Abstract
Residential racial segregation in the U.S. has been hypothesized as a fundamental cause driving health disparities across racial groups. Potential mechanisms include economic and social marginalization, subsequent constrained opportunities, and high stress. Yet evidence on residential segregation's association with health among Black and White children—particularly longitudinally—is sparse. This study aims to address this gap. We used data from the Panel Study of Income Dynamics (PSID), a national longitudinal study of U.S. households, analyzing information on 1,251 Black and 1,427 White children who participated in the Child Development Supplement (CDS) at least twice (survey waves 1997, 2002, 2007, 2014). We fit individual fixed-effects models to estimate the within-person association of neighborhood-level residential segregation, measured with local Getis-Ord G* statistics, with three outcomes (general health, weight status, and behavioral problems). We examined heterogeneous effects by age and sex. We also examined associations between health and childhood segregation trajectories, i.e., the pattern of children's residential segregation exposures from birth through when their health outcomes were measured, providing additional insight on dynamic experiences of segregation. In fixed effects models, among Black children, higher segregation was associated with worse self-rated health, especially for Black children who were older (aged 11–17 years). In trajectory models, among White children, moving out of highly segregated neighborhoods was associated with a lower probability of poor self-rated health, while moving into those neighborhoods or back and forth between neighborhood types were both associated with increased behavioral problems. Our findings highlight the importance of early-life residential segregation in shaping persistent racial health disparities, as well as the costs of segregation for all children living in highly segregated neighborhoods.
Keywords: Segregation, Neighborhoods, Racism, Child health, Health inequities
Highlights
-
•
We used a national longitudinal data set with rich health and residential history data observed throughout childhood.
-
•
We employed fixed effects models and trajectory models.
-
•
Living in segregated neighborhoods was associated with poorer self-rated health among Black and White children.
-
•
Moving into segregated neighborhoods was associated with more behavioral problems among White children.
-
•
Interventions are needed to reduce segregation and improve health-promoting resources for children in segregated communities.
1. Introduction
In the U.S., Black-White inequities persist across an array of health outcomes (Beck et al., 2020; Forde et al., 2019; Ghafoor et al., 2002; Mensah et al., 2005). Disparities arise early in life, with Black infants having significantly worse outcomes at birth (e.g., low birth weight, mortality) (Lu et al., 2010). Black children are more likely to have worse self-rated health (Montgomery et al., 1996) and higher levels of blood lead (Chen et al., 2006; Pamuk et al., 1998), to be overweight or obese (May et al., 2013), and to be hospitalized for treatable conditions such as asthma (Starfield, 1989).
Residential racial segregation has been hypothesized as a fundamental cause driving these inequities, as predominantly Black segregated neighborhoods on average have fewer resources and opportunities that promote physical and mental health (White & Borrell, 2011; Williams & Collins, 2016). Accordingly, prior research has shown negative associations between residential segregation and health among Black people in the U.S., with most work focused on infant mortality and adult outcomes including cardiovascular disease, cancer, dementia, obesity, and diabetes-related mortality (Kershaw et al., 2015; Kershaw & Pender, 2016; Landrine et al., 2017; Pohl et al., 2021; Polednak, 1996; Schwartz et al, 2022). Less work has investigated the association between residential segregation and health during childhood, a critical development stage for determining lifelong health. Early health can have enduring consequences for chronic morbidity in later life (Blackwell et al., 2001); hence, early disparities can produce a wide range of long-run impacts on population well-being. Moreover, existing evidence on the health effects of residential segregation relies heavily on analyses using a single exposure period or based on narrow geographies that limit generalizability.
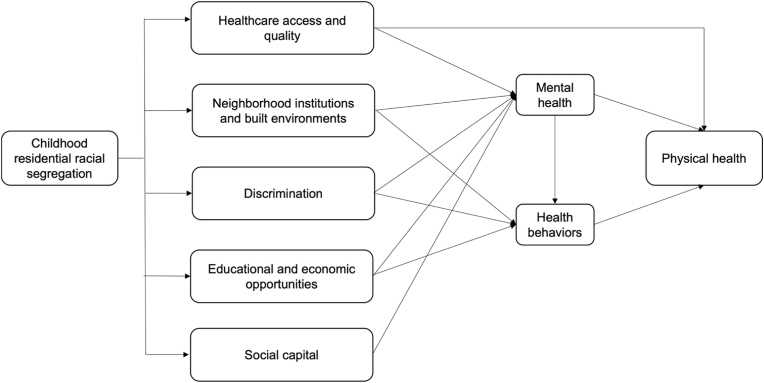
Understanding the health effects of residential segregation is critical. More than 80% of U.S. metropolitan regions are more segregated now than in 1990, and segregation levels nationally remain high (Natividad, 2021). Between 2014 and 2018, a typical White person in a large metropolitan area lived in a neighborhood with 71% White and 8% Black people, while a typical Black person lived in a neighborhood with 45% Black and 31% White people (Loh et al., 2020). Residential racial segregation is a manifestation of structural racism driven by both historical racist government policies and laws (e.g., redlining) (Finkelman, 1992; Krieger et al., 2020) and current political and economic arrangements that marginalize low-income and racial/ethnic minority people (Lichter et al., 2012). As a result, racially/ethnically segregated, majority of-color (particularly, Black) communities receive a lower distribution of health-promoting resources compared to segregated White communities and a higher distribution of health risks, leading to racial/ethnic inequities in health through multiple pathways (Fig. 1).
Fig. 1.
Conceptual framework.
First, segregated Black communities often lack high-quality healthcare facilities and physicians (Gaskin et al., 2012; Vaughan Sarrazin et al., 2009; White et al., 2012). Second, segregated neighborhoods are more likely to serve as environments that damage health, such as being targeted for advertising of unhealthy products (e.g., fast food, sugar-sweetened beverages, and tobacco products), having limited access to healthy groceries (e.g., fresh fruits and vegetables) (Fischer et al., 2021; Harris et al., 2019; Kirchner et al., 2015; Primack et al., 2007; Scott et al., 2020), or being exposed to higher levels of harmful pollutants and poor living conditions (e.g., poor housing quality) (Jesdale et al., 2013; Woo et al., 2019). Third, living in segregated neighborhoods can lead to a sense of isolation or experiences of discrimination (e.g., disproportionate policing), thereby increasing stress (Massey, 2004; Williams & Mohammed, 2009). Chronic stress can dysregulate endocrine, immune, and nervous system function, causing higher allostatic load and inflammation that increases risk of poor physical health (Beck et al., 2020; Fagundes et al., 2013; Gouin, 2011). High stress can also lead to poor mental health and a higher likelihood of turning to unhealthy coping behaviors (Jackson et al., 2010; Yoo, 2019). Fourth, living in segregated neighborhoods that are denied quality educational opportunities and that experience economic disinvestment may worsen educational and economic outcomes, which are essential for healthy development and future socioeconomic opportunities (Adler & Ostrove, 1999; Glymour et al., 2014). Finally, social capital, identified as the degree of social trust and support provided reciprocally between individuals in a given area, has been proposed to contribute to positive health (Kawachi, 1999). The impact of segregation on social capital is mixed (Kramer & Hogue, 2009), and a few studies have found that segregation could potentially offer protective effects for minoritized people by providing stronger social cohesion and lowering exposure to interpersonal racism (Diette et al., 2021; Fang et al., 1998; Halpern, 1993).
Given these mechanisms, we hypothesized that childhood experiences of residential racial segregation may adversely affect children's health. We also hypothesized that this relationship may differ by age and sex. Prior work has found that the association of neighborhood environment with health and social outcomes differs by age due to differences in how neighborhood environments are experienced at different ages (Chetty et al., 2016; Hamad et al., 2020). For example, while changes that improve the built environment and lower stress are likely to improve well-being, disruptions in existing social networks may outweigh the benefits of positive neighborhood change for older children, whose development is more reliant on social relationships outside of the home compared to their younger peers (Anderson et al., 2014; Chetty et al., 2016). Prior work has also found that girls experience positive health or behavioral effects from interventions providing an incentive to move to lower-poverty neighborhoods, while boys' mental and behavioral health may be harmed, suggesting that gendered social experiences may powerfully modify the health effects of neighborhood change (Smith & Schwartz, 2021).
In this study, we used data from a national panel study of U.S. households and rigorous methods to take advantage of the longitudinal data set. We focused on Black and White children's health outcomes, including self-rated health, weight status, and behavioral problems, and we examined whether the associations differed by age and sex. This study therefore provides important evidence to understand the effects of social and structural factors on racial health inequities throughout childhood.
2. Methods
2.1. Data
We used data from the Child Development Supplement (CDS) of the U.S. Panel Study of Income Dynamics (PSID). PSID is a longitudinal household survey initiated in 1968 that includes rich information about individual and family characteristics. PSID was designed to be nationally representative and has since followed participants, their descendants, and their descendants' families with annual surveys through 1997 and biennial surveys thereafter. While PSID's core surveys only collect health information on household heads and their spouses, PSID began the CDS in 1997 to collect extensive data on children aged 0–12 years. Two follow-up surveys of children under 18 were conducted in 2002 and 2007. In 2014, a new CDS cohort was launched for all PSID children aged 0–17 years; this was the most recent available wave of CDS data when analysis began.
We linked all available CDS waves through 2014 with the core PSID data to compile a longitudinal history of each child's family information, including geocoded residential location, family income, and parental marital status. We used sample participants' residential census tracts to merge in residential segregation measures generated from the U.S. Census (described below).
2.2. Sample selection
The total number of children included in the CDS waves was 7820. We only included Black and White children because of small sample sizes and inconsistent categorization of racial/ethnic groups across time for other racial/ethnic groups within PSID. Given our use of fixed effects models (described below), we then restricted the sample to children with at least two CDS observations, as estimation of these models is only driven by changes in exposures and outcomes between repeated observations of the same individual. Of 7229 children (Black = 3354, White = 3875) that ever participated in any CDS wave, 2762 children (Black = 1263, White = 1499) participated at least twice. All of them had at least one measured health outcome in each wave. Among these 2762 children, we excluded 84 children (∼3%) who had missing data on any relevant covariates or exposure data (e.g., due to missing address or unavailable segregation measures in their residential census tract). We therefore conducted complete case analysis, as this is not thought to result in bias at such low levels of missingness (Allison, 2009). The final sample size was thus 2678 children (Black = 1251, White = 1427).
2.3. Exposure
Residential racial segregation was measured with local Getis-Ord G* statistics, a widely used measure among segregation-health studies that robustly captures spatial features of segregation (Caunca et al., 2020; Kershaw & Albrecht, 2015; Kershaw & Pender, 2016; Salow et al., 2018). We calculated G* statistics at the census tract level using data from the decennial Census (1990, 2000, 2010) and American Community Survey 5-year estimates (2010–2014, 2014–2018), with tracts normalized to 2010 boundaries. G* statistics for each observed year were calculated using the nearest available Census in time. For example, G* statistics for 1996–2005 were calculated using the 2000 decennial Census.
G* statistics are Z-scores that measure how unusual the racial composition of a given census tract and neighboring tracts are in relation to the racial composition of their larger surrounding area (e.g., Metropolitan or Micropolitan Statistical Area). To focus on the ways that the segregation of Black people in the U.S. leads to disinvestment and a concentration of disadvantage produced by anti-Black racism, we focus on the segregation of Black residents. Specifically, we calculated a Z-score representing the difference in standard deviations between (A) the average percentage of residents who were Black in a focal tract and its neighboring tracts and (B) the mean percentage of residents who were Black across all of the tracts within its surrounding Core-Based Statistical Area (CBSA), or within the same county if tracts did not belong to a CBSA. In estimating each tract's G* statistics, we spatially weighted the contribution of the racial composition of focal tract vs. neighborhood tracts using “queen” spatial contiguity, whereby all tracts whose borders touched the focal tract were considered its neighbors. More details on this exposure measure are provided in Appendix A.
2.4. Health outcomes
We selected three indicators of child health that are likely to be affected by residential segregation based on hypothesized mechanisms mentioned above: general health status, obesity, and behavioral problems. General health status (a 5-point Likert scale from poor to excellent) was asked of both primary caregivers (for children at any age) and children aged 8 years and above. In the case that caregivers and children both answered this question and gave different answers, we chose the one indicating poorer health. We dichotomized general health as poor, fair, or good versus very good or excellent, a common way to categorize general health in the literature about child health (Bauman et al., 2006; Flores et al., 1999) (Appendix B). Second, we included a binary outcome indicating whether the child was overweight or obese. The CDS interviewer gathered data about the child's height and weight at the time of the interview. In wave I, height was measured by the interviewer and weight was reported by the primary caregiver. Height and weight were both measured by the interviewer in later waves. Categories for body mass index (BMI) were calculated based on standard growth charts that take into account children's age and sex (Kuczmarski, 2000). Overweight or obese was defined as BMI over the 85th percentile (Hofferth et al., 1997). Although these weight categories are not reliable individual-level health indicators, they are useful correlates of future risk of cardiometabolic health problems when considered at the population level (Carbone et al., 2019; Krauss et al., 1998). Third, we included the Behavioral Problems Index (BPI: range: 0–27), a validated scale that measures externalizing or aggressive behavior, and internalizing or sad behavior (Peterson & Zill, 1986). A higher score indicates worse socioemotional well-being. A large literature has linked inequities in child behavioral problems with social and economic marginalization, and children with worse behavioral conditions are more likely to have lower educational attainment, an important determinant of future health (Currie et al., 2010; Gupta et al., 2007; Hamad & Rehkopf, 2016).
2.5. Covariates
We adjusted for time-variant individual and family covariates that may represent confounders of the relationship between residential segregation and child health, including age (at the time of outcome ascertainment), sex, inflation-adjusted family income, parental marital status. We also adjusted for census tract-level population and poverty rate. The latter was defined as the proportion of individuals living under the federal poverty threshold, a specified dollar amount updated annually by the U.S. Census Bureau that is considered to be the minimum level of resources necessary to meet the basic needs of a family unit.
2.6. Analysis
2.6.1. Primary analysis: fixed effects models
To explore the relationship between residential segregation and child well-being, we used fixed-effects (FE) regression models. In essence, these FE models involved the inclusion of an indicator variable for each child, thereby estimating the within-person association of neighborhood-level segregation changes with changes in the outcomes of interest. The advantage of these FE models is that they account for all observed and unobserved individual-level, time-invariant confounders, reducing bias from between-person comparisons.
In these models, we included the segregation exposure (i.e., the G* statistic) as a continuous variable and controlled for time-varying covariates listed above. As a robustness check, we excluded family income and neighborhood characteristics because they may also serve as mediators of the relationship between residential segregation and child health (Quillian, 2012). For all analyses, we estimated linear models using ordinary least squares (OLS). For binary outcomes, these are considered linear probability models. The estimated coefficients for binary outcomes thus represent a percentage point change in the risk of the outcome. Logistic regression was not used for binary outcomes in the FE models for two reasons: first, it is difficult to compute the maximum likelihood estimation (MLE) of the coefficients of non-linear models with a large number of dummy variables (i.e., indicators for each child), as the models fail to converge (Greene, 2004); and second, logistic regression in FE models drops observations that have no variation in the outcome, reducing the power of the analyses (Timoneda, 2021). While linear probability models may result in predicted probabilities of the outcome that are outside of the 0–1 range, prior work has also shown that the statistical properties of linear regression for binary outcomes are less problematic with large sample sizes like ours (Hellevik, 2009).
2.6.2. Subgroup analyses by age and sex
In subgroup analyses, we first assessed whether the relationship between segregation and our outcomes varied by the child's age of exposure by including an interaction term between G* statistics and whether the child was aged 11–17 vs. younger than 11 years at the time of interview. We chose 11 years as the cutoff because it is the age that children typically start middle school and enter early adolescence, and a time when they may interact with their neighborhood environment differently compared with younger peers (Eccles, 1999). We also assessed whether associations varied by sex. Of note, PSID does not include a question on gender identity, so we used the variable for sex as a proxy to capture gendered social experiences. For models testing heterogeneous effects by sex, we conducted FE regressions by including an interaction term between G* statistics and whether the child was female.
2.6.3. Secondary analysis: estimating effects of segregation trajectories
We also examined the relationship between early-life trajectories of segregation exposure and child health, leveraging PSID's longitudinal data on households' residential neighborhoods. We observed the whole trajectories of children's residential locations up until each participant's health outcomes were measured using data on their families' residences since birth from PSID's core data collection. Using trajectories in this way compensates for a drawback of the FE analysis whereby the FE models only capture a few snapshots of time, when participants were interviewed for each CDS wave. Capturing children's early-life trajectories can provide additional insight into the association between longitudinal exposure to residential segregation and child well-being, providing a richer sense of the potential influence of the duration of exposure to segregation. However, we note that this method may generate results that are more likely to suffer from confounding from time-invariant factors than FE models because comparisons are made between rather than only within children.
For this trajectory analysis, we included all children who participated in CDS waves at least once and used their entire observed residential history from birth through outcome ascertainment to measure their trajectories of segregation exposure prior to their observed health outcomes. Among 7229 children (Black = 3354, White = 3875), 15 children had no measured health outcomes and 65 children had missing exposure data. Thus, the final sample for this secondary analysis included 7149 children (Black = 3301, White = 3848). Note that children who participated in multiple CDS survey waves had health outcomes measured multiple times, and we used all available person-year observations (Black = 5198, White = 6089). We thus clustered our standard errors at the individual level to account for within-person correlation across repeated observations.
We categorized each participant's segregation exposure into five trajectories: (1) always lived in a low-segregation neighborhood (reference), (2) always lived in a high-segregation neighborhood, (3) moved from a low-to high-segregation neighborhood, (4) moved from a high-to low-segregation neighborhood, and (5) moved back and forth between high- and low-segregation neighborhoods. Note that “moved” can indicate either moving to a neighborhood with a different segregation level, or a change of segregation level in the current neighborhood. However, the latter was uncommon: in our sample, more than 88% of changes in trajectories were caused by moving to a different neighborhood.
In these models, we defined a neighborhood as highly segregated if its G* was greater than 1.96 (two standard deviations above the mean), and “low” otherwise, a standard dichotomization in the existing segregation literature (Kershaw et al., 2017). A high-segregation neighborhood means that the area and its neighborhoods had a high proportion of residents who were Black compared to the average within their CBSA or county. While tracts with a G* statistic below −1.96 were also highly segregated with disproportionately fewer Black residents, those neighborhoods are not systematically targeted for disinvestment. Models were adjusted for age, sex, inflation-adjusted family income (at baseline, i.e., child's earliest observation in CDS), parental marital status, and census-tract level population and poverty rate (at baseline). As above, we estimated linear models by OLS, and we conducted a robustness check by excluding family income and neighborhood covariates. We did not examine differential associations by age or sex due to limited power caused by smaller sample sizes in each trajectory type stratified by age or sex.
3. Results
3.1. Descriptive summary
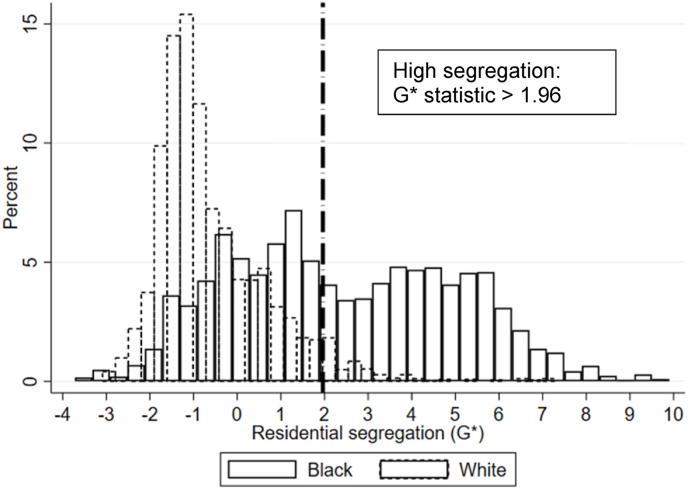
Of the 2678 Black and White children who participated in CDS at least twice, about 47.3% of Black children and 50.2% of White children were female (Table 1). At baseline, the mean age was 6.1 years (SD = 3.6) for Black children and 5.7 years (SD = 3.6) for White children. Black children were more likely to have lower family incomes (mean $44,241, SD $39,263) compared with White children (mean income $92,500, SD $80,526). Black children were also substantially less likely to have married parents compared with White children (40.7% vs. 81.7%) and experienced higher neighborhood poverty rates (22.3% vs. 9.9%). The average level of residential segregation at baseline was 2.7 for Black children and −0.5 for White children, indicating that Black children were more likely to live in high-segregation areas. Fig. 2 illustrates the distribution of residential segregation among Black and White children.
Table 1.
Descriptive statistics.
| Black (N = 1251) Percent or mean (SD) | Person-year observations | White (N = 1427) Percent or mean (SD) | Person-year observations | |
|---|---|---|---|---|
| Health outcomes | ||||
| Poor/fair/good health | 22.4 | 3079 | 10.7 | 3532 |
| Overweight/obese | 41.7 | 2638 | 32.0 | 3035 |
| Behavioral problems index | 8.4 (6.5) | 2786 | 8.4 (6.2) | 3131 |
| Individual characteristics (baseline) | ||||
| Age (years) | 6.1 (3.6) | 5.7 (3.6) | ||
| Female | 47.3 | 49.7 | ||
| Family income (USD) | 44241 (39263) | 92550 (80526) | ||
| Parents married | 40.7 | 81.7 | ||
| Residential segregation | 2.7 (2.7) | −0.5 (1.3) | ||
| Neighborhood characteristics | ||||
| Population | 4263 (1515) | 4357 (1464) | ||
| Poverty rate | 22.3 (13.1) | 9.9 (8.1) | ||
Note: Data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 1251 Black children and 1427 White children who participated in CDS waves at least twice. Residential segregation was measured using local Getis-Ord G* statistics. Neighborhood was defined as census tract.
Fig. 2.
Distribution of residential segregation among Black and White children
Note: Data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 1251 Black children and 1427 White children who participated in CDS waves at least twice. Residential segregation was measured using local Getis-Ord G* statistics.
There were clear health inequities by race. While 22.4% of Black children reported poor/fair/good health (vs. very good/excellent), only 10.7% of White children did so. About 41.7% of Black children vs. 32.0% of White children were classified as overweight/obese. However, the mean BPI score for Black and White children was similar, at 8.4 (SD 6.5 for Black children and 6.2 for White children).
3.2. Primary analysis: residential segregation and child health with fixed effects models
We first estimated the association of neighborhood residential segregation with each outcome (Table 2). Among Black children, a 1-SD increase in segregation was associated with a 1.1 percentage point increase in the probability of having worse self-rated health ( = 0.011; 95% CI, 0.002, 0.020), i.e., a 4.9% change. We were unable to reject the null hypothesis that segregation was not associated with weight status and behavioral problems. For White children, higher segregation was not associated with self-rated health and behavioral problems, while a 1-SD increase in segregation was associated with a 2.6 percentage point decreased probability of being overweight/obese ( = -0.026; 95% CI, −0.051, −0.001), i.e., an 8.1% change. Results were similar when we excluded family income and neighborhood covariates (Appendix Table C1).
Table 2.
Association of residential segregation with child health outcomes, by race.
| Estimated coefficient [95% CI] |
|||
|---|---|---|---|
| Poor/fair/good health | Overweight/obese | Behavioral problems index | |
| Black children | 0.011* [0.002 0.020] | −0.012 [-0.026, 0.002] | 0.031 [-0.122, 0.184] |
| White children | 0.005 [-0.010, 0.019] | −0.026* [-0.051, −0.001] | 0.214 [-0.091, 0.518] |
*p < 0.05, **p < 0.01.
Note: Sample data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 1251 Black children and 1427 White children who participated in CDS waves at least twice. Residential segregation was measured using local Getis-Ord G* statistics. Neighborhood was defined as census tract. Coefficients were estimated using linear regression models with individual fixed effects, adjusting for individual and neighborhood characteristics. Standard errors were clustered at the individual level.
3.3. Subgroup analyses by age and sex
We then assessed whether the relationship between segregation and the outcomes varied by child age (Table 3). For Black children, associations between segregation and self-rated health were stronger among older children (aged 11–17 years). A 1-SD increase in segregation was associated with a 1.3 percentage point greater increase in the probability of reporting worse self-rated health for older children compared with younger children (coefficient on the interaction term = 0.013; 95% CI, 0.001, 0.025). For White children, the association of residential segregation with the health outcomes did not differ by age. In models assessing whether the relationship between segregation and the outcomes varied by child sex (Table 4), no differences were found between male and female children across all outcomes.
Table 3.
Association of residential segregation with child health outcomes, by race and age of exposure.
| Estimated coefficient [95% CI] |
|||
|---|---|---|---|
| Poor/fair/good health | Overweight/obese | Behavioral problems index | |
| Black children | |||
| Segregation * age above 11 years | 0.013* [0.001, 0.025] | −0.005 [-0.018, 0.008] | 0.043 [-0.120, 0.207] |
| Segregation | 0.006 [-0.005, 0.016] | −0.010 [-0.025, 0.006] | 0.011 [-0.156, 0.177] |
| Age above 11 years | −0.062* [-0.120, −0.004] | 0.026 [-0.043, 0.095] | −0.168 [-0.973, 0.636] |
| White children | |||
| Segregation * age above 11 years | 0.004 [-0.012, 0.021] | 0.020 [-0.008, 0.049] | −0.009 [-0.326, 0.307] |
| Segregation | 0.003 [-0.012, 0.018] | −0.032* [-0.061, −0.004] | 0.214 [-0.101, 0.530] |
| Age above 11 years | 0.002 [-0.035, 0.038] | 0.030 [-0.027, 0.087] | −0.145 [-0.782, 0.492] |
*p < 0.05, **p < 0.01.
Note: Sample data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 1251 Black children and 1427 White children who participated in CDS waves at least twice. Residential segregation was measured using local Getis-Ord G* statistics. Neighborhood was defined as census tract. Coefficients were estimated using linear regression models with individual fixed effects, adjusting for individual and neighborhood characteristics. Standard errors were clustered at the individual level.
Table 4.
Association of residential segregation with child health outcomes, by race/ethnicity and sex.
| Estimated coefficient [95% CI] |
|||
|---|---|---|---|
| Poor/fair/good health | Overweight/obese | Behavioral problems index | |
| Black children | |||
| Segregation * female | −0.008 [-0.025, 0.010] | −0.005 [-0.029, 0.019] | 0.210 [-0.068, 0.489] |
| Segregation | 0.015* [0.002, 0.027] | −0.010 [-0.028, 0.009] | −0.076 [-0.284, 0.132] |
| White children | |||
| Segregation * female | −0.005 [-0.032, 0.021] | 0.001 [-0.049, 0.051] | −0.208 [-0.809, 0.393] |
| Segregation | 0.007 [-0.012, 0.026] | −0.027 [-0.063, 0.010] | 0.317 [-0.150, 0.785] |
*p < 0.05, **p < 0.01.
Note: Sample data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 1251 Black children (female = 589; male = 662) and 1427 White children (female = 712; male = 715) who participated in CDS waves at least twice. Residential segregation was measured using local Getis-Ord G* statistics. Neighborhood was defined as census tract. Coefficients were estimated using linear regression models with individual fixed effects, adjusting for individual and neighborhood characteristics. Standard errors were clustered at the individual level. Main effects for sex were omitted because time-invariant variables are not estimated in FE models.
3.4. Secondary analysis: residential segregation trajectories and child health
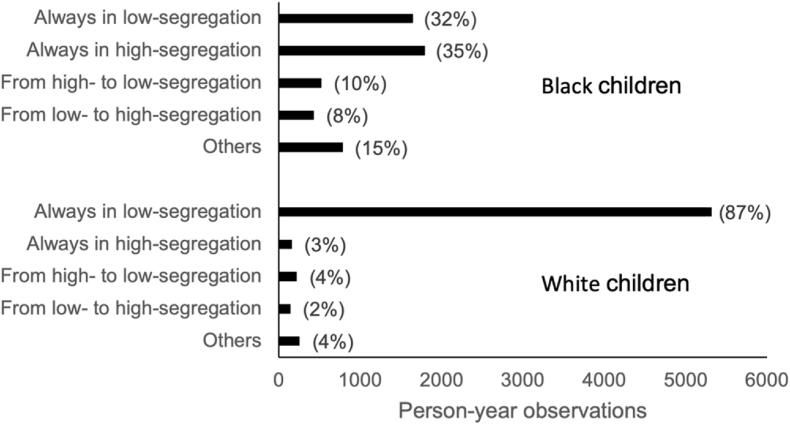
In examining the association between early-life trajectories of exposure to segregation and child health, we found that the distribution of trajectories for Black and White children differed widely (Fig. 3). The percentage of Black children who always lived in high- or low-segregation neighborhoods was about 30% for each neighborhood type; 10% of Black children moved from high-to low-segregation neighborhoods; and 8% moved from low-to high-segregation neighborhoods. The remaining 15% moved back and forth between high- and low-segregation neighborhoods. In contrast, about 87% of White children always lived in low-segregation neighborhoods, while only 3% always lived in high-segregation neighborhoods. The percentage of White children who moved from high-to low-segregation neighborhoods, from low-to high-segregation neighborhoods, or who moved back and forth was 4%, 2%, and 4%, respectively. Thus, White children consistently lived in low-segregation neighborhoods at three times the rate of Black children, while Black children consistently lived in high-segregation neighborhoods at ten times the rate of White children.
Fig. 3.
Residential segregation trajectories, by race
Note: Data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 3253 Black children and 3628 White children who participated in CDS waves at least once. Residential segregation was measured using local Getis-Ord G* statistics.
Regression results from trajectory models (Table 5) showed that Black children who moved from high-to low-segregation neighborhoods were less likely to report poor health ( = -0.060; 95% CI, −0.103, −0.017), compared with those living in low-segregation neighborhoods for the entire period, while those who moved from low-to high-segregation neighborhoods were less likely to be overweight/obese ( = -0.062; 95% CI, −0.122, −0.001). For White children, those who moved from high-to low-segregation neighborhoods were less likely to report poorer health ( = -0.036; 95% CI, −0.055, 0.020), compared with those living in low-segregation neighborhoods throughout. Also, for White children, moving from low-to high-segregation neighborhoods was associated with more behavioral problems ( = 1.52, 95% CI, 0.23, 2.82), as was moving back and forth between low- and high-segregation neighborhoods ( = 1.74; 95% CI, 0.71, 2.77). Results were similar when we excluded family income and neighborhood covariates (Appendix Table C2).
Table 5.
Association of childhood residential segregation trajectories with child health, by race.
| Estimated coefficient [95% CI] |
|||
|---|---|---|---|
| Poor/fair/good health | Overweight/obese | Behavioral problems index | |
| Black children | |||
| Always in low segregation | ref. | ref. | ref. |
| Always in high segregation | −0.030 [-0.064, 0.004] | 0.002 [-0.044, 0.047] | −0.076 [-0.716, 0.564] |
| From high to low segregation | −0.060** [-0.103, −0.017] | −0.024 [-0.083, 0.034] | −0.151 [-0.645, 0.947] |
| From low to high segregation | −0.041 [-0.086, 0.005] | −0.062* [-0.122, −0.001] | 0.635 [-0.199, 1.460] |
| Others | −0.025 [-0.066, 0.017] | −0.006 [-0.059, 0.047] | −0.358 [-1.077, 0.362] |
| White children | |||
| Always in low segregation | ref. | ref. | ref. |
| Always in high segregation | 0.007 [-0.056, 0.070] | 0.006 [-0.087, 0.098] | −0.788 [-2.026, 0.450] |
| From high to low segregation | −0.036* [-0.055, 0.020] | −0.013 [-0.085, 0.058] | −0.200 [-1.257, 0.856] |
| From low to high segregation | 0.053 [0.013, 0.118] | 0.041 [-0.048, 0.131] | 1.523* [0.232, 2.815] |
| Others | 0.044 [-0.010, 0.098] | 0.033 [-0.036, 0.102] | 1.741** [0.711, 2.772] |
*p < 0.05, **p < 0.01.
Note: Data were drawn from the Panel Study of Income Dynamics' Child Development Supplement (CDS) waves in 1997, 2002, 2007, and 2014. Sample includes 3253 Black children and 3628 White children who participated in CDS waves at least once. Residential segregation was measured using local Getis-Ord G* statistics. High segregation was defined as G* statistics greater than 1.96. Neighborhood was defined as census tract. Coefficients were estimated using linear regression models with individual fixed effects, adjusting for individual and neighborhood characteristics. Standard errors were clustered at the individual level to account for within-person correlation.
4. Discussion
In this study, we investigated the association between residential racial segregation and child health using data from a U.S. nationwide longitudinal study that followed respondents’ residential locations and health outcomes throughout childhood, using both fixed effects and trajectory models. We found that higher residential segregation was associated with several worse outcomes among Black and White children, even conditioning on individual and neighborhood characteristics.
First, our results suggest that residential segregation has negative impacts on Black children's self-rated health, a powerful predictor of disease and mortality (Jylhä, 2009). This was especially the case for older Black children (aged 11–17 years). While the majority of prior research has found a negative association between residential segregation and individual health among Black people (Schwartz et al., 2022; Williams et al., 2019), some studies have found the opposite, arguing that segregation could potentially offer protective effects for Black people by providing stronger social cohesion and lowering exposure to interpersonal racism (Fang et al., 1998; Halpern, 1993). Our results are aligned with the majority of past research, indicating that residential segregation has more harms than benefits for individual health, especially for older children, such that the adverse effects of structural and institutional racism in segregated neighborhoods may outweigh any benefits of avoiding interpersonal racism in the immediate neighborhood environment. Further, among White children, moving out of high-segregation neighborhoods during childhood was associated with a lower probability of poor self-rated health. This suggests that at least some of the negative health consequences of under-resourced highly segregated neighborhoods are shared across race.
Interpreting our results on behavioral problems across race similarly requires an eye towards the balance between positive and negative health exposures that may accompany segregation. Specifically, among Black children, we found no relationship between segregation and behavioral problems; in contrast, White children who moved into high-segregation neighborhoods saw more behavioral problems than those who always lived in low-segregation neighborhoods. We interpret this as reflecting a different balance between the countervailing influences alluded to above across race: (A) negative environmental exposures in highly segregated Black neighborhoods resulting from disproportionate disinvestment in these communities—which affect all children, across race—and (B) the positive effects of social cohesion and community among Black people, which only affect Black children. For behavioral problems, unlike for self-rated health, we interpret our findings as suggesting that these two forces appear to balance among Black children. Thus, among Black children we see null results for behavioral problems, while among White children highly segregated neighborhoods appear straightforwardly damaging.
Past research suggests these “negative environmental exposures” for behavioral problems could take several forms. For instance, living in segregated neighborhoods with severely low resources may be associated with higher levels of stress coupled with fewer institutional supports for children's mental health and wellness. This may collectively lead to a heavier burden for managing mental and emotional challenges (Huesmann & Guerra, 1997; Singh & Ghandour, 2012). Further, segregated neighborhoods may incite or exacerbate behavioral health problems through harmful institutional environments downstream of residential segregation. Racially segregated schools, for example—which suffer from inequitable funding and aggressive school discipline—have been found to have a negative impact on behavioral problems among Black children (Wang et al., 2022). In addition, residential segregation may affect child behavioral problems through both family and community exposure to environmental insults (Sellström & Bremberg, 2006). Prior studies have found that living in disadvantaged neighborhoods was associated with adverse childhood experiences through heightened psychological distress for their parents and a less favorable psychosocial environment (e.g., exposure to higher levels of community violence driven by neighborhood disadvantage) (Mersky et al., 2017). Meanwhile, strengthened community ties through shared experiences and Black community institutions may be protective for behavioral problems among Black children (Halpern, 1993; Williams & Collins, 2016). Future research is needed to investigate the degree to which these positive and negative paths mediate the observed associations.
Our results for weight status suggest that residential segregation decreased the risk of being overweight/obese, potentially for both Black and White children. This contradicts our hypothesis that residential segregation may increase the chance of childhood overweight/obesity through channels such as limited access to healthy food or increased stress. Past findings on residential segregation and obesity have been mixed (Kershaw & Pender, 2016). Studies were mostly cross-sectional, focused on adults, and varied by the geographic scale of the segregation measure, gender, and race/ethnicity (Kershaw & Pender, 2016). In our case, we faced an additional measurement challenge: in CDS wave I, weight was reported by the primary caregiver at the time of the interview, which may have been inaccurate. Future research using other data sets with objective measures of height and weight may help clarify the literature and test the robustness of our findings.
Although we focus on child health, health problems during early life can cast a long shadow, and the potential negative impacts of residential segregation may accumulate and lead to poorer adult well-being (Caunca et al., 2020; Schwartz et al, 2022). Chronic stress caused by continuously living in high-segregation neighborhoods can reduce health and physiologic function over time, yielding lasting dysregulation (Glymour & Manly, 2008). Poor child health itself has also been found to be associated with a higher probability of chronic morbidity in later life (e.g., cancer, lung disease, cardiovascular conditions, and arthritis) (Blackwell et al., 2001), and worse social and economic outcomes (Smith, 2009).
Further, while anti-Black structural racism targets Black communities, our findings underscore that its existence makes neighborhoods pathogenic to other residents, not only those who are Black; residential segregation is a cross-racial public health problem. For example, our findings are consistent with prior work examining mortality from a 1995 heatwave in Chicago (Klinenberg, 2015). which demonstrated that older people—regardless of race—died at higher rates in predominantly Black neighborhoods and that these avoidable deaths were driven by Black residential communities systematically receiving less governmental support, making life-saving social support of older adults difficult to sustain. Similarly, while Black-White inequities in childhood asthma are large, disparities disappear in predominantly Black ZIP codes (Alexander & Currie, 2017), suggesting that children of many races are impacted by the negative health consequences of Black segregation.
Our study has several strengths. First, it is among the first to use a rich longitudinal data set and robust longitudinal analytic techniques to examine the association between residential segregation and child health outcomes. It thereby addresses challenges in previous studies that have been largely cross-sectional, only capturing a snapshot of the relationship between residential segregation and health at a single time point and potentially masking the dynamic nature of neighborhoods. Second, we used data from a nationwide sample, improving upon prior research conducted in more limited geographic areas. Third, despite a well-established literature linking residential racial segregation and adult health, research examining health during childhood, a critical stage of development, is limited; our study contributes to filling this gap.
Our study also has limitations. First, outcomes and covariates were self-reported and therefore may be subject to reporting biases. Second, we could not disentangle the multiple pathways through which residential segregation influences health, as these variables were not captured in PSID—e.g., neighborhood deprivation and disinvestment, constrained socioeconomic opportunities, discrimination, and social cohesion. Third, our results may suffer from reverse causation, in that a move to a high-segregation neighborhood may be the result of a family or child health problem, rather than the cause. Relatedly, while our exposure of interest is residential segregation, other factors associated with this exposure may also confound the relationship between segregation and these health outcomes; more complicatedly still, many of these (e.g., pollution levels) are also likely mediators between residential segregation and poor health, requiring more sophisticated methods, such as marginal structural models. Future studies can further tease apart specific mechanisms and address this through the identification and analysis of natural experiments. Finally, our research is limited to Black and White children and only focuses on anti-Black residential segregation; future research should use data sets with larger samples of other racial/ethnic groups and multi-group segregation measures to further examine how segregation affects children of all racial/ethnic groups.
5. Conclusion
The findings of this study suggest that living in more segregated neighborhoods was associated with poorer self-rated health among both Black and White children, and more behavioral problems among White children. The results highlight the importance of evaluating strategies that improve the health of segregated communities or eliminate segregation to benefit U.S. Americans of many racial groups. This could reduce persistent racial health disparities, ensuring that children are set up for a healthy present and future. Future studies should examine the effects of policies that promote residential integration or that provide more health-promoting resources for those living in segregated neighborhoods.
Ethical statement
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
All sources used are properly disclosed.
-
5)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
-
6)
The UCSF institutional review board provided ethical approval for this study (protocol # 21–33615).
Acknowledgement
This work was supported by a grant from the National Institute of Health under grant number R01 HL151638. The collection of PSID data used in this study by the University of Michigan Institute for Social Research was partly supported by the National Institutes of Health under grant number R01 HD069609 and R01 AG040213, and the National Science Foundation under award numbers SES 1157698 and 1623684. The funders had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101250.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The data that were used for this analysis are confidential due to the inclusion of geocodes. Interested users can apply for access to these data at https://psidonline.isr.umich.edu/.
References
- Adler N.E., Ostrove J.M. Socioeconomic status and health: What we know and what we don't. Annals of the New York Academy of Sciences. 1999;896(1):3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Alexander D., Currie J. Is it who you are or where you live? Residential segregation and racial gaps in childhood asthma. Journal of Health Economics. 2017;55:186–200. doi: 10.1016/j.jhealeco.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison P.D. In: Handbook of quantitative methods in psychology. Millsap R.E., Maydeu-Olivares A., editors. Sage Publications; 2009. Missing data; pp. 72–89. [Google Scholar]
- Anderson S., Leventhal T., Newman S., Dupéré V. Residential mobility among children: A framework for child and family policy. Cityscape. 2014;16(1):5–36. [Google Scholar]
- Bauman L.J., Silver E.J., Stein R.E. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321–1328. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- Beck A.F., Edwards E.M., Horbar J.D., Howell E.A., McCormick M.C., Pursley D.M. The color of health: How racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatric Research. 2020;87(2):227–234. doi: 10.1038/s41390-019-0513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell D.L., Hayward M.D., Crimmins E.M. Does childhood health affect chronic morbidity in later life? Social Science & Medicine. 2001;52(8):1269–1284. doi: 10.1016/s0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Carbone S., Canada J.M., Billingsley H.E., Siddiqui M.S., Elagizi A., Lavie C.J. Obesity paradox in cardiovascular disease: Where do we stand? Vascular Health and Risk Management. 2019;15:89. doi: 10.2147/VHRM.S168946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caunca M.R., Odden M.C., Glymour M.M., Elfassy T., Kershaw K.N., Sidney S., Yaffe K., Launer L., Al Hazzouri A.Z. Association of racial residential segregation throughout young adulthood and cognitive performance in middle-aged participants in the CARDIA Study. JAMA Neurology. 2020;77(8):1000–1007. doi: 10.1001/jamaneurol.2020.0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E., Martin A.D., Matthews K.A. Understanding health disparities: The role of race and socioeconomic status in children's health. American Journal of Public Health. 2006;96(4):702–708. doi: 10.2105/AJPH.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R., Hendren N., Katz L.F. The effects of exposure to better neighborhoods on children: New evidence from the moving to opportunity experiment. The American Economic Review. 2016;106(4):855–902. doi: 10.1257/aer.20150572. [DOI] [PubMed] [Google Scholar]
- Currie J., Stabile M., Manivong P., Roos L.L. Child health and young adult outcomes. Journal of Human Resources. 2010;45(3):517–548. [Google Scholar]
- Diette T.M., Hamilton D., Goldsmith A.H., Darity W.A. Does the negro need separate schools? A retrospective analysis of the racial composition of schools and black adult academic and economic success. RSF: The Russell Sage Foundation Journal of the Social Sciences. 2021;7(1):166–186. [Google Scholar]
- Eccles J.S. The development of children ages 6 to 14. The Future of Children. 1999:30–44. [PubMed] [Google Scholar]
- Fagundes C.P., Glaser R., Kiecolt-Glaser J.K. Stressful early life experiences and immune dysregulation across the lifespan. Brain, Behavior, and Immunity. 2013;27:8–12. doi: 10.1016/j.bbi.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J., Madhavan S., Bosworth W., Alderman M.H. Residential segregation and mortality in New York City. Social Science & Medicine. 1998;47(4):469–476. doi: 10.1016/s0277-9536(98)00128-2. Record #124 is using a reference type undefined in this output style. [DOI] [PubMed] [Google Scholar]
- Finkelman P. The color of law book review. Northwestern University Law Review. 1992;87:937–991. [Google Scholar]
- Fischer N.M., Duffy E.Y., Michos E.D. Protecting our youth: Support policy to combat health disparities fueled by targeted food advertising. Journal of American Heart Association. 2021;10(1) doi: 10.1161/JAHA.120.018900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G., Bauchner H., Feinstein A.R., Nguyen U.-S. The impact of ethnicity, family income, and parental education on children's health and use of health services. American Journal of Public Health. 1999;89(7):1066–1071. doi: 10.2105/ajph.89.7.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forde A.T., Crookes D.M., Suglia S.F., Demmer R.T. The weathering hypothesis as an explanation for racial disparities in health: A systematic review. Annals of Epidemiology. 2019;33:1–18. doi: 10.1016/j.annepidem.2019.02.011. e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin D.J., Dinwiddie G.Y., Chan K.S., McCleary R. Residential segregation and disparities in health care services utilization. Medical Care Research and Review. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghafoor A., Jemal A., Cokkinides V., Cardinez C., Murray T., Samuels A., Thun M.J. Cancer statistics for african americans. CA: A Cancer Journal for Clinicians. 2002;52(6):326–341. doi: 10.3322/canjclin.52.6.326. [DOI] [PubMed] [Google Scholar]
- Glymour M.M., Avendano M., Kawachi I. Socioeconomic status and health. Social epidemiology. 2014;2:17–63. [Google Scholar]
- Glymour M.M., Manly J.J. Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review. 2008;18(3):223–254. doi: 10.1007/s11065-008-9064-z. [DOI] [PubMed] [Google Scholar]
- Gouin J.-P. Chronic stress, immune dysregulation, and health. American Journal of Lifestyle Medicine. 2011;5(6):476–485. [Google Scholar]
- Greene W. The behaviour of the maximum likelihood estimator of limited dependent variable models in the presence of fixed effects. The Econometrics Journal. 2004;7(1):98–119. [Google Scholar]
- Gupta R.P.-S., de Wit M.L., McKeown D. The impact of poverty on the current and future health status of children. Paediatrics and Child Health. 2007;12(8):667–672. doi: 10.1093/pch/12.8.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern D. Minorities and mental health. Social Science & Medicine. 1993;36(5):597–607. doi: 10.1016/0277-9536(93)90056-a. [DOI] [PubMed] [Google Scholar]
- Hamad R., Öztürk B., Foverskov E., Pedersen L., Sørensen H.T., Bøtker H.E., White J.S. Association of neighborhood disadvantage with cardiovascular risk factors and events among refugees in Denmark. JAMA Network Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.14196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamad R., Rehkopf D.H. Poverty and child development: A longitudinal study of the impact of the earned income tax credit. American Journal of Epidemiology. 2016;183(9):775–784. doi: 10.1093/aje/kwv317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris J.L., Frazier W., III, Kumanyika S., Ramirez A.G. Increasing disparities in unhealthy food advertising targeted to Hispanic and Black youth. 2019. https://media.ruddcenter.uconn.edu/PDFs/TargetedMarketingReport2019.pdf Rudd Reports, Issue.
- Hellevik O. Linear versus logistic regression when the dependent variable is a dichotomy. Quality and Quantity. 2009;43(1):59–74. [Google Scholar]
- Hofferth S., Davis-Kean P.E., Davis J., Finkelstein J. Survey Research Center, Institute for Social Research, University of Michigan; Ann Arbor: 1997. The child development supplement to the panel study of income dynamics: 1997 user guide. [Google Scholar]
- Huesmann L.R., Guerra N.G. Children's normative beliefs about aggression and aggressive behavior. Journal of Personality and Social Psychology. 1997;72(2):408. doi: 10.1037//0022-3514.72.2.408. [DOI] [PubMed] [Google Scholar]
- Jackson J.S., Knight K.M., Rafferty J.A. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesdale B.M., Morello-Frosch R., Cushing L. The racial/ethnic distribution of heat risk–related land cover in relation to residential segregation. Environmental Health Perspectives. 2013;121(7):811–817. doi: 10.1289/ehp.1205919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kawachi I. Social capital and community effects on population and individual health. Annals of the New York Academy of Sciences. 1999;896(1):120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kershaw K.N., Albrecht S.S. Racial/ethnic residential segregation and cardiovascular disease risk. Current Cardiovascular Risk Reports. 2015;9(3):1–12. doi: 10.1007/s12170-015-0436-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw K.N., Osypuk T.L., Do D.P., De Chavez P.J., Diez Roux A.V. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: The multi-ethnic study of atherosclerosis. Circulation. 2015;131(2):141–148. doi: 10.1161/CIRCULATIONAHA.114.011345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw K.N., Pender A.E. Racial/ethnic residential segregation, obesity, and diabetes mellitus. Current Diabetes Reports. 2016;16(11):1–11. doi: 10.1007/s11892-016-0800-0. [DOI] [PubMed] [Google Scholar]
- Kershaw K.N., Robinson W.R., Gordon-Larsen P., Hicken M.T., Goff D.C., Carnethon M.R., Kiefe C.I., Sidney S., Roux A.V.D. Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among black adults: The CARDIA study. JAMA Internal Medicine. 2017;177(7):996–1002. doi: 10.1001/jamainternmed.2017.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner T.R., Villanti A.C., Cantrell J., Anesetti-Rothermel A., Ganz O., Conway K.P., Vallone D.M., Abrams D.B. Tobacco retail outlet advertising practices and proximity to schools, parks and public housing affect Synar underage sales violations in Washington, DC. Tobacco Control. 2015;24(e1):e52–e58. doi: 10.1136/tobaccocontrol-2013-051239. [DOI] [PubMed] [Google Scholar]
- Klinenberg E. University of Chicago Press; 2015. Heat wave: A social autopsy of disaster in Chicago. [DOI] [PubMed] [Google Scholar]
- Kramer M.R., Hogue C.R. Is segregation bad for your health? Epidemiologic Reviews. 2009;31(1):178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krauss R.M., Winston M., Fletcher B.J., Grundy S.M. Obesity: Impact on cardiovascular disease. Circulation. 1998;98(14):1472–1476. [PubMed] [Google Scholar]
- Krieger N., Van Wye G., Huynh M., Waterman P.D., Maduro G., Li W., Gwynn R.C., Barbot O., Bassett M.T. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. American Journal of Public Health. 2020;110(7):1046–1053. doi: 10.2105/AJPH.2020.305656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski R.J.… . US Department of Health and Human Services, Centers for Disease Control and; 2000. CDC growth charts: United States. [Google Scholar]
- Landrine H., Corral I., Lee J.G., Efird J.T., Hall M.B., Bess J.J. Residential segregation and racial cancer disparities: A systematic review. Journal of Racial and Ethnic Health Disparities. 2017;4(6):1195–1205. doi: 10.1007/s40615-016-0326-9. [DOI] [PubMed] [Google Scholar]
- Lichter D.T., Parisi D., Taquino M.C. The geography of exclusion: Race, segregation, and concentrated poverty. Social Problems. 2012;59(3):364–388. [Google Scholar]
- Loh H., Coes C., Buthe B. Brookings Institution; Washington, D.C.: 2020. Separate and unequal: Persistent residential segregation is sustaining racial and economic injustice in the U.S. [Google Scholar]
- Lu M.C., Kotelchuck M., Hogan V., Jones L., Wright K., Halfon N. Closing the black-white gap in birth outcomes: A life-course approach. Ethnicity & Disease. 2010;20(1 0 2):S2. [PMC free article] [PubMed] [Google Scholar]
- Massey D.S. Segregation and stratification: A biosocial perspective. Du Bois Review: Social Science Research on Race. 2004;1(1):7–25. doi: 10.1017/S1742058X04040032. [DOI] [Google Scholar]
- May A.L., Freedman D., Sherry B., Blanck H.M., Control C.f.D., Prevention Obesity—United States, 1999–2010. MMWR Surveill Summary. 2013;62(Suppl 3):120–128. [PubMed] [Google Scholar]
- Mensah G.A., Mokdad A.H., Ford E.S., Greenlund K.J., Croft J.B. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Mersky J.P., Janczewski C.E., Topitzes J. Rethinking the measurement of adversity: Moving toward second-generation research on adverse childhood experiences. Child Maltreatment. 2017;22(1):58–68. doi: 10.1177/1077559516679513. [DOI] [PubMed] [Google Scholar]
- Montgomery L.E., Kiely J.L., Pappas G. The effects of poverty, race, and family structure on US children's health: Data from the NHIS, 1978 through 1980 and 1989 through 1991. American Journal of Public Health. 1996;86(10):1401–1405. doi: 10.2105/ajph.86.10.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natividad I. How American racism is rooted in residential segregation. 2021. https://news.berkeley.edu/2021/06/21/how-american-racism-is-rooted-in-residential-segregation/
- Pamuk E., Makuc D., Heck K., Reuben C., Lochner K. U.S. Department of Health and Human Services; Hyattsville, Maryland: 1998. (Health, United States. Socioeconomic status and health chartbook). [Google Scholar]
- Peterson J.L., Zill N. Marital disruption, parent-child relationships, and behavior problems in children. Journal of Marriage and Family. 1986:295–307. [Google Scholar]
- Pohl D.J., Seblova D., Avila J.F., Dorsman K.A., Kulick E.R., Casey J.A., Manly J. Relationship between residential segregation, later-life cognition, and incident dementia across race/ethnicity. International Journal of Environmental Research and Public Health. 2021;18(21) doi: 10.3390/ijerph182111233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polednak A.P. Trends in US urban black infant mortality, by degree of residential segregation. American Journal of Public Health. 1996;86(5):723–726. doi: 10.2105/ajph.86.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack B.A., Bost J.E., Land S.R., Fine M.J. Volume of tobacco advertising in african American markets: Systematic review and meta-analysis. Public Health Reports. 2007;122(5):607–615. doi: 10.1177/003335490712200508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quillian L. Segregation and poverty concentration: The role of three segregations. American Sociological Review. 2012;77(3):354–379. doi: 10.1177/0003122412447793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salow A.D., Pool L.R., Grobman W.A., Kershaw K.N. Associations of neighborhood-level racial residential segregation with adverse pregnancy outcomes. American Journal of Obstetrics and Gynecology. 2018;218(3):351. e1–351. e7. doi: 10.1016/j.ajog.2018.01.022. [DOI] [PubMed] [Google Scholar]
- Schwartz G.L., Wang G., Kershaw K.N., McGowan C., Kim M.H., Hamad R. The long shadow of residential racial segregation: Associations between childhood residential segregation trajectories and young adult health among Black US Americans. Health & place. 2022;77 doi: 10.1016/j.healthplace.2022.102904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott J., Danos D., Collins R., Simonsen N., Leonardi C., Scribner R., Herd D. Structural racism in the built environment: Segregation and the overconcentration of alcohol outlets. Health & Place. 2020;64 doi: 10.1016/j.healthplace.2020.102385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellström E., Bremberg S. The significance of neighbourhood context to child and adolescent health and well-being: A systematic review of multilevel studies. Scandinavian Journal of Public Health. 2006;34(5):544–554. doi: 10.1080/14034940600551251. [DOI] [PubMed] [Google Scholar]
- Singh G.K., Ghandour R.M. Impact of neighborhood social conditions and household socioeconomic status on behavioral problems among US children. Maternal and Child Health Journal. 2012;16(1):158–169. doi: 10.1007/s10995-012-1005-z. [DOI] [PubMed] [Google Scholar]
- Smith J.P. The impact of childhood health on adult labor market outcomes. The Review of Economics and Statistics. 2009;91(3):478–489. doi: 10.1162/rest.91.3.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L.H., Schwartz G.L. Mediating to opportunity: The challenges of translating mediation estimands into policy recommendations. Epidemiology. 2021;32(3):347–350. doi: 10.1097/EDE.0000000000001335. [DOI] [PubMed] [Google Scholar]
- Starfield B. Child health care and social factors: Poverty, class, race. Bulletin of the New York Academy of Medicine. 1989;65(3):299. [PMC free article] [PubMed] [Google Scholar]
- Timoneda J.C. Estimating group fixed effects in panel data with a binary dependent variable: How the LPM outperforms logistic regression in rare events data. Social Science Research. 2021;93 doi: 10.1016/j.ssresearch.2020.102486. [DOI] [PubMed] [Google Scholar]
- Vaughan Sarrazin M.S., Campbell M.E., Richardson K.K., Rosenthal G.E. Racial segregation and disparities in health care delivery: Conceptual model and empirical assessment. Health Services Research. 2009;44(4):1424–1444. doi: 10.1111/j.1475-6773.2009.00977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Schwartz G.L., Kim M.H., White J.S., Glymour M.M., Reardon S.…Hamad R. School racial segregation and the health of Black children. Pediatrics. 2022;149(5) doi: 10.1542/peds.2021-055952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Borrell L.N. Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health & Place. 2011;17(2):438–448. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Haas J.S., Williams D.R. Elucidating the role of place in health care disparities: The example of racial/ethnic residential segregation. Health Services Research. 2012;47(3pt2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2016;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo B., Kravitz-Wirtz N., Sass V., Crowder K., Teixeira S., Takeuchi D.T. Residential segregation and racial/ethnic disparities in ambient air pollution. Race And Social Problems. 2019;11(1):60–67. doi: 10.1007/s12552-018-9254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo C. Stress coping and mental health among adolescents: Applying a multi-dimensional stress coping model. Children and Youth Services Review. 2019;99:43–53. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that were used for this analysis are confidential due to the inclusion of geocodes. Interested users can apply for access to these data at https://psidonline.isr.umich.edu/.