Abstract
Purpose
To report the case of an immunocompetent 62-year old woman with acute syphilitic posterior placoid chorioretinitis.
Observations
The patient presented with sudden, painless vision loss in the left eye (OS) four months after self-resolving decreased vision in the right eye (OD) which was incorrectly attributed to ischemic optic neuropathy. At the time of presentation, visual acuity (VA) was hand motion OS and 20/30 OD. The dilated fundus exam demonstrated a flat, yellow-white macular lesion, deep to the retinal vasculature with a temporal, curvilinear demarcation line OS and was unremarkable OD. Trace vitreous cells and veils OS were observed. Optical coherence tomography demonstrated loss of photoreceptor layers. Rapid plasma reagin and fluorescent treponemal antibody absorption were positive. The patient was treated with intravenous penicillin and prednisolone acetate drops with resolution of vitreous cells and return of VA.
Conclusions and Importance
Acute syphilitic posterior placoid chorioretinitis can be the single presenting symptom in syphilis. It is imperative for ophthalmologists to consider this relatively uncommon manifestation of syphilis in the differential in immunocompetent patients presenting with unsuspecting histories and perplexing vision loss.
Keywords: Ocular syphilis, Retina, Treponema pallidum, Masquerade conditions, Vision loss
1. Introduction
Syphilis, a multiorgan infectious process, can lead to progressive vision loss when there is ocular involvement. Its presentation lacks uniformity, spans a variety of physical manifestations, produces a variety of symptoms, and mimics other disease.1,2 The various presentations may lead to misdiagnoses and delays in treatment resulting in long-term or permanent vision loss for patients. This delay is becoming increasingly relevant as the incidence of ocular syphilis continues to rise.3
Ocular syphilis has been extensively described in the immunocompromised patient, as 33% of individuals with HIV who are co-infected with neurosyphilis present with ocular manifestations.4 Additionally, patients who are HIV positive often exhibit more severe symptoms that are bilateral.5 This research has allowed ophthalmologists to have a higher index of suspicion for ocular syphilis when a patient who is HIV positive presents with posterior placoid chorioretinitis, necrotising retinitis, or interstitial keratitis. By identifying ocular syphilis early, potentially harmful interventions (e.g. administration of steroids) and permanent damage can be avoided.
There is less information on ocular syphilis in the immunocompetent patient as it may present in subtler forms.6 In turn, research is now attempting to characterize ocular syphilis in immunocompetent patients. This report discusses a case of ocular syphilis in an immunocompetent patient with no suspecting history, the steps necessary to appropriately diagnose the condition, and the appropriate course of action.
2. Case report
A 62-year-old female presented with a five-day history of sudden vision loss in the left eye (OS). Visual acuity (VA) was hand motion OS and 20/30 in the right eye (OD). There was no afferent pupillary defect. The dilated fundus exam demonstrated a flat, yellow-white macular lesion, deep to the retinal vasculature with a temporal, curvilinear demarcation line OS and was unremarkable OD (Fig. 1A). Optical coherence tomography (OCT) revealed loss of the ellipsoid zone OS (Fig. 1B).
Fig. 1A.
Fundus photograph of the left eye demonstrating placoid lesion localized to macula.
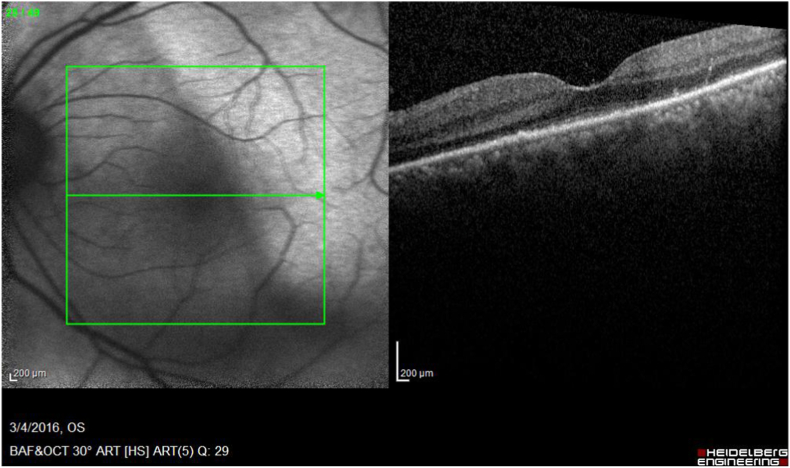
Fig. 1B.
Left eye optical coherence tomography: Subfoveal thickening and nodularity of the retinal pigment epithelium with disruption of the adjacent photoreceptor inner segment-outer segment junction.
At one-week follow-up, the patient's VA was 20/30 and 20/150. The macular yellow-white placoid lesion persisted and OCT continued to demonstrate loss of photoreceptor layers. However, OS now exhibited trace vitreous cells and veils. Macular ischemia was absent on fluorescein angiography, but leakage of the temporal macular vessels and late hyperfluorescence of the disc were noted (Fig. 2). Rapid plasma reagin (RPR) was reactive and the fluorescent treponemal antibody absorption indicated a positive titer. The patient's cerebral spinal fluid tested positive for RPR and she tested negative for HIV. The patient was hospitalized for treatment with intravenous penicillin G. Within 10 days of receiving penicillin G, the patient's VA returned to 20/30 OU. At follow-up, OCT revealed restoration of the ellipsoid zone, suggesting a temporary physiologic impairment of photoreceptor function by the disease process. The patient was prescribed prednisolone acetate, one drop four times daily for mild vitritis OS. At one-month follow-up, the patient had resolution of vitreous cells and prednisolone acetate was tapered.
Fig. 2.
Late-staining hyperfluorescence at the disc and temporal arcade seen on fluorescein. Image taken at follow-up and vision was 20/150 with vitreous cells.
Four months prior to presentation, she had experienced subacute central cloudiness of vision of the right eye. Per outside records, the best corrected visual acuity (BCVA) at that time was 20/60 OD and 20/20 OS. Right sided central visual field loss and decreased color vision were noted. Examination of the right eye showed drusenoid macular changes without visible optic nerve findings. The patient was diagnosed with ischemic optic neuropathy and had gradual spontaneous improvement in right eye vision. Visual evoked potential test three months later revealed normal high-contrast response and abnormal low-contrast response of both eyes (OU).
3. Discussion
Syphilis is an infectious disease caused by the spirochete Treponema pallidum. Known as the great masquerader of ocular diseases, diagnosis of ocular syphilis can be clinically challenging as the disease manifests with a multitude of symptoms and severity. Ocular involvement may be the only presenting sign of syphilis and can occur at any stage of the disease.7 The patient presented with acute syphilitic posterior placoid chorioretinitis (ASPPC), a disease first described in 1990.8 ASPPC often presents with yellowish placoid lesions in the posterior pole or mid-periphery of the fundus. This lesion typically includes a faded center and stippled hyperpigmentation of the retinal pigment epithelium (RPE) and can coalesce into large confluent lesions.9 It can be associated with vitreous inflammation, hemorrhages, retinal vasculitis, disc edema and serous detachment of the RPE.10 Increased retinal thickness and subretinal fluid on OCT, and disruption of ellipsoid zone and the external limiting membrane have also been reported.6,7 Placoid lesions of ASPPC are theorized to result from an active inflammatory reaction at the level of choriocapillaris-RPE-retinal photoreceptor complex.11 ASPPC is most commonly reported in immune-compromised individuals, with human immunodeficiency virus (HIV) co-infection in 56.3% of ASPPC patients.12
4. Conclusion
In this patient, the lack of a retinal lesion on initial presentation, absent systemic symptoms, and spontaneous improvement of vision OD, led to a provisional diagnosis of ischemic optic neuropathy, delaying the diagnosis and treatment of syphilis. The spontaneous resolution may represent the immunological reaction of the patient to syphilis.11 To diagnose and manage this condition, lumbar puncture and HIV testing are recommended as immune-compromised patients may have accelerated presentation of neurosyphilis.10 Treatment consists of intravenous penicillin and intravenous corticosteroid taper over a period of one month. Intraocular corticosteroids with active syphilitic uveitis are contraindicated.7 Visual prognosis is favorable with prompt antibiotic treatment. As ASPPC can be the presenting symptom in syphilis, it is imperative for ophthalmologists to consider this uncommon manifestation of syphilis in the differential to ensure adequate and timely treatment of this condition, particularly in the immunocompetent patient as it occurs less commonly and may present in subtler forms.
Patient consent
Written consent from the patient was obtained for publication of this report.
Declaration of competing interest
The authors declared that they have no conflicts of interest.
Acknowledgments and Disclosures
The authors declared that they have no conflicts of interest.
References
- 1.Russell J.F., Pichi F., Scott N.L., Hartley M.J. Masqueraders of multiple evanescent white dot syndrome (MEWDS) Int Ophthalmol. 2020;40(3):627. doi: 10.1007/s10792-019-01223-4. [DOI] [PubMed] [Google Scholar]
- 2.Klein A., Fischer N., Goldstein M., Shulman S., Habot‐Wilner Z. The great imitator on the rise: ocular and optic nerve manifestations in patients with newly diagnosed syphilis. Acta Ophthalmol (Copenh) 2019;97(4):e641–e647. doi: 10.1111/aos.13963. [DOI] [PubMed] [Google Scholar]
- 3.Lin P. Infectious Uveitis. Curr Ophthalmol Rep. 2015;3(3):170–183. doi: 10.1007/s40135-015-0076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz D.A., Berger J.R., Duncan R.C. Neurosyphilis. A comparative study of the effects of infection with human immunodeficiency virus. Arch Neurol. 1993;50(3):243–249. doi: 10.1001/archneur.1993.00540030009006. [DOI] [PubMed] [Google Scholar]
- 5.Moramarco A., Mallone F., Pirraglia M.P., Bruscolini A. Clinical features of ocular syphilis: a retrospective clinical study in an Italian referral centre. Semin Ophthalmol. 2020;35(1):50. doi: 10.1080/08820538.2020.1723651. [DOI] [PubMed] [Google Scholar]
- 6.Joseph A., Rogers S., Browning A., et al. Syphilitic acute posterior placoid chorioretinitis in nonimmuno-compromised patients. Eye Lond Engl. 2007;21(8):1114–1119. doi: 10.1038/sj.eye.6702504. [DOI] [PubMed] [Google Scholar]
- 7.Brito P., Penas S., Carneiro Â., Palmares J., Reis F.F. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: the role of autoimmune response in pathogenesis. Case Rep Ophthalmol. 2011;2(1):39–44. doi: 10.1159/000324086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gass J.D., Braunstein R.A., Chenoweth R.G. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):1288–1297. doi: 10.1016/s0161-6420(90)32418-1. [DOI] [PubMed] [Google Scholar]
- 9.Kiss S., Damico F.M., Young L.H. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005;20(3):161–167. doi: 10.1080/08820530500232092. [DOI] [PubMed] [Google Scholar]
- 10.Aldave A.J., King J.A., Cunningham E.T. Ocular syphilis. Curr Opin Ophthalmol. 2001;12(6):433–441. doi: 10.1097/00055735-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Zamani M., Garfinkel R.A. Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2003;135(6):891–894. doi: 10.1016/s0002-9394(02)02160-8. [DOI] [PubMed] [Google Scholar]
- 12.Eandi C.M., Neri P., Adelman R.A., Yannuzzi L.A., Cunningham E.T., International Syphilis Study Group Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina Phila Pa. 2012;32(9):1915–1941. doi: 10.1097/IAE.0b013e31825f3851. [DOI] [PubMed] [Google Scholar]