Abstract
Introduction
As healthcare systems are adapting due to COVID-19, there has been an increased need for telehealth in the outpatient setting. Not all patients have been comfortable with this transition. We sought to determine the relationship between health literacy and technological comfort in our cancer patients.
Methods
We conducted a survey of patients that presented to the oncology clinics at a single-center over a 2-month period. Patients were given a voluntary, anonymous, survey during their visit containing questions regarding demographics, health literacy and technological comfort.
Results
344 surveys were returned (response-rate 64.3%). The median patient age was 61 years, 70% of responders were female and the most common race was White (67.3%). Increasing patient age, male gender, Black and Native-American race, decreased health literacy and lack of home broadband were associated with lower technological comfort score.
Conclusion
In our cohort, patients with lower health literacy scores, older and male patients, or who have poor internet access showed a lower level of technological comfort. At risk patients can be identified and provided additional support in their use of telehealth services.
Keywords: Health literacy, Telehealth, Health disparity
1. Introduction
In March 2020 the World Health Organization (WHO) declared COVID-19 as a global pandemic,1 and health systems began to implement strategies that would protect both patients and healthcare workers. A key component of limiting communicable disease is the concept of “social distancing”.2 In the outpatient setting, the elimination of crowded waiting rooms and the avoidance of unnecessary patient contact are key factors in limiting disease spread. In order to facilitate this transition, many healthcare services have invested in improving and expanding their telemedicine capabilities.
Although the benefits of telehealth, providing both electronic consultations and image-based triage are clear, its adoption into practice has been slow and inconsistent.3, 4, 5 Reasons commonly cited for this include clinician resistance, diminished financial reimbursement, and the costly need for healthcare system re-organization.6 Yet in other parts of the world, governments and healthcare services have successfully developed and utilized telehealth during critical situations.7, 8, 9 With the global spotlight on the COVID-19 pandemic, there has been a renewed investment in telehealth at the physician, institution, and government levels to facilitate its success. Follow up for cancer patients usually involves a patient interview and review of imaging or bloodwork. This lends itself well to a telehealth approach and has been shown to be preferred by patients.10
However, the efficacy of telehealth is not only dependent on the service availability, but also hinges on patient engagement. Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate healthcare decisions”.11 Poorer health literacy has been noted to be more prevalent in specific populations, including low income and racial or ethnic minorities.12 Studies have shown that patients with poor health literacy are more likely to have inferior healthcare outcomes13; these patient are also less likely to engage with healthcare information technology, including telehealth.14
Given the changing nature of healthcare delivery, it is important to identify these potentially at-risk patients in a vulnerable cancer population. We therefore sought to investigate the association between patient demographics, health literacy and comfort with technology in our cancer population.
2. Methods
Setting: The University of Alabama at Birmingham (UAB) Medical Center is a tertiary referral hospital serving the population of Alabama. We conducted this study in the outpatient cancer clinic setting in the divisions of Surgical Oncology, Medical Oncology, Gynecologic Oncology, and Breast Oncology over the course of 2 months (October to November 2020). All patients attending these clinics were given an anonymous paper survey to prior to their provider in-person visit. Completion was voluntary and participants returned unidentified surveys in secure lockboxes to ensure anonymity. Surveys were collected weekly and transcribed into a secure online database. The UAB Institutional Review Board approved the conduct of this study (IRB-300005711).
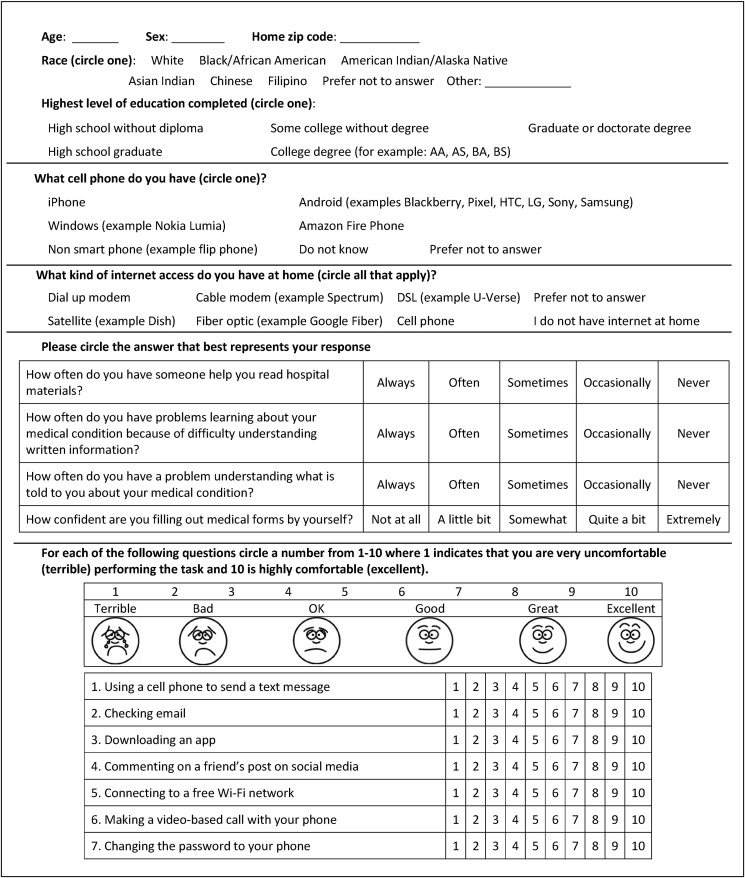
Survey: The survey was a multiple choice, 5-part questionnaire (Appendix 1). Patients were asked questions regarding their demographics, health literacy and comfort with technology. Race was self-reported by study participants from race categories defined by investigators. Health literacy was assessed using the validated Brief Health Literacy tool.15
We were unable to find a validated tool for measuring technological comfort; therefore, one was developed for this project and its accuracy validated. Each technology comfort question was created to assess one of three constructs: communication (Q1 and Q6), device maintenance (Q5 and Q7), and the performance of complex tasks with the technological device (Q2, Q3 and Q4). The responses were scored using a 10-point Likert scale. The survey was reviewed by experts not involved in the research to optimize accuracy, minimize bias, maintain appropriate grammar, and eliminate item construction problems. The survey was first administered to a group of 35 volunteers before being given to the patient population. The volunteer group did not have any suggestions for improvement. Internal consistency was determined for all 7 questions in association with the validated Brief Health Literacy Tool15 using Cronbach's alpha coefficient (Table 1 ). Construct validity was determined by measuring correlation coefficients between questions within the same constructs (Table 2 , all > 0.7).
Table 1.
Internal consistency of technological comfort survey questions.
| Item | Observations | Correlation | Item-test correlation | Item-rest correlation | Average inter-item covariance | Alpha |
|---|---|---|---|---|---|---|
| Q1 | 332 | + | 0.7938 | 0.7425 | 8.470239 | 0.9355 |
| Q2 | 331 | + | 0.8476 | 0.8023 | 8.113042 | 0.9312 |
| Q3 | 330 | + | 0.9261 | 0.8998 | 8.113042 | 0.9236 |
| Q4 | 322 | + | 0.8586 | 0.8099 | 7.758425 | 0.9296 |
| Q5 | 330 | + | 0.9335 | 0.9087 | 7.486007 | 0.9229 |
| Q6 | 325 | + | 0.8752 | 0.8307 | 7.687584 | 0.9284 |
| Q7 | 329 | + | 0.9007 | 0.8633 | 7.504819 | 0.9259 |
| Brief Health Literacy | 334 | + | 0.6694 | 0.5441 | 8.268669 | 0.9549 |
Table 2.
Construct validity of technological comfort survey questions.
| Construct | Variables | Correlation Coefficient |
|---|---|---|
| Communication | Q1 Q6 | 0.7756 |
| Maintenance | Q5 Q7 | 0.9305 |
| Tasks | Q2 Q3 | 0.8909 |
| Q3 Q4 | 0.8732 | |
| Q2 Q4 | 0.8354 |
Income: Income was extrapolated using IRS data for individual zip codes. Median income was determined as 48,486 USD based on the data for Alabama US Census 2014–2018. Income was grouped into tertiles.
Statistical Analysis: The mean of the composite score was reported. Statistical analysis was performed using Stata 16.0 (StataCorp). Analysis was performed using either an ordered logistic regression for univariable or mixed model ordered logistic regression multivariable analysis.
3. Results
344 surveys were returned with a response rate of 64.3%. The median age of participants was 61 years (IQR 47–68) and 70% of respondents (n = 219) were women. The majority of patients were White (n = 214, 67.3%). The highest education level among patients in the study demonstrated considerable variation; the most common answers were high school with diploma (n = 97, 29.8%), college with degree (n = 93, 28.5%), and college without degree (n = 81, 24.9%). Fifteen participants (4.6%) attended high school but did not complete it, one participant did not attend high school and a number were graduate degree holders (n = 39, 12%). The majority of patients had smart phones, with the most common devices being iPhones (n = 171, 52.9%) and Android devices (n = 123, 38.1%). Sixteen participants (5%) reported non-smart phone ownership and some patients did not know the type of cell phone they owned (n = 10, 3.1%). The most common means of internet access were cable-based (n = 174, 52.1%), Digital Subscriber Line (DSL) (n = 50, 15%), and cell phone (n = 35, 10.5%). Of note, 24 patients (7.2%) did not have any access to internet at home (Table 3 ).
Table 3.
Characteristics of included patients.
| Participants (n = 344) | |
|---|---|
| Median age (years) [IQR] | 61 (47–68) |
| Sex | |
| Male | 94 (30%) |
| Female | 219 (70%) |
| Race | |
| White | 214 (67.3%) |
| Black | 81 (25.5%) |
| Asian (Chinese or Asian Indian) | 8 (2.5%) |
| Native American | 5 (1.6%) |
| Other | 5 (1.6%) |
| Declined to answer | 5 (1.6) |
| Highest level of education | |
| Did not attend high school | 1 (0.3%) |
| High school without diploma | 15 (4.6%) |
| High school with diploma | 97 (29.8%) |
| College without degree | 81 (24.9%) |
| College degree | 93 (28.5%) |
| Graduate degree | 39 (12%) |
| Type of Cellphone | |
| iPhone | 171 (52.9%) |
| Android | 123 (38.1%) |
| Non-smart phone | 16 (5%) |
| Do not know | 10 (3.1%) |
| Decline to answer | 3 (0.9%) |
| Internet Access | |
| Cable Modem | 174 (52.1%) |
| Satellite | 15 (4.5%) |
| Fiber Optic | 14 (4.2%) |
| Digital Subscriber Line (DSL) | 50 (15.0%) |
| Dial-up Modem | 7 (2.1%) |
| Cell Phone | 35 (10.5%) |
| No internet at home | 24 (7.2%) |
| Decline to answer | 15 (4.5%) |
When comparing demographic factors to patient's health literacy in a multivariable analysis, education level, age, income, and gender were all predictive of health literacy. All other factors including race and type of internet access were not predictive (Table 4 ).
Table 4.
Multivariable ordinal logistic analysis predicting for health literacy.
| Variable | Coefficient | 95% CI | p-value | |
|---|---|---|---|---|
| Age | 0–40 | REF | ||
| 41–50 | 0.132 | −0.725–0.988 | 0.763 | |
| 51–60 | −0.276 | −1.06–0.511 | 0.491 | |
| 61–69 | −0.242 | −0.918–0.434 | 0.482 | |
| 70–79 | −0.635 | −1.41–0.413 | 0.109 | |
| ≥80 | −1.81 | −3.15–−0.484 | 0.008 | |
| Male | −0.687 | −1.21 to −0.162 | 0.010 | |
| Race | White | REF | ||
| Black | −0.326 | −0.852–0.201 | 0.226 | |
| Native American | −0.140 | −2.21–1.93 | 0.895 | |
| Asian Indian | 0.032 | −2.50–2.57 | 0.980 | |
| Chinese | −0.194 | −2.07–1.68 | 0.839 | |
| Prefer not to answer | −2.73 | −6.18–0.722 | 0.121 | |
| Other | −1.86 | −4.91–1.20 | 0.234 | |
| Education level | High school without diploma | REF | ||
| High School | −0.216 | −1.27–0.840 | 0.688 | |
| Some College | 1.21 | 0.097–2.32 | 0.033 | |
| College Degree | 1.40 | 0.261–2.53 | 0.016 | |
| Graduate degree | 1.97 | 0.758–3.19 | 0.001 | |
| Lack of broadband internet | −0.373 | −0.970–0.224 | 0.221 | |
| Cell Phone | Non-Smart phone/no phone | REF | ||
| Android | 0.464 | −0.359–1.29 | 0.269 | |
| iPhone | −0.595 | −2.48–1.29 | 0.536 | |
| Income | 1st Tertile | REF | ||
| 2nd Tertile | 0.525 | 0.034–1.02 | 0.036 | |
| 3rd Tertile | 1.15 | 0.107–2.42 | 0.043 | |
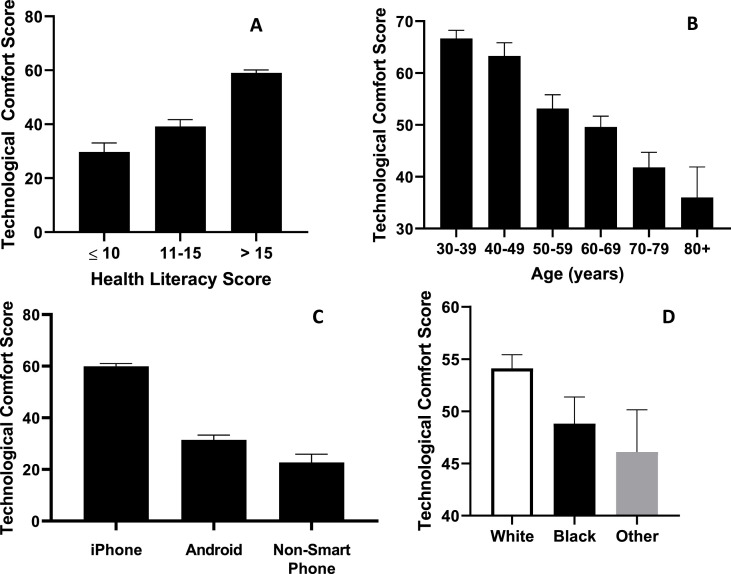
In univariable analysis, health literacy correlated with overall technologic comfort (p < 0.001, Fig. 1 A). Additionally, there were clear associations with patient age (p < 0.001, Fig. 1B), type of cell phones (p < 0.001, Fig. 1C), and race (p < 0.001, Fig. 1D). In multivariable mixed model ordinal logistic analysis (Table 5 ), increasing patient age (51–60 years p = 0.006, 61–70 p < 0.001, 71–80 p<0.001, >80 p = 0.023), male gender (p < 0.001), Black race (p = 0.044), Native American race (p = 0.028), and lack of home broadband internet access (p < 0.001) were all associated with decreasing technological comfort score. However, increased health literacy (score 12–16 p = 0.033, score 17 p < 0.001), Chinese race (p = 0.006), and iPhone ownership (Android p = 0.06, iPhone p < 0.001) were predictive of improved technological comfort. Interestingly, neither income level (2nd tertile p = 0.194, 3rd tertile p = 0.378) nor education level (high school diploma p = 0.395, graduate degree p = 0.327) were predictive of technological comfort.
Fig. 1.
Effect of different factors on technological comfort.
Table 5.
Multivariable ordinal logistic analysis of technological comfort scores.
| Variable | Coefficient | 95% CI | p-value | |
|---|---|---|---|---|
| Age | 0–40 | REF | ||
| 41–50 | −0.427 | −1.46–0.610 | 0.419 | |
| 51–60 | −1.20 | −2.06–−0.342 | 0.006 | |
| 61–69 | −2.10 | −2.89–−1.32 | <0.001 | |
| 70–79 | −2.40 | −3.29–−1.51 | <0.001 | |
| ≥80 | −1.65 | −3.08–−0.232 | 0.023 | |
| Male | −1.35 | −1.87–−0.777 | <0.001 | |
| Race | White | REF | ||
| Black | −0.578 | −1.14–−0.015 | 0.044 | |
| Native American | −2.01 | −3.80–−0.215 | 0.028 | |
| Asian Indian | −1.42 | −3.35–0.497 | 0.146 | |
| Chinese | 4.09 | 1.15–7.03 | 0.006 | |
| Prefer not to answer | −0.752 | −3.48–1.98 | 0.589 | |
| Other | −0.175 | −2.78–2.43 | 0.895 | |
| Education level | High school without diploma | REF | ||
| High School | −0.495 | −1.64–0.645 | 0.395 | |
| Some College | 1.04 | −0.190–2.26 | 0.098 | |
| College Degree | 0.718 | −0.510–1.95 | 0.252 | |
| Graduate degree | 0.670 | −0.671–2.01 | 0.327 | |
| Lack of broadband internet | −1.51 | −2.14–−0.883 | <0.001 | |
| Health literacy score | <11 | REF | ||
| 12–16 | 0.963 | 0.675–1.20 | 0.033 | |
| ≥17 | 1.92 | 1.03–2.81 | <0.001 | |
| Cell Phone | Non Smart phone/no phone | REF | ||
| Android | 0.746 | −1.52–0.033 | 0.060 | |
| iPhone | 1.59 | 0.971–2.20 | <0.001 | |
| Income | 1st Tertile | REF | ||
| 2nd Tertile | −0.334 | −0.837–0.169 | 0.194 | |
| 3rd Tertile | 0.507 | −0.621–1.64 | 0.378 | |
4. Discussion
Cancer patients form a large population that require regular outpatient care and follow up. At our institution over 20,000 cancer patients are seen annually in the outpatient setting. In light of the shift towards providing more care through telehealth, it is important to ensure that patients are able to access this care equally. Our study shows that our included cancer population was older (median age 61 years) and predominantly female (70%). Age did not demonstrate any correlation with health literacy until reaching the oldest patients, and race did not predict health literacy in our population. Male gender was associated with decreased health literacy. This is the first study to evaluate the variables that may predict technological comfort in a diverse patient population. We found clear disparities among our cancer patients with respect to technological comfort. Specifically, advanced age, male gender, Black and Native American races, poor health literacy, and the lack home internet access all correlate to decreased technological comfort, which may limit use of telehealth technology. Although the results are somewhat expected based on anecdotal suspicion, this is the first study to demonstrate the factors that impact technological comfort and its association with health literacy. Additionally, we received a response rate greater than 60% which we believe is excellent and representative for a study of this type.
Poor health literacy has been noted to be more prevalent in specific populations, including low income and racial or ethnic minorities.12 While income correlated with health literacy in our population; race did not. Furthermore, studies focusing on health literacy in the population show that between a half and a third of patients in the US struggle with understanding and subsequently applying health information.12 , 16 Clear communication between the patient and healthcare provider is imperative to the mutual understanding of the patient's treatment plan, in what can be a complex and confusing process. Even prior to the initiation of the widespread use of telemedicine, the identification of patients with low health literacy is critical to ensure the joint understanding of their care plan.
As this is the first study focusing on factors that predict technological comfort in a diverse population, we do not have data for comparison. Although our score is an indicator of technological comfort, it is not possible to define what score would predict an ability to use telehealth successfully. Additionally, we believe that comfort is only one aspect of telehealth literacy. Patient knowledge and application of technology is also an important aspect that will act as an indicator for telehealth uptake by patients (which is not able to be addressed in this study). Further studies and addition of new validated tools may expand our ability to study this area of health services research and allow us to create more predictive models for determination of at-risk patients.
The sharp rise of telehealth across the US over the past year has been well documented, with one institution reporting an increase in telehealth use of over 2000% over just 24 days.17 While these numbers are exciting, it is important to ensure telehealth is accessible to underserved populations as well. Our study found that those patient with the lowest health literacy were also most likely to report lower technological comfort and we conclude that they are less likely to engage with telemedicine. Poor health literacy has already been shown to correlate with worse patient outcomes.13 Additionally, there is evidence to show that patients with lower health literacy are less likely to trust physicians and health systems.18 This adds another complicating factor to establishing a strong patient-physician relationship, which may already be disadvantaged by the lack of in-person communication. As a consequence, patient engagement may be difficult, and patients lost to follow-up may increase. A large disparity in the use of the internet to obtain health information has previously been shown to exist between patients with proficient health literacy (85% of patients) and those with below basic health literacy (19% of patients).16 There are also concerns that those patients with low health literacy may benefit less from telehealth resources.19 This myriad of factors highlights the potential negative impact patients with poor health literacy may suffer in a telehealth-driven healthcare encounter and in a model that uses this mode of healthcare delivery on a larger scale. Therefore, it is important that we recognize that patients in these populations are at increased risk, and we must engage them in alternative ways to allow the delivery of high-quality healthcare to all our patients. Although the technology currently utilized in telehealth has been present for some time and is largely seen as accessible and relatively user-friendly, this must not be taken for granted because certain populations may have decreased knowledge, comfort or access to necessary resources.
We anticipate that the shift to telehealth will likely have a durable effect in the future treatment of cancer patients. The advantages of telehealth are plentiful: allowing health systems to expand their catchment areas, reducing referral to consultation time, and reducing patient travel to unfamiliar locations. The nature of a cancer follow-up visits usually consists of the patient interview and review of any necessary surveillance imaging or bloodwork. This lends itself well to a telehealth approach and has been shown to be preferred by patients.10 Therefore, the identification of patients at-risk for being unable to engage with telehealth is not necessarily a short-term objective but may have long-term implications. Furthermore, as telehealth becomes more established it may permit expansion into rural communities and access to care that may not once have been possible. However, the ability to utilize telehealth requires access to a certain level of resources. In addition to poor internet access being associated with reduced technological comfort (p < 0.001); a significant number of patients in our study relied on their cellphone for internet access (n = 35, 10.5%) or did not have internet access at home (n = 24, 7.2%). Given current technologies, it would not be possible for these groups to access telehealth resources in an efficient and confidential manner. The increased difficulty and potential lack of privacy are factors that may deter an at-risk group from engaging with telemedicine. These patients may require alternative consultation methods (telephone calls) or may need to be identified as a group that requires prioritization for in-person visits. Plans for government bills to be passed to increase internet accessibility are underway. While this is a step in the right direction, we have demonstrated that accessibility is not the only factor that correlates with technological comfort and engagement.
Even though at-risk populations have been identified, we cannot “improve” a patient's health or digital literacy. Therefore, to combat the issue, robust and easily applicable solutions need to be implemented to allow appropriate engagement. It is important to ensure that the platforms on which these visits are being conducted are simple and streamlined and that access to them is an easy process. Additionally, the inclusion of accessibility features (large image of physician, voice control, text-to speech) may also allow patient to communicate in the manner in which they are most comfortable. Technical support should be available to patients (either with the incorporations of FAQs or a technician) both in the initial set-up phase and throughout return visits.20 As telehealth is expanded into more rural communities, research needs to continues to focus on the development and implementation of these tools. It's hoped that this will allow an improvement in communication and compliance in those with limited digital health literacy and allow the delivery of effective care. However, despite these interventions, a subset of the population will continue to struggle with the use of telehealth in its current form. It is imperative that these patients are identified, and alternatives are sought; whether that is a different telehealth format or prioritization of an in-person visit.
This study needs to be interpreted in the context of its limitations. Our survey was designed to focus on patients’ perceptions of technology comfort, it however does not necessarily translate to real-life abilities and knowledge. Additionally, all patients included in this study came to our institution for an in-person clinic visit. Telemedicine would potentially permit patients who could not travel to our institution improved access to care. Therefore, our study cohort may not be an accurate representation of the patients most in need of technological engagement. Additionally, when this survey was taken, a small proportion of patients were already utilizing telehealth services. It is possible that this population may have been more telehealth literate and not included in our sample. Finally, due to the anonymous nature of the survey, we were unable to subdivide groups based on the specific oncology clinic that they attended.
As telehealth becomes more commonplace in our healthcare system, we hope to determine in future studies if disparities exist in our patients who have participated in telemedicine visits. Correlating such findings with those of this study may elucidate significant areas in telemedicine which require refinement. This will be a complex process requiring investment from government, medical institutions, physicians, and patients but has the potential to maximize the generalizable potential benefit of telehealth in delivering high quality healthcare to the entire population.
5. Conclusion
As a shift toward increased telemedicine continues, it is important that we engage all patients that require service. In our study, lower technology comfort score was seen in older patients, males, Black and Native American individuals, those with poor health literacy, and lack of high-speed home internet access. Our study demonstrates that cancer patients that would likely benefit the most from telehealth may be at risk of not engaging due to low comfort with the associated technologies. It is important to identify these at-risk patients and assist them in utilizing telehealth services.
Disclosures
The authors have nothing to disclose.
Appendix 1. Survey
References
- 1.World Health Organization . 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19.https://www.who.int/dg/speeches/detail/wh o-director-general-s-opening-remarks-at-the-media-brief ing-on-covid-19-11-march-2020 [Google Scholar]
- 2.Public Health England. Coronavirus (COVID-19): what is social distancing?,. https://publichealthmatters.blog. gov.uk/2020/03/04/coronavirus-covid-19-what-is-social- distancing/.
- 3.Caffery L.J., Farjian M., Smith A.C. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. 2016;22:504–512. doi: 10.1177/1357633X16670495. [DOI] [PubMed] [Google Scholar]
- 4.Peddle K. Telehealth in context: socio-technical barriers to telehealth use in labrador, Canada. Comput Support Coop Work. 2007;16:595–614. [Google Scholar]
- 5.Wade V., Soar J., Gray L. Uptake of telehealth services funded by Medicare in Australia. Aust Health Rev. 2014;38:528–532. doi: 10.1071/AH14090. [DOI] [PubMed] [Google Scholar]
- 6.Smith A.C., Thomas E., Snoswell C.L., et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26:309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao J., Zhang Z., Guo H., et al. E-health in China: challenges, initial directions, and experience. Telemed J e Health. 2010;16:344–349. doi: 10.1089/tmj.2009.0076. [DOI] [PubMed] [Google Scholar]
- 8.Doarn C.R., Latifi R., Poropatich R.K., et al. Development and validation of telemedicine for disaster response: the north Atlantic treaty organization multinational system. Telemed J e Health. 2018;24:657–668. doi: 10.1089/tmj.2017.0237. [DOI] [PubMed] [Google Scholar]
- 9.Caffery L.J., Bradford N.K., Smith A.C., Langbecker D. How telehealth facilitates the provision of culturally appropriate healthcare for Indigenous Australians. J Telemed Telecare. 2018;24:676–682. doi: 10.1177/1357633X18795764. [DOI] [PubMed] [Google Scholar]
- 10.Onuma A.E., Palmer Kelly E., Chakedis J., et al. Patient preferences on the use of technology in cancer surveillance after curative surgery: a cross-sectional analysis. Surgery. 2019;165:782–788. doi: 10.1016/j.surg.2018.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ratzen S., Parker R. 2000. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. [Google Scholar]
- 12.Health Literacy . (National Academies Press (US); 2004. A Prescription to End Confusion. [DOI] [PubMed] [Google Scholar]
- 13.Chisolm D.J., Hardin D.S., McCoy K.S., Johnson L.D., McAlearney A.S., Gardner W. Health literacy and willingness to use online health information by teens with asthma and diabetes. Telemed J e Health. 2011;17:676–682. doi: 10.1089/tmj.2011.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mackert M., Mabry-Flynn A., Champlin S., Donovan E.E., Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18:e264. doi: 10.2196/jmir.6349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haun J., Luther S., Dodd V., Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun. 2012;17(3):141–159. doi: 10.1080/10810730.2012.712615. [DOI] [PubMed] [Google Scholar]
- 16.Kutner M., Greenberg E., Jin Y., Paulsen C. U.S. Department of Education; 2006. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy.https://nces.ed.gov/pubs2006/2006483.pdf National Center for Education Statistics website: [Google Scholar]
- 17.Contreras C.M., Metzger G.A., Beane J.D., Dedhia P.H., Ejaz A., Pawlik T.M. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai T.-I., Yu W.-R., Lee S.-Y.D. Is health literacy associated with greater medical care trust? Int J Qual Health Care. 2018;30:514–519. doi: 10.1093/intqhc/mzy043. [DOI] [PubMed] [Google Scholar]
- 19.Birru M.S., Monaco V.M., Charles L., et al. Internet usage by low-literacy adults seeking health information: an observational analysis. J Med Internet Res. 2004;6:e25. doi: 10.2196/jmir.6.3.e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeNamur L. How technology is improving access and empowering older adults to embrace telehealth. https://www.forbes.com/sites/jumio/2020/10/06/how-technology-is-improving-access-and-empowering-older-adults-to-embrace-telehealth/?sh=23bb10d68588 Forbes.com.