scholar]
- Valente, V. G. , & Marotta, A. (2011). Prescribing yoga to supplement and support psychotherapy, Spiritually Oriented Interventions for Counseling and Psychotherapy (pp. 251–276). American Psychological Association. [Google Scholar]
- Veritas Health Innovation . (2021). Covidence systematic review software. Melbourne, Australia. www.covidence.org
- Vorkapic, C. F. , & Rangé, B. (2014). Reducing the symptomatology of panic disorder: The effects of a yoga program alone and in combination with cognitive‐behavioral therapy. Frontiers in Psychiatry, 5, 177. 10.3389/fpsyt.2014.00177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, P. S. , Aguilar‐Gaxiola, S. , Alonso, J. , Angermeyer, M. C. , Borges, G. , Bromet, E. J. , Wells, J. E. , Bruffaerts, R. , de Girolamo, G. , de Graaf, R. , Gureje, O. , Haro, J. M. , Karam, E. G. , Kessler, R. C. , Kovess, V. , Lane, M. C. , Lee, S. , Levinson, D. , Ono, Y. , … Wells, J. E. (2007). Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. The Lancet, 370(9590), 841–850. 10.1016/s0140-6736(07)61414-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware, C. J. (2007). Yoga and psychotherapy. Yoga Therapy in Practice, 3(2), 15–17. [Google Scholar]
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. , Marx, B. , & Schnurr, P. (2013). The PTSD checklist for DSM‐5 (PCL‐5). www.ptsd.va.gov
- Weintraub, A. (2012). Yoga skills for therapists: Basic yoga principles & preparations. Somatics, 16(4), 26–31. [Google Scholar]
- West, J. , Liang, B. , & Spinazzola, J. (2017). Trauma sensitive yoga as a complementary treatment for posttraumatic stress disorder: A qualitative descriptive analysis. International Journal Of Stress Management, 24(2), 173–195. 10.1037/str0000040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, R. C. , Biggs, J. T. , Ziegler, V. E. , & Meyer, D. A. (1978). A rating scale for mania: Reliability, validity and sensitivity. The British Journal of Psychiatry, 133(5), 429–435. [DOI] [PubMed] [Google Scholar]
- Zalta, A. K. , Held, P. , Smith, D. L. , Klassen, B. J. , Lofgreen, A. M. , Normand, P. S. , Karnik, N. S. , Brennan, M. B. , Rydberg, T. S. , Boley, R. A. , Pollack, M. H. , & Karnik, N. S. (2018). Evaluating patterns and predictors of symptom change during a three‐week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18(1), 242. 10.1186/s12888-018-1816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zepeda Méndez, M. , Nijdam, M. J. , ter Heide, F. J. J. , van der Aa, N. , & Olff, M. (2018). A five‐day inpatient EMDR treatment programme for PTSD: Pilot study. European Journal of Psychotraumatology, 9(1), 1425575. 10.1080/20008198.2018.1425575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoogman, S. , Goldberg, S. B. , Vousoura, E. , Diamond, M. C. , & Miller, L. (2019). Effect of yoga‐based interventions for anxiety symptoms: A meta‐analysis of randomized controlled trials. Spirituality in Clinical Practice, 6, 256–278. 10.1037/scp0000202 [DOI] [Google Scholar]
- Zuehlke, J. B. (2008). Traditional and non‐traditional techniques for women with postpartum depression: An integrative group treatment manual. (69). ProQuest Information & Learning. EBSCOhost psyh database.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


