Abstract
Here, we report a case of hepatocellular carcinoma detected on computed tomography and treated with laparoscopic anatomical liver resection in a 69-year-old woman who was being followed-up for hepatitis C. Intraoperative liver segmentation is necessary to accomplish laparoscopic anatomical liver resection. Therefore, the day before surgery, hepatic artery embolization was performed with an indocyanine green-LipiodolⓇ mixture and GelpartⓇ containing indocyanine green to mark the region for hepatectomy. The next day, surgeons visually confirmed the resection segments on indocyanine green fluorescence imaging and performed laparoscopic anatomical liver resection. No major complications resulted from this method. In conclusion, hepatic artery embolization with an indocyanine green-LipiodolⓇ mixture is effective and safe for liver segment identification during laparoscopic anatomical liver resection.
Keywords: hepatic artery embolization, indocyanine green, LipiodolⓇ
Introduction
Laparoscopic hepatectomy is more difficult compared to laparotomy because of the utilization of two-dimensional images (no stereoscopic effect or depth of field) and narrow visual field. Therefore, intraoperative liver segmentation is necessary to accomplish laparoscopic anatomical liver resection (LALR). Ueno et al. reported the usefulness of hepatic artery embolization (HAE) with indocyanine green (ICG; DiagnogreenⓇ for injection, 2.5 mg/mL, Daiichi Sankyo, Tokyo, Japan) to identify the liver segments for resection [1]. They mixed ICG with a water-soluble contrast medium and had to perform surgery on the same day because ICG washes out within 24 h after infusion. In the present case, we mixed ICG with LipiodolⓇ (Lipiodol 480 injection; Guerbet Japan, Tokyo, Japan), a lipid-soluble contrast medium, to delay the washout of ICG, enabling us to perform surgery the next day.
Institutional review board approval was obtained for publication of this case report, and informed consent was obtained from the patient.
Case Report
A 69-year-old woman was being followed-up for hepatitis C. Blood tests showed high levels of tumor markers (α-fetoprotein: 174 ng/mL, protein induced by vitamin K absence or antagonist Ⅱ: 50 mAU/mL). Because computed tomography (CT) revealed hepatocellular carcinoma (HCC) in segment VIII, we decided to perform LALR.
The day before surgery, HAE was performed to mark the liver segments for LALR. Under local anesthesia, a 3-Fr sheath (Radifocus Introducer IIH; Terumo, Tokyo, Japan) was inserted in the right femoral artery. A shepherd-hook catheter (1 CJ 70 cm; Medikit, Tokyo, Japan) was inserted into the celiac artery, and a microcatheter (Veloute 1.7 Fr 125 cm; ASAHI INTECC, Tokyo, Japan) was advanced into the right hepatic artery and A8 (hepatic artery for segment VIII). After confirming that A8 was the only feeding artery for the tumor by CT during arteriography (Fig. 1), A8 was embolized using 9.5 mL of mixture A (5 mL ICG and 5 mL LipiodolⓇ) and mixture B (5 mL ICG and GelpartⓇ [Gelpart 1 mm 80 mg; Nippon Kayaku, Tokyo, Japan] mixed in 5 mL of contrast medium). Mixture A was initially injected into A8, which was subsequently embolized with mixture B until blood flow stopped. CT performed immediately after HAE confirmed that the ICG-LipiodolⓇ mixture had accumulated in segment VIII, which included the tumor (Fig. 2a). This procedure took 2 h. The next day, the surgeons visually confirmed the target area (segment VIII) by ICG fluorescence imaging and performed LALR (Fig. 3). This operation took 7 h and 30 min. Postoperative CT revealed that segment VIII was selectively resected (Fig. 2b). No major complications resulted from this method. The pathological diagnosis in this case was moderately differentiated HCC with approximately 85% necrosis of the tumor. GelpartⓇ was detected in the hepatic artery around the tumor. It was difficult to identify LipiodolⓇ in the portal vein using hematoxylin and eosin staining.
Fig. 1.
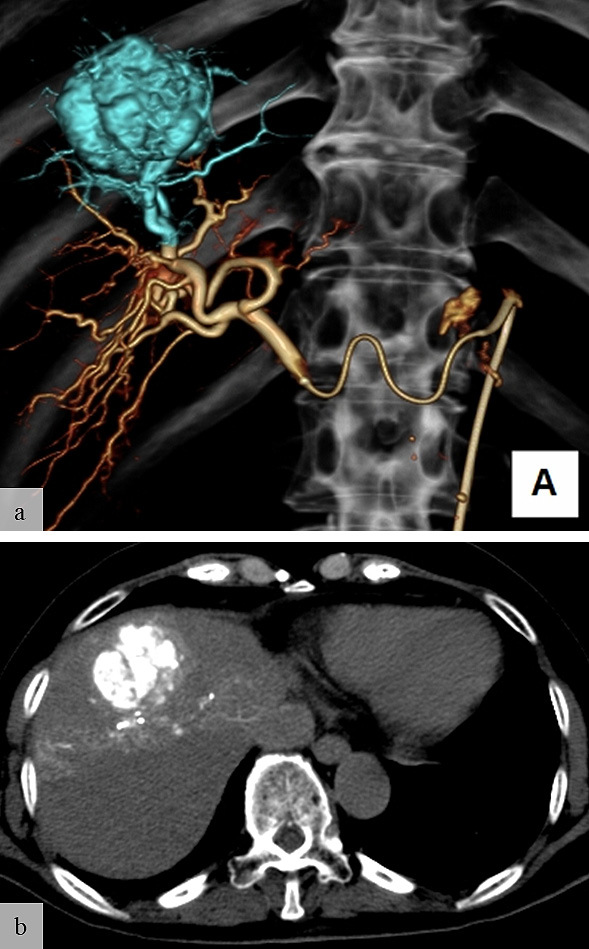
(a) Computed tomography during arteriography of the right hepatic artery shows that the tumor’s feeding artery is A8 (light blue). (b) Computed tomography during arteriography of A8 confirms that the tumor is fed by A8 alone.
Fig. 2.
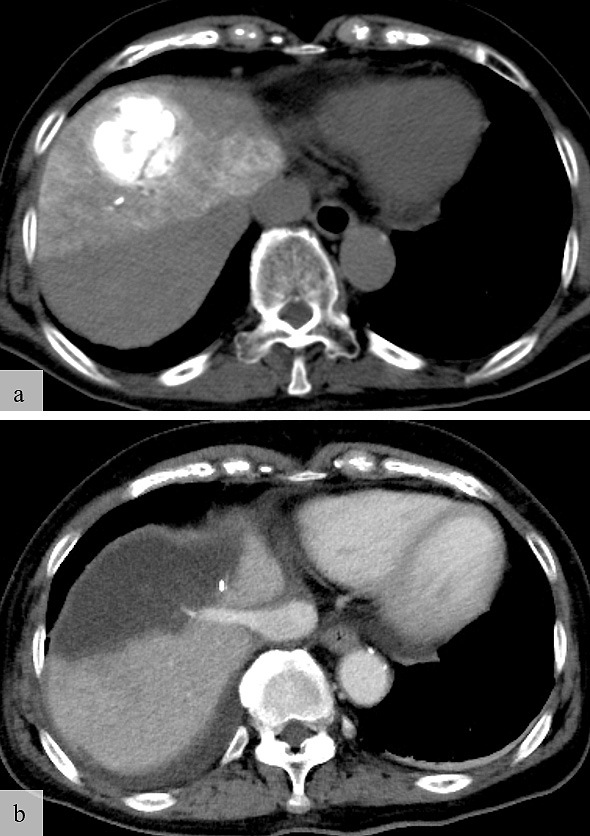
(a) Computed tomography performed immediately after hepatic artery embolization shows accumulation of the indocyanine green-Lipiodol® mixture in segment VIII, which includes the entire tumor. (b) Computed tomography after laparoscopic anatomical liver resection shows that segment VIII has been selectively resected.
Fig. 3.
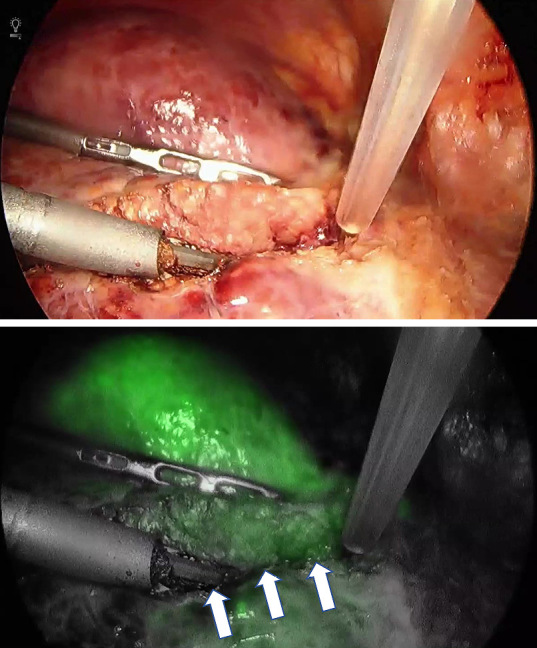
The day after infusion of the indocyanine green-Lipiodol® mixture, surgeons detected residual indocyanine green in segment VIII and performed laparoscopic anatomical liver resection. The three arrows represent the boundaries of the resected and non-resected regions.
Discussion
The tattooing method [2, 3] or the Glissonian approach [4] are commonly used to identify hepatic segments in conventional open liver surgery. Using the Glissonian approach, we can observe ICG fluorescence in the remnant liver by clamping the target Glissonian pedicle and injecting ICG intravenously (counter perfusion method). However, technical difficulties occasionally arise when performing LALR of segment V, VI, VII, or VIII. In such situations, the tattooing method (direct perfusion method) is performed. However, it is occasionally difficult to inject ICG into the portal vein under laparoscopic intraoperative ultrasonography (IOUS), and ICG washes out from the liver rapidly. To overcome these challenges, Ueno et al. performed HAE using ICG mixed with a water-soluble contrast medium [1]. In our past clinical experience with this method, ICG had completely washed out from the liver within 24 h after HAE. Therefore, it is necessary to perform HAE and LALR simultaneously in a hybrid operation room. However, performing angiography in the operation room restricts the movement of personnel, and CT during arteriography cannot be performed in the operating room. Surgeons also need to wait for radiologists to complete their procedures and cannot place the patient in an open-leg or a semi-prone position because the bed is prepared for interventional radiology (IR).
In the present case, we used ICG mixed with LipiodolⓇ, a lipid-soluble contrast medium, to delay the washout of ICG. Furthermore, the use of additional embolic materials (GelpartⓇ) can prevent ICG from being washed out due to blood flow. This allows surgeons to visualize the target segments for resection on ICG fluorescence imaging and perform LALR the day after HAE. LipiodolⓇ is commonly used as a carrier of anticancer drugs in transcatheter arterial chemoembolization (TACE) for HCC. In TACE, LipiodolⓇ is injected into the hepatic arteries and flows into the portal vein branches and hepatic sinus through the peribiliary vascular plexus around the tumor [5, 6]. LipiodolⓇ is a hyperviscous material that prevents the washout of ICG by blocking microvessels, including the portal vein branches and peribiliary vascular plexus, around the tumor. We are now planning experimental studies including pigs to assess the degree to which the LipiodolⓇ infusion delays the washout of ICG from the liver.
This new method has some limitations. Preoperative HAE with LipiodolⓇ could cause tumor necrosis before LALR contrary to the original technique performed immediately before surgery. If the entire tumor is necrotic, a pathologic diagnosis cannot be made. This approach might become more difficult in patients with significant arteriovenous shunting or arterial communication around the target region. IR also increases surgical costs, although laparoscopic hepatectomy is associated with lower hospital costs compared to open hepatectomy. The additional time taken to perform IR is another disadvantage of this method. However, surgeons can perform LALR without losing the cutting direction by using ICG fluorescence imaging. This enables surgeons to reduce the frequency of laparoscopic IOUS to confirm the cutting direction during hepatectomy. Consequently, our method might reduce the overall operating time.
In conclusion, HAE with an ICG-LipiodolⓇ mixture and GelpartⓇ containing ICG delays the washout of ICG and helps surgeons identify the liver segments during LALR. Further studies including more patients are required to confirm the efficacy of this method.
Conflict of interest
The authors declare that they have no conflicts of interest to report.
This case report has been presented at CIRSE2019.
Abbreviations
- CT
computed tomography
- HAE
hepatic artery embolization
- HCC
hepatocellular carcinoma
- ICG
indocyanine green
- IR
interventional radiology
- IOUS
intraoperative ultrasonography
- LALR
laparoscopic anatomical liver resection
- TACE
transcatheter arterial chemoembolization
References
- 1.Ueno M, Hayami S, Sonomura T, Tanaka R, Kawai M, Hirono S, et al. Indocyanine green fluorescence imaging techniques and interventional radiology during laparoscopic anatomical liver resection (with video). Surg Endosc 2018; 32(2): 1051-1055. [DOI] [PubMed] [Google Scholar]
- 2.Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet 1985; 161(4): 346-350. [PubMed] [Google Scholar]
- 3.Ahn KS, Kang KJ, Park TJ, Kim YH, Lim TJ, Kwon JH. Benefit of systematic segmentectomy of the hepatocellular carcinoma: revisiting the dye injection method for various portal vein branches. Ann Surg 2013; 258(6): 1014-1021. [DOI] [PubMed] [Google Scholar]
- 4.Takasaki K. Glissonean pedicle transection method for hepatic resection: A new concept of liver segmentation. J Hepatobiliary Pancreat Sci 1998; 5(3): 286-291. [DOI] [PubMed] [Google Scholar]
- 5.Kan Z, Ivancev K, Lunderquist A. Peribiliary plexa--important pathways for shunting of iodized oil and silicon rubber solution from the hepatic artery to the portal vein. An experimental study in rats. Invest Radiol 1994; 29(7): 671-676. [DOI] [PubMed] [Google Scholar]
- 6.Demachi H, Matsui O, Takashima T. Scanning electron microscopy of intrahepatic microvasculature casts following experimental hepatic artery embolization. Cardiovasc Intervent Radiol 1991; 14(3): 158-162. [DOI] [PubMed] [Google Scholar]


