Abstract
Purpose
To demonstrate a case where Alternaria fungus grew on top of cyanoacrylate glue used to seal a perforated corneal ulcer.
Observations
We document the clinical course of a rare case of Alternaria keratitis over the course of 6 months. Despite the purported antifungal properties of cyanoacrylate glue demonstrated in vitro, this case provides in vivo evidence that this substance can serve as a scaffold on which pathogenic fungi may grow.
Conclusion
This report demonstrates the importance of close follow up of patients with corneal glue patches in place. Ophthalmologists should continue to inspect the cornea and glue for possible development of secondary infection, particularly with concomitant contact lens and/or steroid use.
Keywords: Cyanoacrylate glue, Alternaria, Fungus, Ulcer
1. Introduction
Cyanoacrylate glue is commonly used to treat corneal perforations, and may have additional utility in cases of perforated infectious keratitis due to its purported antimicrobial and antifungal activity.1, 2, 3, 4 Alternaria is a rare cause of infectious keratitis.5 Herein we present a case of an Alternaria fungal infection that developed on top of cyanoacrylate glue used to seal a perforated corneal ulcer.
2. Case report
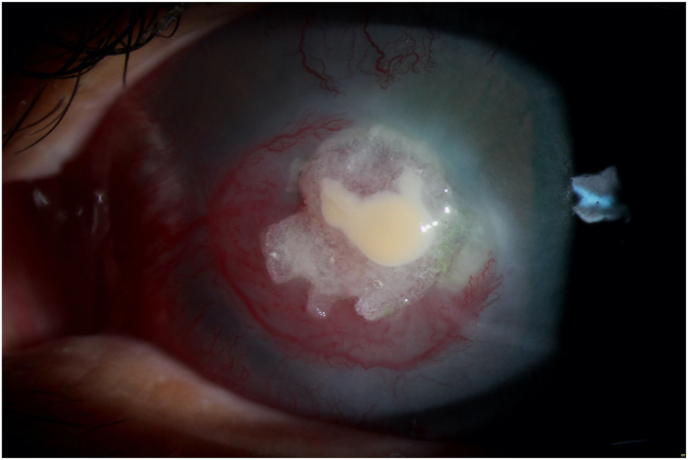
A 44-year-old otherwise healthy male with a refractory corneal ulcer was referred to our tertiary care academic center for continued management. His past ocular history was notable for an unclear degree of deprivation amblyopia in the left eye due to a “corneal infection” during childhood. The patient performed intermittent farm work but does not recall any specific incidence of vegetative trauma to his eye. The current episode of infectious keratitis was culture negative and had been ongoing for approximately 7 months. The initial history of the ulcer was vague. It was complicated by perforation 6 months prior to arrival, prompting 2 applications of cyanoacrylate glue and bandage contact lens which sealed the leak. Treatment had also included 6 months of 0.5% moxifloxacin QID, 1% prednisolone acetate QID, atropine, 400 mg oral acyclovir QID, 3 months of 100 mg oral doxycycline BID, 2 weeks of polytrim QID, intermittent bandage contact lens use, and a 9 week course of topical cenegermin. His visual acuity without correction was 20/20–1 OD and hand motion OS. Slit lamp exam showed a central 4.0 × 4.8 mm stromal infiltrate with overlying glue in the left eye, as well as a nasal pseudopterygium with marked neovascularization. An amorphous, creamy white plaque was noted on the anterior surface of the glue patch (Fig. 1), which was cultured and demonstrated a dry, rough texture during scraping. Empiric treatment with amphotericin was initiated for presumed fungal keratitis, and his prednisolone was tapered over the course of 12 days and then stopped. Ultrasonography demonstrated moderate vitritis, prompting vitreous aspiration and injection of voriconazole, vancomycin, and ceftazidime for presumed endophthalmitis. Cultures of the glue plaque subsequently grew Alternaria, while the vitreous sample demonstrated no growth. Once this filamentous fungus had been identified and sensitivities showed it was sensitive to both voriconazole and amphotericin, therapy was changed from amphotericin to voriconazole as the amphotericin was no long available at our pharmacy.
Fig. 1.
Central corneal ulcer with overlying glue patch and extensive corneal neovascularization with nasal pseudopterygium. Overlying the glue patch is a lobular, sharply demarcated, creamy-white plaque, which grew Alternaria on subsequent cultures.
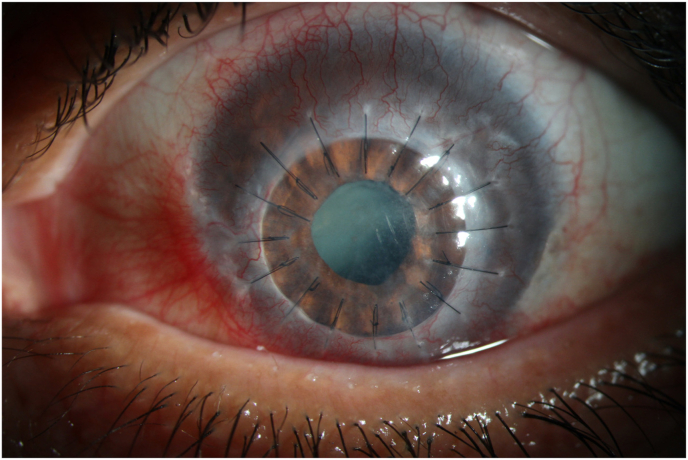
The superficial plaque on the surface of the glue gradually reduced in size, but one month after initiation of antifungal therapy the glue dislodged. The underlying perforation was Seidel positive and not sealable with repeat glue, prompting a 6.5 mm tectonic penetrating keratoplasty (Fig. 2). Notably, the excised corneal button demonstrated no fungal elements on Grocott methenamine silver stain and no bacteria on Brown-Hopps staining, and the eye has remained infection free for the ensuing 16 months. The patient underwent uncomplicated cataract surgery 4 months after the penetrating keratoplasty. His best vision following the cataract removal was pinhole 20/250. The tectonic graft has now opacified, and large-diameter optical penetrating keratoplasty is planned in the near future.
Fig. 2.
The same eye at postoperative month 1 following therapeutic penetrating keratoplasty. The eye has remained free of infection for 17 months following surgery.
3. Discussion
Cyanoacrylate glues are effective tools for ophthalmologists. This inexpensive, easily accessible, and fast drying glue can be used to address multiple ophthalmic problems but is most commonly employed to non-invasively seal corneal perforations.1 While it's use is primarily to prevent continued aqueous leakage and provide tectonic stability to the anterior segment, in vitro evidence suggests it may also have anti-inflammatory and antimicrobial properties. Specifically, it has been shown to prevent stromal melting by inhibiting polymorphonuclear neutrophils which have collagenolytic and proteolytic activity.1 The bacteriostatic, bactericidal, and anti-fungal properties of cyanoacrylate glue are well documented. 1, 2, 3, 4 In vitro studies have shown that cyanoacrylate glue inhibits growth of gram positive microorganisms including Staphylococcus aureus and coagulase-negative Staphylococcus. The response of gram-negative bacteria is mixed. Dogan et al. demonstrated in vitro inhibition of growth of 18 out of 21 tested fungi which included numerous Candida and Aspergillus species and other fungi, though Alternaria species were not evaluated and they used N-butyl-2-cyanoacrylate rather than 2-octyl cyanoacrylate (the compound used in the case described above).2
Despite these potential direct antimicrobial effects of cyanoacrylate, infections occurring underneath corneal glue patches have been reported.6,7 Weiss et al. describe a relationship between greater time of glue on the cornea and the incidence of complications, especially microbial keratitis.6 They postulate that bandage contact lenses, such as those worn by the patient in our case, were the source of the infection. However, we are not aware of any reported cases of pathogenic microbes growing directly on top of glue, as we report in this case. This represented a therapeutic challenge because the glue could not be safely removed, thus the secondary infection had to be managed medically. This case also provides in vivo evidence that directly contradicts the purported antifungal effects of cyanoacrylate, at least for this particular fungal pathogen. Indeed, rather than damaging these Alternaria filaments, the glue served as a scaffold on which they proliferated, presumably serving as the nidus of infection for the recrudescence of infectious keratitis in this case. Almost certainly, the combined use of a bandage contact lens over the glue and prolonged topical steroid provided a favorable microenvironment for this fungal pathogen to develop on top of the glue patch in this case.
Alternaria sp. is a filamentous dematiaceous fungus that is found in indoor air, soil, plants, and food and is an uncommon cause of fungal keratitis. It can be a normal flora on human and animal skin and conjunctiva.8 Ocular Alternaria infections are seen in people who have had exposure to soil and garbage or trauma. 8,9 In 2014 Hsiao et al. published data that combined 7 patients who had culture proven Alternaria keratitis in a Taiwanese hospital over a 10 year period with 25 cases identified from the literature.5 These data showed that 44% (14 of 32) of the infections followed trauma to the eye, and 31% (10) were associated with preexisting corneal disease or previous ocular surgery. Five (16%) patients wore soft contact lenses and 23 (72%) patients had successful medical management.5 Natamycin and amphotericin B were the most used medications and 9 patients required penetrating keratoplasty. In vitro, Itraconazole, Voriconazole, and Posaconazole showed good activity against Alternaria. Amphotericin B has shown variable activity and fluconazole showed no activity.8 Recently, Voriconazole has been used to treat Alternaria more frequently because it has high bioavailability and therapeutic levels can be reached after topical and oral doses.5
In summary, despite the antifungal properties of cyanoacrylate glue, we have demonstrated a rare case of Alternaria fungus growing directly on top of a cyanoacrylate glue patch. While following patients with cyanoacrylate glue on their corneas, providers should continue to inspect the surface of the glue for plaque-like abnormalities and culture the glue and surrounding cornea if unexpected changes are noted. Nonetheless, cyanoacrylate remains a viable option for nonsurgical management of some corneal perforations.
Patient consent
The patient consented to publication of the case orally.
Acknowledgments
This work is supported by the National Institutes of Health (NIH K12EY027720 and core grant P30EY10572) and unrestricted departmental funding provided by Research to Prevent Blindness. These funding organizations had no role in the design or conduct of this research.
The following authors have no financial disclosures: EN, TR.
All authors attest that they meet the current ICMJE criteria for Authorship.
No additional acknowledgements.
Contributor Information
Erin M. NaPier, Email: napierin@gmail.com.
Travis K. Redd, Email: redd@ohsu.edu.
References
- 1.Vote B.J., Elder M.J. Cyanoacrylate glue for corneal perforations: a description of a surgical technique and a review of the literature. Clin Exp Ophthalmol. 2000;28(6):437–442. doi: 10.1046/j.1442-9071.2000.00351.x. [DOI] [PubMed] [Google Scholar]
- 2.Dogan C., Aygun G., Bahar-Tokman H., et al. In vitro antifungal effect of acrylic corneal glue (N-Butyl-2-Cyanoacrylate) Cornea. 2019;38(12):1563–1567. doi: 10.1097/ICO.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 3.de Almeida Manzano R.P., Naufal S.C., Hida R.Y., Guarnieri L.O.B., Nishiwaki-Dantas M.C. Antibacterial analysis in vitro of ethyl-cyanoacrylate against ocular pathogens. Cornea. 2006;25(3):350–351. doi: 10.1097/01.ico.0000183490.16131.e3. [DOI] [PubMed] [Google Scholar]
- 4.Ciapetti G., Stea S., Cenni E., et al. Cytotoxicity testing of cyanoacrylates using direct contact assay on cell cultures. Biomaterials. 1994;15(1):63–67. doi: 10.1016/0142-9612(94)90199-6. [DOI] [PubMed] [Google Scholar]
- 5.Hsiao C.H., Yeh L.K., Chen H.C., et al. Clinical characteristics of alternaria keratitis. J Ophthalmol. 2014;2014 doi: 10.1155/2014/536985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiss J.L., Williams P., Lindstrom R.L., Doughman D.J. The use of tissue adhesive in corneal perforations. Ophthalmology. 1983;90(6):610–615. doi: 10.1016/s0161-6420(83)34508-5. [DOI] [PubMed] [Google Scholar]
- 7.Leahey A.B., Gottsch J.D., Stark W.J. Clinical experience with N-butyl cyanoacrylate (Nexacryl) tissue adhesive. Ophthalmology. 1993;100(2):173–180. doi: 10.1016/s0161-6420(93)31674-x. [DOI] [PubMed] [Google Scholar]
- 8.Pastor F.J., Guarro J. Alternaria infections: laboratory diagnosis and relevant clinical features. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2008;14(8):734–746. doi: 10.1111/j.1469-0691.2008.02024.x. [DOI] [PubMed] [Google Scholar]
- 9.Monno R., Alessio G., Guerriero S., et al. Alternaria is an infrequent cause of keratitis: a case report and review of the literature. Eye Contact Lens. 2015;41(4):e14–e17. doi: 10.1097/ICL.0000000000000012. [DOI] [PubMed] [Google Scholar]