Abstract
Purpose
To describe a case of bilateral pseudophakic malignant glaucoma treated with a new variant of irido-zonulo-hyaloid-vitrectomy.
Observations
A patient who developed refractory bilateral pseudophakic malignant glaucoma underwent an irido-zonulo-hyaloid-vitrectomy via the anterior chamber in both eyes, one 2-months apart from the other. The procedure involved the use of an 18 Gauge needle to perform a straight vertical irido-zonulo-hyaloidotomy and a 25 Gauge vitreous cutter to complete the vitrectomy. The intraocular pressure was recorded on day 1, day 7, day 14, then monthly until 6 months postoperatively, whereas an ultrasound biomicroscopy of the anterior chamber was performed on day 1 and 6 months after the operation. The malignant glaucoma resolved in both eyes with no intra- nor post-operative complications. At 6 months from the surgeries none of the eyes developed recurrences.
Conclusions
The new variant of irido-zonulo-hyaloid-vitrectomy we propose for the management of refractory pseudophakic malignant glaucoma resulted to be a safe and effective technique.
Keywords: Malignant glaucoma, Aqueous misdirection, Ciliary block glaucoma, Irido-zonulo-hyaloidotomy, Anterior vitrectomy
1. Introduction
The term “malignant” glaucoma was introduced by Von Graefe back in 1869 to describe a form of glaucoma that was resistant to any of the treatments known at that time.1 Since then, many medical (i.e., cycloplegics, aqueous suppressants, hyper osmotic agents), and surgical options have been described with varying results, and today, even though the exact pathogenesis of this disease is not fully understood, this condition is also referred to as ciliary block glaucoma or aqueous misdirection syndrome. Indeed, a forward movement of the lens-iris-diaphragm due to an over hydration of the vitreous is thought to be one major causative mechanism of the disease.2
After the first-line medical managements fail, a surgical approach aiming at creating a communication between the posterior and the anterior segment of the eye is usually needed. An alternative would be the creation of this communication using a laser (i.e., laser irido-capsulo-hyaloidotomy), however, this is not always feasible.
Through the years, various surgical approaches have been described. These include pars plana vitrectomy,3 vitrectomy-phacoemuslification-vitrectomy in phakic eyes,4 vitrectomy with hyaloid-zonulectomy and peripheral iridectomy,5 and vitrectomy with insertion of a glaucoma drainage device.6
Herein, we describe a case of bilateral malignant glaucoma occurring after phacoemulsification and intraocular lens (IOL) implantation surgery that was treated with a variant to the usually adopted surgical approaches.
2. Methods
A 44-year-old female hyperopic patient with bilateral pseudophakic malignant glaucoma that was resistant to the previously described medical therapies, underwent an irido-zonulo-hyloidectomy and vitrectomy in both eyes separately, at the University Hospital of Verona, Italy.
The patient had a history of bilateral angle closure glaucoma and had already undergone bilateral iridotomies and phacoemulsification and IOL implantation, in both eyes, approximately 3 months before. The two clear lens extraction surgeries were performed 10 days apart from each other and were uneventful. Except for the anterior chamber (AC) being described as to be somewhat shallower than normal in the right eye (the second eye that had been treated), the rest of the findings (including the intraocular pressure - IOP) on the first day after the procedures, were normal in both eyes. Four weeks after the first clear lens extraction, the patient presented at our department with bilateral vision loss (i.e., uncorrected visual acuity of 0.4 logMAR in both eyes), a bilateral myopic shift (i.e., from −0.25 Diopters after the cataract surgery, to −3.00 Diopters), a high IOP (28 mmHg in the right eye and 19 mmHg in the left) and a diffusely shallow AC without any ongoing posterior chamber pathologies, again in both eyes. Her iridotomies were patent and an ultrasound biomicroscopy (UBM) demonstrated bilateral anterior rotation of the ciliary body with subsequent anterior displacement of the lens-iris-diaphragm and AC shallowing. Therefore, a diagnosis of bilateral malignant glaucoma was made. The surgical procedure was performed in both eyes, once the written informed consent had been signed, after the medical treatment had failed. The latter consisted of topical cyclopentolate t.i.d., timolol + dorzolamide b.i.d., dexamethasone q.i.d. and oral acetazolamide, 250mg q.d. After the procedures, the patient was visited one, seven and fourteen days postoperatively. Thereafter she received a monthly follow up-visit for 6 months. Visual acuity and IOP were recorded at each visit, whereas an UBM was performed on day 1 and 6 months after the operation.
2.1. Surgical technique
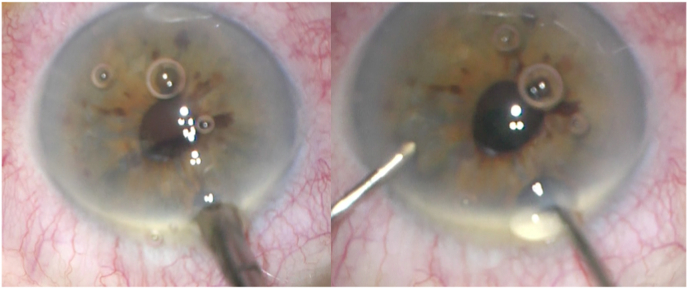
The surgeon (R.T.) performed two peripheral corneal tunnels: one above the previous iridotomy (i.e., 10 o'clock in the right eye and 2 o'clock in the left eye) and the other, two clock hours away, nasally. The former was used to introduce an 18 Gauge needle in the AC, whereas the latter would have been needed later to place an AC infusion cannula during the successive anterior vitrectomy. After the corneal tunnels were completed, the needle was introduced in the AC and was then passed vertically through the iridotomy and through the underlying zonule and anterior hyaloid, taking care to direct it toward the center of the eye rather than its periphery, safeguarding the retina and the ciliary processes (Fig. 1).
Fig. 1.
On the left-hand side, the 18 Gauge needle is being introduced in the AC and through the zonule, into the vitreous cavity. On the right-hand side an anterior vitrectomy is being performed while an infusion cannula is being held in the AC.
After that, a 25 Gauge vitreous cutter was introduced through the same structures as the needle and was used to perform an anterior vitrectomy (Fig. 1). This way, a guarded pathway between the vitreous cavity and the anterior chamber was secured. At the end of the surgery, a 10-0 Nylon stich was placed on the main incision to prevent any possible leakage from the AC.
3. Results
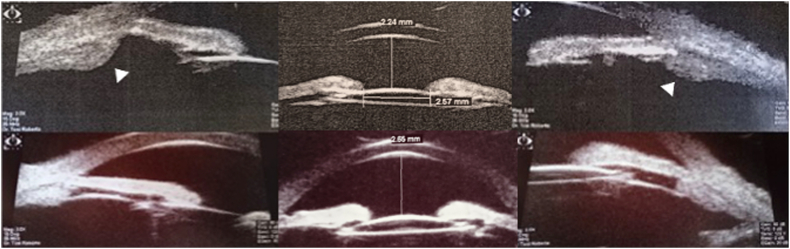
At the moment the anterior vitrectomy had been performed, we observed a widening of the AC. Indeed, the day following the procedure the patient's refractive error went back to 0 Diopters in one eye and −0.75 Diopters in the other, and the AC angle resulted to be opened on UBM (Fig. 2). No complications occurred during, nor after the procedure. Particularly, no malignant glaucoma recurrence was observed.
Fig. 2.
Preoperative (left eye and right eye respectively on the upper left and right corners; right eye in the center) and postoperative (left eye and right eye respectively on the lower left and right corners; right eye in the center) UBMs. Arrowheads point at the anteriorly displaced ciliary body.
The day following the procedures, the untreated IOP was 20 mmHg and 16 mmHg, respectively in the right and in the left eye. These values went down to- and were stable at 14–15 mmHg in both eyes, from 14 days postoperatively, on to the last follow-up visit (i.e., 6 months after the surgery). The final best corrected visual acuity was 0.0 logMAR in both eyes, with a correction of −0.50 sphere in the left eye and no correction in the right one.
4. Discussion
Even though the exact physiopathology of malignant glaucoma is still debated, there seems to be a consensus about the nature of its management.7 In fact, whether the AC shallowing derives from a posterior diversion of aqueous flow,8 a concomitant laxity of the lens zonules,9 or a choroidal expansion,10 the establishment of a continuous communication between the posterior and the anterior segment of the eye is still necessary. This can be achieved with various approaches, each of which has its drawbacks. Neodymium-doped yttrium aluminum garnet (Nd:YAG) lasering of the anterior hyaloid is a non-invasive, reasonable option, however, it is not always easy to detect the targeted structures and it may be difficult to perform through small previous iridotomies (such as those in our patient). Pars plana vitrectomy has also been previously advocated to resolve cases of malignant glaucoma. This technique has shown to have high success rates in the past,11 however, it is an invasive technique that requires some experience in vitreoretinal surgery, and has the downside of creating some subconjunctival scarring. This could jeopardize future filtering surgeries these patients might need.
The technique we propose is very similar to that used by Lois et al.,5 the major difference being that we used an 18 Gauge needle previous to the vitreous cutter. As the authors stated in their study, when performing a zonulectomy through the AC, it is mandatory to avoid the excision of larger parts of the lens zonule. In fact, this could lead to IOL instability, and possibly to IOL luxation. By creating a path with a non-aspirating, but sharp and pointed instrument, such as a needle, the chances of damaging larger portions of the zonule decrease. Moreover, by using a needle to enlarge or to create an iridotomy, one reduces the likelihood of bleeding from the iris. Since the vitreous cutter has the working end on its side, rather than on its apex, one needs to tilt the instrument when working with it. This might not be as comfortable as using the instruments in a straight vertical fashion, and might lead to difficulties in the creation of a symmetric pathway through the iris, the zonule and the anterior hyaloid. While extending the operative times only by a few minutes compared to an irido-zonulo-hyloid-vitrectomy performed using a vitreous cutter only technique, this technique resulted to be effective in both of the patient's eyes.
To be fair, it must be specified that all the above are assumptions based on the experience of our glaucoma clinic, and that other surgeons might experience different results using the technique we propose. As an example, one might experience bleeding when passing the needle through the iris. Nonetheless, the purpose of this study is to propose a new surgical variant. Comparing the results of two or more techniques is beyond the scopes of this study.
This is not the first time a needle has been adopted to solve a case of malignant glaucoma. Indeed, there are several other reports of irido-zonulo-hyaloidectomies being performed with needles of various sizes.12, 13, 14 Nevertheless, these had all been performed at the slit lamp and did not involve a concomitant anterior vitrectomy, which we feel like being fundamental for the durability of the procedure's results.
Even though we report the results of this new approach only on two eyes, and the follow-up period is limited to 6 months, we feel like this study could inspire future larger randomized studies in order to better understand which of the present surgical managements of malignant glaucoma is the more effective.
5. Conclusions
The new variant of irido-zonulo-hyaloid-vitrectomy we propose for the management of refractory pseudophakic malignant glaucoma resulted to be a safe and effective technique. Given the lack of guidelines on the surgical management of malignant glaucoma, prospective randomized studies would be required, even though the relative rarity of this entity makes such studies difficult to complete.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Patient consent
A written informed consent to publish this case report has been obtained from the patient. This report does not contain any personal identifying information.
Declaration of competing interest
None of the authors has any conflicting interest.
Acknowledgements
None.
References
- 1.von Graefe A. Beiträge zur pathologie und therapie des glaukoms. Arch Ophthalmol. 1869;15(108) [Google Scholar]
- 2.Shahid H., Salmon J.F. Malignant glaucoma: a review of the modern literature. J Ophthalmol. 2012;2012 doi: 10.1155/2012/852659. Epub 2012 Mar 27. PMID: 22545204; PMCID: PMC3321564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch M.G., Brown R.H., Michels R.G., Pollack I.P., Stark W.J. Surgical vitrectomy for pseudophakic malignant glaucoma. Am J Ophthalmol. 1986 Aug 15;102(2):149–153. doi: 10.1016/0002-9394(86)90135-2. PMID: 3740172. [DOI] [PubMed] [Google Scholar]
- 4.Debrouwere V., Stalmans P., Van Calster J., Spileers W., Zeyen T., Stalmans I. Outcomes of different management options for malignant glaucoma: a retrospective study. Graefes Arch Clin Exp Ophthalmol. 2012 Jan;250(1):131–141. doi: 10.1007/s00417-011-1763-0. Epub 2011 Aug 20. PMID: 21858468. [DOI] [PubMed] [Google Scholar]
- 5.Lois N., Wong D., Groenewald C. New surgical approach in the management of pseudophakic malignant glaucoma. Ophthalmology. 2001 Apr;108(4):780–783. doi: 10.1016/s0161-6420(00)00642-4. PMID: 11297497. [DOI] [PubMed] [Google Scholar]
- 6.Azuara-Blanco A., Katz L.J., Gandham S.B., Spaeth G.L. Pars plana tube insertion of aqueous shunt with vitrectomy in malignant glaucoma. Arch Ophthalmol. 1998 Jun;116(6):808–810. doi: 10.1001/archopht.116.6.808.PMID:9639455. [DOI] [PubMed] [Google Scholar]
- 7.Balekudaru S., Choudhari N.S., Rewri P., et al. Surgical management of malignant glaucoma: a retrospective analysis of fifty eight eyes. Eye. 2017 Jun;31(6):947–955. doi: 10.1038/eye.2017.32. Epub 2017 Mar 3. PMID: 28257136; PMCID: PMC5518837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaffer R.N. The role of vitreous detachment in aphakic and malignant glaucoma. Trans Am Acad Ophthalmol Otolaryngol. 1954 Mar-Apr;58(2):217–231. PMID: 13157051. [PubMed] [Google Scholar]
- 9.Chandler P.A. Malignant glaucoma. Am J Ophthalmol. 1951 Jul;34(7):993–1000. doi: 10.1016/0002-9394(51)91168-3. PMID: 14846865. [DOI] [PubMed] [Google Scholar]
- 10.Quigley H.A., Friedman D.S., Congdon N.G. Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma. 2003 Apr;12(2):167–180. doi: 10.1097/00061198-200304000-00013. PMID: 12671473. [DOI] [PubMed] [Google Scholar]
- 11.Byrnes G.A., Leen M.M., Wong T.P., Benson W.E. Vitrectomy for ciliary block (malignant) glaucoma. Ophthalmology. 1995 Sep;102(9):1308–1311. doi: 10.1016/s0161-6420(95)30870-6.PMID:9097767. [DOI] [PubMed] [Google Scholar]
- 12.Mardelli P.G., Mardelli M.E. Slit-lamp needling of the anterior capsule for aqueous misdirection after hyaloido-zonulectomy and iridectomy. J Glaucoma. 2018 Apr;27(4):e77–e79. doi: 10.1097/IJG.0000000000000877. PMID: 29329140. [DOI] [PubMed] [Google Scholar]
- 13.Francis B.A., Wong R.M., Minckler D.S. Slit-lamp needle revision for aqueous misdirection after trabeculectomy. J Glaucoma. 2002 Jun;11(3):183–188. doi: 10.1097/00061198-200206000-00004. PMID: 12140393. [DOI] [PubMed] [Google Scholar]
- 14.Thomas M., Boese E.A., Lieu P., Shah M. Slit-lamp pars plana needle hyaloidotomy-zonulotomy-iridotomy for the treatment of spontaneous malignant glaucoma. J Glaucoma. 2020 May;29(5):e31–e32. doi: 10.1097/IJG.0000000000001473. PMID: 32097257. [DOI] [PubMed] [Google Scholar]