Abstract
Purpose:
To compare the clinical characteristics and high-resolution optical coherence tomography (HR-OCT) findings between corneal squamous metaplasia and ocular surface squamous neoplasia (OSSN).
Methods:
A retrospective case control study of eight patients, four with histologically confirmed squamous metaplasia and four with histologically confirmed OSSN, that presented to the Miami Veterans Administration Medical Center and Bascom Palmer Eye Institute between 2016 and 2020, was performed. Clinical characteristics, HR-OCT findings, and pathology were evaluated and compared.
Results:
Four patients with squamous metaplasia and four with OSSN were evaluated. In the metaplasia group, 75% were male, two were white, and two were black. In the OSSN group, all four were white males. All lesions were opalescent and occurred at the limbus; however, the borders were more smooth and rounded in the metaplastic lesions compared to OSSN. HR-OCT findings were indistinguishable between the two groups.
Conclusion:
There is overlap in clinical characteristics and HR-OCT findings between corneal squamous metaplasia and OSSN, highlighting one limitation of HR-OCT. As such, if a corneal opacity has some but not all HR-OCT findings of OSSN, squamous metaplasia should also be considered. A biopsy may be indicated to further evaluate and guide treatment.
Keywords: Ocular surface squamous neoplasia, corneal lesion, squamous metaplasia, high-resolution OCT
Introduction
Ocular surface squamous neoplasia (OSSN) represents a spectrum of epithelial squamous malignancies, ranging from dysplasia to invasive squamous cell carcinoma, that affects the cornea and conjunctiva.1,2 It is the most common ocular surface tumor in adults.1,2 OSSN typically presents as a limbal lesion with irregular borders and hairpin configuration of associated vessels at 3 or 9 o’clock and may have leukoplakic or gelatinous features.3 However, presentation can be variable, and clinical exam cannot always reliably distinguish OSSN from benign lesions.
High-resolution optical coherence tomography (HR-OCT) was introduced in the early 2000s and is used as an in vivo diagnostic modality for OSSN.4 Three key features of OSSN on HR-OCT include hyperreflectivity, thickened epithelium, and an abrupt transition between normal and abnormal tissue.5 These features have been shown to have a 94–100% sensitivity and a 100% specificity for diagnosing OSSN.6–7 HR-OCT has also been shown to aid in the detection of OSSN in individuals with concomitant ocular surface diseases, such as corneal scarring, limbal stem cell deficiency, and Salzmann’s nodular degeneration.4,8 Furthermore, HR- OCT has been used to help monitor disease resolution as it can highlight areas of residual subclinical disease, preventing early termination of topical therapy.9 Finally, HR-OCT can assist the surgeon in obtaining appropriate margins at the time of excisional biopsy.10 Overall, HR-OCT has become a valuable tool in all stages of the disease process, assisting with tumor diagnosis, monitoring the effect of treatment, and examining for disease recurrence.
While HR-OCT is a powerful addition to the work-up and management of OSSN, there are instances of non-neoplastic lesions presenting with characteristics similar to OSSN on imaging. We present four cases of squamous metaplasia that are indistinguishable from OSSN on HR-OCT. These cases required incisional biopsy and histopathological examination to differentiate between metaplasia and neoplasia.
Materials and Methods
This is a retrospective chart review of eight patients with clinical findings suspicious for OSSN who presented to the Miami Veterans Administration Medical Center and the Bascom Palmer Eye Institute at the University of Miami in Miami, Florida. The institutional review boards of the Miami Veterans Administration Medical Center and the University of Miami approved this retrospective study and the methods adhered to the tenets of the Declaration of Helsinki.
Chart review from 2016 to 2021 captured history, exam findings, and histopathological results. The epithelial thickness of each suspicious lesion was quantified by comparing it to the normal epithelium in the same scan (reported as a fold increase in thickening). An incisional biopsy was performed at the slit lamp in all patients with the majority of visible abnormalities removed. Margins were not prioritized, and neither absolute alcohol nor cryotherapy were used at the time of incisional biopsy. All patients with biopsy proven OSSN received topical chemotherapy for residual disease after incisional biopsy
Results
Eight total patients with clinical findings suspicious for OSSN were evaluated with HR-OCT and eventual incisional biopsy. Four patients, two white and two black, had biopsy-proven squamous metaplasia. The other four patients, all white, had biopsy confirmed OSSN. All individuals had opalescent corneal lesions. The lesions themselves were not vascular and feeder vessels were not noted on examination. In the metaplasia group, 1 lesion was in the inferotemporal quadrant and 3 were in the nasal quadrant. Similarly, in the OSSN group, 1 lesion was in the inferotemporal quadrant and 3 lesions in the nasal quadrant. No lesions in either group were bilateral. HR-OCT images were similar in all 8 cases, showing two out of three of the following characteristics: hyperreflectivity, thickened epithelium, and/or an abrupt transition between normal and abnormal tissue. The cases are summarized below.
Metaplasia: Cases 1–4
Case 1 (Figure 1)
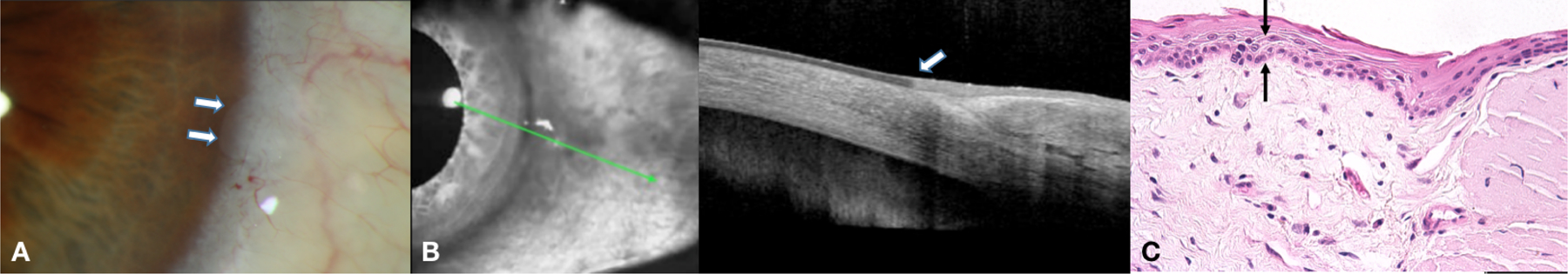
Figure 1.

a. Slit lamp photograph of a 72-year-old black male with a left nasal limbal opacity at 9 o’clock with smooth round borders. b. HR-OCT demonstrating a hyperreflective, thickened epithelium with an abrupt transition between normal and abnormal tissue. c. Examination discloses acanthotic mucosal epithelium with a focus of overlying keratosis (asterisk) and melanosis without atypia present at the basal aspect of the tissue (arrows) (Hematoxylin and eosin, original magnification × 400).
A 72-year-old black male with a 20-pack year smoking history presented for evaluation of a left, opalescent, smooth nasal corneal lesion at 9 o’clock. HR-OCT was characteristic for OSSN with hyperreflective, thickened epithelium (2.2X as compared to normal) and an abrupt transition from normal to abnormal epithelium. He was started on topical interferon alfa-2b (INFα2b). After one month of treatment, no change in the lesion was noted and a biopsy was performed which demonstrated squamous metaplasia of the cornea and melanosis without atypia of the conjunctiva. INFα2b was discontinued and the patient has remained under observation without any changes in his corneal lesion.
Case 2 (Figure 2)
Figure 2.

a. Slit lamp photograph of an 83-year-old white male with a bilobed left opalescent nasal limbal opacity at 8:30 o’clock with overall smooth borders. b. HR-OCT demonstrating a hyperreflective, thickened epithelium with an abrupt transition between normal and abnormal tissue. The epithelium of the limbal conjunctiva was normal. c. Examination discloses acanthotic epithelium with squamous metaplasia and melanosis without atypia (arrows) overlying substantia propria that contains a moderate-to-marked amount of solar elastosis (asterisk) (Hematoxylin and eosin, original magnification × 400).
An 83-year-old white male with a history of excess sun exposure presented for evaluation of a smooth, bilobed, opalescent lesion of the left nasal cornea at 8:30 o’clock. HR-OCT had several features characteristic of OSSN, including a hyperreflective, thickened epithelium (2.0X as compared to normal) with an abrupt transition from abnormal to normal epithelium. Biopsy revealed squamous metaplasia of the cornea and melanosis without atypia of the conjunctiva. As such, the patient has remained under observation with no change in lesion characteristics.
Case 3 (Figure 3)
Figure 3.

a. Slit lamp photograph of a 61-year-old white male with a bilobed left nasal corneal opacity with mostly smooth borders. b. HR-OCT showed a hyperreflective, thickened epithelium with an abrupt transition between normal and abnormal tissue suggesting OSSN. c. Examination discloses acanthotic epithelium, with no dysplasia, overlying substantia propria that contains a mild amount of solar elastosis (asterisk) (Hematoxylin and eosin, original magnification × 400).
A 61-year-old white male with an insignificant past medical history was referred for a left, bilobed, smooth nasal corneal opacity at 4 o’clock with HR-OCT suggestive of OSSN (hyperreflective, thickened epithelium (2.5X as compared to normal) with an abrupt transition). Biopsy demonstrated squamous metaplasia of the cornea and melanosis without atypia of the conjunctiva. The patient has remained under observation with no change in lesion characteristics.
Case 4 (Figure 4)
Figure 4.

a. Slit lamp photograph of a 48-year-old black female with a left opalescent, gelatinous, inferotemporal limbal corneal lesion with irregular borders. b. HR-OCT showing a thickened, hyperreflective epithelium without an abrupt transition. c. Examination discloses acanthotic epithelium with squamous metaplasia overlying substantia propria that contains solar elastosis (asterisk) and a chronic inflammatory cell infiltrate (arrows) (Hematoxylin & eosin, original magnification × 200).
A 48-year-old black female with a history of excess sun exposure presented with a left opalescent, slightly irregular, and gelatinous corneal lesion inferotemporal at 4 o’clock adjacent to a pinguecula. The lesion stained with Lissamine green and HR-OCT was concerning for OSSN with a thickened (2.7X as compared to normal), hyperreflective epithelium heaped on top of normal epithelium. However, there was not an abrupt transition. The patient underwent a biopsy that confirmed squamous metaplasia. No treatment was indicated, and the patient has remained under observation.
OSSN: Cases 5–8
Case 5 (Figure 5)
Figure 5.

a. Slit lamp photograph of a 76-year-old white male with a right slightly elevated inferonasal limbal corneal lesion with irregular borders. b. HR-OCT showing a thickened, hyperreflective epithelium with an abrupt transition. c. Examination discloses conjunctival epithelium with faulty maturational sequencing that extends up to full thickness (carcinoma in situ) (between arrows) (Hematoxylin and eosin, original magnification × 400).
A 76-year-old white male smoker (unknown pack years) was referred for a right irregular, elevated, nasal, limbal corneal lesion at 4 o’clock. HR-OCT suggested the diagnosis of OSSN with a hyperreflective, thickened epithelium (1.8X as compared to normal) and abrupt transition. A biopsy confirmed corneal epithelial carcinoma in situ and the patient received 4 cycles of topical 5-fluorouracil 1% (5FU) with resolution of OSSN.
Case 6 (Figure 6)
Figure 6.
a. Slit lamp photograph of a 68-year-old white male with a right corneal nasal opacity at 3 o’clock with mostly smooth borders. b. HR- OCT demonstrated a thickened, hyperreflective epithelium with an abrupt transition. c. Examination discloses faulty epithelial maturational sequencing that extends up to approximately half thickness (arrow) with overlying substantia propria that contains a mild amount of solar elastosis, (corneal intraepithelial neoplasia: dysplasia, moderate) (between arrows) (Hematoxylin and eosin, original magnification × 400).
A 68-year-old white male with a history of basal cell carcinoma and 8-pack year smoking history was referred for evaluation of a right, smooth, nasal corneal opacity at 3 o’clock next to a pinguecula. An abrupt transition with hyperreflective, thickened epithelium (1.8X as compared to normal) was seen on HR-OCT suggesting OSSN and biopsy confirmed corneal dysplasia. He was treated with topical INFα2b for 3 months with resolution of the lesion.
Case 7 (Figure 7)
Figure 7.

a. Slit lamp photograph of a 77-year-old white male with a right inferotemporal corneal opacity with irregular borders. b. HR-OCT demonstrated thickened hyperreflective epithelium with abrupt transition. c. Examination discloses faulty epithelial maturational sequencing that extends up to near full thickness (between arrows) with a thin layer of overlying mature epithelium (asterisk), (corneal intraepithelial neoplasia: dysplasia, severe) (Hematoxylin and eosin, original magnification × 400).
A 77-year-old white male with a history of cutaneous squamous cell carcinoma presented with a right, inferotemporal, corneal opacity with irregular borders at 8 o’clock. HR-OCT showed a hyperreflective, thickened epithelium (1.8X as compared to normal) with an abrupt transition between abnormal and normal epithelium, consistent with OSSN. Biopsy revealed corneal dysplasia. The patient was treated with topical INFα2b for 5 months with no response and then switched to topical 5FU, with subsequent resolution of the OSSN after 3 cycles of therapy.
Case 8 (Figure 8)
Figure 8.

a. Slit lamp photo of a 78-year-old white male who presented with a right nasal corneal opacity with irregular borders. b. HR-OCT revealed a thickened, hyperreflective epithelium with an abrupt transition point. c. Examination discloses faulty epithelial maturational sequencing that extends up to approximately half thickness (between arrows) (cornea intraepithelial neoplasia: dysplasia, moderate) (Hematoxylin & eosin, original magnification × 400).
A 78-year-old white male with a history of multiple cutaneous squamous cell carcinomas presented with a right, nasal corneal opacity at 3 o’clock with irregular borders, and HR-OCT was consistent with OSSN given hyperreflective, thickened epithelium (2.0X as compared to normal) and an abrupt transition. Corneal biopsy revealed dysplasia. The patient was treated with 5 cycles of topical 5FU with complete resolution of the lesion.
Discussion
We report four cases of ocular surface squamous metaplasia and four cases of corneal OSSN that presented with similar HR-OCT findings. All cases were of opalescent corneal lesions in the exposure zone with at least 2 out of 3 HR-OCT characteristics suggestive of OSSN. Seven of eight had a HR-OCT showing hyperreflectivity, an abrupt transition, and variable thickening. Case 4 had hyperreflectivity and epithelial thickening but did not have an abrupt transition.
Despite similar HR-OCT features, there were some notable differences on examination. First, 2 individuals with metaplasia were black versus the OSSN group where all individuals were white. This is consistent with prior studies as individuals with OSSN are most often white males in their seventh decade of life.1–3 Second, some differences were noted in the clinical characteristics of the lesions, with irregular borders noted in 1 metaplasia case and 3 OSSN cases. Though all squamous metaplasia cases involved the left eye and all OSSN cases involved the right eye, both groups demonstrated similarities with regards to lesion location in the exposure zone, with a nasal location in 75% of lesions in each group. Notably, none of the lesions had vascular abnormalities.
The strongest risk factor for OSSN is exposure to ultra-violet (UV) light, with other factors such as HPV infection, systemic immunosuppression, and smoking perhaps having contributary roles.11 Risk factors for metaplasia include chronic ocular surface inflammation, xerophthalmia, and vitamin A and zinc deficiencies.12 When confronted with a suspicious lesion, the first goal of ophthalmologists is to exclude vision threatening neoplasia. However, in cases that are less clinically suspicious for OSSN, such as lesions seen in black individuals, or lesions that present with rounded and regular borders, it is important to address risk factors that may manifest with metaplasia. The clinician must inquire about symptoms of vitamin deficiency, such as difficulties with night vision; and about conditions that may impact vitamin metabolism, such as poor diet, alcoholism, inflammatory bowel disease, and bariatric surgery; and pursue work up in appropriate cases. In our cohort of squamous metaplasia cases, 2 patients had excess sun exposure while 1 had a history of smoking. Comparatively, 3 patients with OSSN had a history of skin cancer while 1 also had a history of smoking. Interestingly, none of our patients with squamous metaplasia had typical risk factors for metaplasia but 3 had risk factors for OSSN, highlighting the potential for overlapping features between the two conditions.
In our series, all patients had similar findings on HR-OCT. To understand why cases of squamous metaplasia appear similar to OSSN on HR-OCT, shared pathologic findings must be considered. Histologically, the epithelium in OSSN demonstrates hyperplasia, surface keratinization, loss of goblet cells, loss of cell polarity, nuclear hyperchromasia and pleomorphism, and mitotic figures. On histopathology, metaplasia shares some of these features including epithelial thickening, loss of goblet cells, and keratinization. The shared features between the two conditions likely explain the overlap in HR-OCT finding. Missing from metaplasia are dysplasia and mitotic figures12–14, features that cannot be detected on HR-OCT due to resolution issues.11 In theory, these features may be detected with in vivo confocal microscopy (IVCM), a device that has higher resolution than HR-OCT and can thus demonstrate microscopic features of a lesion. In IVCM for OSSN, one can expect to see features of neoplastic epithelial cells such as hyperreflective nuclei, heteromorphic and hyperreflective borders, an abrupt transition zone between normal and abnormal cells, and possibly mitotic figures.14–15 However, an East African study found that it was also difficult to distinguish between OSSN and benign lesions on IVCM given an overlap in findings, including irregular sized, hyperreflective cells, and prominent nucleoli in malignant and benign cases.16
Given the examples above, if treatment for OSSN is solely based on HR-OCT, or even confocal microscopy findings, it is possible that a small subset of patients with squamous metaplasia could potentially undergo unnecessary therapies and procedures. The key point of this study is to highlight that if a patient does not fit the demographics of OSSN or if a lesion does not respond to topical chemotherapy, an alternative diagnosis should be considered, and an incisional biopsy performed.
As with all studies, our findings must be considered bearing in mind the study limitations which include a retrospective review with a limited number of patients. All of our cases were corneal lesions and thus had minimal epithelial thickening. In addition, our first case of metaplasia was treated with topical INFα2b prior to biopsy, which may have affected the pathology results. Despite these limitations, the strength of the study is that it highlights a limitation of HR-OCT, the inability to differentiate between metaplasia and dysplasia of corneal lesions, which is important for clinicians to recognize. Interestingly, it was the clinical exam that was most helpful in guiding us to a correct diagnosis, specifically the presence of darkly-pigmented skin and lesions with round borders.
To conclude, in cases of opalescent corneal opacities and HR-OCT findings that demonstrate features suggestive of OSSN (i.e., epithelial thickening, hyperreflectivity, and abrupt transition from normal to abnormal epithelium), the clinician should consider metaplasia in the appropriate clinical setting. Histopathological examination remains the gold standard for the diagnosis of OSSN and an incisional biopsy should be considered when needed. Finally, the frequency of conversion from metaplasia to dysplasia (and vice versa with treatment of OSSN) is unknown and future studies are needed to further examine this question.
Funding
Supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences R&D (CSRD) I01 CX002015 (Dr. Galor) and Biomedical Laboratory R&D (BLRD) Service I01 BX004893 (Dr. Galor), Department of Defense Gulf War Illness Research Program (GWIRP) W81XWH-20-1-0579 (Dr. Galor) and Vision Research Program (VRP) W81XWH-20-1-0820 (Dr. Galor), National Eye Institute R01EY026174 (Dr. Galor) and R61EY032468 (Dr. Galor), NIH Center Core Grant P30EY014801 (institutional) and Research to Prevent Blindness Unrestricted Grant (institutional), Dr. Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The Robert Farr Family Grant, The Grant and Diana Stanton-Thornbrough, The Robert Baer Family Grant, The Roberto and Antonia Menendez Grant, The Emilyn Page and Mark Feldberg Grant, The Calvin and Flavia Oak Support Fund, The Robert Farr Family Grant, The Jose Ferreira de Melo Grant, The Richard and Kathy Lesser Grant, The Honorable A. Jay Cristol Grant, The Michele and Ted Kaplan Grant and the Richard Azar Family Grant (institutional grants).
Footnotes
Conflicts of Interest
No conflicting relationship exists for any author.
References
- 1.Grossniklaus HE, Green WR, Luckenbach M, Chan CC. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea. 1987;6(2):78–116. [DOI] [PubMed] [Google Scholar]
- 2.Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39(6):429–450. [DOI] [PubMed] [Google Scholar]
- 3.Kiire CA, Srinivasan S, Karp CL. Ocular surface squamous neoplasia. Int Ophthalmol Clin. 2010;50(3):35–46. [DOI] [PubMed] [Google Scholar]
- 4.Shousha MA, Karp CL, Perez VL, et al. , Diagnosis and management of conjunctival and corneal intraepithelial neoplasia using ultra high-resolution optical coherence tomography, Ophthalmology, vol. 118, no. 8, pp. 1531–1537, 2011. [DOI] [PubMed] [Google Scholar]
- 5.Thomas BJ, Galor A, Nanji AA, et al. Ultra high-resolution anterior segment optical coherence tomography in the diagnosis and management of ocular surface squamous neoplasia. Ocul Surf. 2014;12(1):46–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kieval JZ, Karp CL, Abou Shousha M, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology. 2012;119(3):481–486. [DOI] [PubMed] [Google Scholar]
- 7.Nanji AA, Sayyad FE, Galor A, Dubovy S, Karp CL. High-Resolution Optical Coherence Tomography as an Adjunctive Tool in the Diagnosis of Corneal and Conjunctival Pathology. Ocul Surf. 2015;13(3):226–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atallah M, Joag M, Galor A, et al. Role of high resolution optical coherence tomography in diagnosing ocular surface squamous neoplasia with coexisting ocular surface diseases. Ocul Surf. 2017;15(4):688–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tran AQ, Venkateswaran N, Galor A, Karp CL. Utility of high-resolution anterior segment optical coherence tomography in the diagnosis and management of sub-clinical ocular surface squamous neoplasia. Eye Vis (Lond). 2019;6:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karp CL, Mercado C, Venkateswaran N, et al. Use of High-Resolution Optical Coherence Tomography in the Surgical Management of Ocular Surface Squamous Neoplasia: A Pilot Study. Am J Ophthalmol. 2019;206:17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sayed-Ahmed IO, Palioura S, Galor A, Karp CL. Diagnosis and Medical Management of Ocular Surface Squamous Neoplasia. Expert Rev Ophthalmol. 2017;12(1):11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobayashi A, Wajima R, Sugiyama K, Nonomura A, Huang AJ. Idiopathic limbal squamous metaplasia. Arch Ophthalmol. 2003;121(10):1473–1475. [DOI] [PubMed] [Google Scholar]
- 13.Mittal R, Rath S, Vemuganti GK. Ocular surface squamous neoplasia - Review of etio-pathogenesis and an update on clinico-pathological diagnosis. Saudi J Ophthalmol. 2013;27(3):177–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weisenthal RW, American Academy of Ophthalmology. External disease and cornea, 2020–2021. 2020–2021. ed. San Francisco, CA: American Academy of Ophthalmology; 2020. [Google Scholar]
- 15.Venkateswaran N, Sripawadkul W, Karp CL. The role of imaging technologies for ocular surface tumors. Curr Opin Ophthalmol. 2021;32(4):369–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguena MB, van den Tweel JG, Makupa W, et al. Diagnosing ocular surface squamous neoplasia in East Africa: case-control study of clinical and in vivo confocal microscopy assessment. Ophthalmology. 2014;121(2):484–491. [DOI] [PMC free article] [PubMed] [Google Scholar]


