Abstract
Pneumothorax and unintended arterial puncture are well-known complications of central venous (CV) access via the internal jugular vein (IJV), whereas injury to nerves around the IJV is a relatively rare complication. We describe the case of a male patient in his 60s who developed Horner syndrome after CV port placement via the IJV. We also point out the anatomical nerve structures around the IJV that clinicians should be aware of in order to minimize the risk of nerve injury during CV access. Additionally, with a brief literature review, we describe other nerve injuries that can be caused by CV access.
Keywords: Horner syndrome, central venous access, internal jugular vein, nerve injury, venous access port
Introduction
Central venous (CV) catheter insertion and CV port placement are integral components of chemotherapy and parenteral nutrition [1]. These are common interventional procedures in clinical practice. The IJV or the subclavian vein is usually selected as an access site because of the lower thrombotic and infectious complication rate compared to femoral access [2].
Although pneumothorax and hematoma due to unintended arterial puncture are common complications of CV puncture via the IJV [1-4], nerve injury is rare [5,6]. We describe a case of Horner syndrome caused by sympathetic nerve trunk injury during IJV puncture for CV port placement and also highlight anatomical nerve structures that an operator should be aware of with a literature review.
Case Report
Institutional review board (IRB) approval was waived for this case report because this is not necessary for a case report in our hospital. A male patient in his 60s who had multiple pulmonary metastases from colon cancer was referred to our department for CV port placement for chemotherapy. The patient was diagnosed with sigmoid colon cancer and bladder invasion and had undergone sigmoidectomy, cystectomy, and ileostomy, followed by five courses of capecitabine as adjuvant chemotherapy. Partial hepatectomy had also been performed for hepatic oligometastases 7 months after the initial surgery. However, as new multiple pulmonary metastases were found 14 months after the initial surgery, CV port placement was performed in our department for additional systemic chemotherapy.
The procedure was performed using a PowerPort with Groshong silicone catheter (Bard Access Systems, Salt Lake City, UT, USA) by an interventional radiologist with 2 years' experience. The patient's neck was rotated 45 degrees to the left to permit easier access for puncture. The right IJV puncture with real-time ultrasound guidance was attempted under local anesthesia with 1% lidocaine, using an echogenic 18-gauge needle included in the PowerPort kit. The IJV was visualized and punctured on axial (or short-axis) view in an anterior approach (short-axis out-of-plane approach). Because the patient had been dehydrated, the IJV collapsed, and therefore several attempts were needed even with the Valsalva maneuver. Finally, the puncture was successfully performed, but the needle had also penetrated the posterior wall of the IJV. The patient started complaining of slight pain in the neck immediately after the puncture. After that, a 0.035-inch J-shaped guidewire and a peel-away sheath were smoothly inserted without the patient complaining of pain, followed by successful catheter placement. An infraclavicular subcutaneous pocket and tunnel between the puncture site and the subcutaneous pocket was made under local anesthesia with lidocaine, and the catheter was connected to the CV port chamber placed through the subcutaneous tunnel after confirming the position of the catheter tip under fluoroscopy. The chamber was flushed using heparinized saline. Afterward, the incision site was closed with 3-0 nylon sutures.
The patient was fine during the procedure, except for the slight pain he felt in his neck. A radiograph taken immediately after the procedure showed neither pneumothorax nor catheter kink (Fig. 1). No other major complication was observed at that time, and he was allowed to return home after three hours of observation in the outpatient department. On the day after the procedure he came back to the hospital, with a chief complaint of“difficulty seeing”with his right eye. Actually, he had realized the symptom immediately after the procedure; however, he did not complain of the symptom and observed himself until the following day. He was referred to an ophthalmologist the same day. At that time, his symptoms were considered to be those of transient Horner syndrome with right ptosis and miosis caused by a transient nerve block of the cervical sympathetic nerve by local anesthesia. Although computed tomography (CT) with contrast enhancement taken 3 months after the procedure showed no abnormality around the puncture site and the catheter of the CV port (Fig. 2), his symptoms did not improve after three months of observation. Hence, he was referred to a neurologist for further evaluation. Eventually, Horner syndrome due to sympathetic nerve injury by the puncture needle was confirmed. A photograph of the face of the patient showing symptoms was not recorded in the chart. Twelve months after the procedure, the symptoms of Horner syndrome were still present.
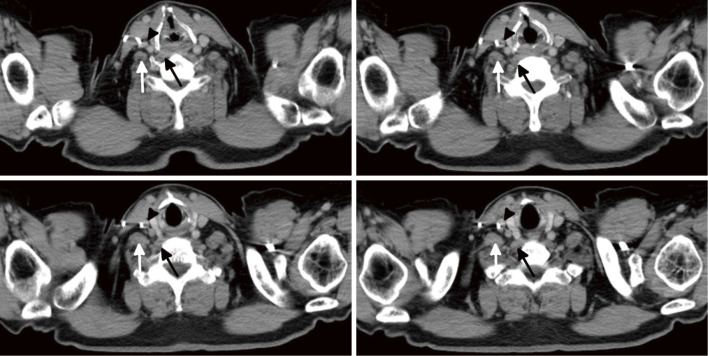
Fig. 1.
A chest radiograph taken immediately after central venous port placement. No pneumothorax is observed. Puncture point for the internal jugular vein is between C6 and C7 levels of the cervical spine. No catheter kink is seen.
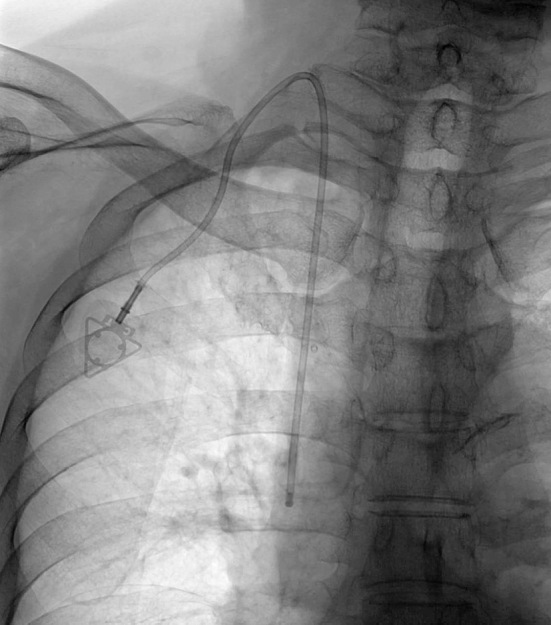
Fig. 2.
Axial computed tomography images with contrast enhancement taken three months after the procedure. Neither a procedure related abnormality nor any metastatic lesion that may cause Horner syndrome is observed around the internal jugular vein (black arrowhead) and the catheter. The black arrow indicates the longus colli muscle, and the white arrow indicates the anterior scalene muscle.
Discussion
According to previous reports, injury to the cervical sympathetic nerve trunk (CSNT) causing Horner syndrome, injury to the brachial plexus, phrenic nerve, and vagus nerve were reported as being uncommon complications of CV access via the IJV [7-13]. Butty et al. reported in their prospective study that the frequency of Horner syndrome after CV catheter insertion was 2%. The authors concluded that Horner syndrome is a definite complication of CV catheter insertion even with ultrasound guidance, although a not insignificant 70% of the cases in their report were performed by trainees from postgraduate year (PGY) 1 to PGY 4 [14]. These results suggest that the risk of this complication might have been underestimated in clinical practice.
Horner syndrome is a combination of symptoms caused by injury or disruption of the cervical sympathetic nerve pathway to the eye and face, including miosis (persistent small pupil) and anisocoria, ptosis (drooping eyelid), and anhidrosis (decreased sweating) on the affected side [15]. The CSNT is derived from the anterior rami of the upper section of the thoracic cord, ascending anterior to the transverse processes of the cervical vertebrae, and composed of the superior, middle, and inferior cervical ganglia [16]. At the lower level of the cervical spine, the CSNT runs in front of the longus colli muscle, which is anterior to the transverse processes and is also located posteromedial to the carotid sheath. The schema of the axial anatomical structure at C6 level is shown in Fig. 3.
Fig. 3.
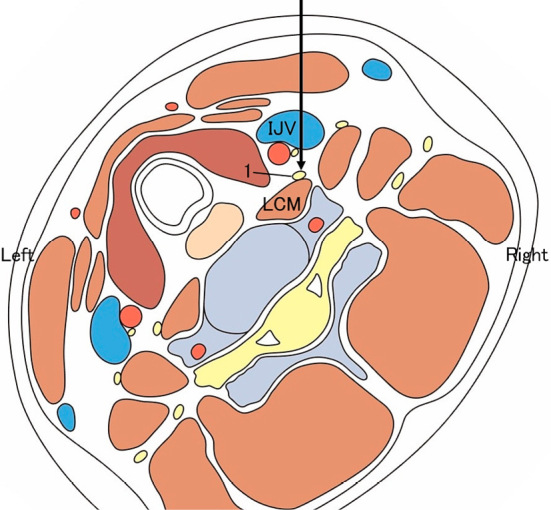
A schematic illustration of the anatomical structures in axial image (from the view of the operator standing on the cranial side of the patient) at C6 level of the cervical spine. CA, the right common carotid artery; IJV, the right internal jugular vein; VA, the right vertebral artery; LCM, the right longus colli muscle; ASM, the right anterior scalene muscle; 1, the right cervical sympathetic nerve trunk; 2, the right vagus nerve; 3, the right phrenic nerve; 4, the right brachial plexus. (This figure was constructed using an article by Akashi et al. [22].)
The CSNT is located posteromedially to the carotid sheath, and therefore, the puncture needle will not impinge on the CSNT when advanced in an anteroposterior (perpendicular) direction without neck rotation. (Fig. 3). However, it is common to rotate the patient's neck to the opposite side of the puncture site by some degrees to make the procedure easier. This neck rotation does not change the absolute location of the CNST in the neck, but it can change the relative direction of the needle toward the CSNT, as shown in Fig. 4. This seems to have contributed to CSNT injury in the present case, while the IJV posterior wall puncture itself was the main cause of this complication. A randomized controlled trial (RCT) by Lamperti et al. reported no significant difference in complication rates between IJV cannulation in the 45-degree neck rotation group and the no neck rotation group [17]; however, no nerve injury was reported in either group in their study population.
Fig. 4.
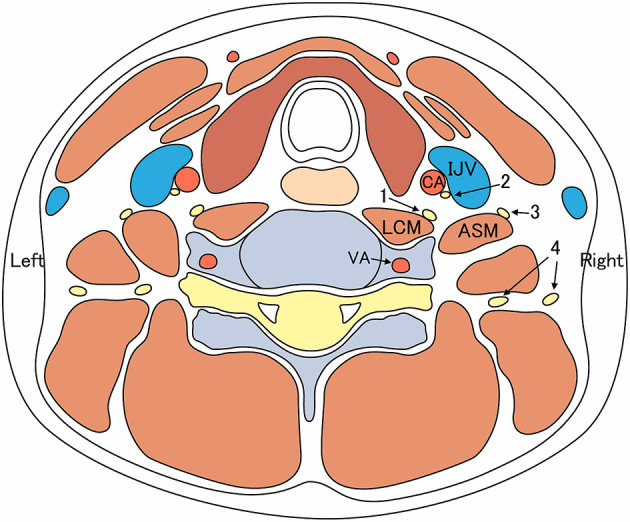
A schematic illustration of the puncture tract (shown as a large black arrow) for the right internal jugular vein, with 45-degree neck rotation to the left (the same anatomical schema as seen in Fig. 3) . If vertical puncture from anterior to posterior is performed on axial (short-axis) view, the cervical sympathetic nerve and longus colli muscle are located in the path of the puncture tract. IJV, the right internal jugular vein; LCM, the right longus colli muscle; 1, the right cervical sympathetic nerve trunk.
In the IJV puncture technique with ultrasound guidance, a short-axis out-of-plane approach and a long-axis in-plane approach are two widely used techniques [18]. Although a lower complication rate was reported with the long-axis approach compared to the short-axis approach in a recent prospective RCT [18], and although a long-axis in-plane approach reportedly improved the visibility of the needle tip during vessel puncture [19], this approach is not feasible for long-term catheter placement, such as a tunneled CV catheter or a CV port [20]. Since the long-axis in-plane approach requires puncturing from a superior part of the IJV due to the length of the ultrasound probe, a long subcutaneous tract is necessary. This may increase the risk of mechanical malfunction of the catheter and of patient discomfort. In addition to these two approaches, a short-axis lateral in-plane approach has been described [20,21]. According to previous reports, this technique provides good visualization of the needle and the surrounding tissue, which can contribute to a low complication rate; it also provides a smoother angle of the subcutaneous tract for a tunneled catheter or CV port [20,21]. Since the needle is advanced from lateral to medial in this technique, the risk of the IJV posterior wall puncture that may cause complications is considered to be minimal. Among these approach techniques, the short-axis out-of-plane approach at the inferior part of the neck was used in the present case. It is important to always visualize the needle tip with ultrasound to avoid complications; however, posterior puncture of the IJV may occur in the short-axis out-of-plane approach even with ultrasound guidance as in the current case; hence the short-axis lateral in-plane approach might have been useful to prevent the nerve injury. Changing the puncture site might also have aided prevention of this complication.
In addition to the CSNT, the phrenic and vagus nerves are located around the IJV (Fig. 3). Shawyer et al. [11] reported a pediatric case of phrenic nerve injury caused by tunneled CV catheter insertion via the IJV. Vagus nerve injury can cause unilateral vocal cord palsy (or hoarseness) because the recurrent laryngeal nerve is derived from the vagus nerve.
Conclusion
We presented a case of Horner syndrome caused by CSNT injury as a complication of IJV catheterization. Although nerve injury is unfamiliar and an uncommon complication of CV access via the IJV, the risk is not negligible. In addition to more common complications, physicians performing CV access should be educated about the nerve anatomy around the IJV as well as the risks and symptoms of these nerve injuries that can be induced by CV access in order to minimize the risk and enable prompt diagnosis of these complications.
Conflict of interest
None of the authors have any conflict of interest to declare for this article.
Disclaimer
Kentaro Yamada and Hiroshi Kondo are the Editorial Board members of Interventional Radiology. They were not involved in the peer-review or decision-making process for this paper.
References
- 1.Barbetakis N, Asteriou C, Klentas A, Tsilikas C. Totally implantable central venous access ports. Analysis of 700 cases. J Surg Oncol 2011; 104: 354-656. [DOI] [PubMed] [Google Scholar]
- 2.Heffner AC, Androes MP. Overview of central venous access. In: Collins KA (Ed.), UpToDate: 2018. Accessed June 5, 2019, from: https://www.uptodate.com/contents/overview-of-central-venous-access [Google Scholar]
- 3.Araújo C, Silva JP, Antunes P, Fernandes JM, Dias C, Pereira H, et al. A comparative study between two central veins for the introduction of totally implantable venous access devices in 1201 cancer patients. Eur J Surg Oncol 2008; 34: 222-226. [DOI] [PubMed] [Google Scholar]
- 4.Plumhans C, Mahnken AH, Ocklenburg C, Keil S, Behrendt FF, Günther RW, et al. Jugular versus subclavian totally implantable access ports: catheter position, complications and intrainterventional pain perception. Eur Radiol 2011; 79: 338-342. [DOI] [PubMed] [Google Scholar]
- 5.Goldfarb G, Lebrec D. Percutaneous cannulation of the internal jugular vein in patients with coagulopathies: an experience based on 1,000 attempts. Anesthesiology. 1982; 56: 321-323. [DOI] [PubMed] [Google Scholar]
- 6.Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular versus subclavian access--a systematic review. Crit Care Med. 2002; 30: 454-460. [DOI] [PubMed] [Google Scholar]
- 7.Parikh RK. Horner's syndrome: a complication of percutaneous catheterization of internal jugular vein. Anaesthesia 1972; 27: 327-329. [DOI] [PubMed] [Google Scholar]
- 8.Butty Z, Gopwani J, Mehta S, Margrolin E. Horner's syndrome in patients admitted to the intensive care unit that have undergone central venous catheterization: a prospective study. Eye 2016; 30: 31-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suominen PK, Korhonen AM, Vaida SJ, Hiller AS. Horner's syndrome secondary to internal jugular venous cannulation. J Clin Aneth 2008; 20: 304-306. [DOI] [PubMed] [Google Scholar]
- 10.Taskapan H, Oymak O, Dogukan A, Utas C. Horner's syndrome secondary to internal jugular vein catheterization. Clin Nephrol 2001; 56: 78-80. [PubMed] [Google Scholar]
- 11.Shawyer A, Chippington S, Quyam S, Schulze-Neick I, Roebuck D. Phrenic nerve injury after image-guided insertion of a tunneled right internal jugular central venous catheter. Pediatr Radiol 2012; 42: 875-877. [DOI] [PubMed] [Google Scholar]
- 12.Sim DW, Robertson MR. Right vocal cord paralysis after internal jugular vein cannulation. J Laryngol Otol 1989; 103: 424. [DOI] [PubMed] [Google Scholar]
- 13.Martin-Hirsch DP, Newbegin CJ. Right vocal fold paralysis as a result of central venous catheterization. J Laryngol Otol 1995; 109: 1107-1108. [DOI] [PubMed] [Google Scholar]
- 14.Paschall RM, Mandel S. Brachial plexus injury from percutaneous cannulation of the internal jugular vein. Ann Emerg Med 1983; 12: 58-60. [DOI] [PubMed] [Google Scholar]
- 15.Kedar S, Biousse V, Newman NJ. Horner syndrome. In: Wilterdink JL (Ed.), UpToDate: 2018. Accessed June 5, 2019, from: https://www.uptodate.com/contents/horner-syndrome [Google Scholar]
- 16.Ellis H, Feldman S, Harrop-Griffiths W. The sympathetic system. In: Anatomy for Anaesthetists, 8th ed. Oxford, England: Blackwell; 2004: pp. 218-228. [Google Scholar]
- 17.Lamperti M, Subert M, Cortellazzi P, Vailati D, Borrelli P, Montomolic C, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg 2012; 114: 777-784. [DOI] [PubMed] [Google Scholar]
- 18.Rath A, Mishra SB, Pati B, Dhar SK, Ipsita S, Samal S, et al. Short versus long axis ultrasound guided approach for internal jugular vein cannulations: A prospective randomized controlled trial. Am J Emerg Med 2019; doi: 10.1016/j.ajem.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach. Am J Emerg Med 2010; 28: 343-347. [DOI] [PubMed] [Google Scholar]
- 20.Rossi UG, Rigamonti P, Tichà V, Zoffoli E, Giordano A, Gallieni M, et al. Percutaneous ultrasound-guided central venous catheters: the lateral in-plane technique for internal jugular vein access. J Vasc Access 2014; 15: 56-60. [DOI] [PubMed] [Google Scholar]
- 21.Pittiruti M, Malerba M, Carriero C, Tazza L, Gui D. Which is the easiest and safest technique for central venous access? A retrospective survey of more than 5,400 cases. J Vasc Access 2000; 1: 100-107. [DOI] [PubMed] [Google Scholar]
- 22.Akashi N, Paku K. Technique of ultrasound-guided stellate ganglion block. Pain Clinic 2014; 35: 163-170. (in Japanese) [Google Scholar]