Abstract
Background: During the second wave of COVID-19 cases within Scotland, local evidence suggested that a large number of interhospital transfers occurred due to both physical capacity and staff shortages. Although there are inherent risks with transferring critically ill patients between hospitals, there are signals in the literature that mortality is not affected in COVID-19 patients when transferred between intensive care units. With a lack of evidence in the Scottish population, and as the greatest source of capacity transfers in our critical care network at that time, we sought to determine whether these transfers impacted on survival to hospital discharge.Methods: We conducted a retrospective cohort study of all patients admitted to our unit between the 1st October 2020 and the 31st March 2021 with a primary diagnosis of COVID-19 pneumonia. Patients were grouped according to whether they underwent an interhospital capacity transfer or not, either for unit shortage of beds or unit shortage of staff. The primary outcome measure was survival to ultimate hospital discharge, and secondary outcomes included total ventilator days and total intensive care unit length of stay. Baseline characteristic data were also collected for all patients. Survival data were entered into a backward stepwise logistic regression analysis that included transfer status, and coefficients transformed into odds ratios and 95% confidence intervals.Results: A total of 108 patients were included. Of these, 30 were transferred to another intensive care unit due to capacity issues at the base hospital. From the baseline characteristic data, age was significantly higher in those transferred out, while other characteristics were similar. Unadjusted mortality rates were 30.8% for those not transferred, and 40% for those transferred out. However, when entered into a logistic regression analysis to attempt to control for confounders in the baseline characteristics, being transferred had an odds ratio of 1.14 (95% confidence interval 0.43–3.1) for survival to hospital discharge. Total ventilator days and total ICU length of stay were both higher in the transferred patients.Conclusion: This unique study of COVID-19 patients transferred from a Scottish district general hospital did not show an association between transfer status and survival to hospital discharge. However, the study was likely underpowered to detect small differences. As the situation continues to evolve, a prospective regional multi-centre study may help to provide more robust findings.
Keywords: COVID-19, interhospital, transfer, intensive care, capacity
Introduction
COVID-19 disease, caused by the SARS-CoV-2 virus, has been the focus of a worldwide pandemic which has involved the UK from early 2020. In its severe form, this disease requires supplemental oxygen and may necessitate invasive mechanical ventilation within an intensive care unit. Thus, an additional stress has been placed on intensive care units, including within Scotland. Reporting from the Scottish Intensive Care Society Audit Group (SICSAG) states that from the 1st of August 2020 to the 9th of May 2021, during the period defined as the ‘second wave’ of infections, there were 1326 patients admitted to Scottish intensive care units with laboratory confirmed COVID-19. 1 For comparison, there were 11,107 total admissions to intensive care and combined units in Scotland in the year 2020 (excluding specialist units). 2 In the West of Scotland Critical Care Network (WoSCCN) a large number of interhospital transfers occurred in this time frame to cope with limited capacity. From the 1st of October 2020 to the 31st of March 2021, there were 124 clinical and capacity transfers within the WoSCCN, excluding those to the tertiary neurosurgical ICU.
Locally, a solution was necessary to deal with the large surge in intensive care occupancy. At times, the unit was running at up to 250% of baseline capacity with extra ICU beds created within the theatre recovery area and in operating theatres. Initially, staff were redeployed from the physiotherapy and theatre nursing teams. However, as the pandemic continued, staffing shortages led to increasing difficulty in nursing level 3 patients optimally at 1:1 as set out in the Faculty of Intensive Care Medicine (FICM) Guidelines for the Provision of Intensive Care Services (GPICS). 3 Ratios of 1:2 were not infrequent and occasionally 1:3 was necessary. In addition, GPICS includes a supernumerary senior registered nurse to act as a clinical coordinator, as well as an additional supernumerary senior registered nurse in units with greater than 10 patients. 3 This standard was simply not possible at the times of greatest stress, which is a matter of great clinical concern. Despite adequate staffing, it is also important to consider the implications of compromising staff skill mix, oversight of the team, and access to interventions. For example, utilising physiotherapists to mitigate nursing shortages may dilute an already junior nursing team, as well as limiting availability of physiotherapy to the patient cohort. There is also an unmeasured effect from staff wellbeing which may be negatively affected by increased workload.
Supporting the FICM standards, there is evidence from both before and during the pandemic that increased patient load in ICU is associated with increased mortality,4,5 and evidence from an Australian study that minimum nurse-to-patient ratio mandates can decrease mortality and help to reduce length of stay. 6 Therefore, in the second wave staffing ratios became the main driver for transferring patients across the critical care network.
The Faculty of Intensive Care Medicine recommends that acute hospital sites have arrangements in place to ensure that capacity transfers occur only as a last resort. 7 There are multiple risks inherent with critical care transfers including technical (clinical events relating to the patient or equipment used), non-technical (for example issues with communication, an isolated team, and working in a cramped environment), and organisational risks (for example increasing load on remaining staff, ensuring best practice during transfer, and delays in admission or transfer). 8 In conjunction with a critically ill patient, these risks have the potential to increase patient morbidity and mortality.
There has been early evidence published to suggest that interhospital transfers do not increase mortality in COVID-19 patients, although existing data on interhospital transfers yield an adverse event rate between 1.7% and 34% with a variety of definitions.9–14 There are signals that specialised teams may improve safety and outcomes during transfers,9,15,16 while checklists or protocolised tools can reduce antibiotic changes and emergency central venous line insertions on arrival. 17 A multicentre cohort study from France during the first wave reported a 10% versus 12% intensive care unit mortality rate for transferred and non-transferred patients respectively. 18 Another study of a national French database suggests that mortality in transferred patients is lower, albeit with no standardisation of patient baseline characteristics. 19 When corrected for comorbidities and disease severity, a cross-sectional study of all public and private hospitals in France still found lower intensive care unit mortality in patients that underwent inter-regional transfer. 20 Aside from the French data, there is early evidence from a retrospective review in the United States that critical care transport was associated with few adverse events and similar mortality to patients in other COVID-19 studies. 21
There is still a lack of apparent evidence for the Scottish population, and so we sought to determine whether this impacted upon the survival of our patients. As the greatest source of capacity transfers within our critical care network during the second wave, our district general hospital was uniquely placed to conduct a retrospective cohort study of the survival to hospital discharge of patients transferred, versus those that remained in our intensive care unit.
Methods
The study dataset was already available as part of the SICSAG database maintained on the WardWatcher program (Critical Care Audit Ltd.). Patients admitted to our unit between the 1st of October 2020 and the 31st March 2021 with a primary diagnosis of COVID-19 pneumonia were included in the study. Patients were grouped according to whether they underwent a capacity transfer, defined as interhospital transfer due to unit shortage of beds or unit shortage of staff. Transfers for other reasons were excluded. Readmission episodes were excluded from the non-transfer group to avoid duplicates but were included in the transfer group with the intention of capturing all transfer instances. It was then necessary to remove one duplicate patient from the non-transfer group as the individual had been transferred after readmission.
In our cohort, transfer practice was standardised as much as feasible. There is a standard operating procedure including checklists pre-, during, and post-transfer. All transfers are conducted by a member of medical staff with FICM transfer competencies and a registered nurse with critical care competencies. Transfer documentation is standardised across the health board and includes clinical details, patient observations, timings, governance checks, and any critical incidents that occurred. Data from the transfer documents are collated by the transfer clinical lead. A transfer trolley with standard set-up and regular checks is utilised for all transfers.
The following steps denote the process used for selecting a destination unit and patient for transfer: (1) capacity issue identified; (2) capacity discussed between the intensive care consultant and senior charge nurse; (3) WardWatcher used to identify units within the network with potentially less pressure; (4) consultant to consultant discussion with each identified unit regarding available beds, staffing and anticipated admissions; (5) judgement made in conjunction with receiving units about most appropriate destination; (6) the patient judged by the intensive care consultant to have the lowest likelihood of adverse events in transfer selected; (7) transfer discussed with the selected patient’s next of kin and agreed.
The primary outcome measure was survival to ultimate hospital discharge. Secondary outcomes included total ventilator days and total intensive care unit length of stay. Information on critical incidents was sought from a database collated by the transfer clinical lead. Baseline characteristic data were also collected. Socioeconomic status quintiles were measured using the Scottish Index of Multiple Deprivation (SIMD) based on patient home postcode. Obesity was included as a comorbidity, defined as a body mass index greater than 30 kg m−2. Frailty was measured using the Rockwood Clinical Frailty Scale (CFS), with a score of less than 4 being non-frail, a score of 4 being vulnerable, and a score of greater than 4 being frail. APACHE II scores – which predict mortality using age, underlying health, and physiological variables from the initial 24 h ICU period – were included.
Baseline characteristics were analysed for significant differences between groups. Categorical variables were compared using Fisher’s exact test. Continuous variables were first tested for normal distribution using the Shapiro-Wilk test, and then compared using the Mann-Whitney test for variables that were not normally distributed, and Welch’s unpaired t-test for normally distributed variables.
The primary outcome measure of survival to ultimate hospital discharge was entered into a backward stepwise logistic regression analysis, including transfer status as a minimum variable. All other measured baseline characteristics were input as possible variables. The aim of performing this analysis was to control for confounders in the baseline data, while a stepwise reduction minimised the number of independent variables given the small sample size. Coefficients from the regression analysis were then transformed into odds ratios and 95% confidence intervals.
All statistical analyses were performed with R version 4.1.0 (R Foundation for Statistical Computing).
Results
A total of 108 patients were included in the study. Of these, 30 (28%) were transferred to another intensive care unit due to capacity issues. There were 7 receiving units. Table 1 demonstrates the baseline characteristics of patients during the first 24 h of their intensive care stay. Age was significantly higher in those transferred out, with a median of 63 years, compared with 57 in the non-transfers group. The non-transfers group included patients spanning all frailty categories and the transfers group did not, although the numbers were small in the remaining categories. The non-transfers group included a patient with no initial organ support as well as a patient with 3 organ systems supported, while the majority had between 1 and 2 organ systems supported. This was similar in the transfers group where the patients were split evenly in these categories. The groups were similar in all other characteristics.
Table 1.
Baseline characteristics of patients included in the study.
| Characteristic | Non-transfers (n = 78) | Transfers (n = 30) | p value | |
|---|---|---|---|---|
| Age (years) | Median (IQR) | 57 (48.5,64) | 63 (59.25,69.75) | .0079 |
| Sex | Female | 33 (42.3%) | 11 (36.7%) | .67 |
| Male | 45 (57.7%) | 19 (63.3%) | ||
| Socioeconomic status quintile (SIMD) | 1 – Most deprived | 28 (35.9%) | 12 (40.0%) | .13 |
| 2 | 23 (29.5%) | 4 (13.3%) | ||
| 3 | 13 (16.7%) | 3 (10.0%) | ||
| 4 | 11 (14.1%) | 7 (23.3%) | ||
| 5 – Least deprived | 3 (3.8%) | 4 (13.3%) | ||
| Ethnicity | White | 76 (97.4%) | 28 (93.3%) | .31 |
| Asian | 2 (2.6%) | 2 (6.7%) | ||
| Comorbidities | Cardiovascular disease | 29 (22.8%) | 16 (31.4%) | .14 |
| Respiratory disease | 24 (18.9%) | 9 (17.6%) | 1 | |
| Diabetes mellitus | 16 (12.6%) | 8 (15.7%) | .61 | |
| Cancer | 0 (0.0%) | 0 (0.0%) | 1 | |
| Other (including obesity) | 58 (45.7%) | 18 (35.3%) | .16 | |
| Clinical frailty score (CFS) | Non-frail | 63 (80.8%) | 27 (90.0%) | .45 |
| Vulnerable | 7 (9.0%) | 3 (10.0%) | ||
| Frail | 6 (7.7%) | 0 (0.0%) | ||
| Not known | 2 (2.6%) | 0 (0.0%) | ||
| APACHE II score | Median (IQR) | 13 (10,16) | 14 (11,17) | .15 |
| PF ratio (kPa) | Median (IQR) | 13.5 (10.625,20.3) | 13 (11,16.9) | .59 |
| Time from hospital admission to ICU admission (days) | Median (IQR) | 1 (0,2) | 0 (0,1.75) | .68 |
| Number of organ systems supported on ICU admission | 0 | 1 (1.3%) | 0 (0.0%) | .29 |
| 1 | 51 (65.4%) | 15 (50.0%) | ||
| 2 | 25 (32.1%) | 15 (50.0%) | ||
| 3 | 1 (1.23%) | 0 (0.0%) |
IQR: interquartile range; PF ratio: PaO2/FiO2 ratio; ICU: intensive care unit.
For the 30 patients that were transferred out, time from intensive care admission to transfer had a median value of 6 days (interquartile range 3–10). For 4 of the patients, time from admission to transfer was just 1 day, while the highest value was 26 days for one patient. These patients were selected for transfer by the duty ICU consultant on the day of transfer, using clinical judgement to select the most stable and appropriate patient. No critical incidents were documented or reported to the transfer clinical lead.
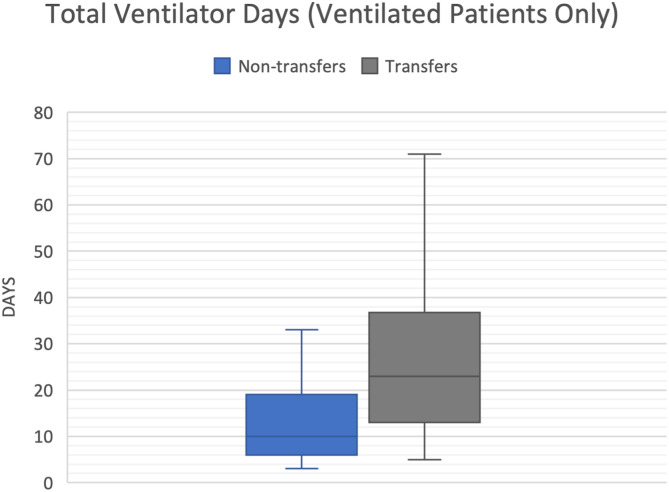
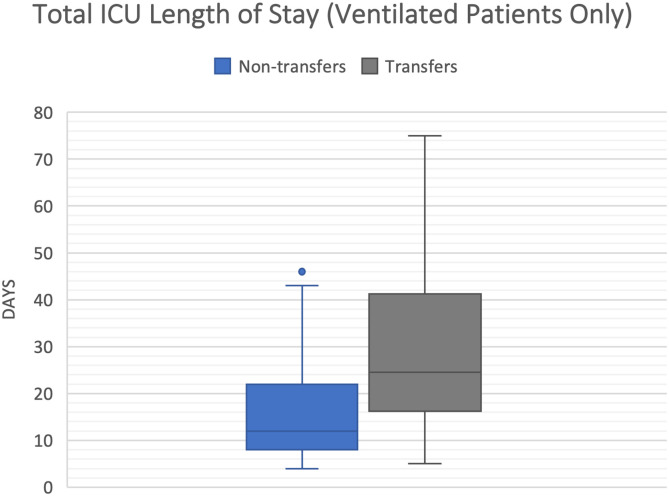
The primary outcome of survival to ultimate hospital discharge is shown in Table 2. Unadjusted mortality rates were 30.8% for those not transferred, and 40.0% for those transferred out. There was a large difference in median and interquartile ranges for both total ventilator days, and total intensive care unit length of stay. This persisted when only considering invasively ventilated patients. As seen in Figures 1 and 2, the lower end of the ranges for the transfers group were comparable with the non-transfers group, however the upper ends were much higher.
Table 2.
Patient outcomes at ultimate hospital discharge.
| Characteristic | Non-transfers (n = 78) | Transfers (n = 30) | |
|---|---|---|---|
| Ultimate hospital outcome | Lived | 54 (69%) | 18 (60%) |
| Died | 24 (31%) | 12 (40%) | |
| Total ventilator days | Median (IQR) | 4.5 (0,13) | 23 (13,37) |
| Ventilated patients only | Median (IQR) | 10 (6,19) | 23 (13,37) |
| Total ICU length of stay (Calendar days) | Median (IQR) | 7.5 (3.3,15) | 25 (16,41) |
| Ventilated patients only | Median (IQR) | 12 (8,22) | 25 (16,41) |
Figure 1.
Box and whisker plot of total ventilator days in the ventilated patients only.
Figure 2.
Box and whisker plot of total ICU length of stay.
Table 3 shows the results of the backward stepwise logistic regression analysis performed to predict survival to ultimate hospital discharge. Transfer status, age, ethnicity, and baseline APACHE II score were included as variables, while all other baseline characteristics were excluded from the model. 72 out of 78 non-transferred patients and 29 out of 30 transferred patients had complete data. Of the variables included, only age had a significant effect with a confidence interval that avoided reaching or crossing 1, although it approached this point. Therefore, the evidence for its negative effect on mortality is weak.
Table 3.
Results of logistic regression analysis to predict survival to hospital discharge.
| Odds ratio | 95% Confidence interval | p value | |
|---|---|---|---|
| Transferred out | 1.14 | 0.43–3.1 | .80 |
| Age | 0.95 | 0.90–0.99 | .036 |
| Ethnicity (White) | 9.10 | 1.0–200 | .071 |
| Baseline APACHE II score | 0.92 | 0.83–1.0 | .049 |
Discussion
This study was unique as it adds preliminary regional data on the mortality risk associated with transferring COVID-19 patients for capacity reasons in a Scottish district general hospital population. Existing literature at the time of writing on transfer of critically ill adult COVID-19 patients includes data on safety,21,22 narrative experience, 23 and mortality of transferred patients in a French population.18–20
Allen et al. described the interhospital transport of 20 critically ill patients in Washington DC, 19 of whom were intubated. 22 One patient in their group was unintentionally extubated during movement from transfer trolley to bed. They concluded that interfacility transfer of severely ill COVID-19 patients was safe and feasible. A retrospective review of transfers in Boston agreed adverse events were infrequent and transferring these patients did not appear to affect mortality when compared with other studies of COVID-19 patients. 21 Mazzoli et al. described the organisation, logistics, equipment/vehicles, decontamination plan, and activity/complications from the transfer of 159 critically ill COVID-19 patients in Italy between March and April 2020. 23 There were no fatal events and 2 non-fatal events during the series of transfers – one ventilator failure, and one supraventricular tachycardia. Almost a quarter of cases experienced oxygen desaturation below 90% that was not correctable during transfer and a third needed hemodynamic support. In France, retrospective analysis has been conducted regarding ventilated COVID-19 patients that underwent interhospital transfer. 18 In the 133 patients studied, there was no significant difference in mortality and length of stay within intensive care between the transferred patients and non-transferred patients, however there was a significant increase in median length of mechanical ventilation in the transferred group. In contrast, cross-sectional study from a French hospital database demonstrated lower mortality with inter-regional transfer, with an adjusted odds ratio of 0.26 when corrected for comorbidity and disease severity on multivariate analysis. 20
As mentioned previously, a surge in bed occupancy and accompanying staffing shortages played a significant role in the requirement to transfer patients. Transfers were by necessity ad hoc. In most cases, staff from the base hospital had to be released to accompany patients, which may have had a detrimental effect on the patients that remained. Equally, since nursing ratios were not measured in the base or receiving units, it is possible that workload in the receiving unit rose unexpectedly in the days after transfer and affected patient outcome. This data on staffing is not available retrospectively, however a tool has now been introduced within NHS Scotland to monitor staffing levels.
During the study period, there were no national guidelines on decision making for capacity transfers. There is a significant ethical consideration when selecting a patient for transfer due to the potential risks. The Intensive Care Society (ICS) and FICM produced a joint position statement on capacity transfers in November 2021, 24 although this focuses more on planned surgery capacity transfers (i.e. to create capacity for expedited or elective surgery). However, NHS England produced a framework with guidance on interhospital transfer of critically ill patients in December 2021 25 which centred on emergency and urgent patients. The transfers in this study followed most of the principles set out in this document, although they did not involve a dedicated transfer service. There remains a scarcity of guidance on selecting the ideal patient to transfer. However, safe transfer requiring a significant or deleterious change in the patient’s treatment is cited as a reason to avoid selecting them.
All transfers involved Scottish Ambulance Service resources and aside from two instances, were performed by medical staff from within our unit. Grade of the transferring doctor ranged from CT1 to consultant. There were 7 destination units within the West of Scotland Critical Care Network, and although many of the patients were kept within our health board, distances travelled ranged from 9.7 to 72.3 miles. Ambulances were booked and allocated according to the Scottish Ambulance Service interhospital transfer protocol which includes capacity transfers in its description for a 1–2 h response. There was no set protocol for managing patients during transfer and this was not specifically measured as part of the study. However, for some patients the process involved increased depth of sedation and/or the addition of neuromuscular blockade, with the potential to affect respiratory weaning progress. Additionally, we did not measure the transfer process itself for the purposes of this study. Therefore, time waiting for an available ambulance, journey time, grade of accompanying staff, and handover process are among the unmeasured factors which could have had an effect. For example, communication incidents have previously been identified as significant factors associated with harm during interhospital transfer of patients. 26
This study had several additional weaknesses. Firstly, the data is inherently biased through its observational and retrospective nature. The patients all came from a single centre and numbers were small. Therefore, the findings are not generalisable to the entire region and the data is likely underpowered to detect a small mortality difference. Although attempts were made to control for confounders, there may have been others not considered. There is inherent selection bias as the patients were chosen for transfer based on their stability, and so may have been further on in their disease process or have clinically less severe disease. This may falsely lower mortality or ventilator days in the transferred group, although this trend was not observed. Additionally, patient physiology and staffing of transferring and receiving units were unmeasured at the time of transfer. This precludes attempts to control for variations in these factors in the interpretation of the results.
There were also several strengths to this study. The primary outcome is important to both intensivists and families of critically ill patients with COVID-19. The data is locally applicable and may be of use to other district general hospitals within Scotland and the UK. All patients were followed up to completion of their hospital stay, which is arguably a more valuable endpoint to patients and families. At the analysis stage, attempts were also made to control for confounders despite unmatched cohorts and small numbers.
Although overall ventilator days and ICU length of stay have been included in the results, great caution should be taken with interpreting this data. Firstly, these are secondary outcomes and were not within the original aims of the study. The sample size is small and easily prone to bias from confounding factors. Patients may have been excluded from transfer when felt to be unlikely to require intensive care for much longer, or equally if felt to have a poor prognosis. The recent NHS England guidance cautions against transferring patients who are close to being extubated if they would require re-sedation for safe transport and so supports this practice. 25 Practices may also vary between the transferring unit and numerous receiving units.
Overall, no difference was found in survival to ultimate hospital discharge between patients who underwent capacity transfer and those who remained. The study was prone to bias and likely underpowered to detect small differences in mortality. It will not immediately change practice within the region but rather provides preliminary data for clinicians. Any comparisons between the groups should be made with caution as they are likely affected by unmeasured confounders, and so correlations cannot be inferred. However, it signals areas for further study such as patient selection and measuring capacity along with staffing. Our experience was that patient selection, along with communicating this to next of kin, could be challenging. Although guidance has been published in the interim, this is likely to still be the case. While the total numbers were small, our data appears to agree with published literature that transfer of critically ill COVID-19 patients is safe and feasible given there were no adverse events. Since staffing was a major issue identified in the requirement for transfers and in the possible sequelae of ad-hoc transfers, ongoing monitoring of critical care staffing will be worthwhile. Subsequent to starting this study, a regional critical care network transfer team has been introduced. This should help to standardise transfer practice, maintain a low adverse event rate, and relieve pressure on staff at transferring units. In the future, a prospective regional multi-centre study of survival in transferred patients with COVID-19 could focus on these points and provide more robust findings.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics statement: This study was undertaken in accordance with the NHS Lanarkshire Caldicott approval process. As a service evaluation audit utilising data available to the clinicians in the normal course of their duties, neither formal ethics approval nor further Caldicott Guardian approval was deemed necessary.
ORCID iD
Adam J Stark https://orcid.org/0000-0002-4369-7202
References
- 1.Scottish Intensive Care Society Audit Group . scottish intensive care society audit group report on COVID-19. As at 10 May 2021 https://beta.isdscotland.org/media/9117/2021-06-02_sicsag_report.pdf (2021, accessed 5 September 2021).
- 2.Scottish Intensive Care Society Audit Group . Audit of critical care in scotland 2021: reporting on 2020, https://publichealthscotland.scot/media/8661/audit-of-critical-care-in-scotland-2021-aug21-english.pdf (2021, accessed 17 January 2022).
- 3.Faculty of Intensive Care Medicine . Guidelines for the provision of intensive care services: Edition 2, https://staging.ficm.ac.uk/sites/ficm/files/documents/2021-10/gpics-v2.pdf (2019, accessed 2 November 2021).
- 4.Neuraz A, Guérin C, Payet C, et al. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit Care Med 2015; 43(8): 1587–1594. [DOI] [PubMed] [Google Scholar]
- 5.Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US department of veteran affairs hospitals during the COVID-19 pandemic. JAMA Netw Open 2021; 4(1): e2034266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McHugh MD, Aiken LH, Sloane DM, et al. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals. The Lancet 2021; 397(10288): 1905–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faculty of Intensive Care Medicine . Guidance on: the transfer of the critically ill adult, https://www.ficm.ac.uk/sites/default/files/transfer_critically_ill_adult_2019.pdf (2019, accessed 5 September 2021).
- 8.Bourn S, Wijesingha S, Nordmann G. Transfer of the critically ill adult patient. BJA Educ 2018; 18(3): 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ligtenberg JJ, Arnold LG, Stienstra Y, et al. Quality of interhospital transport of critically ill patients: a prospective audit. Crit Care 2005; 9(4): R446–R451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kue R, Brown P, Ness C, et al. Adverse clinical events during intrahospital transport by a specialized team: a preliminary report. Am J Crit Care 2011; 20(2): 153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melgarejo Urendez A, Bernat Adell MD, Lorente Garcia P, et al. Analysis of adverse events associated with interhospital transfer of critically ill patients. Safety checklist. Enferm Intensiva 2014; 25(2): 58–64. [DOI] [PubMed] [Google Scholar]
- 12.Van Lieshout EJ, Binnekade J, Reussien E, et al. Nurses versus physician-led interhospital critical care transport: a randomized non-inferiority trial. Intensive Care Med 2016; 42: 1146–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lyphout C, Bergs J, Stockman W, et al. Patient safety incidents during interhospital transport of patients: A prospective analysis. Int Emerg Nurs 2018; 36: 22–26. [DOI] [PubMed] [Google Scholar]
- 14.Grier S, Brant G, Gould TH, et al. Critical care transfer in an English critical care network: analysis of 1124 transfers delivered by an ad-hoc system. J Intensive Care Soc 2020; 21(1): 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellingan G, Olivier T, Batson S, et al. Comparison of a specialist retrieval team with current United Kingdom practice for the transport of critically ill patients. Intensive Care Med 2000; 26(6): 740–744. [DOI] [PubMed] [Google Scholar]
- 16.Wiegersma JS, Droogh JM, Zijlstra JG, et al. Quality of interhospital transport of the critically ill: impact of a Mobile Intensive Care Unit with a specialized retrieval team. Crit Care 2011; 15(1): R75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malpass HC, Enfield KB, Keim-Malpass J, et al. The interhospital medical intensive care unit transfer instrument facilitates early implementation of critical therapies and is associated with fewer emergent procedures upon arrival. J Intensive Care Med 2015; 30(6): 351–357. [DOI] [PubMed] [Google Scholar]
- 18.Painvin B, Messet G, Rodriguez M, et al. Inter-hospital transport of critically ill patients to manage the intensive care unit surge during the COVID-19 pandemic in France. Ann Intensive Care 2021; 11: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanchez M, Vuagnat A, Grimaud O, et al. Impact of ICU transfers on the mortality rate of patients with COVID-19: insights from comprehensive national database in France. Ann Intensive Care 2021; 11(1): 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guillon A, Laurent E, Godillon L, et al. Inter-regional transfers for pandemic surges were associated with reduced mortality rates. Intensive Care Med 2021; 47(7): 798–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frakes MA, Richards JB, Cocchi MN, et al. Critical Care Transport of Patients With COVID-19. J Intensive Care Med 2021; 36(6): 704–710. [DOI] [PubMed] [Google Scholar]
- 22.Allen R, Wanersdorfer K, Zebley, et al. Interhospital transfer of critically Ill patients because of coronavirus disease 19-related respiratory failure. Air Med J 2020; 39(6): 498–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mazzoli CA, Gamberini L, Lupi C, et al. Interhospital transfer of crtitically ill Covid-19 patients: preliminary considerations from the Emilia-Romagna experience. Air Med J 2020; 39(5): 423–426. [Google Scholar]
- 24.Faculty of Intensive Care Medicine . Capacity transfer of adult critical care patients: position statement, https://www.ficm.ac.uk/capacity-transfer-of-adult-critical-care-patients-position-statement (2021, accessed 8 January 2022).
- 25.NHS England . Framework to support inter-hospital transfer of critical care patients, https://www.england.nhs.uk/wp-content/uploads/2021/12/B1215-framework-to-support-inter-hospital-transfer-of-critical-care-patients.pdf (2021, accessed 25 Jan 2022).
- 26.Lyphout C, Bergs J, Stockman W, et al. Patient safety incidents during interhospital transport of patients: A prospective analysis. Int Emerg Nurs 2018; 36: 22–26. [DOI] [PubMed] [Google Scholar]