Abstract
Background
In this questionnaire-based study, we evaluated the prevalence and awareness level of occupational hazards among dental professionals (students, interns, dentists, and specialists) at different dentistry colleges.
Materials/Methods
A self-administered questionnaire was designed from previously conducted studies and distributed to 310 participants from different dental colleges of dentistry in Sana’a City, Yemen. The questionnaire was divided into 4 parts. The first part comprised questions involving sex, age, and clinical professions; the second part, questions on awareness about different occupational hazards; the third part, questions about prevalence of occupational hazards; and the fourth part, questions related to bringing down the prevalence of occupational hazards associated with a dental practice. Data were analyzed using one-way analysis of variance and chi-square tests.
Results
Significant differences were detected between sex, age groups, and clinical professions. Musculoskeletal disorders were the most common physical hazard, whereas infections were the greatest biological hazard, accounting for 68% and 74%, respectively. Of the participants, 63.5% answered that “patient, practice, and finance” together were the most common causes of stress among practicing dentists and dental students. The use of gloves and/or masks was the most efficient preventive measure among participants. A significant difference was found among most of the parameters, with P≤0.001. Almost 50% of respondents answered “yes” in relation to vaccination for hepatitis-B, with P=0.062.
Conclusions
The prevalence of occupational hazards was low among dentists and dental students among the tested participants, with significant differences for most of the parameters.
Keywords: Chemical Hazard Release, Cross-Sectional Studies, Dentists, General Practitioners
Background
Occupational risk is a hazard or danger due to the nature of the working environment of a particular job [1]. The first records of occupational risk or risk awareness are from the 18th century, when Bernardino Ramazzini, the father of occupational treatment, identified the role of one’s occupation in a dynamic range of physical conditions and illnesses [1,2]. Analyses have shown that dentists experience more frequent and serious health problems than do individuals in other high-risk health professions [3–5].
Hazards can be broadly categorized as follows. Mechanical occupational hazards include injuries caused by cuts with sharp tools or puncture wounds with needles or other sharp items. Such injuries can lead to the transmission of infectious diseases to the dentist [2]. Physical occupational hazards comprise harmful radiation, such as non-ionizing radiation, including visible light and UV rays, or ionizing radiation (X-rays), which can injure different body cells. Chemical occupational hazards are from inorganic substance (mercury) toxicity, organic materials (solvents, resins, and gases), or caustic materials (formaldehyde and hydrogen peroxide) and can included latex glove allergy (contact dermatitis) [2,4]. Biological occupational hazards can arise from allergens of biological origin, infections, contamination of dental materials, and cross-contamination [4]. Lastly, psychological occupational hazards can arise from stress/excessive workload, lack of job satisfaction/insecurity, and medical/legal problems [2,4–6]. Other factors that are considered as initiating factors for stress, such as noise and vibration from the handpiece, can lead to hearing problems [5–8]. Musculoskeletal problems like lower backache, wrist ache, and neck pain can occur from conducting work in specific locations as needed and using continuous repetitive motions for lengthy periods of time [4–9].
Consequently, dentists ought to be aware of these hazards and the techniques to counteract them. Before implementing such an educational course, we need to have baseline information on the prevalence and awareness among the research group [7,8]. Most research papers on occupational hazards among dentists are directed at more developed countries, such as India [6,9,10–13]. A single study has been conducted each in Saudi Arabia, Australia, Thailand, Poland, Croatia, and Italy [5,8,14–17]. Table 1 reveals details of the studies conducted, including the year of publication, sample size, and questionnaires used. Studies among dental students were carried out in different countries [5,9,10,13,15,16].
Table 1.
Details of studies, including the year of publication, sample size, and questions used.
| Author (s), publication year, and country | Sample size,% of male/female | Study participants | Contents of questionnaire |
|---|---|---|---|
| Present study, 2022, Sana’a-Yemen | 310 37% Male 63% Female |
174 Dental students, 50 Interns, 72 General practitioners, 14 Specialists | Demographic details, Awareness about different occupational hazards, Prevalence of occupational hazards, Different means to decrease prevalence of occupational hazards |
| Al-Aslami et al, 2018, Jazan, Saudi Arabia [5] | 200 62% Male 38% Female |
No clinical profession was mentioned | Personal information, Awareness about occupational hazards, Seminar attendance, Safety measures practiced, Experience of occupational hazard while in practice. |
| Bhuvaneshwari et al, 2020, Odisha, India [6] | 572 60% Male 40% Female |
General practitioners | Personal information, Years of experience, Type of occupational hazard, Awareness about occupational hazards, Safety measures practiced, Working hours per week |
| Leggat and Smith, 2006, Queensland, Australian [8] | 285 73% Male 27% Female |
General practitioners | Personal information Years of experience, number of working hours per day Level of awareness. Preventive measures undertaken |
| Sheik and Bhoj, 2020, Chennai-India [9] | 200 No sex identification |
100 Dental students, 100 General practitioners | Personal data, Awareness about occupational hazards, Safety measures practiced, occupational hazard experiences while in practice |
| Mehta et al, 2013, Chandigar, India [10] | 113 68% Male 32% Female |
55 Dental graduates, 58 Post-graduates | Occurrence of occupational Hazards, Necessary steps taken for their prevention |
| Leggat et al, 2001, Southern Thailand [14] | 220 47% Male 53% Female |
General practitioners | Personal information Information on a range of occupational hygiene Practices. This included infection control; HBV immunization, management of HBV and HIV patients |
| Garus-Pakowska et al, 2016, Łódź, Poland [15] | 103 No sex identification |
Denturists | Assessment of somatic and psychosomatic ailments related to denturists’ job Analysis and evaluation of harmful agents associated with denturists’ workplace Evaluation of preventive measures and compliance with safety rules among denturists. |
| Reddy et al 2015, Bellary, India [11] | 66 71% Male 29% Female |
General practitioners | Demographic questions Work conditions. Physical, chemical, psychosocial, litigation problems experienced. dentist’s work schedule(number of breaks and their purpose) |
| Ramaswami et al, 2020, Mumbai, India [12] | 200 No gender identification |
General practitioners | Demographic data, Years of experience of dentists, Number of clinical hours working on patients Awareness of various occupation-related hazards and various measures taken by their management |
| Tadakamadla et al, 2012, Bhimavaram, India [13] | 290 20% Male 80% Female |
Dental professionals | Personal information Experience in Years, number of working hours per day Level of awareness. Preventive measures undertaken. Occupational hazards experienced |
| Pavičin et al, 2020, Croatia [16] | 406 39% Male 61% Female |
Dental professionals | Demographics information, length of service, specialization. Dentist’s awareness of occupational health risks. Previous experience in dental offices |
| Saccucci et al, 2022, Italy [17] | 468 15% Male 85% Female |
Dental hygienists | Personal information Training, working hours, and patient numbers per week, Type of pain, Type of MSD reported, Absence from work due to MSDs, Need for medical care due to MSDs |
The questions used in the present study were collected from published articles, with some adjustments [4–6,8–17]. However, minimal data are available from developing countries, particularly among Yemeni dental professionals. Hence, the aims of the present questionnaire-based study included investigating and comparing the prevalence and level of awareness of occupational hazards among dental professionals, such as fifth-year students, interns, general practitioners, and specialists, at different colleges of dentistry in Sana’a, Science and Technology, and Queen Arwa Universities in Sana’a, Yemen. Moreover, we aimed to identify means to bring down the prevalence of occupational hazards associated with the dental practice.
Material and Methods
Study Design
In this cross-sectional questionnaire-based study, questionnaires were enlisted to clinics at the College of Dentistry, Sana’a, Science and Technology, and Queen Arwa University. The study was approved by the Medical Ethics Committee of Dental Faculty in the University of Science and Technology, Sana’a, Yemen [EAC/UST 219]. Each participant signed a consent form before answering the questions. All participants were recruited from a pool of regular fifth-year students, general practitioners, interns, and specialists. Ethical clearance was obtained from the Ethics Committee, College of Dentistry, Science and Technology. Other details of the study were discussed with the participants before the delivery of questions and collection of data. All participants signed a written consent. This study was conducted in accordance with the guidelines of the Declaration of Helsinki. The reliability and validity of the questions were assessed. (December 2021 to February 2022) in Sana’a.
Study Samples and Criteria
The study sample was determined based on the number of final (fifth)-year dental students, interns, general practitioners, and their specialist supervisors at 3 dental schools. A population size of about 310 participants was verified on the basis of the G*Power software (http://www.gpower.hhu.de/en.html). The self-confidence quantity was adjusted at 85%, power was altered at 80%, and the resulting quantity was satisfactory. The principles for inclusion were as follows: participants aged 20 years old and older; regular students at the last level (fifth year); and graduated dentists who worked as interns, general practitioners, or supervisors with a master’s degree and a minimum of 2 years of teaching experience.
Participants Grouping and Data Collection
Data collection was carried out from December 2021 to February 2022. A total of 420 participants (160 men and 260 women) were enrolled. Participants of both sexes (≤20 years) who were stakeholders in any of the 3 colleges were included in the study. The participants were selected through convenience sampling. Data were collected by one dentist (M. Al Y) who was provided a short period of training by using a predesigned questionnaire.
Questionnaire Parts
A single-page questionnaire was created. The questions were direct and gathered from previous studies with some modifications [4–6,8–17]. Participants were asked to fill out the anonymous self-administered questionnaire. The questionnaire was divided into 4 parts and consisted of 13 questions.
The first part of this cross-sectional survey study involved asking and answering questions related to personal and demographic data, such as sex (male or female), age groups (selected participants were divided into 5 age groups, namely, ≤20, 21–30, 31–40, 41–50, and ≥51 years old), and dental clinical professions (fifth-year students, interns, general practitioners, and specialists).
The second part consisted of 3 questions related to awareness about different occupational hazards and the causes of stress. The questions were as follows: Q1 and Q2 were “What do you think is the most common physical (Q1) and biological (Q2) occupational hazard?” Q3 was “ What do you think is the most common cause of stress among dentists and dental students?” After each question, the participant was asked to choose from different answers that were presented as options.
The third part involved questions related to the prevalence of occupational hazards, and it consisted of 7 questions, as follows: Q1 was “As a result of workload, do you have any musculoskeletal problems.” Q2 was “Have you been exposed to any of the following risks?” Q3, Q4, and Q5 were combined as “Have you had a needlestick injury before? if yes, when did it happen, and where was the location and site of injury?” Q6 was “Have you been exposed to any aerosol or allergic infections?” Q7 asked about the cause of allergic reactions, if any, such as “latex, monomer, drug, and other materials.”
The fourth and last part was complicated and had important questions regarding different measures adopted to bring down the occurrence of occupational hazard associated with dental practice. The first part was “To protect yourself from dental occupational hazard, you use: gloves, masks, lead barrier, head cap, protective-eye wear alone or together.” The second question was “Are you vaccinated for hepatitis B?” The options were “Yes, no, yes, but not the 3 doses.”
Data Analysis
Data from 310 participants were collected and summarized in an Excel sheet (Office 2010). The results of the descriptive statistical analysis were presented as mean, frequency, percentages, and standard deviation using SPSS version 25.0 (IBM Corp, Armonk, NY, USA). The comparisons and associations between different sexes, age groups, clinical professions, and levels of awareness about occupational hazards were assessed using ANOVA, with P<0.05 indicating statistical significance.
Results
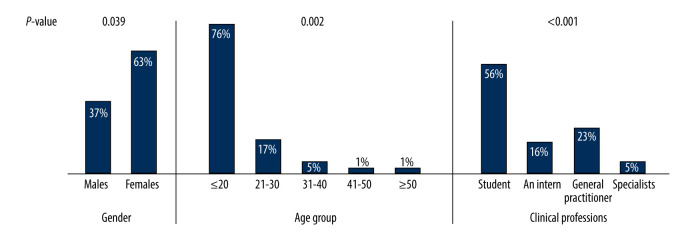
Out of 420 questionnaires distributed, 310 were received, thereby setting the response rate at 74%. Participant demographic data are presented in Figure 1. Men comprised 37%, and women comprised 63%. Most participants were in the ≤20-year group. Dental interns formed 16% of the total clinical profession, whereas the parameter of specialized clinical profession included 6 orthodontists, 6 pediatric dentists, and 2 maxillofacial surgeons (5%). Significant differences were detected between sexes, age groups, and clinical professions, with P values of 0.039, 0.002, and 0.001, respectively.
Figure 1.
Demographic data of the participants.
Table 2 lists the frequency at which hazards occurred and the percentage of participants who were affected by such hazards. “Musculoskeletal problems” were the most common physical occupation hazards (211; 68%), whereas “infections” were the most common biological hazard (230; 74%). For the question “What do you think is the most common cause of stress among dentists and dental students?”, from all participants, 63.5% chose the option “patient, practice, finances, and studies-related”, whereas each of those were listed separately as other options (Table 2). There was a significant difference between all parameters (P<0.001).
Table 2.
Percentage of participant answers in relation to awareness of the types and causes of hazard (n=310).
| Questions | Answer | Frequency | % | P value |
|---|---|---|---|---|
| Q1. What do you think is the most common physical hazard? | Radiation | 37 | 12% | 0.000* |
| Noise & vibration from handpiece | 50 | 16% | ||
| Musculoskeletal problems | 211 | 68% | ||
| Other | 12 | 4% | ||
| Q2. What do you think is the most common biological hazard? | Infections | 230 | 74% | 0.000* |
| Allergies | 20 | 6.5% | ||
| I have no idea | 60 | 19.5% | ||
| Q3. What do you think is the most common cause for stress among dentists and dental students? | Patient-related | 43 | 14% | 0.000* |
| Practice-related | 33 | 11% | ||
| Finance-related | 8 | 2.5% | ||
| Study-related | 29 | 9% | ||
| All | 197 | 63.5% |
Significant difference, P<0.05.
For the section on the outcomes of workload, 73% of participants chose “yes” when asked “As a result of workload, do you have any musculoskeletal problems?” When participants were asked if they have had any exposure to risks and a few options were listed, 41% chose “needlestick injury,” and 31% respondents chose “any other sharp instrument injury”. More than half of the participants had experienced a “needlestick injury” between 1 and 5 times. Of those who experienced needlestick injuries, 23% experienced then while treating the patient, 14% experienced them while recapping needles, and 15% experienced them while picking up instruments. From all participants, 51% chose the fingers as the most frequent site or location of needlestick injuries. Only 5% of participants chose “arms,” making this the least affected site for needlestick injuries. Most of the questions and participants’ answers showed significant differences, except for the questions “Have you been exposed to any of the following risks?” and “When did you experience a needle stick injury?”, with P values of 0.124 and 0.072, respectively (Table 3).
Table 3.
Frequency and percentage of participants answers in relation to hazard outcome and preventive measured (n=310).
| Questions | Answer | Frequency | % | P value |
|---|---|---|---|---|
| Q1. As a result of workload, do you have any musculoskeletal problems | Yes | 225 | 73% | 0.042* |
| No | 85 | 27% | ||
| Q2. Have you been exposed to any of the following risks? | Needlestick injury | 137 | 41% | 0.124 |
| Any other sharp instrument injury | 117 | 31% | ||
| None at all | 56 | 28% | ||
| Q3. Have you had a needlestick injury before? | Never | 126 | 40.6% | 0.032* |
| 1–5 times | 159 | 51.3% | ||
| 6–10 times | 17 | 5.5% | ||
| More than 10 times | 8 | 2.6% | ||
| Q4. If yes, when? | During treating the patient | 72 | 23% | 0.072 |
| During recapping a needle | 45 | 14% | ||
| During picking-up instrument | 42 | 15% | ||
| During replacing instrument | 25 | 8% | ||
| Others | 126 | 40% | ||
| Q5. If yes, locate the site | Finger | 160 | 51% | 0.000* |
| Palms | 20 | 7% | ||
| Arms | 16 | 5% | ||
| Other sites | 28 | 9% | ||
| Other | 86 | 28% | ||
| Q6. Have you been exposed to any of the following? | Aerosol infections | 49 | 16% | 0.000* |
| Allergic reaction | 117 | 38% | ||
| I don’t know | 144 | 46% | ||
| Q7. Are you allergic to | Latex | 51 | 16.5% | 0.006* |
| Monomer | 54 | 17.5% | ||
| Medicine/drugs | 193 | 62% | ||
| Other materials | 12 | 4% |
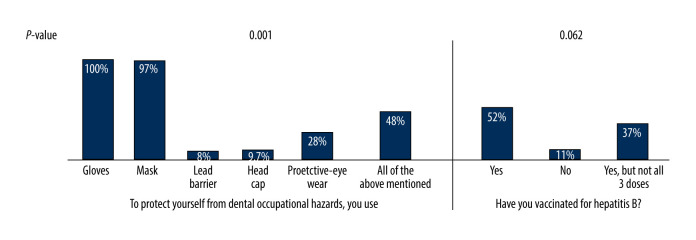
Figure 2 shows the use of personal protective equipment by the participants to protect themselves from dental occupational hazards. All participants chose “gloves”, and 97% participants also chose “mask”. From all participants, 48% were in favor of all types of preventive measures, including the use of “lead barrier, head cap, and protective eye wear”, apart from masks and gloves. Significant differences were recorded among the answers to this question (P<0.001). A total of 52% of participants responded “yes” that they had been vaccinated for hepatitis B. No significant differences were detected in the answers to the question.
Figure 2.
Shows the percentage of the participants by protection type and vaccination for hepatitis B.
Discussion
This was a cross-sectional survey based on a questionnaire. Few data on occupational hazards were available in developing countries [5,6,8,9,13–17], and to the best of our knowledge, this was the first study conducted in Yemen. The present study was conducted among dental students, interns, general practitioners, and specialists in 3 facilities of dentistry. The objectives were to investigate awareness about occupational hazards and to find ways to lower their prevalence associated with the dental practice. Overall, the participants exhibited a better attitude and awareness about occupational hazards and the associated risk factors in their workplace, as compared with participants in the other studies mentioned in Table 1.
We included 310 participants, of which 116 (37%) were men, and 194 (63%) were women. This number of participants is average compared with the number of participants recruited in the previous studies shown in Table 1. The age group ranged from ≤20 years to ≥50 years, and most of the participants were dental students, explaining the lower awareness than the other studies, which were conducted mainly among dental practitioners. Dental students tend to have lower awareness than dental practitioners.
Musculoskeletal disorders (MSD) can happen owing to the requirement to work in particular positions using continuous repetitive motions for long periods of time. At work, the dentist adopts a tense posture while standing and sitting next to the patient, who is sitting or lying down. This extreme stress adversely affects the musculoskeletal system [4]. Of the respondents, 73% showed a history of MSD. This rate was very high compared with the results reported in studies conducted in India, Greece, Australia, and Denmark, in which most dentists reported at least 1 MSD [8–10,18,19]. Comparable results were documented by Reddy et al, who stated that 60% of dentists working in private practice in India experienced some MSD. Similar findings were identified from a different study, in which 60% of participants reported having MSD. A recent study by Saccucci et al in Italy showed the highest rate of MSD at 91% [17]. A study from Queensland, Australia, found that younger and less experienced dentists were more likely to report MSDs of the neck, upper back, and shoulders. It is possible that experienced dentists adopt better positions and working techniques [8].
From patients and the environment, dentists are always at risk of exposure to various infectious agents, which can be transmitted through oral and oropharyngeal secretions, blood, air, and water [20]. In the present study, 16% of participants reported exposure to aerosol infection, making it a common infection transmitted by infected air. However, this result was quite low compared with that of a study conducted in Chennai, India, in which 30% of participants reported exposure to aerosol infections [9]. Legnani et al performed an assessment of aerosol contamination from dental procedures. Air contamination was measured using the Surface Air System method and the “plate” method (Air Microbial Index). During working hours, the average bacterial load in the air was found to increase more than thrice, and the load levels in the air were 1.5 times (aerobic bacteria) and 2 times (anaerobic) higher than the initial load [21].
Many potentially toxic materials used in dentistry can pose a health occupational hazard if proper precautions are not taken. In the present study, 38% of the participants had previous allergies to different materials, including latex, monomer, and other materials. Of participants, 16.5% were allergic to latex, 17.5% were allergic to monomer, 62% were allergic to some types of medicines/drugs (possibly be due to khat shewing habit), and 4% were allergic to other materials. These findings are different from those revealed by Sheik and Bhoj [9], who stated that 60% of participants were allergic to latex gloves, 30% were allergic to monomer, and 10% were allergic to anesthetic gases. The prevalence of allergy in our study was higher than the results reported in the studies by Leggat and Smith (29%), Chowanadisai et al (22%), and Gijbels et al (22.5%) [8,22,23]. This difference can be related to difference in the level of experiences of the participants in the studies, because more than half of our participants were fifth-year students.
In dentistry, sharp object injuries occur because of the small operating area, frequent patient movement, and the variety of sharp instruments used in dental procedures [20,21,24]. Sharp instrument injuries are the most effective method of transmitting blood-borne infections between patients and healthcare professionals [25]. These injuries are a concern because needles often contain residual bodies from the puncture sites that occur during anesthetic procedures. It was alarming to learn that 59.4% of participants in the present study population had a needlestick injury more than once, and 51.3% encountered a needle injury 1 to 5 times over the course of their practice. A study conducted in Croatia by Paviin et al revealed a considerable prevalence of needlestick injuries (57.75%) [16]. A lower percentage (23%) was reported by Cheng et al [26], who found that 100 of 434 participants experienced more than 1 needle stick per week [25,26].
In relation to the site of needlestick injury, the most affected part of the body was the finger, with a percentage of 51%. This percentage was lower than that in another study, in which participants reported that the finger was the most common site of needlestick injury, with a rate of 90.8% [25]. Additionally, our study showed that the most common needlestick injuries occurred while treating patients (23%). This finding is similar to that reported by another study conducted by Cheng et al, who said the most common needlestick injuries occurred when treating patients [26]. Another study conducted in the United States [27] revealed that 70% of percutaneous injuries among dental students occurred while administering local anesthesia, specifically by puncturing their fingers while recapping a needle [27,28]. The conflicting results were due to the fact that we included experienced clinicians, faculty members, and specialists, who adopted a series of precautions and protocols that have become universally accepted to prevent accidental needlestick injuries.
The main explanations for stress among dentists are associated to working hours, job satisfaction, interactions between staff and patients, and medico-legal issues [29,30]. Source of stress exist in all professions, and dentistry is no exclusion, as 63.5% of our research contributors reported experiencing stress at work. These self-reported beliefs are considered slightly lower than the percentages mentioned in studies conducted by Leggat et al in Thailand [14]. Kay and Lowe in England [29] reported a prevalence of 96.1% and 86%, respectively. The present study results showed that 14% of students attribute their stress to patient-related concerns, 11% to practice, 2.5% to finances, 9% to studies, and 63.5% to all of the above. These findings are unlike those revealed by Sheik and Bhoj [9], who stated that 38% of students attribute their stress to patient-related issues, 18% to practice, 8% to finance, and 36% to all of the above. Of practitioners, 10% attribute their stress to patient-related issues, 12% to practice, 20% to economics, and 58% to all the above-mentioned causes. Patient-related stress, according to respondents in a study by Al-Khatib et al [30], was associated with the treatment of patients who had a medical history of other conditions (especially heart disease), were pregnant, or were deliberately or involuntarily hiding the truth about their health status. Most participants were from private colleges. Hence, it is logical that only 2.5% of respondents cited finances as a cause of stress. When it comes to prevention of the abovementioned health hazards, a high-level implementation of infection control measures is done by most participants, such as changing of gloves for each patient (100%), using face mask (97%), and working with protective eyeglasses (28%). However, only 8% of respondents reported wearing a lead apron while taking X-rays, and 9.7% wore head caps. These constitute very low percentages and differed from those in a study by Morris et al [31], who showed that around 90% of dentists in Kuwait wore gloves, 52% wore glasses, and 75% wore masks.
There are health risks in the workplace of all occupations, including dentistry. Despite these dangers, dental professionals cannot stop caring for and serving the community. The only solution would be to avoid the dangers [32]. The literature from different countries focuses mainly on infection control and the correct handling of potentially infected materials, as the transmission of infection is very high in dentistry. Usage of personal protective barriers, such as gloves, masks, and goggles, as well as the availability of high-powered suction and good ventilation reduces the risks of aerosols and vapor hazards [33]. Parallel findings have been recorded in several studies [2,11–13,23,34].
In the present study, only 52% of students and respondents were vaccinated against hepatitis B: 37% were not vaccinated, and 11% had not received all 3 doses. This is likely a reflection of the attitudes of students, who may feel less at risk of exposure. This outcome is lower than that of a study conducted in Saudi Arabia [5], in which 93% of dentists were vaccinated, and 64% of students were vaccinated. This can be attributed to the financial status in both countries and the socioeconomic status of the students, interns, and general practitioners. Thus, it is recommended that all students be properly vaccinated against hepatitis B owing to the risk of infection through body fluids.
Gaining adequate knowledge and information regarding occupational risks and their prevention will contribute to the delivery of better-quality care to patients [25]. The prevention and reduction of MSD among dentists should include their education in dental ergonomics and awareness of the importance of work-related risk factors [28]. Various continuing dental education programs (seminars, workshops, and videos) should be organized for students and general practitioners so that dental professionals can acquire knowledge on different methods of prevention [25,34].
The limitations of the present study are as follows. It included only 1 city in Yemen. It did not compare between different levels of dental clinical professions. The study does not include auxiliary staff, who are an important stakeholder in dentistry. Comparison between sexes and a larger number of participants are required in future studies.
Conclusions
According to the overall findings, there is a low prevalence and awareness of occupational hazards among dentists and dental students. Further education on prevention methods is needed to reduce the risk of occupational dental hazards. In addition, long-term studies with larger sample sizes and that consider other factors are needed.
Footnotes
Conflict of interest: None declared
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Fasunloro A, Owotade FJ. Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5(2):134–52. [PubMed] [Google Scholar]
- 2.Gambhir RS, Singh G, Sharma S, et al. Occupational health hazards in the current dental profession – a review. Open Occup Health Safe J. 2011;3:57–64. [Google Scholar]
- 3.Brooks SL, Rowe NH, Drach JC, Young SK. Prevalence of herpes simplex virus disease in a professional population. J Am Dent Assoc. 1981;102(1):31–34. doi: 10.14219/jada.archive.1981.0017. [DOI] [PubMed] [Google Scholar]
- 4.Health and Safety Authority. Guidance on Occupational. Hazards in Dentistry. 2016. pp. 1–17. Available from: www.hsa.ie/eng/Publications_and_Forms/Publications/Healthcare_Sector/Guidance_on_Occupational_Hazards_in_Dentistry.html.
- 5.Al-aslami RA, Elshamy FMM, Maamar EM, et al. Knowledge and awareness towards occupational hazards and preventive measures among students and dentists in Jazan Dental College, Saudi Arabia. Open Access Maced J Med Sci. 2018;6(9):1722–26. doi: 10.3889/oamjms.2018.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhuvaneshwari S, Shveta J, Kaur J, et al. Assessment of various dental occupational hazards and safety measures among dentists of Odisha, India. J Contemp Dent Pract. 2020;21(10):1165–69. [PubMed] [Google Scholar]
- 7.Szymanska J. Occupational hazards of dentistry. Anna Agricul Envir Medi. 1999;6(1):13–19. [PubMed] [Google Scholar]
- 8.Leggat PA, Smith DR. Prevalence of percutaneous exposure incidents amongst dentists in Queensland. Aust Dent J. 2006;51(2):158–61. doi: 10.1111/j.1834-7819.2006.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 9.Sheik R, Bhoj M. Awareness and prevalence of dental students and dental practitioners towards occupational hazards in dentistry. Int J Sci Res. 2020;5(2):197–206. [Google Scholar]
- 10.Mehta A, Gupta M, Upadhyaya N. Status of occupational hazards and their prevention among dental professionals in Chandigarh, India: A comprehensive questionnaire survey. J Dent Res. 2013;10(4):446–51. [PMC free article] [PubMed] [Google Scholar]
- 11.Reddy V, Bennadi D, Satish G, Kura U. Occupational hazards among dentists: A descriptive study. J Oral Hyg Health. 2015;3(5):1–4. [Google Scholar]
- 12.Ramaswami E, Nimma V, Jakhete A, Lingam I, et al. Assessment of occupational hazards among dentists practicing in Mumbai. J Fam Med Prim Care. 2020;9(4):2016–21. doi: 10.4103/jfmpc.jfmpc_1180_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tadakamadla J, Kumar S, Swapna LA, Reddy S. Occupational hazards and preventive practices among students and faculty at a private dental institution in India. Stomatologija. 2012;14(1):28–32. [PubMed] [Google Scholar]
- 14.Leggat PA, Chowanadisai S, Kukiattrakoon B, et al. Occupational hygiene practices of dentists in southern Thailand. Int Dent J. 2001;51(1):11–16. doi: 10.1002/j.1875-595x.2001.tb00811.x. [DOI] [PubMed] [Google Scholar]
- 15.Garus-Pakowska A, Leśniewska A, Gaszyńska G, Szatko F. Occupational exposure and health problems among Polish denturists: A population-based study in Łódź province. Int Dent J. 2016;66(4):237–46. doi: 10.1111/idj.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pavičin IS, Lovrić Ž, Çeshko AZ, Vodanović M. Occupational injuries among dentists in Croatia. Acta Stomatologica Croatica. 2020;54(1):51–59. doi: 10.15644/asc54/1/6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saccucci M, Zumbo G, Mercuri P, et al. Musculoskeletal disorders related to dental hygienistprofession. Int J Dent Hygiene. 2022;20:571–79. doi: 10.1111/idh.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexopoulos EC, Stathi I-C, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;5(1):1–8. doi: 10.1186/1471-2474-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milerad E, Ericson MO, Nisell P, Kilbom A. An electromyographic study of dental work. Ergonomics. 1991;34(7):953–62. doi: 10.1080/00140139108964837. [DOI] [PubMed] [Google Scholar]
- 20.Laheij AM, Kistler JO, Belibasakis GN, et al. European Oral Microbiology Workshop (EOMW) 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4(1):17659. doi: 10.3402/jom.v4i0.17659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Legnani P, Checchi L, Pelliccioni GA, D’Achille C. Atmospheric contamination during dental procedures. Quintessence Int. 1994;25(6):435–39. [PubMed] [Google Scholar]
- 22.Chowanadisai S, Kukiattrakoon B, Yapong B, et al. Occupational health problems of dentists in southern Thailand. Int Dent J. 2000;50(1):36–40. doi: 10.1111/j.1875-595x.2000.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 23.Gijbels F, Jacobs R, Princen K, et al. Potential occupational health problems for dentists in Flanders, Belgium. Clin Oral Invest. 2006;10(1):8–16. doi: 10.1007/s00784-005-0003-6. [DOI] [PubMed] [Google Scholar]
- 24.Henderson KA, Matthews IP. Environmental monitoring of nitrous oxide during dental anesthesia. Br Dent J. 2000;188(11):617–19. doi: 10.1038/sj.bdj.4800556. [DOI] [PubMed] [Google Scholar]
- 25.Ayatollahi J. Needle-stick injuries in a general hospital: Continuing risk and under reporting. Ann Iranian Med. 2006;3:47–50. [Google Scholar]
- 26.Cheng HC, Su CY, Yen AM, Huang CF. Factors affecting occupational exposure to needlestick and sharps injuries among dentists in Taiwan: A nationwide survey. PLoS One. 2012;7(4):e34911. doi: 10.1371/journal.pone.0034911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah SM, Merchant AT, Dosman JA. Percutaneous injuries among dental professionals in Washington State. BMC Public Health. 2006;6(1):1–5. doi: 10.1186/1471-2458-6-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: A review. Ind Health. 2007;45:611–21. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]
- 29.Kay E, Lowe J. A survey of stress levels, self-perceived health and health-related behaviors of UK dental practitioners in 2005. Br Dent J. 2008;204(11):E19. doi: 10.1038/sj.bdj.2008.490. [DOI] [PubMed] [Google Scholar]
- 30.Al-Khatib IA, Ishtayeh M, Barghouty H, Akkawi B. Dentists’ perceptions of occupational hazards and preventive measuresin East Jerusalem. East Mediterr Health J. 2006;12:153–60. [PubMed] [Google Scholar]
- 31.Morris E, Hassan FS, Al Nafisi A, Sugathan TN. Infection control knowledge and practices in Kuwait: a survey on oral health care workers. Saudi Dent J. 1996;8(1):699–703. [Google Scholar]
- 32.Babaji P, Samadi F, Jaiswal JN, Bansal A. Occupational hazards among dentists: A review of literature. Journal of International Dental and Medical Research. 2011;4(2):87–93. [Google Scholar]
- 33.Kumar R, Manish G, Ferreira A. Occupational hazards among dental surgeons. Ind J Occup Environ Med. 2000;4(3):139–41. [Google Scholar]
- 34.Labafchi A, Rahpeyma A, Khajehahmadi S. A study on PEI among private dentists in Mashhad, Iran. J Family Med Prim Care. 2020;9:1403–6. doi: 10.4103/jfmpc.jfmpc_900_19. [DOI] [PMC free article] [PubMed] [Google Scholar]