Abstract
Purpose of Review
In 2019, vaccine hesitancy (VH) was named as one of the top 10 threats to global health by the World Health Organization (WHO). We highlight the factors affecting VH, the role of VH in limiting vaccine uptake and inability to achieve collective immunity, and possible solutions.
Recent Findings
There are still uncertainties and concerns about the safety and efficacy of vaccines, which promote VH and undermine public confidence in immunization. WHO has designed the behavioral and social drivers (BeSD) tools and survey instruments that can be used by countries to assess reasons for poor vaccine uptake in childhood for COVID-19 and plan national vaccination programs to counter these misconceptions.
Summary
Vaccines are one of the best preventative measures that public health care has to offer. Evidence from across the world both in high-income countries (HICs) and low/middle-income countries (LMICs) show that VH is a significant phenomenon which is translating into geographical clustering of epidemics. A reasonably high acceptance and coverage rates are necessary for an immunization program to be successful. A context-specific and multifactorial intervention with more high-quality research is needed globally.
Keywords: Vaccine hesitancy measurement, Behavioral and social drivers, Multicomponent interventions, Health literacy, Motivational interviewing, Vaccine uptake
Introduction
With the advent of social media and the internet, vaccine hesitancy (VH) seems to be a new phenomenon. However, VH has existed since the first vaccine was administered over 200 years ago. Despite the undisputed scientific understanding that vaccines are beneficial to public health, there is no similar consensus when it comes to making individual choices. Many studies have shown that a significant number of parents and sometimes even healthcare professionals are uncertain and apprehensive about getting certain vaccines. The WHO SAGE Working Group on Vaccine Hesitancy describes hesitancy on a continuum between full acceptance and outright refusal and recognizes that VH can be to single or multiple vaccines [1].
These reservations and concerns can cause one or more recommended vaccinations to be missed or delayed. In both high-income countries (HICs) and low/middle-income countries (LMICs), there is a growing concern that vaccination campaigns are going through tough times. “Vaccine hesitancy (VH),” a term increasingly being used in vaccination discourse, is partly responsible for this.
The publication of a significant number of research articles analyzing the factors influencing vaccine acceptance and hesitancy around the world demonstrates the growing interest in the topic of VH. Numerous literature reviews describing specific aspects of this diverse and multifaceted problem have been published over the past decade and increasingly over the past 2 years.
What is Vaccine Hesitancy?
Vaccine hesitancy (VH) refers to delay in acceptance or refusal of vaccination despite availability of vaccination services. VH is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence (The “3 C’s” model) [2].
Vaccination confidence is defined as trust in (a) the effectiveness and safety of vaccines; (b) the system that delivers them, including the reliability and competence of the health services and health professionals; and (c) the motivations of policy-makers who decide on the needed vaccines.
Vaccination complacency exists where perceived risks of vaccine-preventable diseases are low and vaccination is not deemed a necessary preventive action. Complacency about a particular vaccine or about vaccination in general is influenced by many factors, including other life/health responsibilities that may be seen to be more important at that point in time. Immunization program success may, paradoxically, result in complacency and, ultimately, hesitancy, as individuals weigh risks of vaccination against risks of the disease the vaccine prevents that is no longer common. Self-efficacy (the self-perceived or real ability of an individual to take action to be vaccinated) also influences the degree to which complacency determines hesitancy.
-
Vaccination convenience is a significant factor when physical availability, affordability and willingness-to-pay, geographical accessibility, ability to understand (language and health literacy), and appeal of immunization services affect uptake. The quality of the service (real and/or perceived) and the degree to which vaccination services are delivered at a time and place and in a cultural context that is convenient and comfortable also affect the decision to be vaccinated and could lead to VH.
In the current scenario of COVID-19, the authors would like to bring to the attention of readers additional two C’s [3].
Vaccination communication: Repeated risk communication is crucial to facilitate informed decision-making regarding VH. It is important to let the families and friends know the importance of greater societal benefits of population-level immunity and the protection it offers to those who are vulnerable.
Vaccination context: The communication needs to take into account the recognition of context, including ethnicity, religion, occupation, and socioeconomic status.
While high levels of VH lead to low vaccine demand, low levels of VH do not necessarily mean high vaccine demand.
The Vaccine Hesitancy Determinants Matrix displays the factors influencing the behavioral decision to accept, delay, or reject some or all vaccines under three categories: contextual, individual and group, and vaccine/vaccination-specific influences [2] as described in Table 1.
Table 1.
The Vaccine Hesitancy Determinants Matrix
|
Contextual influences: Influences arising due to historic, socio-cultural, environmental, health system/institutional, economic, or political factors |
• Communication and media environment • Influential leaders, immunization program gatekeepers, and anti- or pro-vaccination lobbies • Historical influences • Religion/culture/gender/socio-economic • Politics/policies • Geographic barriers • Perception of the pharmaceutical industry |
|
Individual and group influences: Influences arising from personal perception of the vaccine or influences of the social/peer environment |
• Personal, family, and/or community members’ experience with vaccination, including pain • Beliefs, attitudes about health and prevention • Knowledge/awareness • Health system and providers—trust and personal experience • Risk/benefit (perceived, heuristic) • Immunization as a social norm vs. not needed/harmful |
|
Vaccine/vaccination-specific issues Directly related to vaccine or vaccination |
• Risk/benefit (epidemiological and scientific evidence) • Introduction of a new vaccine or new formulation or a new recommendation for an existing vaccine • Mode of administration • Design of vaccination program/mode of delivery (e.g., routine program or mass vaccination campaign) • Reliability and/or source of supply of vaccine and/or vaccination equipment • Vaccination schedule • Costs • The strength of the recommendation and/or knowledge base and/or attitude of healthcare professionals |
How Do We Assess Vaccine Hesitancy?
Given that VH is specific to sub-groups within populations and is rarely population-wide, it is important to first understand WHO? is hesitant about vaccination, WHAT? their concerns are—i.e., which of the various possible reasons outlined above are driving their hesitancy, and WHERE? the hesitant individuals are located, i.e., in which geographic, socio-cultural, or political context that may be contributing to the hesitancy. Not all vaccine hesitancy is specific to a vaccine or vaccination, and some influences are well beyond the scope of an immunization program; however, they must be understood in order to know how to best minimize the hesitancy [4].
Ways of Measuring VH
- Pre-designed, validated population surveys using categorized questionnaires—Box 1Box 1 QuestionnairesImmunization behavior(a) Have you ever delayed having your child get a shot for reasons other than illness or allergy? Have you ever decided not to have your child get a shot for reasons other than illness or allergy?(b) How sure are you that following the recommended shot schedule is a good idea for your child? Do you agree with the following statement?(c) It is my role as a parent to question shots(d) If you had another infant today, would you want him/her to get all the recommended shots? Overall, how hesitant about childhood shots would you consider yourself to be?Beliefs about vaccine safety and efficacy(a) Do you agree with the following beliefs about vaccine safety and efficacy?• Children get more shots than are good for them• Many of the illnesses that shots prevent are severe• It is better for my child to develop immunity by getting sick than by getting a shot• It is better for children to get fewer vaccines at the same time(b) How concerned are you that your child might have a serious side effect from a shot?(c) How concerned are you that any one of the childhood shots might not be safe?(d) How concerned are you that a shot might not prevent the disease?(e) Do you know of anyone who has had a bad reaction to a shot?General attitudes and trust(a) Which of the following statements reflect your general attitude and trust toward vaccines?• The only reason I have my child get shots is so that they can enter day-care or school• I trust the information I receive about shots• I am able to openly discuss my concerns about shots with my child’s doctor(b) All things considered, how much do you trust your child’s doctor?
VH Index calculation
This study [5•], seminal and ground-breaking in its breadth and depth, was done to understand and explore the reasons why VH exists. They used VH Index as a method to quantitatively assess the degree of VH.
This index was used to amalgamate critical data points related to opinion and country data on vaccination levels. This allows stakeholders to establish a baseline and track movements in public opinion, or country data, from a perfect 1 to an imperfect 10.
The index combines:
The percentage of unvaccinated persons (national data)
The percentage of persons surveyed who are eligible but are unvaccinated (survey data)
The percentage of unvaccinated persons who answered negatively to the question: “I would be persuaded to change my mind IF I were given more scientific or medical information”
These averages are multiplied by 10 to generate an index on a scale ranging from 1 to 10 with 1, as suggested, being the least hesitant and 10 being the most hesitant.
In another study [6], three main areas of interest related to VH were surveyed: (1) the participants’ experience with COVID-19 and the impact of the pandemic on their lives and activities, (2) attitudes regarding preventive health behaviors and routine immunizations, and (3) attitudes and intentions relating to COVID-19 vaccines. Where a respondent was hesitant to take the COVID-19 vaccination, a question followed: Could anything change their minds and encourage them to become vaccinated? This was mainly to assess what respondents expected from the administrators. Importantly, the survey also sought the views of respondents concerning the vaccination of their children.
A study conducted at Byramjee Jeejeebhoy Government Medical College, Pune by Dr. Kinikar et al. between 1st July and 31st October 2021 at a tertiary care referral hospital postnatal ward among 250 lactating mothers showed COVID-19 vaccine acceptance rate to be very low (8%), in view of potential safety concern and long-term negative effects on the breastfeeding child (52%). After addressing their concerns about the same, nearly 78% lactating mothers accepted the vaccination. This small yet unpublished data reveals that there is a need to create awareness among lactating mothers about positive effects and safety of COVID-19 vaccinations.
Global Magnitude of Vaccine Hesitancy
A worldwide gain in vaccination coverage is threatened by growing VH. Although the vaccination coverage globally has increased significantly since the 1980s, the immunization coverage for tuberculosis, diphtheria, tetanus, pertussis, measles, and polio vaccines has relatively declined since 2012 [7].
Many studies over the last decade in the HICs and LMICs on VH have shown inconsistent yet insightful results. In 2018, a survey conducted by the Wellcome Global Monitor in 140,000 individuals in 140 countries regarding public attitudes to health and science showed that more than 90% of participants in South Asia and East Africa had an opinion that vaccinations were useful and effective. Similarly, more than 92% of people in South Asia and East Africa perceived vaccines as safe. In comparison with Western Europe, only 59% of participants believed vaccines to be safe. According to this study, in general, vaccinations were relatively well accepted in LMICs [8•]. A study conducted in 2019 using the WHO SAGE Vaccine Hesitancy Scale in LMICs (from Bangladesh, China, Ethiopia, Guatemala, and India) found that, even among the pro-vaccine population, more than 50% agreed or were neutral to the question—whether the new vaccine was riskier than the old one [9]. Studies from HICs suggest that it is more naturally acceptable for individuals to be willing to take more risks against new infant vaccines when the direct benefits are greater, but this may not be the case for children with respect to COVID-19 vaccines [10].
With respect to the COVID-19 vaccine acceptance, a study across 15 survey samples covering 10 LMICs, Russia (an upper-middle-income country), and the USA (HIC), which included 44,260 individuals, showed considerably higher willingness to take a COVID-19 vaccine in LMICs compared with the USA and Russia [11]. Another recent scoping review exploring VH in HICs among the four continents showed that Asia had the highest proportion of studies with vaccine hesitancy of 30% or more (72.7%) while North America ranked second (59.5%). Studies conducted in Europe and Oceania had a lower proportion of studies with VH of 30% or more. Individually, VH rates were highest in UAE (77.9%), USA (66.8%), Hong Kong (60%), and Italy (59.9%). In contrast, the VH rates were lowest in Canada (7%) and Saudi Arabia (7%) [12].
It is important to also note that in the current ongoing pandemic of COVID-19, major disparities in vaccine access between HICs and LMICs have further contributed to vaccine hesitancy. In 2021, WHO set the target for 70% global vaccination coverage by mid-2022. As of June 2022, only 58 of WHO’s 194 Member States had reached the 70% target and in low-income countries; just 37% of healthcare workers had received a complete course of primary vaccination [13•].
Is Vaccine Hesitancy a Recent Phenomenon?
Vaccine hesitancy is a complicated and multi-faceted phenomenon that dates back to the first vaccinations performed by Dr. Zabdiel Boylston (1721) and Edward Jenner (1796–1798) as shown in Fig. 1. It is a highly heterogeneous and dynamic phenomenon; it is also highly unpredictable and is attitude and vaccine specific [14].
Fig. 1.
In this cartoon, the British satirist James Gillray caricatured a scene at the Smallpox and Inoculation Hospital at St. Pancras, showing cowpox vaccine being administered to frightened young women, and cows emerging from different parts of people’s bodies (source: https://en.wikipedia.org/wiki/File:The_cow_pock.jpg)
Although the term “personal belief exemption” was first popularized in the 1990s, the idea of waiving vaccination based on worldly beliefs dates back to the late nineteenth century. Smallpox led to the earliest vaccination regulations, and in the late nineteenth century this promoted personal belief exemption. Since then, the exemption has evolved in several stages, each triggered by a new vaccine or immunization law [15]. At every stage, the exemptions were utilized for political mileage, placating or securing the support of opposition parties [16, 17].
In 1998, Andrew Wakefield, a British physician, infamously claimed that the Measles, Mumps, and Rubella (MMR) vaccine caused inflammatory bowel disease and autism. He proposed that the live attenuated measles vaccine caused toxic, autism-causing chemicals in the intestines that reach the brain and cause the disease. The publication was promptly retracted by the journal after swift criticism of the work. He was finally proved to be a liar and a fraud, who had been funded by lawyers who were working with the parents of the children in the study to try to find a reason to sue the vaccine manufacturers. Although more than 20 years of medical literature have shown no link between the development of autism and vaccination, many still believe this myth.
What Is Leading to Vaccine Hesitancy?
The reasons why people in HICs and LMICs choose not to vaccinate are complex and varied in nature; a vaccines advisory group to WHO identified complacency, inconvenience in accessing vaccines, and lack of confidence as key reasons underlying hesitancy [17].
Political populism and VH are both fueled by the same narrative, a deep mistrust in authorities and vaccine experts. It is quite convenient for populists to target the vaccine-hesitant population because they only need to convince a minority of citizens not to be vaccinated to achieve their destabilizing goals. If the minimum herd immunity coverage is not achieved, new outbreaks will emerge, reinforcing a vicious circle of distrust in elites [18•].
VH can be due to various other factors like lack of knowledge, false religious beliefs, or anti-vaccine misinformation. Beliefs regarding the benefit and effectiveness of vaccines, wariness of the motives behind, the influence of family especially parents’ attitude, and conversation with friends on vaccination decisions also influence the vaccine acceptance and hesitancy. Fear of needles and pain after vaccine injection especially in children is also documented as one of the greatest opponents of vaccination [19–21]. An interesting finding was noted among physicians in Switzerland. Those interested in immunization, a significant proportion of non-pediatricians, had the fear of “immune overload” and declined or delayed the immunization of their own children with the recommended MMR- or DTP-based combination vaccines [22].
For the past three decades, social media usage has increased exponentially, leading to misinformation to have a free run via mostly unregulated social media sites. During pandemics/outbreaks, a plethora of information from many sources, including social media, has led to what is now called an “infodemic.” An infodemic is created by a vast amount of correct and misinformation from experts and the general public. Many times, it becomes difficult for social media users to distinguish between correct and misinformation. Social media users are more likely to be swayed by unscientific/pseudoscientific “influencers” more than verified scientific expert information [23–26].
During the current COVID-19 pandemic, many studies suggest that young, non-white females with lower education status were more vaccine hesitant. A belief that COVID-19 was not serious, a lack of recent flu vaccination history, a lower self-perceived risk of COVID-19, no chronic illness, and false concerns about fast development of COVID-19 vaccines were associated with increased VH [27, 28••, 29].
How To Tackle Vaccine Hesitancy?
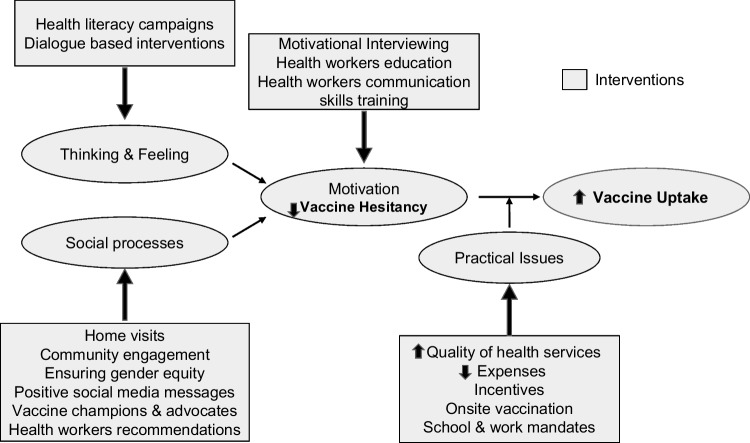
Multicomponent, tailor-made, and contextually specific interventions are needed to tackle the growing problem of VH. “One size fits all” approach does not work in dealing with VH. For example, in LMICs, interventions to improve health literacy in the population are important while in HICs, building trust in healthcare messaging and professionals is vital. The interventions need to be planned at various levels—individual, family, community, technology, healthcare worker, and governmental (Fig. 2).
Fig. 2.
Domain specific interventions to increase vaccine uptake
According to the recently published WHO position paper on “understanding the behavioral and social drivers (BeSD) of vaccine uptake,” VH is defined as a motivational state of being conflicted about, or opposed to, getting vaccinated; this includes intentions and willingness [30••]. BeSD are beliefs and experiences specific to vaccination that are potentially modifiable to increase vaccine uptake. These include four interrelated domains of thinking and feeling, social process, motivation, and practical issues. VH is under the motivation domain. WHO has designed BeSD tools and survey instruments that can be used by countries to assess reasons for poor vaccine uptake in childhood and for COVID-19 and plan national vaccination programs to counter these. Domain-specific interventions are elucidated below (Fig. 2).
Thinking and feeling include cognitive and emotional responses to vaccines.
It is essential to build vaccine confidence in the population to improve its uptake. People should believe that vaccines are effective, safe, and part of a trustworthy medical system. According to the health belief model (HBM), vaccine confidence is influenced by perceived susceptibility and severity of a disease, perceived benefits and barriers to vaccination, cues (like social media messages and recommendations by family members and healthcare workers), and self-efficacy [31]. For COVID-19 vaccines, health messaging that decrease perceived risks and highlight benefits were effective in overcoming vaccine hesitancy [31]; HBM modifiers including education, age, geographical locations, occupation, income, employment, marital status, race, and ethnicity have inconsistent effects on VH.
Depending on individual and contextual factors, parents of children who require vaccinations lie on a spectrum of VH from total acceptance of all childhood vaccines to acceptance of a few to cautious consideration to total rejection. Healthcare providers should understand these factors, empathize, and use non-confrontational motivational interviewing techniques along with other interventions to overcome parental VH [32••].
Migrants and few faith-based and religious communities need special interventions to counter existing VH. These population groups usually face marginalization, discrimination, have rigid anti-vaccine sentiments, and mistrust the government mandates. Improving access to inclusive and quality health services for minorities and marginalized population along with dialogue-based interventions are known to enhance vaccine uptake [33].
-
2.
Social processes include societal norms regarding vaccination and receiving recommendations from healthcare workers. Home visits by healthcare workers and parental engagement community programs are found to be effective in improving knowledge and dispelling doubts regarding vaccination and ensuring gender equity [34, 35•]. Imparting technology-based health literacy through videos, posters, and lectures was found to be beneficial in building vaccine confidence for DPT, MMR, Hemophilus influenza B (Hib), and pneumococcal vaccines [34]. Experience sharing and health education sessions by prominent community and religious leaders in person or through digital media like TV and radio also encourage vaccine uptake.
Parents usually trust their healthcare providers (HCPs) and they strongly influence their decisions regarding vaccination for their children. A strong science-based recommendation delivered in a safe congenial medical setting with an open and flexible attitude can convert nearly 30% of VH parents to vaccine compliant ones [35•]. All queries raised by the parents should be answered by HCP patiently while respecting the family beliefs and norms. In a recent review regarding HPV vaccine, it was stated that HCP can improve vaccine uptake in adolescents by overcoming their own VH through education and by acquiring skills for effective communication and by providing supportive information resources [36].
-
3.
Motivation includes people’s intention, willingness, and hesitancy to get vaccinated. Interventions in domains of thinking and feeling and social processes that decrease VH have been described in the preceding paragraphs. In addition, mistrust regarding introduction of new vaccines without adequate trials under emergency authorization for profit-based incentives of pharmaceutical companies also need to be addressed by HCP [30••]. To motivate individuals and parents from pre-contemplation to action and vaccine acceptance, it is essential to understand their perceptions, cultural and religious beliefs, world views, and moral values [33, 37]. Using the technique of motivational interviewing with respect and empathy, validating emotions, providing concise information highlighting the benefits of vaccines, and by addressing concerns, individuals and parents can be helped to overcome VH.
-
4.
Practical issues include challenges that individuals experience in getting vaccinated like availability, accessibility, affordability, and quality of health services [37]. Improved quality of health services, free vaccines, government mandates, cash incentives, reminder recall SMS services, and workplace and health worker vaccination increase vaccine acceptance [32••, 38].
Vaccine Hesitancy and Moral Values
According to the moral foundations theory, six moral values influence people’s thinking and behavior, namely, care, fairness, loyalty, authority, sanctity, and liberty. People who disregard authority, personal and societal well-being, and endorse liberty and sanctity/purity are vaccine hesitant [39]. Parents who are hesitant to vaccinate their children also give importance to liberty and purity [40]. Understanding the value system of individuals and community groups helps in planning appropriate patient-centered and public health interventions and messaging to enhance vaccine uptake [39, 40].
Conclusion
The post-pandemic world is more challenging and requires more public health efforts to return to previous levels of public confidence in vaccination programs. Vaccine hesitancy is a significant, living phenomenon that is translating into geographical clustering of epidemics in both HICs and LMICs and requires attention on both the micro- and macro-levels to be addressed successfully. Trust at various system levels appears to be important in modifying vaccine hesitancy. Acceptance and coverage rates must be substantial for a mass vaccination program to be successful. When planning and developing future strategies on widespread vaccination and public health messages, healthcare administrators must keep these new and emerging factors that contribute to VH in mind. The future research should focus on creating a Multidimensional Vaccine Hesitancy Scale for a multifactorial approach that can address these challenges.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
This article is part of the Topical Collection on Technology and Pediatrics.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Appendices to the report of the sage working group. Retrieved October 5, 2022, from https://cdn.who.int/media/docs/default-source/immunization/sage/2014/october/2-sage-appendicies-background-final.pdf?sfvrsn=2259f1bf_4
- 2.MacDonald NE, SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 3.Razai MS, Oakeshott P, Esmail A, Wiysonge CS, Viswanath K, Mills MC. COVID-19 vaccine hesitancy: the five Cs to tackle behavioural and sociodemographic factors. J R Soc Med. 2021;114(6):295–298. doi: 10.1177/01410768211018951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: The development of a survey tool. Vaccine. 2015;33(34):4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 5.• COVID-19 Vaccine Hesitancy Survey Report 2021. Retrieved October 5, 2022, from https://www.unicef.org/easterncaribbean/media/3006/file/COVID%20vaccine%20hesitancy%20rep%20-%20T%22T.pdf. An elegant survey on the topic.
- 6.Middleman AB, Klein J, Quinn J. Vaccine hesitancy in the time of COVID-19: attitudes and intentions of teens and parents regarding the COVID-19 vaccine. Vaccines (Basel) 2021;10(1):4. doi: 10.3390/vaccines10010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organisation. (2021, September 15). Global covid-19 vaccination strategic vision for 2022. SAGE meeting October 2021. Retrieved October 6, 2022, from https://cdn.who.int/media/docs/default-source/immunization/sage/covid/global-covid-19-vaccination-strategic-vision-for-2022_sage-yellow-book.pdf
- 8.• Wellcome-global-monitor-2018.pdf. Retrieved October 5, 2022, from https://cms.wellcome.org/sites/default/files/wellcome-global-monitor-2018.pdf. An elegant report on the topic.
- 9.Wagner AL, Masters NB, Domek GJ, et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines (Basel) 2019;7(4):155. doi: 10.3390/vaccines7040155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakhache P, Rodrigo C, Davie S, et al. Health care providers' and parents' attitudes toward administration of new infant vaccines—a multinational survey. Eur J Pediatr. 2013;172(4):485–492. doi: 10.1007/s00431-012-1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Solís Arce JS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aw J, Seng JJB, Seah SSY, Low LL. COVID-19 vaccine hesitancy–a scoping review of literature in high-income countries. Vaccines (Basel) 2021;9(8):900. doi: 10.3390/vaccines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.• Vaccine equity. Retrieved October 5, 2022, from https://www.who.int/campaigns/vaccine-equity. An elegant report on the topic.
- 14.Shrivastava SR, Shrivastava PS, Ramasamy J. The growing global problem of vaccine hesitancy: time to take action. Int J Prev Med 2016;7:18. 10.4103/2008-7802.173924. [DOI] [PMC free article] [PubMed]
- 15.Conis E. The history of the personal belief exemption. Pediatrics. 2020;145(4):e20192551. doi: 10.1542/peds.2019-2551. [DOI] [PubMed] [Google Scholar]
- 16.Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines. 2015;14(1):99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 17.Ten threats to global health in 2019. Retrieved October 5, 2022, from https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- 18.Recio-Román A, Recio-Menéndez M, Román-González MV. Political populism, institutional distrust and vaccination uptake: a mediation analysis. Int J Environ Res Public Health. 2022;19(6):3265. doi: 10.3390/ijerph19063265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Machingaidze S, Wiysonge CS. Understanding COVID-19 vaccine hesitancy. Nat Med. 2021;27(8):1338–1339. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- 20.Bullock J, Lane JE, Shults FL. What causes COVID-19 vaccine hesitancy? Ignorance and the lack of bliss in the United Kingdom. Humanit Soc Sci Commun. 2022;9:87. doi: 10.1057/s41599-022-01092-w. [DOI] [Google Scholar]
- 21.21. Larson H, Mnookin S. Chapter 27 - Trust and Confidence in Vaccines: Tales of Three Vaccines, Lessons for Others. In Lambert P-H, Bloom B, editors. The vaccine book. 2nd edn. Academic Press; 2016. p. 529–540
- 22.Posfay-Barbe KM, Heininger U, Aebi C, Desgrandchamps D, Vaudaux B, Siegrist CA. How do physicians immunize their own children? Differ pediatr nonpediatricians Pediatr. 2005;116(5):e623–e633. doi: 10.1542/peds.2005-0885. [DOI] [PubMed] [Google Scholar]
- 23.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark SE, Bledsoe MC, Harrison CJ. The role of social media in promoting vaccine hesitancy. Curr Opin Pediatr. 2022;34(2):156–162. doi: 10.1097/MOP.0000000000001111. [DOI] [PubMed] [Google Scholar]
- 25.Misinformation on social media is linked to vaccine hesitancy, says study | Gavi, the Vaccine Alliance. [cited 30 September 2022]. Retrieved October 5, 2022, from https://www.gavi.org/vaccineswork/misinformation-social-media-linked-vaccine-hesitancy-says-study
- 26.Mascherini M, Nivakoski S. Social media use and vaccine hesitancy in the European Union. Vaccine. 2022;40(14):2215–2225. doi: 10.1016/j.vaccine.2022.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazarus JV, Wyka K, White TM, et al. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. 2022;13(1):3801. doi: 10.1038/s41467-022-31441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sallam M. COVID-19 Vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klein JK, Middleman AB, Quinn JR. COVID-19 impact on parent/young adult attitudes and beliefs toward vaccines for adolescents and young adults. J Adolesc Health. 2021;68:S6. doi: 10.1016/j.jadohealth.2020.12.017. [DOI] [Google Scholar]
- 30.•• Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022. (2022, May 20). Retrieved October 5, 2022, from. https://www.who.int/publications/i/item/who-wer9720-209-224. A very relevant and useful position paper on the topic.
- 31.Limbu YB, Gautam RK, Pham L. The health belief model applied to COVID-19 vaccine hesitancy: a systematic review. Vaccines (Basel) 2022;10(6):973. doi: 10.3390/vaccines10060973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lafnitzegger A, Gaviria-Agudelo C. Vaccine hesitancy in pediatrics. Adv Pediatr. 2022;69(1):163–176. doi: 10.1016/j.yapd.2022.03.011. [DOI] [PubMed] [Google Scholar]
- 33.Tankwanchi AS, Bowman B, Garrison M, Larson H, Wiysonge CS. Vaccine hesitancy in migrant communities: a rapid review of latest evidence. Curr Opin Immunol. 2021;71:62–68. doi: 10.1016/j.coi.2021.05.009. [DOI] [PubMed] [Google Scholar]
- 34.Singh P, Dhalaria P, Kashyap S, et al. Strategies to overcome vaccine hesitancy: a systematic review. Syst Rev. 2022;11(1):78. doi: 10.1186/s13643-022-01941-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shapiro GK, Kaufman J, Brewer NT, et al. A critical review of measures of childhood vaccine confidence. Curr Opin Immunol. 2021;71:34–45. doi: 10.1016/j.coi.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Efua Sackey M, Markey K, Grealish A. Healthcare professional's promotional strategies in improving human papillomavirus (HPV) vaccination uptake in adolescents: a systematic review. Vaccine. 2022;40(19):2656–2666. doi: 10.1016/j.vaccine.2022.03.054. [DOI] [PubMed] [Google Scholar]
- 37.June 8, 2021 human centered recommendations for increasing vaccine uptake. (n.d.). Retrieved October 5, 2022, from https://www.aha.org/system/files/media/file/2021/06/Human-Centered-Recommendations-For-Increasing-Vaccine-Uptake.pdf
- 38.Perroud JM, Soldano S, Avanceña ALV, Wagner A. Adult vaccination uptake strategies in low- and middle-income countries: a systematic review. Vaccine. 2022;40(36):5313–5321. doi: 10.1016/j.vaccine.2022.07.054. [DOI] [PubMed] [Google Scholar]
- 39.Schmidtke KA, Kudrna L, Noufaily A, et al. Evaluating the relationship between moral values and vaccine hesitancy in Great Britain during the COVID-19 pandemic: a cross-sectional survey. Soc Sci Med. 2022;308:115218. doi: 10.1016/j.socscimed.2022.115218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amin AB, Bednarczyk RA, Ray CE, et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1(12):873–880. doi: 10.1038/s41562-017-0256-5. [DOI] [PubMed] [Google Scholar]