Abstract
Background
Guidelines recommend moderate to high-intensity statins and antithrombotic agents in patients with atherosclerotic cardiovascular disease (ASCVD). However, guideline-directed medical therapy (GDMT) remains suboptimal.
Methods
In this quality initiative, best practice alerts (BPA) in the electronic health record (EHR) were utilized to alert providers to prescribe to GDMT upon hospital discharge in ASCVD patients. Rates of GDMT were compared for 5 months pre- and post-BPA implementation. Multivariable regression was used to identify predictors of GDMT.
Results
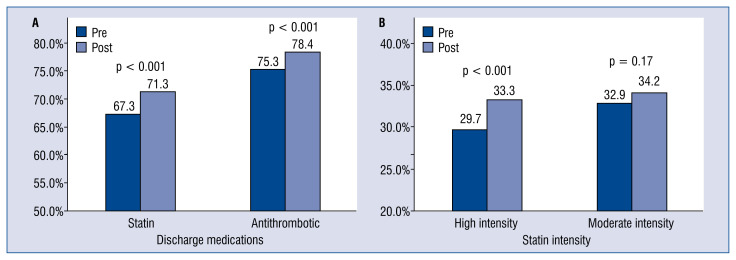
In 5985 pre- and 5568 post-BPA patients, the average age was 69.1 ± 12.8 years and 58.5% were male. There was a 4.0% increase in statin use from 67.3% to 71.3% and a 3.1% increase in antithrombotic use from 75.3% to 78.4% in the post-BPA cohort.
Conclusions
This simple EHR-based initiative was associated with a modest increase in ASCVD patients being discharged on GDMT. Leveraging clinical decision support tools provides an opportunity to influence provider behavior and improve care for ASCVD patients, and warrants further investigation.
Keywords: cardiovascular disease, secondary prevention, guideline-directed medical therapy, optimal medical therapy, best practice alerts, clinical decision support tools, electronic health records
Introduction
Secondary prevention guidelines from major medical societies in the United States emphasize at least moderate to high-intensity statins, antiplatelet agents, and lifestyle change in patients with established atherosclerotic cardiovascular disease (ASCVD) (AHA/ACC, AACE, NLA, IAS) [1–5] based on an abundance of data demonstrating both morbidity and mortality benefit [6, 7]. However, patient medical regimens and risk factors remain suboptimal in clinical practice [8–10], and even in large randomized controlled trials where emphasis is placed on optimal medical therapy [11]. Inpatient interventions to improve utilization and adherence to secondary prevention strategies may improve outcomes. At our own institution, we previously reported improvements in guideline-directed medication therapy (GDMT) associated with inpatient preventive cardiology consultations, and a prescription given at the time of discharge was associated with improved medicine regimens at 6-month follow-up [12]. In addition, lifestyle education at the time of discharge is not universal [13]. Patients may leave the hospital without understanding the potential benefit of lifestyle changes, which risk factors need to be improved, and how best to optimize their cardiovascular risk.
Clinical decision support instruments built into electronic health record (EHR) systems provide an opportunity to improve provider adherence to cardiovascular clinical practice guidelines. These instruments have been shown to increase the appropriateness of antimicrobial prescribing in the inpatient setting [14, 15]. Customized educational hand-outs specific to patient diagnosis at the time of discharge printed in the EHR after-visit summary can ensure that all patients receive the same basic information and resources for lifestyle improvement. Educational materials are currently available online from many organizations (Cardiosmart, National Lipid Association, American Heart Association) and can be customized based on institutional guidelines.
The impact of clinical decision support and educational materials provided in the after-visit summary on utilization and adherence to cardiovascular secondary prevention guidelines has not been established. We sought to determine the impact of a quality improvement initiative using clinical decision support to optimize adherence to GDMT and patient education at the time of hospital discharge in patients with established ASCVD.
Methods
Patients
Adults age ≥ 18 years with an established diagnosis of ASCVD discharged from inpatient hospitalization, medical observation, or ambulatory procedures at New York University Langone Health from February 2016 to February 2018 were eligible for inclusion. A diagnosis of ASCVD was defined by ≥ 1 ASCVD-associated diagnoses in the principal problem list of the EHR. Patients were excluded if they expired during the hospitalization, were discharged to hospice, had a known allergy to statin therapy, or had liver enzymes that were greater than two-times the upper limit of normal. Among patients with multiple visits during the study timeframe, only the first eligible encounter was included in the primary analysis.
Clinical decision support interventions
As part of ongoing quality improvement initiatives at New York University Langone Health, the Division of Value Based Medicine championed a ‘discharge-centered’ secondary prevention program to improve compliance with the medical center’s Clinical Practice Guidelines for patients with ASCVD. In collaboration with our institution’s Medical Center Information Technology group, we developed best practice alerts (BPAs) in the EHR to serve as real-time reminders about GDMT to providers caring for inpatients with ASCVD. The first BPA was designed as a ‘passive’ notification of recent hemoglobin A1c (HbA1c) and lipid results that included an optional one-click order to repeat lipid and HbA1c laboratory testing. The second and third BPAs were designed to interrupt the provider’s workflow with recommendations for statin and antithrombotic therapy at the time of discharge and included a link to prescribe appropriate statin and/or antithrombotic therapy. These alerts were targeted to selected patients with an ASCVD diagnosis who did not have an existing prescription for moderate or high-intensity statin or antithrombotic therapy. The BPAs allowed providers to decline statin and antithrombotic therapy orders and provide a rationale for this clinical decision. The BPA for statin therapy at discharge was not displayed for patients with documented statin allergies in the EHR.
Patient education intervention
To complement the decision support intervention, patient educational materials were developed for patients with ASCVD. These materials provided descriptions of ASCVD diagnoses, optimal diets for risk reduction, physical activity recommendations, and patient lifestyle resources. To allow patients to understand their own ASCVD risk factor control, each form was customized with patient-specific values for HbA1c, blood pressure, low-density lipoprotein cholesterol (LDL-C), body mass index (BMI), smoking status, and the corresponding target values. Patient educational materials were distributed via the EHR-generated after-visit summary provided at discharge to all eligible patients with ASCVD.
Provider education
Once the BPAs and educational material in the after-visit summary were fully incorporated into the EHR, hospital providers (nurse practitioners, physician assistants, and graduate medical education trainees) were notified about the initiative and provided hospital ASCVD guidelines. Representatives of each hospital inpatient, observation, and ambulatory unit received dedicated education from a member of the Division of Cardiology during the initial implementation phase.
Assessment of the quality improvement intervention and outcomes
The EHR-based intervention was launched on July 24, 2017, and the education of providers was conducted between June and September 2017. In order to evaluate the impact of the EHR-based intervention, data was collected over two 5-month periods, prior to (January 2017 to May 2017), and following (October 2017 to February 2018), the full implementation of the EHR-based intervention. The primary outcome of interest was the proportion of ASCVD patients prescribed GDMT with a moderate or high-intensity statin and antithrombotic therapy at the time of discharge. Data regarding actions in response to the interruptive BPAs was collected to understand provider behavior. Additional data collected from the electronic medical record included patient demographics, HbA1c, total cholesterol, LDL, serum liver enzymes, hospital service, and discharge diagnosis. Preadmission and discharge medication lists were obtained from the EHR. Moderate and high-intensity statins were classified based on ACC/AHA definitions. Specifically, high-intensity statins included atorvastatin 40 mg, atorvastatin 80 mg, rosuvastatin 20 mg, and rosuvastatin 40 mg. Moderate-intensity statins included atorvastatin 10 mg, atorvastatin 20 mg, rosuvastatin 5 mg, rosuvastatin 10 mg, pravastatin 40 mg, simvastatin 40 mg, and lovastatin 40 mg. Eligible antithrombotic therapy included acetylsalicylic acid, clopidogrel, prasugrel, ticagrelor, vorapaxar, as well as warfarin, rivoraxaban, dabigatran, apixiban, and edoxaban.
Statistical analysis
Continuous variables were reported as means and standard deviations and were compared by the Student t-test. Categorical variables were reported as proportions and compared by χ2 tests. Univariate and multivariable regression was performed to identify predictors of discharge on GDMT after adjusting for age, sex, admission type, admitting service, and whether the admission occurred before or after implementation of the BPA and patient education intervention. Statistical significance was defined as two-tailed p < 0.05 for all tests. Statistical analysis was performed using the R Foundation for Statistical Computing’s R version 3.5.0 (Vienna, Austria).
Results
Among 11,553 patients who were included in the analysis, the mean age was 69.1 ± 12.8 years, 58.5% were male, and 66.2% and 74.3% were on a statin and antithrombotic agent on admission, respectively (Table 1). The pre-BPA (n = 5985) and post-BPA (n = 5568) cohorts were similar with regards to baseline characteristics; however, a greater proportion of patients in the post-BPA cohort were on a statin on admission (67.7% vs. 64.8%, p = 0.001). Patients were primarily treated on a cardiology (37.9%), medicine (27.6%), or surgical (20.2%) service. A majority of patients were treated in the outpatient setting for an ambulatory procedure (57.6%) or the inpatient setting (32.8%).
Table 1.
Baseline characteristics in the pre- and post-best practice alert implementation cohorts.
| Total cohort (n = 11,553) | Pre-implementation (n = 5985) | Post-implementation (n = 5568) | P | |
|---|---|---|---|---|
| Age [years] | 69.1 ± 12.8 | 69.2 ± 12.8 | 68.9 ± 12.8 | 0.27 |
| Male sex | 58.5% | 57.7% | 59.3% | 0.07 |
| Admission statin | 66.2% | 64.8% | 67.7% | 0.001 |
| Admission antithrombotic | 74.3% | 73.8% | 74.9% | 0.18 |
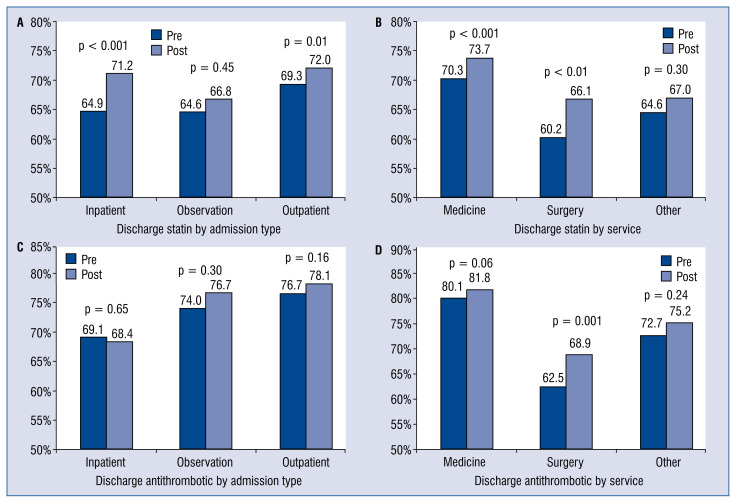
Comparing pre- and post-BPA implementation, there was a 4.0% increase in discharge statins, 3.6% increase in high-intensity statins, and 3.1% increase in antithrombotic agents in the post-BPA cohort (p < 0.001 for all comparisons) (Fig. 1). There were significant increases in the rates of statin prescriptions at discharge among inpatients, patients undergoing ambulatory procedures, and among patients admitted to a medicine or surgical service (Fig. 2A, B). A significant increase in discharge antithrombotic rates among surgical patients was also observed (Fig. 2C, D). There were 5.3% and 6.8% new antithrombotic prescriptions at discharge compared to admission in the pre- and post-BPA cohorts, respectively (p < 0.001). There were 4.4% and 5.1% new statin prescriptions at discharge compared to admission in the pre- and post-BPA cohorts, respectively (p = 0.08).
Figure 1.
Rates of guideline-directed medical therapy on hospital discharge; A. Compares pre- and post-best practice alert implementation rates of discharge statin and antithrombotic rates; B. Compares the breakdown of moderate and high-intensity statin rates on discharge.
Figure 2.
Rates of guideline-directed medical therapy on discharge by admitting service and admission type. Distribution of discharge statin pre- and post-best practice alert implementation by admission type (A) and admitting service (B). Distribution of discharge antithrombotic pre- and post-best practice alert implementation by admission type (C) and admitting service (D).
After multivariable regression, older age, male sex, admission post-BPA implementation, and admission to a cardiology or medicine service were associated with an increased odds of discharge on a statin or antithrombotic agent for ASCVD (Table 2).
Table 2.
Multivariable regression for predictors of discharge statin or antithrombotic agent.
| Statin prescribing at hospital discharge | Antithrombotic prescribing at hospital discharge | |||
|---|---|---|---|---|
|
|
|
|||
| β (SEM) | P | β (SEM) | P | |
| Age [year] | 0.02 (0.00) | < 0.001 | 0.03 (0.00) | < 0.001 |
| Sex: Male (vs. Female) | 0.53 (0.04) | < 0.001 | 0.64 (0.05) | < 0.001 |
| Post-BPA implementation (vs. Pre-BPA implementation) | 0.19 (0.04) | < 0.001 | 0.17 (0.05) | < 0.001 |
| Patient class: Inpatient (vs. All other patient classes as control) | −0.05 (0.05) | 0.32 | 0.14 (0.05) | < 0.001 |
| Service: Cardiology (vs. All other services as control) | 0.89 (0.05) | < 0.001 | 1.72 (0.06) | < 0.001 |
| Service: Medicine (vs. All other services as control) | 0.35 (0.04) | < 0.001 | 0.67 (0.05) | < 0.001 |
Adjusted for age, sex, admission time relative to BPA implementation (pre- or post-BPA implementation), patient class and admitting service;
BPA — best practice alert; SEM — structural equation modeling
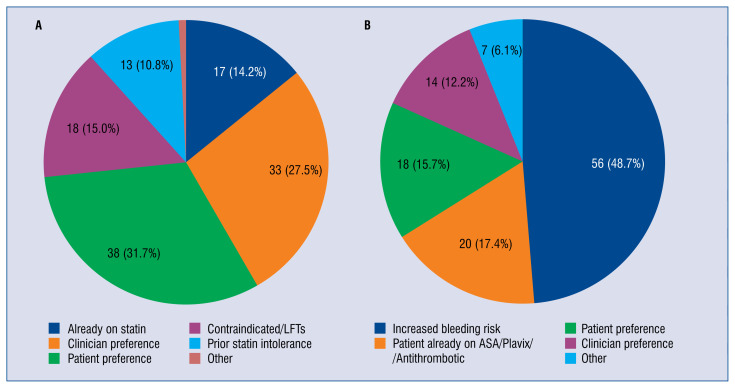
During the course of the study, the BPA was activated during 1,117 discharges to prompt providers to prescribe statins and 1,067 discharges to prompt providers to prescribe antithrombotic agents. Providers dismissed the BPA over 80% of the time; it changed prescribing behavior in a minority of cases (8%). Reasons for the BPA being dismissed are listed in Figure 3. Clinician or patient preferences were leading justifications for failure to discharge patients on a statin. Increased bleeding risk was the leading justification for failure to discharge patients on an antithrombotic agent.
Figure 3.
Reasons clinicians dismissed best practice alert recommendations; A. Statin best practice alert (BPA): Reasons clinicians disregarded the BPA; B. Antithrombotic BPA: Reasons clinicians disregarded the BPA; ASA — acetylsalicylic acid; LFT’s — liver function tests.
Discussion
Despite the impressive cardiovascular advances of our time, limitations persist in seemingly simple factors such as achieving optimal medical therapy and the implementation of lifestyle modification to promote cardiovascular health [16]. This quality improvement initiative at our institution illustrates a straightforward, cost-effective mechanism whereby medical centers with EHR capabilities can modestly improve compliance with GDMT and provide patient-centered educational materials at the critical juncture of hospital discharge. This type of initiative may help overcome health system, provider and patient factors that frequently stand in the way of health improvement [16].
After implementation of our initiative, we observed a statistically significant, albeit modest, increase in provider compliance with GDMT; specifically, a 4.0% increase was identified in discharge prescriptions for statins, a 3.6% increase in high-intensity statins and 3.1% increase in antithrombotic agents in the cohort post-BPA implementation. Moreover, significant increases in discharge statin rates were noted among inpatients admitted to a medicine or surgical service. The intervention also had an impact in patients undergoing ambulatory procedures as well, even though the window for medical optimization prior to discharge was brief.
Unfortunately, in this study providers dismissed the BPA recommendations over 80% of the time, and the BPA impacted prescribing behavior in only 8% of cases. While we were able to collect broad information regarding the reasons that the BPA was dismissed by discharging providers (Fig. 3), future work at our institution will aim to clarify the etiologies of “clinician preference” and “patient preference” in order to identify additional interventions to improve compliance with GDMT in the hospital discharge process. It was suspected that some responses to the BPA may have been a result of alarm fatigue. The constant inundation of EHR alerts may drive providers to bypass the alerts in order to complete the remainder of the workflow for patient care. Institutions may need to prioritize which alerts are essential and limit others that may impede care.
While more limited in scope and duration, our institution’s quality initiative shares similarities with the impressive Intermountain Health System’s “Hospital-Based Discharge Medication Program” for cardiovascular disease implemented in the early 2000’s at all ten Intermountain hospitals. These investigators were able to achieve upwards of 90% compliance with GDMT and saw significant decreases in the relative risk for death at 1 year as well as readmission at 30 days [17]. One key difference that might account for the high compliance and success of the Intermountain program was that discharge-planning nurses were required to directly contact an attending or resident physician if an appropriate medication was not prescribed — essentially creating a ‘hard stop’ during the discharge process until the medication was prescribed or a specific contraindication was documented. Future iterations of our quality initiative could include a similar hard stop in the discharge process to more effectively influence discharge providers’ prescribing behaviors.
The present study is limited by its observational, non-randomized, single-center design. Although the overall effect of the intervention was small and must be balanced against other competing factors such as alarm fatigue and provider frustration, this study demonstrates the feasibility of a simple intervention to increase provider adherence to prescribe GDMT. Refinement in patient selection or the addition of potential ‘hard stops’ for providers in the discharge process (‘obstructive intervention’) may further enhance the impact of BPAs. Additionally, a relatively short duration of time for analysis was utilized; further trends in prescribing behavior and compliance to GDMT might be clarified with a longer period of follow-up post-BPA implementation. To better ascertain the downstream effects of our simple EHR-based initiative, we intend to investigate changes in future hospital cardiovascular readmission rates. Lastly, although we were able to successfully implement a mechanism for discharging patients with educational materials and resources, we were unable to directly link improvements in lifestyle, cardiovascular risk factors or medication use to these educational materials.
Conclusions
In summary, with a simple, cost-effective EHR-based quality initiative we were able to demonstrate a modest increase in compliance with GDMT for ASCVD patients and improve the quality of care delivered at hospital discharge at a large academic medical center. As demonstrated in the current study, quality improvement programs are feasible and may be easily implemented to significantly increase adherence to GDMT. Improvements in GDMT adherence may pave the way for reductions in cardiovascular readmission rates and mortality, thereby reducing the tremendous burden of cardiovascular disease [18, 19].
Footnotes
Conflict of interest: None declared
References
- 1.Jacobson TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 - executive summary. J Clin Lipidol. 2014;8(5):473–488. doi: 10.1016/j.jacl.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64:1929–1949. doi: 10.1016/j.jacc.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Grundy S, Arai H, Barter P, et al. An International Atherosclerosis Society. Position Paper: Global recommendations for the management of dyslipidemia-Full report. J Clin Lipid. 2014;8(1):29–60. doi: 10.1016/j.jacl.2013.12.005.. [DOI] [PubMed] [Google Scholar]
- 4.Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease. Endocr Pract. 2017;23(Suppl 2):1–87. doi: 10.4158/EP171764.APPGL. [DOI] [PubMed] [Google Scholar]
- 5.Stone NJ, Robinson JG, Lichtenstein AH, et al. American College of Cardiology/American Heart Association Task Force on Practice G. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borden WB, Spertus JA, Mushlin AI, et al. Patterns and intensity of medical therapy in patients undergoing percutaneous coronary intervention. JAMA. 2011;305(18):1882–1889. doi: 10.1001/jama.2011.601. [DOI] [PubMed] [Google Scholar]
- 9.Rosenson RS, Kent ST, Brown TM, et al. Underutilization of high-intensity statin therapy after hospitalization for coronary heart disease. J Am Coll Cardiol. 2015;65(3):270–277. doi: 10.1016/j.jacc.2014.09.088. [DOI] [PubMed] [Google Scholar]
- 10.Tully L, Gianos E, Vani A, et al. Suboptimal risk factor control in patients undergoing elective coronary or peripheral percutaneous intervention. Am Heart J. 2014;168(3):310–316e3. doi: 10.1016/j.ahj.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Farkouh ME, Boden WE, Bittner V, et al. Risk factor control for coronary artery disease secondary prevention in large randomized trials. J Am Coll Cardiol. 2013;61(15):1607–1615. doi: 10.1016/j.jacc.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 12.Gianos E, Schoenthaler A, Guo Yu, et al. Investigation of Motivational Interviewing and Prevention Consults to Achieve Cardiovascular Targets (IMPACT) trial. Am Heart J. 2018;199:37–43. doi: 10.1016/j.ahj.2017.12.019.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kitakata H, Kohno T, Kohsaka S, et al. Patient confidence regarding secondary lifestyle modification and knowledge of ‚heart attack’ symptoms following percutaneous revascularisation in Japan: a cross-sectional study. BMJ Open. 2018;8(3):e019119. doi: 10.1136/bmjopen-2017-019119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baysari MT, Lehnbom EC, Li L, et al. The effectiveness of information technology to improve antimicrobial prescribing in hospitals: A systematic review and meta-analysis. Int J Med Inform. 2016;92:15–34. doi: 10.1016/j.ijmedinf.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Curtis CE, Al Bahar F, Marriott JF. The effectiveness of computerised decision support on antibiotic use in hospitals: a systematic review. PLoS One. 2017;12(8):e0183062. doi: 10.1371/journal.pone.0183062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirsh BJ, Smilowitz NR, Rosenson RS, et al. Utilization of and adherence to guideline-recommended lipid-lowering therapy after acute coronary syndrome: opportunities for improvement. J Am Coll Cardiol. 2015;66(2):184–192. doi: 10.1016/j.jacc.2015.05.030. [DOI] [PubMed] [Google Scholar]
- 17.Lappé JM, Muhlestein JB, Lappé DL, et al. Improvements in 1-year cardiovascular clinical outcomes associated with a hospital- based discharge medication program. Ann Intern Med. 2004;141(6):446–453. doi: 10.7326/0003-4819-141-6-200409210-00010. [DOI] [PubMed] [Google Scholar]
- 18.Laing ST. High-Intensity statins: guideline expectations and clinical application. JAMA. 2017;317(24):2543–2544. doi: 10.1001/jama.2017.5781. [DOI] [PubMed] [Google Scholar]
- 19.De Smedt D, Kotseva K, De Bacquer D, et al. Cost-effectiveness of optimizing prevention in patients with coronary heart disease: the EUROASPIRE III health economics project. Eur Heart J. 2012;33(22):2865–2872. doi: 10.1093/eurheartj/ehs210. [DOI] [PubMed] [Google Scholar]