Abstract
The current study examined the temporal precedence of change in obsessive-compulsive symptoms and change in depressive symptoms during the course of an Exposure and Response Prevention (ERP) for pediatric OCD. Participants included 142 children and adolescents (7–17 years; mean age=12.39, SD= 2.92; 51.40% female; 60.40% Non-Hispanic White) with a primary or co-primary diagnosis of OCD who received ERP in a two-site randomized controlled trial on d-cycloserine augmentation of CBT for pediatric OCD. Participants completed clinician-administered assessments of OC symptoms (Children’s Yale-Brown Obsessive Compulsive Scale) and depressive symptoms (Children’s Depression Rating Scale-Revised) from baseline to post-treatment follow-up. Lagged mediational analyses did not yield evidence in support of a mediating role for the change in OC symptoms in the effect of ERP on the change in depressive symptoms. In contrast, change in depressive symptoms mediated the effect of ERP treatment on the subsequent change in OC symptoms (95% confidence interval for indirect effect= −0.13 to −0.005), though the effect size was small. Controlling for the prior levels of the depressive symptoms this indirect effect became non-significant. Theoretical and clinical implications of the findings for the youth with OCD and comorbid depression are discussed.
Keywords: Exposure and Response Prevention, Obsessive-Compulsive Disorder, Depression, Pediatrics, Longitudinal Mediation, Mechanisms of Change
Obsessive-compulsive disorder (OCD), characterized by distressing, intrusive, unwanted obsessions and/or ritualistic actions, has a lifetime prevalence of 1 to 2% among children and adolescents (Douglass, Moffitt, Dar, McGee, & Silva, 1995; Zohar, 1999). Pediatric OCD negatively affects the quality of life of children with manifestations such as impaired academic and social performance and higher family conflict (Lack et al., 2009; Storch et al., 2018), which is exacerbated in the presence of comorbid mental illnesses (Canavera, Ollendick, May, & Pincus, 2010). Among the comorbid psychiatric conditions present among youth with OCD, depressive disorders are uniquely associated with poor quality of life and may affect as many as 50–70% of children with OCD (Geller, Biederman, Griffin, Jones, & Lefkowitz, 1996; Geller et al., 2003). As such, the identification of the association between comorbid depressive and obsessive-compulsive symptoms during the course of OCD or its treatment is imperative to develop interventions that could lead to more successful outcomes among OCD youth with comorbid depression.
However, the existing evidence regarding the relationship between OCD and depressive symptoms during the course of treatment for pediatric OCD is inconsistent. Some studies have suggested that depression severity decreases over the course of evidence-based OCD treatments for youth and argued against the need for simultaneously targeting depression in this patient population (Brown, Lester, Jassi, Heyman, & Krebs, 2015). Meanwhile, others have proposed a role for severe comorbid depression as a clinical predictor of outcome among youth receiving OCD treatment and advocated for treating depression in these cases (Keeley, Storch, Merlo, & Geffken, 2008; Wilhelm et al., 2018). To address this inconsistency, recent work has attempted to investigate this issue using rigorous analytical methods, conducting mediational research on processes of change in OC and depressive symptoms during the course of OCD treatments (Olatunji et al., 2013; Zandberg et al., 2015). Specifically, by examining the temporal precedence of the change in depressive symptoms and the change in obsessive-compulsive symptoms for each other, these studies have attempted to elucidate the processes of symptom change in OCD treatments. Unfortunately, these efforts have led to more inconsistent findings and ongoing debate (Anholt et al., 2011; Olatunji et al., 2013; Zandberg et al., 2015).
Two studies have examined these temporal relationships in adults using the suggested time-lagged mediation methodology over the course of treatment. In a sample of 62 adult OCD patients receiving either cognitive therapy (n= 30) or behavior therapy (n= 32), Olatunji et al. found that change in depressive symptoms mediated the effect of the intervention on the change in obsessive-compulsive symptoms over 52 weeks (Olatunji et al., 2013). Notably, these effects were above the impact of two other hypothesized mediators in the model; behavioral avoidance and dysfunctional beliefs regarding responsibility. The hypothesized reverse mediation pathway from obsessive-compulsive symptoms to depressive symptoms was not significant. However, the authors did not examine this reverse path without the contribution of the dysfunctional beliefs and avoidance which both covary with OC symptoms that could have led to this null finding. The only study to date that has examined this issue with a sole focus on exposure and response prevention (ERP) yielded different results. In this study, in a sample of 40 adult OCD patients, Zandberg and colleagues found that both changes in obsessive-compulsive symptoms and depressive symptoms mediated the effect of ERP on each other over 32 weeks (Zandberg et al., 2015). However, these effects were much larger for the mediating role of obsessive-compulsive symptoms than depressive symptoms; obsessive-compulsive symptoms accounted for 64.8% of the change in depressive symptoms while depressive symptoms only accounted for 19.6% of the change in obsessive-compulsive symptoms (Zandberg et al., 2015). Based on the theoretical model that changes in the targeted symptoms of a fear-based disorder (OCD) accounts for a larger proportion of the variance of change in depressive symptoms than the reverse (Alloy, Kelly, Mineka, & Clements, 1990; Anholt et al., 2011), the authors concluded that the reduction in comorbid depressive symptoms during ERP is driven mainly by the reduction in obsessive-compulsive symptoms. Given these inconsistent findings, further investigations of this issue are required in both adults and children.
To date, no study has examined the temporal precedence of change in OC and depressive symptoms during the course of ERP as the first-line treatment for pediatric OCD (Bloch & Storch, 2015), which has demonstrated considerable efficacy across randomized clinical trials (McGuire et al., 2015). Replicating the above-mentioned findings among youth with OCD could help to generalize these findings to this population and address some of the inconsistencies in previous research. This research is of particular importance given the differences in neurobiological underpinnings, clinical presentations, and diagnostic criteria between adult and pediatric OCD (Farrell, Barrett, & Piacentini, 2006). For example, compared to adult OCD, pediatric OCD includes different types of obsessive themes (e.g., less sexual and more contamination obsessions) and is associated with lower levels of clinically significant comorbid depression and social impairment (Farrell et al., 2006; Geller et al., 2001). Recognition of this developmental discontinuity through examination of the symptom change processes during the course of ERP for pediatric OCD with comorbid depression could improve our knowledge regarding the relative clinical significance of these comorbid symptoms in a more precise manner. This knowledge, in turn, could help with decisions regarding theoretically-driven modifications to ERP for pediatric OCD with comorbid depression.
Therefore, using a lagged mediation hypothesis, this study examined the temporal precedence of change in obsessive-compulsive symptoms for change in depressive symptoms as well as the change of depressive symptoms for change in obsessive-compulsive symptoms during the course of an ERP for pediatric OCD. Based on previous findings, we hypothesized that changes in obsessive-compulsive and depressive symptoms would mediate the effects of the ERP on each other. We also hypothesized that the size of the mediation effect for OC symptoms would be larger than the size of the mediation effect for the depressive symptoms. Further, we hypothesized that these effects would be above the variance in each of the outcome variables explained by the prior levels of each symptom.
Methods
Participants
The current study is a secondary analysis of data from a two-site randomized controlled trial on d-cycloserine augmentation of CBT for pediatric OCD [University of South Florida (USF) and Massachusetts General Hospital (MGH)]. The details of the study are described elsewhere (Storch et al., 2016). Participants included 142 children and adolescents (7–17 years; mean age=12.39, SD= 2.92; 51.40% female; 60.40% Non-Hispanic White) with a primary or co-primary diagnosis of OCD based on a structured clinical interview (Kaufman et al., 1997). Other inclusion criteria were a Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) total score of at least 16 (Scahill et al., 1997), and a full-scale intelligence quotient (IQ) of at least 85 (Wechsler, 1999). Exclusion criteria were: 1) receiving concurrent psychotherapy or a past trial of CBT for OCD, 2) initiation of an antidepressant within 12 weeks or antipsychotic medication within 6 weeks before enrollment, or having an increase in medication dosage before enrollment (8 weeks for antidepressants, 6 weeks for antipsychotics), 3) any changes in the dosage of the current medication throughout treatment, 4) clinically significant suicidality in the past year, 5) diagnosis of conduct disorder, autism, bipolar, schizophrenia or schizoaffective disorders, substance abuse, anorexia nervosa, or non-OCD primary hoarding, 6) contraindications for DCS (e.g., epilepsy, renal insufficiency, weight of less than 22.5 kg, DCS allergy), 7) inability to swallow study medication, 8) currently pregnant or engaging in unprotected sex (for females only), and 9) presence of a significant and/or unstable medical illness.
For participating youth, the mean CY-BOCS score at baseline was 25.58 (SD = 5.74, Range: 13–38) that corresponds with moderate-severe OC symptoms (Lewin et al., 2014). Only 14.9% of the sample (n = 21) met criteria for current depressive disorder (i.e., major depressive disorder, dysthymia, or depressive disorder NOS). Baseline Children’s Depression Rating Scale-Revised (CDRS-R)(Poznanski & Mokros, 1996) scores ranged from 17 to 61 with an average score of 27.06 (SD = 9.84), corresponding to mild depression and below the remission cutoff score of 28 (minimal to no symptoms). Indeed, using this cutoff score, only 26.3% (n = 37) of the sample was in the clinical range.
Measures
The Kiddie Schedule for Affective Disorders and Schizophrenia. (KSADS-PL)(Kaufman et al., 1997).
The KSADS-PL is a clinician-administered structured diagnostic interview of The Diagnostic and Statistical Manual for Mental Disorders, 4th Edition (DSM-IV) childhood disorders. It was administered to both parents and children, and clinical judgment used to determine diagnoses based upon combined reports. The K-SADS-PL has demonstrated good test-retest reliability and validity.
Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS)(Goodman et al., 1989; Scahill et al., 1997).
The CY-BOCS is a 10-item semi-structured clinician-administered interview used to assess symptom severity of obsessions and compulsions in the past week. Each item is rated on a 5-point Likert scale (0 = no symptoms, 4 = extreme). Total scores range from 0 to 40. The CY-BOCS has good internal consistency, excellent inter-rater reliability, and good test-retest reliability (Goodman et al., 1989; Scahill et al., 1997). Internal consistency across assessments in the present sample (baseline, visits 5, 8, and 12) ranged from 0.84 to 0.92.
Children’s Depression Rating Scale-Revised (CDRS-R)(Poznanski & Mokros, 1996).
The CDRS-R is a clinician-administered scale that assesses depression severity. It consists of 17-items that are summed to produce a total depression severity score. The CDRS-R has demonstrated good psychometric properties among children and adolescents (Poznanski & Mokros, 1996). Internal consistency across assessments in the present sample (baseline, visits 5, 8, and 12) ranged from 0.82 to 0.87.
Procedures
Eligible participants were screened by a trained independent evaluator who administered the KSADS-PL and the CY-BOCS to the parent and child. Children who met inclusion criteria, completed the informed consent process and began a 10-session cognitive behavioral treatment at a rate of two sessions per week for the first two weeks. The first three sessions (visits 2 to 4) included psychoeducation, cognitive interventions, and hierarchy development. Before the fourth CBT session (visit 5; i.e., the first E/RP session), youth who continued to meet inclusion/exclusion criteria were randomly assigned to DCS + CBT or placebo + CBT. The remainder of the treatment (sessions 4–10) was conducted weekly, and involved exposure with response prevention (ERP) exercises specific to the patient’s symptom profile. All patients were administered the CY-BOCS, and CDRS-R at study visits 1 (baseline), 5 (session 4), 8 (session 7), and 12 (within one week following the final CBT session). Most of the participants completed the full course of treatment (98%), with only three youth discontinuing treatment after randomization. Treatment integrity was monitored by weekly CBT supervision calls and confirmed by the use of session content checklists that corresponded to the treatment manual. Twenty percent of sessions were randomly selected for review found to have good fidelity (see Storch et al. 2016 for further detail). About one-third of the participants reported using a psychiatric medication. There were no group differences between treatment conditions or individuals with and without psychiatric medication regarding the levels of OC symptom severity (CY-BOCS total score) and depression symptom severity (CDRS-R total score) at pre and post ERP.
Data Analyses
Data were analyzed using multilevel linear modeling (MLM) through linear mixed-effects models (MIXED) procedure in SPSS, version 23. The estimation of unknown parameters in the models was based on the restricted maximum-likelihood estimation. The models included two levels, where repeated assessments across time (Level 1; variables included time, obsessive-compulsive and depressive symptoms) were nested within participants (Level 2). Multilevel modeling technique is one of the principled methods for dealing with missing data that permits the number of observations to vary between participants (Raudenbush, 2001).Prior to running mediation analyses, we compared a model with a linear time variable, and a quadratic time variable using Akaike’s information criterion (Akaike, 1987) and the deviance statistic. Results indicated a better fit for the linear model across all study variables. To allow for the time irregularity in the assessments, a time-structured predictor was included. Thus, the time values corresponded with the actual time spaces (in weeks) between each follow-up assessment (Singer, Willett, & Willett, 2003). Lagged mediational analyses (Kenny, Korchmaros, & Bolger, 2003) were conducted to evaluate the relationship between obsessive-compulsive and depressive symptoms from visit 5 to visit 12 (three time-points Figure 1). Lagged mediation models establish the temporal precedence of mediator versus outcome variables. These models examine whether within-individual changes in the mediator variable at Time t would account for changes in the outcome variable at Time t+1. (length of each lag = 1 week). The within- vs. between-subject component of crossed lagged effects is what could be used for inference on causality (Blackwell & Glynn, 2018). In order to differentiate the effects of the between and within-subject components of each time-varying mediator on the outcome variable, the between and within-subject components of these mediators were disaggregated (Wang & Maxwell, 2015). Specifically, a grand mean centered variable, and a person mean-centered variable (representing the between and within-subject components of the mediator variable respectively) were introduced to the models that included the mediators. Two models were tested (Figure 1). The first one examined the mediating role of within-individual changes in obsessive-compulsive symptoms for the changes in depressive symptoms between visit 5 to visit 12, with Time being the predictor, obsessive-compulsive symptoms the mediator, and depressive symptoms the outcome. The second models tested the mediating role of within-individual changes in depressive symptoms for changes in obsessive-compulsive symptoms, with Time being the predictor, depressive symptoms as the mediator, and obsessive-compulsive symptoms as the outcome. We used RMediation package (Tofighi & MacKinnon, 2011) to calculate the confidence interval (CI) of the indirect effects. Percent mediation was used to estimate the effect size of the mediation (K. J. Preacher & Kelley, 2011). The 95% confidence intervals that do not contain zero indicate that an indirect effect is statistically significant (Kristopher J Preacher & Selig, 2012). We ran each model twice. First, we ran the models without controlling for the prior levels of the outcome variable to compare the results with the only other existing similar analysis among adults. Next, we run the models another time after controlling for the prior levels of the outcome variable in each model (i.e., a time-lagged outcome variable). Since we found no significant differences in outcomes between the patients in each treatment condition as well as medication receivers and non-receivers these variables were not included in the analyses.
Figure 1.
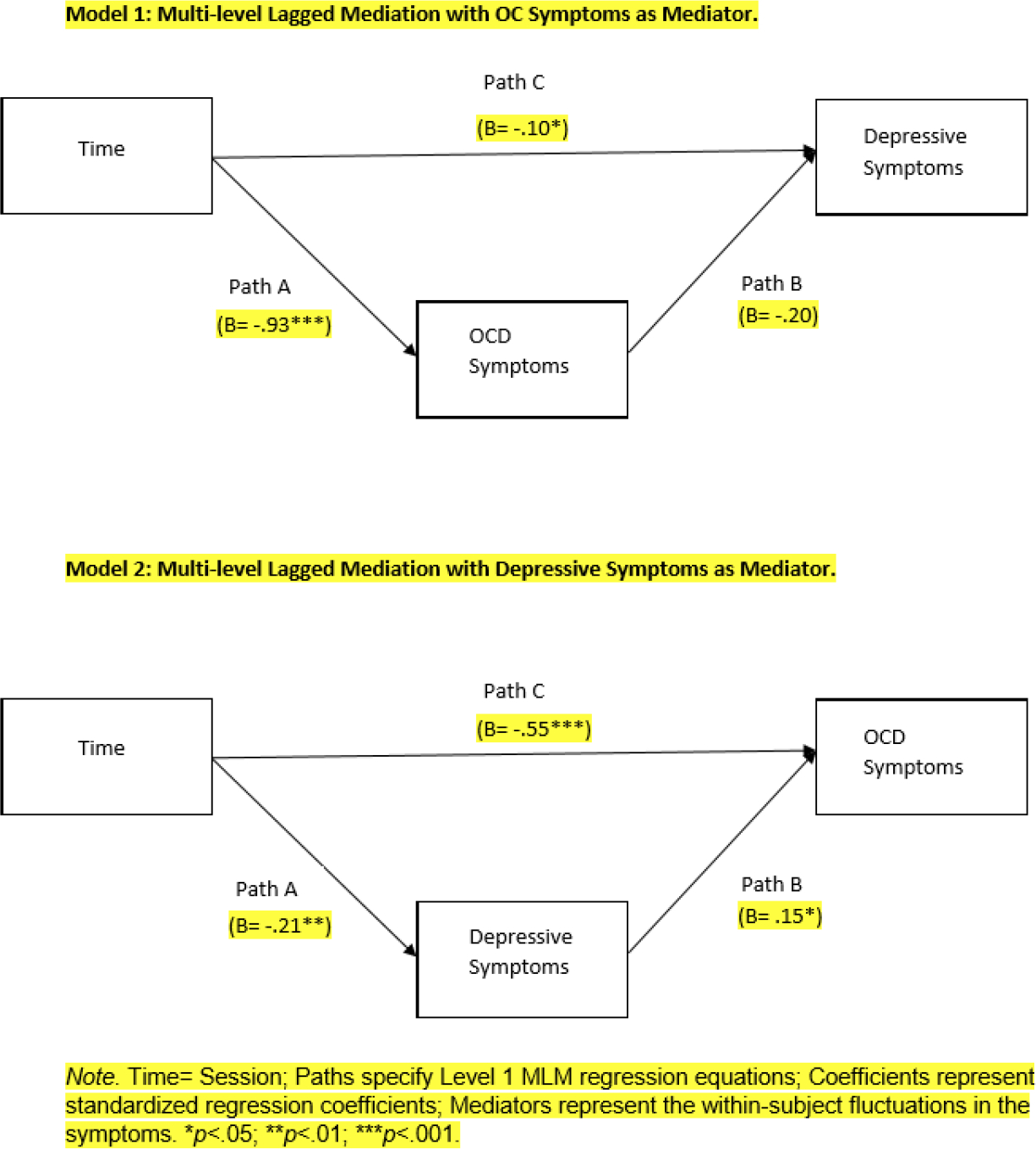
Mediational models testing the effect of change in OC Symptoms and Change in Depressive Symptoms on each other.
Results
Mediation Analyses
For model one with obsessive-compulsive symptoms as the hypothesized mediator, the A path (obsessive-compulsive symptoms regressed on time) was significant (b= −.83, SE= 0.04, t= −19.80, p< .001) indicating that obsessive-compulsive symptoms significantly decreased during the treatment at a within-person level. Path B with depressive symptoms regressed on within-individual change in obsessive-compulsive symptoms was not significant (b= −0.04, SE= 0.31, t= −0.13, p= .79). Next, path C (depressive symptoms regressed on time) was significant (b= −0.32, SE= 0.12, t= −2.52, p= .012) indicating that depressive symptoms significantly decreased between visit 5 to visit 12. The confidence intervals for the indirect effect (path a*path B) did include zero, 95% CI [−0.47 to 0.54], thus rejecting the hypothesized mediation. Controlling for the prior levels of the obsessive-compulsive symptoms the indirect effect remained non-significant (95% CI [−0.17 to 0.81]; see results for the regression analyses of the adjusted model in Table 1).
Table 1.
Summary of Multilevel Regression Analyses for the Mediational Model 1: OC Symptoms as Mediator, Controlling For Prior Levels of OC Symptoms.
| Step | Path | Predictor | Outcome | b | SE | t | p |
|---|---|---|---|---|---|---|---|
|
| |||||||
| 1 | C | Time | Depressive symptoms | −.11 | .19 | −.96 | .33 |
| 2 | A | Time | OCD symptoms | −.80 | .04 | −17.90 | <.001 |
| 3 | B | OCD symptoms | Depressive symptoms | −.04 | .31 | −.13 | . 79 |
Regarding model two with depressive symptoms as the hypothesized mediator, the A path (depressive symptoms regressed on time) was significant (b=−0.22, SE=0.07, t= −3.43, p= .001) indicating that depressive symptoms significantly decreased during the treatment at a within-person level. Path B with OC symptoms regressed on within-individual change in depressive symptoms was significant (b= 0.27, SE= 0.12, t= 2.23, p= .03). Next, Path C (obsessive-compulsive symptoms regressed on time) was significant (b= −1.50, SE= 0.09, t= −17.24, p<.001) indicating that obsessive-compulsive symptoms significantly decreased between visit 5 to visit 12. The confidence intervals for the indirect effect (path a*path b) did not include zero, 95% CI [−.13 to −0.005], providing evidence for mediation. Only 5.2% of the variance of the change in obsessive-compulsive symptoms was accounted for by the indirect (mediation) effect. Controlling for the prior levels of the depressive symptoms the mediation effect became non-significant (95% CI [−0.15 to 0.02]; see results for the regression analyses of the adjusted model in Table 2).
Table 2.
Summary of Multilevel Regression Analyses for the Mediational Model 2: Depressive Symptoms as Mediator, Controlling For Prior Levels of Depressive Symptoms.
| Step | Path | Predictor | Outcome | b | SE | t | p |
|---|---|---|---|---|---|---|---|
|
| |||||||
| 1 | C | Time | OCD symptoms | −.86 | .09 | −9.62 | <.001 |
| 2 | A | Time | Depressive symptoms | −0.22 | 0.06 | −3.44 | .001 |
| 3 | B | Depressive symptoms | OCD symptoms | .26 | .18 | .14 | .88 |
Discussion
The current study examined the temporal precedence of the change in obsessive-compulsive symptoms and depressive symptoms for each other during the course of ERP treatment for youth with OCD. Study findings were generally not in line with our expectations. Specifically, change in obsessive-compulsive symptoms did not mediate change in depressive symptoms during ERP. The change in depressive symptoms also did not turn out to have a significant impact on the change in obsessive-compulsive symptoms. However, since the only other study with a sole focus on ERP that has examined this model did not control for the prior levels of the outcome variables, and because of the reported dramatic attenuation of the effect sizes in longitudinal designs that adjust for prior levels of the outcome (Adachi & Willoughby, 2015), we also decided to discuss and (with caution) interpret the findings of the models with no prior levels of outcome variable. Observing the unadjusted models, change in OC symptoms still did not significantly mediate the effect of ERP on change in depressive symptoms. The change in depressive symptoms was a significant mediator of the effect of ERP on change in obsessive-compulsive symptoms, although this mediating effect only accounted for a small proportion of the change in obsessive-compulsive symptoms. Thus, we could not replicate the findings of Zandberg et al. who suggested a mediating role for the change in obsessive-compulsive symptoms in adults. However, similar to Zandberg et al., the current study also found a mediating role (although small) for change in depressive symptoms in the effect of ERP on obsessive-compulsive symptoms among youth with OCD which suggests a temporal precedence for the change in depressive symptoms compared to the change in obsessive-compulsive symptoms during a course of ERP. This mediating role of the change in depressive symptoms has also been observed by Olatunji et al. who found that change in depressive symptoms mediates the effect of the OCD interventions on obsessive-compulsive symptoms above and beyond the effect of the other hypothesized cognitive mediators (i.e., obsessions-related beliefs and avoidance).
There may be several reasons that we did not find a significant mediating role for change in obsessive-compulsive symptoms. For example, the relatively short follow-up period of the current study may be one other reason for the null finding regarding the mediating role of change in obsessive-compulsive symptoms. Indeed, past research has shown that the impact of obsessive-compulsive and depressive symptoms on each other could follow a non-linear pattern that may not be detected in shorter follow-up periods. (Tibi et al., 2017). Alternatively, this null finding may reflect the underestimation of the “b” paths in cross-lagged MLM models, which could lead to insignificant indirect effects (a*b) (Falkenström et al., 2017). Further, the relatively long lags between the assessment points (3 to 4 weeks) that could potentially obscure meaningful temporal associations could be another reason for this negative finding. Finally, the shorter duration of the treatment and milder levels of depressive symptoms in the current study sample compared to Zandberg et al. (with only about one in four being in the clinical range), as well as different manifestations of OCD and depression in youth compared to adults, could have led to this negative finding (Jones, Mair, Riemann, Mugno, & McNally, 2018; Piacentini, Bergman, Keller, & McCracken, 2003).
Although it needs to be interpreted with caution, the comparability of the current study’s findings regarding the mediating role of the change in depressive symptoms to those among adult OCD patients also has some prior empirical support in pediatric OCD literature. Indeed, past research has demonstrated that change in depressive symptoms over the course of an OCD treatment can predict post-treatment obsessive-compulsive symptom severity (Leonard, Jacobi, Riemann, Lake, & Luhn, 2014). Better ERP adherence following the enhancement of the patients’ motivation and concentration is one possible mechanism by which the reduction of depressive symptoms might result in a positive obsessive-compulsive-related symptomatic outcome (Simpson et al., 2011). Notably, given past work demonstrating the benefits of combining interventions targeting depression with ERP to improve the outcome of pediatric OCD with severe comorbid depressive symptoms (Leonard et al., 2014), the current study’s mediation model needs to be replicated among youth with OCD who have higher levels of comorbid depression. If replicated with larger effect sizes, the findings might have implications regarding the development of specialized treatments for this sub-population of youth with OCD. It may be that these patients could benefit from interventions targeting their comorbid depressive symptoms as an adjuvant to the standard ERP treatments. This is an important next research step since while ERP might improve depressive symptoms related to OCD (i.e., withdrawal from activities due to OC symptoms), it is not specifically focused on addressing these symptoms.
The current study has several limitations. First, we ran the lagged mediation analyses with just four time-points for which data on obsessive-compulsive and depressive symptoms were available. In addition to the limitations that this small number of time-points can impose on our analyses, it also reflects the current study’s shorter follow-up period compared to that in previous studies which may have been the reason for some of our null findings. Future studies need to replicate these findings with more follow-up time points and across the acute and maintenance phases of ERP treatment. Second, the present study sample mainly consisted of pediatric OCD patients with mild-to-moderate depressive symptoms. Given the greater clinical relevance of severe (compared to mild-to-moderate) forms of depressive symptoms to OCD treatment outcome (Leonard et al., 2014), future studies need to examine these models among OCD patients with severe comorbid depression.1 Third, we did not have data regarding the temporal precedence of the onset of obsessive-compulsive symptoms over depressive symptoms in this sample. Past research in adults has suggested that the precedence of the onset of obsessive-compulsive symptoms to the depressive symptoms is a clinical determinant of the impact of the change in obsessive-compulsive symptoms on the change in depressive symptoms during the course of OCD treatment (Zandberg et al., 2015). Thus, future work needs to control for this factor. Fourth, we did not have data regarding the theoretically relevant confound variables (e.g., treatment adherence). Future work needs to control for these variables in similar models, to strengthen the argument regarding the causal inference.
In conclusion, the current findings did not support a mediating role for the change in OC symptoms in the effect of ERP on the change in depressive symptoms for youth with primary OCD diagnosis. However, similar to past research there was support for the reverse direction suggesting that change in depressive symptoms may partially mediate the effect of ERP treatment on the change in obsessive-compulsive symptoms among youth, though the effect was small. Future theory-driven work among clinical and non-clinical samples of youth with obsessive-compulsive symptoms and a broader range of depressive symptomatology is needed to better understand the temporal relationship between the change in obsessive-compulsive and depressive symptoms and use such information to develop more personalized approaches to OCD treatment.
Funding:
This work was supported by the National Institutes of Mental Health grants (R01MH09338 and R01MH093402) awarded to Drs. Storch and Geller, respectively. The clinicaltrials.gov Identifier is NCT00864123. The sponsor was not involved in the design, data collection, analysis, writing of the report, or in the decision to submit the paper for publication.
Footnotes
Summary declaration of interest statement:
Dr. Bakhshaie, Ms. Cepeda, and Ms. Porth report no potential conflicts of interests.
Dr. Schneider receives grant support from the American Red Cross and the Texas Higher Education Coordinating Board.
Dr. Small reports receiving research support from the National Institutes of Health.
Dr. McGuire receives research support from the Tourette Association of America and the American Academy of Neurology. He receives consulting fees from Brackett, Syneos Health, and Luminopia, and also receives book royalties from Elsevier.
Dr. Geller reports receiving grant support from the National Institutes of Health and a book honorarium from the American Academy of Child and Adolescent Psychiatry; reported receiving speaking honoraria for Advanced Institute lectures from the American Academy of Child and Adolescent Psychiatry and Massachusetts General Hospital Psychiatry Academy in educational programs supported through independent medical education grants from pharmaceutical companies; and reported receiving lifetime funding support from the International OCD Foundation, Tourette Association of America, McIngvale Family Foundation, Eli Lilly, Pfizer, GlaxoSmithKline, and Neurocrine Bioscience.
Dr. Murphy reports receiving research funding from Auspex Pharmaceuticals, National Institute of Mental Health, Shire Pharmaceuticals, Pfizer, F. Hoffmann–La Roche Ltd, AstraZeneca Pharmaceuticals, Centers for Disease Control and Prevention, Massachusetts General Hospital, Sunovion Pharmaceuticals, Neurocrine Biosciences, PANDAS Network, and Psyadon Pharmaceuticals.
Dr. Wilhelm reports receiving research support in the form of free medication and matching placebo from Forest Laboratories for clinical trials funded by the NIH. Dr. Wilhelm is a presenter for the Massachusetts General Hospital Psychiatry Academy in educational programs supported through independent medical education grants from pharmaceutical companies; she has received royalties from Elsevier Publications, Guilford Publications, New Harbinger Publications, and Oxford University Press. Dr. Wilhelm has also received speaking honorarium from various academic institutions and foundations, including the International Obsessive Compulsive Disorder Foundation, Tourette Association of America, and Brattleboro Retreat. In addition, she received payment from the Association for Behavioral and Cognitive Therapies for her role as Associate Editor for the Behavior Therapy journal, as well as from John Wiley & Sons, Inc. for her role as Associate Editor on the journal Depression & Anxiety. Dr. Wilhelm has also received honorarium from One-Mind for her role in PsyberGuide Scientific Advisory Board. Dr. Wilhelm has received salary support from Novartis and Telefonica Alpha, Inc.
Dr. Storch reports receiving research support from the National Institutes of Health, Red Cross, Greater Houston Community Foundation, ReBuild Texas, International OCD Foundation, and Texas Higher Education Coordinating Board; reported receiving royalties from Elsevier Publications, Springer, Oxford Press, American Psychological Association, John Wiley & Sons Inc, and Lawrence Erlbaum; reported being a consultant for Levo Therapeutics; reported serving on the speaker’s bureau and scientific advisory board for the International OCD Foundation.
We ran sensitivity analyses in children with more severe depressive symptoms based on the CDRS cut off scores of 28 (minimal to no symptoms). The pattern of the results stayed the same across the sub-samples with high versus low depressive symptomatology, although future comparisons with larger sample sizes are needed.
References
- Adachi P, & Willoughby T (2015). Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: Implications for psychological science. European Journal of Developmental Psychology, 12(1), 116–128. [Google Scholar]
- Akaike H (1987). Model selection and Akaike’s Information Criterion (AIC): The general theory and its analytical extensions. Psychometrica, 52(3), 345–370. [Google Scholar]
- Alloy LB, Kelly KA, Mineka S, & Clements CM (1990). Comorbidity of anxiety and depressive disorders: a helplessness-hopelessness perspective.
- Anholt GE, Aderka IM, van Balkom AJ, Smit JH, Hermesh H, de Haan E, & van Oppen P (2011). The impact of depression on the treatment of obsessive-compulsive disorder: results from a 5-year follow-up. J Affect Disord, 135(1–3), 201–207. doi: 10.1016/j.jad.2011.07.018 [DOI] [PubMed] [Google Scholar]
- Blackwell M, & Glynn ANJAPSR (2018). How to make causal inferences with time-series cross-sectional data under selection on observables. 112(4), 1067–1082. [Google Scholar]
- Bloch MH, & Storch EA (2015). Assessment and management of treatment-refractory obsessive-compulsive disorder in children. J Am Acad Child Adolesc Psychiatry, 54(4), 251–262. doi: 10.1016/j.jaac.2015.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown HM, Lester KJ, Jassi A, Heyman I, & Krebs G (2015). Paediatric Obsessive-Compulsive Disorder and Depressive Symptoms: Clinical Correlates and CBT Treatment Outcomes. J Abnorm Child Psychol, 43(5), 933–942. doi: 10.1007/s10802-014-9943-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canavera KE, Ollendick TH, May JT, & Pincus DB (2010). Clinical correlates of comorbid obsessive-compulsive disorder and depression in youth. Child Psychiatry Hum Dev, 41(6), 583–594. doi: 10.1007/s10578-010-0189-y [DOI] [PubMed] [Google Scholar]
- Douglass HM, Moffitt TE, Dar R, McGee R, & Silva P (1995). Obsessive-compulsive disorder in a birth cohort of 18-year-olds: prevalence and predictors. J Am Acad Child Adolesc Psychiatry, 34(11), 1424–1431. doi: 10.1097/00004583-199511000-00008 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Finkel S, Sandell R, Rubel JA, Holmqvist R. J. J. o. C., & Psychology C (2017). Dynamic models of individual change in psychotherapy process research. 85(6), 537. [DOI] [PubMed] [Google Scholar]
- Farrell L, Barrett P, & Piacentini J (2006). Obsessive–compulsive disorder across the developmental trajectory: Clinical correlates in children, adolescents and adults. Behaviour Change, 23(2), 103–120. [Google Scholar]
- Geller DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, . . . Coffey BJ (2001). Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis, 189(7), 471–477. [DOI] [PubMed] [Google Scholar]
- Geller DA, Biederman J, Griffin S, Jones J, & Lefkowitz TR (1996). Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry, 35(12), 1637–1646. doi: 10.1097/00004583-199612000-00016 [DOI] [PubMed] [Google Scholar]
- Geller DA, Coffey B, Faraone S, Hagermoser L, Zaman NK, Farrell CL, . . . Biederman J (2003). Does comorbid attention-deficit/hyperactivity disorder impact the clinical expression of pediatric obsessive-compulsive disorder? CNS Spectr, 8(4), 259–264. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, . . . Charney DS (1989). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry, 46(11), 1006–1011. [DOI] [PubMed] [Google Scholar]
- Jones PJ, Mair P, Riemann BC, Mugno BL, & McNally RJ (2018). A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J Anxiety Disord, 53, 1–8. doi: 10.1016/j.janxdis.2017.09.008 [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, . . . Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry, 36(7), 980–988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Keeley ML, Storch EA, Merlo LJ, & Geffken GR (2008). Clinical predictors of response to cognitive-behavioral therapy for obsessive-compulsive disorder. Clin Psychol Rev, 28(1), 118–130. doi: 10.1016/j.cpr.2007.04.003 [DOI] [PubMed] [Google Scholar]
- Kenny DA, Korchmaros JD, & Bolger N (2003). Lower level mediation in multilevel models. Psychol Methods, 8(2), 115–128. [DOI] [PubMed] [Google Scholar]
- Lack CW, Storch EA, Keeley ML, Geffken GR, Ricketts ED, Murphy TK, & Goodman WK (2009). Quality of life in children and adolescents with obsessive-compulsive disorder: base rates, parent-child agreement, and clinical correlates. Soc Psychiatry Psychiatr Epidemiol, 44(11), 935–942. doi: 10.1007/s00127-009-0013-9 [DOI] [PubMed] [Google Scholar]
- Leonard RC, Jacobi DM, Riemann BC, Lake PM, & Luhn R (2014). The effect of depression symptom severity on OCD treatment outcome in an adolescent residential sample. Journal of Obsessive-Compulsive and Related Disorders, 3(2), 95–101. [Google Scholar]
- Lewin AB, Piacentini J, De Nadai AS, Jones AM, Peris TS, Geffken GR, . . . Storch, E. A. (2014). Defining clinical severity in pediatric obsessive-compulsive disorder. Psychol Assess, 26(2), 679–684. doi: 10.1037/a0035174 [DOI] [PubMed] [Google Scholar]
- McGuire JF, Piacentini J, Lewin AB, Brennan EA, Murphy TK, & Storch EA (2015). A META-ANALYSIS OF COGNITIVE BEHAVIOR THERAPY AND MEDICATION FOR CHILD OBSESSIVE-COMPULSIVE DISORDER: MODERATORS OF TREATMENT EFFICACY, RESPONSE, AND REMISSION. Depress Anxiety, 32(8), 580–593. doi: 10.1002/da.22389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Rosenfield D, Tart CD, Cottraux J, Powers MB, & Smits JA (2013). Behavioral versus cognitive treatment of obsessive-compulsive disorder: an examination of outcome and mediators of change. J Consult Clin Psychol, 81(3), 415–428. doi: 10.1037/a0031865 [DOI] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Keller M, & McCracken J (2003). Functional impairment in children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol, 13 Suppl 1, S61–69. doi: 10.1089/104454603322126359 [DOI] [PubMed] [Google Scholar]
- Poznanski EO, & Mokros HB (1996). Children’s depression rating scale, revised (CDRS-R): Western Psychological Services Los Angeles. [Google Scholar]
- Preacher KJ, & Kelley K (2011). Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods, 16(2), 93–115. doi: 10.1037/a0022658 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Selig JP (2012). Advantages of Monte Carlo confidence intervals for indirect effects. Communication Methods and Measures, 6(2), 77–98. [Google Scholar]
- Raudenbush SW (2001). Comparing personal trajectories and drawing causal inferences from longitudinal data. Annu Rev Psychol, 52, 501–525. doi: 10.1146/annurev.psych.52.1.501 [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, . . . Leckman JF (1997). Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry, 36(6), 844–852. doi: 10.1097/00004583-199706000-00023 [DOI] [PubMed] [Google Scholar]
- Simpson HB, Maher MJ, Wang Y, Bao Y, Foa EB, & Franklin M (2011). Patient adherence predicts outcome from cognitive behavioral therapy in obsessive-compulsive disorder. J Consult Clin Psychol, 79(2), 247–252. doi: 10.1037/a0022659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence: Oxford university press. [Google Scholar]
- Storch EA, Small BJ, McGuire JF, Murphy TK, Wilhelm S, & Geller DA (2018). Quality of Life in Children and Youth with Obsessive-Compulsive Disorder. J Child Adolesc Psychopharmacol, 28(2), 104–110. doi: 10.1089/cap.2017.0091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Wilhelm S, Sprich S, Henin A, Micco J, Small BJ, . . . Geller DA (2016). Efficacy of Augmentation of Cognitive Behavior Therapy With Weight-Adjusted d-Cycloserine vs Placebo in Pediatric Obsessive-Compulsive Disorder: A Randomized Clinical Trial. JAMA psychiatry, 73(8), 779–788. doi: 10.1001/jamapsychiatry.2016.1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibi L, van Oppen P, van Balkom AJLM, Eikelenboom M, Rickelt J, Schruers KRJ, & Anholt GE (2017). The long-term association of OCD and depression and its moderators: A four-year follow up study in a large clinical sample. Eur Psychiatry, 44, 76–82. doi: 10.1016/j.eurpsy.2017.03.009 [DOI] [PubMed] [Google Scholar]
- Tofighi D, & MacKinnon DP (2011). RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods, 43(3), 692–700. doi: 10.3758/s13428-011-0076-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang LP, & Maxwell S. E. J. P. m. (2015). On disaggregating between-person and within-person effects with longitudinal data using multilevel models. 20(1), 63. [DOI] [PubMed] [Google Scholar]
- Wechsler D (1999). Manual for the Wechsler abbreviated scale of intelligence. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Wilhelm S, Berman N, Small BJ, Porth R, Storch EA, & Geller D (2018). D-Cycloserine augmentation of cognitive behavior therapy for pediatric OCD: Predictors and moderators of outcome. J Affect Disord, 241, 454–460. doi: 10.1016/j.jad.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandberg LJ, Zang Y, McLean CP, Yeh R, Simpson HB, & Foa EB (2015). Change in obsessive-compulsive symptoms mediates subsequent change in depressive symptoms during exposure and response prevention. Behav Res Ther, 68, 76–81. doi: 10.1016/j.brat.2015.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zohar AH (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics, 8(3), 445–460. [PubMed] [Google Scholar]


