Abstract
The Compendium of Physical Activities reports that walking at 2.5 mph associates with absolutely-defined moderate intensity (i.e., ≥3 metabolic equivalents [METs]). However, it is unclear whether this speed threshold is accurate during overground walking and/or across the adult age-span. This study aimed to identify optimal and heuristic speed thresholds associated with 3 METs during overground walking across age groups. Healthy adults (n=248, 21–85 years of age, 49% women) performed a 5-minute self-paced overground walking trial. Speed was measured using an electronic gait mat, and oxygen uptake was measured using indirect calorimetry and converted to METs. Optimal and heuristic thresholds and classification accuracy metrics were determined and compared using ROC curve analyses. Speed thresholds (95% CIs) associated with 3 METs for the whole sample, young (21–40 years), middle-aged (41–60 years) and older-aged (61–85 years) groups were 1.29 (1.25, 1.33), 1.30 (1,26, 1,35) and 1.25 (1.21, 1.29) m/s, respectively. Overall, 3 mph and 5 km/h performed better than 2.5 mph and 4.5 km/h in balancing both sensitivity and specificity (higher Youden’s Indices). Overground walking speeds associated with 3 METs were similar across age groups. A heuristic threshold of 3 mph or 5 km/h may better identify absolutely-defined moderate intensity overground walking.
Keywords: Walking speed, moderate intensity, physical activity
1. Introduction
Current public health physical activity (PA) guidelines recommend that adults should accumulate at least 150–300 minutes per week of moderate-intensity PA (i.e., ≥ 3 metabolic equivalents [METs]; 1 MET = 3.5 mL O2/kg/min) to attain health benefits (2018 Physical Activity Guidelines Advisory Committee, 2018; World Health Organization, 2020). Walking is an essential component of many activities of daily living and requires little skill and low cost, thus making it an ideal choice for most individuals to achieve PA guidelines (Morris & Hardman, 1997). With the wide-spread availability of wearable technologies (e.g., cell phones or smartwatches), individuals can now easily self-monitor and modulate their walking speed in order to meet recommended intensity levels (Saevereid et al., 2014). However, it is unclear “how fast is fast enough” to reach a moderate intensity during overground walking.
The Compendium of Physical Activities reports that walking at 2.5 mph (activity code 1717) is associated with a metabolic cost of 3 METs (Ainsworth et al., 2011). However, this speed was derived from a limited number of studies (n = 9) mainly conducted in younger adults (mean age: 22.4 – 36.6 years). Further, four studies employed a treadmill walking protocol (Anjos et al., 2008; Barkley & Penko, 2009; Dal et al., 2010; Dufour, 1984), and five studies reported energy expenditure of walking (around 3 METs) under free-living conditions without corresponding speed values (Brun et al., 1981; de Guzman, 1978, 1984, 1979; Torún et al., 1982). Another widely used resource to estimate walking intensity or speed is the American College of Sports Medicine (ACSM)’s metabolic equation (VO2 [mL O2/kg/min] = 0.1*speed [m/min] + speed*grade*1.8 + 3.5) ( American College of Sports Medicine, 1980). Solving this equation for 3 METs yields a speed of 2.6 mph. However, this equation was developed using data collected from three trained men during level treadmill walking (Dill, 1965). Considering the potential differences in metabolic cost under various walking conditions (Dal et al., 2010; Parvataneni et al., 2009) and/or age categories (Mian et al., 2006; Peterson & Martin, 2010), the speed cut-point(s) enacted from controlled treadmill protocols among younger participants might be not representative of all ages during overground walking. For example, Parvataneni et al. (2009) reported a higher oxygen uptake (mean difference: 2.59 mL/kg/min, or 0.74 METs) for treadmill compared to overground walking among middle-aged and older adults. This difference might be explained by the distinct muscle activation and joint movement patterns adopted under the two different walking conditions (Lee & Hidler, 2008). As such, simply applying the above-mentioned treadmill-based speed thresholds during overground walking may result in lower energy expenditure than expected. In addition, older adults typically have a higher energy expenditure at a preferred or set walking speed compared to young adults due to an increased coactivation of antagonist muscles to ensure adequate joint stability during walking (Peterson & Martin, 2010). Thus, a lower speed threshold for moderate intensity may be appropriate for older adults. Other anthropometric factors, such as body mass index (BMI) (Browning & Kram, 2005), may also affect the generalizability of a single speed threshold when universally applied.
In an effort to translate technical definitions of intensity (i.e., VO2, METs) into lay language, moderate intensity is commonly described by public health guidelines as “brisk walking” at ~3 to 4 mph (2018 Physical Activity Guidelines Advisory Committee, 2018; Pate et al., 1995). However, this term is subjective and may result in a wide range of enacted speeds (and thus intensities) when instructing individuals to walk briskly (Murtagh et al., 2002; Parise et al., 2004). Moving beyond this apparently vague descriptive terminology, there is a need for an evidence-based moderate intensity speed threshold that balances both accuracy across the adult lifespan and utility for public health application under varied settings. Therefore, the current study aimed to identify both the optimal and heuristic (i.e., evidence-based, practical, rounded) walking speed thresholds associated with absolutely-defined moderate intensity (i.e., ≥ 3 METs) during overground walking among young (21–40 years), middle- (41–60 years) and older-aged (61–85 years) adults. Furthermore, we also evaluated potential factors (i.e., age, height, weight, BMI, waist circumference, leg length, and walk ratio) that might contribute to misclassification when using the identified speed thresholds.
2. Methods
2.1. Study design and setting
The current study is a secondary data analysis of the CADENCE-Adults study (ClinicalTrials.gov #NCT02650258). The CADENCE-Adults study is a laboratory-based, cross-sectional investigation of the relationship between cadence and metabolic intensity in adults aged 21–85 years. Data used for this analysis were collected in the Physical Activity and Health Laboratory, Department of Kinesiology, University of Massachusetts Amherst from Jan 2016 to August 2019. The study protocol was approved by the University of Massachusetts Amherst Institutional Review Board. Informed consent was obtained from all participants before data collection. The eligibility criteria, complete methodology, procedures, primary aims, and results of the original study are reported elsewhere (Tudor-Locke et al., 2019; Tudor-Locke et al., 2020; Tudor-Locke et al., 2021).
2.2. Participants
The original study recruited 10 men and 10 women for each 5-year age group ranging from 21 to 85 years (i.e., 21–25 years, 26–30 years, etc.) to ensure a sex- and age-balanced sample that would minimize these sources of bias. Full details of the sample size calculation relevant to the original study’s inclusion/exclusion criteria, and risk stratification are available elsewhere (Tudor-Locke et al., 2019; Tudor-Locke et al., 2020). Briefly, eligible participants were ambulatory and generally healthy, and not taking medications that would affect physiological responses to exercise.
2.3. Procedures and measures
A full description of the procedures and equipment used in this study are presented in a previous report (Tudor-Locke et al., 2019). Briefly, demographic (age, sex, race/ethnicity) and anthropometric data (height, weight, BMI, waist circumference and leg length) were self-reported or collected, respectively, using standardized procedures. Participants completed a single 5-minute overground walking trial at a preferred (normal, usual) walking pace in a level indoor hallway, looping back and forth across a 13-m distance between two cones. Participants were instructed to walk at their normal pace, just as they usually do in their daily life such as walking to their car or around a shopping center. Walking speed (m/s) was measured using an electronic mat (GAITRite®, CIR Systems Inc., Sparta, NJ; dimensions are 7.0 m [L] *0.9 m [W] *0.0032 m [H]) placed centrally between the two cones. This GAITRite system has previously been demonstrated to be valid and reliable to measure gait parameters at preferred speed (intra-class correlation coefficient: 0.99, repeatability coefficient: 1.4% for speed measure) (Webster et al., 2005). The cones were placed 3 m beyond the mat on either end to minimize the effects of acceleration/deceleration on the measured preferred walking speed; thus the total distance between two cones was 13 m. Note, since the electronic mat did not collect the speed during turnings, the measured walking speed was considered as congruent with continuous straight-line overground walking at a self-selected pace. Oxygen uptake (VO2, mL/kg/min) was measured using a portable, validated indirect calorimeter (Oxycon Mobile, Vyaire Medical Inc., Chicago, IL) and exported in 5-second epochs. The system has been shown to accurately (relative difference from the Douglas Bag Method of −1.4 to +2.6%) and reliably measure oxygen uptake (coefficient of variation of 2.8 to 5.8%) across a range of workloads (~25 to 220 Watts, and workload at VO2max) (Rosdahl et al., 2010).
2.4. Data processing and analytic sample
Gait spatiotemporal parameters (speed, step length, cadence) were analyzed and exported using the GAITRite® software. Walk ratio (WR) was calculated by dividing step length (mm) by cadence (steps/min), and expressed in mm/steps/min (Rota et al., 2011). Custom MATLAB (The MathWorks, Natick, MA) and R (Version 3.6.1, R Core Team, Vienna, Austria) scripts were used to combine and process sample characteristics, gait variables and metabolic data. We averaged the VO2 values during the last 2 minutes (2:45 to 4:45) of the 5-minute walking trial to obtain an approximate steady-state oxygen uptake, with a 15-second offset to minimize the impact of changes in oxygen uptake that might occur if the participant were to slow down in anticipation of the end of the 5 min trial (Aguiar et al., 2019). VO2 values were then converted to METs (dividing by 3.5 mL/kg/min). Moderate intensity was defined as ≥ 3 METs and < 6 METs. Individuals who reached ≥ 6 METs (vigorous intensity) were removed from the dataset (n = 2). Additionally, data from 10 participants were removed due to equipment malfunction (n = 9) or early termination of the walking trial (n = 1) due to pre-defined safety criteria. The final analytic sample was composed of 248 participants (21–85 years, 49% women) with complete measures of sample characteristics, gait variables and VO2 data. The final analytic dataset and data dictionary are provided in the Supplementary material 1.
2.5. Statistical analysis
Sample characteristics are presented as mean (standard deviation), range (min-max), or mean (95% confidence intervals [95% CIs]) by age groups where appropriate. The 95% CIs were interpreted as significantly different if there was no overlap between two confidence intervals, and not significantly different if the confidence interval for one group overlapped the point estimate of the other group (Greenland et al., 2016). Correlations between speed and intensity were calculated using Pearson’s r.
Receiver operating characteristic (ROC) curve analyses were performed for the whole sample (N = 248) and separately for the three age groups: young (21–40 years; n=75), middle-aged (41–60 years; n=79) and older-aged (61–85 years; n=94). Optimal speed thresholds with 95% CIs were determined using Youden’s Index (J = Sensitivity + Specificity −1) and bootstraps with 20,000 replicates (Youden, 1950). The threshold corresponding with the maximum Youden’s Index was chosen to optimize prevalence-independent summary measures of sensitivity and specificity. Where applicable, classification accuracy for each speed threshold was evaluated by sensitivity, specificity, overall accuracy, area under the curve (AUC; interpreted as excellent [≥ 0.90], good [0.80–0.89], fair [0.70–0.79], and poor [< 0.70]) (Metz, 1978), positive predictive value (PPV) and negative predictive value (NPV). The overall performance of the identified threshold(s) as a classifier of moderate intensity were also summarized using a confusion matrix of true positive (TP; i.e., ≥ speed threshold and ≥ 3 METs), false positive (FP; i.e., ≥ speed threshold, but < 3 METs), true negative (TN; i.e., < speed threshold and < 3 METs) and false negative (FN; i.e., < speed threshold, but ≥3 METs).
To further explore the potential factors contributing to misclassification in our sample, we also performed one-way analyses of variance (ANOVA) with post-hoc Tukey’s HSD tests to compare participant characteristics (i.e., age, height, weight, BMI, waist circumference, leg length, and walk ratio) based on classification (i.e., TP, TN, FP, and FN groups) using the identified age-specific thresholds. The data were checked for violations against the assumptions for ANOVA using Normal QQ plot and Levene’s Test. Where applicable, Cohen’s d effect sizes were calculated using raw group means and pooled standard deviations to examine magnitude of difference between two groups (Cohen, 2013). The significance level was set at p < 0.05.
Using the obtained optimal speed threshold (in m/s) for the whole sample, we next compared classification accuracy metrics for potential heuristic thresholds associated with moderate intensity when converted it into commonly used speed units (mph and km/h) for ease of interpretation. Consistent with previous reports (Tudor-Locke et al., 2021), when selecting the most appropriate heuristic threshold associated with moderate intensity, we favored a declared tolerance for FN vs. FP. In other words, we tolerated individuals exceeding a moderate intensity when below the speed threshold (i.e., FN), while seeking to minimize the probability of individuals being below a moderate intensity when above the speed threshold (i.e., FP). In practice, this places more importance overall on the specificity value of the threshold. All analyses were performed in R (version 4.1.1), and the “pROC” package was used for ROC curve analyses.
3. Results
3.1. Participant characteristics
Descriptive and bout characteristics of the analytic sample (N = 248) are summarized in Table 1. The sample was approximately evenly distributed by sex (48.8% female), and predominantly Caucasian (79%). The average self-selected walking speed was similar across age groups during the overground walking trial; mean values (95% CIs) for young, middle-aged, and older adults were 1.29 (1.25, 1.33), 1.30 (1,26, 1,35), and 1.25 (1.21, 1.29) m/s, respectively. Older adults tended to walk at a lower intensity (3.3 [3.2, 3.4] METs) than young adults (3.5 [3.4, 3.7] METs). The overall sample prevalence of achieving ≥ 3 METs was 75%, and was higher in young adults (78.7%) compared to middle-aged (77.2%) and older adults (70.2%). Figure 1 displays the relationship between preferred walking speed and intensity during overground walking for the whole sample separated by age groups. Strong positive correlations between speed and intensity were observed in the whole sample, young, middle- and older-aged groups (r = 0.74, 0.69, 0.83, and 0.71, respectively).
Table 1.
Descriptive and bout characteristics of the analytical sample
| Variables | Young (n = 75) | Middle-aged (n = 79) | Older-aged (n = 94) | Whole Sample (n = 248) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean (SD) | Min – Max | Mean (SD) | Min – Max | Mean (SD) | Min – Max | Mean (SD) | Min – Max | |
| Sex (% female) | 49.3 | -- | 49.4 | -- | 47.9 | -- | 48.8 | -- |
| Age (years) | 30.5 (5.8) | 21.0 – 40.0 | 50.2 (6.0) | 41.0 – 60.0 | 72.8 (6.9) | 61.0 – 85.0 | 52.8 (18.6) | 21.0 – 85.0 |
| Height (cm) | 170.7 (9.4) | 149.1 – 194.1 | 171.0 (9.2) | 150.1 – 190.1 | 167.4 (8.4) | 150.2 – 188.3 | 169.5 (9.1) | 149.1 – 194.1 |
| Weight (kg) | 72.8 (14.2) | 51.6 – 119.0 | 76.2 (14.3) | 47.8 – 128.8 | 72.5 (12.6) | 46.3 – 100.4 | 73.8 (13.7) | 46.3 – 128.8 |
| BMI (kg/m2) | 24.8 (3.4) | 19.4 – 36.9 | 26.4 (4.0) | 19.0 – 37.6 | 25.8 (3.5) | 18.5 – 36.0 | 25.6 (3.7) | 18.5 – 37.6 |
| Waist Circumference (cm) | 80.7 (9.2) | 64.5 – 109.4 | 86.1 (10.8) | 68.3 – 116.2 | 90.0 (11.3) | 66.4 – 114.5 | 85.9 (11.2) | 64.5 – 116.2 |
| Leg Length (cm) | 79.7 (5.9) | 65.7 – 94.4 | 80.7 (5.3) | 66.6 – 92.0 | 80.0 (5.1) | 69.0 – 94.8 | 80.1 (5.4) | 65.7 – 94.8 |
| Speed (m/s) | 1.29 (0.18) | 0.94 – 1.86 | 1.30 (0.18) | 0.88 – 1.77 | 1.25 (0.18) | 0.75 – 1.65 | 1.28 (0.18) | 0.75 – 1.86 |
| Intensity (METs) | 3.5 (0.7) | 2.4 – 6.0 | 3.4 (0.6) | 1.8 – 5.0 | 3.3 (0.6) | 2.0 – 5.1 | 3.4 (0.6) | 1.9 – 6.0 |
| Intensity ≥3 METs (%) | 78.7 | -- | 77.2 | -- | 70.2 | -- | 75.0 | -- |
| Cadence (steps/min) | 107.7 (8.2) | 90.0 – 123.0 | 108 (9.6) | 86.0 – 135.0 | 108.2 (8.9) | 87.0 – 129.0 | 108.0 (8.9) | 86.0 – 135.0 |
| Step Length (cm) | 70.5 (7.0) | 58.7 – 94.7 | 71.0 (6.7) | 54.8 – 85.7 | 67.8 (7.5) | 43.8 – 87.2 | 69.7 (7.2) | 43.8 – 94.7 |
| Walk Ratio (mm/steps/min) | 6.4 (0.7) | 5.1 – 8.3 | 6.5 (0.7) | 5.1 – 8.5 | 6.2 (0.8) | 4.3 – 8.5 | 6.4 (0.7) | 4.3 – 8.5 |
Note: Values are presented as mean (SD), Min – Max. Young, middle- and older-aged represents participants 21–40, 41–60 and 61–85 years, respectively. Abbreviations: BMI, body mass index; METs, metabolic equivalents; Min = minimum, Max = maximum; SD, standard deviation.
Figure 1.
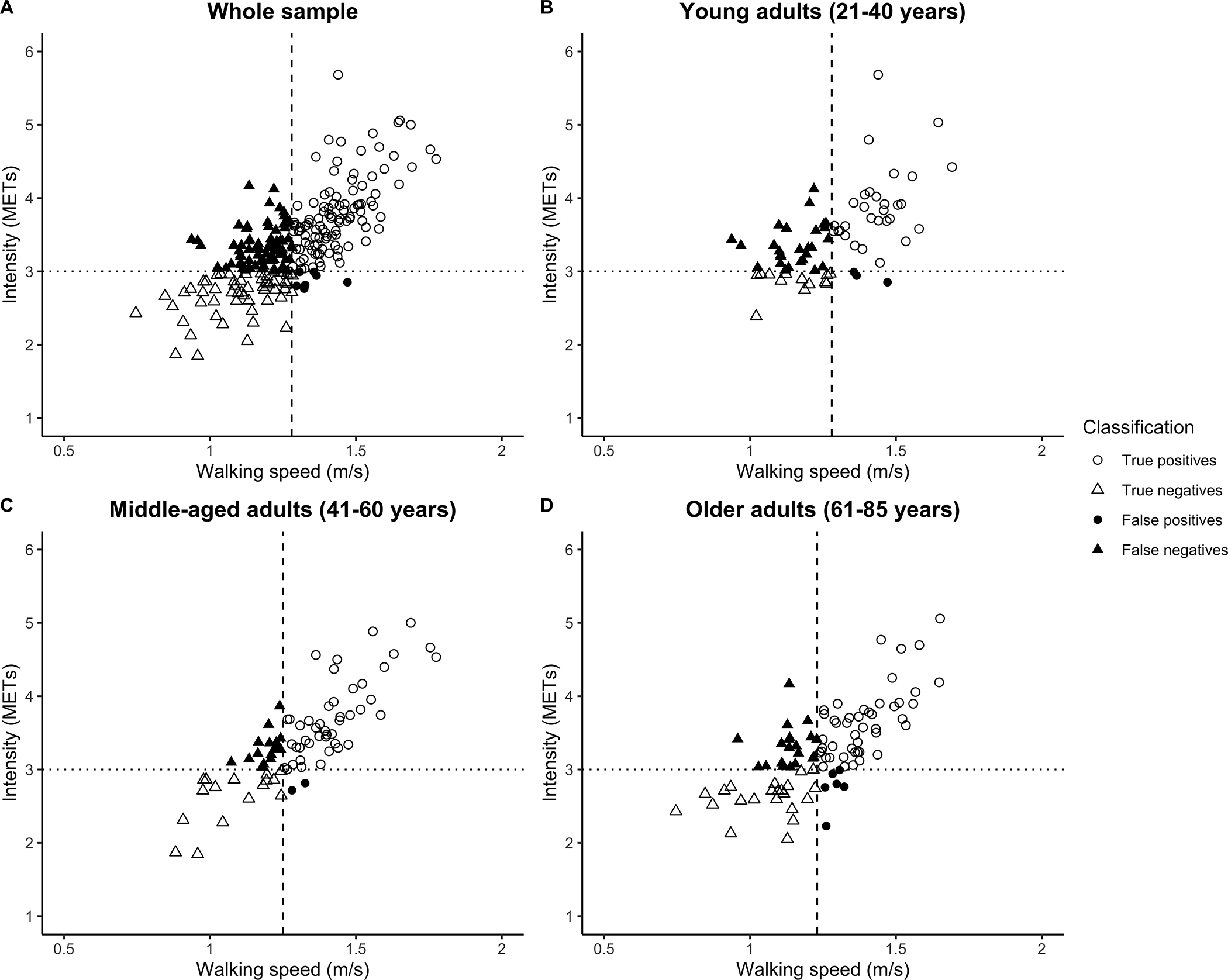
Scatter plot of walking speed (m/s) and intensity (METs) values observed during overground walking at a self-selected preferred walking pace for the whole sample and separated by age group. The shapes of the data points represent the classification of bouts as true positives (open circles), true negatives (open triangles), false positives (filled circles), and false negatives (filled triangles). The dotted line represents absolutely-defined moderate intensity (≥ 3 METs). The dashed line in each subplot represents the identified age-specific moderate-intensity walking speed (1.28, 1.25 and 1.23 m/s for healthy young, middle-aged and older adults, respectively).
3.2. Moderate-intensity overground walking speed thresholds across age groups
Table 2 presents the results of ROC curve analysis for optimal speed thresholds related to absolutely-defined moderate intensity across three age groups. The optimal speed thresholds (95% CIs) associated with 3 METs for the whole sample, young, middle-aged, and older-aged groups were 1.28 (1.13, 1.33), 1.28 (1.07, 1.38), 1.25 (1.13, 1.33) and 1.23 (1.11, 1.33) m/s, respectively. For the middle- and older-aged groups, overall accuracy values for the respective speed thresholds were both over 70%, sensitivities and specificities were between 71.2–88.9%, and AUC values for middle- and older-aged groups were excellent (Metz, 1978). However, we observed relatively lower sensitivity (54.2%), overall accuracy (60.0%) and AUC (68.6%) in young adults.
Table 2.
Walking speed thresholds (m/s) for moderate intensity based on ROC curve analyses
| Threshold (95% CIs), m/s | Sensitivity (%) | Specificity (%) | Accuracy (%) | AUC | PPV (%) | NPV (%) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Young | 1.28 (1.07, 1.38) | 54.2 | 81.2 | 60.0 | 0.69 | 91.4 | 32.5 |
| Middle-aged | 1.25 (1.13, 1.33) | 73.8 | 88.9 | 77.2 | 0.90 | 95.7 | 50.0 |
| Older-aged | 1.23 (1.11, 1.33) | 71.2 | 78.2 | 73.4 | 0.83 | 88.7 | 53.7 |
| Whole sample | 1.28 (1.13, 1.33) | 58.1 | 88.7 | 65.7 | 0.82 | 93.9 | 41.4 |
Note: Young, middle- and older-aged represents participants 21–40, 41–60 and 61–85 years, respectively. Abbreviations: AUC, area under the curve; CI, confidence interval; mph, mile per hour; NPV, negative predictive value; PPV, positive predictive value; ROC, Receiver operating characteristic.
3.3. Comparison of characteristics based on classification (TP, TN, FP and FN)
Table 3 presents the confusion matrix of classification accuracy metrics using the identified age-specific moderate-intensity speed thresholds. Given 75% of the sample achieved ≥ 3 METs, 25% of the participants who walked above 3 METs were misclassified as FN (n = 62). Comparisons (means [SDs]) of descriptive characteristics are presented in Table 4. There was a significant main effect of classification on BMI, waist circumference and walk ratio (p = 0.007, 0.007 and 0.002, respectively). Specifically, participants who were classified as TN had a significantly higher mean BMI compared to the TP and FN groups (mean difference [95% CIs] = 1.8 [0.3, 3.4] and 1.9 [0.1, 5.0] kg/m2, p = 0.01 and 0.03, Cohen’s d = 0.48 and 0.51, respectively); while both TN and FP groups had a greater mean waist circumference than that in the FN group (5.5 [0.08, 10.8] and 9.3 [0.04, 18.6] cm, p = 0.01 and 0.03, d = 0.50 and 0.94, respectively). Moreover, the mean walk ratio of those classified as TP was significantly higher compared to the TN and FN groups (0.4 [0.09, 0.4] and 0.3 [0.02, 0.6], mm/steps/min, p = 0.005 and 0.03, d = 0.55 and 0.13, respectively). No significant differences were observed for height, weight, or leg length (p-values > 0.05).
Table 3.
Confusion matrix displaying the classification of moderate intensity (≥ 3 METs) using the identified age-specific speed thresholds
| Age Group | ≥ Age-specific speed thresholds | ≥ 3 METs |
|
|---|---|---|---|
| Yes | No | ||
|
| |||
| Young | Yes | 32 (42.7%) | 3 (4.0%) |
| No | 27 (46.0%) | 13 (17.3%) | |
| Middle-aged | Yes | 45 (56.9%) | 2 (2.5%) |
| No | 16 (20.3%) | 16 (20.3%) | |
| Older-aged | Yes | 47 (50.0%) | 6 (6.4%) |
| No | 19 (20.2%) | 22 (23.4%) | |
Note: Values represent n (%). Young, middle- and older-aged represents participants 21–40, 41–60 and 61–85 years, respectively. Percentages are calculated as [cell value / total number of bouts] * 100. Abbreviations: METs –metabolic equivalents (1 MET = 3.5 mL/kg/min). Abbreviations: METs, metabolic equivalents (1 MET = 3.5 mL/kg/min).
Table 4.
Comparisons of characteristics based on classifications (Mean [SD])
| Variables | True positivesa (n = 123) |
True negativesb ( n = 51) |
False positivesc ( n = 11) |
False negativesd ( n = 63) |
F value | P |
|---|---|---|---|---|---|---|
|
| ||||||
| Age (years) | 53.1 (17.2) | 55.7 (18.7) | 55.9 (23.3) | 49.2 (20.0) | 1.3 | 0.27 |
| Height (cm) | 170.1 (9.3) | 168.1 (9.2) | 171.0 (10.0) | 168.3 (8.3) | 1.5 | 0.21 |
| Weight (kg) | 73.5 (14.3) | 76.7 (16.2) | 78.8 (8.9) | 71.2 (10.0) | 2.0 | 0.11 |
| BMI (kg/m2) | 25.1 (3.6) | 27.0 (4.3) | 27.0 (3.0) | 25.1 (3.1) | 4.1 | 0.007** |
| Waist Circumference (cm) | 85.1 (11.1) | 89.2 (12.0) | 93.1 (9.6) | 83.7 (10.0) | 4.1 | 0.007** |
| Leg length (cm) | 80.7 (5.5) | 79.4 (5.7) | 80.3 (6.4) | 79.6 (4.8) | 0.9 | 0.45 |
| Walk Ratio (mm/steps/min) | 6.5 (0.8) | 6.1 (0.6) | 6.2 (0.8) | 6.2 (0.7) | 5.1 | 0.002** |
Note: Values are presented as mean (SD).
True positives: ≥ age-specific threshold(s) and ≥ 3 METs
True negatives: < age-specific threshold(s) and < 3 METs
False positives: ≥ age-specific threshold(s) but < 3 METs
False negatives: < age-specific thresholds but ≥ 3 METs.
Abbreviations: BMI = body mass index; SD = standard deviation.
p < 0.01.
3.4. Heuristic moderate-intensity speed threshold during overground walking
The classification accuracy metrics for the candidate moderate intensity heuristic speed thresholds using commonly used units of speed (2.5 vs. 3 mph, and 4.5 vs. 5 km/h) are presented in Table 5. Compared to 2.5 mph, the 3 mph threshold had higher specificity (95.2% vs. 45.2%), PPV (96.6% vs. 83.3%), and Youden’s Index (0.41 vs. 0.37). Similarly, higher specificity (98.4% vs. 75.8%), PPV (98.6% vs. 89.1%) and Youden’s Index (0.42 vs. 0.35) were found for 5 km/h than 4.5 km/h. Moreover, both 2.5 mph and 4.5 km/h had higher FP rates (13.7% and 6.0%, respectively) than their counterparts, meaning that individuals were more likely to be walking below 3 METs when at 2.5 mph or 4.5 km/h. Thus, overall, the 3 mph and 5 km/h thresholds performed better at classifying moderate intensity among the whole sample.
Table 5.
Classification accuracy metrics for identification of moderate intensity (≥ 3 METs) using candidate heuristic speed thresholds expressed in commonly used speed units
| Sensitivity (%) | Specificity (%) | Accuracy (%) | PPV (%) | NPV (%) | True positives n (%) |
True negatives n (%) |
False positives n (%) |
False negatives n (%) |
|
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 2.5 mph | 91.4 | 45.2 | 79.8 | 83.3 | 63.6 | 170 (68.5%) | 28 (11.3%) | 34 (13.7%) | 16 (6.5%) |
| 3 mph | 46.2 | 95.2 | 58.5 | 96.6 | 37.1 | 86 (34.7%) | 59 (23.8%) | 3 (1.2%) | 100 (40.3%) |
|
| |||||||||
| 4.5 km/h | 66.1 | 75.8 | 68.5 | 89.1 | 42.7 | 123 (49.6%) | 47 (19.0%) | 15 (6.0%) | 63 (25.4%) |
| 5 km/h | 36.6 | 98.4 | 52.0 | 98.6 | 34.1 | 68 (27.4%) | 61 (25.0%) | 1 (0.4%) | 118 (47.6%) |
Note: The above values were calculated using the whole sample (i.e., not age specific). The optimal speed threshold for the whole sample is 1.28 m/s, and was converted into 2.87 mph or 4.61 km/h. We herein compared the classification metrics of two sets of candidate heuristic thresholds in different units for ease of interpretation. Abbreviations: METs, metabolic equivalents (1 MET = 3.5 mL/kg/min). NPV, negative predictive value; PPV, positive predictive value.
4. Discussion
The identified speed thresholds (95% CIs) associated with absolutely-defined moderate intensity ranged between 1.23 to 1.28 m/s, and trended lower for older adults. We also observed significant differences in BMI, waist circumference and walk ratio based on classification (TP, TN, FP, and FN groups), indicating these factors might contribute to misclassification using the identified aged-specific speed thresholds. Moreover, for public application, our results supported a heuristic threshold of 3 mph and 5 km/h (compared to 2.5 mph and 4.5 km/h) as an evidence-based, heuristic speed threshold for moderate-intensity overground walking that minimized the probability of misclassification, especially the FN rate.
The identified age-specific thresholds demonstrated good-to-excellent overall performance in the middle- and older-aged groups (AUC values > 0.8), but lower overall accuracy was found in the young group (AUC = 0.69). The difference in the probabilities of achieving (or not) the identified speed thresholds and intensity was expected as the prevalence of achieving ≥ 3 METs was distinct across age groups, i.e., highest in young adults but lowest in older adults (78.7% vs. 70.2%). Notably, all of the optimal speed thresholds identified in the current study were > 2.5 mph, the corresponding speed for 3 METs catalogued by the PA Compendium (Ainsworth et al., 2011). Although 2.5 mph fell on/inside the lower CI for most age-groups, the higher optimal thresholds and upper CIs suggested that a faster speed may be required to elicit a moderate intensity during overground walking. As alluded to previously, this discrepancy might be the result of interpreting previous research that varied in terms of walking conditions and age categories. Similar to the findings in middle-aged and older adults by Parvataneni et al. (2009), Dal et al. (2010) also reported that when walking at a same speed, there was a 6% greater oxygen cost (i.e., volume of oxygen taken up per kilogram body weight per unit distance) under treadmill condition compared to overground walking (0.158 vs. 0.148 mL/kg/m; p < 0.05). Based on Lee & Hidler (2008), individuals modified muscle activation patterns (e.g., greater hip extensor moments but less dorsiflexor and knee extensor moments) and subsequently joint moments and powers (e.g., greater propulsion forces but less braking forces) to maintain relatively constant limb kinematics and spatiotemporal gait parameters, which might lead to a higher metabolic cost than overground walking. Furthermore, previous studies showed that the speed-intensity relationship was also shaped by the sample characteristics (e.g., age). Both Mian et al. (2006) and Peterson & Martin (2010) reported an elevated energy cost (per unit distance) of walking in healthy older adults than young adults (23% and 31% higher, respectively). In the current study, age-specific speed thresholds trended lower from young to middle- and older-aged participants, however, all thresholds were within the 95% CIs across age groups (1.07–1.38 m/s). Thus, our results may support using a single heuristic threshold for all age groups when making general recommendations for moderate-intensity overground walking across the adult age span.
We compared anthropometric and bout characteristics using the identified age-specific speed thresholds to determine the characteristics of those who were correctly classified vs. misclassified. The relatively greater mean BMI and waist circumference in the TN group was not surprising - previous studies have demonstrated that obesity was associated with a slower preferred walking speed (Fernández Menéndez et al., 2019; Malatesta et al., 2009), thus individuals who had greater BMI or waist circumference might also walk slower at their self-selected pace, leading to less energy expenditure when walking at that pace. In addition, individuals classified as obese are known to have a relatively lower resting MET value (Aadland & Anderssen, 2012), and using a standardized MET value (3.5 mL/kg/min) may underestimate their energy expenditure. In turn, this may result in a potential differential misclassification across BMI categories (e.g., higher FN rate). However, when using standardized METs herein, we did not observe any major differences in misclassification (FN and FP) rates among individuals classified as overweight or obese compared to individuals classified as normal-weight (32%, 32% vs. 37% respectively). To address the potential for inter-individual variability in resting metabolic rate, previous studies (Hall et al., 2013; Kozey et al., 2010) have suggested the calculation of individualized METs as an alternative approach to standardized METs (i.e., individualized METs = task VO2 / resting metabolic rate). Although the present study did not include a measure of true resting metabolic rate, we did measure the oxygen uptake of three 5-min seated tasks (resting quietly, watching a movie, and computer work). Means [SDs] of the sitting metabolic rate for obese, overweight, and normal-weight groups were 2.6 [0.6], 2.9 [0.5], and 3.4 [0.7] mL/kg/min, respectively. With this caveat in mind, we conducted an exploratory analysis of individualized METs (calculated using the average metabolic rate of seated tasks) to determine any effects on misclassification rates (Supplementary material 2). Briefly, when using individualized METs, the optimal speed threshold was lower for the obese group (1.02 m/s) compared to the overweight (1.20 m/s) and normal-weight (1.21 m/s) groups. In addition, we observed higher misclassification rates among the obese and overweight groups compared to the normal-weight group for the two heuristic thresholds (3 mph: 84.0%, 61.4% vs. 45.9%; 5 km/h: 84.0%, 70.3% vs. 51.6%, respectively). We noted that this exploratory analysis should be interpreted with caution for several reasons: 1) the sample of obese individuals was small (n = 25) relative to the remaining sample; 2) participants had a mean BMI of 25.6 kg/m2, so we cannot examine how extreme values of BMI might influence misclassification (e.g., the original study excluded individuals with BMI <18.5 kg/m2 or > 40 kg/m2); and 3) there were few FP cases overall, especially among the obese group (n = 0), which impacts the calculation of classification accuracy metrics. Moreover, the greater waist circumference in FP vs. FN groups also indicated that central adiposity might influence the probability of reaching 3 METs even among misclassified individuals. To date, previous studies have predominately focused on BMI as a factor when investigating the effect of obesity on the speed-intensity relationship. Given the significant group differences (based on classification) observed in the current analysis, other obesity-related indicators (e.g., waist circumference) should also be considered in future studies.
Interestingly, we also found that while walking at or above moderate intensity, those who were misclassified as FNs (i.e., below the speed threshold) had a lower walk ratio compared to the TP group (i.e., equal or above the speed threshold), indicating that the walk ratio might influence the intensity of walking at a self-selected pace, and also contribute to misclassification of the speed thresholds. Since the walk ratio (i.e., the relationship between step length and cadence) remains invariant across speed(s) during unconstrained overground or treadmill walking, it represents an innate tendency for locomotor self-optimization that minimizes the metabolic cost of walking and gait variability (Ducharme et al., 2018). Herein, it is plausible that individuals with lower walk ratios in these groups might compensate for shorter step length or relatively poor quality of gait control (Rota et al., 2011), thereby increasing their metabolic cost even while walking below the speed thresholds. Future efforts might also explore whether other spatiotemporal parameters of gait (e.g., gait variability) contribute to the misclassification of the speed thresholds related to specific benchmark intensity values.
In addition, we considered 2.5 vs. 3 mph and 4.5 vs. 5 km/h as two sets of candidate heuristic thresholds based on our obtained optimal thresholds and previous studies (Ainsworth et al., 2011; Parise et al., 2004) for public health application. We herein report lower specificity and PPV values when using the 2.5 mph or 4.5 km/h among the whole sample, meaning that individuals were more likely to be misclassified as FPs (i.e., ≥ speed threshold but < 3 METs). This type of misclassification is particularly undesirable - in practice, individuals might assume they are walking at a moderate intensity based on meeting/exceeding the required speed threshold(s) but their actual intensity is below 3 METs. Note, although higher accuracy values were observed for 2.5 mph or 4.5 km/h, relying only on accuracy is misleading as it is determined by the proportion of true results (TP and TN), and is often considered a poor metric for measuring performance in unbalanced datasets (Devarriya et al., 2020). In contrast, the 3 mph and 5 km/h thresholds had a higher Youden’s Index than their counterparts, which reflects better performance in balancing both sensitivity and specificity. Furthermore, using 3 mph as an example, there was a trade-off in sensitivity (54.2–71.2% vs. 46.2%) and specificity (78.2–88.9% vs. 95.2%) when comparing it to the identified age-specific thresholds. In other words, more individuals were classified as TPs but less as FPs while walking at 3 mph and 5 km/h. Thus, to reduce the risk of misclassification, especially FPs, we recommend 3 mph and 5 km/h as heuristic thresholds for moderate-intensity overground walking. Such a heuristic threshold could be applied in situations where implementing age-specific thresholds is inconvenient (e.g., limitation of equipment or lack of information), or when absolute precision is less important (e.g., making general recommendations to the public).
The present study has several strengths. First, we used criterion standards to assess overground walking speed and intensity (validated electronic gait mat and indirect calorimetry). Second, given the relatively large sex- and age-balanced sample, these findings are generalizable for both men and women across different ages. Third, unlike the majority of previous studies that used constraints to manipulate walking speed or other bouts characteristics (e.g., rhythmic auditory cueing) (Ducharme et al., 2018), we implemented a preferred or self-selected walking pace protocol which is more representative of the natural walking pattern performed in free-living settings (Holt et al., 1995) and also minimizes the potential for additional metabolic cost due to the constraints placed on preferred gait (Dal et al., 2010). To our knowledge, this is the first study to provide age-specific moderate-intensity speed thresholds, and to explore the potential factors that contributed to misclassification of individuals. Nevertheless, several limitations should be acknowledged. First, there were less data points in FP, FN and TN classifications compared to TP due to the prevalence of preferred walking speed and intensity above the identified optimal speed thresholds and/or moderate intensity (3 METs). This may have impacted some of the classification metrics that are based on prevalence (e.g., accuracy). Second, the results from the current analysis are limited to preferred walking speed. Moreover, the use of a short track and the back-and-forth nature of our walking protocol may also add some variability (e.g., extra energy expenditure during turns) to the underlying speed-intensity relationship, yet this variability is difficult to quantify in the present study. Future work should investigate the speed-intensity relationship across a wide range of speeds (i.e., slow, preferred, fast) and also with varying walking conditions (i.e., continuous walking vs. walking with directional changes. Lastly, we only investigated the speed thresholds corresponding with absolute moderate intensity based on its prevalent use in physical activity guidelines. Future research should also investigate other benchmark values in terms of relative intensity (e.g., heart rate reserve).
5. Conclusion
Optimal age-specific overground walking speeds associated with absolutely-defined moderate intensity ranged from 1.23–1.28 m/s, and trended lower for older adults. Notably, all thresholds were greater than the Compendium of Physical Activities threshold (2.5 mph), suggesting that a faster speed is required among all age groups to attain moderate intensity during overground walking. A heuristic threshold of 3 mph or 5 km/h performed better overall in balancing both sensitivity and specificity, and is therefore suggested for use in public health guidelines and application among adults across the age span.
Supplementary Material
Funding
The CADENCE-Adults study was supported by an award NIH NIA Grant 5R01AG049024.
Footnotes
Disclosure of interest
The authors report no conflict of interest.
References
- 2018 Physical Activity Guidelines Advisory Committee Scientific Report. (2018). Washington, DC: U.S. Department of Health and Human Services. [Google Scholar]
- Aadland E, & Anderssen SA (2012). Treadmill calibration of the Actigraph GT1M in young-to-middle-aged obese-to-severely obese subjects. J Obes, 2012, 318176. 10.1155/2012/318176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguiar EJ, Gould ZR, Ducharme SW, Moore CC, McCullough AK, & Tudor-Locke C (2019). Cadence-based Classification of Minimally Moderate Intensity During Overground Walking in 21- to 40-Year-Old Adults. J Phys Act Health, 16(12), 1092–1097. 10.1123/jpah.2019-0261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr., Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, & Leon AS (2011). 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc, 43(8), 1575–1581. 10.1249/MSS.0b013e31821ece12 [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. (1980). Guidelines for graded exercise testing and exercise prescription. Lea & Febiger. [Google Scholar]
- Anjos LA, Wahrlich V, Bossan FM, Salies MN, & Silva PB (2008). Energy expenditure of walking at different intensities in Brazilian college women. Clin Nutr, 27(1), 121–125. 10.1016/j.clnu.2007.09.007 [DOI] [PubMed] [Google Scholar]
- Barkley JE, & Penko A (2009). Physiologic Responses, Perceived Exertion, and Hedonics of Playing a Physical Interactive Video Game Relative to a Sedentary Alternative and Treadmill Walking in Adults. Journal of Exercise Physiology Online, 12(3). [Google Scholar]
- Browning RC, & Kram R (2005). Energetic cost and preferred speed of walking in obese vs. normal weight women. Obes Res, 13(5), 891–899. 10.1038/oby.2005.103 [DOI] [PubMed] [Google Scholar]
- Brun T, Bleiberg F, & Goihman S (1981). Energy expenditure of male farmers in dry and rainy seasons in Upper-Volta. Br J Nutr, 45(1), 67–75. 10.1079/bjn19810077 [DOI] [PubMed] [Google Scholar]
- Cohen J (2013). Statistical power analysis for the behavioral sciences. Academic press. [Google Scholar]
- Dal U, Erdogan T, Resitoglu B, & Beydagi H (2010). Determination of preferred walking speed on treadmill may lead to high oxygen cost on treadmill walking. Gait Posture, 31(3), 366–369. 10.1016/j.gaitpost.2010.01.006 [DOI] [PubMed] [Google Scholar]
- de Guzman MPE, Cabrera JP, et al. (1978). A study of the energy expenditure, dietary intake and pattern of daily activity among various occupational groups: clerk-typist. Philippine Journal of Nutrition, 31, 147–156. [Google Scholar]
- de Guzman MPE, Cabrera JP, et al. (1984). A study of energy expenditure, dietary intake and pattern of daily activity among various occupational group - Laguna Rice farmers. Philippine Journal of Nutrition, 37, 1–5. [Google Scholar]
- de Guzman MPE, Recto MRC, et al. (1979). A study of the energy expenditure, dietary intake and pattern of daily activity among various occupational groups - Textile Mill workers. Philippine Journal of Nutrition, 32, 134–148. [Google Scholar]
- Devarriya D, Gulati C, Mansharamani V, Sakalle A, & Bhardwaj A (2020). Unbalanced breast cancer data classification using novel fitness functions in genetic programming. Expert Systems with Applications, 140, 112866. [Google Scholar]
- Dill DB (1965). Oxygen used in horizontal and grade walking and running on the treadmill. J Appl Physiol, 20, 19–22. 10.1152/jappl.1965.20.1.19 [DOI] [PubMed] [Google Scholar]
- Ducharme SW, Sands CJ, Moore CC, Aguiar EJ, Hamill J, & Tudor-Locke C (2018). Changes to gait speed and the walk ratio with rhythmic auditory cuing. Gait Posture, 66, 255–259. 10.1016/j.gaitpost.2018.09.006 [DOI] [PubMed] [Google Scholar]
- Dufour DL (1984). The time and energy expenditure of indigenous women horticulturalists in the northwest Amazon. Am J Phys Anthropol, 65(1), 37–46. 10.1002/ajpa.1330650107 [DOI] [PubMed] [Google Scholar]
- Fernández Menéndez A, Saubade M, Hans D, Millet GP, & Malatesta D (2019). The Determinants of the Preferred Walking Speed in Individuals with Obesity. Obes Facts, 12(5), 543–553. 10.1159/000501968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, & Altman DG (2016). Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. European journal of epidemiology, 31(4), 337–350. 10.1007/s10654-016-0149-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Howe CA, Rana SR, Martin CL, & Morey MC (2013). METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exerc, 45(3), 574–582. 10.1249/mss.0b013e318276c73c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt KJ, Jeng SF, Rr RR, & Hamill J (1995). Energetic Cost and Stability During Human Walking at the Preferred Stride Velocity. J Mot Behav, 27(2), 164–178. 10.1080/00222895.1995.9941708 [DOI] [PubMed] [Google Scholar]
- Kozey S, Lyden K, Staudenmayer J, & Freedson P (2010). Errors in MET estimates of physical activities using 3.5 ml· kg− 1· min− 1 as the baseline oxygen consumption. J Phys Act Health, 7(4), 508–516. 10.1123/jpah.7.4.508 [DOI] [PubMed] [Google Scholar]
- Lee SJ, & Hidler J (2008). Biomechanics of overground vs. treadmill walking in healthy individuals. J Appl Physiol (1985), 104(3), 747–755. 10.1152/japplphysiol.01380.2006 [DOI] [PubMed] [Google Scholar]
- Malatesta D, Vismara L, Menegoni F, Galli M, Romei M, & Capodaglio P (2009). Mechanical external work and recovery at preferred walking speed in obese subjects. Med Sci Sports Exerc, 41(2), 426–434. 10.1249/MSS.0b013e31818606e7 [DOI] [PubMed] [Google Scholar]
- Metz CE (1978). Basic principles of ROC analysis. Semin Nucl Med, 8(4), 283–298. 10.1016/s0001-2998(78)80014-2 [DOI] [PubMed] [Google Scholar]
- Mian OS, Thom JM, Ardigò LP, Narici MV, & Minetti AE (2006). Metabolic cost, mechanical work, and efficiency during walking in young and older men. Acta Physiol (Oxf), 186(2), 127–139. 10.1111/j.1748-1716.2006.01522.x [DOI] [PubMed] [Google Scholar]
- Morris JN, & Hardman AE (1997). Walking to health. Sports Med, 23(5), 306–332. 10.2165/00007256-199723050-00004 [DOI] [PubMed] [Google Scholar]
- Murtagh EM, Boreham CA, & Murphy MH (2002). Speed and exercise intensity of recreational walkers. Prev Med, 35(4), 397–400. 10.1006/pmed.2002.1090 [DOI] [PubMed] [Google Scholar]
- Parise C, Sternfeld B, Samuels S, & Tager IB (2004). Brisk walking speed in older adults who walk for exercise. J Am Geriatr Soc, 52(3), 411–416. 10.1046/j.0002-8614.2003.52114.x [DOI] [PubMed] [Google Scholar]
- Parvataneni K, Ploeg L, Olney SJ, & Brouwer B (2009). Kinematic, kinetic and metabolic parameters of treadmill versus overground walking in healthy older adults. Clin Biomech (Bristol, Avon), 24(1), 95–100. 10.1016/j.clinbiomech.2008.07.002 [DOI] [PubMed] [Google Scholar]
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, & et al. (1995). Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Jama, 273(5), 402–407. 10.1001/jama.273.5.402 [DOI] [PubMed] [Google Scholar]
- Peterson DS, & Martin PE (2010). Effects of age and walking speed on coactivation and cost of walking in healthy adults. Gait Posture, 31(3), 355–359. 10.1016/j.gaitpost.2009.12.005 [DOI] [PubMed] [Google Scholar]
- Rosdahl H, Gullstrand L, Salier-Eriksson J, Johansson P, & Schantz P (2010). Evaluation of the Oxycon Mobile metabolic system against the Douglas bag method. Eur J Appl Physiol, 109(2), 159–171. 10.1007/s00421-009-1326-9 [DOI] [PubMed] [Google Scholar]
- Rota V, Perucca L, Simone A, & Tesio L (2011). Walk ratio (step length/cadence) as a summary index of neuromotor control of gait: application to multiple sclerosis. Int J Rehabil Res, 34(3), 265–269. 10.1097/MRR.0b013e328347be02 [DOI] [PubMed] [Google Scholar]
- Saevereid HA, Schnohr P, & Prescott E (2014). Speed and duration of walking and other leisure time physical activity and the risk of heart failure: a prospective cohort study from the Copenhagen City Heart Study. PLoS One, 9(3), e89909. 10.1371/journal.pone.0089909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torún B, McGuire J, & Mendoza RD (1982). Energy cost of activities and tasks of women from a rural region of Guatemala. Nutrition research, 2(2), 127–136. [Google Scholar]
- Tudor-Locke C, Aguiar EJ, Han H, Ducharme SW, Schuna JM Jr., Barreira TV, Moore CC, Busa MA, Lim J, Sirard JR, Chipkin SR, & Staudenmayer J (2019). Walking cadence (steps/min) and intensity in 21–40 year olds: CADENCE-adults. Int J Behav Nutr Phys Act, 16(1), 8. 10.1186/s12966-019-0769-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C, Ducharme SW, Aguiar EJ, Schuna JM Jr., Barreira TV, Moore CC, Chase CJ, Gould ZR, Amalbert-Birriel MA, Mora-Gonzalez J, Chipkin SR, & Staudenmayer J (2020). Walking cadence (steps/min) and intensity in 41 to 60-year-old adults: the CADENCE-adults study. Int J Behav Nutr Phys Act, 17(1), 137. 10.1186/s12966-020-01045-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C, Mora-Gonzalez J, Ducharme SW, Aguiar EJ, Schuna JM Jr., Barreira TV, Moore CC, Chase CJ, Gould ZR, Amalbert-Birriel MA, Chipkin SR, & Staudenmayer J (2021). Walking cadence (steps/min) and intensity in 61–85-year-old adults: the CADENCE-Adults study. Int J Behav Nutr Phys Act, 18(1), 129. 10.1186/s12966-021-01199-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster KE, Wittwer JE, & Feller JA (2005). Validity of the GAITRite® walkway system for the measurement of averaged and individual step parameters of gait. Gait & posture, 22(4), 317–321. 10.1016/j.gaitpost.2004.10.005 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020). WHO guidelines on physical activity and sedentary behaviour: at a glance. [DOI] [PMC free article] [PubMed]
- Youden WJ (1950). Index for rating diagnostic tests. Cancer, 3(1), 32–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


