Abstract
Background and objective
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), has affected all regions, demographics, and age groups worldwide. However, few studies have investigated the prevalence of childhood obesity and severe COVID-19 presentation in a predominately Hispanic population. In light of this, we investigated the role of underlying obesity in COVID-19 presentations and outcomes at a tertiary care children’s hospital by using subcategories based on patients' body mass index (BMI).
Methods
We conducted a single-center retrospective study involving 77 pediatric patients aged 18 years and younger, who were hospitalized with suspected or verified COVID-19 between February 2020 and January 2021. We collected data on height, weight, and BMI and categorized patients based on the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) definition(s) of obesity. We also collected data on demographics, mode of presentation, need for pediatric intensive care unit (PICU) admission, the severity of illness at the time of PICU admission, and data related to outcomes. We analyzed the data using logistical regression with Firth’s biased reduction method wherever applicable.
Results
In our cohort, over 85% of the patients identified as belonging to Hispanic ethnicity (n=66); the median age of the cohort was 8.69 years, and 50.65% were classified as obese (n=39). We found a statistically significant relationship between underlying obesity and one or more comorbidities (p<0.001). BMI classification was significantly dependent on the incidence of multisystem inflammatory syndrome in children (MIS-C) (p=0.0353). Furthermore, the bivariate analysis confirmed that acute kidney injury (AKI) (p=0.048) and MIS-C predictors (p<0.001) were significantly associated with PICU admission status. The combined model confirmed a significant relationship between MIS-C and both PICU admission status (p<0.001) and obese BMI classification (p=0.002). PICU admission status led to increased hospital length of stay (LOS) (p<0.001). Patient age (p=0.003), underweight BMI (p=0.034), and obese BMI (P=0.008) were significant predictors of PICU LOS. Of note, the survival rate among admitted COVID-19 patients was 93.5%.
Conclusion
Based on our findings on the prevalence of underlying obesity in admitted COVID-19 patients at the Children’s Hospital of San Antonio, over 50% of pediatric patients were obese and predominately Hispanic. Obesity was significantly associated with patient age, comorbidities, MIS-C status, and PICU LOS. Hospital mortality in pediatric COVID-19 patients was low (6.49%) and consistent with other studies in the literature showing lower rates of mortality in children versus mortality in adult patients with COVID-19.
Keywords: outcomes, body mass index, obesity, sars-cov-2, covid-19, children
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has cost countless lives globally, affecting all regions, demographics, and age groups. Over the past year, clinical research has been paramount in identifying significant risk factors, important clinical presentation features, and potential therapeutic modalities to combat severe COVID-19 infection.
In adults, obesity is associated with immune dysfunction with increased SARS-CoV-2 viral load/shedding, leading to symptom severity [1]. As SARS-CoV-2 penetrates angiotensin-converting enzyme 2 (ACE2) receptors more copiously in adipose tissue (compared to lungs or respiratory tract), obese patients are predisposed to more severe illness [2]. Along with acute respiratory distress and hypoxia, obese COVID-19 adults are predisposed to systemic inflammation and a higher risk of thrombotic events, including venous thromboembolism [2]. These comorbid factors have led to worsening outcomes in COVID-19 illness including respiratory failure, the need for mechanical ventilation, and higher mortality [2]. In March of 2021, the Centers for Disease Control and Prevention (CDC) released a report comparing body mass index (BMI) classification in adults with characteristics of severe COVID-19 hospital presentation. BMI classifications of overweight and obese in adults were significant risk factors for the need for invasive mechanical ventilation, and obese adults with COVID-19 infection had higher rates of hospitalization, ICU admission, and mortality [3].
In addition to risk factors and comorbidities, ethnic and other minority statuses and low socioeconomic status have played a role in the impact of the COVID-19 pandemic [4]. Hispanics, the largest minority group in the United States, have accounted for 46.4% of the positive cases in Texas as of May 14, 2020 [4]. Hispanic ethnicity has been associated with higher rates of chronic comorbid disease including obesity, more severe COVID-19 infection, and a two-fold higher age-adjusted death rate compared to Whites [4]. Multiple chronic conditions, barriers to accessing healthcare, immigration status and exclusion from Medicaid coverage, language barriers, and financial burden are all significant issues faced by minority populations in the United States [4].
Currently, most data related to COVID-19 infection in children report mild symptoms for the most part [5-7], as derived from case reports, case series, small retrospective reviews, systematic reviews, and meta-analyses [1-11]. Obesity has been recognized as an independent risk factor for critical COVID-19 infection in children [12-14].
Retrospective studies that specifically focus on pediatric obesity and severe COVID-19 infection and outcomes among Hispanics are sparse. Therefore, this study looks to build upon these studies by analyzing presenting factors, illness severity markers, and outcomes in a predominately Hispanic population with a higher prevalence of obesity at a tertiary hospital in Southwest Texas. Due to the high, disproportionate prevalence of obesity among Hispanic children in San Antonio compared to national estimates, our study provides a unique perspective on the health disparities experienced by pediatric patients with underlying obesity within the context of the ongoing COVID-19 pandemic, with a view to improving (1) risk management strategies within intensive care and (2) prognostic value for acute illness presentation of the minority pediatric patients [15].
This article was previously presented as a meeting abstract at the 2022 National PAS Annual Scientific Meeting on April 24, 2022.
Materials and methods
Study design and setting
We conducted a single-center retrospective study involving children aged 18 years and younger who were hospitalized with COVID-19 infection at the Children's Hospital of San Antonio, a tertiary care children’s hospital, between February 2020 and January 2021. We obtained institutional review board approval/exempt status, with a waiver for informed consent. Patients aged >18 years of age or surgical patients with incidental COVID-19 diagnosis were excluded. Data on height, weight, and BMI were collected from the electronic medical records (EMR); the World Health Organization (WHO) and CDC criteria and age-based growth charts were used to classify obesity [16,17]. BMI classification was then used to analyze its role in demographics, comorbidities, presenting factors, illness severity, and hospital outcomes. This methodology has been accepted and used in prior retrospective studies comparing pediatric BMI and pediatric intensive care unit (PICU) outcomes in the context of severe infection [18].
Illness severity
For patients admitted to the PICU, Pediatric Risk of Mortality III (PRISM III) and Pediatric Logistic Organ Dysfunction-2 (PELOD-2) scores were calculated to quantify illness severity. We classified illness severity into mild (PRISM III score <10 or PELOD-2 score ≤5), moderate (PRISM III score 10-19 or PELOD-2 score 6-12), and severe illness (PRISM III score >19 or PELOD-2 score >12) based on Goncalves et al. [19].
Outcome measure
Our primary outcome measure was PICU admission based on BMI classification. Secondary outcomes included the incidence of acute kidney injury (AKI) utilizing the Pediatric Risk, Injury, Failure, Loss, End Stage Renal Disease (pRIFLE) criteria, the incidence of multisystem inflammatory syndrome in children (MIS-C), the need for invasive mechanical ventilation, PICU length of stay (LOS), hospital LOS, and hospital mortality [20,21].
Statistical analysis
Descriptive statistics were used to summarize demographics and clinical presenting factors. We used the Kruskal-Wallis test to analyze the relationships between continuous dependent and categorical independent variables, while Fisher’s exact test was utilized to analyze the relationship between categorical variables [22,23]. The logistic regression model was employed to investigate the bivariate relationships between binary dependent and continuous/categorical independent variables. The significance of age, BMI classification, and other hospital outcomes was also considered based on potential predictive factors of severe illness. Furthermore, our combined model utilized the logistic regression model for multivariate analysis to check the relationships between binary dependent and multiple continuous/categorical independent variables based on these predictors. Our combined model selected the best model using the backward elimination process where variables with p<0.05 were retained. For the bivariate and multivariate analyses, the odds ratios (OR) and their 95% confidence intervals (CI) were calculated. Since the distribution of binary outcomes was unbalanced in our data, we utilized the logistic regression model with Firth’s biased reduction approach for both bivariate and combined models. Imputation and statistical analysis were computed using the R software (The R Foundation for Statistical Computing, Institute for Statistics and Mathematics, Vienna, Austria) [24].
Results
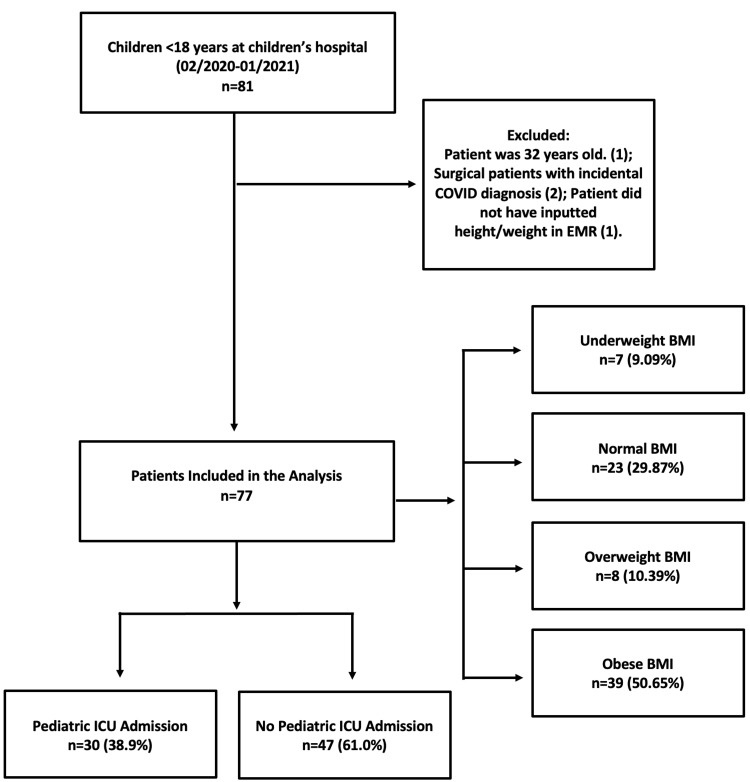
Our sample consisted of 77 pediatric patients (38 males and 39 females) admitted with COVID-19 infection at a tertiary care center (Figure 1).
Figure 1. Consort diagram.
Consort diagram demonstrating the sample size of pediatric COVID-19 patients in the study
BMI: body mass index; COVID-19: coronavirus disease 2019; EMR: electronic medical record
Demographics, comorbidities, and presenting factors
Of note, 50.65% of pediatric patients in our cohort fulfilled the obese BMI classification criteria (n=39), while our normal BMI subsample included 23 patients for reference comparison. Significantly, over 85% of our patient sample identified as belonging to Hispanic ethnicity (n=66), and the prevalence of obesity was 54.5%. All demographic and predisposing factors are detailed in Table 1. There was a significant difference in age distribution among the four BMI categories (p=0.002). Specifically, differences were observed in age distributions of normal BMI compared to overweight patients (p=0.047) and normal BMI compared to obese patients (p=0.016), as displayed in Figure 2. The prevalence of one or more comorbidities within our sample had a significant dependent relationship with BMI status (p=1.34E-15). Further analysis showed a statistically significant difference in association with comorbidities of the following BMI categories: normal, obese BMI (p=1.04E-11); obese, overweight BMI (p=9.54E-09); obese, underweight BMI (p=3.74E-08). Even though Hispanic patients accounted for 85% of our sample, there was no significant relationship between race or ethnicity and BMI classification (Table 1).
Table 1. Demographic information.
Demographics and comorbidities by BMI classification in pediatric COVID-19 patients
BMI: body mass index; COVID-19: coronavirus disease 2019
| Demographics and predisposing factors | ||||||
| Total (n=77) | Underweight (n=7) | Normal BMI (n=23) | Overweight (n=8) | Obese (n=39) | P-value | |
| Mean age (years) | 8.69 | 4.31 | 5.38 | 10.52 | 10.68 | 0.002 |
| Sex | 0.4214 | |||||
| Male | 49.4% (n=38) | 5.3% (n=2) | 36.84% (n=14) | 7.9% (n=3) | 50% (n=19) | |
| Female | 50.65% (n=39) | 12.8% (n=5) | 23.1% (n=9) | 12.82% (n=5) | 51.28% (n=20) | |
| Race | 0.642 | |||||
| White/Caucasian | 68.8% (n=53) | 7.55% (n=4) | 30.19% (n=16) | 7.55% (n=4) | 54.72% (n=29) | |
| Black/African American | 3.90% (n=3) | 67% (n=2) | 33.3% (n=1) | |||
| American Indian/Alaska Native | 2.6% (n=2) | 50% (n=1) | 50% (n=1) | |||
| Other | 24.68% (n=19) | 10.53% (n=2) | 31.58% (n=6) | 15.79% (n=3) | 42.11% (n=8) | |
| Ethnicity | 0.1468 | |||||
| Hispanic | 85.71% (n=66) | 9.09% (n=6) | 24.24% (n=16) | 12.12% (n=8) | 54.55% (n=36) | |
| Non-Hispanic | 14.29% (n=11) | 9.09% (n=1) | 63.64% (n=7) | 27.27% (n=3) | ||
| Comorbidities | <0.0001 | |||||
| One or more | 55.84% (n=43) | 9.30% (n=4) | 90.69% (n=39) | |||
Risk factors for critical illness
There was a high incidence of AKI, MIS-C, and patients requiring PICU admission in our sample (Table 2).
Table 2. Presentation.
Presenting factors and outcomes by BMI classification in pediatric COVID-19 patients
AKI: acute kidney injury; BMI: body mass index; COVID-19: coronavirus disease 2019; MIS-C: multisystem inflammatory syndrome in children; PICU: pediatric intensive care unit
| Presenting factors and outcomes | ||||||
| Total (n=77) | Underweight BMI (n=7) | Normal BMI (n=23) | Overweight BMI (n=8) | Obese BMI (n=39) | P-value | |
| Binomial factors | ||||||
| AKI | 27.27% (n=21) | 14.26% (n=1) | 17.39% (n=4) | 50% (n=4) | 30.77% (n=12) | 0.1955 |
| MIS-C | 14.29% (n=11) | 14.29% (n=1) | 21.74% (n=5) | 37.5% (n=3) | 5.13% (n=2) | 0.0353 |
| PICU admission | 38.96% (n=30) | 28.57% (n=2) | 26.09% (n=6) | 62.50% (n=5) | 43.59% (n=17) | 0.134 |
| Mortality | 6.49% (n=5) | 25% (n=2) | 7.69% (n=3) | 0.0989 | ||
Of the 21 admitted patients who presented with COVID-19 and AKI, 57.14% were classified as obese, and 76.19% were classified as either overweight or obese. Using the pRIFLE criteria, the 21 patients with AKI were further classified as risk (n=6), injury (n=6), and failure (n=9). Of the patients who were classified as having renal failure, all were either overweight or obese. As shown in Table 3, AKI was a significant independent predictor of PICU admission status (p=0.048).
Table 3. Severity of illness.
Risk factors for critical illness in pediatric COVID-19 patients
AKI: acute kidney injury; BMI: body mass index; CI: confidence interval; COVID-19: coronavirus disease 2019; LOS: length of stay; MIS-C: multisystem inflammatory syndrome in children; OR: odds ratio; PICU: pediatric intensive care unit
| Severity of illness factors | |||||
| Bivariate analysis (n=77) | Combined model (n=77) | ||||
| Predictors | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| AKI | |||||
| Age | 1.009 (0.931-1.093) | 0.829 | |||
| Underweight BMI | 1.00 (0.114-8.737) | 1 | |||
| Overweight BMI | 4.33 (0.763-24.614) | 0.081 | |||
| Obese BMI | 1.97 (0.566-6.854) | 0.264 | |||
| PICU admission status | 2.73 (0.984-7.618) | 0.048 | 2.73 (0.984-7.618) | 0.048 | |
| MIS-C | |||||
| Age | 0.997 (0.902-1.102) | 0.953 | |||
| Underweight BMI | 0.776 (0.092-6.548) | 0.802 | 0.299 (0.012-7.26) | 0.425 | |
| Overweight BMI | 2.14 (0.382-11.98) | 0.368 | 0.402 (0.032-5.041) | 0.457 | |
| Obese BMI | 0.224 (0.044-1.134) | 0.054 | 0.046 (0.005-0.452) | 0.002 | |
| AKI | 1.69 (0.456-6.310) | 0.8 | |||
| PICU admission status | 56.02 (3.047-1030.15) | <0.0001 | 126.505 (5.932-2697.925) | <0.0001 | |
| Hospital LOS | 1.021 (0.955-1.092) | 0.484 | |||
| Mechanical vent status (reference is 0 or "No Vent") | 0.486 (0.019-12.341) | 0.2 | |||
| PICU admission status | |||||
| Age | 1.049 (0.974-1.131) | 0.194 | |||
| Underweight BMI | 1.224 (0.194-7.736) | 0.821 | |||
| Overweight BMI | 4.231 (0.778-22.997) | 0.0737 | |||
| Obese BMI | 2.094 (0.686-6.394) | 0.177 | |||
| AKI | 2.738 (0.979-7.661) | 0.048 | |||
| Hospital LOS | 1.436 (1.159-1.780) | <0.0001 | 1.436 (1.159-1.780) | <0.0001 | |
| Mechanical vent status | 2.316 (0.368-14.595) | 0.325 | |||
MIS-C affected 11 patients in our sample. BMI classification and MIS-C status were statistically dependent (p=0.0353), as detailed in Table 3. Furthermore, the bivariate analysis confirmed that MIS-C predictors were significantly associated with PICU admission status (p=5E-06). The combined model confirmed a significant relationship between MIS-C and both PICU admission status (p=4.42E-07) and obese BMI classification (p=0.002). Table 4 provides an analysis of Hispanic ethnicity on risk factors for critical illness, which revealed no significant findings.
Table 4. Ethnicity.
Hispanic ethnicity and risk factors for critical illness in pediatric COVID-19 patients
AKI: acute kidney injury; CI: confidence interval; COVID-19: coronavirus disease 2019; MIS-C: multisystem inflammatory syndrome in children; OR: odds ratio; PICU: pediatric intensive care unit
| Hispanic ethnicity and risk factors for critical illness | ||
| Predictors | OR (95% CI) | P-value |
| Hispanic ethnicity | ||
| AKI (reference is 0 or "No AKI") | 0.554 (0.053-3.048) | 0.7146 |
| MIS-C (reference is 0 or "No MIS-C") | 2.67 (0.379-14.620) | 0.1872 |
| PICU admission status (reference is 0 or "No PICU") | 0.881 (0.171-3.882) | 1 |
Hospital course
Determining factors of hospital course are detailed in Table 5.
Table 5. Risk factors.
Determining factors of hospital course in pediatric COVID-19 patients
*Measured in about 50% of admitted COVID-19 patients. **Includes two patients not admitted to PICU with invasive mechanical ventilation
BMI: body mass index; COVID-19: coronavirus disease 2019; CRP: C-reactive protein; LOS: length of stay; PICU: pediatric intensive care unit
| Determining factors of hospital course | ||||||||
| Total (n=77) | Underweight BMI (n=7) | Normal BMI (n=23) | Overweight BMI (n=8) | Obese BMI (n=39) | P-value | |||
| Continuous factors | ||||||||
| CRP levels (mg/dL)* | 8.56 (n=39) | 4.05 (n=4) | 10.27 (n=12) | 19.32 (n=5) | 5.42 (n=18) | 0.2435 | ||
| Mechanical ventilation** | 6.49% (n=5) | 16.67% (n=1) | 5.88% (n=1) | 0.1727 | ||||
| Hospital LOS (days) | 4.76 (n=77) | 5.4 (n=7) | 2.7 (n=23) | 5.02 (n=8) | 5.8 (n=39) | 0.282 | ||
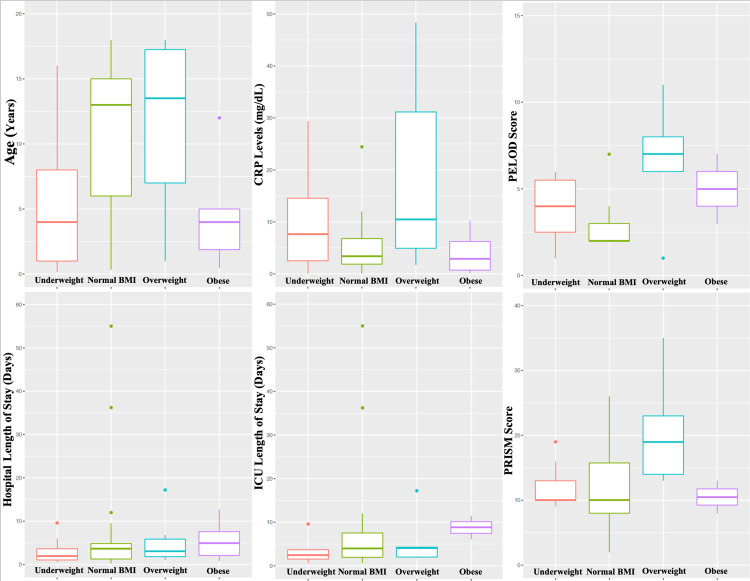
In a subset of patients (n=39), CRP levels were measured at day 0 of hospitalization. No significant differences in CRP levels were observed among the four BMI categories, with their respective distributions shown in Figure 2.
Figure 2. Outcomes.
Age distribution, CRP levels, hospital LOS, PICU LOS, and PELOD-2 and PRISM III scores by BMI classification in pediatric COVID-19 patients
BMI: body mass index; COVID-19: coronavirus disease 2019; CRP: C-reactive protein; LOS: length of stay; PELOD-2: Pediatric Logistic Organ Dysfunction-2; PICU: pediatric intensive care unit; PRISM III: Pediatric Risk of Mortality III
Of the 39 acutely presenting COVID-19 pediatric patients in our sample with underlying obesity, 43.59% required PICU admission (n=17). When comparing all PICU-admitted patients (n=30), there was no significance between PICU admission status and variables including BMI classification, and PELOD-2 and PRISM III scores (Table 6). In our cohort, none of the patients needed dialysis or continuous renal replacement therapy (CRRT), and their renal function recovered completely with supportive care during the hospital course.
Table 6. Hospital course.
Hospital course for critically ill COVID-19 patients admitted to the PICU. We classified illness severity into mild (PRISM III score <10 or PELOD-2 score ≤5), moderate (PRISM III score 10-19 or PELOD-2 score 6-12), and severe illness (PRISM III score >19 or PELOD-2 score >12)
*PRISM III scores given to n=37 patients: n=30 on the PICU floor and n=7 on the PIMC floor
BMI: body mass index; COVID-19: coronavirus disease 2019; LOS: length of stay; PELOD-2: Pediatric Logistic Organ Dysfunction-2; PICU: pediatric intensive care unit; PRISM III: Pediatric Risk of Mortality III
| Hospital course | ||||||||
| Total (n=30) | Underweight BMI (n=2) | Normal BMI (n=6) | Overweight BMI (n=5) | Obese BMI (n=17) | P-value | |||
| Continuous factors | ||||||||
| PICU LOS (days) | 7.39 (n=30) | 8.79 (n=2) | 3.76 (n=6) | 5.86 (n=5) | 8.95 (n=17) | 0.2753 | ||
| Mean PELOD-2 score | 3.7 (n=30) | 5 (n=2) | 4.17 (n=6) | 6.6 (n=5) | 2.59 (n=17) | 0.0842 | ||
| Mean PRISM III score* | 12.7 (n=37) | 10.5 (n=2) | 12.3 (n=8) | 20.8 (n=5) | 10.71 (n=24) | 0.1128 | ||
Figure 2 shows the distribution of PELOD-2 and PRISM-III scores of PICU-admitted patients by BMI classification.
Outcomes
Though higher mean hospital LOS was seen in both overweight and obese BMI categories, there were no statistically significant differences in hospital LOS by BMI classification. However, PICU admission status was significantly associated with overall hospital LOS (p=1.5E-05), as shown in Table 3. For patients admitted to the PICU (n=30), age (p=0.003), obese BMI classification (p=0.008), and underweight BMI classification (p=0.034) were found to have a significant relationship with PICU LOS, as detailed in Table 7.
Table 7. Outcomes.
Outcomes in critically ill COVID-19 patients admitted to the PICU
BMI: body mass index; CI: confidence interval; COVID-19: coronavirus disease 2019; LOS: length of stay; PICU: pediatric intensive care unit
| Outcomes | ||
| Bivariate analysis (n=30) | ||
| Predictors | Coefficient estimate (95% CI) | P-value |
| PICU LOS | ||
| Age | -1.385 (-2.256, -0.514) | 0.003 |
| Obese BMI (reference=normal BMI) | 17.055 (4.726, 29.385) | 0.008 |
| Underweight BMI | 16.901 (1.310, 32.492) | 0.034 |
| Overweight BMI | 6.230 (-10.6726, 23.133) | 0.458 |
Obese BMI was not found to have significance in terms of overall case mortality, and the survival rate from COVID-19 within our patient population was 93.5%.
Discussion
Our findings contribute to the data on the impact of obesity and acute COVID-19 infection in pediatric patients. In the context of acute COVID-19 presentation, our pediatric sample contained an 85% Hispanic population, a high prevalence of obesity, and a significant difference in age distribution based on BMI classification. Obese patients in our sample were more likely to be older, have one or more comorbidities, present with MIS-C, and require PICU admission. These findings complement the results of recent meta-analyses on the prevalence of obesity in hospitalized COVID-19 pediatric patients [12,13], and its impact on critical illness and hospital course [13]. Although almost 40% of pediatric patients with acute COVID-19 presentation were admitted to the PICU, we were not able to show obesity as an independent risk factor for PICU admission status, invasive mechanical ventilation status, and quantitative PELOD-2 and PRISM III assessments. Underweight and obese BMI levels also led to a significantly longer LOS in the ICU, consistent with prior studies showing a J-curve association of pediatric BMI abnormalities with increased hospital and ICU LOS [13]. We also observed the independent significance of AKI and MIS-C on PICU admission, and these should continue to be appreciated in children with severe COVID-19 infection to improve hospital outcomes [8-12]. Overall mortality at our tertiary center was low at 6.49% (n=5), and hence the findings in our small sample were not able to better correlate the role of pediatric obesity in COVID-19 case mortality.
Bhalala et al. have published a large retrospective study that outlined the characteristics and outcomes of COVID-19 in pediatric patients [12]. In a cohort of 874 children, 62.9% identified as non-Hispanic, 46.2% required PICU admission, and there was a 36.35% prevalence of obesity among admitted children [12]. Another study (n=795) by Tripathi et al. showed that admitted COVID-19 patients had a 31.5% prevalence of obesity and they were also more likely to be diagnosed with MIS-C, have higher ICU admission rates, and increased hospital LOS [13]. They also recognized obesity as an independent risk factor for critical COVID-19 infection, with a more significant impact on pediatric outcomes than those diagnosed with MIS-C [13]. Finally, The Journal of Pediatrics published a related study (n=281), identifying obesity as one of the predictive independent risk factors for severe COVID-19 infection and respiratory disease in pediatric patients [14]. Common hospital complications included acute respiratory distress syndrome and AKI [14]. As recognized by Fernandes et al., these effects could be further studied on a minority population, which has shouldered a disproportionate burden during the COVID-19 pandemic [14].
Further studies with larger sample sizes may be able to indicate a stronger significance between underlying obesity and elevated inflammatory markers and MIS-C status. As pediatric obesity becomes increasingly prevalent, especially in South Texas [15], effective identification of risk factors for critical illness will improve COVID-19 hospital outcomes. Based on the findings of this single-center study, providers can better appreciate obesity as a significant risk factor in hospitalized COVID-19 pediatric patients. Obesity has been shown to be a significant independent risk factor for critical illness and hospital LOS [13], and our study also uncovers its role in MIS-C status, PICU admission, and longer PICU LOS.
Our single-center study had some limitations. The pediatric sample included patients admitted to the Children’s Hospital of San Antonio, and represented only that particular geographic region and respective demographic(s). The hospital and PICU admission criteria that we utilized may or may not be representative of the criteria employed by other hospital systems. Our pediatric sample was small (n=77) and efforts at a more focused analysis were limited by this small sample size. Statistical analysis was carefully carried out to reflect accepted models for analysis and feasible tests that could be satisfied by the appropriate sample size. Due to the retrospective nature of the study and a lack of access to clinic records, our study was limited in terms of determining obesity-related, pre-existing mild AKI with microalbuminuria in our cohort. Since the key objective of the study was to investigate the role of underlying obesity in COVID-19 presentations and outcomes at a tertiary care children’s hospital, the study did not analyze the association between outcomes of COVID-19 and adolescence and/or LGBTQ population and comorbidities other than obesity. In the future, we plan to assess these parameters, including the progression of the disease or any delay in accessing medical care among obese children.
Conclusions
Pediatric obesity is becoming increasingly prevalent, and this single-center report captures the prevalence of childhood obesity in the context of the COVID-9 pandemic. Of the admitted COVID-19 patients, more than half had an obese BMI classification, and they were predominantly of Hispanic ethnicity. Obese BMI classification was found to be significant in terms of patient age distribution, comorbidities, MIS-C status, and PICU LOS. Hospital mortality in pediatric COVID-19 patients was low and consistent with other studies in the literature showing lower rates of mortality in children versus mortality in adult patients with COVID-19.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. IRB at Baylor College of Medicine issued approval H-47558
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Sattar N, McInnes IB, McMurray JJ. Circulation. 2020;142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 2.Obesity and outcomes in COVID-19: when an epidemic and pandemic collide. Sanchis-Gomar F, Lavie CJ, Mehra MR, Henry BM, Lippi G. Mayo Clin Proc. 2020;95:1445–1453. doi: 10.1016/j.mayocp.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. Kompaniyets L, Goodman AB, Belay B, et al. MMWR Morb Mortal Wkly Rep. 2021;70:355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 pandemic: disparate health impact on the Hispanic/Latinx population in the United States. Macias Gil R, Marcelin JR, Zuniga-Blanco B, Marquez C, Mathew T, Piggott DA. J Infect Dis. 2020;222:1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Ludvigsson JF. Acta Paediatr. 2020;109:1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Mehta NS, Mytton OT, Mullins EW, et al. Clin Infect Dis. 2020;71:2469–2479. doi: 10.1093/cid/ciaa556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 infection prevalence in pediatric population: etiology, clinical presentation, and outcome. Alsohime F, Temsah MH, Al-Nemri AM, Somily AM, Al-Subaie S. J Infect Public Health. 2020;13:1791–1796. doi: 10.1016/j.jiph.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Renal dysfunction in hospitalised children with COVID-19. Stewart DJ, Hartley JC, Johnson M, Marks SD, du Pré P, Stojanovic J. Lancet Child Adolesc Health. 2020;4:0–9. doi: 10.1016/S2352-4642(20)30178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acute kidney injury in children with COVID-19: a retrospective study. Kari JA, Shalaby MA, Albanna AS, Alahmadi TS, Alherbish A, Alhasan KA. BMC Nephrol. 2021;22:202. doi: 10.1186/s12882-021-02389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Multisystem inflammatory syndrome in children and SARS-CoV-2: a scoping review. Panigrahy N, Policarpio J, Ramanathan R. J Pediatr Rehabil Med. 2020;13:301–316. doi: 10.3233/PRM-200794. [DOI] [PubMed] [Google Scholar]
- 11.COVID-19 and multisystem inflammatory syndrome in Latin American children: a multinational study. Antúnez-Montes OY, Escamilla MI, Figueroa-Uribe AF, et al. Pediatr Infect Dis J. 2021;40:0–6. doi: 10.1097/INF.0000000000002949. [DOI] [PubMed] [Google Scholar]
- 12.Characterization and outcomes of hospitalized children with coronavirus disease 2019: a report from a multicenter, viral infection and respiratory illness universal study (coronavirus disease 2019) registry. Bhalala US, Gist KM, Tripathi S, et al. Crit Care Med. 2022;50:0–51. doi: 10.1097/CCM.0000000000005232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The impact of obesity on disease severity and outcomes among hospitalized children with COVID-19. Tripathi S, Christison AL, Levy E, et al. Hosp Pediatr. 2021;11:0–316. doi: 10.1542/hpeds.2021-006087. [DOI] [PubMed] [Google Scholar]
- 14.Severe acute respiratory syndrome coronavirus 2 clinical syndromes and predictors of disease severity in hospitalized children and youth. Fernandes DM, Oliveira CR, Guerguis S, et al. J Pediatr. 2021;230:23–31. doi: 10.1016/j.jpeds.2020.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trends and disparities in the prevalence of childhood obesity in south Texas between 2009 and 2015. Foster BA, Maness TM, Aquino CA. J Obes. 2017;2017:1424968. doi: 10.1155/2017/1424968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. A SAS program for the 2000 CDC growth charts (ages 0 to 20 years) the. [ Aug; 2022 ]. 2019. https://www.cdc.gov/nccdphp/dnpao/growthcharts/%20resources/sas.htm https://www.cdc.gov/nccdphp/dnpao/growthcharts/%20resources/sas.htm
- 17.Centers for Disease Control and Prevention. A SAS program for the WHO growth charts (ages 0 to <2 years) [ Aug; 2022 ]. 2019. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/ https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/
- 18.Weight as a risk factor for mortality in critically ill patients. Ayalon I, Woo JG, Basu RK, Kaddourah A, Goldstein SL, Kaplan JM. Pediatrics. 2020;146:3–7. doi: 10.1542/peds.2019-2829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Performance of PRISM III and PELOD-2 scores in a pediatric intensive care unit. Gonçalves JP, Severo M, Rocha C, Jardim J, Mota T, Ribeiro A. Eur J Pediatr. 2015;174:1305–1310. doi: 10.1007/s00431-015-2533-5. [DOI] [PubMed] [Google Scholar]
- 20.Pediatric Risk, Injury, Failure, Loss, End-Stage renal disease score identifies acute kidney injury and predicts mortality in critically ill children: a prospective study. Soler YA, Nieves-Plaza M, Prieto M, García-De Jesús R, Suárez-Rivera M. Pediatr Crit Care Med. 2013;14:0–95. doi: 10.1097/PCC.0b013e3182745675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Multisystem inflammatory syndrome (MIS-C) [ Aug; 2022 ]. 2020. https://www.cdc.gov/mis-c/index.html https://www.cdc.gov/mis-c/index.html
- 22.Daniel WW, Cross CL. New York, NY: Wiley Publishers; 2018. Biostatistics: A Foundation for Analysis in the Health Sciences. [Google Scholar]
- 23.Agresti A. New York, NY: Wiley Publishers; 2018. An Introduction to Categorical Data Analysis. [Google Scholar]
- 24.RStudio Team (2021. RStudio Team. [ Aug; 2022 ]. 2021. http://www.rstudio.com/ http://www.rstudio.com/