Abstract
Objective:
Understanding COVID-19–related mortality among the large population of people experiencing homelessness (PEH) in Los Angeles County (LA County) may inform public health policies to protect this vulnerable group. We investigated the impact of COVID-19 on PEH compared with the general population in LA County.
Methods:
We calculated crude COVID-19 mortality rates per 100 000 population and mortality rates adjusted for age, race, and sex/gender among PEH and compared them with the general population in LA County from March 1, 2020, through February 28, 2021.
Results:
Among adults aged ≥18 years, the crude mortality rate per 100 000 population among PEH was 20% higher than among the general LA County population (348.7 vs 287.6). After adjusting for age, the mortality rate among PEH was 570.7 per 100 000 population. PEH had nearly twice the risk of dying from COVID-19 as people in the general LA County population; PEH aged 18-29 years had almost 8 times the risk of dying compared with their peers in the general LA County population. PEH had a higher risk of mortality than the general population after adjusting for race (standardized mortality ratio [SMR] = 1.4; 95% CI, 1.2-1.6) and sex/gender (SMR = 1.3; 95% CI, 1.1-1.5).
Conclusions:
A higher risk of COVID-19–related death among PEH compared with the general population indicates the need for public health policies and interventions to protect this vulnerable group.
Keywords: homeless, COVID-19 mortality, unhoused
Los Angeles County (LA County) has one of the largest populations of people experiencing homelessness (PEH) in the United States, with 66 436 people identified as experiencing homelessness in 2020. 1 The experience of homelessness has an adverse effect on health status, accounting in part for the increased prevalence of chronic medical conditions, mental health disorders, and substance use disorders in this population. 2 These health disparities likely contribute to premature mortality among PEH, whose average age of death is 42 to 52 years, compared with 72 to 80 years among people with stable housing.3-6
Early prevalence estimates of COVID-19 among PEH vary across US regions. A study of PEH in sheltered settings in Boston, San Francisco, Atlanta, and Seattle through April 2020 cited high COVID-19 prevalence in shelter-wide testing after detection of a cluster of cases, ranging from 17% to 37%, and a low COVID-19 prevalence when 1 or 0 cases preceded the testing event.7-9 Another study found a higher prevalence of COVID-19 among sheltered PEH than among unsheltered PEH in Atlanta in April and May 2020. 10
Among several jurisdictions with publicly reported PEH-specific data from March 2020 through February 2021, PEH had a higher relative risk of death than the general population overall, but case fatality rates varied across jurisdictions. 11 However, case fatality rates may be subject to detection bias. In populations with historical barriers to consistent health care access, those who are most ill may be the ones seeking and receiving medical evaluations. In addition, COVID-19 has differentially affected racial and ethnic minority groups with higher case rates and more clinically severe disease than among White people, and the contribution of differences in race and ethnicity of comparison populations needs to be examined in mortality studies. 12
Because homelessness itself can be an independent risk factor for any-cause mortality, 13 LA County performed an early evaluation of all-cause mortality among PEH from January through July 2020 and found that COVID-19 had become the fifth-leading cause of death among PEH. 14 Since that report, LA County experienced a rapid surge in COVID-19 cases among all population sectors. To further investigate the impact of COVID-19 on PEH in LA County, we calculated COVID-19 mortality rates among PEH and compared them with the general population in LA County from March 1, 2020, through February 28, 2021. To our knowledge, this study is the first to evaluate COVID-19 mortality rates and trends in a large jurisdiction that also has a large PEH population, separately adjusting for age, race, and sex/gender, while presenting concurrent case fatality rates for comparison of COVID-19 mortality among PEH versus the general LA County population.
Methods
Mandatory reports of COVID-19 diagnoses were submitted to the Los Angeles County Department of Public Health (LACDPH) through medical provider case report forms and directly by laboratories performing COVID-19 testing. LACDPH routinely investigated people diagnosed with COVID-19 for indications of homelessness to surveil disease incidence among sheltered and unsheltered PEH. PEH included those who sleep in sheltered settings, such as emergency shelters or transitional housing, and in unsheltered settings, such as on the street, in tents and in vehicles, or in groups at encampments, according to the US Department of Housing and Urban Development (HUD) definitions for homelessness. 15 We assessed housing status as of the time of COVID-19 diagnosis or symptom onset through case interviews, database matches against the Homeless Management Information System, medical provider reports, medical examiner reports, shelter operator or social worker reports, and family member interviews when the patient was not available.
LACDPH ascertained COVID-19–related deaths from medical provider reports, death certificates, reports from the medical examiner’s office, and vital records death matches against COVID-19 case data in LACDPH. Confirmed COVID-19–related deaths included those resulting from nontraumatic, nonaccidental causes within 60 days of the first confirmed positive SARS-CoV-2 molecular test result or up to 90 days if intubated, or if COVID-19 was listed as a cause on the death certificate.16-19 We categorized COVID-19–related deaths as PEH when we determined patients to have been experiencing homelessness at the time of COVID-19 diagnosis.
We examined separate age, race, and sex/gender-specific COVID-19 mortality rates per 100 000 population and standardized mortality ratios (SMRs) with 95% CIs for PEH and the general population in LA County from March 1, 2020, through February 28, 2021. We based PEH population estimates on the 2020 point-in-time count, the annual census of PEH, for the Los Angeles Continuum of Care (ie, an administrative designation by HUD to coordinate services for PEH in the area), in accordance with the methodology used for that count. 20 The estimated total population of PEH in the Los Angeles Continuum of Care in January 2020 was 63 706, of whom 56 215 were aged ≥18 years. Point-in-time count population denominators are available by age, race, and sex/gender. Population estimates stratified by both age and sex/gender or both age and race are not available. LA County 2018 population estimates were prepared for the LA County Internal Services Department and included all LA County except Long Beach and Pasadena (Hedderson Demographic Services), which have health departments that function independently of LACDPH. As such, data from Long Beach and Pasadena were excluded from this analysis. LACDPH routinely transfers case records to Long Beach and Pasadena for public health surveillance and disease intervention. We included in this analysis PEH case records with location information indicating residence in Glendale, which are investigated by LACDPH. We used distributions by age, race, and sex/gender categories for LA County COVID-19 deaths as the reference population for indirect standardization of the COVID-19 mortality rate among PEH. We assessed these indirectly standardized rates separately because of the lack of additional denominator stratifications available.
We routinely analyze COVID-19 case records among PEH for quality assurance, including identifying and removing duplicate cases for people who receive a positive test result more than once in 90 days.
We calculated age-specific case fatality rates by dividing the total number of deaths by the total number of cases in each age group for PEH and the general LA County population. We calculated case fatality rate ratios by dividing the PEH case fatality rate by the LA County case fatality rate for each age group.
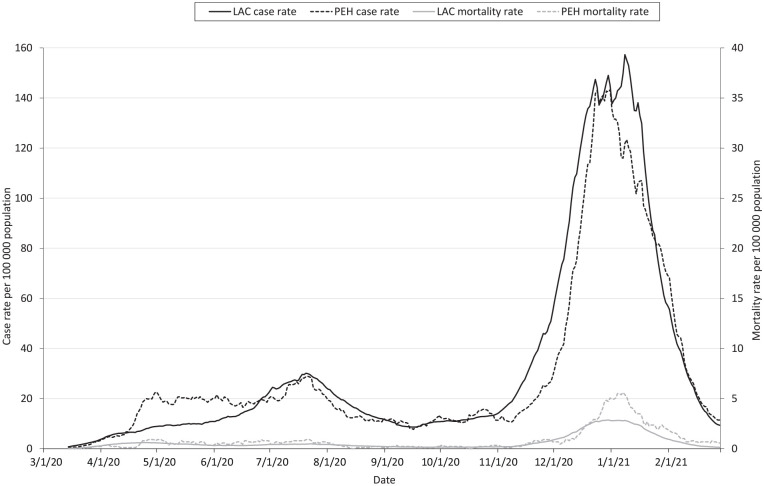
To examine trends in COVID-19 diagnoses and deaths over time, we calculated 14-day rolling averages of the crude COVID-19 case and mortality rates per 100 000 LA County residents and per 100 000 PEH. We plotted rolling 14-day average daily case and mortality rates from March 1, 2020, through February 28, 2021.
We conducted a sensitivity analysis to assess the impact of including people who may be bouncing between homes or “couch surfing” in our definition of experiencing homelessness because they are unable to be enumerated in the point-in-time count denominator.
To compare the impact of COVID-19 on PEH with other geographic communities in LA County, we reported COVID-19 mortality rates, crude and directly standardized by age to the US population, in a supplemental table. We included mortality rates for the 10 communities with the highest mortality rates as of March 9, 2021, with the indirectly standardized mortality rate calculated as previously described.
We computed 14-day average case and mortality rates using Microsoft Excel, and we used SAS version 9.4 (SAS Institute, Inc) to conduct all other analyses. LACDPH’s Institutional Review Board determined this activity to be a surveillance activity necessary for public health work and, therefore, did not require institutional review board review.
Results
From March 1, 2020, through February 28, 2021, a total of 1 142 307 cases of COVID-19 occurred among LA County residents reported to LACDPH, 6900 (0.6%) of whom were experiencing homelessness at the time of COVID-19 diagnosis (Table 1). During the same period, 21 929 people in LA County diagnosed with COVID-19 died, of whom 198 (0.9%) were PEH. Compared with COVID-19 deaths in the general population, PEH who died were more likely to be male (84.3% vs 58.7%) and Black or African American (24.2% vs 7.9%). Documented race or ethnicity was missing for 5.1% of PEH with COVID-19 who died versus 0.2% among deaths in the general population.
Table 1.
Characteristics of COVID-19 cases and deaths among people experiencing homelessness and the general population, Los Angeles County, March 2020–February 2021 a
| Characteristic |
People experiencing homelessness
|
Los Angeles County
|
||
|---|---|---|---|---|
| No. (%) of cases | No. (%) of deaths | No. (%) of cases | No. (%) of deaths | |
| Total, no. | 6900 | 198 | 1 142 307 | 21 929 |
| Age, y | ||||
| <18 | 406 (5.9) | 0 | 150 920 (13.2) | <5 b |
| 18-29 | 1114 (16.1) | 6 (3.0) | 269 656 (23.6) | 138 (0.6) |
| 30-39 | 1372 (19.9) | 10 (5.1) | 204 020 (17.9) | 391 (1.8) |
| 40-54 | 1974 (28.6) | 55 (27.8) | 261 483 (22.9) | 2043 (9.3) |
| 55-64 | 1379 (20.0) | 69 (34.8) | 135 423 (11.9) | 3507 (16.0) |
| ≥65 | 646 (9.4) | 56 (28.3) | 120 348 (10.5) | 15 846 (72.3) |
| Unknown | 9 (0.1) | <5 b | 457 (0) | <5 b |
| Race and ethnicity c | ||||
| American Indian/Alaska Native | 41 (0.6) | 0 | 1938 (0.2) | 42 (0.2) |
| Asian | 99 (1.4) | <5 b | 52 929 (4.6) | 2879 (13.1) |
| Black or African American | 1648 (23.9) | 48 (24.2) | 42 308 (3.7) | 1730 (7.9) |
| Hispanic/Latino | 3060 (44.3) | 96 (48.5) | 583 667 (51.1) | 11 694 (53.3) |
| Native Hawaiian or Other Pacific Islander | 25 (0.4) | <5 b | 4101 (0.4) | 92 (0.4) |
| White | 1076 (15.6) | 38 (19.2) | 119 986 (10.5) | 5099 (23.3) |
| Other | 23 (0.3) | 0 | 101 745 (8.9) | 345 (1.6) |
| Missing or unknown | 928 (13.4) | 10 (5.1) | 235 633 (20.6) | 48 (0.2) |
| Sex/gender | ||||
| Female | 2243 (32.5) | 31 (15.7) | 579 367 (50.7) | 9054 (41.3) |
| Male | 4583 (66.4) | 167 (84.3) | 541 314 (47.4) | 12 871 (58.7) |
| Transgender female/trans woman | 27 (0.4) | 0 | 125 (0) | <5 b |
| Transgender male/trans man | <5 b | 0 | 129 (0) | <5 b |
| Gender nonbinary, gender nonconforming | <5 b | 0 | 7 (0) | 0 |
| Unknown | 41 (0.6) | 0 | 21 365 (1.9) | <5 b |
Data source: Mandatory reports of COVID-19 cases and deaths to the Los Angeles County Department of Public Health.
Cells with counts of <5 people are suppressed to protect patient identity.
Non-Hispanic ethnicity for all race categories except Hispanic/Latino. Missing or unknown race did not have data for race or ethnicity.
The average daily case and crude mortality rates differed among PEH and the general LA County population during the study period. In April and May 2020, the 14-day rolling average daily case rates of COVID-19 per 100 000 population were higher among PEH, averaging 16.9 cases per day, than in the general LA County population, averaging 8.8 cases per day. During the same period, the 14-day average crude mortality rates per 100 000 population were similar for PEH and the LA County population, both averaging 0.5 deaths per 100 000 population per day. The 14-day rolling average case and crude mortality rates remained similar from June through October 2020. In November 2020, as COVID-19 diagnoses began to surge in LA County, the 14-day rolling average daily case rate per 100 000 population for LA County surpassed the PEH case rate as both increased, but mortality rates were similar between PEH and the general LA County population. During the 2020-2021 winter surge in COVID-19 diagnoses in LA County, PEH mortality rates per 100 000 population surpassed mortality rates for the general population, even as case rates were the same or lower than in the general population. The 14-day average daily mortality rate per 100 000 population peaked at 5.5 deaths among PEH compared with 2.8 deaths in the general LA County population (Figure).
Figure.
COVID-19 case and mortality rates per 100 000 population for the general population in Los Angeles County (LAC) and people experiencing homelessness (PEH) in Los Angeles County, March 2020–February 2021. Rates are 14-day rolling averages of unadjusted daily case and mortality rates per 100 000 population. The Los Angeles County population denominator was estimated from a 2018 Population Estimates and Projections System provided by Hedderson Demographic Services for Los Angeles County; excludes Pasadena and Long Beach. PEH population denominator estimated from 2020 point-in-time count of PEH 20 ; excludes Pasadena, Long Beach, and Glendale. A different scale is used for case and mortality rates.
COVID-19 mortality rates differed between PEH and the general LA County population by age. Among adults aged ≥18 years, crude mortality rates per 100 000 population among PEH were 20% higher than among the LA County population (348.7 vs 287.6; Table 2). After adjusting for age, the mortality rate among PEH was 570.7 per 100 000 population, and the SMR of 2.0 (95% CI, 1.7-2.2) indicated that PEH had nearly 2 times the risk of dying from COVID-19 as did people in the general LA County population. Age-specific mortality rate ratios showed that the risk of dying from COVID-19 was higher for PEH in every age group than for the LA County population in each corresponding age group. Mortality rates were heterogeneous across age groups. PEH aged 18-29 years were at the highest relative risk of mortality, with nearly 8 times the mortality rate as that experienced by their peers in the general LA County population (7.9; 95% CI, 1.6-14.1). Those aged 30-39 and 20-54 years had 2.9 (95% CI, 1.1-4.7) and 2.8 (95% CI, 2.1-3.6) times the risk of mortality from COVID-19 as their peers in the general population, respectively. The relative risk decreased with increasing age, with those aged 55-64 years having 2.1 (95% CI, 1.6-2.6) times the risk of the general population; the point estimate for those aged ≥65 years was not significant (1.3; 95% CI, 1.0-1.6).
Table 2.
COVID-19 mortality rates and standardized mortality rate ratios for the general population and people experiencing homelessness (PEH), by age, race and ethnicity, and sex, Los Angeles County, March 2020–February 2021 a
| Characteristic |
Los Angeles County
|
PEH
|
||||||
|---|---|---|---|---|---|---|---|---|
| No. of COVID-19 deaths | Population b | Crude mortality rate | No. of deaths | Population c | Crude mortality rate | Standardized mortality ratio (95% CI) | Adjusted mortality rate per 100 000 population (95% CI) d | |
| Total | 21 729 | 7 554 336 | 287.6 | 196 | 56 215 | 348.7 | ||
| Age, y | ||||||||
| 18-29 | 132 | 1 703 423 | 7.8 | 6 | 9780 | 61.4 | 7.9 (1.6-14.1) e | — |
| 30-39 | 381 | 1 397 120 | 27.5 | 10 | 12 418 | 80.5 | 2.9 (1.1-4.7) e | — |
| 40-54 | 1988 | 1 982 479 | 101.3 | 55 | 19 121 | 287.6 | 2.8 (2.1-3.6) e | — |
| 55-64 | 3438 | 1 202 639 | 288.6 | 69 | 11 457 | 602.3 | 2.1 (1.6-2.6) e | — |
| ≥65 | 15 790 | 1 268 675 | 1248.0 | 56 | 3439 | 1628.4 | 1.3 (1.0-1.6) e | — |
| Total by age f | 21 729 | 7 554 336 | 287.6 | 196 | 56 215 | 348.7 | 2.0 (1.7-2.2) e | 570.7 (490.8-650.6) |
| Race and ethnicity | ||||||||
| Asian | 2875 | 1 395 605 | 206.0 | 4 | 774 | 516.8 | 2.5 (0.1-5.0) | — |
| Black or African American | 1682 | 789 202 | 213.1 | 48 | 21 059 | 223.2 | 1.0 (0.8-1.3) | — |
| Hispanic/Latino | 11 598 | 4 758 809 | 243.7 | 96 | 23 005 | 417.3 | 1.7 (1.4-2.1) e | — |
| Native Hawaiian or Other Pacific Islander | 90 | 19 152 | 469.9 | 2 | 205 | 975.6 | 2.1 (0-5.0) | — |
| White | 5061 | 2 666 559 | 234.5 | 38 | 16 208 | 234.5 | 1.2 (0.8-1.6) | — |
| Total by race and ethnicity g | 21 306 | 7 229 327 | 294.7 | 188 | 45 043 | 417.4 | 1.4 (1.2-1.6) e | 307.6 (263.6-351.6) |
| Sex | ||||||||
| Female | 9023 | 4 890 980 | 184.5 | 31 | 20 671 | 150.0 | 0.8 (0.6-1.1) | — |
| Male | 12 704 | 4 760 352 | 266.9 | 167 | 42 797 | 390.2 | 1.5 (1.2-1.7) e | — |
| Total by sex/gender h | 21 727 | 9 651 332 | 225.1 | 198 | 63 468 | 312.0 | 1.3 (1.1-1.5) e | 292.6 (251.8-333.3) |
Data source: Mandatory reports of COVID-19 cases and deaths to the Los Angeles County Department of Public Health.
Los Angeles County population by age from 2018 Population Estimates and Projections System provided by Hedderson Demographic Services for Los Angeles County, excluding Pasadena and Long Beach.
PEH population estimates from Los Angeles County point-in-time count of people experiencing homelessness, 20 excluding Pasadena, Long Beach, and Glendale.
PEH adjusted mortality rate and standardized mortality ratio calculated using Los Angeles County population and rates to estimate expected counts.
95% CIs that do not include 1.0 are significant.
Excludes people aged <18 years.
Excludes people with unknown and other race and ethnicity.
Excludes people with unknown sex/gender.
Differences in race-specific SMRs were not significant in any race group between PEH and the general LA County population except among Hispanic/Latino PEH, who had 1.7 (95% CI, 1.4-2.1) times the risk of mortality from COVID-19 (Table 2). The race-adjusted SMR showed that after accounting for race, PEH still had 1.4 (95% CI, 1.2-1.6) times the risk of death compared with the general LA County population.
The sex/gender-specific SMR indicated that males experiencing homelessness had 1.5 times the risk of dying from COVID-19 compared with the general LA County population, but the difference in risk of dying was not significant between females experiencing homelessness and females in the general LA County population (SMR = 0.81; 95% CI, 0.56-1.1; Table 2).
COVID-19 case fatality rates were also higher among PEH than in the general population (Table 3). The difference was noted only for people aged 18-64 years when stratified by age. Among those aged 18-29 years, the case fatality rate among PEH was almost 11 times higher than in the general population (0.54% vs 0.05%).
Table 3.
Age-specific COVID-19 case fatality rates and rate ratios for people experiencing homelessness (PEH) and the general Los Angeles County (LA County) population, March 2020–February 2021 a
| Age, y |
No. of cases
|
No. of deaths
|
Case fatality rate
|
||||
|---|---|---|---|---|---|---|---|
| In LA County | Among PEH | In LA County | Among PEH | In LA County, % | Among PEH, % | Age-specific rate ratio (95% CI) b | |
| 18-29 | 269 656 | 1114 | 138 | 6 | 0.05 | 0.54 | 10.8 (4.9-24.8) b |
| 30-39 | 204 020 | 1372 | 391 | 10 | 0.19 | 0.73 | 3.8 (1.6-6.6) b |
| 40-54 | 261 483 | 1974 | 2043 | 55 | 0.78 | 2.79 | 3.6 (2.8-4.8) b |
| 55-64 | 135 423 | 1379 | 3507 | 69 | 2.59 | 5.00 | 2.0 (1.5-2.5) b |
| ≥65 | 120 348 | 646 | 15 846 | 56 | 13.17 | 8.67 | 0.7 (0.4-0.8) b |
| Total | 990 930 | 6485 | 21 925 | 196 | 2.20 | 3.00 | 1.3 (1.1-1.5) b |
Data source: Mandatory reports of COVID-19 cases and deaths to the Los Angeles County Department of Public Health.
95% CIs that do not include 1.0 are significant.
The sensitivity analysis found no significant change in mortality rate estimates when excluding 443 cases and 12 deaths among people identified as “couch surfing” by public health investigators.
Discussion
These findings indicate that in LA County, PEH had a higher risk of death from COVID-19 than their counterparts in the general population, particularly PEH aged 18-64 years. This finding is consistent with other early regional literature in the United States. 21 In LA County, the age-adjusted mortality rate of PEH was twice that of the general population. However, some age groups appeared to have even higher risk, up to almost 8 times that of the general population. In LA County, mortality rates also varied widely by geographic area and race and ethnicity, with multiple neighborhoods experiencing higher cumulative age-adjusted COVID-19 mortality rates than rates among PEH, nearly 600 deaths per 100 000 population in the hardest-hit communities (Supplemental Table). 22 The race-adjusted mortality rate for PEH was 1.4 times that of the general population, indicating that some, but not all, of the increased mortality among PEH may be accounted for by the same underlying factors that put Black and Hispanic/Latino LA County residents at higher risk of severe outcomes from COVID-19 than other racial and ethnic groups in LA County. Further analysis is needed to identify overlap in neighborhoods with higher numbers of PEH and neighborhoods that have high COVID-19 mortality and to investigate the impacts of systemic racism and the intersections of age, race, and sex/gender on COVID-19 mortality.
Although local public health response efforts have mitigated worse outcomes among PEH, sustained efforts continue to be needed, including vaccinations to prevent unnecessary deaths. While the earliest immunization efforts appropriately prioritized health care workers and people aged ≥65 years according to an increased risk of incidence and death from COVID-19, the higher age-standardized mortality rates among PEH support the need to prioritize younger age groups in populations experiencing homelessness. Given the disproportionate impact of COVID-19 on racial and ethnic minority groups, culturally appropriate education and outreach campaigns are needed in this population to increase testing acceptance, vaccination readiness, and equity in accessing these medical services.
Limitations
Our analysis had several limitations. First, our analysis was affected by the limitations of the point-in-time homeless count. Homelessness is a fluid state, with people entering periods of homelessness ranging from less than a month to many years. No data on person-years of homelessness are available to produce more accurate estimates of mortality rates than with the point-in-time count population denominator. The point-in-time count is limited by probable undercounting of PEH overall and especially those who are imminently homeless and, thus, meet the US Department of Housing and Urban Development category 2 definition of homelessness. 15 Population estimates stratified by both age and sex/gender or both age and race are not available from published point-in-time estimates, making it difficult to fully examine potentially intersecting risk factors. In addition, we were unable to exclude COVID-19 patients among PEH in Glendale, and the Glendale Continuum of Care population of 169 was not included in our population denominator because of a lack of sufficient data on age. 23
For the study period, the impact of COVID-19 on housing and homelessness is not yet fully known and could not be accounted for in our analysis. On one hand, the pandemic likely resulted in more PEH from job loss and financial strain. However, the eviction moratorium 24 that was enacted in March 2020 and continued through September 2021 in California may have prevented some people from entering homelessness. Further difficulty in ascertaining changes in the baseline population experiencing homelessness was exacerbated by the cancellation of the 2021 point-in-time count because of surging COVID-19 cases.
Although limitations of the point-in-time count as a population denominator remain, in collaboration with the University of Southern California, the Los Angeles Housing Services Authority has used methods to better enumerate PEH by surveying all census tracts, reducing barriers to participation for unsheltered PEH aged 18-24 years, and training a large number of volunteers and staff to conduct the point-in-time count and improve confidence in their estimate.20,25 Despite these known limitations, the point-in-time count serves as an appropriate denominator for disease and mortality rate analyses in PEH according to Mosites et al and as recommended by the National Healthcare for the Homeless Council.26,27 LACDPH’s ability to actively investigate housing status at the time of diagnosis strengthened the reliability of estimates using the point-in-time count. 26 In addition, using the point-in-time count facilitated comparisons with previous reports that have been published locally and in other jurisdictions. 25
Second, the LA County definition for COVID-19–related death, which includes deaths occurring within 60 days after the positive test date, may attribute some nontraumatic deaths to COVID-19 that may have been from other causes. High rates of mortality among PEH may result in more misclassified deaths using the 60-day definition than in the general population. In addition, deaths from long-term sequelae of COVID-19 that occur more than 60 days after diagnosis may be undercounted.
Third, case fatality ratios rely on detection of cases and, thus, may be biased upward to the extent that cases are not 100% detected, and only those who are most ill may be presenting for care and diagnosis. However, LACDPH established asymptomatic screening testing for both sheltered and unsheltered PEH, with 10% to 20% of residents at shelters and encampments offered testing weekly beginning in June 2020. 22 Systematic testing in this population helped minimize the potential bias from lack of case detection. 28 Although neither mortality rate nor case fatality rate is without its limitations, both measures similarly indicate that PEH experience increased the risk of death from COVID-19.
Fourth, this analysis did not account for comorbidities among PEH. Studies suggest that PEH have a higher prevalence of chronic health conditions and environmental risk factors than housed residents do, which increases their risk of death in general 2 and may also increase the impact of COVID-19 in this population. Comorbidity data were not systematically nor reliably available for either PEH or the general population to further enhance these analyses.
Conclusions
Our findings indicate that people in LA County experiencing homelessness are at increased risk of death from COVID-19, regardless of age, race, or sex/gender, even without ascertainment of underlying health conditions that put people at risk for severe outcomes from COVID-19. Sustained public health interventions such as screening and diagnostic testing, contact tracing, outbreak investigations and response, providing safe places to isolate and quarantine, as well as vaccination efforts should continue to prioritize PEH. As population-level COVID-19 mitigation efforts are rescinded with the evolving epidemiology of COVID-19, PEH-specific outcomes should continue to be evaluated.
Supplemental Material
Supplemental material, sj-docx-1-phr-10.1177_00333549221115658 for COVID-19 Mortality Rates in Los Angeles County Among People Experiencing Homelessness, March 2020–February 2021 by Alicia H. Chang, Jennifer J. Kwon, Chelsea L. Shover, Lisa Greenwell, Ayodele Gomih, Jerome Blake, Aubrey Del Rosario, Padma S. Jones, Rebecca Fisher, Sharon Balter and Hannah K. Brosnan in Public Health Reports
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Public health surveillance and analysis for this article were completed as part of 2019-2024 ELC Cooperative Agreement activities under Centers for Disease Control and Prevention grant no. 6NU50CK000498-01-09.
ORCID iD: Hannah K. Brosnan, MPH  https://orcid.org/0000-0002-2234-2533
https://orcid.org/0000-0002-2234-2533
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Los Angeles Homeless Services Authority. 2020 Greater Los Angeles homeless count—data summary. Total point-in-time homeless population by geographic areas. 2020. Accessed October 24, 2021. https://www.lahsa.org/documents?id=4692-2020-greater-los-angeles-homeless-count-total-point-in-time-homeless-population-by-geographic-areas
- 2. Lebrun-Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 Patient Survey. Health Serv Res. 2013;48(3):992-1017. doi: 10.1111/1475-6773.12009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nusselder WJ, Slockers MT, Krol L, Slockers CT, Looman CWN, van Beeck EF. Mortality and life expectancy in homeless men and women in Rotterdam: 2001-2010. PLoS One. 2013;8(10):e73979. doi: 10.1371/journal.pone.0073979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O’Connell JJ. Premature Mortality in Homeless Populations: A Review of the Literature. National Health Care for the Homeless Council; 2005. [Google Scholar]
- 5. Romaszko J, Cymes I, Dragańska E, Kuchta R, Glińska-Lewczuk K. Mortality among the homeless: causes and meteorological relationships. PLoS One. 2017;12(12):e0189938. doi: 10.1371/journal.pone.0189938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vuillermoz C, Auoba A, Grout L, et al. Mortality among homeless people in France, 2008-10. Eur J Public Health. 2016;26(6):1028-1033. doi: 10.1093/eurpub/ckw083 [DOI] [PubMed] [Google Scholar]
- 7. Mosites E, Parker EM, Clarke KEN, et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters—four U.S. cities, March 27–April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):521-522. doi: 10.1101/2020.04.12.20059618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020;323(21):2191-2192. doi: 10.1001/jama.2020.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tobolowsky FA, Gonzales E, Self JL, et al. COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):523-526. doi: 10.15585/mmwr.mm6917e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yoon JC, Montgomery MP, Buff AM, et al. Coronavirus disease 2019 (COVID-19) prevalences among people experiencing homelessness and homelessness service staff during early community transmission in Atlanta, Georgia, April–May 2020. Clin Infect Dis. 2021;73(9):e2978-e2984. doi: 10.1093/cid/ciaa1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Leifheit KM, Chaisson LH, Medina JA, Wahbi RN, Shover CL. Elevated mortality among people experiencing homelessness with COVID-19. Open Forum Infect Dis. 2021;8(7):ofab301. doi: 10.1093/ofid/ofab301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pan D, Sze S, Minhas JS, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23:100404. doi: 10.1016/j.eclinm.2020.100404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol. 2009;38(3):877-883. doi: 10.1093/ije/dyp160 [DOI] [PubMed] [Google Scholar]
- 14. Los Angeles County Department of Public Health. Recent Trends in Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County. 2021. Accessed May 23, 2021. http://www.publichealth.lacounty.gov/chie/reports/HomelessMortality2020_CHIEBrief_Final.pdf
- 15. US Department of Housing and Urban Development. Criteria for defining homelessness and recordkeeping requirements. Published January 2012. Accessed May 23, 2021. https://files.hudexchange.info/resources/documents/HomelessDefinition_RecordkeepingRequirementsandCriteria.pdf
- 16. Traub E, Amoon AT, Rollin-Alamillo L, et al. Excess mortality associated with the COVID-19 pandemic—Los Angeles County, March–September 2020. J Public Health Manag Pract. 2021;27(3):233-239. doi: 10.1097/PHH.0000000000001344 [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization. International Guidelines for Certification and Classification (Coding) of COVID-19 as Cause of Death. 2020. Accessed October 29, 2021. https://www.who.int/classifications/icd/Guidelines_Cause_of_Death_COVID-19.pdf
- 18. Griffin JB, Haddix M, Danza P, et al. SARS-CoV-2 infections and hospitalizations among persons aged ≥16 years, by vaccination status—Los Angeles County, California, May 1–July 25, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(34):1170-1176. doi: 10.15585/mmwr.mm7034e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scobie HM, Johnson AG, Suthar AB, et al. Monitoring incidence of COVID-19 cases, hospitalizations, and deaths, by vaccination status—13 U.S. jurisdictions, April 4–July 17, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(37):1284-1290. doi: 10.15585/mmwr.mm7037e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Henwood BF, Kaileh L, Wilson N, et al. Los Angeles Continuum of Care Homeless Count. University of Southern California; 2020. Accessed October 24, 2021. https://www.lahsa.org/documents?id=4658-usc-2020-homeless-count-methodology-report [Google Scholar]
- 21. Richard L, Booth R, Rayner J, Clemens KK, Forchuk C, Shariff SZ. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: a retrospective cohort study. CMAJ Open. 2021;9(1):E1-E9. doi: 10.9778/cmajo.20200287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. LA County Department of Public Health. LA County COVID-19 surveillance dashboard: map of adjusted rates for deaths by city/community. Published 2021. Accessed May 23, 2021. http://dashboard.publichealth.lacounty.gov/covid19_surveillance_dashboard
- 23. City of Glendale. 2020 Homeless Count Report. Published 2020. Accessed October 29, 2021. https://www.glendaleca.gov/home/showdocument?id=57789#:~:text=
- 24. Executive Department State of California. Executive order N-28-20. 2020. Accessed March 23, 2021. https://www.gov.ca.gov/wp-content/uploads/2020/03/3.16.20-Executive-Order.pdf
- 25. Nicholas W, Greenwell L, Henwood BF, Simon P. Using point-in-time homeless counts to monitor mortality trends among people experiencing homelessness in Los Angeles County, 2015-2019. Am J Public Health. 2021;111(12):2212-2222. doi: 10.2105/AJPH.2021.306502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mosites E, Bamrah Morris S, Self J, Butler JC. Data sources that enumerate people experiencing homelessness in the United States: opportunities and challenges for epidemiologic research. Am J Epidemiol. 2020;190(11):2432-2436. doi: 10.1093/aje/kwab051 [DOI] [PubMed] [Google Scholar]
- 27. National Healthcare for the Homeless Council. Homeless mortality. Accessed October 29, 2021. https://nhchc.org/homeless-mortality
- 28. Los Angeles County Department of Public Health. Novel Coronavirus (COVID-19) Los Angeles County Department of Public Health Guidance on COVID-19 Testing Priorities and Recommendations for People Experiencing Homelessness. Accessed May 23, 2021. http://www.publichealth.lacounty.gov/media/Coronavirus/docs/homelessness/GuidancePEHTestingPriorities.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-phr-10.1177_00333549221115658 for COVID-19 Mortality Rates in Los Angeles County Among People Experiencing Homelessness, March 2020–February 2021 by Alicia H. Chang, Jennifer J. Kwon, Chelsea L. Shover, Lisa Greenwell, Ayodele Gomih, Jerome Blake, Aubrey Del Rosario, Padma S. Jones, Rebecca Fisher, Sharon Balter and Hannah K. Brosnan in Public Health Reports