Abstract
Background
Despite the associated health risks of self-medication during pregnancy, recent evidence suggests that the phenomena persist in most countries. However, self-medication during pregnancy in Ghana is poorly understood due to the lack of a comprehensive review study.
Objectives
We sought to review existing literature on the prevalence of self-medication, drugs used in self-medication, diseases associated with self-medication, and why pregnant women in Ghana self-medicate.
Methods
A comprehensive search was conducted in PubMed, Science Direct, African Journal Online (AJOL), Google Scholar, and the websites of Ghanaian universities to identify studies that were published until February 2022. We performed this review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A random-effects meta-analysis was done in StatsDirect statistical software and OpenMeta [Analyst] to estimate the prevalence of self-medication during pregnancy and was reported in a forest plot. Simple charts and tables were used to summarize evidence on drugs used in self-medication, diseases associated with self-medication, and reasons for self-medication.
Results
Six (6) studies met our inclusion criteria and the pooled prevalence of self-medication during pregnancy was 65.4% (95% CI = 58.2%–72.6%; I2 = 88.32%; p < 0.001). Common drugs used for self-medication included analgesics (48.1%) and herbal drugs (45.9%). Headache and lower abdominal pain were the most common conditions for which pregnant women self-medicated. The main reasons for self-medication were the perceived unserious nature of diseases, previous experience with drugs, and easy access to over-the-counter drugs.
Conclusions
Self-medication among pregnant women in Ghana is substantially high. Measures need to be implemented to reduce the high prevalence of self-medication during pregnancy to achieve sustainable development goals on maternal health in Ghana. A limitation of this study was the small number of included studies, which calls for more studies on self-medication during pregnancy in Ghana.
Keywords: Self-medication, Pregnant women, Systematic review, Meta-analysis, Ghana
Self-medication; Pregnant women; Systematic review; Meta-analysis; Ghana.
1. Introduction
The issue of self-medication has gained significant attention in recent decades as a phenomenon of global public health interest (Alhomoud et al., 2017; Arikpo et al., 2010; Ramay et al., 2015). Self-medication is usually the initial health-seeking behavior for most people with most illness conditions, making it a common practice worldwide (Rahman et al., 2008). The World Health Organization (WHO) defined self-medication as the treatment of self-recognized ailments or symptoms with medications without the prescription of a qualified health professional or the intermittent/continued use of drugs previously prescribed by a health professional for chronic or recurring disorders (WHO, 2000).
Self-medication has several advantages if practiced with the required knowledge and health orientation (Yeika et al., 2021). Specifically, self-medication reduces pressure on healthcare systems, decreases time spent by patients seeking care, and reduces costs (Alhomoud et al., 2017; Ayalew, 2017; Bennadi, 2013). However, if not practiced appropriately, self-medication could lead to a waste of medical resources and severe health complications (Amaha et al., 2019; Ruiz, 2010; Shafie and Eyasu, 2018).
Among pregnant women, self-medication could have severe health ramifications for the mother and the unborn child (Botchwey et al., 2022). For instance, self-medication is linked to fetal death, neonatal morbidity, and maternal death (Oluwakemi et al., 2016). Moreover, the safety of several commonly used medicines for pregnant women is unknown since clinical trials do not usually include pregnant women as participants (Smolina et al., 2015). Also, self-medication is a known predictor of common psychopathological symptoms among pregnant women (Akinnawo et al., 2020). Using untested herbal products as medicines could lead to severe congenital disabilities and fetal malformations (Ameade et al., 2018).
Despite the associated health risks of self-medication during pregnancy, recent evidence suggests that the phenomena persist in most countries. A recent global study, for instance, found the pooled prevalence of self-medication during pregnancy to be 32% (95% CI, 22%–44%) (Mohseni et al., 2018). Another review focused on low and middle-income countries found that self-medication during pregnancy could be as high as 93% (Torres et al., 2019). Additionally, a recent scoping review in sub-Saharan Africa reported that self-medication with over-the-counter analgesics among pregnant women was between 26 and 78% (Kawuma et al., 2021). However, the generalizability of these accounts to Ghana is problematic since these reviews did not include any primary research on self-medication during pregnancy in Ghana.
Although primary studies exist on self-medication during pregnancy in Ghana, research has yet to map the available evidence on the phenomena in Ghana. As a result of this limitation in the literature, our understanding of self-medication during pregnancy in Ghana is notably underdeveloped. Also, despite growing concerns that self-medication during pregnancy limits Ghana’s ability to achieve safe motherhood and sustainable development goals for improved maternal health (Gbagbo and Nkrumah, 2020a; Makam et al., 2021), there is no public health policy on self-medication during pregnancy in the country. Therefore, we aimed to map the available evidence on the prevalence of self-medication, drugs used in self-medication, diseases associated with self-medication, and reasons for self-medication among pregnant women in Ghana. This review is necessary to inform local policies and reforms aimed at controlling self-medication during pregnancy and improving maternal health outcomes in Ghana.
2. Methods
2.1. Study design
The present study reviews prevalence studies on self-medication among pregnant women in Ghana. The review is not associated with a registered protocol and was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., 2021).
2.2. Search strategy
PubMed, Science Direct, and African Journals Online (AJOL) databases were used to identify primary studies published until February 2022. Additionally, Google Scholar was used to perform a confirmatory search to ensure no primary studies were missed. To identify grey literature, we searched the digital collections of the Kwame Nkrumah University of Science and Technology, the University of Ghana, and the University of Development Studies. The strategies for the search have been presented in Table 1. The reference lists of the included records were manually inspected for additional studies. The first author did the last search for studies on 28 February 2022 (21:17 GMT).
Table 1.
Search strategies.
| PubMed | ||
|---|---|---|
| Step | Search query | Results |
| #1 | ((((self-medication[Title/Abstract]) OR (nonprescription drug[Title/Abstract])) OR (over-the-counter drug [Title/Abstract])) OR (OTC drug[Title/Abstract])) OR (home remedies [Title/Abstract])) OR (herbal medication[Title/Abstract])) OR (herbal drug[Title/Abstract])) AND (Ghana[Title/Abstract]) | 42 |
| #2 | ((((pregnant women[Title/Abstract]) OR (pregnancy[Title/Abstract])) OR (pregnancy[Title/Abstract])) OR (gestation[Title/Abstract])) OR (maternal[Title/Abstract])) AND (Ghana[Title/Abstract]) | 1718 |
| #3 | #1 AND #2 | 17 |
| Science Direct/African Journals Online/Google Scholar | ||
| Search terms | ||
| (self-medication OR nonprescription drug OR over-the-counter drug OR herbal) AND (pregnant women OR pregnancy OR gestation OR maternal) AND Ghana | 139,202 | |
| Digital collections of the University of Ghana, the Kwame Nkrumah University of Science and Technology, and the University of Development Studies. | ||
| Step | Search query | |
| #1 | Self-medication | 14 |
| #2 | Pregnant OR pregnancy | 69 |
| #3 | #1 AND #2 | 1 |
2.3. Inclusion and exclusion criteria
The modified population-intervention-comparison-outcome-context (PICOC) framework was used to establish the eligibility criteria in this review (see Table 2). Studies qualified for inclusion if they reported self-medication among pregnant women in Ghana and provided primary evidence on any of the following: prevalence of self-medication, drugs used in self-medication, diseases associated with self-medication, and reasons for self-medication. Studies were excluded if they did not report primary outcomes, were conducted within a population other than pregnant women, or reported intervention(s) on the use of prescribed medicines among pregnant women.
Table 2.
Framework for determining the eligibility of studies (PICOC).
| Criteria | Description |
|---|---|
| Population | Pregnant women |
| Intervention | Self-medication |
| Comparison | Not applicable in this review |
| Outcome | Prevalence of self-medication, drugs used in self-medication, diseases associated with self-medication, and reasons for self-medication. |
| Context | Ghana |
2.4. Study selection
We followed a robust plan for selecting studies using the already established eligibility criteria. Initially, title screening was conducted in the respective databases, and eligible titles were exported into a Microsoft Excel spreadsheet for further screening. All authors then applied the eligibility criteria for abstract and full-text screening of the studies. All disagreements arising from using the eligibility criteria to select studies were resolved through discussion and consensus.
2.5. Methodological quality and risk of bias assessment
The Mixed Methods Appraisal Tool (MMAT) Version 2018 (Hong et al., 2018) was used to assess the methodological quality of the included studies. The MMAT is used to assess primary studies with various research designs based on a seven-item scale covering the clarity of research questions, representativeness of the sample, and the appropriateness of data collection procedures and analysis. This meant that each study could have a maximum quality score of 7. We interpreted studies with quality scores of 6–7 as having a low risk of bias, 4–5 as having a medium risk of bias, and 1–3 as having a high risk of bias. Since few studies were included in this review, all reviewers assessed the quality of the included studies independently, and the results were brought together in a virtual meeting. All discrepancies during this process were resolved through discussion and consensus.
2.6. Data extraction
Data were extracted using an excel spreadsheet to complete the following information about the selected studies: author and year of publication, sample size, study location, study design/type, study year, and results on the outcomes of interest. Data extraction was done by all authors independently, and the results were brought together in a series of virtual meetings. All disagreements were resolved through discussion and consensus among reviewers.
2.7. Data analysis
The pooled prevalence of self-medication among pregnant women in Ghana was estimated using meta-analytic techniques in StatsDirect statistical software (StatsDirect Ltd., 2013) and OpenMeta [Analyst] (Wallace et al., 2012). A random-effects model (DerSimonian and Laird, 1986) was selected over a fixed-effects models since the assumption of functional equivalence among included studies was violated (Borenstein et al., 2007). Cochran’s Q and the I2 statistics were used to examine heterogeneity among the included studies. The cut-off I2 values of 0%, 25%, 50%, and 75% were interpreted as no, low, moderate, and high heterogeneity, respectively (Bosu and Bosu, 2021). To assess the robustness of our analysis, we conducted a leave-one-out sensitivity analysis (Steichen, 2001) to identify the influence of eliminating each study on the pooled estimate of the prevalence of self-medication.
Additionally, to provide a more comprehensive understanding of the results, a subgroup analysis was conducted using the geographical belt of the study (northern, middle, and coastal). There is a likelihood that the studies included in a meta-analysis would have significant publication bias, which might affect the quantitative analysis (Conti et al., 2019). Therefore we assessed the risk of publication bias using a funnel plot with Egger’s regression test of funnel plot asymmetry (Egger et al., 1997) and the Fail-Safe N statistic (Rosenthal, 1979). All statistical analyses were conducted at a 95% confidence level.
Additionally, to summarize the evidence on drugs used in self-medication and reasons for self-medication, the proportions of respondents answering in the affirmative to the use of a particular drug or a particular reason for self-medication were estimated by simply adding the frequencies across studies and expressing them as a percentage of the total number of respondents engaged in self-medication in the included studies. The common drugs used in self-medication and the reasons for self-medication were presented with simple charts. However, we did not estimate cumulative proportions of diseases associated with self-medication across the studies because one study (Ameade et al., 2018) reported the conditions/symptoms related to self-medication qualitatively. Therefore, the diseases/symptoms identified in each study were summarized separately and reported in a table.
3. Results
3.1. Search results
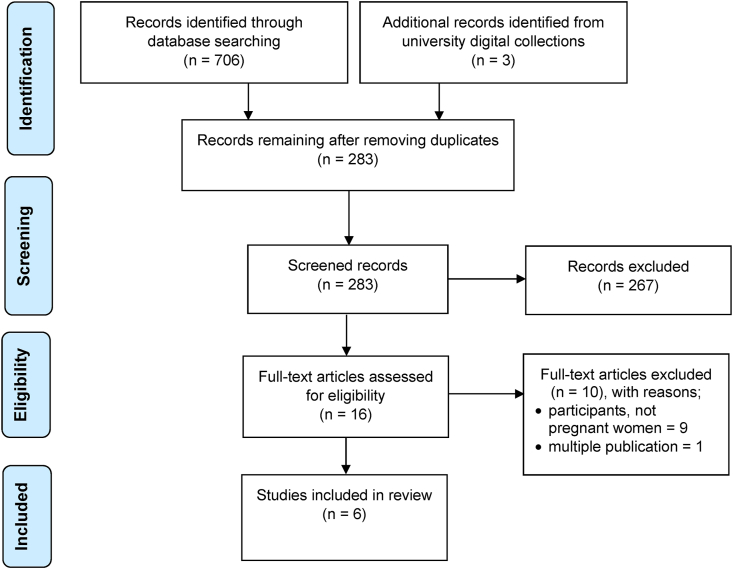
Our robust search for literature through databases and online university collections resulted in 709 papers (see Figure 1). After identifying and removing all duplicate records, 283 articles were screened, and 267 papers that were not relevant for this review were excluded. The full texts of the remaining 16 papers were then assessed for eligibility, and only six (6) qualified for inclusion in the review. The detailed diagrammatic view of the study selection process has been presented on a PRISMA flow chart (see Figure 1).
Figure 1.
PRISMA Flow chart describing the process of selecting reviewed records.
3.2. General characteristics of studies
The characteristics of the included papers have been presented in Table 3. The six studies were conducted in six of the 16 regions in Ghana (i.e., Upper West, Northern, Oti, Volta, Central, and Ashanti Regions). The studies were evenly distributed in the three geographical belts of Ghana, with two studies in each of the coastal belt, middle belt, and northern belt. Five (5) of the included studies (83.3%) were peer-reviewed journal articles, and the remaining one (16.7%) was an unpublished master’s thesis. Three studies had a moderate risk of bias, and another three had a low risk of bias from the methodological quality assessment with the MMAT. The studies were published from 2015 to 2022, with a combined sample size of 1558 pregnant women.
Table 3.
Characteristics of included studies.
| References | Year of Study | Sample size | Prevalence | Age | Region | Geographical zone | Risk of Bias |
|---|---|---|---|---|---|---|---|
| Botchwey et al. (2022) | 2021 | 50 | 68% | 13–49 | OR | Middle belt | Moderate |
| Adama et al. (2021) | 2017 | 367 | 74% | 28.6 ± 4.9 | UWR | Northern belt | Low |
| Makam et al. (2021) | 2018 | 371 | 62% | 27 ± 6.4 | VR | Coastal belt | Moderate |
| Gbagbo and Nkrumah (2020b) | 2018 | 100 | 69% | 29 ± 5.0 | CR | Coastal belt | Low |
| Ameade et al. (2018) | 2017 | 370 | 52.7% | 10–50 | NR | Northern belt | Moderate |
| Agyei-Boateng (2015) | 2015 | 300 | 68.3% | n.s | AR | Middle belt | Low |
Note: OR = Oti Region, UWR = Upper West Region, VR = Volta Region, CR = Central Region, NR = Northern Region, AR = Ashanti Region; n.s = not specified.
3.3. Prevalence of self-medication among pregnant women in Ghana
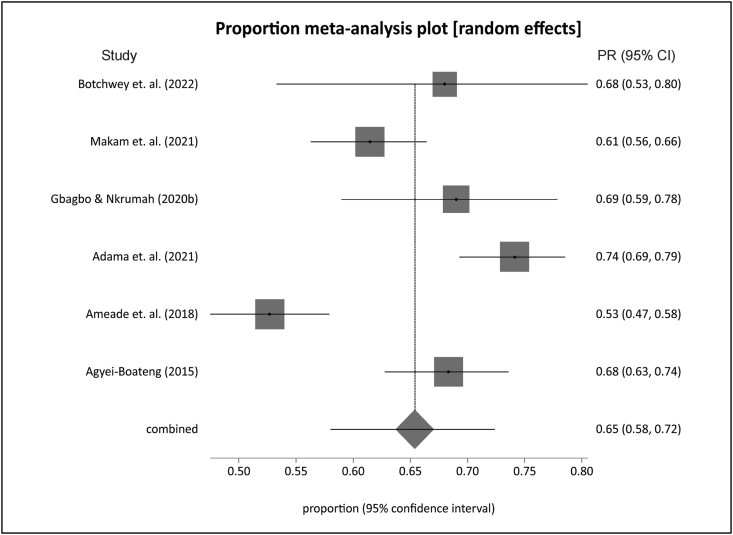
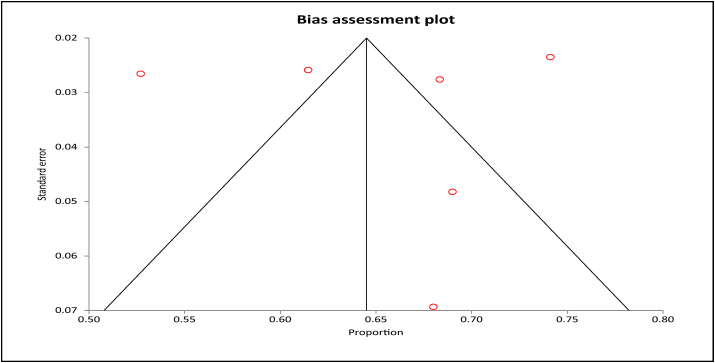
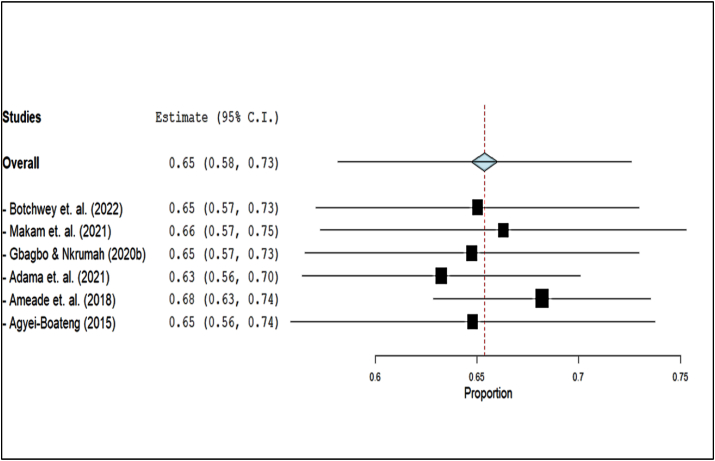
The pooled prevalence of self-medication among pregnant women in Ghana from the six studies was 65.4% (95% CI = 58.2%–72.6%; p < 0.001) (Figure 2). There was high heterogeneity among the studies with Cochran’s Q = 42.79 (d.f = 5) and I2 = 88.32% (p < 0.001). The funnel plot for assessing publication bias was not completely symmetrical for the included studies (Figure 3). However, the Fail-Safe N of 6023 (p < .001) and Egger’s regression test for funnel plot asymmetry (p = 0.717) showed that there was no evidence of publication bias. The results of the sensitivity analysis revealed that the prevalence estimate was dominated by Adama et al. (2021) and Ameade et al. (2018) (see Figure 4). Also, prevalence of self-medication was highest among studies in the middle belt of Ghana with a pooled estimate of 68.3% (95% CI = 63.4%–73.2%; I2 = 0%) followed by the coastal belt with 64.2% (95% CI = 57.1%–71.4%; I2 = 51.2%) and the northern belt with 63.4% (95% CI = 42.5%–84.4%; I2 = 97.39 %) (Table 4).
Figure 2.
Forest plot of prevalence of self-medication during pregnancy in Ghana.
Figure 3.
Funnel plot for assessing publication bias.
Figure 4.
Leave-one-out sensitivity plot of included studies.
Table 4.
Self-medication from studies in the three geopolitical zones of Ghana.
| Zone | Prevalence | p | CI Lower Bound | CI Upper Bound | I2 | p |
|---|---|---|---|---|---|---|
| Middle belt | 68.3% | <.001 | 63.4% | 73.2% | 0.0% | 0.963 |
| Coastal belt | 64.2% | <.001 | 57.1% | 71.4% | 51.2% | 0.152 |
| Northern belt | 63.4% | <.001 | 42.5% | 84.4% | 97.39% | <.001 |
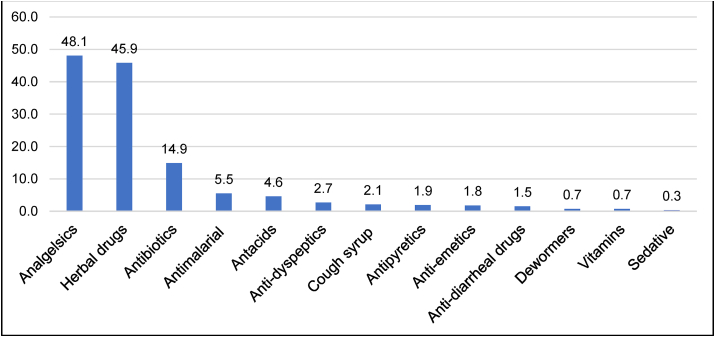
3.4. Drugs used in self-medication during pregnancy
Another important aspect of this review was to map the available literature on the drugs used for self-medication during pregnancy in Ghana. All six studies reported drugs used for self-medication; the results are summarized in Figure 5. From the data in Figure 5, it is apparent that common medications used for self-medication during pregnancy included analgesics (48.1%), herbal drugs (45.9%), antibiotics (14.9%), antimalarial drugs (5.5%), and antacids (4.6%).
Figure 5.
Drugs used in self-medication among pregnant women in Ghana (Percentages).
3.5. Diseases/symptoms associated with self-medication
In Table 5, we presented the diseases/symptoms that warrant self-medication among pregnant women. Five (83.3%) studies presented percentage responses of common conditions/symptoms that warrant self-medication, while Ameade et al. (2018) provided qualitative results. Three out of the five studies that reported proportions had headaches as the most common disease/symptom for pregnant women in Ghana practicing self-medication (Adama et al., 2021; Agyei-Boateng, 2015; Gbagbo and Nkrumah, 2020b). While Botchwey et al. (2022) reported lower abdominal pains (35.3%) as the most common symptom of self-medication, Makam et al. (2021) found anemia (46%) to be the most common disease for which pregnant women self-medicate. Several other diseases/symptoms were reported as conditions for which pregnant women self-medicate, and the details of these conditions can be found in Table 5.
Table 5.
Diseases/symptoms associated with self-medication among pregnant women in Ghana.
| Study | Diseases/Symptoms |
|---|---|
| Botchwey et al. (2022) | Lower abdominal pains (35.3%), malaria (23.5%), headache (17.6%), stomach problems (8.8%), cold and flu (5.9%), sexually transmitted infections (5.9%), and others (2.9%). |
| Ameade et al. (2018) | Nausea, lower abdominal pain, skin rashes, jaundice, blood pressure, malaria, gum bleeding, constipation, cardiovascular conditions such as hypertension, worm, headache, boils, body pain, catarrh, diarrhea infestation, waist pain, piles, blood booster, fever, stomach aches, improve health, loss of appetite, body weakness, edema, for easy delivery. |
| Adama et al. (2021) | Headache (34.2%), upper back pain (33.1%), waist pain (32.7%), lower abdominal pain (20.6%), malaria (16.2%). |
| Makam et al. (2021) | Anemia (46%), headaches (43%), pain (40%), malaria (23%), nausea (14%), cough/fever (10%), diarrhea (6%), dizziness (3%). |
| Gbagbo and Nkrumah (2020b) | Headache (55.2%), lower abdominal pains (17.9%), body pains (11.9%), malaria (9.0%), cold and flu (3.0%), vagina infection (3.0%). |
| Agyei-Boateng (2015) | Headache (44.8%), flu and cold (17.7%), stomach conditions (14.2%), body pains (10.9%), sexually transmitted infections (7.1%), malaria (5.3%). |
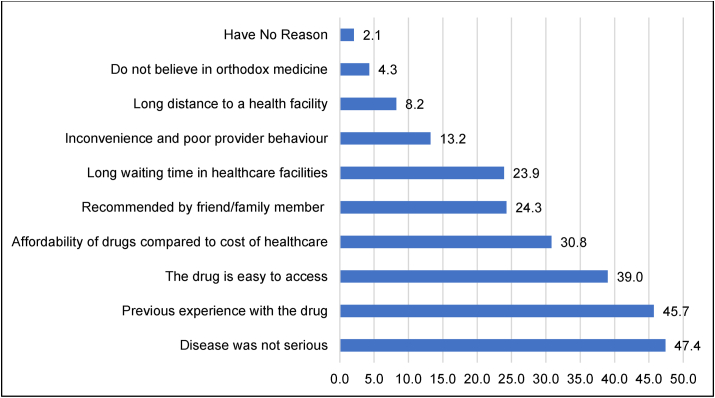
3.6. Reasons for self-medication among pregnant women
Figure 6 shows the reasons why pregnant women self-medicate as health-seeking behavior. Four (66.7%) of the six studies provided reasons pregnant women self-medicate. The cumulative results for the four studies are summarized in Figure 6. From Figure 6, the most common reason pregnant women self-medicate is their perception that diseases/symptoms were not serious (47.4%). Also, previous experience with drugs (45.7%), easy access to medication (39.0%), and affordability of medicines (30.8%) were common reasons for self-medication during pregnancy in Ghana.
Figure 6.
Reasons for self-medication among pregnant women in Ghana (Percentages).
4. Discussion
Self-medication during pregnancy still abounds in several parts of the world, including Ghana (Adanikin and Awoleke, 2017; Botchwey et al., 2022; Mohseni et al., 2018; Oluwakemi et al., 2016). Goal 3 of the sustainable development goals requires that by the year 2030, all nations of the world reduce maternal deaths considerably (UN, 2017). The implications of self-medication during pregnancy on Ghana’s commitment to achieving this global agenda of improving maternal health outcomes have been discussed by previous research (Gbagbo and Nkrumah, 2020a). In this review, we sought to map the evidence available in Ghana to inform public health policy decisions aimed at curbing the phenomena and, thus, improving maternal health outcomes. We included six relevant studies conducted in six of the sixteen regions and all three geographical belts of Ghana.
We estimated 65.4% (95% CI = 58.2%–72.6%; p < 0.001) as the pooled prevalence of self-medication among pregnant women in Ghana. Our pooled prevalence is considerably high compared to the 32% (95% CI, 22%–44%) reported in a global review of self-medication among pregnant women (Mohseni et al., 2018). Also, previous studies among pregnant women in several other countries reported lower rates; 38.46% in Iran (Rahmani et al., 2019), 40% in the United Arab Emirates (Abduelkarem and Mustafa, 2017), 21.9% in Mexico (Alonso-Castro et al., 2018), and 26.6% in Ethiopia (Beyene and Beza, 2018). While these comparisons present a chilling picture of the phenomena in Ghana, it is, however, not entirely surprising since previous reviews reported as high as 93% in some developing countries (Torres et al., 2019) and between 26 and 78% in sub-Saharan Africa (Kawuma et al., 2021).
A possible explanation for the variability in the prevalence of self-medication among pregnant women in different parts of the world might include differences in the robustness of regulations on the use of over-the-counter medications (Abduelkarem and Mustafa, 2017), knowledge of consumers on the consequence of self-medication (Kawuma et al., 2021), marketing and advertisement policies (Ofosu, 2020), and prescription systems (Yeika et al., 2021). In Ghana, for instance, it is easy to access scientific herbal, traditional, and conventional medicines (nonprescribed medicines in general) without a prescription from qualified health personnel (Bonti, 2017; Gbagbo and Nkrumah, 2020b; Kretchy et al., 2021).
Another important finding of this review is that most pregnant women in Ghana self-medicate with analgesics (48.1%) and herbal drugs (45.9%). This finding compares closely to the results of other studies, which reported between 26 and 78% self-medication with over-the-counter analgesics (Kawuma et al., 2021) and 52.7% for herbal products in sub-Saharan Africa (Ameade et al., 2018). These observations can partly be explained by the poor regulatory and enforcement practices, which is a common feature in the operations of pharmacies and drug outlets in sub-Saharan African countries (Meessen et al., 2011; Wafula et al., 2012). However, it is important to note that misuse of over-the-counter analgesics is particularly cited as a global challenge (Cooper, 2013).
In this review, headache and pain (related to the musculoskeletal system) were the most common conditions related to self-medication during pregnancy in Ghana. Medication use for self-diagnosed conditions has been reported as a common practice in most low and middle-income countries (Kawuma et al., 2021; Torres et al., 2019; Wafula et al., 2012). This practice is usually not based on standard practice and professional advice, making it awful health-seeking behavior, especially among vulnerable populations like pregnant women (Torres et al., 2019).
It is worthy to note that the common reasons pregnant women self-medicated are the use of drugs previously used to treat similar conditions/diseases and the perception that some medical conditions/illnesses were not serious to warrant a visit to a healthcare facility. We find these perceptions to be extremely risky since the self-ascribed severity of disease conditions could be underestimated, and the potential adverse effects of a drug used for self-medication could seriously affect the pregnancy. Literature has shown that exposure to particular medications during the first trimester of pregnancy could have devastating consequences on the mother and the unborn child both in the short and long term (Gbagbo and Nkrumah, 2020a). Other impetus for self-medication included easy access to drugs, affordability of medications compared to healthcare costs, and limited access to healthcare. These findings support evidence in the literature that suggests that the free maternal health policy under the National Health Insurance Scheme in Ghana is bewildered with serious implementation and sustainability challenges, limiting access to maternal healthcare (Alhassan et al., 2016; Bonfrer et al., 2016; Mensah et al., 2010; Wang et al., 2017).
4.1. Strengths and limitations of the study
This systematic review is the first to comprehensively map the evidence available on self-medication among pregnant women in Ghana. It is also among the few country-specific reviews in sub-Saharan Africa. Before this study, there was no coherent and comprehensive information on self-medication during pregnancy in Ghana. Our review has contributed to filling this gap. The use of a robust screening procedure, guided by the widely acknowledged PICOC framework for selecting studies, and adherence to the PRISMA checklist gave credence to the study methodology.
Despite the above strengths, this review study has some inherent limitations. Firstly, there is the possibility of bias in the primary studies used for this review since respondents relied on self-recall, with the likelihood of recall bias. Additionally, some primary studies failed to report essential data in forms that will allow further exploration of heterogeneity in the pooled prevalence. Also, the sample for the review was relatively small; therefore, meta-regression analysis was not performed to identify additional sources of heterogeneity. Notwithstanding these limitations, this review has provided relevant and comprehensive information on self-medication among pregnant women, elevating the need to swiftly deploy measures to curb this public health menace in Ghana.
4.2. Implications for research
The findings of this study will guide future research to provide a deep understanding of the practice of self-medication in Ghana. Specifically, future research should focus on the pharmacological effects of drugs used in self-medication during pregnancy on the unborn fetus. Also, research should focus on providing further understanding of the socio-demographic factors associated with self-medication to tailor health promotion efforts among the most vulnerable groups of pregnant women. Additionally, research should investigate the role of male partners in practicing self-medication among pregnant women and how men could be involved in interventions that aim to reduce self-medication during pregnancy.
5. Conclusion
Self-medication among pregnant women in Ghana is substantially high. Pregnant women self-medicate with various conventional and herbal medicines for different health conditions due to a multiplicity of individual, social, and health systems factors. This combination of findings supports the practical recommendation that active steps must be taken to reduce the prevalence of self-medication among pregnant women to achieve sustainable development goals for improved maternal health in Ghana. Such measures should include health education programs integrated into the healthcare delivery system and the country’s formal and informal social and cultural systems. We recommend further that sustainable health promotion and education strategies should draw on the involvement of all key stakeholders to ensure that user-centered outcomes are achieved.
Declarations
Author contribution statement
Richmond Opoku: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Denis Dekugmen Yar; Charles Owusu-Aduomi Botchwey: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We are grateful to the authors of all the primary studies included in this review since, without their timely research outputs, this work would not have been a success.
References
- Abduelkarem A., Mustafa H. Use of over-the-counter medication among pregnant women in Sharjah, United Arab Emirates. J. Pregnancy. 2017 doi: 10.1155/2017/4503793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adama S., Wallace L.J., Arthur J., Kwakye S., Adongo P.B. Self-medication practices of pregnant women attending antenatal clinic in northern Ghana: an analytical cross-sectional study. Afr. J. Reprod. Health. 2021;25(4):89–98. doi: 10.29063/ajrh2021/v25i4.10. [DOI] [PubMed] [Google Scholar]
- Adanikin A., Awoleke J. Antenatal drug consumption: the burden of self-medication in a developing world setting. Trop. Doct. 2017;47:193–197. doi: 10.1177/0049475516653067. [DOI] [PubMed] [Google Scholar]
- Agyei-Boateng R. Kwame Nkrumah University of Science and Technology; 2015. Self-medication Practices Among Pregnant Women in Ejisu-Juaben Municipality in Partial Fulfillments. [Google Scholar]
- Akinnawo E.O., Bello I.B., Akpunne B.C., Ajibola B.S. Self-medication in pregnancy and associated psychopathological symptoms of antenatal Nigerian women. Psychology. 2020;11(12):2039–2054. [Google Scholar]
- Alhassan R.K., Nketiah-Amponsah E., Arhinful D.K. A review of the national health insurance scheme in Ghana: what are the sustainability threats and prospects? PLOS ONE. 2016;11(1) doi: 10.1371/journal.pone.0165151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhomoud F., Aljamea Z., Almahasnah R., Alkhalifah K., Basalelah L., Alhomoud F.K. Self-medication and selfprescription with antibiotics in the Middle East-do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int. J. Infect. Dis. 2017;57:3–12. doi: 10.1016/j.ijid.2017.01.014. [DOI] [PubMed] [Google Scholar]
- Alonso-Castro A., Ruiz-Padilla A., Ruiz-Noa Y., Alba-Betancourt C., Domínguez F., Ibarra-Reynoso L., et al. Self-medication practice in pregnant women from central Mexico. Saudi Pharm. J. 2018;26:886–890. doi: 10.1016/j.jsps.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaha M.H., Alemu B.M., Atomsa G.E. Self-medication practice and associated factors among adult community members of Jigjiga town, Eastern Ethiopia. PloS One. 2019;14 doi: 10.1371/journal.pone.0218772. –e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameade E.P.K., Zakaria A.P., Abubakar L., Sandow R. Herbal medicine usage before and during pregnancy – a study in Northern Ghana. Int. J. Compl. Alternative Med. 2018;11(4):235–242. [Google Scholar]
- Arikpo G.E., Eja M.E., Enyi-Idoh K.H. Self-medication in rural Africa: the Nigerian experience. Int. J. Health. 2010;11(1):1–7. [Google Scholar]
- Ayalew M.B. Self-medication practice in Ethiopia: a systematic review. Patient Prefer. Adher. 2017;11:401–413. doi: 10.2147/PPA.S131496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennadi D. Self-medication: a current challenge. J. Basic Clin. Pharm. 2013;5:19–23. doi: 10.4103/0976-0105.128253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyene K., Beza S. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop. Med. Health. 2018;46(10) doi: 10.1186/s41182-018-0091-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonfrer I., Breebaart L., Poel E. Van De. The effects of Ghana’s national health insurance scheme on maternal and infant health care utilization. PLOS ONE. 2016:1–13. doi: 10.1371/journal.pone.0165623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonti D. The Ohio State University; 2017. Bridging the gap between Self-Medication and Access to Healthcare in Ghana (Doctoral Dissertation) [Google Scholar]
- Borenstein M., Hedges L., Rothstein H. 2007. Meta-analysis: Fixed Effect vs. Random Effects. MEta-Analysis.Com. [DOI] [PubMed] [Google Scholar]
- Bosu W.K., Bosu D.K. Prevalence, awareness and control of hypertension in Ghana: a systematic review and meta-analysis. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0248137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botchwey C.O.-A., Quaye E., Boateng A.A., Aggrey-Bluwey L., Acquah F., Opoku R., Baidoo M.A. Self-medication among pregnant women in the Jasikan district of Ghana. Asian J. Pregnancy Childbirth. 2022;5(1):32–45. [Google Scholar]
- Conti A.A., McLean L., Tolomeo S., Steele J.D., Baldacchino A. Chronic tobacco smoking and neuropsychological impairments: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2019;96:143–154. doi: 10.1016/j.neubiorev.2018.11.017. [DOI] [PubMed] [Google Scholar]
- Cooper R. Over-the-counter medicine abuse - a review of the literature. J. Subst. Use. 2013;18(2):82–107. doi: 10.3109/14659891.2011.615002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey S.G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin. Res. Ed.). 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. Epub 1997/10/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gbagbo F.Y., Nkrumah J. Implications of self-medication in pregnancy for safe motherhood and sustainable development goal-3 in selected Ghanaian communities. Publ. Health Pract. 2020;1 doi: 10.1016/j.puhip.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gbagbo F.Y., Nkrumah J. Self-medication among pregnant women in two municipalities in the Central Region of Ghana. Health Care Women Int. 2020;42(4–6):547–562. doi: 10.1080/07399332.2020.1716235. [DOI] [PubMed] [Google Scholar]
- Hong Q.N., Fàbregues S., Bartlett G., Boardman F., Cargo M., Dagenais P., Gagnon M.P., Griffiths F., Nicolau B., O’Cathain A., Rousseau M.C. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018;34(4):285–291. [Google Scholar]
- Kawuma R., Chimukuche R.S., Francis S.C., Seeley J., Weiss H.A. Knowledge, use (misuse) and perceptions of over- the-counter analgesics in sub-Saharan Africa: a scoping review. Global Health Action. 2021;14(1) doi: 10.1080/16549716.2021.1955476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretchy J.-P., Adase S.K., Gyansa-Lutterodt M. The prevalence and risks of antibiotic self-medication in residents of a rural community in Accra, Ghana. Sci. Afr. 2021;14 [Google Scholar]
- Makam C.E., Adam A., Fusheini A. Self-medication and pregnancy care: the use of herbal products and prescription drugs among pregnant women attending antenatal clinics in Hohoe Municipality of Volta region, Ghana. J. Nurs. Midwifery Res. 2021;1(2):1–8. [Google Scholar]
- Meessen B., Hercot D., Noirhomme M., et al. Removing user fees in the health sector: a review of policy pro cesses in six sub-Saharan African countries. Health Pol. Plann. 2011;26 doi: 10.1093/heapol/czr062. [DOI] [PubMed] [Google Scholar]
- Mensah J., Oppong J.R., Bobi-Barimah K., Frempong G., Sabi W. 2010. An Evaluation of the Ghana National Health Insurance Scheme in the Context of the Health MDGs. Working Paper No. 40. [Google Scholar]
- Mohseni M., Azami-Aghdash S., Gareh S.S., Moosavi A., Nakhaee M., Pournaghi-Azar F., Rezapour A. Prevalence and reasons of self-medication in pregnant women: a systematic review and meta-analysis. IJCBNM. 2018;6(4):272–284. [PMC free article] [PubMed] [Google Scholar]
- Ofosu A.T. University of Ghana; 2020. Channels of Medicinal Advertisements and its Association with Self-Medication Among Adults in Effia-Kwesimintsim Municipality. [Google Scholar]
- Oluwakemi K.A., Tijani A.W., Adeniran D.A. Self-medication practices among pregnant women attending the state hospital, Osogbo, Nigeria. Int. J. Commun. Ment. Health Nurs. 2016;2(1):1–8. [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(n71) doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A.A., Sulaiman S.A., Ahmad Z., Daud W.N.W., Hamid A.M. Prevalence and pattern of use of herbal medicines during pregnancy in Tumpat district, Kelantan. Malays. J. Med. Sci. 2008;15(3):40. [PMC free article] [PubMed] [Google Scholar]
- Rahmani A., Hamanajm S.A., Fallahi A., Gheshlagh R.G., Dalvand S. Prevalence of self-medication among pregnant women: a systematic review and meta-analysis. Nurs. Midwifery Stud. 2019;8:169–175. [Google Scholar]
- Ramay B.M., Lambour P., Ceron A. Comparing antibiotic selfmedication in two socio-economic groups in Guatemala City: a descriptive cross-sectional study. BMC Pharmacol. Toxicol. 2015;16(1):11. doi: 10.1186/s40360-015-0011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979;86(3):638. [Google Scholar]
- Ruiz M.E. Risks of self-medication practices. Curr. Drug Saf. 2010;5:315–323. doi: 10.2174/157488610792245966. [DOI] [PubMed] [Google Scholar]
- Shafie M., Eyasu M. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. Plos One. 2018;13 doi: 10.1371/journal.pone.0194122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolina K., Hanley G., Mintzes B., Oberlander T., Morgan S. Trends and determinants of prescription drug use during pregnancy and postpartum in British Columbia, 2002–2011: a population-based cohort study. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0128312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StatsDirect Ltd. 2013. Proportion Meta-Analysis.http://www.statsdirect.com/help/%0Adefault.htm#meta/analysis/proportion.htm [Google Scholar]
- Steichen T. Boston College Department of Economics; Chestnut Hill, MA, USA: 2001. METANINF: Stata Module to Evaluate Influence of a Single Study in Meta-Analysis Estimation. (EconPapers). [Google Scholar]
- Torres N.F., Chibi B., Middleton L.E., Solomon P., Mashamba-Thompson T.P. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Publ. Health. 2019;168:92–101. doi: 10.1016/j.puhe.2018.11.018. [DOI] [PubMed] [Google Scholar]
- UN, (United Nations) 2017. The Sustainable Development Goals Report. (New York) [Google Scholar]
- Wafula F., Miriti E., Goodman C. Examining characteristics, knowledge and regulatory practices of specialized drug shops in Sub-Saharan Africa: a systematic review of the literature. BMC Health Serv. Res. 2012;12(1):223. doi: 10.1186/1472-6963-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace B.C., Dahabreh I.J., Trikalinos T.A., Lau J., Trow P., Schmid C.H. Closing the gap between methodologists and end-users: R as a computational back-end. J. Stat. Softw. 2012;49(5) [Google Scholar]
- Wang H., Otoo N., Dsane-Selby L. World Bank; Washington, DC: 2017. Ghana National Health Insurance Scheme: Improving Financial Sustainability Based on Expenditure Review. (World Bank Studies). [Google Scholar]
- WHO . WHO; Geneva: 2000. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Selfmedication. [Google Scholar]
- Yeika E.V., Ingelbeen B., Kemah B.-L., Wirsiy F.S., Fomengia J.N., van der Sande M.A.B. Comparative assessment of the prevalence, practices and factors associated with self-medication with antibiotics in Africa. Trop. Med. Int. Health. 2021;26(8):862–881. doi: 10.1111/tmi.13600. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.