Abstract
Behcet's disease is a systemic vasculitis that can manifest as an intracardiac thrombus, which is rare but a serious complication. We report a case of a young male with a history of diabetes mellitus and erythema nodosum, who was admitted for pulmonary embolism associated with a huge serpentine right ventricle thrombus leading to the diagnosis of Behcet's disease. The patient was managed medically with a favorable evolution. The development of intracardiac thrombus is a life-threatening manifestation of the disease, and its discovery, especially in young subjects must suggest the diagnosis of Behcet's disease even if there is no predisposing ethnic or geographical factor.
Keywords: Behcet's disease, Intracardiac thrombus, Pulmonary embolism
Introduction
Behcet's disease is a systemic vasculitis that can affect vessels of any size or type. It is especially frequent among the Turkish, Japanese, and Mediterranean basin populations [1,2].
Behcet's disease does not have any specific clinical, radiological, or biological findings, thus the diagnosis is made using several arguments recommended in the International Criteria for Behcet's Disease [3].
The disease is characterized by numerous manifestations, the most frequent being bipolar aphtosis and skin lesions but it can affect the neurological, gastrointestinal, ophthalmological, pulmonary, and cardiovascular systems [3].
On the cardiovascular level, Behcet's disease can manifest as intracardiac thrombi, endocarditis, myocarditis, pericarditis, endomyocardial fibrosis, coronary arteritis, myocardial infarction, and valvular disease [4].
We present a case of a young patient with Behcet's disease in whom we discovered a right ventricular thrombus following a pulmonary embolism.
Clinical case
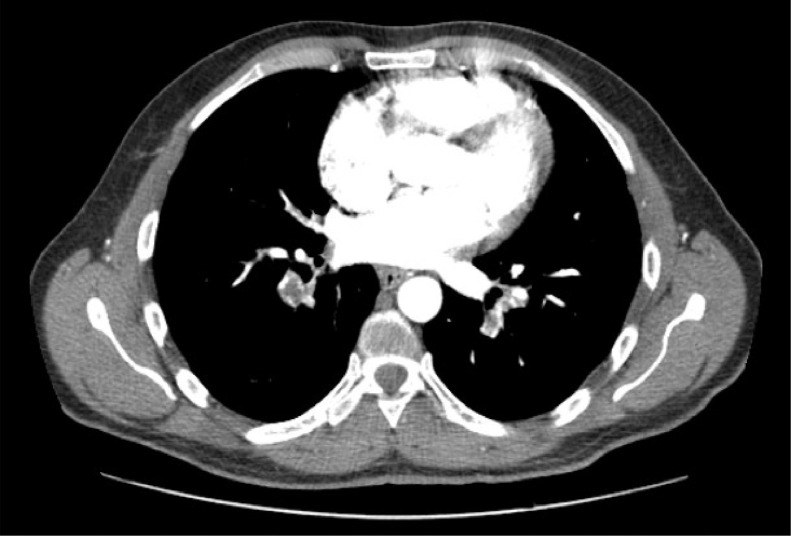
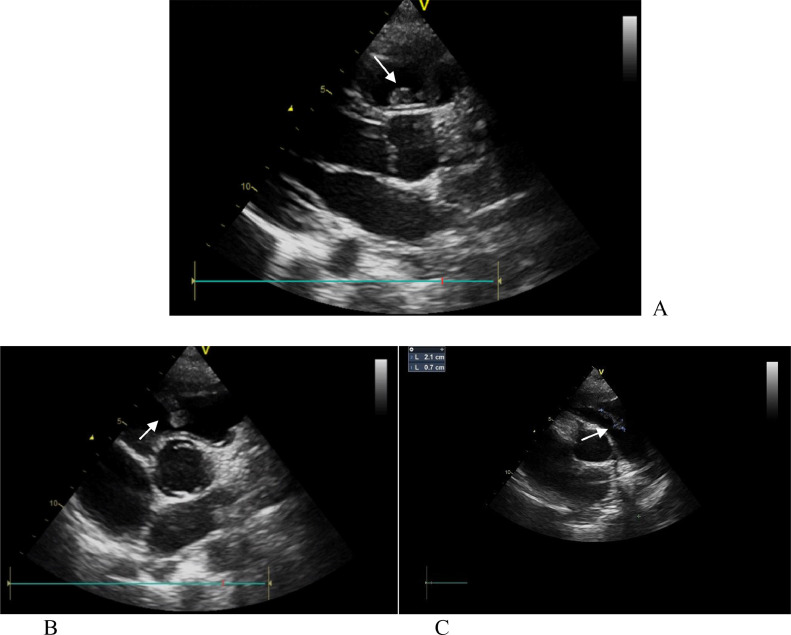
A 46-year-old male with a history of diabetes mellitus and erythema nodosum presented with acute dyspnea associated with chest pain and moderate hemoptysis. The physical examination revealed oral and scrotal lesions compatible with bipolar aphtosis. No clinical sign of deep vein thrombosis was detected in admission. The patient was diagnosed with Behcet's disease based on the International Criteria for Behcet's Disease. EKG and chest X-ray were normal. Laboratory investigations showed an inflammatory reaction with hyperleukocytosis at 17 G/l (4-11 G/l) and a high level of C reactive protein at 78 mg/l (0-6 mg/l). D-dimer values were elevated at 1317 ng/ml (<500 ng/ml). SARS Cov-2 serology was in favor of previous non-active infection and PCR was negative. Chest computed tomography (CT) scan showed an embolism of right segmental and sub-segmental pulmonary arteries associated with a focal right dorso-basal pulmonary infarction. It also showed a lacunar image in the right ventricle suggestive of intracardiac thrombus (Figs. 1 and 2). The CT scan didn't show signs of pulmonary artery aneurysm. Transthoracic echocardiography (TTE) showed a serpentine mass occupying the outflow tract of the right ventricle measuring 21 mm for its large diameter, suggestive of intracardiac thrombus (Fig. 3).
Fig. 1.
CT scan image showing a right ventricle thrombus.
Fig. 2.
CT scan image showing right pulmonary artery embolism.
Fig. 3.
TTE parasternal long-axis view (A) and parasternal short-axis view (B & C) showing right ventricle serpentine thrombus.
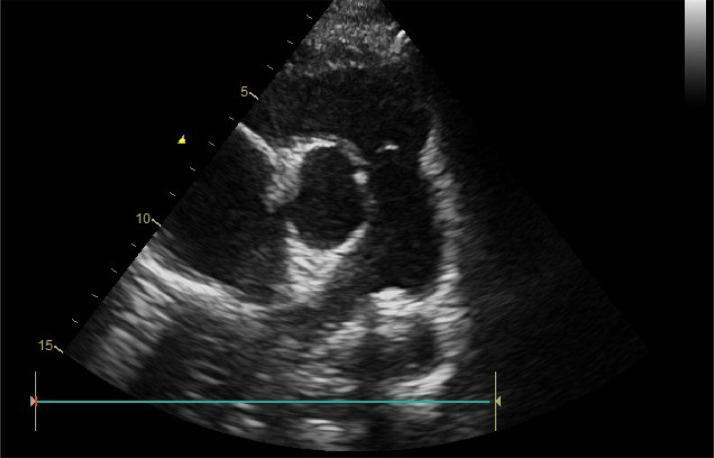
The patient received corticosteroids and cyclophosphamide in combination with acenocoumarol after a short overlap with heparin with an INR objective of 2.5. On follow-up, a TTE was performed 3 months later, and complete lysis of thrombus was observed (Fig. 4).
Fig. 4.
Control TTE parasternal short-axis view 3 months later showing complete lysis of thrombus.
Discussion
Behcet's disease is a variable vessel vasculitis with important divergence regarding demographic features, clinical manifestations, frequency and severity of relapses, the natural evolution of the illness, response to treatment, and prognosis [5].
Cardiovascular manifestations of Behcet's disease have been reported in 7%-46% of subjects with a high mortality rate approaching 20% of patients with manifest cardiovascular involvement. The most common manifestation of cardiovascular Behcet is thrombosis; however, sporadic cases of pericarditis, myocarditis, coronary disease, congestive heart failure, ventricular thrombosis, aortic aneurysm, and valvular disease have been reported [6].
The most common site of thrombosis associated with Behcet's disease is the deep veins of the lower extremities, but thrombosis of other sites such as portal venous thrombosis, pulmonary artery thrombosis, sagittal sinus thrombosis, and intracardiac thrombosis has been described.
Cardiac thrombus is a life-threatening condition that has been reported rarely in no more than 1.9% of subjects affected with Behcet's disease. It usually occurs in men younger than 40 years old and mostly involves the right chambers of the heart [7,8].
The precise mechanism leading to the formation of thrombi in Behcet's disease is unknown; however, endothelial cell injury and hypercoagulability are incriminated in the pathogenetic process similar to other disorders with increased risk of thrombosis.
There is currently, no consensus regarding the treatment of cardiac thrombus associated with Behcet's disease, but most experts recommend an aggressive immunosuppressive treatment with a combination of cyclophosphamide and high-dose corticosteroid, associated or not with anticoagulation.
The use of anticoagulation remains controversial. At first glance it looks like a contradiction to not use anticoagulation in a patient with thrombosis, however, the most important cause of mortality in patients with Behcet's disease is pulmonary arterial aneurysm rupture, and the use of anticoagulation exposes the patient to high hemorrhagic risk, the reason for which, some authors do not recommend anticoagulation and treat patients with cardiac thrombus with only immunosuppressive therapy [7].
Our patient received oral anticoagulation with close follow-up, and no adverse events have been reported to date.
Conclusion
The development of intracardiac thrombi is a rare and life-threatening manifestation of Behcet's disease. It should be kept in mind facing young patients with Behcet's disease, especially in the presence of pulmonary embolism or pulmonary artery aneurysm. The treatment is still not codified by clear consensus, making immunosuppressive therapy the only sure option facing the controversy of anticoagulation use in the absence of controlled trials.
Patient consent
Informed written consent was obtained from the patient for publication of the case report and all imaging studies.
Footnotes
Competing Interests: The authors declare no competing interest.
Contributor Information
Mohamed El Minaoui, Email: m.elminaoui@uiz.ac.ma.
Amine EL Houari, Email: dr.elhouari.amine@gmail.com.
References
- 1.Aksu T, Tufekcioglu O. Intracardiac thrombus in Behçet's disease: four new cases and a comprehensive literature review. Rheumatol Int. 2015;35(7):1269–1279. doi: 10.1007/S00296-014-3174-0. [DOI] [PubMed] [Google Scholar]
- 2.Jennette JC. Overview of the 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Clin Exp Nephrol. 2013;17(5):603. doi: 10.1007/S10157-013-0869-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davatchi F, Assaad-Khalil S, Calamia KT, Crook J E, Sadeghi-Abdollahi B, Schirmer M, et al. The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28(3):338–347. doi: 10.1111/JDV.12107. [DOI] [PubMed] [Google Scholar]
- 4.Demirelli S, Degirmenci H, Inci S, Arisoy A. Cardiac manifestations in Behcet's disease. Intractable Rare Dis Res. 2015;4(2):70. doi: 10.5582/IRDR.2015.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hatemi G, Seyahi E, Fresko I, Talarico R, Hamuryudan V. One year in review 2020: Behçet's syndrome. Clin Exp Rheumatol. 2020;38(5):3–10. https://www.clinexprheumatol.org/abstract.asp?a=16573 [PubMed] [Google Scholar]
- 6.Farouk H, el Chilali K, Said K, Sakr B, Salah H, Mahmoud G, et al. Value of certain echocardiographic findings in the initial suspicion of Behçet’s disease. Echocardiography (Mount Kisco, NY) 2014;31(8):924–930. doi: 10.1111/ECHO.12601. [DOI] [PubMed] [Google Scholar]
- 7.Emmungil H, Yaşar Bilge NŞ, Küçükşahin O, Kılıç L, Okutucu S, Gücenmez S, et al. A rare but serious manifestation of Behçet’s disease: intracardiac thrombus in 22 patients. Clin Exp Rheumatol. 2014;32:S87–S92. https://www.clinexprheumatol.org/abstract.asp?a=8163 [PubMed] [Google Scholar]
- 8.Yıldırım R, Dinler M, Yaşar Bilge NŞ, Kaşifoğlu T. A rarely seen manifestation in Behcet's disease: intracardiac thrombosis. Clin Rheumatol. 2021;40(10):4355–4356. doi: 10.1007/S10067-021-05720-9. [DOI] [PubMed] [Google Scholar]