Abstract
The pathogenesis of metabolic-associated fatty liver disease (MAFLD) is complex and thought to be dependent on multiple parallel hits on a background of genetic susceptibility. The evidence suggests that MAFLD progression is a dynamic two-way process relating to repetitive bouts of metabolic stress and inflammation interspersed with endogenous anti-inflammatory reparative responses. In MAFLD, excessive hepatic lipid accumulation causes the production of lipotoxins that induce mitochondrial dysfunction, endoplasmic reticular stress, and over production of reactive oxygen species (ROS). Models of MAFLD show marked disruption of mitochondrial function and reduced oxidative capacitance with impact on cellular processes including mitophagy, oxidative phosphorylation, and mitochondrial biogenesis. In excess, ROS modify insulin and innate immune signaling and alter the expression and activity of essential enzymes involved in lipid homeostasis. ROS can also cause direct damage to intracellular structures causing hepatocyte injury and death. In select cases, the use of anti-oxidants and ROS scavengers have been shown to diminish the pro-apoptopic effects of fatty acids. Given this link, endogenous anti-oxidant pathways have been a target of interest, with Nrf2 activation showing a reduction in oxidative stress and inflammation in models of MAFLD. Thyroid hormone receptor β (THRβ) agonists and nuclear peroxisome proliferation-activated receptor (PPAR) family have also gained interest in reducing hepatic lipotoxicity and restoring hepatic function in models of MAFLD. Unfortunately, the true interplay between the clinical and molecular components of MAFLD progression remain only partly understood. Most recently, multiomics-based strategies are being adopted for hypothesis-free analysis of the molecular changes in MAFLD. Transcriptome profiling maps the unique genotype-phenotype associations in MAFLD and with various single-cell transcriptome-based projects underway, there is hope of novel physiological insights to MAFLD progression and uncover therapeutic targets.
Keywords: Fatty liver disease, Metabolic-associated fatty liver disease, Non-alcoholic steatohepatitis, Reactive oxidation species, Oxidative stress
Graphical abstract
Introduction
Metabolic-associated fatty liver disease (MAFLD) is now the most common chronic liver condition worldwide and will soon be the leading indication for liver transplantation.1 MAFLD represents a pathological spectrum of liver injury ranging from simple steatosis to liver fibrosis with an evolutionary course to cirrhosis. Approximately 30% of adults in the general population have MAFLD, 10–20% have steatohepatitis and in these patients, 20–30% go on to develop cirrhosis within 20 years.2
The link between MAFLD development and obesity, insulin resistance and type 2 diabetes mellitus is well established with MAFLD considered a hepatic manifestation of the metabolic syndrome.3 Given the increasing prevalence of these related conditions, the incidence of MAFLD is projected to increase with data suggesting a 56% rise over the next decade.4 Although MAFLD is typically associated with a western lifestyle, data demonstrates a rapid increase in disease burden in developing counties.5
The MAFLD disease continuum has the associated sequelae of end-stage liver disease and hepatocellular carcinoma (HCC).2 Patients with significant fibrosis have a higher risk of detrimental outcomes compared to those with simple steatosis and alarmingly, these patients may develop HCC without progression to cirrhosis first.6,7
MAFLD pathogenesis
The pathogenesis of MAFLD is complex and still not fully understood; it remains a challenge to stratify and identify specific drug targets and currently there are no licensed therapies for its management. The original two hit hypothesis proposed by Day et al8,9 is now largely obsolete having been replaced with the multiple parallel hits hypothesis.
The development of MAFLD is dependent on multiple cumulative insults including a nonmodifiable genetic susceptibility. MAFLD has been shown to be polygenic with the PNPLA3, MBOAT7 and TM6SF2 gene variants identified as predisposing risk for disease development.10 Additional factors which have a putative pathogenic role are excessive dietary intake, products of the microbiota and/or maladaptation to environmental stimuli. The multiple, parallel hits model suggests that in the presence of significant lipid accumulation in hepatocytes and systemic and hepatic insulin resistance, there are multiple coincident metabolic alterations which leads to an imbalance between free radical production from gut and adipose tissue and anti-lipotoxic protective mechanisms of the liver. The pathophysiological mechanisms involved in this include endoplasmic reticulum (ER) stress, excessive generation of reactive oxygen species (ROS) and diminished catabolism of fatty acids which lead to a pro-inflammatory state.7 The mechanisms, which have associations with insulin resistance, involve numerous cell responses, pro-inflammatory cytokines, chemokines, and toll-like receptors with complex interaction profiles. It is imperative to note that although ROS are agents of damage, one of their most important biological roles is cell signaling through acting as sensors of cellular stress and setting the oxidative tone of the cell.
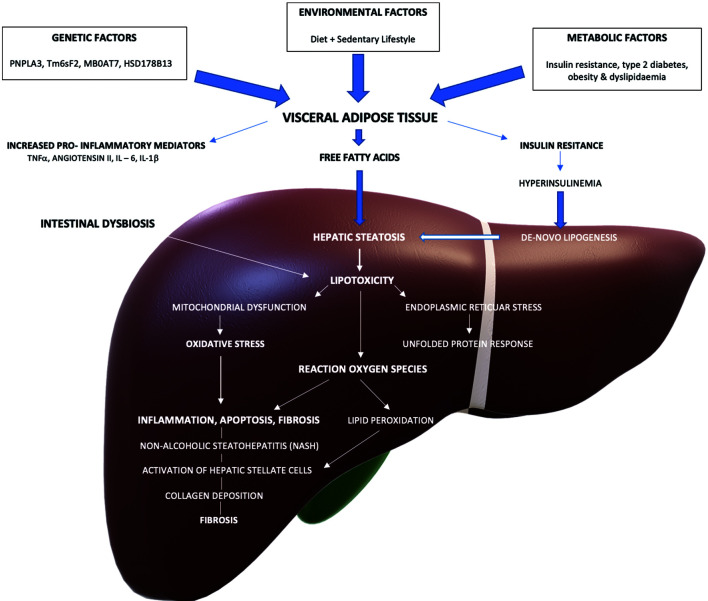
Overall, the evidence suggests that MAFLD progression is a dynamic two-way process relating to repetitive bouts of metabolic stress and inflammation interspersed with endogenous anti-inflammatory reparative responses. An overlay of these pathophysiological concepts underlying MAFLD are best illustrated by means of the schematic in Figure 1.11,12 Given the current lack of treatment for MAFLD, the soaring global epidemic presents a major challenge. It is becoming increasingly essential to uncover the specific pathogenic mechanisms underlying this disease in order to identify pharmacological targets for novel therapies.
Fig. 1. General overview of MAFLD pathogenesis. Schematic adapted from Akshintala et al and Cusi.11,12.
Role of ROS in MAFLD progression
One of the most important roles of ROS is cellular signaling. Through modulating transcription factors, ROS have a key role in cell proliferation and differentiation, metabolism, and immune defense mechanisms. ROS are continually produced by various intracellular organelles including mitochondria, ER, and peroxisomes as by-products of normal cellular metabolism. In normal physiology, ROS are buffered at a steady state in order to maximize cellular redox signaling. Oxidative stress describes an imbalance between the production of reactive oxygen species (ROS) and the host antioxidant scavenging capacity in favor of the former.13 Oxidative stress and ROS are intrinsically linked in the pathogenesis of MAFLD. The discrepancy between ROS generation as a potent proinflammatory, and antioxidant defense proponents; potentiates both DNA and cellular injury.14 The proinflammatory cascades may be propagated through increasing pro-oxidant signaling, or relative antioxidant dysfunction and there likely exists an important inflection point beyond which fibrosis develops. ROS signaling is therefore considered as a strong pro-determinant in hepatic fibrogenesis. These complex pathways likely involve a number of coexistent pro-oxidative triggers which synergistically interact in concert with mitochondrial dysfunction as a principle potentiator of OS.
Mitochondrial ROS generation is typically considered as the most quantitative supply of ROS in the context of energy-derived metabolism.13 ROS have varying chemical properties and are subdivided into free radicals and nonradicals based on these. Free superoxide anion radicals (O2−) and nitric oxide (NO) along with nonradical hydrogen peroxide (H2O2) are some of the first produced ROS in cell metabolism and are key redox signaling molecules in controlling both physiological and pathological cellular functions. The hydroxyl free radical (HO), hypochlorous acid (HOCl), peroxynitrite (ONOO−) and peroxynitrous acid (ONOOH) are all nonradicals with secondary products typically associated with pathology. Finally, the downstream free radicals alkoxyl/alkyl peroxyl (RO/ROO) and the carbonate radical ion (CO3) are deemed potent inducers of oxidative stress and generate widespread cellular damage.14,15 Given the significance of this metabolic maladaptation, there is increasing interest in determining pharmacological targets in the implicated pathways to develop novel targeted therapeutics.16,17
Mitochondrial dysfunction in MAFLD
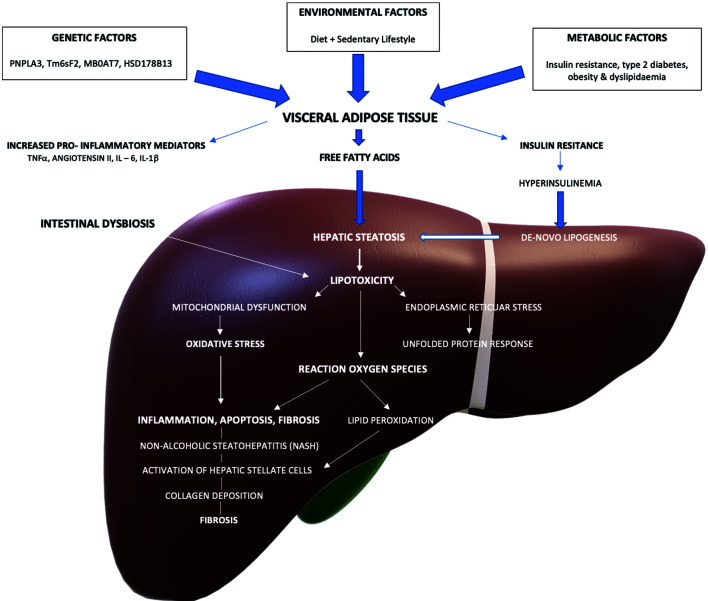
Mitochondria are complex organelles with diverse roles in energy metabolism, cell signaling, and calcium homeostasis.18 Mitochondria are central to cellular energy modulation, given their inherent role in ATP regulation. There are intrinsic gate-keeper mechanisms responsible for maintaining mitochondrial integrity; known as the mitochondrial quality control (MQC) system. This MQC comprises facets including mitochondrial fission and fusion, mitophagy and redox regulation.19 Excessive and dysregulated ROS production within the mitochondrial matrix may damage constituent structures including mitochondrial membrane, mitochondrial DNA (mtDNA) and may induce pro-apoptotic pathways including mitochondrial autophagy, a process also known as mitophagy. These interactions are illustrated in Figure 2.20
Fig. 2. General overview of some aspects of mitochondrial dysfunction in metabolic associated liver disease as described in the text, diagram adapted from Wu et al.20.
Aerobic respiration with ATP synthase highlighted as essential co-factor in oxidative phosphorylation in making ATP. Fis1 is an outer mitochondrial membrane protein that interacts with DRP1 to initiate fission and damaged mitochondria purged by mitophagy. Healthy mitochondria fuse to continue network facilitated by MFN1/2.
Structurally, mitochondria are composed of an inner mitochondrial membrane, and an outer mitochondrial membrane that are separated by an intermembranous space.21 Mitochondria contain double-stranded circular DNA (mtDNA) that encodes 13 polypeptides of the respiratory chain complexes, including adenosine triphosphate (ATP) synthase and additional RNAs responsible for intramitochondrial translation.22
Functionally, mitochondrial energy coupling occurs via the electron transfer chain (ETC), whereby ATP is generated by controlled movement of electrons along the ETC from a high energy state to low energy state in a step wise fashion. This process is facilitated by sequential reduction of nicotinamide adenine dinucleotide and flavin adenine dinucleotide to NADH and FADH2 respectively, which subsequently are donated at regulatory points in the ETC.23 The energy potential released from this electron transfer potentiates a proton gradient and facilitates the phosphorylation of ADP to ATP in a process called oxidative phosphorylation (OXPHOS). Given the fundamental role of the mitochondria in energy regulation, mitochondrial dysfunction appears to be a key component in the pathogenesis of MAFLD.
There are a number of essential nuclear-encoded proteins within mitochondria that have specific functions, but together play a role in mitochondrial biogenesis, the formation of new mitochondria. Peroxisome proliferation-activated receptor gamma (PPARγ) is a ligand-activated transcription factor with a spectrum of function including regulation of mitochondrial production and function, redox balance, and fatty acid oxidation. PPARγs coactivator-1 alpha (PGC-1α) regulates mitochondrial biogenesis and once activated by de-acetylation or phosphorylation, it stimulates nuclear respiratory factor (NRF)1 and NRF2.24 In addition to their separate functions, both NRF1 and NRF2 mediate the expression of the ETC subunits that are encoded by the nuclear genome. NRF1 binds to specific promoter sites of genes involved in mtDNA transcription and is known to regulate the expression of transcription factor A (Tfam).25 Tfam is an mtDNA binding protein that activates transcription of mtDNA. Through regulating mitochondrial stability and replication, Tfam coats and packages the mitochondrial genome.26 Activation of this PGC-1α-NRF-Tfam pathway leads to mitochondrial DNA and protein synthesis and the formation of new mitochondria.
ATP synthase
There are a number of markers of mitochondrial function which are disrupted in MAFLD. ATP synthase is essential cofactor involved in oxidative phosphorylation, localized on the inner mitochondrial membrane and is considered a reliable indicator of mitochondrial functionality. Murine MAFLD models demonstrated impaired ATP synthase stability in both subunit alpha and ATP synthase F(0) complex subunit B1, which contributed to relative ATP deficiency.27,28 Human MAFLD tissue has also demonstrated impaired ATP synthase/Complex V functionality relative to normal controls (42.4% ± 9.1%).29
Mitochondrial fission protein 1 (FIS1)
FIS1 is another important marker of mitochondrial functionality in MAFLD. It is a complex molecule involved in both apoptotic and mitophagy pathways and may influence peroxisomal fusion.30 There appears to be a reciprocal association between FIS1 and mitofusin 1/2 (MFN1/MFN2) whereby an overall increase in mitochondrial fission (FIS1), with parallel reduction in fusion (MFN1/2), induces adiposity and increased preponderance to MAFLD.28 This characteristic expressional profile is associated with impaired mitochondrial function and integrity and may be used as a surrogate disease marker.
Peroxisome proliferator-activated receptor-γ coactivator 1 alpha (PGC-1α)
PGC-1α is a key moderator of lipid and glucose metabolism with wide ranging cell-specific functions in addition to its role in mitochondrial biogenesis. There is relative ubiquity preserved in its interactions with the nuclear receptor peroxisome proliferator-activated receptor alpha (PPAR-α), which is integral for hepatic adaptation to prolonged fasting and integral in β-oxidation.16 Impaired activity of PGC-1α has been demonstrated and noted as a consequence of decreased interaction with promotors containing NRF-1/2 response elements.17 Similarly, phosphoenolpyruvate carboxykinase induction by PGC1α was diminished, suggestive of suboptimal mitochondrial biogenesis in MAFLD in association with reduced activity index of PGC1α.17 Within targeted knockout models of PGC-1α, there is clear reduction in mitochondrial oxidative capacitance, with features of mitochondrial distress with a hepatic steatosis phenotype.31 Conversely, overexpression of hepatic PGC-1α resulted in incremental fatty acid oxidation and reduced triglyceride and secretion.32 Therefore, PGC-1α homeostasis is a key regulatory element of hepatic energy coordination, and is a putative treatment target.
Role of lipid dysregulation in MAFLD pathogenesis
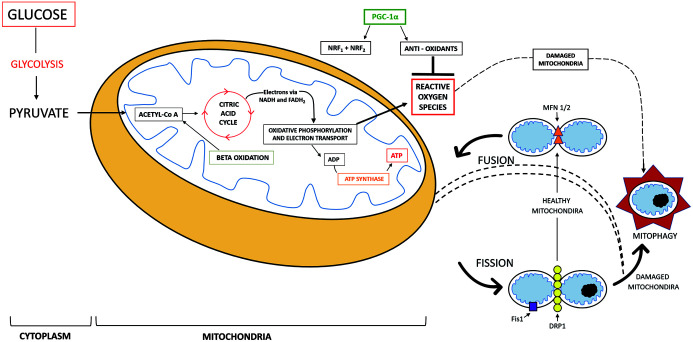
The most direct etiology of MAFLD is disequilibrium of lipid metabolism, and hepatic steatosis is the result of an imbalance in lipid production and degradation.13 The link between diet and MAFLD is well established. Excessive consumption of refined carbohydrates, saturated fats, and animal protein is associated with the development of steatosis and MAFLD progression. Obesity results from a failure to regulate body mass and is the result of excess energy intake, reduced energy expenditure, or both. Obesity causes a marked increase in visceral adipose tissue and profound changes to its function, which has significant secondary effects on the liver. In obese individuals, visceral adipose tissue is highly biologically active. Adipocytes develop an inflammatory phenotype, become necrotic, and secrete cytokines into systemic circulation, which modulates hepatic immune function and induces hepatocyte death. Triglyceride storage in adipocytes is also disrupted, this leads to the inappropriate delivery of free fatty acids (FFAs) to nonadipose tissue causing lipotoxicity, a crucial event in MAFLD pathogenesis. Delivery of FFAs to the liver impairs insulin sensitivity, causes transcription of sterol responsive element binding protein 1c (SREBP-1c) and promotes de novo lipogenesis which further contributes to steatosis.33
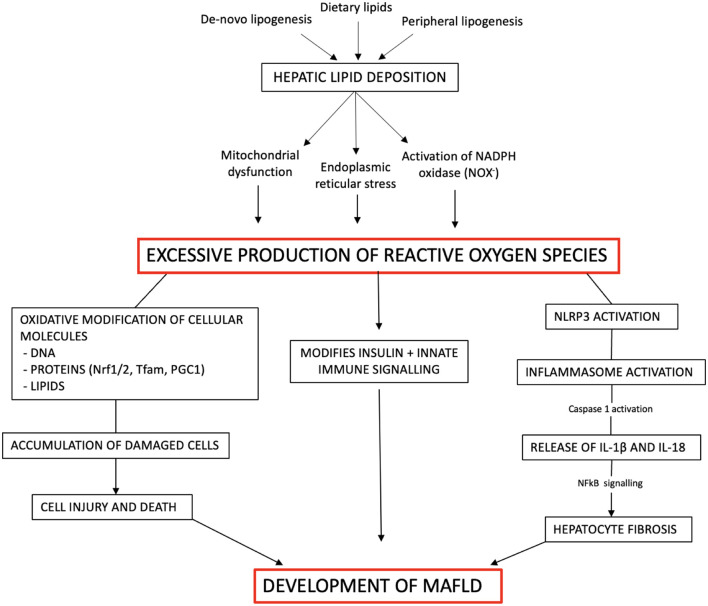
In MAFLD, as hepatic lipid deposition increases, intracellular processes become overwhelmed, and ROS generating mechanisms are potentiated. In general, there are three primary sources of FFAs, which precipitate hepatic lipid accumulation. They are peripheral lipolysis, de novo lipogenesis and dietary.13 Hepatic FFAs typically have two major metabolic fates, they undergo mitochondrial beta oxidation or they undergo esterification to form triglycerides. In MAFLD, the increased influx of FFAs overwhelms hepatocytic metabolic capacity, causing failure of beta oxidation and mitochondrial dysfunction. The surplus of fatty acids can, instead, be converted into triglycerides, stored as lipid droplets, and partially released into circulation as very low-density lipoproteins.13 The excess FFAs can also act as a substrate for the generation of lipotoxic lipid species such as ceramides and diacylglycerols. These lipotoxins are known to cause hepatocellular stress and, in combination with the free pool of hepatic fatty acids, to induce mitochondrial dysfunction and endoplasmic reticular stress. They also activate NADPH oxidase (NOX). an enzyme complex that catalyzes the production of superoxide free radicals, a major source of cellular ROS. These three primary mechanisms account for the increased production of ROS from hepatic lipid deposition, O2−, H2O2, malondialdehyde (MDA) and 4-hydroxy-2-nonenal (4-HNE) in particular. The elevated ROS signals modify insulin and innate immune signaling, and alter the expression and activity of essential enzymes involved in lipid hemostasis. In combination, these effects result in the redox-dependent dysregulation of hepatic lipid metabolism seen in MAFLD.13
One further, more recently identified, endogenous influence on hepatic lipid regulation is thyroid hormone (TH) by its activation of THβ receptor in the liver. TH has been shown to have an essential role in hepatic cholesterol synthesis and fatty acid metabolism.34 Through its ability to alter the function of transcription factors, moderate cell signaling cascades, and through binding to proteins other than TH receptors, TH can modulate gene expression for hepatic fatty acid biosynthesis, cholesterol, and metabolism. The ability of TRβ1 selective agonism of TH in modulating lipid homeostasis may be partly explained by increased clearance, and increased hepatic Ldlr expression in addition to synergistic effects on cholesterol 7α-hydroylase (CYP7A1) related cholesterol synthesis. Various studies have demonstrated the relationship between TH levels and MAFLD, with patients who have hypothyroidism and high levels of TSH at an increased risk of MAFLD, with greater TSH elevation correlating with more extensive steatosis. In mouse models with a negative mutation in THβ, hepatic steatosis was present by 4–5 months of age. Hepatic lipid accumulation in the models was thought to be caused by increased PPARγ signaling and decreased THR-mediated fatty acid β-oxidation.35 Consistent with that, use of TH and THRβ-specific ligands were shown to reduce hepatic triglyceride content in these models thus re-enforcing this relationship.
Oxidative modification of intracellular components
As well as causing dysfunctional lipid metabolism, at high concentrations, ROS can induce oxidative modification of important cellular molecules including proteins, lipids and DNA.9 The accumulation of damaged cellular components causes cellular injury and death. Various in vitro models have shown that cellular apoptosis induced by FFAs may be mediated by ROS, as the pro-apoptotic effects of fatty acids were decreased by anti-oxidants and ROS scavengers in select cases.36–38
With regard to oxidative damage to proteins, there are a number of essential nuclear-encoded proteins within mitochondria, including Nrf1 and Nrf2, Tfam and PGC1 as previously mentioned.39 In MAFLD, increased levels of ROS and subsequent oxidative damage to nuclear DNA can alter the transcription of mitochondria proteins that are necessary for mitochondrial metabolism and DNA maintenance. There is consistent evidence of decreased Nrf2, Tfam, and PGC-1 expression in models of MAFLD.17,40
ROS and inflammasome activation
During periods of metabolic stress or redox imbalance, pattern recognition receptors in hepatic cells, including toll-like receptors and nucleotide-binding oligomerization domain like receptors (NLRs), sense pathogen-associated molecular patterns (PAMPs), danger associated molecular patterns (DAMPs), and cellular metabolites that trigger complex downstream immune signaling cascades.13 As part of the NLR family, pyrin domain-containing 3 (NLRP3), is activated by various PAMPs and DAMPs including ROS, FFAs, ATP, and mitochondrial DNA. Both mitochondrial and NOX-generated ROS have been shown to activate NLRP3 and lead to downstream induction of inflammasome complexes. Once stimulated, these inflammasomes initiate the release interleukin (IL)-1β) and IL18 via caspase-1 activation. These pro-inflammatory cytokines are well known to precipitate hepatocyte necrosis and to contribute to the development of hepatic fibrosis orchestrated by NFkB downstream signaling.41
Potential therapeutic targets
Given the increasing interest to determine the association between oxidative stress and MAFLD development, endogenous antioxidant pathways have been a target of interest for therapeutics. Nrf2 is known to be a master regulator of cell defenses by modulation of cellular anti-oxidant responses and its anti-inflammatory and cytoprotective properties. Nrf2 is activated in both acute and chronic states of oxidative stress, and through regulating the gene expression of cytoprotective enzymes and proteins, there is a reduction in ROS generation with subsequent reduction in oxidative damage, inflammation and cell apoptosis.42 Research has shown Nrf2 is a key modulator in the natural defense against MAFLD and studies to support this show that loss of Nrf2, or Nrf2 deletion accelerates the progression of MAFLD in mouse models.43,44
Given these findings, there is enormous interest in exploiting the therapeutic potential of Nrf2 activation. Du et al.45 found that though using osteocalcin, a small protein found in bone and dentin which activates Nrf2, there could be reduction in oxidative stress and inhibition of the JNK pathway which plays an essential role in MAFLD pathogenesis and thus improving disease progression. Studies have shown that ezetimibe (a Niemann-Pick-C1-Like 1 inhibitor used to treat hypercholesterolemia) and green tea extract both promote the protective features of Nrf2 against hepatic lipid deposition and the inflammatory response in MAFLD. Despite this, Nrf2-related therapeutics remain unlicensed for use in MAFLD, and the development of promising agents to target oxidative stress in management of this disease remains challenging.46,47
Intracellular hepatic lipid accumulation can activate Kupffer cells and the release of pro-inflammatory cytokines including IL1, TNF-α and IL6 whose effects are known to enhance MAFLD progression to fibrosis and cirrhosis.48 A study in mice with diet-induced obesity showed that pharmacological blockade of IL1 using anakinra, a recombinant IL1 receptor antagonist, significantly improved hepatic steatosis by decreasing inflammation and lipogenic gene expression.49 Although there is currently a lack of research in its effects in humans with MAFLD, studies of anakinra in patients with type 1 and 2 diabetes showed an improvement in insulin sensitivity and a reduction is systemic inflammation, and thus could be a promising therapeutic target in the future for MAFLD.50,51
Another attractive therapeutic target, given the relationship between thyroid hormone, hepatic fatty acid, cholesterol metabolism and MAFLD, is the THRβ receptor. There are currently a number of THRβ agonists demonstrated the potential to reduce hepatic lipotoxicity and restore function in models of MAFLD in clinical trials. Resmetirom is a highly specific THRβ agonist designed to improve MAFLD. Its selectivity to the THRβ receptor enhances its safety profile, as it has therapeutic effectiveness without the unwanted systemic events in the heart, bones, and thyroid axis through activation of THRα. One randomized, double-blind, placebo-controlled trial in patients with biopsy-confirmed MAFLD showed that treatment with resmetirom resulted in a significant reduction in hepatic fat at both 12 and 36 weeks. Those positive results have initiated a phase 3 multinational trial to evaluate long-term outcomes of resmetirom with an estimated completion date of March 2024.52,53
Lastly, the PPAR family of nuclear receptor transcription factors, has gained interest as a novel therapeutic target in MAFLD as their dysregulation is known to affect lipid metabolism, contribute to insulin resistance, inflammation, and hepatic fibrogenesis. There are three PPAR isoforms, PPARα, PPARβ, and PPARγ, which have varied expression among cell types and tissues. PPARα is the main form expressed in the liver, but all three isoforms have a role in the regulation of normal liver function. Multiple studies have looked into the benefits of activating one or several PPAR forms in preclinical models of liver disease with positive outcomes. However, pharmacological activation of all three PPAR isoforms concomitantly has only recently been investigated.54
A number of studies have shown that pioglitazone, a selective PPARγ agonist, significantly improves hepatic steatosis, inflammation and insulin resistance, independent of blood glucose control, in patients with type 2 diabetes.55 Lanibranor is a pan-PPAR agonist that has been shown to reduce portal hypertension and hepatic fibrosis in preclinical models of decompensated cirrhosis in both cirrhotic rat models and human liver cells from patients with cirrhosis.54 Although pioglitazone remains the only PPAR agonist with a proven protective role in human MAFLD, these promising findings support further work in the development of PPAR agonists for their use in liver disease. An overview of potential therapeutic targets and agents in the future of MAFLD is outlined in Table 1.55,56–61
Table 1. Overview of recognized molecular targets, pharmacological agents, and clinical trials supporting their use in the treatment of MAFLD.
| Molecular target | Therapeutic agent | Clinical trial |
|---|---|---|
| Nrf2 activation | Broccoli spout/sulforaphane | Randomized, placebo control, double-blind trial56 |
| Neimann-Pick-C1 Like 1 inhibition | Ezetimibe | ESSENTIAL study57 |
| IL1 antagonist | Canakinumab | CANTOS (cardiovascular trial)58 |
| THRβ receptor agonist | Resmetirom | Phase 3 multinational trial59 |
| PPAR agonist | Pioglitazone Lanibranor | TOSCA. IT55; PIVENS60; NATIVE (phase 2b)61 |
Future directions
With the rapidly rising global prevalence of MAFLD and its associated healthcare costs, there is increasing focus on the development of novel therapies to prevent, manage or even cure this disease.62 The pathogenesis of MAFLD is complex and driven by dynamic molecular mechanisms with multifaceted, parallel signaling pathways as shown in Figure 1. Unfortunately, the direct interplay between the clinical and molecular components linked to MAFLD progression remain only partly understood. To date, potential treatments of MAFLD have typically targeted one of the hallmark pathophysiological risk factors driving the disease, inflammation, steatosis, fibrosis, or the gut microbiota. However, given its heterogeneous nature, managing MAFLD through alteration of one mechanism is nearly impossible. A general overview of the implicit pathophysiological mechanisms linking ROS to MAFLD development is presented in Figure 3.9,13,17,41
Fig. 3. General overview of the potential pathophysiological mechanisms linking reactive oxygen species (ROS) to MAFLD development.9,13,17,41.
In order to gain a better understanding of the complex biological processes underlying MAFLD development, multiomics-based strategies have been adopted by researchers for hypothesis-free analysis of the molecular changes in MAFLD.63 The underlying genomic structure of every cell within a given organism is principally the same. However, the physiological fate of a cell depends on the intrinsic cellular genome expression signature. Differing phenotypes are the result of genotypic alterations and their varying patterns of expression, abnormalities of this typically result in disease. Transcriptome profiling is required for the mapping of this unique genotype-phenotype association, and there are a number of single-cell transcriptome-based projects underway that should provide novel physiological insights from which translational targets will be derived.64
Abbreviations
- ATP
Adenosine Triphosphate
- ETC
Electron Transfer Chain
- HCC
Hepatocellular Carcinoma
- IL1β
Interleukin-1β
- MAFLD
Metabolic-Associated Fatty Liver Disease
- NASH
Non-Alcoholic Steatohepatitis
- OS
Oxidative Stress
- PPAR (α/γ/δ)
Peroxisome proliferator-Activated Receptor (α/γ/δ)
- PGC-1α
Peroxisome proliferator-activated receptor-γ coactivator 1 alpha
- ROS
Reactive Oxygen Species
- THR (α/β)
Thyroid Hormone Receptor (α/β)
References
- 1.Sanyal AJ. Past, present and future perspectives in nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2019;16(6):377–386. doi: 10.1038/s41575-019-0144-8. [DOI] [PubMed] [Google Scholar]
- 2.Dyson JK, Anstee QM, McPherson S. Non-alcoholic fatty liver disease: a practical approach to diagnosis and staging. Frontline Gastroenterol. 2014;5(3):211–218. doi: 10.1136/flgastro-2013-100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313(22):2263–2273. doi: 10.1001/jama.2015.5370. [DOI] [PubMed] [Google Scholar]
- 4.Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18(4):223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected Rapid Increase in the Burden of NAFLD in China From 2008 to 2018: A Systematic Review and Meta-Analysis. Hepatology. 2019;70(4):1119–1133. doi: 10.1002/hep.30702. [DOI] [PubMed] [Google Scholar]
- 6.Cai J, Zhang XJ, Li H. Progress and challenges in the prevention and control of nonalcoholic fatty liver disease. Med Res Rev. 2019;39(1):328–348. doi: 10.1002/med.21515. [DOI] [PubMed] [Google Scholar]
- 7.Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology. 2010;52(5):1836–1846. doi: 10.1002/hep.24001. [DOI] [PubMed] [Google Scholar]
- 8.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114(4):842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 9.Takaki A, Kawai D, Yamamoto K. Multiple hits, including oxidative stress, as pathogenesis and treatment target in non-alcoholic steatohepatitis (NASH) Int J Mol Sci. 2013;14(10):20704–20728. doi: 10.3390/ijms141020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eslam M, George J. Genetic contributions to NAFLD: leveraging shared genetics to uncover systems biology. Nat Rev Gastroenterol Hepatol. 2020;17(1):40–52. doi: 10.1038/s41575-019-0212-0. [DOI] [PubMed] [Google Scholar]
- 11.Akshintala D, Chugh R, Amer F, Cusi K. Nonalcoholic Fatty Liver Disease: The Overlooked Complication of Type 2 Diabetes. South Dartmouth (MA): MDText.com, Inc; 2000. [Google Scholar]
- 12.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications. Gastroenterology. 2012;142(4):711–725.e6. doi: 10.1053/j.gastro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Chen Z, Tian R, She Z, Cai J, Li H. Role of oxidative stress in the pathogenesis of nonalcoholic fatty liver disease. Free Radic Biol Med. 2020;152:116–141. doi: 10.1016/j.freeradbiomed.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 14.Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ Res. 2018;122(6):877–902. doi: 10.1161/CIRCRESAHA.117.311401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang L, Wang X, Cueto R, Effi C, Zhang Y, Tan H, et al. Biochemical basis and metabolic interplay of redox regulation. Redox Biol. 2019;26:101284. doi: 10.1016/j.redox.2019.101284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herzig S, Long F, Jhala US, Hedrick S, Quinn R, Bauer A, et al. CREB regulates hepatic gluconeogenesis through the coactivator PGC-1. Nature. 2001;413(6852):179–183. doi: 10.1038/35093131. [DOI] [PubMed] [Google Scholar]
- 17.Aharoni-Simon M, Hann-Obercyger M, Pen S, Madar Z, Tirosh O. Fatty liver is associated with impaired activity of PPARγ-coactivator 1α (PGC1α) and mitochondrial biogenesis in mice. Lab Invest. 2011;91(7):1018–1028. doi: 10.1038/labinvest.2011.55. [DOI] [PubMed] [Google Scholar]
- 18.Jia Q, Sieburth D. Mitochondrial hydrogen peroxide positively regulates neuropeptide secretion during diet-induced activation of the oxidative stress response. Nat Commun. 2021;12(1):2304. doi: 10.1038/s41467-021-22561-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li R, Toan S, Zhou H. Role of mitochondrial quality control in the pathogenesis of nonalcoholic fatty liver disease. Aging (Albany NY) 2020;12(7):6467–6485. doi: 10.18632/aging.102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu Q, Luo CL, Tao LY. Dynamin-related protein 1 (Drp1) mediating mitophagy contributes to the pathophysiology of nervous system diseases and brain injury. Histol Histopathol. 2017;32(6):551–559. doi: 10.14670/HH-11-841. [DOI] [PubMed] [Google Scholar]
- 21.Prasun P, Ginevic I, Oishi K. Mitochondrial dysfunction in nonalcoholic fatty liver disease and alcohol related liver disease. Transl Gastroenterol Hepatol. 2021;6:4. doi: 10.21037/tgh-20-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson S, Bankier AT, Barrell BG, de Bruijn MH, Coulson AR, Drouin J, et al. Sequence and organization of the human mitochondrial genome. Nature. 1981;290(5806):457–465. doi: 10.1038/290457a0. [DOI] [PubMed] [Google Scholar]
- 23.Walsh CT, Tu BP, Tang Y. Eight Kinetically Stable but Thermodynamically Activated Molecules that Power Cell Metabolism. Chem Rev. 2018;118(4):1460–1494. doi: 10.1021/acs.chemrev.7b00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corona JC, Duchen MR. PPARγ as a therapeutic target to rescue mitochondrial function in neurological disease. Free Radic Biol Med. 2016;100:153–163. doi: 10.1016/j.freeradbiomed.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gureev AP, Shaforostova EA, Popov VN. Regulation of Mitochondrial Biogenesis as a Way for Active Longevity: Interaction Between the Nrf2 and PGC-1α Signaling Pathways. Front Genet. 2019;10:435. doi: 10.3389/FGENE.2019.00435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ngo HB, Lovely GA, Phillips R, Chan DC. Distinct structural features of TFAM drive mitochondrial DNA packaging versus transcriptional activation. Nat Commun. 2014;5:3077. doi: 10.1038/ncomms4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee K, Haddad A, Osme A, Kim C, Borzou A, Ilchenko S, et al. Hepatic Mitochondrial Defects in a Nonalcoholic Fatty Liver Disease Mouse Model Are Associated with Increased Degradation of Oxidative Phosphorylation Subunits. Mol Cell Proteomics. 2018;17(12):2371–2386. doi: 10.1074/mcp.RA118.000961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sacerdoti D, Singh SP, Schragenheim J, Bellner L, Vanella L, Raffaele M, et al. Development of NASH in Obese Mice is Confounded by Adipose Tissue Increase in Inflammatory NOV and Oxidative Stress. Int J Hepatol. 2018;2018:3484107. doi: 10.1155/2018/3484107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pérez-Carreras M, Del Hoyo P, Martín MA, Rubio JC, Martín A, Castellano G, et al. Defective hepatic mitochondrial respiratory chain in patients with nonalcoholic steatohepatitis. Hepatology. 2003;38(4):999–1007. doi: 10.1053/jhep.2003.50398. [DOI] [PubMed] [Google Scholar]
- 30.Ihenacho UK, Meacham KA, Harwig MC, Widlansky ME, Hill RB. Mitochondrial Fission Protein 1: Emerging Roles in Organellar Form and Function in Health and Disease. Front Endocrinol (Lausanne) 2021;12:660095. doi: 10.3389/fendo.2021.660095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Estall JL, Kahn M, Cooper MP, Fisher FM, Wu MK, Laznik D, et al. Sensitivity of lipid metabolism and insulin signaling to genetic alterations in hepatic peroxisome proliferator-activated receptor-gamma coactivator-1alpha expression. Diabetes. 2009;58(7):1499–1508. doi: 10.2337/db08-1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morris EM, Meers GM, Booth FW, Fritsche KL, Hardin CD, Thyfault JP, et al. PGC-1α overexpression results in increased hepatic fatty acid oxidation with reduced triacylglycerol accumulation and secretion. Am J Physiol Gastrointest Liver Physiol. 2012;303(8):G979–G992. doi: 10.1152/ajpgi.00169.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parker R. The role of adipose tissue in fatty liver diseases. Liver Research. 2018;2(1):35–42. doi: 10.1016/j.livres.2018.02.002. [DOI] [Google Scholar]
- 34.Mullur R, Liu YY, Brent GA. Thyroid hormone regulation of metabolism. Physiol Rev. 2014;94(2):355–382. doi: 10.1152/physrev.00030.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sinha RA, Singh BK, Yen PM. Direct effects of thyroid hormones on hepatic lipid metabolism. Nat Rev Endocrinol. 2018;14(5):259–269. doi: 10.1038/nrendo.2018.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arita K, Kobuchi H, Utsumi T, Takehara Y, Akiyama J, Horton AA, et al. Mechanism of apoptosis in HL-60 cells induced by n-3 and n-6 polyunsaturated fatty acids. Biochem Pharmacol. 2001;62(7):821–828. doi: 10.1016/s0006-2952(01)00723-7. [DOI] [PubMed] [Google Scholar]
- 37.Yi SJ, Choi HJ, Yoo JO, Yuk JS, Jung HI, Lee SH, et al. Arachidonic acid activates tissue transglutaminase and stress fiber formation via intracellular reactive oxygen species. Biochem Biophys Res Commun. 2004;325(3):819–826. doi: 10.1016/j.bbrc.2004.10.122. [DOI] [PubMed] [Google Scholar]
- 38.Pompeia C, Freitas JJ, Kim JS, Zyngier SB, Curi R. Arachidonic acid cytotoxicity in leukocytes: implications of oxidative stress and eicosanoid synthesis. Biol Cell. 2002;94(4-5):251–265. doi: 10.1016/s0248-4900(02)01200-5. [DOI] [PubMed] [Google Scholar]
- 39.Begriche K, Massart J, Robin MA, Bonnet F, Fromenty B. Mitochondrial adaptations and dysfunctions in nonalcoholic fatty liver disease. Hepatology. 2013;58(4):1497–1507. doi: 10.1002/hep.26226. [DOI] [PubMed] [Google Scholar]
- 40.Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015;21(5):739–746. doi: 10.1016/j.cmet.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Yang G, Lee HE, Lee JY. A pharmacological inhibitor of NLRP3 inflammasome prevents non-alcoholic fatty liver disease in a mouse model induced by high fat diet. Sci Rep. 2016;6:24399. doi: 10.1038/SREP24399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bataille AM, Manautou JE. Nrf2: a potential target for new therapeutics in liver disease. Clin Pharmacol Ther. 2012;92(3):340–348. doi: 10.1038/clpt.2012.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gupte AA, Lyon CJ, Hsueh WA. Nuclear factor (erythroid-derived 2)-like-2 factor (Nrf2), a key regulator of the antioxidant response to protect against atherosclerosis and nonalcoholic steatohepatitis. Curr Diab Rep. 2013;13(3):362–371. doi: 10.1007/s11892-013-0372-1. [DOI] [PubMed] [Google Scholar]
- 44.Chowdhry S, Nazmy MH, Meakin PJ, Dinkova-Kostova AT, Walsh SV, Tsujita T, et al. Loss of Nrf2 markedly exacerbates nonalcoholic steatohepatitis. Free Radic Biol Med. 2010;48(2):357–371. doi: 10.1016/j.freeradbiomed.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 45.Du J, Zhang M, Lu J, Zhang X, Xiong Q, Xu Y, et al. Osteocalcin improves nonalcoholic fatty liver disease in mice through activation of Nrf2 and inhibition of JNK. Endocrine. 2016;53(3):701–709. doi: 10.1007/s12020-016-0926-5. [DOI] [PubMed] [Google Scholar]
- 46.Lee DH, Han DH, Nam KT, Park JS, Kim SH, Lee M, et al. Ezetimibe, an NPC1L1 inhibitor, is a potent Nrf2 activator that protects mice from diet-induced nonalcoholic steatohepatitis. Free Radic Biol Med. 2016;99:520–532. doi: 10.1016/j.freeradbiomed.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 47.Li J, Sapper TN, Mah E, Rudraiah S, Schill KE, Chitchumroonchokchai C, et al. Green tea extract provides extensive Nrf2-independent protection against lipid accumulation and NFκB pro-inflammatory responses during nonalcoholic steatohepatitis in mice fed a high-fat diet. Mol Nutr Food Res. 2016;60(4):858–870. doi: 10.1002/mnfr.201500814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Anderson N, Borlak J. Molecular mechanisms and therapeutic targets in steatosis and steatohepatitis. Pharmacol Rev. 2008;60(3):311–357. doi: 10.1124/pr.108.00001. [DOI] [PubMed] [Google Scholar]
- 49.Negrin KA, Roth Flach RJ, DiStefano MT, Matevossian A, Friedline RH, Jung D, et al. IL-1 signaling in obesity-induced hepatic lipogenesis and steatosis. PLoS One. 2014;9(9):e107265. doi: 10.1371/journal.pone.0107265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van Asseldonk EJ, van Poppel PC, Ballak DB, Stienstra R, Netea MG, Tack CJ. One week treatment with the IL-1 receptor antagonist anakinra leads to a sustained improvement in insulin sensitivity in insulin resistant patients with type 1 diabetes mellitus. Clin Immunol. 2015;160(2):155–162. doi: 10.1016/j.clim.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 51.Larsen CM, Faulenbach M, Vaag A, Vølund A, Ehses JA, Seifert B, et al. Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N Engl J Med. 2007;356(15):1517–1526. doi: 10.1056/NEJMoa065213. [DOI] [PubMed] [Google Scholar]
- 52.Harrison SA, Bashir M, Moussa SE, McCarty K, Pablo Frias J, Taub R, et al. Effects of Resmetirom on Noninvasive Endpoints in a 36-Week Phase 2 Active Treatment Extension Study in Patients With NASH. Hepatol Commun. 2021;5(4):573–588. doi: 10.1002/hep4.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harrison SA, Bashir MR, Guy CD, Zhou R, Moylan CA, Frias JP, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2019;394(10213):2012–2024. doi: 10.1016/S0140-6736(19)32517-6. [DOI] [PubMed] [Google Scholar]
- 54.Boyer-Diaz Z, Aristu-Zabalza P, Andrés-Rozas M, Robert C, Ortega-Ribera M, Fernández-Iglesias A, et al. Pan-PPAR agonist lanifibranor improves portal hypertension and hepatic fibrosis in experimental advanced chronic liver disease. J Hepatol. 2021;74(5):1188–1199. doi: 10.1016/j.jhep.2020.11.045. [DOI] [PubMed] [Google Scholar]
- 55.Della Pepa G, Russo M, Vitale M, Carli F, Vetrani C, Masulli M, et al. Pioglitazone even at low dosage improves NAFLD in type 2 diabetes: clinical and pathophysiological insights from a subgroup of the TOSCA.IT randomised trial. Diabetes Res Clin Pract. 2021;178:108984. doi: 10.1016/j.diabres.2021.108984. [DOI] [PubMed] [Google Scholar]
- 56.Kikuchi M, Ushida Y, Shiozawa H, Umeda R, Tsuruya K, Aoki Y, et al. Sulforaphane-rich broccoli sprout extract improves hepatic abnormalities in male subjects. World J Gastroenterol. 2015;21(43):12457–12467. doi: 10.3748/wjg.v21.i43.12457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cho Y, Rhee H, Kim YE, Lee M, Lee BW, Kang ES, et al. Ezetimibe combination therapy with statin for non-alcoholic fatty liver disease: an open-label randomized controlled trial (ESSENTIAL study) BMC Med. 2022;20(1):93. doi: 10.1186/s12916-022-02288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017;377(12):1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 59. ClinicalTrials.gov. A Phase 3 Study to Evaluate Safety and Biomarkers of Resmetirom (MGL-3196) in Patients With Non-alcoholic Fatty Liver Disease (NAFLD), MAESTRO-NAFLD-Open-Label-Extension (MAESTRO-NAFLD-OLE). Available from: https://clinicaltrials.gov/ct2/show/NCT04951219.
- 60.Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362(18):1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Francque SM, Bedossa P, Ratziu V, Anstee QM, Bugianesi E, Sanyal AJ, et al. A Randomized, Controlled Trial of the Pan-PPAR Agonist Lanifibranor in NASH. N Engl J Med. 2021;385(17):1547–1558. doi: 10.1056/NEJMoa2036205. [DOI] [PubMed] [Google Scholar]
- 62.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 63.Ægidius HM, Veidal SS, Feigh M, Hallenborg P, Puglia M, Pers TH, et al. Multi-omics characterization of a diet-induced obese model of non-alcoholic steatohepatitis. Sci Rep. 2020;10(1):1148. doi: 10.1038/s41598-020-58059-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Angerer P, Simon L, Tritschler S, Wolf FA, Fischer D, Theis FJ. Single cells make big data: New challenges and opportunities in transcriptomics. Current Opinion in Systems Biology. 2017;4:85–91. doi: 10.1016/j.coisb.2017.07.004. [DOI] [Google Scholar]