Abstract
Background
Diabetic kidney disease (DKD), the most common cause of kidney failure and end-stage kidney disease worldwide, will develop in almost half of all people with type 2 diabetes. With the incidence of type 2 diabetes continuing to increase, early detection and management of DKD is of great clinical importance.
Main body
This review provides a comprehensive clinical update for DKD in people with type 2 diabetes, with a special focus on new treatment modalities. The traditional strategies for prevention and treatment of DKD, i.e., glycemic control and blood pressure management, have only modest effects on minimizing glomerular filtration rate decline or progression to end-stage kidney disease. While cardiovascular outcome trials of SGLT-2i show a positive effect of SGLT-2i on several kidney disease-related endpoints, the effect of GLP-1 RA on kidney-disease endpoints other than reduced albuminuria remain to be established. Non-steroidal mineralocorticoid receptor antagonists also evoke cardiovascular and kidney protective effects.
Conclusion
With these new agents and the promise of additional agents under clinical development, clinicians will be more able to personalize treatment of DKD in patients with type 2 diabetes.
Keywords: Type 2 diabetes, Diabetic kidney disease, Kidney protective agents
Background
According to the International Diabetes Federation, 537 million adults (20–79 years of age) were living with diabetes mellitus worldwide in 2021, and this number is expected to increase to more than 780 million by the year 2045 [1]. Of these, an estimated 90–95% have type 2 diabetes (T2D) [2, 3]. Among people with T2D, nearly half will develop diabetic kidney disease (DKD), previously termed “diabetic nephropathy” [4, 5]. DKD is the most common cause of kidney failure and end-stage kidney disease (ESKD) leading to the need for kidney replacement therapy (dialysis or transplant) in the world [6, 7]. Moreover, DKD is a leading cause of cardiovascular disease and overall mortality in people with diabetes [8, 9]. Given the ever-increasing prevalence of T2D, early detection and proper management of DKD is of great clinical importance. This review provides an update on DKD pathophysiology, clinical manifestations, and recent breakthroughs in DKD therapies.
Pathophysiology
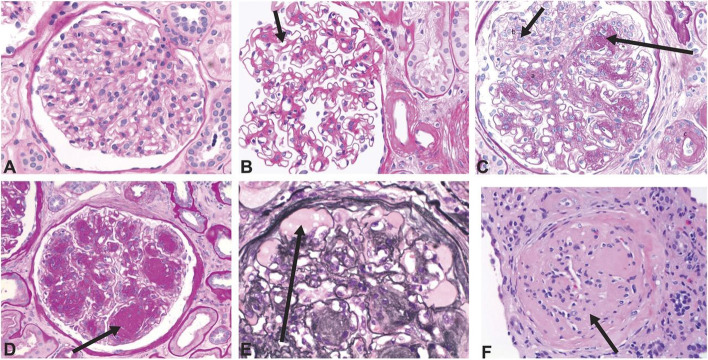
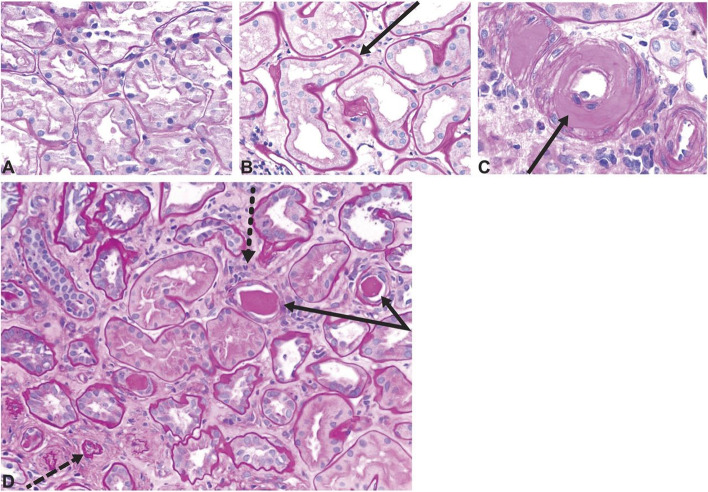
Multiple diabetes-driven pathways including hyperglycemia and associated metabolic disturbances, glomerular hemodynamic changes, and proinflammatory and profibrotic factors contribute to kidney damage in DKD [10–13]. These pathways often lead to glomerular hyperfiltration accompanied by glomerular hypertrophy, and evidence suggests that this may further lead to sclerosis, particularly with comorbid hypertension [11]. Obesity and systemic hypertension, common among people with T2D, also exacerbate glomerular hyperfiltration [14]. Arteriolar hyalinosis along with tubulointerstitial inflammation and fibrosis are also dominant features of DKD (Figs. 1 and 2) [11]. Increasing permeability to albumin, marked by high levels of albuminuria, results from progressive glomerular injury [15]. Albuminuria typically develops prior to loss of filtration, but eGFR decline may also occur without the occurrence of albuminuria in DKD [16–18]. In people who experience a decline in eGFR without albuminuria, the kidney tissue typically shows prominent vascular lesions and interstitial fibrosis [18]. Table 1 provides a description of typical findings of glomerular lesion biopsies common in DKD.
Fig. 1.
Histology images showing structural changes related to diabetic glomerulopathy. A Normal glomerulus. B Diffuse mesangial expansion with mesangial cell proliferation. C Prominent mesangial expansion with early nodularity and mesangiolysis. D Accumulation of mesangial matrix forming Kimmelstiel-Wilson nodules. E Dilation of capillaries forming microaneurysms, with subintimal hyaline (plasmatic insudation). F Obsolescent glomerulus. A–D and F were stained with period acid-Schiff stain. E was stained with Jones stain. Original magnification ×400. Reprinted with permission from American Society of Nephrology (Alicic et al., Diabetic Kidney Disease: Challenges, Progress, and Possibilities; CJASN 2017; 12; (2032-45) [11]
Fig. 2.
Histology images showing tubulointerstitial changes seen in diabetic kidney disease. A Normal kidney cortex. B Thickened tubular basement membrane and interstitial widening. C Arteriole with an intimal accumulation of hyaline material with significant luminal compromise. D Renal tubules and interstitium in advancing diabetic kidney disease, with thickening and wrinkled tubular basement membranes (solid arrows), atrophic tubules (dashed arrow), some containing casts, and interstitial widening with fibrosis and inflammatory cells (dotted arrow). All sections stained with period acid-Schiff stain, original magnification ×200. Reprinted with permission from American Society of Nephrology (Alicic et al. [11])
Table 1.
Overview of classes and biopsy findings seen in glomerular lesions associated with diabetic kidney disease (DKD)
| Class | Biopsy findings |
|---|---|
| I | Thickening of glomerular basement membrane >430 nm in males ages 9 years and older, >395 nm in females ages 9 years and older |
| II | Mild to severe expansion of mesangial extracellular material: width of interspace exceeds two mesangial cell nuclei in two or more glomerular lobules; also known as “diffuse diabetic glomerulosclerosis” |
| III | Nodular sclerosis, Kimmelstiel-Wilson lesions: focal, lobular, mesangial lesions with acellular, hyaline/matrix core. Generally, these lesions indicate transition from early to later stages diabetic kidney disease |
| IV | More than 50% global glomerulosclerosis attributed to diabetes: fibrotic lesions with a build-up of extracellular matrix proteins in the mesangial space. Presence indicates advanced diabetic kidney disease |
| Other changes, lesions | Interstitial fibrosis and tubular atrophy; hyalinosis of the efferent, and possibly the afferent, arterioles; insudative lesions known as “capsular drop lesions” when found in Bowman’s capsule, as “hyalinized afferent and efferent arterioles when found in the afferent and efferent arterioles, and as fibrin cap lesions or hyalinosis when found in glomerular capillaries; “tip lesion” refers to abnormality in the tubuloglomerular junction, with atrophic tubules and no visible glomerular opening, and related to advanced DKD and macroalbuminuria |
Source: Tervaert et al. [19]
Clinical manifestations
DKD often progresses to kidney failure or leads to cardiovascular events that cause death in about half of those affected [11, 20]. Therefore, early awareness, detection, and intervention are essential to improve clinical outcomes.
Diagnostic tools and laboratory practices for DKD
A persistent elevation in urinary albumin to creatinine ratio (UACR, ≥30mg/g [≥3 mg/mmol]), and/or a persistent reduction in eGFR (<60 mL/min/1.73m2) in a person with diabetes indicates DKD [21]. To qualify as DKD, however, these lesions must be due only to diabetes-related factors [21].
The American Diabetes Association (ADA) Standards of Medical Care recommends that people with T2D be screened for DKD at their initial diagnosis and annually thereafter [21].
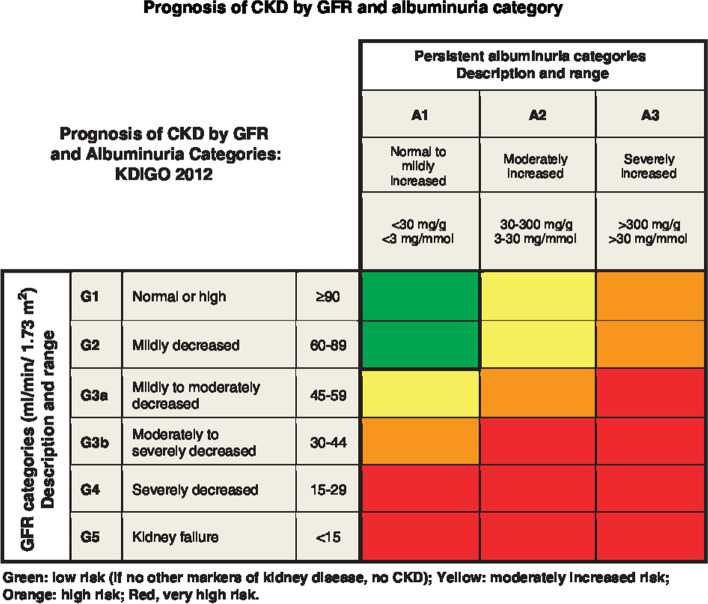
As shown in Fig. 3, there are three categories of albuminuria [22]:
Stage A1, normal to mildly increased albuminuria: <30 mg/g (<3 mg/mmol) UACR in urine sample
Stage A2, moderately increased albuminuria, microalbuminuria: 30–300 mg/g (3–30 mg/mmol) UACR; occurring ≥2 times, 3–6 months apart [21]. This low-grade albuminuria is a less effective predictor of disease progression than macroalbuminuria [23]
Stage A3, severely increased albuminuria, macroalbuminuria: >300 mg/g (>30 mg/mmol) UACR; occurring ≥2 times, 3–6 months apart [21]
Fig. 3.
Prognosis of chronic kidney disease by GFR and albuminuria category. This figure was developed by Kidney Disease Improving Global Outcomes (KDIGO) [22] and reproduced with permission from KDIGO
The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is the most commonly used formula to estimate GFR from the serum creatinine. Recently, the American Society of Nephrology and the National Kidney Foundation have made recommendations to use race-agnostic methods excluding race in the equation to diagnose and classify chronic kidney disease as a path toward equitable healthcare [24, 25]. A major development is a new CKD-EPI 2021 eGFR equation. This new equation does not include a term for race, with the intent to increase awareness of chronic kidney disease as well as to encourage more timely detection and therapeutic interventions, for all groups of people. Addition of the serum cystatin-C to the CKD-EPI 2021 eGFR equation improves accuracy and precision [25]. Although the serum cystatin-C test is available in some regions of the world, it is not widely used yet due to costs and lack of assay standardization [26–29]. Albuminuria and decreased eGFR, in both general and high-risk populations, are also associated with increased risks for cardiovascular events and mortality, as well as all-cause mortality [30, 31].Therefore, as a holistic approach to assess kidney and cardiovascular risks, these tests should be checked at least twice a year in people with diabetes and UACR >30 mg/g (>3 mg/mmol) and/or eGFR <60 mL/min/1.73 m2 [21].
In addition to monitoring for kidney damage and function, people with T2D should have their glycated hemoglobin (HbA1c) tested every 3–6 months to monitor their blood glucose control [32]. The ADA recommends that people with T2D work with their physician to set an individualized goal for glycemic control avoiding hypoglycemia, but with a general target of HbA1c <7% (53 mmol/mol) [32].
Treatments and medications
Several strategies exist that can help prevent DKD development and slow its progression [8, 33]. While healthy lifestyle changes are foundational, achieving optimal glycemic, blood pressure, and cholesterol levels generally require use of medications. A summary of the Kidney Disease Improving Global Outcomes (KDIGO) guideline for people with chronic kidney disease and diabetes is shown in Fig. 4.
Fig. 4.
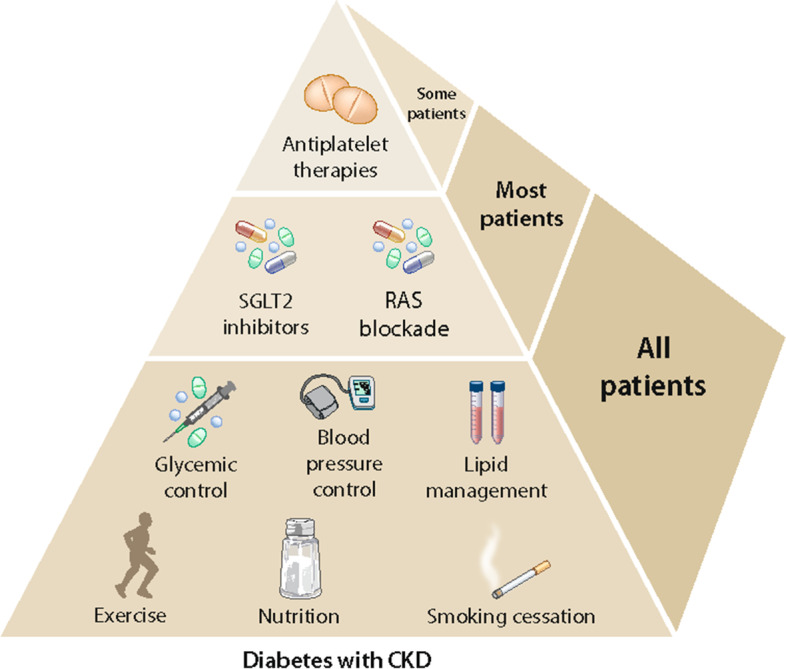
Clinical strategies to prevent development/progression of chronic kidney disease in people with diabetes. This figure was developed by Kidney Disease Improving Global Outcomes (KDIGO) [27] and reproduced with permission from KDIGO. Abbreviations: SGLT2, sodium glucose transport protein 2; RAS, renin-angiotensin system; CKD, chronic kidney disease
Current goals/targets for people with T2D are:
Manage glycemic control—goal HbA1C ≤7% (53 mmol/mol) [32]
- Control blood pressure—the ADA recommends blood pressure below 140/90 mmHg for people with diabetes, with a lower target (e.g., 130/80 mmHg) potentially beneficial for those with macroalbuminuria [21]. KDIGO recommends treating to a target systolic blood pressure of <120 mmHg, as tolerated, in people with chronic kidney disease with or without diabetes, but not those having had a kidney transplant or on dialysis [34]. Measures to control blood pressure should include use of either:
-
i.Angiotensin-converting enzyme inhibitors (ACEi) or
-
ii.Angiotensin II receptor blockers (ARB) [22]
-
i.
Lifestyle changes—weight reduction, increased physical activity, and smoking cessation [8, 27]
In addition to the beneficial effects that blood pressure lowering medications have on progression of DKD [37], other types of medications are also used to manage DKD in people with T2D. Table 2 lists classes, examples, and modes of action of these medications. Optimal management of blood glucose is the first step in preventing the onset of DKD. Both sodium glucose transport protein 2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1 RA) have shown beneficial effects on DKD, such as a reduction in albuminuria or lower risk of new-onset albuminuria, largely beyond glycemic control [44, 51].
Table 2.
Medications used in type 2 diabetes and their role in managing diabetic kidney disease
| Drug class | Example(s) | Mechanism/action | Evidence of kidney protective effects | GFR range (ml/min/ 1.73m2) |
|---|---|---|---|---|
| Biguanides | Metformin | Reduces hepatic gluconeogenesis [38] | No | >30, lower dose if 30–45 |
| Sulfonylureas |
Glipizide Gliclazide Glimepiride Glyburide |
Stimulates insulin secretion [39] | No | Varies by agent; generally >30 |
| Sodium glucose transport protein-2 inhibitors (SGLT-2i) |
Canagliflozin Dapagliflozin Empagliflozin Ertugliflozin |
Inhibits glucose reabsorption in the kidney thereby lowering blood glucose [40] |
Yes (See Table 3, discussion) |
Varies by agent; generally >20 |
| Glucagon-like Peptide Receptor Agonist (GLP-1 RA) |
Exenatide Exenatide ER Liraglutide Albiglutide Dulaglutide Semaglutide |
Induces insulin secretion, reduces glucagon release, lowers hepatic gluconeogenesis, slows gastric emptying [50] |
Yes (See Table 4, discussion) |
Varies by agent; generally >15; Exenatide is contraindicated for GFR <30 or ESKD |
| Insulin |
Degludec Glargine Detemir NPH Aspart Lispro Glulisine Regular |
No | No restriction by GFR, but doses usually must be reduced for GFR <30 | |
| Dipeptidyl peptidase-4 (DPP4) inhibitors |
Sitagliptin Alogliptin Linagliptin Vildagliptin |
Prevent GLP-1 degradation, thereby lowering blood glucose [61] | No | Varies by agent; generally >30 except for linagliptin which can be used with lower GFR |
| Thiazolidinediones | Pioglitazone | Nuclear transcription regulator and insulin sensitizer [62] | No | No restriction by GFR; watch for worsened fluid retention if eGFR <30 |
Abbreviations: GFR glomerular filtration rate, ESKD end-stage kidney disease, eGFR estimated glomerular filtration rate
Tables 3, 4, and 5 provide summaries of recent clinical trials of agents (SGLT-2i, GLP-1 RA, and non-steroidal mineralocorticoid receptor antagonists, MRAs) showing promise in managing DKD.
Table 3.
Recent clinical trials of SGLT-2i agents with kidney outcomes
| Study | Inclusion criteria | Participants | Kidney outcome(s) | HR (95% CI) or other as specified |
|---|---|---|---|---|
| Studies with at least one primary kidney outcome | ||||
|
CREDENCE [41] Feb 2014–Oct 2018 695 sites in 34 countries [42] |
Adults with T2D, HbA1c 6.5% to 12.0%, age ≥30 yrs, eGFR (CKD-EPI) 30 to ≤90 AND UACR 300-5000, taking stable dose of ACEi or ARB for ≥4 weeks prior to randomization |
N=2202 100 mg canagliflozin once daily N=2199 placebo once daily BL: mean age 63 yrs, 66% male, 67% white, mean HbA1c 8.3%, mean duration T2D 16 yrs, mean eGFR 56, median UACR 927 |
A) Primary kidney composite outcome of ESKD (dialysis for ≥30 days or kidney transplantation or eGFR≤15), doubling of serum creatinine from BL sustained for ≥30 days, or death from kidney or CVD cause B) Secondary kidney composite outcome of ESKD, doubling of serum creatinine, or kidney death C) ESKD D) Doubling of serum creatinine E) Dialysis or kidney transplantation F) Kidney death G) ESKD, kidney- or CVD-related death Dialysis, kidney transplantation, or kidney death |
A) 0.70 (0.59–0.82) B) 0.66 (0.53–0.81) C) 0.68 (0.54–0.86) D) 0.60 (0.48–0.76) E) 0.74 (0.55–1.00) F) – G) 0.73 (0.61–0.87) 0.72 (0.54–0.97) |
|
DAPA-CKD [43] Feb 2017–June 2020 386 sites in 21 countries |
Adults with or without T2D, an eGFR of 25-75 AND a UACR of 200–5000, taking stable dose of ACEi or ARB >4 weeks prior to screening |
N=2152 10mg dapagliflozin once daily N=2152 placebo once daily BL: mean age 62 yrs, 67% male, 53% white, 68% T2D, mean eGFR 43, 48% had UACR >1000 |
A) Primary kidney composite outcome of decline of at least 50% in eGFR or death from kidney or CV cause in participants overall; B) Primary kidney composite outcome of decline of at least 50% in eGFR or death from kidney or CV cause in participants with T2D; C) Primary kidney composite outcome of decline of at least 50% in eGFR or death from kidney or CV cause in participants without T2D D) Secondary kidney outcomes: composite of sustained eGFR decline of at least 50%, ESKD, kidney death; Between-group difference in LS mean slope of eGFR from BL to month 30 |
A) 0.61 (0.51–0.72) B) 0.64 (0.52–0.79) C) 0.50 (0.35–0.72) D) 0.56 (0.45–0.68) Difference = 0.93 mL/min/ 1.73m2/yr (0.61–1.25) |
| Studies with kidney outcomes as secondary outcome(s) only | ||||
|
EMPA-REG OUTCOME [44] July 2010–April 2015 590 sites in 42 countries |
Adults with T2D, HbA1c 7.0 to 10% if on antidiabetic therapy or 7 to 9% for drug naïve, age ≥18 yrs, established CVD or high risk for CVD, eGFR (MDRD) ≥30 |
N=4685 empagliflozin (10 or 25 mg) once daily N=2333 placebo once daily BL: mean age 64.5 yrs, 70% male, 72% white, mean HbA1c 8.1% [45] |
A) Incident or worsening nephropathy (UACR >300) B) Doubling of serum creatinine AND eGFR ≤45 C) Initiation of kidney replacement D) Composite outcome of incident or worsening nephropathy or CV-related death E) Progression to macroalbuminuria F) Composite of b + c + kidney-related death G) Incident albuminuria (UACR≥30) in those with normal albuminuria at BL |
A) 0.61 (0.53–0.70) B) 0.56 (0.39–0.79) C) 0.45 (0.21–0.97) D) 0.61 (0.55–0.69) E) 0.62 (0.54–0.72) F) 0.54 (0.40–0.75) G) 0.95 (0.87–1.04) |
|
CANVAS, CANVAS-R [46] Dec 2009–Feb 2017 667 sites in 30 countries |
Adults with T2D, HbA1c 7% to 10.5%, eGFR ≥30, age ≥30 yrs with symptomatic history of CVD, or age ≥50 yrs with 2+ risk factors for CVD |
N=5795 canagliflozin (100 or 300 mg) N=4347 placebo BL: mean age 63.3 yrs, 64% male, 78% white, mean duration T2D=14 yrs, mean HbA1c 8.2% |
A) Composite of progression of albuminuria (more than 30% increase in albuminuria), change from either normoalbuminuria to microalbuminuria or micro- to macroalbuminuria B) Regression of albuminuria C) Composite of 40% reduction in eGFR for at least 2 consecutive measures, need for kidney replacement therapy, and kidney-related death |
A) 0.73 (0.67–0.79) B) 1.70 (1.51–1.91) C) 0.60 (0.47–0.77) |
|
DECLARE-TIMI 58 [47] April 2013–Sept 2018 882 sites, 33 countries |
Adults with T2D, HbA1c 6.5% to 11.9%, age ≥40 yrs, creatinine clearance ≥60 ml/min, with multiple CVD risk factors or established CVD |
N=8582 dapagliflozin (10 mg once daily) N=8578 placebo (once daily) BL: mean age 64 yrs, 63% male, 80% white, mean HbA1c 8.3%, median duration T2D 10.5 yrs, mean eGFR 85 |
A) Composite of sustained decrease in eGFR (per CKD-EPI) of 40% or more to less than 60, new ESKD, or death from kidney or CV cause B) Sustained decrease in eGFR (per CKD-EPI) of 40% or more to less than 60, new ESKD, or death from kidney cause |
A) 0.76 (0.67–0.87) B) 0.53 (0.43–0.66) |
|
VERTIS-CV [48] Nov 2013–Dec 2019 567 sites in 34 countries |
Adults, with T2D and established atherosclerotic CVD, age ≥40 yrs, HbA1c 7.0% to 10.5%, BMI≥18 kg/m2, eGFR ≥30 |
N=5499 5 or 15 mg ertugliflozin once daily N=2747 placebo once daily BL: mean age 64 yrs, 70% male, 88% white, mean HbA1c 8.2%, mean duration T2D 13 yrs, mean eGFR 76 |
Composite of kidney death, kidney replacement therapy, or doubling of serum creatinine | 0.81 (0.63–1.04) |
|
EMPEROR REDUCED [49] March 2017–May 2020 520 sites in 20 countries |
Adults with chronic heart failure and left ventricular ejection fraction <40%, age ≥18 yrs Note: Roughly 7 in 10 participants were taking MRAs at BL |
N=1863 10 mg empagliflozin once daily N=1867 placebo once daily BL: mean age 67 yrs, 76% male, 70% white, 50% DM, mean eGFR 62 |
A) Rate of decline in eGFR calculated per CKD-EPI equation B) Composite kidney outcome of chronic dialysis or kidney transplantation, profound & sustained reduction in eGFR |
A) Between group difference=1.73 ml/min/1.73m2 (1.10–2.37) B) 0.50 (0.32–0.77) |
Abbreviations: SGLT-2i, sodium glucose transport protein 2 inhibitor; HR, hazard ratio; CI, confidence interval; EMPA-REG OUTCOME, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients, T2D type 2 diabetes, HbA1c glycated hemoglobin, CVD cardiovascular disease, eGFR estimated glomerular filtration rate, in mL/min/1.73 m2 body surface area, MDRD Modification of Diet in Renal Disease, BL baseline, yrs years, UACR urine albumin to creatinine ratio, in mg albumin to g creatinine, CV cardiovascular, CANVAS, CANVAS-R Canagliflozin Cardiovascular Assessment Study, DECLARE-TIMI 58 Dapagliflozin Effect on Cardiovascular Events-Thrombolysis in Myocardial Infarction 58, CKD-EPI chronic kidney disease epidemiology collaboration, ESKD end-stage kidney disease, VERTIS-CV EValuation of ERTugliflozin effIcacy and safety – CardioVascular outcomes, BMI body mass index, EMPEROR REDUCED Empagliflozin Outcome Trial in Patients with Chronic Heart Failure, Reduced Ejection Fraction. MRA mineralocorticoid receptor antagonist, DM diabetes mellitus, CREDENCE Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation, ACEi angiotensin-converting enzyme inhibitor(s), ARB angiotensin II receptor blocker(s), DAPA-CKD Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease, LS least-square, BL baseline
Table 4.
Recent clinical trials of GLP-1 RA agents with kidney outcomes
| Study | Inclusion criteria | Participants | Kidney outcome | HR (95% CI) or other as specified |
|---|---|---|---|---|
| Studies with kidney outcomes as secondary outcome(s) only | ||||
|
LEADER [51] Aug 2010–Dec 2015 410 sites in 32 countries |
Adults with T2D, age ≥50 yrs with established CVD, or age ≥60 yrs with CVD risk factors, HbA1c ≥7%, no GLP-1 RA or DPP-4i for 3 months prior to screening |
N=4668 maximum 1.8mg liraglutide (as tolerated) once daily N=4672 placebo once daily BL: mean age 64 yrs, 64% male, 78% white, mean HbA1c 8.7%, mean duration T2D 13 yrs, mean eGFR (MDRD) 80, 26% had microalbuminuria, 11% had BL macroalbuminuria |
A) Composite of new onset persistent macroalbuminuria, persistent doubling of serum creatine, kidney replacement therapy, death from kidney causes B) New onset persistent macroalbuminuria C) Persistent doubling of serum creatinine D) Kidney replacement therapy E) Death from kidney cause F) Decline in eGFR over 36 months G) Increase in UACR H) New onset microalbuminuria |
A) 0.78 (0.67–0.92) B) 0.74 (0.60–0.91) C) 0.90 (0.67–1.20) D) 0.87 (0.61–1.25) E) 1.60 (0.52–4.90) F) Between group difference=1.02 (p=0.01) G) Between group difference=0.83 (p<0.001) H) 0.87 (0.83–0.93) |
|
REWIND [52] July 2011–Aug 2018 371 sites in 24 countries |
Adults with T2D, age ≥50 with previous CVD event or with CVD risk factors, HbA1c ≤9.5% |
N=4949 1.5mg dulaglutide once weekly N=4952 placebo once weekly BL: mean age 66 yrs, 54% male, 76% white, mean duration T2D 11 yrs, mean HbA1c 7.4%, mean eGFR 77 |
A) Composite of development of macroalbuminuria (UACR>33.9 mg/mmol), sustained decline in eGFR ≥30%, or new chronic kidney replacement therapy B) Development of macroalbuminuria C) Sustained decline in eGFR ≥30% D) New chronic kidney replacement therapy |
A) 0.85 (0.77–0.93) B) 0.77 (0.68–0.87) C) 0.89 (0.78–1.01) D) 0.75 (0.39–1.44) |
|
Harmony Outcomes [53] July 2015–March 2018 610 sites in 28 countries |
Adults with T2D and established CVD, age ≥40 yrs, HbA1c >7%, eGFR (MDRD) ≥30, not using GLP-1 RA at screening |
N=4731 30–50 mg albiglutide as tolerated once weekly N=4732 placebo once weekly BL: mean age 64 yrs, 70% male, 70% white, mean duration T2D 14 yrs, mean HbA1c 8.7%, mean eGFR 79 |
Change in eGFR by treatment group |
Mean eGFR difference=−1.11 (−1.84 to −0.39) at 8 months and -0.43 (−1.26 to 0.41) at 16 months. Figure 4 shows significant difference (no CI overlap) favoring albiglutide at 28 months but no numbers provided |
|
SUSTAIN-6 [54] Feb 2013–March 2016 230 sites in 20 countries |
Adults with T2D, age ≥50 yrs with established CVD, heart failure (NYHA class II or III), or chronic kidney failure OR age ≥60 yrs with one or more CVD risk factors, HbA1c ≥7%, no use of DPP-4i within 30 days prior to screening or GLP-1 RA within 90 days prior to randomization |
N=1648 0.5mg or 1.0 mg semaglutide once weekly N=1649 placebo once weekly BL: mean age 65 yrs, 61% male, 83% white, 30% eGFR>90, mean HbA1c 8.7%, mean T2D duration 14 yrs |
A) New or worsening nephropathy B) Persistent macroalbuminuria C) Persistent doubling of serum creatinine and creatinine clearance per MDRD <45 D) Need for continuous kidney replacement therapy |
A) 0.64 (0.46–-0.88) B) 0.54 (0.37–0.77) C) 1.28 (0.64–2.58) D) 0.91 (0.40–2.07) |
|
AMPLITUDE-O [55] April 2018–Dec 2020 344 sites in 28 countries |
Adults with T2D, HbA1c >7%, age ≥18 yrs with history of CVD, OR males ≥50 yrs/females ≥55 yrs with eGFR (MDRD) 25.0 to 59.9 and ≥1 CV risk factor, no use of GLP-1 RA or DPP-4i within 3 months prior to screening |
N=1359 initial dose 2mg efpeglenatide once weekly, titrated to 4mg or 6mg once daily to study end N=1358 6mg efpeglenatide once weekly N=1359 placebo once weekly BL: mean age 65 yrs, 67% male, 87% white, mean HbA1c 8.9%, mean eGFR 72, mean duration T2D 15 yrs, median UACR 28.3 |
A) Incident macroalbuminuria B) Between-group difference in UACR C) LS mean difference in eGFR D) Decrease in eGFR≥40% for ≥30 days, ESKD, or all-cause death E) Composite of MACE, death from non-CV cause, hospitalization for heart failure, or occurrence of (A) |
A) 0.68 (0.57–0.79) B) 0.68 (0.58–0.80) C) Lower by 21% (14–28%) D) Higher by 0.9 (0.3–1.50) E) 0.77 (0.57–1.02) F) 0.71 (0.59–0.87) |
|
ELIXA [56] June 2010–Feb 2015 829 sites in 49 countries [57] |
Adults with T2D, HbA1c 5.5% to 11.0%, age≥30 yrs, with acute coronary syndrome (STEMI, non-STEMI, or unstable angina) <180 days before screening, HbA1c 5.5 to 11%, and eGFR (MDRD) ≥30, taking GLP-1 RA or DPP-4i during study |
N=3034 10μg lixisenatide increased up to 20μg once daily N=3034 placebo once daily BL: mean age 60 yrs, 69% male, 75% white, mean duration T2D 9 yrs, mean HbA1c 7.7%, mean eGFR 76 |
Percent change in UACR from BL to study week 108 (BL UACR and study week 108 data available for n=2830 placebo, n=2803 lixisenatide) |
+34% placebo, +24% lixisenatide, p<0.01, adjusted for BL UACR, treatment, region, BL use of ACEi and ARB; +32% placebo, +26 lixisenatide, p=0.07, adjusted for BL and 3-month HbA1c |
|
EXSCEL [58] June 2010–April 2017 688 sites in 35 countries [59] |
Adults with T2D, HbA1c 6.5% to 10.0%, age≥18 yrs, eGFR (MDRD) ≥30, range of CV risk factors, taking 0 to 3 oral glycemic control drugs or insulin with or without use of 1–2 oral glycemic drugs, never used GLP-1 RA |
Propensity score matched N=572 placebo; N=572 exenatide once weekly +SGLT2i; N=575 exenatide once weekly; N=575 exenatide once weekly + SGLT2i BL: mean age 63 yrs, 62% male, 76% white, mean duration T2D 12 yrs, mean HbA1c 8% |
Outcome comparisons between 1: placebo only with exenatide + SGLT2i, and 2: exenatide only with exenatide + SGLT2i: A) Change over time in eGFR (per MDRD) B) Composite of persistent 40% reduction in eGFR, kidney dialysis, or kidney transplant C) Composite of “B” plus new macroalbuminuria |
A) (1) 1.94 (0.94–2.94); (2) 2.38 (1.40–3.35) B) (1) 0.32 (0.06–1.59); (2) 0.21 (0.05–0.97) C) (1) 0.43 (0.15–1.22); (2) 0.35 (0.13–0.98) |
|
AWARD 7 [60] July 2012–Dec 2016 99 sites in 9 countries |
Adults with T2D and stage 3 or 4 CKD, age≥18 yrs, HbA1c 7.5% to 10.5%, taking insulin alone or with oral glucose control drug, taking maximum tolerated dose of ACEi or ARB, not taking GLP-1 RA or DPP-4i |
N=192 1.5mg dulaglutide once weekly; N=190 0.75mg dulaglutide once weekly; N=194 insulin glargine once daily BL: mean age 65 yrs, 69% white, 52% male, mean HbA1c 8.6%, mean duration T2D 18 yrs, mean eGFR (CKD-EPI) by creatinine 36 (35 by cystatin C), median UACR = 214 for dulaglutide 1.5mg, = 234 for dulaglutide 0.75mg, = 196 for insulin glargine |
Outcome comparisons between (1) insulin glargine vs dulaglutide 1.5mg, and (2) insulin glargine vs dulaglutide 0.75mg A) Change in eGFR per CKD-EPI creatinine B) Change in eGFR per CKD-EPI cystatin C C) UACR change from BL D) Change in eGFR per MDRD E) Kidney events of increase in serum creatinine >30% from BL, ESKD |
A) Week 26 LS mean change (1): −0.1 (p<0.05), (2): −0.4 (p<0.05) Week 52 Change (1): −1.1 (ns), (2): −1.5 (ns) B) Week 26 LS mean change (1): 0.8 (p<0.05), (2): 1.1 (p<0.0001); Week 52 Change (1): −0.7 (p<0.05), (2): −0.7 (p<0.05) C) Week 26 Among those with BL macro-albuminuria, UACR decreased for dulaglutide 1.5mg vs insulin by 43.1% (p=0.008) at week 26 and decreased by 29% (p=0.02) at week 52; for dulaglutide 0.75mg, a decrease of 25.3% (no p-value provided) at week 26 and decrease of 12.3 (no p-value provided) at week 52; for those without BL macroalbuminuria, decrease of 0.4% at week 26 (ns) and decrease of 3.4 % (ns) at week 52 for dulaglutide 1.5mg; for dulaglutide 0.75mg, decrease of 18% (ns) at week 26 and decrease of 15.3% (ns) at week 52 D) Week 26 LS mean change (1): no change (p<0.05), (2): −0.2 (p<0.05); Week 52 change (1): −0.4 (p<0.05), (2) −1.3 (ns) E) Number of events Dulaglutide 1.5mg = 79 (41%); Dulaglutide 0.75mg = 73 (38%); Insulin = 91 (47%) |
Abbreviations: GLP-1 RA glucagon-like peptide-1 receptor agonist, HR hazard ratio, CI confidence interval, LEADER Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results, T2D type 2 diabetes, CVD cardiovascular disease, HbA1c glycated hemoglobin, DPP-4i dipeptidyl peptidase-4 inhibitor, BL baseline, yrs years, eGFR estimated glomerular filtration rate, in mL/min/1.73 m2 body surface area, MDRD Modification of Diet in Renal Disease, UACR urine albumin to creatinine ratio, in mg albumin to g creatinine, Harmony Outcomes Effect of albiglutide, when added to standard blood glucose lowering therapies, on major cardiovascular events in subjects with type 2 diabetes, REWIND Dulaglutide and Cardiovascular Outcomes in Type 2 Diabetes, SUSTAIN-6 Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes, NYHA New York Heart Association, AMPLITUDE-O Effect of Efpeglenatide on Cardiovascular Outcomes, CV cardiovascular, MACE major adverse cardiovascular events, ELIXA Evaluation of Lixisenatide in Acute Coronary Syndrome, STEMI ST-elevation myocardial infarction, ACEi angiotensin-converting enzyme inhibitor, ARB angiotensin II receptor blocker, EXSCEL Exenatide Study of Cardiovascular Event Lowering, SGLT2i sodium glucose transport protein 2 inhibitor, AWARD 7 Assessment of Weekly Administration of LY2189265 (dulaglutide) in Diabetes, CKD-EPI chronic kidney disease epidemiology collaboration, ESKD end-stage kidney disease, LS least squares, ns non-significant, BL baseline
Table 5.
Recent clinical trials of MRA agents with kidney outcomes
| Study | Inclusion criteria | Participants | Kidney outcome | HR (95% CI) or other as specified |
|---|---|---|---|---|
| Studies with at least one primary kidney outcome | ||||
|
FIDELIO DKD [63] Sept 2015–April 2020 978 sites in 48 countries |
Adults with T2D and CKD (UACR 30 to <300 AND eGFR (CKD-EPI) 25 to <60 OR UACR 300-5000 AND eGFR 25 to <75), age ≥18 yrs, taking maximum tolerated dose of ACEi or ARB, serum potassium ≤4.8 mmol/L, HbA1c ≤12% |
N=2833 finerenone, 10mg once daily titrated up to 20mg once daily as tolerated N=2841 placebo once daily BL: mean age 66 yrs, 70% male, 63% white, mean duration T2D 17 yrs, mean HbA1c 7.7%, mean eGFR 44, median UACR 852, mean serum potassium 4.37 mmol/L, 7% taking GLP-1 RA, 5% taking SGLT2i |
Primary outcomes: A) Kidney composite of kidney failure (ESKD or eGFR <15), sustained decrease of ≥40% in eGFR from BL for ≥4 weeks, or kidney-related death B) Kidney failure C) ESKD D) eGFR <15 E) Sustained decrease of ≥40% in eGFR from BL for ≥4 weeks F) Kidney-related death Secondary outcomes G) Change in UACR from BL to study month 4 H) Composite of kidney failure, sustained decrease of ≥57% from BL eGFR for ≥4 weeks, or kidney-related death I) Sustained decrease of ≥57% from BL eGFR for ≥4 weeks |
A) 0.82 (0.73–0.93) B) 0.87 (0.72–1.05) C) 0.86 (0.67–1.10) D) 0.82 (0.67–1.01) E) 0.81 (0.72–0.92) F) -- G) Between group difference=0.69 (0.66, 0.71) H) 0.76 (0.65, 0.90) A) I) 0.68 (0.55–0.82) |
| Studies with kidney outcomes as secondary outcome(s) only | ||||
|
FIGARO DKD [64] Sept 2015–Feb 2021; NOTE: COVID-19 caused trial disruption for 29% of pts, and temporary interruption of trial regiment for 10% of pts 975 sites in 48 countries |
Adults with T2D, age ≥18 yrs, HbA1c <12%, with either UACR 30 to <300 AND eGFR (per CKD-EPI) 25 to 90 OR UACR 300-5000 AND eGFR ≥60, taking ACEi or ARB at maximum tolerated dose, serum potassium ≤4.8 mmol/L at screening |
N=3686 finerenone, 10mg once daily titrated up to 20mg per day as tolerated N=3666 placebo once daily BL: mean age 64 yrs, 69% male, 72% white, mean HbA1c 7.7%, mean eGFR 68, median UACR 308, 8% taking SGLT2i, and 8% taking GLP-1 RA at BL, with additional 16% and 11%, respectively, starting over study period |
A) Composite of 1st occurrence of kidney failure (ESKD or sustained decrease in eGFR <15), sustained decrease of ≥40% from BL eGFR for ≥4 weeks, or kidney-related death B) 1st occurrence of kidney failure C) ESKD D) Sustained decrease in eGFR <15 E) sustained decrease of ≥40% from BL eGFR for ≥4 weeks F) kidney-related death G) Change in UACR from BL to study week 4 H) Composite of 1st occurrence of kidney failure, sustained decrease of ≥57% from BL eGFR for ≥4 weeks, or kidney-related death I) sustained decrease of ≥57% from BL eGFR for ≥4 weeks |
B) 0.87 (0.76–1.01) C) 0.72 (0.49–1.05) D) 0.64 (0.41–0.995) E) 0.71 (0.43–1.16) F) 0.87 (0.75–1.00) G) – H) Between group difference=0.68 (0.65–0.70) I) 0.77 (0.60–0.99) J) 0.76 (0.58–1.00) |
Abbreviations: MRA mineralocorticoid receptor antagonist, HR hazard ratio, CI confidence interval, FIGARO DKD FInerenone in reducinG cArdiovascular moRtality and mOrbidity in Diabetic Kidney Disease, T2D type 2 diabetes, yrs years, HbA1c glycated hemoglobin, UACR urine albumin to creatinine ratio, in mg albumin to g creatinine, eGFR estimated glomerular filtration rate, in mL/min/1.73 m2 body surface area, CKD-EPI chronic kidney disease epidemiology collaboration, ACEi angiotensin-converting enzyme inhibitor, ARB angiotensin II receptor blocker, BL baseline, SGLT2i sodium glucose transport protein 2 inhibitor, ESKD end-stage kidney disease, FIDELIO DKD FInerenone in reducing kiDnEy faiLure and dIsease prOgression in Diabetic Kidney Disease
SGLT-2i agents (Table 3)
Two double-blind, randomized, placebo-control trials, Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) [41] and Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) [43], included kidney disease endpoints as the primary outcome. In CREDENCE, participants assigned to canagliflozin had a 30% reduced risk (hazard ratio (HR)=0.70 [95% confidence interval (CI): 0.59–0.82]) of the primary kidney composite outcome (ESKD, doubling of serum creatinine from baseline sustained for at least 30 days, or death from kidney or cardiovascular disease causes) as compared with participants assigned to placebo [41]. A similar effect was seen in DAPA-CKD, with participants assigned to dapagliflozin having a 39% reduced risk (HR=0.61 [95% CI: 0.51–0.72]) of the primary kidney composite outcome (>50% decline in eGFR from baseline or kidney- or CV-related death) as compared to those in the placebo arm [43]. The majority of participants in both trials were already receiving ACEi or ARBs in maximum tolerated doses where possible. Approximately one third (n=1398) of the participants in DAPA-CKD did not have T2D [43].
Other clinical trials with SGLT-2i investigated kidney disease outcomes as a secondary outcome. Four trials, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME) [44], Canagliflozin Cardiovascular Assessment Study (CANVAS, CANVAS-R) [46], Dapagliflozin Effect on Cardiovascular Events-Thrombolysis in Myocardial Infarction 58 (DECLARE-TIMI 58) [47], and Empagliflozin Outcome Trial in Patients with Chronic Heart Failure, Reduced Ejection Fraction (EMPEROR REDUCED) [49], reported lower rates of kidney disease composite outcomes in those assigned to the active drug than to placebo (EMPA-REG OUTCOME HR=0.61 [95% CI: 0.53–0.70]; CANVAS, CANVAS-R HR=0.73 [95% CI: 0.67–0.79]; DECLARE-TIMI 58 HR=0.76 [95% CI: 0.67–0.87]; EMPEROR REDUCED HR=0.50 [95% CI: 0.32–0.77]) [44, 46, 47, 49]. Composite kidney disease outcomes were somewhat similar between studies (e.g., composite of sustained decrease in eGFR of 40% or more, to less than 60 mL/min/1.73 m2, incident ESKD, death from kidney or cardiovascular disease causes in DECLARE-TIMI 58 and incident chronic dialysis or kidney transplantation, profound and sustained reduction in eGFR in EMPEROR REDUCED) [47, 49]. One study, eValuation of ERTugliflozin effIcacy and safety – CardioVascular outcomes (VERTIS-CV) [48], reported no significant difference in their secondary kidney disease outcome (death due to kidney disease, kidney replacement therapy, or doubling of serum creatinine) between those randomized to ertugliflozin versus placebo (HR=0.80 [95% CI: 0.61–1.05] )[48].
GLP-1 RA agents (Table 4)
Cardiovascular outcome trials have also examined GLP-1 RA in people with T2D with kidney disease outcomes as secondary outcomes; to date, there are no published studies of GLP-1 RAs with kidney outcomes as a primary outcome. Randomized, placebo-controlled trials including Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results (LEADER) [51]; Dulaglutide and Cardiovascular Outcomes in Type 2 Diabetes (REWIND) [42]; Effect of albiglutide, when added to standard blood glucose lowering therapies, on major cardiovascular events in subjects with type 2 diabetes (Harmony Outcomes) [52]; Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes (SUSTAIN-6) [53]; Exenatide Study of Cardiovascular Event Lowering (EXSCEL) [54]; Evaluation of Lixisenatide in Acute Coronary Syndrome (ELIXA) [58]; Assessment of Weekly Administration of dulaglutide in Diabetes (AWARD 7) [56]; and Effect of Efpeglenatide on Cardiovascular Outcomes (AMPLITUDE-O) [60] all reported significantly lower rates of kidney disease outcomes in participants assigned to the active drug as compared with those assigned to placebo, or active drug as compared to insulin in AWARD-7. LEADER, REWIND, and AMPLITUDE-O report significantly lower risk of composite kidney disease outcomes among those assigned to study drug versus placebo (LEADER HR=0.78 [95% CI: 0.67–0.92]; REWIND HR=0.85 [95% CI: 0.77–0.93]; AMPLITUDE-O HR=0.68 [95% CI: 0.57–0.79]) [42, 51, 60]. EXSCEL found no significant difference in risk of their composite outcome (HR=0.43 [95% CI: 0.15–1.22]) [54].
Other GLP-1RA studies reported on individual kidney disease measures. In Harmony Outcomes, there was a between-group difference (albiglutide vs. placebo) in change in eGFR at 8 months (mean difference=−1.11 [95% CI: −1.84 to 0.39]) and at 16 months (mean difference=−0.43 [95% CI: −1.26 to 0.41]) [52]. SUSTAIN-6 reported significantly lower risk of new or worsening nephropathy (HR=0.64 [95% CI: 0.46–0.88]) or persistent macroalbuminuria (HR=0.54 [95% CI: 0.37–0.77]) among those assigned to semaglutide as compared with placebo [53]. In ELIXA, participants assigned to lixisenatide had a 24% increase in UACR from baseline to study week 108 while those assigned to placebo had a 34% increase, a significant difference (p=0.004) [58]. In AWARD 7, participants assigned to dulaglutide had higher eGFR at 52 weeks than those assigned to insulin glargine (eGFR least square means = 34.0 mL/min/1.73m2, p=0.005 for dulaglutide 1.5 mg, eGFR least square means = 33.8 mL/min/1.73 m2, p=0.009 for dulaglutide 0.75mg) [56]. More details of these studies are provided in Table 4. As the kidney outcomes mentioned here were all secondary outcomes from cardiovascular outcomes or glycemic lowering trials, there is a clear need for studies with primary kidney disease outcomes in participants with T2D and DKD [55]. The Effect of Semaglutide Versus Placebo on the Progression of Renal Impairment in Subjects With Type 2 Diabetes and Chronic Kidney Disease (FLOW, NCT03819153) trial is investigating a GLP-1RA with a primary kidney disease outcome (≥50% eGFR decline, kidney failure, and death from kidney or CV disease) [65]. A companion study, Renal Mode of Action of Semaglutide in Patients With Type 2 Diabetes and Chronic Kidney Disease (REMODEL, NCT04865770), is examining the effect of semaglutide on kidney inflammation, perfusion, and oxygenation [66].
MRA agents (Table 5)
Two recent clinical trials report on the effects of a non-steroidal MRA, finerenone, on kidney disease outcomes. Finerenone demonstrated positive results in FInerenone in reducing kiDnEy faiLure and dIsease prOgression in Diabetic Kidney Disease (FIDELIO-DKD) with kidney disease endpoints as primary outcomes [67]. In this study, participants assigned to finerenone had an 18% lower risk of the primary composite outcome (ESKD or eGFR <15 mL/min/1.73 m2, sustained decrease of ≥40% in eGFR from baseline for ≥4 weeks, or kidney disease death) as compared with those assigned to placebo (HR=0.82 [95% CI=0.73–0.93]) [67]. FInerenone in reducinG cArdiovascular moRtality and mOrbidity in Diabetic Kidney Disease (FIGARO-DKD) [68] included kidney disease endpoints as secondary outcomes. Participants assigned to finerenone had a 23% lower risk of the composite kidney disease outcome of first occurrence of kidney failure, sustained decrease from baseline eGFR ≥57% for ≥4 weeks, or kidney disease death as compared to the placebo arm (HR=0.77 [95% CI: 0.60–0.99]) [68]. Both of these clinical trials included participants with T2D and DKD who were on a maximally tolerated dose of an ACE inhibitor or ARB [67, 68]. The FInerenone in chronic kiDney diseasE and type 2 diabetes: Combined FIDELIO-DKD and FIGARO-DKD Trial programme analYsis (FIDELITY) [57] prespecified meta-analysis reported that finerenone significantly reduced risk of kidney disease outcomes (kidney failure, sustained ≥57% decrease in eGFR, or kidney disease death) by 23% and the risk of cardiovascular endpoints (death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure) by 14% versus placebo in >13,000 participants. Finerenone was well tolerated, but investigator-reported hyperkalemia (serum potassium concentration >5.5 mmol/l) was more common versus placebo (14.0% versus 6.9%, respectively) [57].
Conclusions
DKD is a frequent and serious complication in people with T2D and diabetes is the most common cause of ESKD and kidney failure worldwide [59]. Glycemic control and blood pressure management, with preferential use of agents that attenuate the renin-angiotensin aldosterone system, have traditionally represented the cornerstone for prevention and treatment of DKD. Even though these measures may reduce albuminuria, their beneficial effects on GFR decline or progression to ESKD are modest [63, 64, 69, 70].
In recent studies, treatment with SGLT-2i and GLP-1 RA proved to reduce the risk for a combined major adverse cardiovascular event endpoint (including cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) [60, 71]. In the CREDENCE and the DAPA-CKD trials, treatment with canagliflozin and dapagliflozin were shown to reduce risks of substantial eGFR decline or kidney failure with a primary kidney disease outcome in adults with T2D who had DKD. These findings have inspired many organizations that produce clinical practice guidelines across the world to recommend these agents over other treatments in people with T2D and DKD and/or cardiovascular disease.
Despite these new therapeutic opportunities for treating people with T2D, the risk of DKD progression remains [11, 72]. There is evidence to support the role of the mineralocorticoid receptor through inflammation and fibrosis in the progression of DKD [72]. Treatment of DKD with older steroidal MRAs has not been widely implemented because of their high rate of unfavorable side effects such as hyperkalemia [72]. However, finerenone is a new non-steroidal MRA with less side effects and more potent anti-inflammatory and antifibrotic effects as compared with steroidal MRAs [73, 74]. Finerenone was shown to evoke kidney and cardiovascular protective effects in people with T2D and DKD [57, 67]. Therefore, promising new pharmacological drugs are available to be used in people with DKD.
Drugs like phosphodiesterase inhibitors, 5-hydroxytrytamine 2a receptor antagonists, aldosterone synthesis inhibitors, anti-inflammatory agents, and others are under clinical development. Such additional classes of agents might further increase the armamentarium in the treatment of DKD in the future [33, 75]. Even though new drugs will help to improve the prognosis of people with DKD, it becomes more and more a challenge for physicians to choose the most beneficial medication or combination of medications for an individual patient. There is a need to evaluate the kidney-protective effects of different treatment modalities based on individual characteristics. For example, it would be important to evaluate if different drugs might have a distinct efficacy in patients with DKD with and without albuminuria. Combination therapy with SGLT-2is and MRAs also need to be better explored to understand if benefits are additive. Additional clinical and real-world studies are warranted to elucidate best clinical practices.
It is important to emphasize the intention of this review, along with its limitations. We aimed to provide an overview on recent renal data of SGLT-2i, GLP-1 RAs, and MRAs. Most of the studies included in the review were cardiovascular outcome trials, with kidney outcomes as secondary outcomes. As such, they may not have sufficient power to provide confirmative answers on kidney-related endpoints, especially when examined by subgroups. Furthermore, for composite secondary kidney outcomes, examining each individual component of the composite outcome provided interesting information, but again, these results were underpowered to be considered confirmatory. With the composite renal outcomes of studies examining GLP-1 RAs driven primarily by reductions in albuminuria, the studies do not prove any beneficial effect of GLP-1 RA on kidney outcomes. Even though many of the results are not confirmatory, they are of interest to discuss potential effects in an exploratory sense. Results of these trials are thesis generating and should not be interpreted in a confirmatory sense. This highlights the need for future trials with kidney outcomes as primary outcomes of interest.
Acknowledgements
The authors would like to thank Karen Nunley, PhD (Syneos Health), for serving as the medical writer for this article; Joe Durrant (Syneos Health) for editorial assistance; and Nadja Faisst of Clinical Research Services (CRS).
Abbreviations
- ACEi
Angiotensin-converting enzyme inhibitor
- ADA
American Diabetes Association
- AMPLITUDE-O
Effect of Efpeglenatide on Cardiovascular Outcomes
- ARB
Angiotensin II receptor blocker
- AWARD 7
Assessment of Weekly Administration of dulaglutide in Diabetes
- BL
Baseline
- CANVAS/CANVAS-R
Canagliflozin Cardiovascular Assessment Study
- CI
Confidence interval
- CKD
Chronic kidney disease
- CKD-EPI
Chronic Kidney Disease Epidemiology Collaboration
- CREDENCE
Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation
- CVD
Cardiovascular disease
- DAPA-CKD
Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease
- DECLARE-TIMI 58
Dapagliflozin Effect on Cardiovascular Events-Thrombolysis in Myocardial Infarction 58
- DKD
Diabetic kidney disease
- eGFR
Estimated glomerular filtration rate
- ELIXA
Evaluation of Lixisenatide in Acute Coronary Syndrome
- EMPA-REG OUTCOME
Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients
- EMPEROR REDUCED
Empagliflozin Outcome Trial in Patients with Chronic Heart Failure, Reduced Ejection Fraction
- ESKD
End-stage kidney disease
- EXSCEL
Exenatide Study of Cardiovascular Event Lowering
- FIDELIO-DKD
FInerenone in reducing kiDnEy faiLure and dIsease prOgression in Diabetic Kidney Disease
- FIDELITY
FInerenone in chronic kiDney diseasE and type 2 diabetes: Combined FIDELIO-DKD and FIGARO-DKD Trial programme analysis
- FIGARO-DKD
FInerenone in reducinG cArdiovascular moRtality and mOrbidity in Diabetic Kidney Disease
- GFR
Glomerular filtration rate
- GLP-1 RA
Glucagon-like peptide-1 receptor agonist
- Harmony Outcomes
Effect of albiglutide, when added to standard blood glucose lowering therapies, on major cardiovascular events in subjects with type 2 diabetes
- HbA1c
Glycated hemoglobin
- HR
Hazard ratio
- KDIGO
Kidney Disease Improving Global Outcomes
- LDL
Low density lipoprotein
- LEADER
Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results
- LS
Least squares
- LSM
Least square method
- MDRD
Modification of Diet in Renal Disease
- MRA
Mineralocorticoid receptor antagonist
- ns
Non-significant
- NYHA
New York Heart Association
- RAS
Renin-angiotensin system
- REWIND
Dulaglutide and Cardiovascular Outcomes in Type 2 Diabetes
- SGLT-2i
Sodium glucose transport protein 2 inhibitor
- SGLT2
Sodium glucose transport protein 2
- SUSTAIN-6
Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes
- T2D
Type 2 diabetes
- UACR
Urinary albumin to creatinine ratio
- VERTIS- CV
EValuation of ERTugliflozin effIcacy and safety – CardioVascular outcomes
- yrs
Years
Authors’ contributions
TF contributed to the conception of this review, as well as drafting and revising the manuscript. KRT, DCW, NP, FG, RES, AH, MS, OS, and CM contributed to this review by thorough and extensive revision of the structure, draft, and final manuscript. All authors read and approved the final manuscript.
Funding
This review was funded by Clinical Research Services.
Availability of data and materials
Cited sources are available online
Declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
TF provided advisory services to Astra Zeneca, Atrogi, Bayer, Cipla, Eli Lilly, Eysense, Fortbildungskolleg, Novo Nordisk, Pfizer, Sanofi, Remynd, and Roche. TF provided speaker services to Amarin, Astra Zeneca, Böhringer Ingelheim, Berlin Chemie, Cipla, Daiichi-Sankyo, Eli Lilly, Fortbildungskolleg, MSD, Novartis, Novo Nordisk, Sanofi, and Santis.
FG provided advisory services to AstraZeneca, Eli Lilly, Novo Nordisk, Roche Diabetes Care, and Sanofi; received speaker fees and served as a consultant for Boehringer Ingelheim, Lifescan, Merck Sharp & Dohme, Sanofi, AstraZeneca, Medimmune, Roche Diabetes Care, Sanofi, and Medtronic; and received research support from Eli Lilly and Roche Diabetes Care.
KRT is supported by NIH research grants R01MD014712, U2CDK114886, UL1TR002319, U54DK083912, U01DK100846, OT2HL161847, UM1AI109568, and CDC contract 75D301-21-P-12254; other support from Eli Lilly; personal fees and other support from Boehringer Ingelheim; personal fees and other support from AstraZeneca; grants, personal fees, and other support from Bayer AG; grants, personal fees, and other support from Novo Nordisk; grants and other support from Goldfinch Bio; other support from Gilead; and grants from Travere outside the submitted work.
RES is supported by grants from AstraZeneca, Boehringer Ingelheim, Lilly, and NovoNordisk to the Institution (University Hospital Eralngen); personal advisory and speaker fees were received from AstraZeneca, Bohringer Ingelheim, and NovoNordisk.
NP has been an advisory board member of AstraZeneca, Boehringer Ingelheim, MSD, NovoNordisk, Pfizer, Takeda, and TrigoCare International; has participated in sponsored studies by AstraZeneca, Eli Lilly, GSK, MSD, Novo Nordisk, Novartis, and Sanofi-Aventis; has received honoraria as a speaker for AstraZeneca, Boehringer Ingelheim, Eli Lilly, Elpen, MSD, Mylan, NovoNordisk, Pfizer, Sanofi-Aventis, and Vianex; and attended conferences sponsored by TrigoCare International, Eli Lilly, Galenica, NovoNordisk, Pfizer, and Sanofi-Aventis.
DCW has an ongoing consultancy agreement with AstraZeneca. In the last 3 years, he has also received payments from Amgen, Astellas, Bayer, Boehringer Ingelheim, Janssen, Gilead, GlaxoSmithKline, Merck Sharp and Dohme, Mundipharma, Tricida, Vifor, and Zydus.
OS is founder and CEO of Sciarc GmbH, Germany.
CM serves or has served on the advisory panel for NovoNordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, and Vertex. Financial compensation for these activities has been received by KU Leuven; KU Leuven has received research support for CM from Medtronic, Imcyse, NovoNordisk, Sanofi, and ActoBio Therapeutics; CM serves or has served on the speaker’s bureau for NovoNordisk, Sanofi, Eli Lilly, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
AH and MS declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Thomas Forst, Email: Thomas.Forst@crs-group.de.
Chantal Mathieu, Email: chantal.mathieu@uzleuven.be.
Francesco Giorgino, Email: francesco.giorgino@uniba.it.
David C. Wheeler, Email: d.wheeler@ucl.ac.uk
Nikolaos Papanas, Email: papanasnikos@yahoo.gr.
Roland E. Schmieder, Email: roland.schmieder@fau.de
Atef Halabi, Email: atef.halabi@crs-group.de.
Oliver Schnell, Email: oliver.schnell@sciarc.de.
Marina Streckbein, Email: Marina.Streckebein@crs-group.de.
Katherine R. Tuttle, Email: Katherine.Tuttle@providence.org
References
- 1.International Diabetes Federation. IDF Diabetes Atlas. https://diabetesatlas.org/2021. Accessed 30 Aug 2022.
- 2.Xu G, Liu B, Sun Y, Du Y, Snetselaar LG, Hu FB, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497. doi: 10.1136/bmj.k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Diabetes Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 30 Aug 2022.
- 4.Thomas MC, Cooper ME, Zimmet P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016;12:73–81. doi: 10.1038/nrneph.2015.173. [DOI] [PubMed] [Google Scholar]
- 5.Gheith O, Farouk N, Nampoory N, Halim MA, Al-Otaibi T. Diabetic kidney disease: world wide difference of prevalence and risk factors. J Nephropharmacol. 2016;5:49–56. [PMC free article] [PubMed] [Google Scholar]
- 6.Fu H, Liu S, Bastacky SI, Wang X, Tian X-J, Zhou D. Diabetic kidney diseases revisited: a new perspective for a new era. Mol Metab. 2019;30:250–263. doi: 10.1016/j.molmet.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H, Lu W, Wang A, Jiang H, Lyu J. Changing epidemiology of chronic kidney disease as a result of type 2 diabetes mellitus from 1990 to 2017: estimates from Global Burden of Disease 2017. J Diabetes Investig. 2021;3:346–356. doi: 10.1111/jdi.13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Górriz JL, Soler MJ, Navarro-González JF, García-Carro C, Puchades MJ, D'Marco L, et al. GLP-1 receptor agonists and diabetic kidney disease: a call of attention to nephrologists. J Clin Med. 2020;9:947. doi: 10.3390/jcm9040947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson A-M, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–644. doi: 10.1056/NEJMoa1800256. [DOI] [PubMed] [Google Scholar]
- 10.Alicic RZ, Johnson EJ, Tuttle KR. Inflammatory mechanisms as new biomarkers and therapeutic targets for diabetic kidney disease. Adv Chronic Kidney Dis. 2018;25:181–191. doi: 10.1053/j.ackd.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12:2032–2045. doi: 10.2215/CJN.11491116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pichler R, Afkarian M, Dieter BP, Tuttle KR. Immunity and inflammation in diabetic kidney disease: translating mechanisms to biomarkers and treatment targets. Am J Physiol Ren Physiol. 2017;312:F716–Ff31. doi: 10.1152/ajprenal.00314.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cappelli C, Tellez A, Jara C, Alarcón S, Torres A, Mendoza P, et al. The TGF-β profibrotic cascade targets ecto-5'-nucleotidase gene in proximal tubule epithelial cells and is a traceable marker of progressive diabetic kidney disease. Biochim Biophys Acta Mol basis Dis. 2020;1866:165796. doi: 10.1016/j.bbadis.2020.165796. [DOI] [PubMed] [Google Scholar]
- 14.Chagnac A, Herman M, Zingerman B, Erman A, Rozen-Zvi B, Hirsh J, et al. Obesity-induced glomerular hyperfiltration: its involvement in the pathogenesis of tubular sodium reabsorption. Nephrol Dial Transplant. 2008;23:3946–3952. doi: 10.1093/ndt/gfn379. [DOI] [PubMed] [Google Scholar]
- 15.Benzing T, Salant D. Insights into glomerular filtration and albuminuria. N Engl J Med. 2021;384:1437–1446. doi: 10.1056/NEJMra1808786. [DOI] [PubMed] [Google Scholar]
- 16.Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, et al. Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J Hypertens. 2011;29:1802–1809. doi: 10.1097/HJH.0b013e3283495cd6. [DOI] [PubMed] [Google Scholar]
- 17.Dwyer JP, Parving HH, Hunsicker LG, Ravid M, Remuzzi G, Lewis JB. Renal dysfunction in the presence of normoalbuminuria in type 2 diabetes: Results from the DEMAND study. Cardiorenal Med. 2012;2:1–10. doi: 10.1159/000333249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng L, Li W, Xu G. Update on pathogenesis and diagnosis flow of normoalbuminuric diabetes with renal insufficiency. Eur J Med Res. 2021;26:144. doi: 10.1186/s40001-021-00612-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tervaert TWC, Mooyaart AL, Amann K, Cohen AH, Cook HT, Drachenberg CB, et al. Pathologic classification of diabetic nephropathy. J Am Soc Nephrol. 2010;21:556–563. doi: 10.1681/ASN.2010010010. [DOI] [PubMed] [Google Scholar]
- 20.Ballew SH, Matsushita K. Cardiovascular risk prediction in ckd. Semin Nephrol. 2018;38:208–216. doi: 10.1016/j.semnephrol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association 11. Microvascular complications and foot care: Standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S135–Ss51. doi: 10.2337/dc20-S011. [DOI] [PubMed] [Google Scholar]
- 22.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. doi: 10.1038/kisup.2012.73. [DOI] [Google Scholar]
- 23.Perkins BA, Ficociello LH, Ostrander BE, Silva KH, Weinberg J, Warram JH, et al. Microalbuminuria and the risk for early progressive renal function decline in type 1 diabetes. J Am Soc Nephrol. 2007;18:1353–1361. doi: 10.1681/ASN.2006080872. [DOI] [PubMed] [Google Scholar]
- 24.Delgado C, Baweja M, Crews DC, Eneanya ND, Gadegbeku CA, Inker LA, et al. A unifying approach for gfr estimation: recommendations of the NKF-ASN task force on reassessing the inclusion of race in diagnosing kidney disease. Am J Kidney Dis. 2022;79:268–288. doi: 10.1053/j.ajkd.2021.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Williams WW, Hogan JW, Ingelfinger JR. Time to eliminate health care disparities in the estimation of kidney function. N Engl J Med. 2021;385:1804–1806. doi: 10.1056/NEJMe2114918. [DOI] [PubMed] [Google Scholar]
- 26.Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, et al. New creatinine- and cystatin c-based equations to estimate gfr without race. N Engl J Med. 2021;385:1737–1749. doi: 10.1056/NEJMoa2102953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98:S1–s115. doi: 10.1016/j.kint.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Chen DC, Shlipak MG, Scherzer R, Bauer SR, Potok OA, Rifkin DE, et al. Association of intraindividual difference in estimated glomerular filtration rate by creatinine vs cystatin c and end-stage kidney disease and mortality. JAMA Netw Open. 2022;5:e2148940. doi: 10.1001/jamanetworkopen.2021.48940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bargnoux A-S, Piéroni L, Cristol J-P, Kuster N, Delanaye P, Carlier M-C, et al. Multicenter evaluation of cystatin c measurement after assay standardization. Clin Chem. 2017;63:833–841. doi: 10.1373/clinchem.2016.264325. [DOI] [PubMed] [Google Scholar]
- 30.Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, et al. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303:423–429. doi: 10.1001/jama.2010.39. [DOI] [PubMed] [Google Scholar]
- 31.Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–2081. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Diabetes Association 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S66–s76. doi: 10.2337/dc20-S006. [DOI] [PubMed] [Google Scholar]
- 33.Doshi SM, Friedman AN. Diagnosis and management of type 2 diabetic kidney disease. Clin J Am Soc Nephrol. 2017;12:1366–1373. doi: 10.2215/CJN.11111016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kidney Disease Improving Global Outcomes Blood Pressure Work Group KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99:S1–s87. doi: 10.1016/j.kint.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 35.American Diabetes Association 10. Cardiovascular disease and risk management: standards of medical care in diabetes—2021. Diabetes Care. 2020;44:S125–SS50. doi: 10.2337/dc21-S010. [DOI] [PubMed] [Google Scholar]
- 36.Kidney Disease Improving Global Outcomes Lipid Work Group KDIGO clinical practice guideline for lipid management in chronic kidney disease. Kidney Int Suppl. 2013;3:259–305. doi: 10.1038/kisup.2013.27. [DOI] [Google Scholar]
- 37.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–713. doi: 10.1136/bmj.317.7160.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foretz M, Guigas B, Viollet B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat Rev Endocrinol. 2019;15:569–589. doi: 10.1038/s41574-019-0242-2. [DOI] [PubMed] [Google Scholar]
- 39.Lv W, Wang X, Xu Q, Lu W. Mechanisms and characteristics of sulfonylureas and glinides. Curr Top Med Chem. 2020;20:37–56. doi: 10.2174/1568026620666191224141617. [DOI] [PubMed] [Google Scholar]
- 40.Hsia DS, Grove O, Cefalu WT. An update on SGLT2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2017;24:73–79. doi: 10.1097/MED.0000000000000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 42.Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Lancet. 2019;394:131–138. doi: 10.1016/S0140-6736(19)31150-X. [DOI] [PubMed] [Google Scholar]
- 43.Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou F-F, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 44.Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–334. doi: 10.1056/NEJMoa1515920. [DOI] [PubMed] [Google Scholar]
- 45.Zinman B, Inzucchi SE, Lachin JM, Wanner C, Ferrari R, Fitchett D, et al. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOME™) Cardiovasc Diabetol. 2014;13:102. doi: 10.1186/1475-2840-13-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neal B, Perkovic V, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:2099. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 47.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2018;380:347–357. doi: 10.1056/NEJMoa1812389. [DOI] [PubMed] [Google Scholar]
- 48.Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383:1425–1435. doi: 10.1056/NEJMoa2004967. [DOI] [PubMed] [Google Scholar]
- 49.Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–1424. doi: 10.1056/NEJMoa2022190. [DOI] [PubMed] [Google Scholar]
- 50.Neumiller JJ. Differential chemistry (structure), mechanism of action, and pharmacology of GLP-1 receptor agonists and DPP-4 inhibitors. J Am Pharm Assoc (2003) 2009;49(Suppl 1):S16–S29. doi: 10.1331/JAPhA.2009.09078. [DOI] [PubMed] [Google Scholar]
- 51.Mann JFE, Ørsted DD, Brown-Frandsen K, Marso SP, Poulter NR, Rasmussen S, et al. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377:839–848. doi: 10.1056/NEJMoa1616011. [DOI] [PubMed] [Google Scholar]
- 52.Hernandez AF, Green JB, Janmohamed S, D'Agostino RB, Sr, Granger CB, Jones NP, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392:1519–1529. doi: 10.1016/S0140-6736(18)32261-X. [DOI] [PubMed] [Google Scholar]
- 53.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–1844. doi: 10.1056/NEJMoa1607141. [DOI] [PubMed] [Google Scholar]
- 54.Clegg LE, Penland RC, Bachina S, Boulton DW, Thuresson M, Heerspink HJL, et al. Effects of exenatide and open-label SGLT2 inhibitor treatment, given in parallel or sequentially, on mortality and cardiovascular and renal outcomes in type 2 diabetes: insights from the EXSCEL trial. Cardiovasc Diabetol. 2019;18:138. doi: 10.1186/s12933-019-0942-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alicic RZ, Cox EJ, Neumiller JJ, Tuttle KR. Incretin drugs in diabetic kidney disease: biological mechanisms and clinical evidence. Nat Rev Nephrol. 2021;17:227–244. doi: 10.1038/s41581-020-00367-2. [DOI] [PubMed] [Google Scholar]
- 56.Tuttle KR, Lakshmanan MC, Rayner B, Busch RS, Zimmermann AG, Woodward DB, et al. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): a multicentre, open-label, randomised trial. Lancet Diabetes Endocrinol. 2018;6:605–617. doi: 10.1016/S2213-8587(18)30104-9. [DOI] [PubMed] [Google Scholar]
- 57.Agarwal R, Filippatos G, Pitt B, Anker SD, Rossing P, Joseph A, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2022;43:474–484. doi: 10.1093/eurheartj/ehab777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Køber LV, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373:2247–2257. doi: 10.1056/NEJMoa1509225. [DOI] [PubMed] [Google Scholar]
- 59.Afkarian M, Zelnick LR, Hall YN, Heagerty PJ, Tuttle K, Weiss NS, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. JAMA. 2016;316(6):602–610. doi: 10.1001/jama.2016.10924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gerstein HC, Sattar N, Rosenstock J, Ramasundarahettige C, Pratley R, Lopes RD, et al. Cardiovascular and renal outcomes with efpeglenatide in type 2 diabetes. N Engl J Med. 2021;385:896–907. doi: 10.1056/NEJMoa2108269. [DOI] [PubMed] [Google Scholar]
- 61.Thornberry NA, Gallwitz B. Mechanism of action of inhibitors of dipeptidyl-peptidase-4 (DPP-4) Best Pract Res Clin Endocrinol Metab. 2009;23:479–486. doi: 10.1016/j.beem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 62.Diamant M, Heine RJ. Thiazolidinediones in type 2 diabetes mellitus: current clinical evidence. Drugs. 2003;63:1373–1405. doi: 10.2165/00003495-200363130-00004. [DOI] [PubMed] [Google Scholar]
- 63.UK Prospective Diabetes Study Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–853. doi: 10.1016/S0140-6736(98)07019-6. [DOI] [PubMed] [Google Scholar]
- 64.Wyatt CM, Cattran DC. Intensive glycemic control and the risk of end-stage renal disease: an ADVANCE in the management of diabetes? Kidney Int. 2016;90:8–10. doi: 10.1016/j.kint.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 65.U.S. National Library of Medicine . A Reseach Study to See How Semaglutide Works Compared to Placebo in People with Type 2 Diabetes and Chronic Kidney Disease (FLOW) 2022. [Google Scholar]
- 66.U.S. National Library of Medicine . A research study to find out how semaglutide works in the kidneys compared to placebo, in people with type 2 diabetes and chronic kidney disease (the REMODEL trial) 2022. [Google Scholar]
- 67.Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383:2219–2229. doi: 10.1056/NEJMoa2025845. [DOI] [PubMed] [Google Scholar]
- 68.Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. N Engl J Med. 2021;385:2252–2263. doi: 10.1056/NEJMoa2110956. [DOI] [PubMed] [Google Scholar]
- 69.Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–139. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 70.Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419–430. doi: 10.1016/S0140-6736(10)60576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Caruso I, Giorgino F. SGLT-2 inhibitors as cardio-renal protective agents. Metabolism. 2022;127:154937. doi: 10.1016/j.metabol.2021.154937. [DOI] [PubMed] [Google Scholar]
- 72.Barrera-Chimal J, Girerd S, Jaisser F. Mineralocorticoid receptor antagonists and kidney diseases: pathophysiological basis. Kidney Int. 2019;96:302–319. doi: 10.1016/j.kint.2019.02.030. [DOI] [PubMed] [Google Scholar]
- 73.Grune J, Beyhoff N, Smeir E, Chudek R, Blumrich A, Ban Z, et al. Selective mineralocorticoid receptor cofactor modulation as ,molecular basis for finerenone’s antifibrotic activity. Hypertension. 2018;71(4):599–608. doi: 10.1161/HYPERTENSIONAHA.117.10360. [DOI] [PubMed] [Google Scholar]
- 74.Agarwal R, Kolkhof P, Bakris G, Bauersachs J, Haller H, Wada T, et al. Steroidal and non-steroidal mineralocorticoid receptor antagonists in cardiorenal medicine. Eur Heart J. 2021;42(2):152–161. doi: 10.1093/eurheartj/ehaa736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Frimodt-Møller M, Persson F, Rossing P. Mitigating risk of aldosterone in diabetic kidney disease. Curr Opin Nephrol Hypertens. 2020;29:145–151. doi: 10.1097/MNH.0000000000000557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Cited sources are available online