Abstract
OBJECTIVES
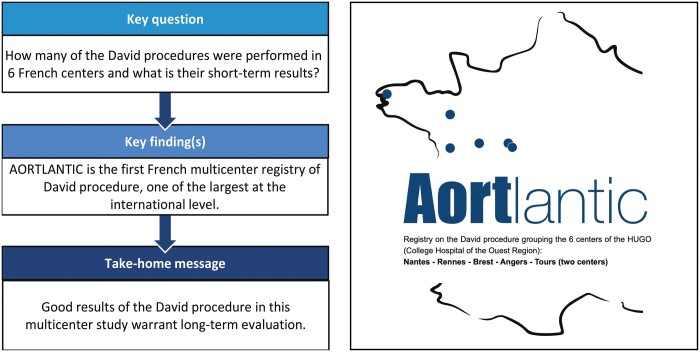
Aortic root aneurysms often affect younger patients in whom valve-sparing surgery is challenging. Among current techniques, aortic valve-sparing root replacement described by Tirone David has shown encouraging results. The AORTLANTIC registry was instituted for a multicentre long-term evaluation of this procedure. The current initial study evaluates the hospital outcomes of the procedure.
METHODS
This is a retrospective study of patients operated between 1 January 2004 and 31 December 2020 in 6 hospitals in western France. All study data were recorded in the national digital database of the French Society of Cardiac Surgery: EPICARD.
RESULTS
A total of 524 consecutive patients with a mean age of 53 (15.1) years underwent surgery. 13% (n = 68) of patients presented with acute aortic dissection, 16.5% (n = 86) had associated connective tissue pathology and 7.3% (n = 37) had bicuspid aortic valves. Preoperative aortic regurgitation (AR) ≥2/4 was present in 65.3% (n = 341) of patients. Aortic valvuloplasty was required in 18.6% (n = 95) of patients. At discharge, 92.8% (n = 461) of patients had no or 1/4 AR. The stroke rate was 1.9% (n = 10). Intra-hospital mortality was 1.9% (n = 10).
CONCLUSIONS
The AORTLANTIC registry includes 6 centres in western France with >500 patients. Despite numerous complex cases (acute aortic dissections, bicuspid aortic valves, preoperative AR), aortic valve-sparing root replacement has a low intra-hospital mortality. The initial encouraging results of this multicentre study warrant further long-term evaluation by future studies.
Keywords: Valve-sparing aortic root replacement, David procedure, Acute aortic dissection, Aortic regurgitation, Bicuspid aortic valve, French multicentric registry
Aortic aneurysm pathology is a silent disease that can affect young people, especially Marfan patients.
INTRODUCTION
Aortic aneurysm pathology is a silent disease that can affect young people, especially Marfan patients. It can develop into a serious complication, acute aortic dissection (AAD), with an in-hospital mortality rate of 57% [1]. Originally, surgical treatment of aortic root aneurysms consisted of replacing the ascending aorta and aortic valve with a prosthetic valve. The challenge of valve-sparing aortic root replacement (VSARR) is to replace the aortic root ± ascending aorta while preserving the native aortic valve, thereby avoiding the need for a biological or mechanical valve prosthesis. VSARR was described in 1983 by Yacoub et al. [2], ‘the remodelling procedure’, and then in 1992 by David and Feindel [3], ‘the reimplantation procedure’.
To date, the long-term results of the reimplantation technique described by David have been evaluated almost exclusively by the single-centre studies: David in Toronto (n = 333), 10-year average follow-up [4]; De Paulis in Rome (n = 124), 5-year average follow-up [5]; El Khoury in Brussels (n = 440 and 303), 5- and 6-year average follow-up [6, 7]; and Beckmann in Hannover (n = 732), 10-year average follow-up [8]. Other large series with >200 patients included multiple techniques (remodelling and reimplantation) and/or had a follow-up period of no more than 5 years [9–12]. The French AORTLANTIC registry is a multicentre registry focused on the reimplantation technique, instituted for ongoing, long-term follow-up. The aim of this initial study is to evaluate the hospital-based outcomes of the AORTLANTIC registry.
MATERIALS AND METHODS
Patients
Between 2004 and 2020, all patients underwent VSARR by the reimplantation technique at 6 centres belonging to the HUGO group (acronym of University Hospital at Ouest Region), a network of university hospitals collaborating in care, teaching and research (Table 1).
Table 1:
Repair of the patients of the AORTLANTIC registry within the 6 centres
| Centre | N (%) |
|---|---|
| Angers University Hospital | 88 (17) |
| Brest University Hospital | 57 (11) |
| Nantes University Hospital | 187 (36) |
| Rennes University Hospital | 152 (29) |
| Tours Clinic (St Gatien) | 28 (5) |
| Tours University Hospital | 12 (2) |
Surgical technique
All patients underwent surgery according to the reimplantation procedure described by David [3, 13] and El Khoury [14]. All procedures were performed by sternotomy. The type of cardioplegia and choice of vascular graft (straight or Valsalva graft) were as per the surgeon's discretion. To decide on the feasibility of conservative surgery and performing a valvuloplasty, we consider the preoperative ultrasound data as well as the peroperative findings: calcification, large fenestration, and presence of prolapse. For this purpose, most surgeons measure the geometric height using the technique described by Schäefers [15]. Some surgeons limit themselves to an eye-balling, while others use the caliper.
After ultrasound evaluation, if there was an aortic regurgitation (AR) ≥2 or a valve prolapse, a second cross-clamp is usually performed before adding a valvuloplasty or to opt for a valve replacement.
Inclusion/no-inclusion criteria
All patients who underwent VSARR with the ‘reimplantation procedure’ between 1 January 2004 and 31 December 2020 in the 6 adult cardiac surgery centres: Nantes, Rennes, Brest, Angers and Tours (2 centres) were included, without age limit. The no-inclusion criteria were redo procedure and remodelling procedure. It is a per-protocol study, only patients who had valve sparing are included. A stratified analysis in the periods 2005–2009, 2010–2014, 2015–2019 and 2020 was performed to compare the evolution of indications and operative technique over the time. The result in the context or outside of AAD has been analysed.
Database
The AORTLANTIC registry is a retrospective study with prospective recording of the patients’ data. It is linked to the official national database (EPICARD) of the French Society of Thoracic and Cardiovascular Surgery, which is prospectively supplemented. For the AORTLANTIC registry, the missing data were retrospectively completed by clinical research technicians from the patients' medical records and the computer databases of each centre.
Ethics statement
This registry was approved by the ethics committee GNEDS (groupe nantais d'éthique dans le domaine de la santé) mandated by the CNIL (Commission Nationale de l'Informatique et des Libertés). This committee was approved this study (notice GNEDS 21-11-71). It was a study based on data, and the rule MR-004 of the CNIL does not require written or oral consent from the patient.
Statistical analyses
Quantitative data are expressed as mean (standard deviation) or median ± interquartile range according to their distribution. Parametric two-sided Chi-squared test was used. A P-value ≤0.05 was considered statistically significant. Statistical analyses were performed with the R software (v4.0.3).
RESULTS
Preoperative
Patient characteristics are listed in Table 2. The mean age of the cohort was 53 (15.1) years. Eighty-six patients (16.5%) have connective tissue diseases, including Marfan disease and 68 (13%) patients underwent surgery for AAD (Stanford classification type A). Preoperative AR ≥2 was described in 65.3% (n = 341) of patients.
Table 2:
Preoperative clinical and imagery characteristics of all patients
| Preoperative data | N = 524 |
|---|---|
| Mean age (years) | 53.1 [15.2] |
| Age range (years) | (14–83) |
| Men | 426 (81.3) |
| Body Surface Area | 2.0 [0.2] |
| Comorbidities | |
| Hypertension | 292 (55.7) |
| Hyperlipidaemia | 145 (27.7) |
| Connective tissue disorder, Marfan | 86 (16.5) |
| Atrial fibrillation | 46 (8.8) |
| Diabetes | 34 (6.5) |
| Chronic obstructive pulmonary disease | 15 (2.9) |
| Peripheral vascular disease symptomatic or operated | 8 (1.5) |
| Pacemaker | 4 (0.8) |
| Renal failure on hemodialysis | 1 (0.2) |
| Previous cardiac surgery | 12 (2.3) |
| Type A acute aortic dissection | 68 (13) |
| Timing of surgery: urgent/emergency | 80 (15.3) |
| New York Heart Association functional class | |
| I | 291 (55.5) |
| II | 164 (31.3) |
| III | 50 (9.5) |
| IV | 19 (3.6) |
| LVEF | 61.2 [7.9] |
| LVEF >50% | 463 (88.7) |
| LVEF 30–50% | 56 (10.7) |
| LVEF <30% | 3 (0.6) |
| Mean LVEDD (mm) | 57.8 [8.2] |
| Grade of aortic regurgitation | |
| None | 80 (15.3) |
| 1 | 101 (19.3) |
| 2 | 147 (28.2) |
| 3 | 128 (24.5) |
| 4 | 66 (12.6) |
| Bicuspid aortic valve | 37 (7.3) |
| Type 0 | 12 (36.4) |
| Type 1 | 21 (63.6) |
| Mitral regurgitation, grade ≥2+ | 49 (9.3) |
| Sinus of Valsalva, mean dimension (mm) | 51.5 [7.6] |
| Ascending aorta, mean dimension (mm) | 47 [11.4] |
Values are expressed as mean [SD] or frequency (%).
LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; SD: standard deviation.
Perioperative
Perioperative data are given in Table 3. The graft used was neo-sinus in 83.1% (n = 432) of cases, including Gelweave™ (VASCUTEK Ltd., Renfrewshire, Scotland, UK) in 69% (n = 359) and Cardioroot™ (MAQUET Cardiovascular LLC, USA) in 14% (n = 73). The most commonly used vascular graft sizes were 28 (31%, n = 161), 30 (29.7%, n = 154) and 32 (25.8%, n = 134).
Table 3:
Perioperative data
| Perioperative data | N = 524 |
|---|---|
| Graft diameter (mm) | 30 |
| Type of graft | |
| Valsalva graft | 432 (83.1) |
| Gelweave™ (VASCUTEK) | 359 (83.1) |
| Cardioroot™ (MAQUET) | 73 (16.9) |
| Straight graft | 88 (16.9) |
| Cusp repair | 95 (18.6) |
| Central plicating stitches | 63 (66.3) |
| Resuspension of the commissures | 20 (21.1) |
| Running suture of Goretex (free edge) | 6 (6.3) |
| Cusp resection | 3 (3.2) |
| Decalcification | 2 (2.1) |
| Patch reconstruction | 1 (1.1) |
| Second aortic cross-clamp for regurgitation | 14 (2.8) |
| Combined operation | 184 (35.1) |
| Aortic arch intervention | 91 (17.4) |
| Coronary artery bypass graft | 39 (7.4) |
| Maze procedure | 26 (5) |
| Mitral valve repair | 24 (4.6) |
| Atrial septal defect closure | 10 (1.9) |
| Tricuspid valve repair | 9 (1.7) |
| Septal myectomy | 2 (0.4) |
| Pulmonary valve repair | 2 (0.4) |
| Cardiopulmonary bypass time (min) | 200.8 [64] |
| VSARR isolated | 182.7 [54.5] |
| Combined operation | 234.2 [66.8] |
| Aortic cross-clamp time (min) | 164.3 [43.7] |
| VSARR isolated | 151.2 [34.1] |
| Combined operation | 188.4 [49.0] |
Values are expressed as mean [SD] or frequency (%).
VSARR: valve-sparing aortic root replacement; SD: standard deviation.
Cusp repair was performed in 95 patients (18.6%), 45.9% for bicuspid aortic valve (BAV) and 16.9% for tricuspid valves (P < 0.001). For the periods 2005–2009, 2010–2014, 2015–2019 and 2020, the valvuloplasty rates were 14.4%, 18%, 20.6% and 24.4%, respectively. In these same periods, between 2005 and 2019, the rates of BAV in our cohort were 8.5%, 8.4% and 7.3%. VSARR was isolated in 318 patients (61.7%).
Postoperative
Postoperative data are shown in Table 4. Fifty-eight patients required re-exploration for bleeding (11.1%) of whom 10 underwent surgery for AAD and 27 combined procedures.
Table 4:
Early postoperative outcome
| Postoperative data | All patients, n = 524 | Acute dissection, n = 68 | Others, n = 456 |
|---|---|---|---|
| Early complication | |||
| Patient requiring ≥1 transfusion | 250 (47.8) | 49 (72.1) | 201 (44.2) |
| Atrial fibrillation with AC at discharge | 111 (21.2) | 7 (10.3) | 104 (22.8) |
| Re-exploration for bleeding | 58 (11.1) | 10 (14.7) | 48 (10.5) |
| Prolonged ventilation ≥24 h | 47 (9.0) | 15 (22.1) | 32 (7.0) |
| Bronchopulmonary infection | 46 (8.8) | 14 (20.6) | 32 (7.0) |
| Pacemaker | 24 (4.6) | 3 (4.4) | 21 (4.6) |
| Renal failure with need for haemodialysis | 20 (3.8) | 8 (11.8) | 12 (2.6) |
| Sternal infection or mediastinitis | 11 (2.1) | 3 (4.4) | 8 (1.8) |
| Stroke | 10 (1.9) | 2 (2.9) | 8 (1.8) |
| CPA with need for ECLS | 7 (1.3) | 3 (4.4) | 4 (0.9) |
| Mesenteric infarction | 2 (0.4) | 1 (1.5) | 1 (0.2) |
| Early reintervention (before discharge) | 91 (17.4) | 23 (33.8) | 68 (14.9) |
| With cardiopulmonary bypass | 7 (1.3) | 2 (2.9) | 5 (1.1) |
| Reintervention for aortic replacement | 4 (0.8) | 1 (1.5) | 3 (0.7) |
| Grade of aortic regurgitation at discharge | |||
| None | 232 (46.6) | 32 (51.6) | 200 (45.9) |
| 1 | 229 (46) | 25 (40.3) | 204 (46.8) |
| Central/eccentric (missing data) | 126/72 (31) | 14/6 (5) | 112/66 (26) |
| 2 | 36 (7.2) | 4 (6.5) | 32 (7.3) |
| Central/eccentric (missing data) | 10/23 (3) | 2/1 (1) | 8/22 (2) |
| 3 | 0 | 0 | 0 |
| 4 | 0 | 0 | 0 |
| Death during hospitalization | 10 (1.9) | 6 (8.8) | 4 (0.9) |
Values are presented as frequencies (%).
AC: anticoagulation; CPA: cardiorespiratory arrest; ECLS: extracorporeal life support.
At discharge, 504 (96.2%) patients had postoperative transthoracic echocardiography with a mean left ventricular ejection fraction of 57 (9)% and left ventricular end-diastolic diameter of 52 (8) mm. No AR or grade 1 was detected in 93% of patients (n = 461). Of the 36 patients with AR grade 2, 70% (n = 23) had an eccentric jet. No patients had AR grade 3 or 4. The mean transvalvular aortic gradient at discharge was 6 (3) mmHg.
Ten patients (1.9%) died during hospitalization, of whom 6 had undergone surgery for AAD. Of the 7 patients requiring extracorporeal life support, 3 (42.9%) died during hospitalization.
Early reintervention
Seven patients (1.3%) required a second procedure with cardiopulmonary bypass (CPB) before discharge: 4 patients (0.8%) because of persistent AR ≥2; in 3 of them, the aortic valve was replaced with a mechanical prosthesis (patients aged 47, 48 and 63 years) and in 1 with a bioprosthesis (65-year-old patient). The other 3 reinterventions with CPB were (i) emergency coronary bypass surgery (AAD extending to the ostium of the left coronary artery), (ii) mitral valve replacement and (iii) surgical embolectomy for massive pulmonary embolism.
DISCUSSION
Long-term data on aortic root surgery described by David are limited to a few single-centre cohorts [4–9]. The AORTLANTIC registry proposes a regional and multicentre French long-term evaluation of this technique under the aegis of the French Society of Thoracic and Cardiovascular Surgery.
The AORTLANTIC registry includes 6 French cardiac surgery centres with a total of 524 patients, >80% of whom underwent Valsalva graft surgery. The main publications specifically addressing the results of this technique range from 303 to 440 patients [4, 6, 7]. A larger cohort was published by Kari et al. [10] included 1015 patients from 4 German centres, 14% of whom underwent surgery using the remodelling procedure and 86% of the procedures were performed with a straight graft. Recently, Beckmann et al. [8] published the results of a cohort of 732 patients with a mean follow-up of 10 years with >90% of straight graft.
Valve-sparing procedures are becoming increasingly important [4, 7, 16]. These techniques avoid the use of biological prosthetic valves with attendant risks of degeneration, or mechanical prostheses mandating lifelong anticoagulant treatment, especially relevant in young patients with connective tissue disease. The AORTLANTIC registry includes a cohort of patients with a mean age of 53 years, comparable to other cohorts associated with VSARR (46–53 years [4–10]), and 16.5% (n = 86) of patients with connective tissue disease vs 8–38% in the others published cohorts [4–10]. The BAV rate was 7.3% (n = 37), which seems lower compared to some publications where it is as high as 41.5% [4–6, 9, 10]. All patients have an aortic aneurysm with the root and/or ascending aorta at least 40 mm. Patients with an aneurysm between 40 and 50 mm have severe aortic insufficiency and/or connective tissue disorder.
Finally, the AORTLANTIC registry includes 68 patients (13%) who underwent surgery for AAD. This rate is higher than in other published series (2.9–8%) [4–7, 9]. Recently, Beckman's publication counts 20% of their population operated on in the context of AAD [8]. Publications especially focused on the results of the VSARR for AAD are limited to 50 patients with a maximum follow-up of 6 years [17–19]. The AORTLANTIC registry provides an opportunity to better evaluate the long-term mortality and the risk of reintervention with this technique for AAD.
The rate of aortic valvuloplasty is 19% (n = 95). This rate has gradually increased over the years, reflecting refinement of the surgical technique. De Kerchove et al. [20] also reported an increase in the proportion of valvuloplasty over the years. In our registry, valvuloplasty is performed more frequently on BAV than on tricuspid valves (45.9% vs 16.9%, P < 0.001). This difference is also found in the De Kerchove series (91% vs 38%, P < 0.001) [20].
The majority of patients included in our registry had AR grade ≥2 (65.3%, n = 341), which remained constant across the different periods between 2005 and 2019 (69.4%, 68%, 60.6% and 64.3%, respectively). The incidence of preoperative AR matches those of other cohorts: 60.1% in De Paulis et al. [5], 65.5% in Mastrobuoni et al. [6] and 66.6% in Tamer et al. [7]. This contrasts with a highly variable rate of aortic valvuloplasty of 6.4%, 72.7% and 55.4% in these 3 previous publications [5–7], respectively. The proportion of patients with AR <2 is relatively stable during these periods (30.6%, 32%, 39.4% and 35.7%, respectively). Aortic valvuloplasty was performed in 13.6% of these cases (n = 24). Tamer et al. reported an even higher rate with valvuloplasty performed in 36% of patients without preoperative AR [7]. The annuloplasty by suturing the vascular prosthesis proximally sub-annularly brings the aortic valve cusps closer together and can unmask valve prolapse [21]. This hypothesis explains the need for valvuloplasty without preoperative AR [6, 20].
The mean duration of CPB and aortic cross-clamping was 199 (62) and 163 (43) min, respectively. These durations are longer than those given in many other publications [4–10]. This difference is partly related to a high rate of concomitant surgery (35.1%), but probably also to a large number of surgeons with some heterogeneity in the experience of individual surgeons with this particular procedure.
At hospital discharge, 93% of patients (n = 461) had AR <2. Only a few studies report echocardiography data at discharge or during the first year. The series by David and Tamer report 99.7% and 93.7% of patients without AR ≥2, respectively [7, 9].
Four patients (0.8%) underwent a second operation with aortic valve replacement. This rate is slightly higher than that reported in published series: 0–0.3% [4, 6, 7, 9]. Of these 4 patients, 1 had been operated for AAD and 3 patients had grade 3 (n = 2) or grade 4 (n = 1) AR in preoperative.
Among the risk factors for long-term failure of the VSARR, Polain de Waroux et al. [22] found 2 significant criteria: persistence of prolapse and level of valve coaptation. Thus, the presence of AR ≥2 or eccentric regurgitant flow postoperatively is a major risk factor for long-term failure. In contrast, persistent minimal AR is acceptable, provided the regurgitant jet is central and there is a valve coaptation level of ≥4 mm [20, 22].
The rates of permanent pacemaker and stroke were consistent with those found in the literature: 4.6% (n = 24) vs 0–4.9% and 1.9% (n = 10) vs 0.5–2.4%, respectively [4–6]. Reexploration rates for bleeding (11.1%, n = 58) were similar to those published in the largest series [4–6] (8–12.2%). ExtraCorporeal Life Support was required in 7 patients. Four were operated outside of an AAD, among them 2 died. These were patients with combined surgery (mitral and bypass) with prolonged CPB (283 min on average, max 412 min).
Our complication rates are in the high range of the rates found in other series. This is probably partly related to the higher rate of AAD and/or of combined procedure (35.1%), compared to <25% in several series [5, 6]. Tamer's team had 33% combined surgery but did not report their early complication rate [7].
Although in-hospital results of the Bentall procedure are often limited to small cohorts, early complication rates related to stroke are comparable, with 1.5–2% [23, 24]. In contrast, Salmasi et al. found a higher incidence of conduction block with the Bentall procedure [25]. This is reflected in a higher rate of pacemaker use, with 3–5% for biologic Bentall procedure and up to 8% for mechanical Bentall [26, 27]. Rates of reoperation for bleeding were lower at 6.7–9.6%, without being statistically significant [23, 24]. Thus, despite shorter CPB and aortic cross-clamping times with the Bentall procedure [23], the VSARR does not represent early excess morbidity compared with the Bentall procedure. It should be noted that the choice between a VSARR and valve replacement depends primarily on patient characteristics. Thus, populations operated on with the VSARR or Bentall procedure have significant differences making direct comparisons challenging, especially with regard to age [26].
The in-hospital mortality in this study was <2% (n = 10) and 0.9% (n = 4) for patients without AAD, comparable to that found in the literature (0.7% to 2% [4–10]), whereas mortality with Bentall procedure ranged from 1.5% to 7% [23, 24, 28]. Two meta-analyses (7313 and 2352 patients) confirm the superiority of VSARR in terms of in-hospital mortality compared with the Bentall procedure [25].
Among the 68 patients operated for AAD in this study, mortality was 8.8% (n = 6). Several studies have found higher in-hospital mortality with the Bentall procedure compared with the VSARR in the treatment of AAD: Kallenbach (n = 48 VSARR vs 65 Bentall, 2004), Beckman (n = 47 VSARR vs 72 Bentall, 2015) and Rosenblum (n = 59 VSARR vs 77 Bentall, 2018), with 10.4%, 12.8% and 3.4% early mortality, respectively, with the VSARR compared with 28%, 29% and 14.3% with the Bentall procedure, respectively [19, 29, 30].
Limitations
Limitations of this study are those inherent to retrospective cohorts, including data completeness. However, AORTLANTIC registry is integrated with the French national cardiac surgery database (EPICARD), which is prospectively completed by every cardiac surgery centre in France. This has facilitated coverage and thus significantly reduced the number of missing data. The partially prospective collection is also an advantage for the reliability of our long-term data.
Patients in whom VSARR could not be performed and the surgical strategy evolved to an intraoperative Bentall procedure are not included in this study. On the other hand, there is no control group.
Finally, the lack of intraoperative trans-oesophageal echography data precludes analyses on specific echocardiographic criteria for predicting eventual long-term outcomes.
CONCLUSION
The AORTLANTIC registry has comparable demographics to the major published studies of outcomes of VSARR using the David inclusion method. In-hospital morbidity and mortality in our registry confirm that this technique is reliably and safely reproducible in both planned and emergency patients, regardless of tricuspid or BAV phenotype. The majority of patients have no AR postoperatively. The initial encouraging results of this multicentre study warrant further long-term evaluation by future studies.
ACKNOWLEDGEMENTS
We thank the French Society of Cardiac Surgery and particularly Pr De Brux for their support of this study through the EPICARD database, the national database of cardiac surgery in France. This article has never been published previously. It has been selected and presented (as an oral presentation) at Francophone and European training days for cardio-thoracic and vascular surgery, structural and endo-vascular (Bordeaux, France, October 2021). We have never been submitted an Abstract of this manuscript for the EACTS or ESTS annual meeting.
Funding
No funding sources are received for this work.
Conflict of interest: none declared.
Glossary
ABBREVIATIONS
- AAD
Acute aortic dissection
- AR
Aortic regurgitation
- BAV
Bicuspid aortic valve
- CPB
Cardiopulmonary bypass
- VSARR
Valve-sparing aortic root replacement
Contributor Information
Clément Dubost, Department of Thoracic and Cardiovascular Surgery, Thorax Institute, Nantes Hospital University, Nantes, France.
Jacques Tomasi, Department of Thoracic and Cardiovascular Surgery, University Hospital Centre—INSERM LTSI 1099, Rennes, France.
Antoine Ducroix, Department of Thoracic and Cardiovascular Surgery, University Hospital, Angers, France.
Kevin Pluchon, Department of Cardiovascular and Thoracic Surgery, Brest University Hospital, Brest, France.
Pierre Escrig, Department of Thoracic and Cardiovascular Surgery, University Hospital Centre—INSERM LTSI 1099, Rennes, France.
Olivier Fouquet, Department of Thoracic and Cardiovascular Surgery, University Hospital, Angers, France.
Arthur Aupart, Department of Cardiothoracic Surgery, Trousseau University Hospital, Tours, France.
Alain Mirza, Department of Cardiac Surgery, New Clinic St Gatien, Tours, France.
Imen Fellah, Department of Thoracic and Cardiovascular Surgery, Thorax Institute, Nantes Hospital University, Nantes, France.
Eric Bezon, Department of Cardiovascular and Thoracic Surgery, Brest University Hospital, Brest, France.
Christophe Baufreton, Department of Thoracic and Cardiovascular Surgery, University Hospital, Angers, France.
Jean Marc El Arid, Department of Cardiothoracic Surgery, Trousseau University Hospital, Tours, France.
Jean-Christian Roussel, Department of Thoracic and Cardiovascular Surgery, Thorax Institute, Nantes Hospital University, Nantes, France.
Jean-Philippe Verhoye, Department of Thoracic and Cardiovascular Surgery, University Hospital Centre—INSERM LTSI 1099, Rennes, France.
Thomas Senage, Department of Thoracic and Cardiovascular Surgery, Thorax Institute, Nantes Hospital University, Nantes, France.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author contributions
Clément Dubost: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing—original draft. Jacques Tomasi: Investigation; Supervision; Validation. Antoine Ducroix: Data curation. Kevin Pluchon: Data curation. Pierre Escrig: Data curation. Olivier Fouquet: Investigation; Supervision; Validation. Arthur Aupart: Data curation. Alain Mirza: Investigation; Supervision; Validation. Imen Fellah: Conceptualization; Data curation; Methodology; Project administration; Resources. Eric Bezon: Investigation; Supervision; Validation. Christophe Baufreton: Investigation; Supervision; Validation. Jean Marc El Arid: Investigation; Supervision; Validation. Jean-Christian Roussel: Conceptualization; Investigation; Methodology; Supervision; Validation; Writing—review & editing. Jean-Philippe Verhoye: Investigation; Supervision; Validation. Thomas Senage: Conceptualization; Formal analysis; Investigation; Methodology; Supervision; Validation; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Tomas Holubec and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
REFERENCES
- 1. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A. et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol 2015;66:350–8. [DOI] [PubMed] [Google Scholar]
- 2. Yacoub MH, Fagan A, Pillai R, Radley Smith R.. Results of a new valve conserving operation for treatment of aneurysms or acute dissection of the aortic root. J Am Coll Cardiol 1983;1:708. [Google Scholar]
- 3. David TE, Feindel CM.. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg 1992;103:617–21; discussion 622. [PubMed] [Google Scholar]
- 4. David TE, David CM, Feindel CM, Manlhiot C.. Reimplantation of the aortic valve at 20 years. J Thorac Cardiovasc Surg 2017;153:232–8. [DOI] [PubMed] [Google Scholar]
- 5. De Paulis R, Chirichilli I, Scaffa R, Weltert L, Maselli D, Salica A. et al. Long-term results of the valve reimplantation technique using a graft with sinuses. J Thorac Cardiovasc Surg 2016;151:112–9. [DOI] [PubMed] [Google Scholar]
- 6. Mastrobuoni S, De Kerchove L, Navarra E, Watremez C, Vancraeynest D, Rubay J. et al. Long-term experience with valve-sparing reimplantation technique for the treatment of aortic aneurysm and aortic regurgitation. J Thorac Cardiovasc Surg 2019;158:14–23. [DOI] [PubMed] [Google Scholar]
- 7. Tamer S, Mastrobuoni S, Lemaire G, Jahanyar J, Navarra E, Poncelet A. et al. Two decades of valve-sparing root reimplantation in tricuspid aortic valve: impact of aortic regurgitation and cusp repair. Eur J Cardiothorac Surg 2021;59:1069–76. [DOI] [PubMed] [Google Scholar]
- 8. Beckmann E, Martens A, Krüger H, Korte W, Kaufeld T, Stettinger A. et al. Aortic valve-sparing root replacement with Tirone E. David’s reimplantation technique: single-centre 25-year experience. Eur J Cardiothorac Surg 2021;60:642–8. [DOI] [PubMed] [Google Scholar]
- 9. David TE, Feindel CM, David CM, Manlhiot C.. A quarter of a century of experience with aortic valve-sparing operations. J Thorac Cardiovasc Surg 2014;148:872–9; discussion 879–80. [DOI] [PubMed] [Google Scholar]
- 10. Kari FA, Doll K-N, Hemmer W, Liebrich M, Sievers H-H, Richardt D. et al. Survival and freedom from aortic valve-related reoperation after valve-sparing aortic root replacement in 1015 patients. Interact CardioVasc Thorac Surg 2016;22:431–8. [DOI] [PubMed] [Google Scholar]
- 11. Kunihara T, Aicher D, Rodionycheva S, Groesdonk H-V, Langer F, Sata F. et al. Preoperative aortic root geometry and postoperative cusp configuration primarily determine long-term outcome after valve-preserving aortic root repair. J Thorac Cardiovasc Surg 2012;143:1389–95.e1. [DOI] [PubMed] [Google Scholar]
- 12. Klotz S, Stock S, Sievers H-H, Diwoky M, Petersen M, Stierle U. et al. Survival and reoperation pattern after 20 years of experience with aortic valve-sparing root replacement in patients with tricuspid and bicuspid valves. J Thorac Cardiovasc Surg 2018;155:1403–1411.e1. [DOI] [PubMed] [Google Scholar]
- 13. Oliveira N d, David TE, Ivanov J, Armstrong S, Eriksson MJ, Rakowski H. et al. Results of surgery for aortic root aneurysm in patients with Marfan syndrome. J Thorac Cardiovasc Surg 2003;125:789–96. [DOI] [PubMed] [Google Scholar]
- 14. De Kerchove L, Mosala Nezhad Z, Boodhwani M, El Khoury G.. How to perform valve sparing reimplantation in a tricuspid aortic valve. Ann Cardiothorac Surg 2013;2:105–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schäfers H-J, Schmied W, Marom G, Aicher D.. Cusp height in aortic valves. J Thorac Cardiovasc Surg 2013;146:269–74. [DOI] [PubMed] [Google Scholar]
- 16. Lansac E, Bouchot O, Arnaud Crozat E, Hacini R, Doguet F, Demaria R. et al. Standardized approach to valve repair using an expansible aortic ring versus mechanical Bentall: early outcomes of the CAVIAAR multicentric prospective cohort study. J Thorac Cardiovasc Surg 2015;149:S37–S45. [DOI] [PubMed] [Google Scholar]
- 17. Tanaka H, Ikeno Y, Abe N, Takahashi H, Inoue T, Okita Y.. Outcomes of valve-sparing root replacement in acute type A aortic dissection. Eur J Cardiothorac Surg 2018;53:1021–6. [DOI] [PubMed] [Google Scholar]
- 18. Aubin H, Akhyari P, Rellecke P, Pawlitza C, Petrov G, Lichtenberg A. et al. Valve-sparing aortic root replacement as first-choice strategy in acute type A aortic dissection. Front Surg 2019;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosenblum JM, Leshnower BG, Moon RC, Lasanajak Y, Binongo J, McPherson L. et al. Durability and safety of David V valve-sparing root replacement in acute type A aortic dissection. J Thorac Cardiovasc Surg 2019;157:14–23.e1. [DOI] [PubMed] [Google Scholar]
- 20. De Kerchove L, Boodhwani M, Glineur D, Poncelet A, Verhelst R, Astarci P. et al. Effects of preoperative aortic insufficiency on outcome after aortic valve-sparing surgery. Circulation 2009;120:S120–126. [DOI] [PubMed] [Google Scholar]
- 21. Schäfers H-J, Aicher D, Langer F, Lausberg HF.. Preservation of the bicuspid aortic valve. Ann Thorac Surg 2007;83:S740–S745; discussion S785–S790. [DOI] [PubMed] [Google Scholar]
- 22. Polain de Waroux J-Bl, Pouleur A-C, Robert A, Pasquet A, Gerber BL, Noirhomme P. et al. Mechanisms of recurrent aortic regurgitation after aortic valve repair: predictive value of intraoperative transesophageal echocardiography. JACC Cardiovasc Imaging 2009;2:931–9. [DOI] [PubMed] [Google Scholar]
- 23. Lee H, Cho YH, Sung K, Kim WS, Park K-H, Jeong DS. et al. Clinical outcomes of root reimplantation and Bentall procedure: propensity score matching analysis. Ann Thorac Surg 2018;106:539–47. [DOI] [PubMed] [Google Scholar]
- 24. Beckerman Z, Leshnower BG, McPherson L, Binongo JN, Lasanajak Y, Chen EP.. The evidence in a Bentall procedure with Valsalva graft: is this standard of care? J Vis Surg 2018;4:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Salmasi MY, Theodoulou I, Iyer P, Al-Zubaidy M, Naqvi D, Snober M. et al. Comparing outcomes between valve-sparing root replacement and the Bentall procedure in proximal aortic aneurysms: systematic review and meta-analysis. Interact CardioVasc Thorac Surg 2019;29:911–22. [DOI] [PubMed] [Google Scholar]
- 26. Hamandi M, Nwafor CI, Baxter R, Shinn K, Wooley J, Vasudevan A. et al. Comparison of the Bentall procedure versus valve-sparing aortic root replacement. Proc (Bayl Univ Med Cent) 2020;33:524–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ouzounian M, Rao V, Manlhiot C, Abraham N, David C, Feindel CM. et al. Valve-sparing root replacement compared with composite valve graft procedures in patients with aortic root dilation. J Am Coll Cardiol 2016;68:1838–47. [DOI] [PubMed] [Google Scholar]
- 28. Mookhoek A, Korteland NM, Arabkhani B, Di Centa I, Lansac E, Bekkers JA. et al. Bentall procedure: a systematic review and meta-analysis. Ann Thorac Surg 2016;101:1684–9. [DOI] [PubMed] [Google Scholar]
- 29. Kallenbach K, Oelze T, Salcher R, Hagl C, Karck M, Leyh RG. et al. Evolving strategies for treatment of acute aortic dissection type A. Circulation 2004;110:II243–249. [DOI] [PubMed] [Google Scholar]
- 30. Beckmann E, Martens A, Alhadi FA, Ius F, Koigeldiyev N, Fleissner F. et al. Is Bentall procedure still the gold standard for acute aortic dissection with aortic root involvement? Thorac Cardiovasc Surg 2016;64:116–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.