ABSTRACT
Objectives:
We previously reported that swallowing in the bridge position (bridge swallowing) increased distal esophageal contractions and lower esophageal sphincter pressure against gravity. Moreover, bridge swallowing had the potential to strengthen esophageal peristalsis. In this study, we sought to evaluate whether the bridge swallowing exercise could improve gastroesophageal reflux disease (GERD) symptoms and gastroscopy findings.
Methods:
Seventeen subjects with scores of 8 points or higher on the Frequency Scale for Symptoms of GERD (FSSG) questionnaire participated in the study. The exercise of dry swallowing in the bridge posture lasted 4 weeks and was performed ten times per day. FSSG scores were compared before and after exercise. Three of the 17 participants underwent upper gastrointestinal endoscopy. The modified Los Angeles classification of reflux esophagitis was used for objective assessment before and after exercise.
Results:
No participants dropped out of this study. FSSG scores improved significantly after exercise (from median [range] 16 [13–21] points before exercise to 5 [4–10] points after exercise, P <0.001). Upper gastrointestinal endoscopy showed improvement in the modified Los Angeles classification grade in one participant.
Conclusions:
The bridge swallowing exercise significantly improves FSSG scores. This exercise can be performed easily and safely without adverse events. Further multicenter prospective studies are needed to validate that the bridge swallowing exercise is effective in improving GERD.
Keywords: dry swallowing, dysphagia, esophageal motility, gastroscopy, GERD
INTRODUCTION
Recently, increased attention has been paid to the effect of different body positions on esophageal motility. Numerous treatments for the oral and pharyngeal phases of swallowing are established in dysphagia therapy1,2); however, effective swallowing rehabilitation treatments for the esophageal phase do not yet exist. We have previously focused on the effect of body position and gravity on esophageal motility to enhance esophageal contractility. We reported that swallowing in the bridge posture (i.e., bridge swallowing) increased distal esophageal contractions and lower esophageal sphincter (LES) pressure against gravity compared with the upright or supine position (measured using high-resolution manometry).3)
Gastroesophageal reflux disease (GERD) and reflux esophagitis are common gastric acid-related disorders characterized by heartburn or acid regurgitation caused by the reflux of gastric contents.4) GERD and reflux esophagitis have an estimated prevalence of 20%–30% of the population in Western countries and greater than 10% of the population in Asia.5,6)
GERD is a condition in which gastroesophageal reflux (GER) causes either esophageal mucosal injuries, annoying symptoms, or both. GERD is generally diagnosed based on a combination of clinical symptoms, objective testing by endoscopy, reflux monitoring, and responses to anti-secretory therapy. When GERD is suspected based on a clinical assessment, two types of algorithms are proposed: (i) endoscopy is initially performed before proton-pump inhibitor (PPI) administration, and (ii) PPI administration is initiated without endoscopy.7)
The goals for clinical management of GERD include symptom relief, healing of erosive esophagitis, prevention of recurrence and complications, and overall improvement of the patient’s quality of life.4,8) Although acid-suppressive therapy using PPIs is recommended as a first-line treatment for GERD,9) PPI treatment results in symptom improvement in only 40%–50% of patients with non-erosive disease.10) Moreover, it is now recommended that PPIs should be used for the shortest time possible at the smallest effective dose11) because of the risk of severe side effects, such as infection, impaired absorption of nutrients, dementia, kidney disease, and hypergastrinemia-related problems, when taken over an extended period.12)
In the esophageal phase, primary peristaltic waves occur after swallowing. These waves are an essential mechanism for acid clearance from the esophagus such that excessive esophageal acid exposure may occur when it is not functioning correctly.13) Iwakiri et al. found that basal LES pressure, wave amplitude, and success rates of primary peristalsis in patients with reflux disease were significantly lower than those in healthy volunteers.14)
Currently, exercises to enhance esophageal motility are not widely used, but the bridge swallowing exercise has the potential to strengthen esophageal peristalsis against gravity. Therefore, in this study, we hypothesized that bridge swallowing could be used as a training method to improve GERD symptoms.
The aims of this study were: (1) to identify whether the exercise of dry swallowing in the bridge posture can improve GERD symptoms without the need for additional medication, (2) to compare gastroscopy findings before and after bridge swallowing exercises.
MATERIALS AND METHODS
Participants
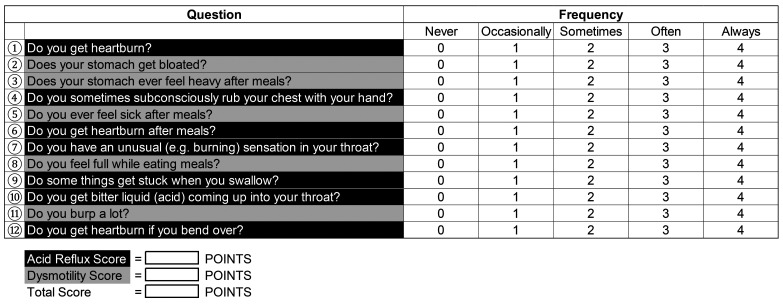
The study participants were medical staff in our hospital. The study was conducted between April and September 2021. The inclusion criteria were as follows: (1) aged 18–65 years, and (2) scores of 8 points or higher on the Frequency Scale for the Symptoms of GERD (FSSG) (Fig. 1).15) The exclusion criteria were as follows: (1) history of major abdominal surgery, and (2) severe weakness (i.e., inability to form postures) or back pain. Regarding participant recruitment, those with GERD symptoms such as heartburn and acid reflux were recruited by posting a notice at the hospital. All participants provided written informed consent. The study was approved by the Ethical Committee of Chikamori Rehabilitation Hospital (approval number: 2021-4).
Fig. 1.
The FSSG questionnaire: Frequency Scale for Symptoms of Gastroesophageal reflux disease.
Study Design
Exercises of dry swallowing in the bridge posture lasted for 4 weeks and were performed ten times per day (Fig. 2). The exercise was performed with 10-s intervals between swallows. Each participant laid down on a flat surface for the bridge posture, raised their hips against gravity, placed a cushion under their back, and bent their knees (i.e., a lower back support position).3) Exercises were performed after at least 4 h of fasting. Exercises were noted on a daily checklist to ensure that they were not forgotten. FSSG scores were used to compare the GERD symptoms before and after exercise. In addition, three participants who provided written informed consent underwent upper gastrointestinal endoscopy before and after exercise to compare the effects of bridge swallowing exercise using the modified Los Angeles classification of reflux esophagitis.16,17)
Fig. 2.
Bridge position.
Statistical Analysis
The Wilcoxon signed-rank test was used to compare FSSG scores before and after exercise. The threshold value for rejecting the null hypothesis was P <0.05. Statistical analysis was performed using IBM SPSS statistics version 28 software (IBM, Tokyo, Japan).
RESULTS
Seventeen participants (4 men, 13 women; mean age 41.4±9.4 years) who scored 8 points or higher on the FSSG, which we considered to indicate a high probability of GERD, were enrolled in this study. Eight of the 17 participants had previously been treated for GERD symptoms with PPIs, histamine H2 receptor antagonists, or Chinese herbal medicine. However, none were currently taking antacids, including PPIs or histamine H2 receptor antagonists. The professions of the study participants were doctors, nurses, medical secretaries, rehabilitation therapists, nutritionists, and social workers.
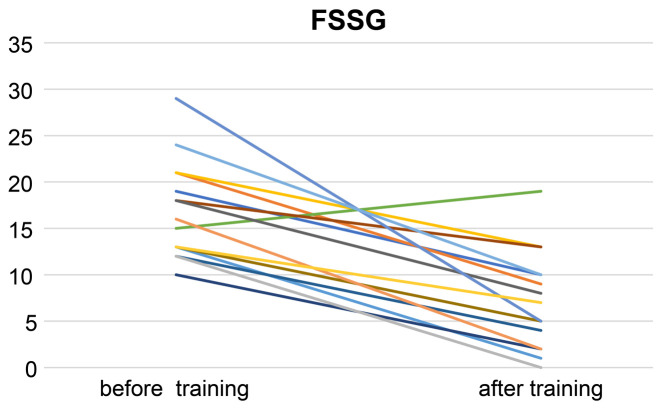
All participants completed the study. One participant’s score worsened after exercise, but the FSSG scores of the others improved (Fig. 3).
Fig. 3.
Plot of FSSG total scores before and after exercise for all participants.
A summary of the results is provided in Table 1. FSSG scores improved significantly from a median score of 16 [range: 13–21] points before exercise to 5 [range: 4–10] points after exercise (Wilcoxon’s signed-rank test, P <0.001).
Table 1. FSSG scores before and after bridge swallowing exercise.
| FSSG score | Before exercise | After exercise | P-value |
| Total | 16 [13–21] | 5 [4–10] | <0.001 |
| Dysmotility | 7 [5–11] | 3 [1–4] | <0.001 |
| Reflux | 9 [7–12] | 3 [1–6] | <0.001 |
Data given as median [range].
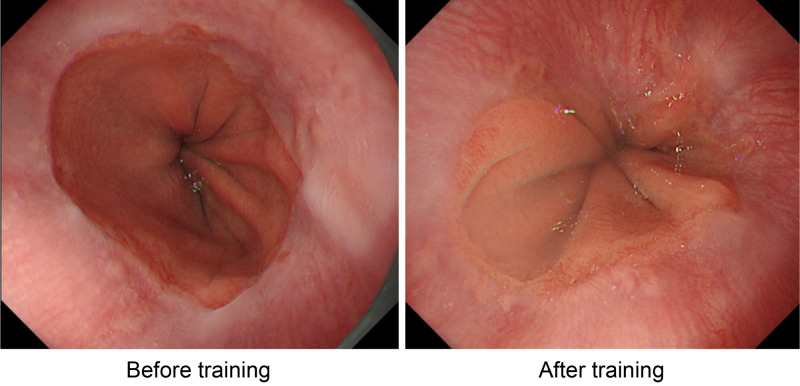
Of the three participants to undergo upper gastrointestinal endoscopy, one showed improvement in the modified Los Angeles classification grade (from A to M) (Table 2; Fig. 4). However, the other two showed no change in modified Los Angeles classification grade. Regarding FSSG, all three participants’ scores showed improvement: participant 1, 19 to 10; participant 2, 21 to 9; participant 3, 13 to 5.
Table 2. Modified Los Angeles classification of reflux esophagitis in three participants that underwent endoscopy.
| Participant | Before exercise | After exercise |
| 1 | A | A |
| 2 | A | M |
| 3 | M | M |
Fig. 4.
Upper gastrointestinal endoscopy findings for one case (participant 2).
DISCUSSION
To the best of our knowledge, this is the first study to demonstrate that the exercise of dry swallowing in the bridge posture can improve GERD symptoms. The most important finding was that FSSG scores improved significantly after the exercise. We previously reported changes in esophageal motility according to changes in position while swallowing, where distal esophageal contractions, integrated relaxation pressure, esophagogastric junction pressure (free of swallows) became stronger against gravity.3) This means that the bridge swallowing exercise increases esophageal contractions and LES pressure. This may help to explain the improvement in acid clearance and prevention of gastroesophageal reflux observed in our study. In addition, these results may be of clinical importance for improving the outcomes of patients who have GERD symptoms.
Although the study was conducted in a small group, one of the three participants who underwent upper endoscopy showed improvement in esophagitis grade (using the Los Angeles classification). This individual had been experiencing GERD symptoms but showed improvements in endoscopic findings and subjective GERD symptoms (FSSG scores). Given that the study was conducted during the COVID-19 epidemic, very few cases were available for endoscopy.18) As such, further studies with larger numbers of participants are needed to investigate the association between endoscopic findings and the efficacy of bridge swallowing.
All participants were able to complete the study. This was not surprising because the task of dry swallowing in the bridge posture ten times each day was not difficult. The exercise could be performed anywhere using cushions and did not require specialized equipment for measuring angles. Essentially, the participants leaned back on a cushion and relaxed in the bridge position. However, our previous study using high-resolution manometry indicated a significantly higher gastric pressure in the bridge position when compared with the supine gastric pressure.3) This may have been caused by the weight of intra-abdominal organs and increased diaphragmatic and/or abdominal wall muscle tone in the bridge position on the LES. Therefore, while there is no need to make an effort to maintain the bridge posture, there may have been some pressure on the LES in the bridge position.
No adverse events were observed in any of the participants. However, efficacy and long-term therapeutic effects of the bridge exercise are unknown and need to be compared with conventional treatments for GERD. These effects should also be studied in a larger number of participants.
Although the benefits of lifestyle change in reducing GERD symptoms have been reported,19,20) there have been no reports of the effectiveness of swallowing rehabilitation treatments. The results of the current study suggest that bridge swallowing exercises improve GERD symptoms. Further study is required to evaluate the subjects’ esophageal motor function before and after bridge swallowing exercise using techniques such as high-resolution manometry. Such a quantitative approach is important for validation and to compare the effectiveness of bridge exercise with medications and other conventional management strategies for GERD.
Our study had some limitations. First, data were collected from a small population of relatively young participants. In addition, although the participants were at high risk of GERD on the FSSG score, the majority of patients were not clearly diagnosed with GERD by endoscopy. However, symptoms are important factors for establishing GERD diagnosis. When GERD is suspected based on a clinical assessment, endoscopy is a somewhat invasive examination, and many patients prefer PPI administration without endoscopy in clinical practice. In this study, we used bridge swallowing instead of PPI. Further studies should include a larger sample size, a more comprehensive age range of participants, and severe cases of GERD diagnosed by endoscopic findings. It is noteworthy that our study enrolled considerably more women than men, which may be because the severity of GERD symptoms in women is much higher than in men.21) Second, given that this study did not include a control group, it is possible that improvements in FSSG were the result of a placebo effect. Third, the body angle of each subject while in the bridge posture was not measured. However, this is the inherent advantage of this method because it can be performed anywhere as long as a cushion is available. Fourth, although GERD symptoms improved after the exercise, the long-term effects were not studied and are unknown. Furthermore, esophageal motor function was not assessed before and after bridge swallowing exercise in this study.
CONCLUSION
The exercise of dry swallowing in the bridge posture significantly improves FSSG scores and symptoms of GERD. This exercise can be performed easily and safely without adverse events. Further studies should be conducted to compare the effectiveness of this technique with conventional treatments for GERD.
Footnotes
CONFLICTS OF INTEREST: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Palmer JB,DuChane AS: Rehabilitation of swallowing disorders in the elderly. In: Felsenthal G, Garrison SJ, Steinberg FU (eds). Rehabilitation of the aging and elderly patient. Williams & Wilkins, Baltimore, 1994; 275–287.
- 2.Palmer JB,DuChane AS: Rehabilitation of swallowing disorders due to stroke. Phys Med Rehabil Clin N Am 1991;2:529–546. 10.1016/S1047-9651(18)30699-5 [DOI] [Google Scholar]
- 3.Aoyama K,Kunieda K,Shigematsu T,Ohno T,Fujishima I: Effect of bridge position swallow on esophageal motility in healthy individuals using high-resolution manometry. Dysphagia 2021;36:551–557. 10.1007/s00455-020-10169-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maradey-Romero C,Fass R: New and future drug development for gastroesophageal reflux disease. J Neurogastroenterol Motil 2014;20:6–16. 10.5056/jnm.2014.20.1.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dent J,El-Serag HB,Wallander MA,Johansson S: Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2005;54:710–717. 10.1136/gut.2004.051821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goh KL: Changing epidemiology of gastroesophageal reflux disease in the Asian-Pacific region: an overview. J Gastroenterol Hepatol 2004;19(Suppl 3):S22–S25. 10.1111/j.1440-1746.2004.03591.x [DOI] [PubMed] [Google Scholar]
- 7.Iwakiri K,Fujiwara Y,Manabe N,Ihara E,Kuribayashi S,Akiyama J,Kondo T,Yamashita H,Ishimura N,Kitasako Y,Iijima K,Koike T,Omura N,Nomura T,Kawamura O,Ohara S,Ozawa S,Kinoshita Y,Mochida S,Enomoto N,Shimosegawa T,Koike K: Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2021. J Gastroenterol 2022;57:267–285. 10.1007/s00535-022-01861-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hershcovici T,Fass R: Gastro-oesophageal reflux disease: beyond proton pump inhibitor therapy. Drugs 2011;71:2381–2389. 10.2165/11597300-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 9.DeVault KR,Castell DO: Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 2005;100:190–200. 10.1111/j.1572-0241.2005.41217.x [DOI] [PubMed] [Google Scholar]
- 10.Fass R: Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol 2007;41:131–137. 10.1097/01.mcg.0000225631.07039.6d [DOI] [PubMed] [Google Scholar]
- 11.Song HJ,Jiang X,Henry L,Nguyen MH,Park H: Proton pump inhibitors and risk of liver cancer and mortality in patients with chronic liver disease: a systematic review and meta-analysis. Eur J Clin Pharmacol 2020;76:851–866. 10.1007/s00228-020-02854-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haastrup PF,Thompson W,Søndergaard J,Jarbøl DE: Side effects of long‐term proton pump inhibitor use: a review. Basic Clin Pharmacol Toxicol 2018;123:114–121. 10.1111/bcpt.13023 [DOI] [PubMed] [Google Scholar]
- 13.Iwakiri K,Kinoshita Y,Habu Y,Oshima T,Manabe N,Fujiwara Y,Nagahara A,Kawamura O,Iwakiri R,Ozawa S,Ashida K,Ohara S,Kashiwagi H,Adachi K,Higuchi K,Miwa H,Fujimoto K,Kusano M,Hoshihara Y,Kawano T,Haruma K,Hongo M,Sugano K,Watanabe M,Shimosegawa T: Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol 2016;51:751–767. 10.1007/s00535-016-1227-8 [DOI] [PubMed] [Google Scholar]
- 14.Iwakiri K,Hayashi Y,Kotoyori M,Tanaka Y,Kawakami A,Sakamoto C,Holloway RH: Transient lower esophageal sphincter relaxations (TLESRs) are the major mechanism of gastroesophageal reflux but are not the cause of reflux disease. Dig Dis Sci 2005;50:1072–1077. 10.1007/s10620-005-2707-5 [DOI] [PubMed] [Google Scholar]
- 15.Kusano M,Shimoyama Y,Sugimoto S,Kawamura O,Maeda M,Minashi K,Kuribayashi S,Higuchi T,Zai H,Ino K,Horikoshi T,Sugiyama T,Toki M,Ohwada T,Mori M: Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol 2004;39:888–891. 10.1007/s00535-004-1417-7 [DOI] [PubMed] [Google Scholar]
- 16.Armstrong D,Bennett JR,Blum AL,Dent J,De Dombal FT,Galmiche JP,Lundell L,Margulies M,Richter JE,Spechler SJ,Tytgat GN,Wallin L: The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 1996;111:85–92. 10.1053/gast.1996.v111.pm8698230 [DOI] [PubMed] [Google Scholar]
- 17.Hoshihara Y,Hashimoto M: Endoscopic classification of reflux esophagitis [in Japanese]. Jpn J Clin Med 2000;58:1808–1812. [PubMed] [Google Scholar]
- 18.Maruyama H,Hosomi S,Nebiki H,Fukuda T,Nakagawa K,Okazaki H,Yamagami H,Hara J,Tanigawa T,Machida H,Aomatsu K,Watanabe Y,Sato H,Uno H,Takaishi O,Nomura T,Ochi M,Oshitani N,Adachi K,Higashimori A,Ominami M,Nadatani Y,Fukunaga S,Otani K,Tanaka F,Kamata N,Nagami Y,Taira K,Watanabe T,Fujiwara Y: Gastrointestinal endoscopic practice during COVID-19 pandemic: a multi-institutional survey. Rom J Intern Med 2021;59:166–173. 10.2478/rjim-2020-0038 [DOI] [PubMed] [Google Scholar]
- 19.Kinoshita Y,Ashida K,Miwa H,Hongo M: The impact of lifestyle modification on the health-related quality of life of patients with reflux esophagitis receiving treatment with a proton pump inhibitor. Am J Gastroenterol 2009;104:1106–1111. 10.1038/ajg.2009.77 [DOI] [PubMed] [Google Scholar]
- 20.Ness-Jensen E,Hveem K,El-Serag H,Lagergren J: Lifestyle intervention in gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2016;14:175–182. 10.1016/j.cgh.2015.04.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin M,Gerson LB,Lascar R,Davila M,Triadafilopoulos G: Features of gastroesophageal reflux disease in women. Am J Gastroenterol 2004;99:1442–1447. 10.1111/j.1572-0241.2004.04147.x [DOI] [PubMed] [Google Scholar]