Abstract
Objectives:
Expanded access to buprenorphine induction, including via emergency departments, increases the likelihood of treatment engagement for patients with opioid use disorder (OUD). However, longer-term retention among these patients remains a challenge. In this study, we aimed to identify barriers to engaging and retaining patients with OUD in care and additional services that might improve retention.
Methods:
We surveyed counselors at an urban safety net addictions treatment clinic.
Results:
Twenty-five of 27 (93%) eligible counselors responded. Counselors described patients who were homeless, had no prior treatment history, or lacked health insurance as hardest to retain in treatment. Housing assistance, residential treatment placement, regular access to a phone, and mental health services were thought to be most beneficial for improving retention. Respondents most often reported that screening for services should happen at intake, and almost all respondents agreed that “retention of patients receiving treatment for OUD would improve with a dedicated case manager and/or more coordinated case management services.”
Conclusions:
Engagement in OUD treatment would be improved with interventions to mitigate the significant social and psychiatric comorbidities of addiction. Community- and emergency department-initiated buprenorphine is a promising intervention whose full promise cannot be realized without interventions to improve treatment retention.
Keywords: access to care, buprenorphine, emergency department, homelessness, opioid use disorder, safety net
Expanding access to buprenorphine treatment for opioid use disorder (OUD) is a national public health priority.1,2 Although there has been much focus on improving access to buprenorphine treatment, less research has examined how to engage patients in treatment beyond the initiation of treatment. The use of buprenorphine in emergency departments (EDs) illustrates these challenges.3,4 Although ED-initiated buprenorphine treatment increases the likelihood of a patient accessing treatment, treatment retention decreases over time. For example, in the landmark trial of ED-initiated buprenorphine for OUD treatment, 74% of patients who were inducted on buprenorphine were engaged in treatment at 30 days, whereas only 55% of patients remained in treatment by 6 months.5 This latter rate is comparable to that of the study’s comparison groups and consistent with community retention rates.5,6
Thus, the full benefits of ED-based buprenorphine induction will be unrealized without better engaging patients in subsequent treatment. Generally, barriers to retention and treatment adherence among patients with OUD include treatment cost, homelessness, comorbid substance use and mental illness, and other sociodemographic determinants of health such as minority race.7,8 Co-occurring substance use and psychiatric disorders are associated more specifically with non-adherence to buprenorphine.9,10 Prior studies of ED-initiated buprenorphine specifically have not tested treatments for mitigating these barriers.3
We surveyed addiction counselors at a specialized addiction treatment program in a safety-net health system to identify barriers and opportunities to improve treatment engagement among patients starting OUD treatment. These data were collected to develop an intervention to enhance retention in treatment after ED-based buprenorphine induction.
METHODS
Study participants were addiction counselors at Denver Health’s Outpatient Behavioral Health Services clinic. Counselors include licensed professional counselors, social workers, and addictions counselors. This clinic provides multimodal treatment for all substance use disorders. Methadone maintenance, buprenorphine, long-acting injectable naltrexone, contingency management, and integrated medical care are available. The clinic had approximately 900 patients at the time of the study. Patients with less severe illness are referred to community-based primary care clinics with integrated addiction counseling. No formal case management services are provided at this clinic. This health system treats about half of all patients in Denver who have an OUD diagnosis.6 Other than the clinic itself, the ED is the most common site of buprenorphine induction for new patients.
All clinic counselors were sent an email that invited them to complete a brief web-based survey.11 The survey was created from content to explore existing barriers to care identified among patients with human immunodeficiency virus (HIV).12,13 Counselors and physicians from outside the study population provided feedback to inform the survey development. The full survey is included as Appendix A, http://links.lww.com/JAM/A318. The survey did not direct respondents to consider barriers for patients from a particular induction site. Descriptive statistics were calculated. There were insufficient qualitative data for thematic analyses, but exemplative quotations supplement these findings. This study was approved by the local institutional review board.
RESULTS
Twenty-five of 27 eligible counselors (93%) completed the survey. No data were missing from returned surveys. Counselors were asked to rate 5 different patient attributes associated with difficulty engaging in treatment on a 5-point Likert scale (with 1 being “extremely difficult to stay engaged” and 5 being the “easiest to stay engaged”). Patients who were homeless were most frequently rated as hardest to retain in treatment (76% of counselors described these patients as a 1 or 2), although patients new to treatment (56%) and without insurance (48%) were also rated as hard to retain. Fewer counselors rated patients who had missed a recent appointment (40%) or were unemployed (16%) as difficult to engage in treatment. One counselor commented that patients recently released from “jail with few resources” posed particular challenges to engagement.
Counselors were asked to identify the top 5 services that would be most helpful to retain patients from a list of options. Counselors were also asked to indicate which of these services they had provided to a patient. Respondents’ perceptions of the importance of services for treatment retention are shown in Figure 1 along with how often these services were provided by counselors. Twenty-four respondents (96%) provided at least one of these services for a patient.
FIGURE 1.
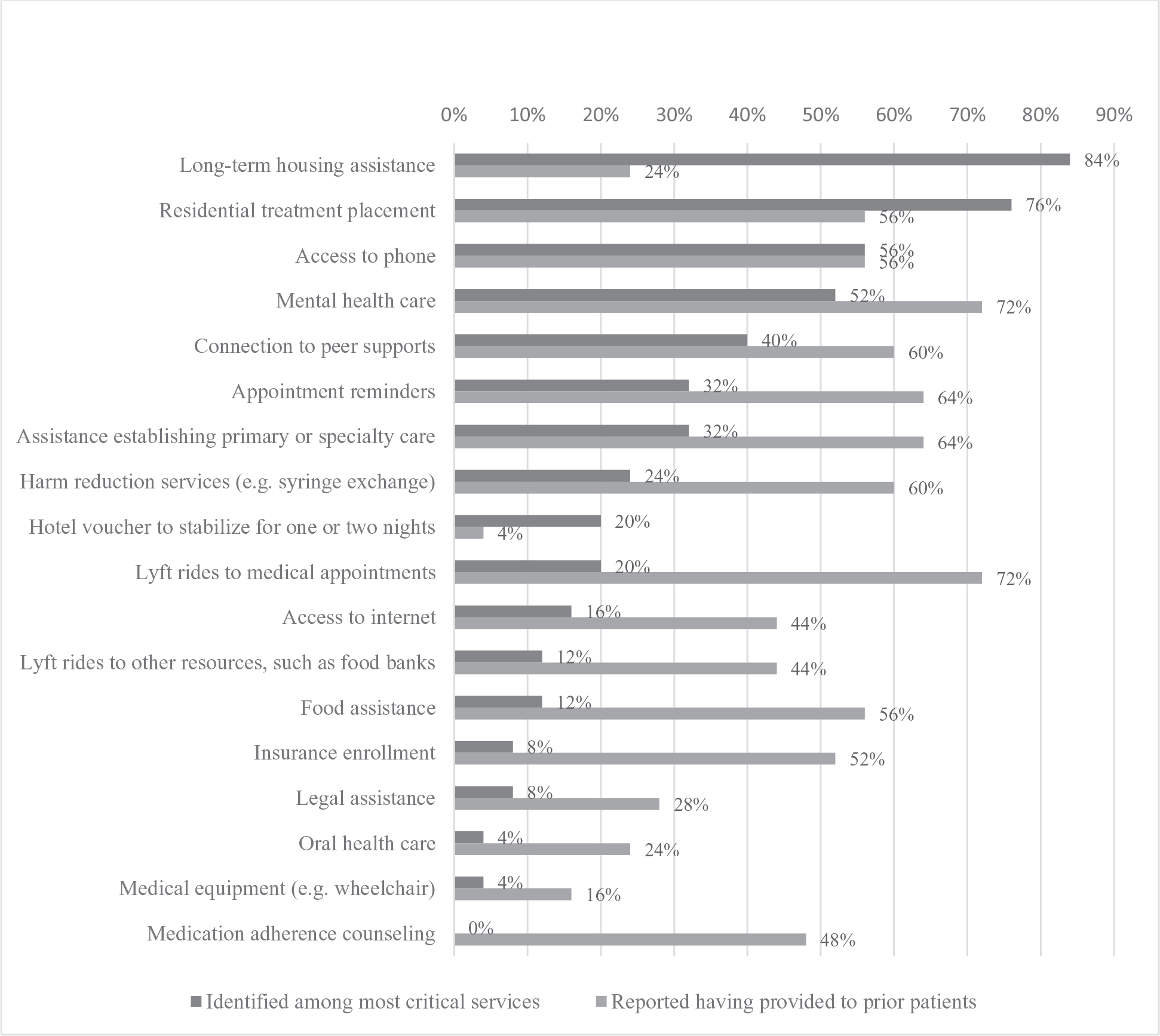
Addiction counselors’ perceptions of services needed and provided for patients with opioid use disorder.
We also sought to understand the best workflow for conducting a needs assessment. The plurality of respondents (44%) felt that screening for the need for these services was best done systematically at intake; 24% answered that screening should happen whenever needed, and 16% felt screening should happen after a period of initial stabilization in treatment. One counselor shared, “At intake makes the most sense but there is already so much for patients and counselors and providers to do at that time. Maybe after initial stabilization would be more appropriate even if that meant some early interventions would be missed [sic].” Counselors reported that either a separate case manager (48%) or the counselors themselves (40%) were best-suited to completing screening. Ninety-two percent of respondents agreed that “retention of patients receiving treatment for OUD would improve with a dedicated case manager and/or more coordinated case management services.”
DISCUSSION
These findings will guide strategies to improve treatment engagement among patients with OUD. Among the most significant barriers to retention in OUD treatment were the need for housing assistance, residential addiction treatment, phone access, and additional mental health care. Improving engagement in addiction treatment after buprenorphine induction in the community requires supportive interventions to mitigate these barriers.
There remains a significant gap in what counselors report patients require to remain engaged in treatment and what services counselors routinely provide. For instance, 84% of counselors felt housing assistance was necessary, but only 24% reported providing this service This discrepancy likely reflects a lack of expertise on the part of the clinical team and the health system’s current capacity to address social barriers impacting recovery. Almost all counselors reported providing social services as part of care, and almost all agreed that specialized case management would improve treatment retention.
One way to address this mismatch is by adapting existing treatment engagement models to the treatment of OUDs. One promising option is the linkage-to-care model for patients with HIV. Linkage-to-care comprises active case management, proactive engagement, and material support to reduce the risk of treatment dropout in spite of social barriers to accessing care; linkage-to-care improves HIV treatment engagement after ED referral.14 The current study identifies several specific needs for patients entering OUD treatment that might be addressed through such a model.
Limitations of this work include generalizability as data were collected at a single site and the lack of description of respondents. Perceived barriers may differ from those reported by patients, and some barriers may reflect particular issues in this locality, such as affordable housing. These findings are not specific to a specific treatment initiation site although our team’s goal was specifically to improve engagement after buprenorphine induction in the ED.
CONCLUSIONS
Improving access to evidence-based treatments, such as ED-initiated buprenorphine, is vital but insufficient for addressing the opioid epidemic. The ongoing effectiveness of these treatments may be limited by patients’ significant social barriers to engaging in ongoing care. Fulfilling the promise of expanded access to addiction treatment requires clinicians and policymakers to address the detrimental impacts of homelessness, co-morbid psychiatric illness, and other social barriers to recovery.
Supplementary Material
Acknowledgments
Supported by the Centers for Disease Control and Prevention [Grant number R01CE003006 to Dr. Al-Tayyib]. This study’s use of Redcap is supported in part by NIH/NCRR Colorado CTSI Grant Number UL1 RR025780. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC or the US Department of Health and Human Services.
Footnotes
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.journaladdictionmedicine.com).
Contributor Information
Scott A. Simpson, Department of Behavioral Health Services, Denver Health and Hospital Authority, Denver, CO.
Melissa Hordes, Public Health Institute at Denver Health, Denver Health and Hospital Authority, Denver, CO.
Joshua Blum, Department of Behavioral Health Services, Denver Health and Hospital Authority, Denver, CO.
Deborah Rinehart, Center for Health Systems Research, Office of Research, Denver Health and Hospital Authority, Denver, CO.
Alia Al-Tayyib, Public Health Institute at Denver Health, Denver Health and Hospital Authority, Denver, CO; Center for Health Systems Research, Office of Research, Denver Health and Hospital Authority, Denver, CO.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. HHS releases new buprenorphine practice guidelines, expanding access to treatment for opioid use disorder. April 27, 2021. Updated April 27, 2021. Available at:https://www.samhsa.gov/newsroom/press-announcements/202104270930. Accessed October 22, 2021.
- 2.Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5): 358–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao SS, Dunham SI, Simpson SA. Prescribing buprenorphine for opioid use disorders in the ED: A review of best practices, barriers, and future directions. Open Access Emerg Med. 2020;12:261–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. Use of medication-assisted treatment in emergency departments. National Mental Health and Substance Use Policy Laboratory. 2021. Accessed May 17, 2021. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/pep21-pl-guide-5.pdf. [Google Scholar]
- 5.D’Onofrio G, Chawarski MC, O’Connor PG, et al. Emergency department-initiated buprenorphine for opioid dependence with continuation in primary care: Outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prieto JT, McEwen D, Davidson AJ, et al. Monitoring opioid addiction and treatment: Do you know if your population is engaged? Drug Alcohol Depend Sep. 2019;202:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Godersky ME, Saxon AJ, Merrill JO, et al. Provider and patient perspectives on barriers to buprenorphine adherence and the acceptability of video directly observed therapy to enhance adherence. Addict Sci Clin Pract. 2019;14(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ronquest NA, Willson TM, Montejano LB, et al. Relationship between buprenorphine adherence and relapse, health care utilization and costs in privately and publicly insured patients with opioid use disorder. Subst Abuse Rehabil. 2018;9:59–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montalvo C, Stankiewicz B, Brochier A, et al. Long-term retention in an outpatient behavioral health clinic with buprenorphine. Am J Addict. 2019;28(5):339–346. [DOI] [PubMed] [Google Scholar]
- 10.Litz M, Leslie D. The impact of mental health comorbidities on adherence to buprenorphine: A claims based analysis. Am J Addict. 2017;26(8): 859–863. [DOI] [PubMed] [Google Scholar]
- 11.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colorado Department of Public Health and Environment. Integrated care and prevention program HIV care and treatment standards of care [version May 1, 2017]. Available at: https://cdphe.colorado.gov/stihiv-funded-partner-policies. Accessed October 22, 2021.
- 13.Centers for Disease Control and Prevention. National HIV Behavioral Surveillance (NHBS). Updated October 13, 2021. Available at: https://www.cdc.gov/hiv/statistics/systems/nhbs/index.html. Accessed October 22, 2021.
- 14.Menon AA, Nganga-Good C, Martis M, et al. Linkage-to-care methods and rates in U.S. emergency department-based HIV testing programs: A systematic literature review brief report. Acad Emerg Med. 2016;23(7): 835–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


