Abstract
Background
The COVID-19 pandemic has had negative effects on mental health. Understanding sex and age differences in the perception of stressors, the use of coping strategies, and the prevalence of depression and anxiety can lead to detecting at-risk groups.
Methods
A cross-sectional online study surveyed perceived stressors, coping strategies, and the PHQ-9 and GAD-7 rating scales for symptoms of depression and anxiety. The study was open from Spring 2020 to Spring 2021 and was aimed at children, adolescents and young adults of Latin America.
Results
The survey was completed by 3965 participants (63.8% females). The sample was divided into children (N = 621, 15.7%), adolescents (N = 1123, 28.3%) and young adults (N = 2021, 56%). Moderate to severe symptoms of depression and anxiety were found in 43.53% and 27%, respectively, being more frequent in females. Children of both sexes showed the lowest scores in rating scales. Adult females reported a higher level of stress in regards to pandemic news, having someone close diagnosed with COVID-19,the possibility of getting sick, academic delays, economic impact, and depression, while female adolescents reported a higher level of stress regarding the lockdown, losing contact with peers and anxiety. In juxtaposition, females also reported a higher frequency of positive coping strategies. A multivariate analysis confirmed the association of several variables with the presence of depression and anxiety.
Conclusion
A high prevalence of depression and anxiety was found among young people. Specific intervention programs must be created taking into account age and sex differences.
Keywords: COVID-19, Pediatric, Depression, Anxiety, Latin America
1. Introduction
In November 2019, the first human case of COVID-19 caused by SARS-CoV-2 was reported in Wuhan, China. In the following months, the virus spread across the globe, forcing numerous countries into lockdown and shutting down non-essential activities. By June 2022, the World Health Organization (WHO) had reported over 535 million cases and 6.32 million deaths worldwide (World Health Organization,). Strategies to mitigate COVID-19 transmission, and stressors such as inadequate or insufficient information, fears of getting sick, financial loss, and long quarantine duration fostered mental health problems, such as depression and anxiety (Brooks et al., 2020).
The effects of the stress resulting from the COVID-19 pandemic have been reported in children, adolescents, and young adults in different countries. Studies from China (Duan et al., 2020; Liu et al., 2020; Ma et al., 2021; Wang et al., 2020; Xie et al., 2020), India (Saurabh and Ranjan, 2020), the United States of America (Hawes et al., 2021), Canada (Cost et al., 2021), Australia, (Li et al., 2021), Spain (Lavigne-Cerván et al., 2021) and Germany (Ravens-Sieberer et al., 2021) have shown that a large percentage of the population manifested symptoms of depression (from 7.2% to 62.1%) and anxiety (from 18.9% to 66.9%). Staying at home for extended periods, not attending school, lack of interaction with peers, having a family member or friend become infected with COVID-19, and limiting physical activity were identified as the main stressors in this age groups (Duan et al., 2020; Ravens-Sieberer et al., 2021; Yeasmin et al., 2020). In addition, being female was associated with an increased risk of developing depression and anxiety (Moccia et al., 2020; Wathelet et al., 2020).
The frequencies of some maladaptive behaviors among the general population during the pandemic were also examined. Non-suicidal self-injuries (NSSI) were reported in 42% of children and adolescents (Zhang et al., 2020) and in 7%–9% of adults (Paul and Fancourt, 2022); while substance use was reported in 25%–30% of adolescents (Larrea-Schiavon et al., 2021; Dumas et al., 2020) and adults (Czeisler et al., 2020; Horigian et al., 2021). Meanwhile, positive coping strategies, such as the use of preventive measures (e.g., hand washing, social distance), or exercising, demonstrated a protective effect against stress, anxiety, and depression (Alkhamees et al., 2020; de Abreu et al., 2022; Peng et al., 2022).
Latin America, a region that includes low- and middle-income countries with more youths than adults and scarce mental health services, has suffered from particularly negative outcomes during the current pandemic, with more than 155 million registered cases, over 2.7 million deaths (WHO, 2022) and a drop of 8.5% in the gross domestic product (International Monetary Fund, 2022). These issues underlie the importance of examining the impact of the pandemic on the mental health of people in this region of the world, considering that only reports from individual countries are available (Canet, 2020; Larraguibel et al., 2021; Rusca-Jordán et al., 2020).
To examine the impact of the pandemic on mental health, as well as the coping strategies in young people, we performed an online study based on a self-reporting questionnaire and targeted various Latin American countries. The aims of this research were a) to evaluate age and sex differences in the frequency and severity of symptoms of depression and anxiety, b) to examine age and sex differences in the perceived stressors and coping strategies and, c) to identify which perceived stressors and coping strategies are associated with the presence of depression and anxiety.
2. Material and methods
The study was approved by the Institutional Review Board of participant institutions which examined the research methods to ensure that they fulfilled the statement of ethical principles in the Declaration of Helsinki.
This survey was conducted from April 2020 to April 2021. Data was gathered via Google Forms, a survey management software that is included in the Docs Editors suite offered by Google (Google, 2021). The survey was aimed at respondents between the ages of 8–24 years, whose answers were anonymous.
The sample was obtained using the snowball sampling method, which is based on referrals from initial subjects to generate additional participants. This method facilitates recruitment by asking respondents and key contact persons such as teachers and health professionals to share the questionnaire with their friends and family through social networks (Dudovskiy, 2022). The questionnaire contained an informed consent section explaining the study purpose, procedures, risks, and benefits. Consent to participate in the study was confirmed by selecting a checkbox. In the case of minors two checkboxes were displayed (one for the parent and one for the child) and respondents were able to proceed only after both boxes were checked. The survey form design did not allow the participant to leave any item unanswered. Responses were automatically saved to a Google spreadsheet. To prevent automated answers, the participants’ country and city were included as open-ended questions.
The questionnaire was constructed by drawing on items reported in previous studies aimed at assessing the impact of COVID in other countries (Alkhamees et al., 2020; Moccia et al., 2020; Wang et al., 2020), following the recommendations of (Hernández Sampieri et al., 2018). It consisted of 34 items that required either open-ended, dichotomous, or Likert responses and were divided as follows:
-
a)
Demographics including sex, school year, country, and city.
-
b)
Perceived stressors were evaluated by a set of researcher-developed questions which required dichotomous answers: being diagnosed with COVID-19 or other illness, having someone close diagnosed with COVID-19, or receiving treatment from a mental health professional. In addition, stress related to several situations was evaluated using a Likert scale (ranging from 0 “not at all” to 3 “to a large extent”) and included the following items: reading or listening to news about the pandemic, having someone close diagnosed with COVID-19, the lockdown, losing contact with peers, the possibility of getting sick, academic delays or the economic impact.
-
c)
Coping strategies, maladaptive behaviors, and locus of control were evaluated in a dichotomous manner using researcher-developed questions. Coping strategies adhered to the WHO recommendations: use of preventive measures (e.g., hand washing, social distance), reaching out to family, volunteering, starting a new activity, and exercising. Maladaptive behaviors were evaluated based on questions about substance use and NSSI. Finally, two more items were aimed at examining the locus of control, considering external locus of control when the participant perceived their life outcomes as arising from factors out of their control (“Do you think your situation is bad regardless of what you do?”) and internal locus of control when the participant described their life outcomes as arising from the exercise of their agency and abilities (“Do you think there are things you can do to be well?”). All 18 items are listed in Table S1 in the supplementary material.
-
d)
Anxiety was assessed using the General Anxiety Disorder −7 (GAD-7), a 7-question scale developed and validated by Spitzer et al. (2006) to detect generalized anxiety disorder and assess its severity. The internal consistency of the scale was excellent with a Cronbach alpha of .92. A cutoff point of 10 is diagnostic of general anxiety disorder with a sensitivity of 89% and a specificity of 82%. The scale was validated in Spanish in a sample of adults (García-Campayo et al., 2010).
-
e)
Depression was assessed using the 9-item Patient Health Questionnaire depression subscale (PHQ-9). This instrument was developed by Spitzer et al. (1999) to evaluate the frequency of each DSM-defined symptom of major depressive disorder. The internal consistency of the scale showed a Cronbach's alpha coefficient of 0.82. A cutoff point of 11 is considered diagnostic of depression, with a sensitivity of 80% and 90% and a specificity of 92% and 86% in adult (Gilbody et al., 2007) and pediatric population (Allgaier et al., 2012) respectively. The Spanish version of the scale was validated both in adult (Merz et al., 2011) and pediatric (Borghero et al., 2018) samples.
2.1. Statistics
Exploratory analyses included filtering out those responses of people who did not consent as well as rows of data with timestamps suggesting that the study was completed in two different moments. There were no missing data.
Statistical analyses were performed with SPSS (version 28) (IBM Corp, 2021) and R (R Core Team, 2018). Three age groups were analyzed: children (8–12 years old), adolescents (13–17 years old), and adults (18–24 years old). Chi-square with a non-adjusted odds ratio (OR) was calculated to determine age and sex differences on categorical variables while two-way analyses of variance (ANOVA) were used to compare continuous variables.
We opted against using the scores of rating scales as continuous variables (as others have done (e.g., Al-Rabiaah et al., 2020; Gloster et al., 2020; Wathelet et al., 2020), as this limits the capacity to differentiate between increments in symptoms that place a participant from going from low to mild to those that go from mild to severe. Instead, we opted for using a dichotomous approach similar to Choi et al. (2020) and classifying scores to distinguish those that could be considered cases according to the rating scales established cut-off points. With this in mind, multivariate analyses were performed to examine the variables associated with being a probable case of depression or anxiety in males and in females, including those variables which showed sex differences. A two-tailed value of P < 0.05 was considered statistically significant.
3. Results
3.1. Description of the sample
The sample included 3965 participants, 63.8% females from 16 different countries. The age distribution was as follows: 621 (15.7%) were children, 1123 (28.3%) were adolescents and 2021 (56%) were young adults. Mexico showed the largest participation (n = 2345, 59.1%), followed by Colombia (n = 1400, 35.3%). See table S2 in the supplementary material for the number of participants from each country.
Table 1 shows the frequency of probable cases of depression and anxiety according to standard cut-off points for the PHQ-9 and GAD-7 rating scales. Almost a third of the sample was above the cut-off point for moderate to severe depression and anxiety scores.
Table 1.
Scores of the PHQ-9 and GAD-7 rating scales.
| Depression rating scale (PHQ-9) | |
|---|---|
| Mean score | 10.55 (6.23) |
| Kurtosis | −0.33 |
| PHQ-9 score 0–4 (none) | 670 (16.9%) |
| PHQ-9 score 5–10 (mild) | 1569 (39.57%) |
| PHQ-9 score ≥11 (moderate to severe) | 1726 (43.53%) |
| Anxiety rating scale (GAD-7) | |
| Mean score | 8.74 (4.7) |
| Kurtosis | −0.13 |
| GAD <10 score | 2498 (63%) |
| GAD ≥10 score | 1467 (27%) |
3.2. Age and sex differences in symptoms of depression and anxiety
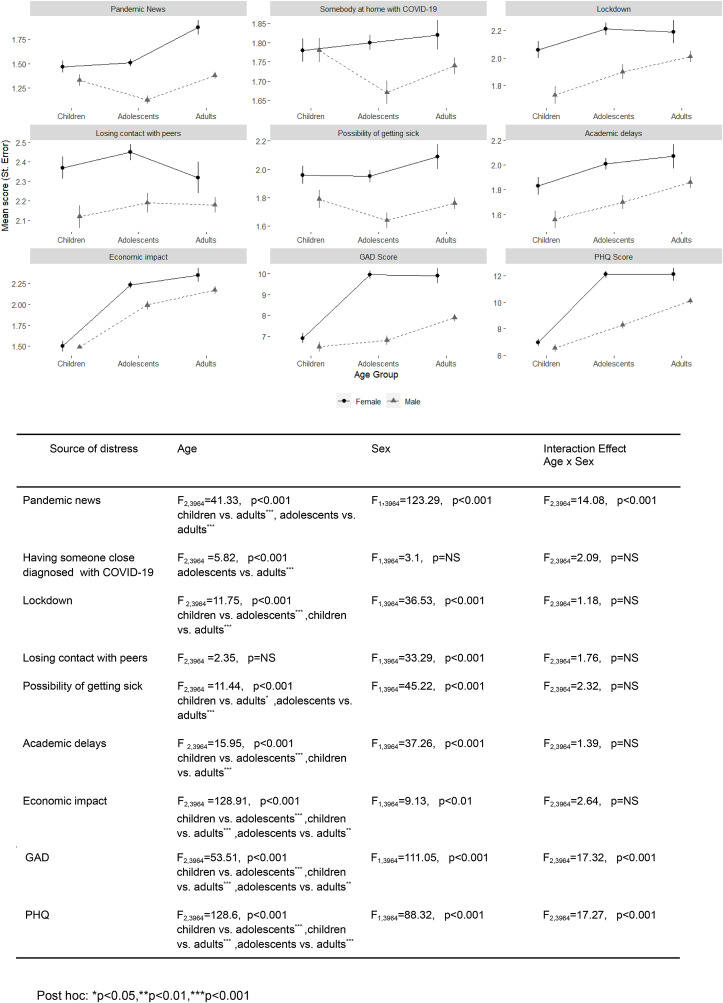
In the case of GAD, scores showed differences according to age (F2,3964 = 53.51, p < 0.001), sex (F1,3964 = 111.05, p < 0.001) and their interaction (F2,3964 = 17.32, p < 0.001), while PHQ scores also showed differences according to age (F2,3964 = 128.6, p < 0.001), sex (F1,3964 = 88.32, p < 0.001) and their interaction (F2,3964 = 17.27, p < 0.001) (Fig. 1 ).
Fig. 1.
Two -way anova for age and sex differences in COVID-19 related distress. Degree of perceived stress was rated from 0 to 3 (0 = “not at all” or 3 = “to a large extent”). Larger GAD 7 (0–21) and PHQ (0–27) scores indicate higher severity.
3.3. Frequency of perceived stressors by age and by sex
The frequency of perceived stressors showed significant differences according to age (Table 2 , upper panel) and sex (Table 2, lower panel). The items “having someone close being diagnosed with COVID-19”, “having another illness” and “receiving mental health treatment” were answered affirmatively more often by adults and adolescents, while the items “having someone close being diagnosed with COVID-19”, and “receiving mental health treatment” were answered affirmatively more often by female respondents.
Table 2.
Age and sex differences in COVID-19 perceived stressors.
| Item | Age | Children(%) | Adolescents(%) | Adults(%) | Chi2 | p | OR(children vs. adolescents) | OR(children vs. adults) |
|---|---|---|---|---|---|---|---|---|
| Diagnosed with COVID-19 | 2.1 | 3.34 | 3.8 | 4.21 | NS | 1.64 (0.87–3.1) | 1.84 (1.01–3.32) | |
| Someone close diagnosed with COVID-19 | 24.2 | 34 | 38.5 | 44.23 | <0.001 | 1.62 (1.30–2.02) | 1.96 (1.60–2.40) | |
| Another illness | 23.3 | 31.5 | 33.1 | 21.61 | <0.001 | 1.51 (1.21–1.89) | 1.62 (1.32–1.99) | |
| Received mental health treatment | 20 | 24.2 | 26.3 | 10.64 | <0.01 | 1.28 (1.01–1.63) | 1.43 (1.15–1.78) | |
| Sex | Males(%) | Females(%) | Chi2 | p | OR(females vs. males) | |||
| Diagnosed with COVID-19 | 3.2 | 3.5 | 0.28 | NS | 1.10 (0.76–1.58) | |||
| Someone close with COVID-19 | 31.3 | 37 | 13.13 | <0.001 | 1.29 (1.12–1.48) | |||
| Another illness | 34 | 29.5 | 8.88 | <0.01 | 0.81 (0.70–0.93) | |||
| Received mental health treatment | 21.3 | 26.7 | 14.18 | <0.001 | 1.34 (1.15–1.56) |
OR = Non-adjusted Odds Ratio; CI = Confidence interval; Children was the reference group for age-related.
The use of coping strategies also differed by age and sex groups, except for “following the health guidelines” which was answered affirmatively by almost all of the total sample. Adolescents showed the highest frequency of use of external locus of control and NSSI, while adults significantly differed from the other two groups in substance use (Table 3 , upper panel). Regarding sex differences, females reported reaching out to family, using an internal locus of control, starting a new activity, and exercising more frequently than males (Table 3, lower panel).
Table 3.
Age and sex differences in coping strategies.
| Item | Age | Children 621(%) | Adolescents 1123(%) | Adults 2221(%) | Chi2 | p | OR (children vs. adolescents) | OR (children vs. adults) |
|---|---|---|---|---|---|---|---|---|
| Reaching out to family/volunteering | 79.5 | 79.9 | 81.4 | 1.82 | NS | 1.02 (0.8–1.30) | 1.13 (0.90–1.41) | |
| Internal locus of control | 95.3 | 93.2 | 95.8 | 10.63 | <0.01 | 0.67 (0.44–1.05) | 1.12 (0.73–1.71) | |
| External locus of control | 14.2 | 23.8 | 21.3 | 22.85 | <0.001 | 1.89 (1.45–2.46) | 1.64 (1.28–2.10) | |
| Substance use | 1.40 | 7.8 | 23.1 | 244.15 | <0.001 | 5.78(2.89–11.56) | 20.47(10.52–39.83) | |
| Start a new activity | 73.6 | 68.6 | 71.5 | 5.57 | NS | 0.78 (0.63–0.97) | 0.90 (0.73–1.10) | |
| Exercising | 73.9 | 79.3 | 75.1 | 9.08 | <0.01 | 1.34 (1.07–1.69) | 1.06 (0.86–1.30) | |
| NSSI | 0.5 | 3 | 0.9 | 27.33 | <0.001 | 6.43 (1.97–21.02) | 1.96 (0.58–6.61) | |
| Sex | Males 1421(%) | Females 2486(%) | Chi2 | p | OR (females vs. males) | |||
| Reaching out to family/volunteering | 76.6 | 83 | 24.19 | <0.001 | 0.86 (0.80–0.92) | |||
| Internal locus of control | 93.5 | 95.9 | 11.38 | <0.001 | 0.81 (0.71–0.93) | |||
| External locus of control | 20 | 21.4 | 0.96 | NS | 0.96 (0.91–1.02) | |||
| Substance use | 14.2 | 16.1 | 2.54 | NS | 0.95 (0.89–1.01) | |||
| Start a new activity | 67.6 | 72.9 | 12.51 | <0.001 | 0.90 (0.86–0.96) | |||
| Exercising | 73.7 | 77.4 | 6.95 | <0.01 | 0.93 (0.87–0.98) | |||
| NSSI | 1.1 | 1.7 | 1.9 | NS | 0.89 (0.75–1.05) |
Fig. 1 shows the mean scores of perceived stress for males and females from each age group. Two-way ANOVAs that compared the level of perceived stress showed significant differences in age for all items except for “losing contact with peers”, while sex comparisons yielded significant differences for all items except for “having someone close diagnosed with COVID-19”; only “reading or listening to news about the pandemic” showed differences according to age (F2,3964 = 41.33, p < 0.001), sex (F1,3964 = 123.29, p < 0.001) and their interaction (F2, 3964 = 14.08, p < 0.001).
The multivariate analyses were constructed using saturated models that included those variables that showed differences according to sex (age, having someone diagnosed with COVID-19, having another illness, receiving mental health treatment, higher stress regarding pandemic news, having someone close w/COVID, lockdown, not seeing friends, the possibility of getting sick, academic delays and economic impact; not reaching out to family, lack of internal locus of control, not starting a new activity, and not exercising) as independent variables and being a probable case of depression (PHQ score ≥11) or anxiety (GAD score ≥10) as dependent variables. The full model statistics and the OR for each variable are shown in Table 4, Table 5 . The full set of statistical parameters of the model can be found in the Supplementary material (Tables S3 and S4).
Table 4.
Variables associated with depression as measured by PHQ in males and females.
| Males OR (95% CI) | Females OR (95% CI) | |
|---|---|---|
| Age | 1.08 (1.05–1.11) | 1.04 (1.02–1.07) |
| Someone close w/COVID-19 | 0.78 (0.59–1.04) | 1.03 (0.85–1.25) |
| Another illness | 1.54 (1.19–2) | 1.61 (1.32–1.96) |
| Received mental health treatment | 1.93 (1.44–2.59) | 2.20 (1.79–2.71) |
| Higher stress about pandemic news | 1.46 (1.24–1.72) | 1.49 (1.32–1.67) |
| Higher stress about someone close w/COVID | 1.11 (1.01–1.21) | 1.04 (0.97-1.11) |
| Higher stress about lockdown | 1.36 (1.15–1.59) | 1.49 (1.31–1.68) |
| Higher stress about not seeing friends | 1.23 (1.03–1.46) | 0.91 (0.81–1.03) |
| Higher stress about the possibility of getting sick | 0.93 (0.81–1.08) | 0.85 (0.77–0.93) |
| Higher stress about academic delays | 1.12 (1–1.26) | 1.25 (1.15–1.36) |
| Higher stress about economic impact | 1.21 (1.06–1.38) | 1.29 (1.17–1.43) |
| Not reaching out to family | 1.09 (0.80–1.49) | 0.68 (0.53–0.87) |
| Lack of internal locus of control | 2.05 (1.22–3.42) | 3.98 (2.17–7.3) |
| Not starting a new activity | 0.83 (0.63–1.10) | 0.66 (0.53–0.82) |
| Not exercising | 1.68 (1.25–2.24) | 1.85 (1.47–2.33) |
| Model | R2 = 0.271, GOF x2 = 6.93, p = NS | R2 = 0.284, GOF x2 = 7.41, p = NS |
Letters in bold represent p < 0.05.
Table 5.
Variables associated with anxiety as measured by the GAD in males and females.
| Males OR (95% CI) | Females OR (95% CI) | |
|---|---|---|
| Age | 1.02 (0.99–1.05) | 1 (0.98–1.03) |
| Someone close w/COVID-19 | 0.85 (0.62–1.16) | 1.09 (0.90–1.33) |
| Another illness | 1.71 (1.28–2.28) | 1.86 (1.52–2.27) |
| Received mental health treatment | 2.09 (1.53–2.85) | 1.90 (1.54–2.33) |
| Higher stress about pandemic news | 1.99 (1.66–2.39) | 1.82 (1.61–2.06) |
| Higher stress about someone close w/COVID | 1.03 (0.94–1.14) | 1.08 (1.02–1.16) |
| Higher stress about lockdown | 1.87 (1.55–2.26) | 1.71 (1.50–1.94) |
| Higher stress about not seeing friends | 1.02 (0.83–1.24) | 0.87 (0.77–0.99) |
| Higher stress about the possibility of getting sick | 1.11 (0.95–1.30) | 1.11 (1–1.22) |
| Higher stress about academic delays | 1.09 (0.96–1.24) | 1.15 (1.06–1.25) |
| Higher stress about economic impact | 1.11 (0.95–1.28) | 1.23 (1.12–1.36) |
| Not reaching out to family | 0.78 (0.56–1.10) | 0.79 (0.62–1.02) |
| Lack of internal locus of control | 2.09 (1.22–3.60) | 3.12 (1.86–5.22) |
| Not starting a new activity | 0.92 (0.67–1.26) | 0.72 (0.58–0.90) |
| Not exercising | 1.49 (1.08–2.06) | 1.45 (1.14–1.83) |
| Model | R2 = 0.299, GOF x2 = 9.54, p = NS | R2 = 0.318, GOF x2 = 6.72, p = NS |
Letters in bold represent p < 0.05.
4. Discussion
This research aimed to evaluate sex and age differences in the frequency and severity of symptoms of depression and anxiety. The research also aimed to identify which perceived stressors and coping strategies were associated with the presence of psychopathology in children, adolescents, and young adults from a Latin American sample. The results showed a high frequency of symptoms of depression and anxiety, age differences in the frequency of identified stressors and coping strategies related to COVID as well as a higher impact in females of all age groups.
In the current study, 43.5% of the sample surpassed the PHQ-9 and 27% the GAD-7 cutoff points, thus they were considered probable cases. Recent meta-analyses examining the mental health of youth in several countries reported pooled prevalence rates of around 25% for depression and 20% for anxiety in children, and adolescents (Racine et al., 2021) and 34% and 38% in adults (Necho et al., 2021). While differences in the rates between these studies and the current one may be explained by the diagnostic instruments and the age groups represented in the sample, the current numbers support previous research and add Latin America to the regions where mental health was heavily impacted by the COVID-19 pandemic (Santomauro et al., 2021). These findings underline the need for urgent local and regional actions for the prevention of psychopathology by incorporating mechanisms to cope with stress (Bhattacharjee and Acharya, 2020).
Regarding the perceived stressors, our results showed that the most frequently perceived stressors were having someone close diagnosed with COVID-19 and the presence of another illness (around 30% for each). The number of people having someone with COVID 19 is much larger than the 10.2%–13.3% described in low- and middle-income countries such as Bangladesh (Yeasmin et al., 2020) and Turkey (Özdin, 2020). Although this number may be inaccurate, it could be associated with some social characteristics of Latin American countries, such as larger social circles, denser living conditions, and extended family networks, as well as with some problems reported in the government's management of the COVID-19 pandemic, like the underreporting of cases (Lima et al., 2021). The large prevalence of having another illness could be associated with the high levels of stress experienced (Ahmed et al., 2020; Wang et al., 2020) or it could also come from the difficulty of getting medical attention during the pandemic lockdown (Silva Tinoco et al., 2021).
As for coping strategies, reaching out to family/volunteering, using an internal locus of control, starting a new activity, and exercising were the most frequently reported, with percentages above 70%. Previous studies on adult samples also showed the association of such coping strategies with a lesser degree of symptoms of depression and anxiety (Meyer et al., 2022).
4.1. Age differences
In the current study adolescents and adults showed higher scores on the rating scales of depression and anxiety. Even under non-pandemic conditions, this trend has been frequently highlighted: higher anxiety levels have been reported for adolescents in contrast to children (Duan et al., 2020), rising prevalence rates of depression and anxiety disorders among young adults (Costello et al., 2011), and increased use of mental health providers in adolescents and young adults (Mojtabai et al., 2016).
An age-related increase in frequency was observed in almost all the perceived stressors: adults reported the highest level of stress related to pandemic news, having someone close diagnosed with COVID-19, the possibility of getting sick, academic delays, and the economic impact of the pandemic. Additionally, there were age differences in terms of coping strategies: adolescents showed the highest frequency of use of external locus of control, while young adults showed the highest frequency of substance use, previous reports have associated substance use with factors related to the lockdown such as loneliness or increased symptoms of depression and anxiety (Horigian et al., 2021; Graupensperger et al., 2021).
4.2. Sex differences
Our study showed that positive coping mechanisms, such as reaching out to family, manifesting an internal locus of control, starting a new activity, and exercising, were reported more frequently by women. However, it was women who were affected by the perceived stressors with greater intensity and frequency, no matter their age group. Studies in adults showed that women scored higher on a range of coping styles compared to men (Fluharty and Fancourt, 2021) and a positive correlation between distress and the use of coping mechanisms (Elkayal et al., 2022). The prevalence of depression and anxiety has been reported to be higher among females, yet the pandemic has accentuated this difference (Santomauro et al., 2021). While biology is sure to have a role in the susceptibility to such disorders (Slavich and Sacher, 2019), environmental and cultural factors including the responsibility for caring for the sick or domestic violence could represent a contributing factor (Connor et al., 2020). The results of the multivariate analysis models confirmed the association of several variables with the presence of depression and anxiety. These characteristics could be used in the construction of a risk index to detect vulnerable populations when experiencing a future pandemic event or even during the subsequent waves of a pandemic.
4.3. Limitations
Present results should be examined considering several limitations. Even though the questionnaire was aimed at all the Latin American region, most respondents were from Mexico and Colombia. The sample is biased as data from those without internet access, who may be among the most impacted, were not obtained. While online studies allowed us to gather data for a large geographical area during a time when personal contact with participants was limited, the symptoms reported on an online survey are not sufficient to imply a formal or accurate diagnosis of depression and anxiety. Data regarding other factors contributing to stress (such as domestic violence) were not included. Finally, some of the instruments used here have not yet been validated for use in young children as young as 8 years.
5. Conclusions
The present study shows a high prevalence of symptoms of depression and anxiety in the region. Adolescent and adult females manifested more stress in response to situations derived from the COVID-19 pandemic, but also were the ones who reported having implemented more coping strategies in the same circumstances.
Author contributions
REU, Conceptualization; Formal analysis; Investigation; Methodology; Project administration; original draft preparation,review & editing. RA, Conceptualization; Investigation; Methodology; Project administration; original draft preparation, review & editing. FR dP, Conceptualization; Investigation; Methodology; original draft preparation,review & editing. RD, Data curation; Formal analysis; Investigation; Methodology; original draft preparation,; review & editing. PM,: Investigation; Methodology; original draft preparation,review & editing. JDP, Conceptualization; Investigation; Methodology; original draft preparation. LPC, Conceptualization; Formal analysis; Methodology; Validation; original draft preparation; review & editing. AH, Investigation; original draft preparation. PG, Investigation; original draft preparation. MFR, Conceptualization; Formal analysis; Investigation; Methodology; original draft preparation; review & editing.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of competing interest
The authors declare that there is no conflict of interest.
Acknowledgments
The authors wish to thank Dr. Vicky Maravillas, Dr. Carolina Remedi, and Dr.Inés Nogales for their support in the distribution of the survey. They also wish to thank Daniela Olvera and Jonathan Marin for their assistance in the manuscript preparation.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jpsychires.2022.10.005.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Ahmed T., Lodhi S.H., Kapadia S., Shah G.V. Community and healthcare system-related factors feeding the phenomenon of evading medical attention for time-dependent emergencies during COVID-19 crisis. BMJ Case Rep. 2020;13 doi: 10.1136/bcr-2020-237817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhamees A.A., Alrashed S.A., Alzunaydi A.A., Almohimeed A.S., Aljohani M.S. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr. Psychiatr. 2020;102 doi: 10.1016/j.comppsych.2020.152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allgaier A.K., Pietsch K., Frühe B., Sigl-Glöckner J., Schulte-Körne G. Screening of depression in adolescents: validity of the patient health questionnaire in pediatric care. Depress. Anxiety. 2012;29:906–913. doi: 10.1002/da.21971. [DOI] [PubMed] [Google Scholar]
- Al-Rabiaah A., Temsah M.H., Al-Eyadhy A.A., Hasan G.M., Al-Zamil F., Al-Subaie S., Alsohime F., Jamal A., Alhaboob A., Al-Saadi B., Somily A.M. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health. 2020;13:687–691. doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borghero F., Martínez V., Zitko P., Vöhringer P.A., Cavada G., Rojas G. Screening depressive episodes in adolescents. Validation of the patient health questionnaire-9 (PHQ-9) Rev. Med. Chile. 2018;146:479–486. doi: 10.4067/s0034-98872018000400479. [DOI] [PubMed] [Google Scholar]
- Bhattacharjee B., Acharya T. The COVID-19 pandemic and its effect on mental health in USA –a review with some coping strategies. Psychiatr. Q. 2020;91:1135–1145. doi: 10.1007/s11126-020-09836-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canet J.L. Seguimiento longitudinal del impacto de la pandemia sobre la salud mental de los argentinos Expos. In: Comisión de Investigaciones Científicas. 2020. https://digital.cic.gba.gob.ar/handle/11746/10760
- Choi E.P.H., Hui B.P.H., Wan E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(3740) doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J., Madhavan S., Mokashi M., Amanuel H., Johnson N.R., Pace L.E., Bartz D. Health risks and outcomes that disproportionately affect women during the COVID-19 pandemic: a review. Soc. Sci. Med. 2020;266 doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cost K.T., Crosbie J., Anagnostou E., Birken C.S., Charach A., Monga S., Kelley E., Nicolson R., Maguire J.L., Burton C.L., Schachar R.J., Arnold P.D., Korczak D.J. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur. Child Adolesc. Psychiatr. 2021;31:671–684. doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E.J., Copeland W., Angold A. Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? JCPP (J. Child Psychol. Psychiatry) 2011;52:1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer Childs E.R., Laura K., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. June 24-30, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Abreu J.M., de Souza R.A., Viana-Meireles L.G., Landeira-Fernandez J., Filgueiras A. Effects of physical activity and exercise on well-being in the context of the Covid-19 pandemic. PLoS ONE 17, e0260465. 2022. [DOI] [PMC free article] [PubMed]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudovskiy J. 2022. The Ultimate guide to writing a dissertation in business studies: a step-by-step assistance. https://research-methodology.net/
- Dumas T.M., Ellis W., Litt D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J. Adolesc. Health. 2020;67:354–361. doi: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkayal M.M., Shahin M.A.H., Hussien R.M. Psychological distress related to the emerging COVID-19 pandemic and coping strategies among general population in Egypt. J. Egypt. Publ. Health Assoc. 2022;97:1–12. doi: 10.1186/s42506-021-00100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fluharty M., Fancourt D. How have people been coping during the COVID-19 pandemic? Patterns and predictors of coping strategies amongst 26, 016 UK adults. BMC Psychol. 2021;9(107) doi: 10.1186/s40359-021-00603-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Campayo J., Zamorano E., Ruiz M.A., Pardo A., Pérez-Páramo M., López-Gómez V. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcome. 2010;8:1–11. doi: 10.1186/1477-7525-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S., Richards D., Brealey S., Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J. Gen. Intern. Med. 2007;22:1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloster A.T., Lamnisos D., Lubenko J., Presti G., Squatrito V., Constantinou M., Nicolaou C., Papacostas S., Aydın G., Chong Y.Y., Chien W.T., Cheng H.Y., Ruiz F., Garcia-Martin J., Obando Posada M.B., Segura Vargas D.P., Vasiliou M.A., McHugh V.S., Höfer L., Baban S., Neto A., Nunes da Silva D., Monestès A., Alvarez Galvez J.L., Paez-Blarrina J., Montesinos M., Valdivia-Salas F., Ori S., Kleszcz D., Lappalainen B., Ivanović R., Gosar I., Dionne D., Merwin F., Kassianos R., Karekla M A. Impact of COVID-19 pandemic on mental health: an international study. PLOS ONE. 15, e0244809. 2020. [DOI] [PMC free article] [PubMed]
- Graupensperger S., Cadigan J.M., Einberger C., Lee C.M. Multifaceted COVID-19-related stressors and associations with indices of mental health, well-being, and substance use among young adults. Int. J. Ment. Health Addiction. 2021 doi: 10.1007/s11469-021-00604-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes M.T., Szenczy A.K., Klein D.N., Hajcak G., Nelson B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2021:1–9. doi: 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández Sampieri R., Fernández Collado C., Baptista Lucio P. Chapter 9, Recoleccción de datos cuantitativos. McGraw-Hill Interamericana; Mexico: 2018. Metodología de la investigación; pp. 196–267. [Google Scholar]
- Horigian V.E., Schmidt R.D., Feaster D.J. Loneliness, mental health, and substance use among US young adults during COVID-19. J. Psychoact. Drugs. 2021;53:1–9. doi: 10.1080/02791072.2020.1836435. [DOI] [PubMed] [Google Scholar]
- International Monetary Fund 2022. Global prospects and policies. Chapter 1, World Economic Outlook. 2022 https://www.imf.org/en/Search#q=RECOVERY%20DURING%20A%20PANDEMIC%20HEALTH%20CONCERNS%2C%20SUPPLY%20DISRUPTIONS%2C%20AND%20PRICE%20PRESSURES&first=20&sort=relevancy April. [Google Scholar]
- Larraguibel M., Rojas-Andrade R., Halpern M., Montt M.E. Impact of the COVID-19 pandemic on the mental health of preschoolers and school in Chile. Rev Chil Psiquiatr Neurol Infanc Adolesc. 2021;32:12–21. [Google Scholar]
- Larrea-Schiavon S., López-Lalinde L., Martínez I.V., Regules R., Gutiérrez J.P., Nevárez R., Mac Gregor C., López P., Haberland N., Ngô T. Population Council; Mexico: 2021. Findings from the Violence Outcomes in COVID-19 Era Study (VoCes-19) Baseline results. [DOI] [Google Scholar]
- Lavigne-Cerván R., Costa-López B., Juárez-Ruiz de Mier R., Real-Fernández M., Sánchez-Muñoz de León M., Navarro-Soria I. Consequences of COVID-19 confinement on anxiety, sleep and executive functions of children and adolescents in Spain. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.565516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S.H., Beames J.R., Newby J.M., Maston K., Christensen H., Werner-Seidler A. The impact of COVID-19 on the lives and mental health of Australian adolescents. Eur. Child Adolesc. Psychiatr. 2021:1–13. doi: 10.1007/s00787-021-01790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima E.E., Vilela E.A., Peralta A., Rocha M., Queiroz B., Gonzaga M.R., Piscoya-Díaz M., Martinez-Folgar K., García-Guerrero V., Freire F.H. Investigating regional excess mortality during 2020 COVID-19 pandemic in selected Latin American countries. Genus. 2021;77:1–20. doi: 10.1186/s41118-021-00139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatr. Res. 2020;289 doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Idris S., Zhang Y., Zewen L., Wali A., Ji Y., Pan Q., Baloch Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: an online survey. BMC Pediatr. 2021;21:1–8. doi: 10.1186/s12887-021-02550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merz E.L., Malcarne V.L., Roesch S.C., Riley N., Sadler G.R. A multigroup confirmatory factor analysis of the Patient Health Questionnaire-9 among English- and Spanish-speaking Latinas. Cult. Divers Ethnic Minor. Psychol. 2011;17:309–316. doi: 10.1037/a0023883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer D., Van Rheenen T.E., Neill E., Phillipou A., Tan E.J., Toh W.L., Sumnerm P.J., Rossell S.L. Surviving the COVID-19 pandemic: an examination of adaptive coping strategies. Heliyon. 5, e09508. 2022. [DOI] [PMC free article] [PubMed]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffoe D., Janiria L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R., Olfson M., Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics December. 2016;138 doi: 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Necho M., Tsehay M., Birkie M., Biset G., Tadesse E. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Int. J. Soc. Psychiatr. 2021 doi: 10.1177/00207640211003121. [DOI] [PubMed] [Google Scholar]
- Özdin S., Bayrak, Özdin Ş. Levels and predictors of anxiety, depression, and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatr. 2020;66:504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul E., Fancourt D. Factors influencing self-harm thoughts and behaviours over the first year of the COVID-19 pandemic in the UK: longitudinal analysis of 49 324 adults. BJPsych. 2022;220:31–37. doi: 10.1192/bjp.2021.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng X., Menhas R., Dai J., Younas M. The COVID-19 pandemic and overall wellbeing: mediating role of virtual reality fitness for physical-psychological health and physical activity. Psychol. Res. Behav. Manag. 2022:1741–1756. doi: 10.2147/PRBM.S369020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a Meta-analysis. JAMA Pediatr. 2021;175:1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry. 2021. [DOI] [PMC free article] [PubMed]
- Rusca-Jordán F., Cortez-Vergara C., Tirado-Hurtado B.C., Strobbe-Barbat M. An approach on mental health of children, adolescents and caregivers in the COVID-19 context in Peru. Acta Méd. Peru. 2020;37 doi: 10.35663/amp.2020.374.1851. [DOI] [Google Scholar]
- Santomauro D.F., Herrera A.M.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafat C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L., Bertolacci G.J., Bloom S.S., Castellano R., Castro E., Chakrabarti S., Chattopadhyay J., Cogen R.M., Collins J.K., Dai X., Dangel W.J., Dapper C., Deen A., Erickson M., Ewald S.B., Flaxman A.D., Frostad J.J., Fullman N., Giles J.R., Giref A.Z., Guo G., He J., Helak M., Hulland E.N., Idrisov B., Lindstrom A., Linebarger E., Lotufo P., Lozano R., Magistro B., Malta D.C., Mansson J.C., Marinho F., Mokdad A.H., Monasta L., Naik P., Nomura S., O'Halloran S.M., Ostroff S.M., Pasovic M., Penberthy L., Reiner R., Jr., Reinke G., Ribeiro A.L., Sholokhov A., Sorensen R., Varavikova E., Truc A., Walcott R., Watson S., Wiysonge C.S., Zigler B., Hay S., Vos T., Murray C., Whiteford H., Ferrari A. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to COVID-19 pandemic. Indian J. Pediatr. 2020 doi: 10.1007/s12098-020-03347-3. 87,532–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva Tinoco R., Cantú A.G., De la Torre-Saldaña V., Guzmán Olvera E., Cuatecontzi Xochitiotzi T., Martínez L.C., Romero Ibarguengoitia M.E., Nahuacatl-Lòpez A., Castillo Galindo C., Orea Tejeda A., Serna Alvarado J., León Garcia E., Ochoa Moreno J. Effect in self-care behavior and difficulties in coping with diabetes during the COVID-19 pandemic: Efecto en el comportamiento de autocuidado y dificultades para hacer frente a la diabetes durante la pandemia de COVID-19. Rev Mex Endocrinol Metab Nutr. 2021;8:13. doi: 10.24875/RME.20000063. [DOI] [Google Scholar]
- Slavich G.M., Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: Extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology. 2019;236:3063–3079. doi: 10.1007/s00213-019-05326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(1729) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., Debien C., Molenda S., Horn M., Grandgenèvre P., Notredame C.E., D'Hondt F. Factors associated with mental health disorders among University students in France confined during the COVID-19 Pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization 2022. WHO COVID-19 dashboard. https://covid19.who.int/
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province. China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics. 174,898–900. 2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S., Banik R., Hossain S., Hossain M.N., Mahumud R., Salma N., Hossain M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child. Youth Serv. Rev. 2020;117 doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Zhang D., Fang J., Wan Y., Tao F., Sun Y. Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 Pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.