Abstract
Background and aim: Use of nicotine can harm adolescents’ brains and increase risk for future addiction to other drugs. Several international studies show that an acceptable attitude towards nicotine products increases the initiation or use of the products. Adolescents have limited or distorted knowledge about nicotine products. Many of them have a positive image of the properties and effects of nicotine products, which increases the chances of smoking or using snus. Yet, we know little about the relationship between youth nicotine use, youth attitudes towards nicotine products and the interventions to influence these attitudes. This systematic review synthesised adolescents’ attitudes towards nicotine products and the ways to influence them. Methods: Systematic searches were carried out from PubMed, MEDLINE, CINAHL, and MEDIC databases and were targeted to randomised controlled trial (RCT) studies published in 2010–2021. Results: A total of seven RCT studies were reviewed with a total population (age range 9–17 years, adolescents 11–17 years) of 15,974. Findings were classified into four categories: school-based interventions, tobacco prevention campaigns, advertisements’ influence on adolescents’ opinions towards nicotine products, and their responses to cigarette pack warnings. Conclusion: Based on this systematic literature review, particularly school-based interventions have an effect on adolescents’ attitudes towards smoking and preventing them from starting to smoke, when they are targeted before the age of puberty. School-based interventions should be further implemented and strengthened, as the school has been shown to have significant potential to support youth’s health. There is a need for further information about the most effective interventions in the different age groups and the qualitative studies on the topic.
Keywords: adolescent, attitude, health promotion, nicotine products, school-based intervention
Smoking is the leading cause of preventable death worldwide (Samet, 2013), causing more than eight million deaths each year. In addition to its effects on health, tobacco use imposes enormous economic costs in terms of healthcare, the loss of productivity, fire damage, and environmental harm (World Health Organization [WHO], 2019). Use of nicotine can harm adolescents’ brains and increase risk of future addiction to other drugs (Everett et al., 2000; Kandel & Kandel, 2015; McCabe et al., 2017; Murthy, 2016).
It is known that children are vulnerable to nicotine addiction (Murthy, 2016; WHO, 2017). Because of the strong addictiveness of nicotine products, large proportions of early experimentations eventually develop into daily, addictive use. The likelihood of developing an addiction depends in partly on age. Adolescent under 15 years who have smoked have an estimated 50% chance of developing nicotine addiction. Risk of nicotine addiction increases if smoking is repeated over a prolonged period (WHO, 2017). Most addiction to tobacco develops before age 21 years (Ali et al., 2020; WHO, 2017).
One of the important problems is children's and adolescents’ use of nicotine products; for example, most smokers begin smoking by age 18 years, and nearly all first experiences of cigarettes occur before the age of 26 years (HHS [US Department of Health and Human Services], 2014). In the Europe, children’s experimentation with cigarettes is common, and smoking often starts at a young age. The WHO’s Health Behaviour in School-Aged Children Survey (2013–2014) reported 13% of girls and 22% of boys surveyed had initiated smoking by age 13 years. A total of 12% of children reported they had started to smoke regularly by the age of 15 years (WHO, 2017).
Several international studies over the last 10 years have found that an acceptable attitude towards nicotine products can increase the use or initiation of nicotine products for their users (Cavazos-Rehg et al., 2014; Edvardsson et al., 2012; Kowitt et al., 2015; Pepper et al., 2013; Trapl et al., 2016; Tseveenjav et al., 2015; Wackowski et al., 2020). Adolescents have limited, incomplete, conflicting, or distorted knowledge about nicotine products (Choi et al., 2012). Many of them have a positive image of the properties and effects of nicotine products, which increases the chances of a young person smoking or using snus (Brennan et al., 2015; Cavazos-Rehg et al., 2014; El-Shahawy et al., 2015; Kowitt et al., 2015; Vogel et al., 2021).
Adolescents have negative perceptions of tobacco products and smokers, but they believe their peers often view tobacco products positively. They also regard the use of tobacco as a functional stress-management strategy. Health and family are strong motivators to avoid nicotine products (Brown et al., 2019). Youth are often unaware of the level of nicotine in the devices they use. Although they know the health effects of tobacco products, particularly nicotine, they have a lack of knowledge about the health effects of e-cigarettes and the amount of nicotine they use (Alexander et al., 2019).
Increased awareness of negative health effects may encourage prevention and cessation of nicotine product use among youth (Alexander et al., 2019). As many previous studies around the world have shown (Alves et al., 2020; Brown et al., 2021; Chavan & Charanrajhave, 2020; Di Giuseppe et al., 2020; Shilco et al., 2020), there is a need to strengthen the multi-professional healthcare system and, for example, various school-based smoking risk campaigns to arouse awareness, to enable early detection, and to implement strategies to prevent nicotine addiction among adolescents. According to Brown et al. (2019), peer-to-peer discussion of tobacco experiences and perceptions may help correct the incongruent viewpoints of the use of tobacco products.
Epidemiological, clinical, and preclinical data have shown that adolescent exposure to tobacco and nicotine can lead to subsequent abuse of nicotine and other substances (Kandel & Kandel, 2015). Cross-sectional studies have demonstrated an association between 30-day tobacco use and risk behaviours such as illicit substance use (Everett et al., 2000). This association is even stronger among adolescents who report use of multiple nicotine products (McCabe et al., 2017).
Aim
The aim of this systematic review was to examine adolescents’ attitudes towards nicotine products and ways of influencing them.
Method
Protocol
This systematic review was carried out using the steps of Fink’s model (2010) to conduct a research literature review. The model was chosen because it is an accurate and reproducible method of identifying, evaluating, and summarising published research material. The model starts by identifying the research questions, selecting the databases and the search terms, conducting the search and synthesising the results, and producing the descriptive review. Studies included in the review were evaluated using valid appraisal tool, the Joanna Briggs Institute’s (JBI) Checklist for Randomized Controlled Trials (Tufanaru et al., 2020). This report follows a modified version of the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2010).
Search strategy
The research questions of the systematic review were “What kind of attitudes do adolescents have towards nicotine products?” and “What kind of methods are there to influence adolescents’ attitudes towards nicotine products?”. The databases PubMed, MEDLINE, CINAHL, and MEDIC were systematically searched in October 2021. A set of search terms was created with Medical Subject Headings (MeSH) and other words to describe the research topic. The search terms were combined into search phrases using Boolean operators, as shown in Table 1. The searches were conducted in English and in Finnish.
Table 1.
Search terms in English and in Finnish and linkage in the databases.
| Database: Pubmed, Medline and Cinahl | Databese: Medic |
|---|---|
| Youth OR young OR teen OR adolescent | Nuori |
| AND | AND |
| Tobacco OR snus OR nicotine OR cigarette | Nikotiini OR tupakka OR nuuska |
| AND | AND |
| Attitude OR perception OR impact OR opinion | Asenne |
All the studies in this review fulfilled the following eligibility criteria:
Participants (people): aged 0 to 24 years
Topic: adolescents’ attitudes towards nicotine products and methods to influence adolescents’ attitudes towards nicotine products
Published between 2010 and 2021
Randomised controlled trials
Peer-reviewed, published and free full text available in English or Finnish
Studies were excluded if they did not fulfil these criteria. Nicotine products encompass all products that include nicotine except nicotine replacement therapy products. Studies that examined both nicotine products and drugs were also included in the review if the results for nicotine products could be separated from the results.
Data extraction
In every database, two independent researchers conducted the same database searches using the same criteria and carried out the evaluation. All papers from the database searches were collated into one file and duplicates were removed. The screening of the papers was conducted to ensure that studies fulfilled the eligibility criteria. In a three-stage process, papers were screened based on title, abstract and full text evaluation using the JBI Checklist for Randomized Controlled Trials. The papers which were relevant to the research question were systematically marked and tabulated into a table. The table included author(s), publication date, country of origin, study design and data collection method, and key findings. The extraction process was conducted by two independent researchers and any disagreements were resolved through discussion in the research team.
Assessment of quality
The quality of eligible studies was assessed using the JBI Checklist for Randomized Controlled Trials. The quality of the articles was estimated and given scores according to the research method, sample size, the authors’ competence, the place of publication, and cultural suitability. The studies were grouped, based on their points, into excellent (11–13 points), good (8–10 points) or moderate (≤ 7 points). All the studies were independently rated by two researchers and any disagreements were resolved through discussion in the research team.
Search results
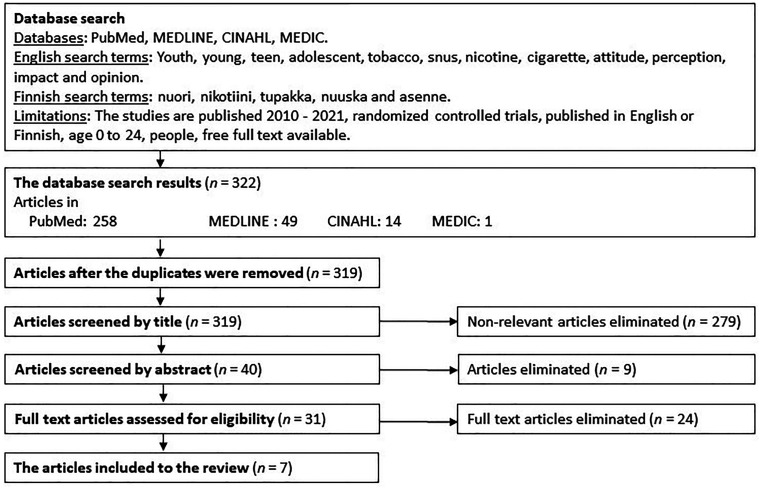
The database search resulted in 322 papers (PubMed 258, MEDLINE 49, CINAHL 14, and MEDIC 1). In every database, two independent researchers conducted the same searches using the same criteria. The material contained three duplicate articles, which were removed. In the next stage, 319 articles were evaluated based on the titles, resulting in 279 articles being eliminated. The remaining 40 articles were screened on abstract, with nine being eliminated, leaving 31 articles. On reading the full text, 24 articles were found to be ineligible, the most common reasons for eliminations were the age range or absence of attitudes towards nicotine products. Ultimately seven articles were eligible for the review. The PRISMA flowchart (Figure 1) (Moher et al., 2010) shows the process of the database search. The database search was conducted for the second time in October 2021 verifying new published studies on the topic, but there were none.
Figure 1.
PRISMA 2010 flow diagram.
Quality assessment
The quality assessment of the eligible studies was carried out using the JBI Checklist for Randomized Controlled Trials. All the studies’ aims were clearly stated in the articles. The articles scored between six and nine points, when the maximum score was 13 points. Three of the articles scored nine points (good) and two eight points (good). Two articles scored either seven or six points (moderate). These articles were scored as moderate, because they failed to clearly define their procedures about participant grouping and the groups’ similarity at baseline. The processes of delivering treatment blinded to treatment assignment, and the randomising of the participants were not clearly shown. Both articles were included in the systematic review because of the value they added to it. A more detailed specification of the quality assessment is shown in Table 2.
Table 2.
Quality assessment.
| Authors and Year of Publication | Quality Rating | Quality Appraisal Findings |
|---|---|---|
| Giannotta et al. (2014) | Good (8) | Participants were randomised. |
| The allocation to treatment groups was concealed and similar at baseline. | ||
| Participants, researchers, and outcome assessors being blind to the treatment assignment is not clearly stated. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups to which they were randomised. | ||
| Outcomes were measured in the same way in treatment groups. | ||
| The measurement of the outcomes was unclear. | ||
| Statistical analysis was appropriate, as well as trial design, but there was some unclarity in trial design. | ||
| Isensee et al. (2014) | Good (9) | Participants were randomised. |
| Treatment groups were similar at baseline, but the allocation to treatment groups being concealed was unclear. | ||
| Participants were blind to the treatment assignment, but researchers and outcomes assessors’ status was unclear. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same reliable way in treatment groups. | ||
| Statistical analysis was appropriate, as well as trial design, but there was some unclarity in trial design. | ||
| La Torre et al. (2010) | Good (9) | Participants were randomised. |
| The allocation to treatment groups was concealed and similar at baseline. | ||
| Participants, researchers, and outcome assessors being blind to the treatment assignment was not clearly stated. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same reliable way in treatment groups. | ||
| Statistical analysis was appropriate, as well as trial design, but there was some unclarity in trial design. | ||
| Miovsky et al. (2012) | Good (9) | Participants were randomised. |
| Treatment groups were similar at baseline, but the allocation to treatment groups being concealed was unclear. | ||
| Participants and researchers were blind to the treatment assignment, but the status of the outcomes assessors was unclear. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same reliable way in treatment groups. | ||
| Statistical analysis was appropriate, as well as trial design, but there was some unclarity in trial design. | ||
| Padon et al. (2018) | Good (8) | Participants were randomised. |
| Treatment groups were similar at baseline, but the allocation to treatment groups being concealed was unclear. | ||
| Participants were blind to the treatment assignment, but the status of the researchers and the outcome assessors was unclear. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same way in treatment groups. | ||
| The measurement of the outcomes was unclear. | ||
| Statical analysis and trial design was appropriate. | ||
| Peebles et al. (2016) | Moderate (6) | Participants were randomised. |
| Treatment groups were similar at baseline, but the allocation to treatment groups being concealed was unclear. | ||
| Participants, researchers, and outcome assessors being blind to the treatment assignment is not clearly stated. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same way in treatment groups. | ||
| The measurement of the outcomes was unclear. | ||
| Statical analysis and trial design was appropriate. | ||
| Zhao et al. (2016) | Moderate (7) | Participants were randomised. |
| Treatment groups were similar at baseline, but the allocation to treatment groups being concealed was unclear. | ||
| Participants, researchers, and outcome assessors being blind to the treatment assignment is not clearly stated. | ||
| Treatment groups were treated identically (other than the part of the intervention of interest). | ||
| Group follow up was adequately described and analysed and participants were analysed in the groups in which they were randomised. | ||
| Outcomes were measured in the same and reliable way in the treatment groups. | ||
| Statistical analysis was appropriate, as well as trial design, but there was some unclarity in trial design. |
Results
A total of seven articles were included in the systematic review. All the studies were randomised controlled trials (RCTs) and study population age range was 9–17 years and the adolescents’ age range was 11–17 years. Four of the articles were conducted in Europe (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010; Miovsky et al., 2012) and three in the USA (Padon et al., 2018; Peebles et al., 2016; Zhao et al., 2016). Four studies were school-based interventions, two studied the effects of tobacco product advertising and one study was based on a tobacco prevention campaign. The summary of the studies is shown in Table 3.
Table 3.
Summary of the studies.
| Study | Sample Characteristics | Aim | Outcome Measures |
|---|---|---|---|
| Giannotta et al. (2014) |
n = 7,079 A four-arm cluster randomiz sed controlled trial where schools were randomly assigned either to one of the three experimental arms or to a control group receiving the usual health education curriculum in seven European countries. (Participants’ mean age 13.25 years) |
To study factors mediating the effects of a European school-based intervention (Unplugged) based on a social influence approach to youths’ substance use. | The intervention significantly reduced participants’ positive attitudes toward drugs, positive beliefs about the consequences of tobacco, alcohol and cannabis use, and the perception of having many friends who smoke cigarettes and cannabis compared with the control group. Their ability to refuse peers’ invitations to smoke cigarettes and their knowledge increased. The intervention improved class climate and marginally significantly increased refusal skills for alcohol and cannabis use, and negative beliefs about the consequences of tobacco use. |
| Isensee et al. (2014) |
n = 2,513 A two-arm prospective cluster randomised controlled trial for students in Grades 5 and 6 in four federal states in Germany with a follow-up survey. (Participants’ mean age 10.37 years and in follow-ups 12.50 years) |
To study the effects of a school-based prevention programme on students’ smoking-related behaviour, attitudes, and knowledge. | School-based prevention significantly increased smoking-related knowledge. The programme participation seems to reduce the prevalence and incidence of lifetime smoking, increase smoking-related knowledge and influence attitudes and perceived risks of smoking towards a more critical perception. |
| La Torre et al. (2010) |
n = 842 The trial included 534 children (ages 9–11 years) and 308 adolescents (ages 14–15 years), who were randomly selected to receive or not to receive the prevention programme. Questionnaires were used before the intervention and two years later. |
To study a school-based programme to prevent children’s and adolescents’ tobacco use. | The prevalence rates of smoking in both groups were increased at the end of the study. The difference of smoking prevalence between the intervention and control groups was statistically significant only for the children's group. The study indicates that the school programmes designed to prevent tobacco use in children and adolescents could become one of the most effective strategies available to reduce tobacco use all over the world. If the onset of smoking occurs predominantly during adolescence, maybe this age is too late to start an effective prevention programme, and targeting young children before they begin to smoke could be a successful method of prevention. |
| Miovsky et al. (2012) |
n = 1,753 6th graders (ages 11–13 years) from three regions in the Czech Republic were randomised to either control or intervention arms. |
To study a school-based intervention (Unplugged) to reduce the risk of alcohol, tobacco, inhalant, and illegal drug use among children. | The Unplugged programme shows evidence of the effectiveness of a school-based intervention. It produced positive effects on reducing current tobacco and marijuana use in the target group and prevented increases in the lifetime prevalence of other drug use two years after the intervention was delivered. Unplugged lays the foundation for evidence-based and effective universal substance abuse prevention programmes to help decrease the high prevalence of tobacco and marijuana use. |
| Padon et al. (2018) |
n = 417 Non-smoking youth (ages 13–17 years) were randomly assigned to either the control group or to view the advertisements. After exposure, there were covert and overt measurements. |
To study the effect of youth appealing e-cigarette advertisements on susceptibility to use e-cigarettes among youth. | Nearly half of the respondents agreed or strongly agreed that e-cigarettes are high-tech, a third thought e-cigarettes were visually appealing, over 25% thought they were socially helpful or cool, and 22% thought they were enjoyable or fun. 15% of the respondents’ agreed e-cigarettes are healthy. 54% were susceptible to trying an e-cigarette and over a third a tobacco cigarette. |
| Peebles et al. (2016) |
n = 112 Adolescents’ (ages 13–17 years) parents received either text-only or pictorial warnings on their cigarette packs for four weeks. Adolescents’ responses to these cigarette packs were measured. |
To study adolescents’ responses to warnings on their parents’ cigarette packs. | Pictorial warnings elicited stronger negative emotional reactions than text-only warnings. Compared with text-only warnings, pictorial cigarette pack warnings were accurately recalled and recognised with greater frequency, captured more attention, elicited stronger negative emotional reactions, and inspired more social interactions among adolescents. |
| Zhao et al. (2016) |
n = 3,258 The adolescents (ages 13–17 years) were randomised to a control group or an ad-viewing group. |
To study youth receptivity to potential campaign advertisements. | Participants who viewed the advertisements generally considered them to be effective. Those exposed to campaign advertisements perceived greater health risks of and chemical intake from smoking and were more likely to believe that smoking could lead to the loss of control in life. They also expressed more negative attitudes toward smoking than those in the control group. |
According to these seven studies approved for this systematic review (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010; Miovsky et al., 2012; Padon et al., 2018; Peebles et al., 2016; Zhao et al., 2016), adolescents have a positive attitude towards tobacco products, and they have incorrect or limited information about nicotine products, particularly about new nicotine products. Adolescents agreed e-cigarettes are high-tech, and thought e-cigarettes were visually appealing. E-cigarettes were thought to be socially helpful or cool, and youth thought the products were enjoyable or fun. The results also showed a strong peer pressure effect, e.g., use of e-cigarettes.
The key findings of the methods to influence adolescents’ attitudes in these articles were classified into four categories: (1) school-based interventions influence adolescents’ attitudes towards smoking, (2) tobacco prevention campaigns influence adolescents’ opinions and attitudes towards smoking, (3) advertisements influence adolescents’ opinions towards e-cigarettes, and (4) adolescents’ responses to cigarette pack warnings.
School-based interventions influence adolescents’ attitudes towards smoking
School-based interventions proved to have an influence on adolescents’ attitudes towards smoking, and they reduced the risk of adolescents starting to smoke or lifetime smoking (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010; Miovsky et al., 2012). The interventions significantly increased knowledge about smoking, and the consequences of smoking and they reduced adolescents’ positive attitudes toward smoking (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010). School-based interventions are effective in reducing smoking habits (La Torre et al., 2010), but it is significant that the interventions should target the right age group. Smoking usually starts at the age of puberty and after this point interventions are not as effective as they are amongst younger children (Isensee et al., 2014; Miovsky et al., 2012).
Advertisements and tobacco prevention campaigns influence adolescents’ opinions and attitudes towards smoking and use of e-cigarettes
Padon et al. (2018) studied the influence of advertisements on adolescents’ opinions towards e-cigarettes and their beliefs and susceptibility to trying e-cigarettes and tobacco. The study showed that just under 50% of adolescents agreed or strongly agreed that e-cigarettes are high-tech, and a third thought e-cigarettes were visually appealing. Over 25% thought e-cigarettes were socially helpful or cool, and 22% thought they were enjoyable or fun. More than half of the adolescents (54%) were susceptible to trying e-cigarettes. Adolescents are more likely to try e-cigarettes if the product is offered by a friend (Padon et al., 2018).
Zhao et al. (2016) studied a tobacco prevention campaign’s influence on adolescents’ opinions and attitudes towards smoking. The adolescents, who were exposed to campaign advertisements, had more knowledge of the health risk of smoking and chemical intake from smoking than the control group. They were also more likely to believe that smoking could lead to the loss of control in life. They also expressed more negative attitudes towards smoking than the control group (Zhao et al., 2016).
Adolescents’ responses to cigarette pack warnings
Peebles et al. (2016) studied adolescents’ responses to pictorial or text-only warnings on their parents’ cigarette packs. Among the adolescents who reported seeing any warnings pictorial warnings were more effective than text-only warnings. Adolescents who had seen pictorial warnings were more likely to discuss them with their parents than were adolescents who saw text-only warnings. Adolescents reported feeling sadder and more “grossed out” by seeing the pictorial warnings. All adolescents who had seen the warnings (either pictorial or text-only warnings) reacted to them. They felt discouragement from wanting to smoke, and they worried about their parents’ health due to smoking. They perceived the harm of smoking and smoking susceptibility despite the warning type (Peebles et al., 2016).
Over 60% of the adolescents who had seen the warnings on their parents’ cigarette packs talked to parents, other family members, friends, boyfriends or girlfriends and classmates about the warnings. Most frequently the discussions included the negative consequences of smoking, quitting smoking, the specific health consequence depicted on the warning, and the impact of second-hand smoke on others. Adolescents who had seen a pictorial warning were more likely to talk to someone about the warnings than those who had seen the text-only warnings (Peebles et al., 2016).
Discussion
This systematic review examined adolescents’ attitudes towards nicotine products and ways of influencing them. The findings of seven eligible studies were categorised. Four studies were about school-based interventions and three were about advertising (pictorial and text and text-only warning labels on cigarette packs, or tobacco prevention campaign advertisements or e-cigarette advertisements). School seems to be a good place to influence adolescents’ attitudes and reach the right target group, and advertisements are also effective.
Adolescents can be interested in nicotine products for many reasons. Padon et al. (2018) showed that some adolescents thought e-cigarettes are high-tech, and they were visually appealing as well socially helpful or cool and enjoyable or fun. Some of them thought e-cigarettes are healthy, and they were susceptible to trying e-cigarettes and cigarettes (Padon et al., 2018). According to Peebles et al. (2016), pictorial warnings elicited stronger negative emotional reactions than text-only warnings. Pictorial warnings may be well suited to reach the group of adolescents at higher risk of smoking initiation. Compared with text-only warnings, pictorial cigarette pack warnings were accurately recalled and recognised with greater frequency, captured more attention, elicited stronger negative emotional reactions, and inspired more social interactions among adolescents (Peebles et al., 2016).
However, exposing adolescents to advertisements on e-cigarettes can increase adolescents’ interest in the use of e-cigarettes and cigarettes. It still indicates that prevention advertisements on nicotine products are a good and effective way to prevent adolescents’ desire to try nicotine products (Padon et al., 2018).
Tobacco preventing campaigns and warnings on nicotine product packing (especially pictorial warnings) can result in good conversations about the topic and give more knowledge and, at the same time, have a positive impact on adolescents’ behaviour. Most of the adolescents who recalled seeing a warning on their parents’ cigarette packs, talked about it with the person closest to them. Most commonly, youth discuss health issues and quitting smoking. This finding is particularly important for adolescents living with smokers (Peebles et al., 2016). However, the quality and effectiveness of the discussions depends on accurate knowledge of the participants and their interaction skills. The recurrence of these discussions may also make a difference.
Even though advertisements for nicotine products have been prohibited in several countries for decades there is still subliminal advertising, for example, in social media and the film industry. The influence of social media on adolescents’ attitudes towards nicotine products and the effects on adolescents’ own postings in social media did not come up in the review. It is interesting, because the use of social media is a very common and everyday activity among adolescents. Social media does offer a useful way of educating and reaching adolescents to promote their wellbeing (O’Reilly et al., 2019).
However, Zhao et al. (2016) stated that adolescents who were exposed to campaign advertisements generally considered them to be effective. They perceived greater health risks of smoking and chemical intake from smoking. They also believed that smoking could lead to the loss of control in life and expressed more negative attitudes toward smoking than those in the control group. It may be that social media could be effectively used to prevent the use of nicotine products. Social media campaigns should be targeted to adolescents and utilise social media, which is widely used by adolescents. Then it would be possible to increase the adolescents’ knowledge about the nicotine products, affect their opinions about the nicotine products and make an impact to encourage the adolescents’ non-smoking habits.
Adolescents are interested in nicotine products for their visual appeal and because they consider them cool to use (Padon et al., 2018). Peer pressure can have an impact on starting to use nicotine products. School is a good place to reach adolescents and conduct health promotion interventions. Because of that, school-based health promotion interventions are widely studied around the world. Based on this systematic literature review, school-based interventions have an effect on adolescents’ attitudes towards smoking and preventing them from starting to smoke (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010; Miovsky et al., 2012).
This review identified that school-based interventions affect adolescents’ smoking-related attitudes (Giannotta et al., 2014; Isensee et al., 2014; Miovsky et al., 2012), reduce their positive attitudes towards drugs, and decrease their positive beliefs about the consequences of tobacco, alcohol, and cannabis use (Giannotta et al., 2014). School-based interventions have increased smoking-related knowledge (Giannotta et al., 2014; Isensee et al., 2014; Miovsky et al., 2012). They have had an impact on adolescents’ ability to refuse peers’ invitations to smoke cigarettes and their refusal skills for alcohol and cannabis and negative beliefs about the consequences the use of tobacco (Giannotta et al., 2014). School-based interventions produced positive effects on reducing current tobacco and marijuana use (Isensee et al., 2014; Miovsky et al., 2012) and prevented increases in the lifetime prevalence of other drug use two years after the intervention was delivered (Miovsky et al., 2012). Through interventions, adolescents’ perceptions became more critical towards tobacco products (Isensee et al., 2014).
La Torre et al. (2010) indicated that school programmes designed to prevent tobacco use in children and adolescents could become one of the most effective strategies available to reduce tobacco use globally. The Unplugged intervention lays the foundation for evidence-based and effective universal substance abuse prevention programmes to help decrease the high prevalence of tobacco and marijuana use. This intervention shows evidence of effectiveness among primary school students in the Czech Republic (Miovsky et al., 2012).
However, it must be considered that the use of nicotine products occurs during adolescence, and it would be better to target the interventions towards younger children before they begin to smoke. This will ensure the effectiveness of the interventions (La Torre et al., 2010). The majority of adult daily smokers have reported starting smoking by the age of 18 years (Zhao et al., 2016). It seems to be crucial to influence adolescents before they start smoking.
Strengths and limitations
Although the results of this systematic review contribute to the existing literature by providing considerable evidence for adolescents’ attitudes towards nicotine products, several limitations in the review process have been identified. First, the relatively small, and varying sample size and the use of convenience sampling in some studies limited representativeness and generalisability to a larger adolescent population. Second, all studies included in the review used self-report measures which may not provide reliable outcomes because of some sources of risk of bias. Third, this review did not include grey literature, qualitative studies, or non-English-language articles, leading to the possibility that some relevant results could have been missed.
On the other hand, the strengths of the current review are reliable information retrieval by two researchers, accurate and gradual application process, and acceptance of good quality research for the review. In order to increase reliability, the research searches were based on research tasks and various databases were used in the searches. The keywords used were chosen to be as comprehensive as possible of phenomenon under study. Keywords and delimitations were accurately reported in the review.
The reliability of the study is enhanced by the quality of the selected research articles: most of the studies were of good quality. No low-quality studies (JBI scores under 6) were accepted for review. In addition, the sample sizes of all approved studies were relatively large and had been published on peer-reviewed publication channels in the field. Finally, the review produced new information on the current topic.
Conclusion
School-based health promotion interventions are widely studied globally and adolescents’ use of nicotine products are a known problem, which needs to be attended to. Based on this systematic literature review, school-based interventions have an effect on adolescents’ attitudes towards smoking and preventing them from starting to smoke (Giannotta et al., 2014; Isensee et al., 2014; La Torre et al., 2010; Miovsky et al., 2012) when they are targeted before the age of puberty (Isensee et al., 2014; La Torre et al., 2010). School-based interventions should be further implemented and strengthened, as the school has been shown to have significant potential to support youth’s health (Isensee et al., 2014; La Torre et al., 2010).
In addition to school-based interventions, tobacco prevention campaigns and pictorial or text-only warnings on the hazards of nicotine products have also been proven to be an effective way to reduce positive attitudes towards nicotine products and increase negative reactions towards nicotine products (Peebles et al., 2016; Zhao et al., 2016). The campaigns should be targeted to adolescents and utilise social media, which is widely used by adolescents.
There is a need for further research in relation to the influence of social media on adolescents’ use of nicotine products and in supporting non-smoking habits. In addition to quantitative data, qualitative methods should be used to find out adolescents’ attitudes towards and perceptions about nicotine products. Information is also needed on what adolescents expect from school-based interventions to make them effective.
Through this systematic review, we hope we contribute to the existing literature by addressing gaps and highlighting adolescents’ attitudes towards nicotine products and the ways of influencing them. With this review, we want to emphasise the importance of adolescents’ use of nicotine products being a global public health problem.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Anu Vaihekoski https://orcid.org/0000-0003-4177-1269
Contributor Information
Anu Vaihekoski, University of Turku, Turku, Finland.
Hanna Lagström, University of Turku, Turku, Finland; and Turku University Hospital, Turku, Finland.
Sini Eloranta, University of Turku, Turku, Finland; University of Oulu, Oulu, Finland; and Turku University of Applied Science, Turku, Finland.
Susanna Bäärs, City of Turku, Turku, Finland.
Annika Hannula, Turku University Hospital, Turku, Finland.
Mari Lehvikkö, Turku University Hospital, Turku, Finland.
Minna Salakari, Turku University of Applied Science, Turku, Finland.
References
- Alexander J. P., Williams P., Lee Y. O. (2019). Youth who use e-cigarettes regularly: A qualitative study of behavior, attitudes, and familial norms. Preventive Medicine Reports, 13, 93–97. 10.1016/j.pmedr.2018.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali F. R. M., Agaku I. T., Sharapova S. R., Reimels E. A., Homa D. M. (2020). Onset of regular smoking before age 21 and subsequent nicotine dependence and cessation behavior among US adult smokers. Preventing Chronic Disease, 17, Article 190176. 10.5888/pcd17.190176externalicon [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves R. F., Precioso J., Becoña E. (2020). Smoking behavior and secondhand smoke exposure among university students in northern Portugal: Relations with knowledge on tobacco use and attitudes toward smoking. Pulmonology. 10.1016/j.pulmoe.2020.03.004 [DOI] [PubMed] [Google Scholar]
- Brennan E., Gibson L., Momjian A., Hornik R. C. (2015). Are young people’s beliefs about menthol cigarettes associated with smoking-related intentions and behaviors? Nicotine and Tobacco Research, 17(1), 81–90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4296170/. 10.1093/ntr/ntu134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown E., O’Donoghue B., White S., Chanen A., Bedi G., Adams S., Killackey E. (2021). Tobacco smoking in young people seeking treatment for mental ill-health: What are their attitudes, knowledge and behaviours towards quitting? Irish Journal of Psychological Medicine, 38(1), 30–39. 10.1017/ipm.2020.18 [DOI] [PubMed] [Google Scholar]
- Brown L. D., Bandiera F. C., Harrell M. B. (2019). Cluster randomized trial of teens against tobacco use: Youth empowerment for tobacco control in El Paso, Texas. American Journal of Preventive Medicine, 57(5), 592–600. 10.1016/j.amepre.2019.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavazos-Rehg P. A., Krauss M. J., Spitznagel E. L., Grucza R. A., Bierut L. J. (2014). Hazards of new media: Youth’s exposure to tobacco ads/promotions. Nicotine & Tobacco, 16(4), 437–444. https://www.ncbi.nim.nih.gov/pmc/articles/PMC3954423/. 10.1093/ntr/ntt168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavan S. S., Charanrajhave K. R. (2020). Prevalence, knowledge, and attitude towards smokeless tobacco use in adolescents of selected colleges at Dakshina Kannada District, Karnataka, India. Journal of Indian Association for Child & Adolescent Mental Health, 16(3), 139–161. [Google Scholar]
- Choi K., Fabian L., Mottey N., Corbett A., Forster J. (2012). Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: Findings from a focus group study. American Journal on Public Health, 102(11), 2088–2093. https://www-ncbl.nim.nih.gov/pubmed/22813086. 10.2105/AJPH.2011.300525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giuseppe G., Pelullo C. P., Mitidieri M., Lioi G., Pavia M. (2020). Cancer prevention: Knowledge, attitudes and lifestyle cancer-related behaviors among adolescents in Italy. International Journal of Environmental Research and Public Health, 17, Article 8294. 10.3390/ijerph17228294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edvardsson I., Troein M., Ejletsson G., Lendahls L. (2012). Snus user identity and addiction: A Swedish focus group study on adolescents. BMC Public Health, 12(975), 1–9. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Shahawy O., Sun P., Tsai J., Rohrbach L., Sussman S. (2015). Sense of coherence and tobacco use myths among adolescents as predictors of at-risk youth cigarette use. Substance Use & Misuse, 50, 8–14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4684587/. 10.3109/10826084.2014.957767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett S. A., Malarcher A. M., Sharp D. J., Husten C. G., Giovino G. A. (2000). Relationship between cigarette, smokeless tobacco, and cigar use, and other health risk behaviors among US high school students. The Journal of School Health, 70(6), 234–240. 10.1111/j.1746-1561.2000.tb07424.x [DOI] [PubMed] [Google Scholar]
- Fink A. (2010). Conducting research literature reviews: From the internet to paper (3rd ed.). Sage Publications. [Google Scholar]
- Giannotta F., Vigna-Taglianti F., Galanti M., Scatigna M., Faggiano F. (2014). Short-term mediating factors of a school-based intervention to prevent youth substance use in Europe. Journal of Adolescent Health, 54(5), 565–573. 10.1016/j.jadohealth.2013.10.009 [DOI] [PubMed] [Google Scholar]
- HHS (US Department of Health and Human Services). (2014). The health consequences of smoking: 50 years of progress. A Report of the Surgeon General. https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf
- Isensee B., Hansen J., Maruska K., Hanewinkel R. (2014). Effects of a school-based prevention programme on smoking in early adolescence: A 6-month follow-up of the “Eigenständig warden” cluster randomized trial. 10.1136/bmjopen-2013-004422 [DOI]
- Kandel D., Kandel E. (2015). The gateway hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Paediatrica, 104(2), 130–137. 10.1111/apa.12851 [DOI] [PubMed] [Google Scholar]
- Kowitt S., Patel T., Ranney L., Huang L., Sutfin E., Goldstein A. (2015). Poly-tobacco use among high school students. International Journal of Environmental Research and Public Health, 12(11), 14477–14489. http://www.mddpi.com/1660-4601/12/11/14477/htm. 10.3390/ijerph121114477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Torre G., Chiaradia G., Monte L., Moretti C., Mannocci A., Capitanio D., Ferrara M., Gentile A., Di Thiene D., De Vito E., Boccia A. (2010). A randomised controlled trial of a school-based intervention to prevent tobacco use among children and adolescents in Italy. Journal of Public Health, 18(6). 10.1007/s10389-010-0328-8
- McCabe S. E., West B. T., Veliz P., Boyd C. J. (2017). E-cigarette use, cigarette smoking, dual use, and problem behaviors among US adolescents: Results from a national survey. The Journal of Adolescent Health, 61(2), 155–162. 10.1016/j.jadohealth.2017.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miovsky M., Novak P., Stastna L., Gabrhelik R., Jurystova L., Vopravil J. (2012). “Unplugged”: A school-based randomized control trial to prevent and reduce adolescent substance use in the Czech Republic. Drug and Alcohol Dependence, 124(1–2), 79–87. 10.1016/j.drugalcdep.2011.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaffa J., Altman D. G. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Murthy V. H. (2016). E-cigarette use among youth and young adults: A major public health concern. JAMA Pediatrics, 171(3), 209–210. 10.1001/jamapediatrics.2016.4662 [DOI] [PubMed] [Google Scholar]
- O’Reilly M., Dogra N., Hughes J., Reilly P., George R., Whiteman N. (2019). Potential of social media in promoting mental health in adolescents. Health Promotion International, 34(5), 981–991. 10.1093/heapro/day056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padon A., Lochbuehler K., Maloney E., Cappella J. (2018). A randomized trial of the effect of youth appealing e-cigarette advertising on susceptibility to use e-cigarettes among youth. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 20(8), 954–961. 10.1093/ntr/ntx155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peebles K., Hall M., Pepper J., Byron J., Noar S., Brewer N. (2016). Adolescents’ responses to pictorial warnings on their parents’ cigarette packs. The Journal of Adolescent Health, 59(6), 635–641. 10.1016/j.jadohealth.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper J. K., Reiter P. L., McRee A. L., Cameron L. D., Gilkey M. B., Brewer N. T. (2013). Adolescent males’ awareness of and willingness to try electronic cigarettes. Journal of Adolescent Health, 52(2), 144–150. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3569032/. 10.1016/j.jadohealth.2012.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet J. M. (2013). Tobacco smoking: The leading cause of preventable disease worldwide. Thoracic Surgery Clinics, 23(2), 103–112. 10.1016/j.thorsurg.2013.01.009 [DOI] [PubMed] [Google Scholar]
- Shilco P., Golshan T., Lande S., Nickfardjam K., Roitblat Y., Morgan A., Nehuliaieva L., Shterenshis M. (2020). Knowledge and attitudes of adolescents to e-cigarettes: An international prospective study. International Journal of Adolescent Medicine and Health, 2020, Article 20190210. 10.1515/ijamh-2019-0210 [DOI] [PubMed] [Google Scholar]
- Trapl E. S., Yoder L. D., Frank J. L., Borawski E. A., Sattar A. (2016). Individual, parental, and environmental correlates of cigar, cigarillo, and little cigar use among middle school adolescents. Nicotine & Tobacco Research, 18(5), 834–841. [DOI] [PubMed] [Google Scholar]
- Tseveenjav B., Pesonen P., Virtanen J. (2015). Use on snus, its association with smoking and alcohol consumption, and related attitudes among adolescents: The Finnish National School Health Promotion Study. BioMed Central, Tobacco Included Diseases, 13(34), 1–9. https://doi.org/10.1186/s12971-015-0058-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tufanaru, C., Munn, Z., Aromataris, E., Campbell, J., & Hopp, L. (2020). Chapter 3: Systematic reviews of effectiveness. In E. Aromataris, & Z. Munn (Eds.), JBI manual for evidence synthesis. JBI. https://synthesismanual.jbi.global. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fjbi.global%2Fsites%2Fdefault%2Ffiles%2F2021-10%2FChecklist_for_RCTs. docx&wdOrigin=BROWSELINK [Google Scholar]
- Vogel E. A., Henriksen L., Schleicher N. C., Prochaska J. J. (2021). Young people’s e-cigarette risk perceptions, policy attitudes, and past-month nicotine vaping in 30 US cities. Drug and Alcohol Dependence, 229(Pt A), Article 109122. 10.1016/j.drugalcdep.2021.109122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wackowski O. A., Rashid M., Greene K. L., Lewis M. J., O’Connor R. J. (2020). Smokers’ and young adult non-smokers’ perceptions and perceived impact of snus and e-cigarette modified risk messages. International Journal of Environmental Research and Public Health, 17(18), Article 6807. 10.3390/ijerph17186807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). Tobacco-free generations: Protecting children from tobacco in the WHO European Region. WHO http://www.euro.who.int/__data/assets/pdf_file/0008/343376/20170428_WHO-TobaccoFreeGenerationDRAFT09. pdf?ua=1
- World Health Organization. (2019). Tobacco control. WHO. http://www.euro.who.int/__data/assets/pdf_file/0009/422838/Tobacco-8-B-002.pdf?ua=1
- Zhao X., Alexander T., Hoffman L., Jones C., Delahanty J., Walker M., Berger A., Talbert E. (2016). Youth receptivity to FDA’s The Real Cost tobacco prevention campaign: Evidence from message pretesting. Journal of Health Communication, 21(11), 1153–1160. 10.1080/10810730.2016.1233307 [DOI] [PMC free article] [PubMed] [Google Scholar]