Abstract
Background
Burnout and other psychological comorbidities were evident prior to the COVID-19 pandemic for critical care healthcare professionals (HCPs) who have been at the forefront of the health response. Current research suggests an escalation or worsening of these impacts as a result of the COVID-19 pandemic.
Objectives
The objective of this study was to undertake an in-depth exploration of the impact of the evolving COVID-19 pandemic on the wellbeing of HCPs working in critical care.
Methods
This was a qualitative study using online focus groups (n = 5) with critical care HCPs (n = 31, 7 medical doctors and 24 nurses) in 2021: one with United Kingdom–based participants (n = 11) and four with Australia-based participants (n = 20). Thematic analysis of qualitative data from focus groups was performed using Gibbs framework.
Findings
Five themes were synthesised: transformation of anxiety and fear throughout the pandemic, the burden of responsibility, moral distress, COVID-19 intruding into all aspects of life, and strategies and factors that sustained wellbeing during the pandemic. Moral distress was a dominant feature, and intrusiveness of the pandemic into all aspects of life was a novel finding.
Conclusions
The COVID-19 pandemic has adversely impacted critical care HCPs and their work experience and wellbeing. The intrusiveness of the pandemic into all aspects of life was a novel finding. Moral distress was a predominate feature of their experience. Leaders of healthcare organisations should ensure that interventions to improve and maintain the wellbeing of HCPs are implemented.
Keywords: COVID-19 pandemic, Critical care, Focus groups, Healthcare professionals, Stress, Psychological, Wellbeing, Healthcare workers, Thematic analysis
1. Introduction
During any public health crisis, critical care healthcare professionals (HCPs) are at the forefront of the response. HCPs have experienced higher rates of COVID-19 infection and mortality than other occupations.1 Furthermore, HCPs in the US and the United Kingdom (UK) were 10 times more likely to be infected with COVID-19 than the community2 and HCPs based in Australia were twice as likely to be infected.3 Unfortunately, HCPs in the UK have been shown to be seven times more likely to experience severe COVID-19 than other occupational groups.4 Although infection rate and severity were lower in many countries, the threat of illness and mortality and fear of infecting loved ones negatively impacted HCPs' mental health across countries.[5], [6], [7] Several systematic reviews have summarised the psychological impact on HCPs working during the COVID-19 pandemic such as increased rates of anxiety, depression, psychological distress, post-traumatic stress symptoms, stress,7 , 8 and burnout.9 Burnout and other psychological comorbidities were evident prior to the COVID-19 pandemic, adding to concerns for those who work in critical care.[10], [11], [12] Current research suggests an escalation or worsening of these impacts as a result of the COVID-19 pandemic.7 , 8 HCPs identified as ‘frontline’ and those working in critical care are considered to be at the highest risk.7
Several qualitative studies have explored the experience of the COVID-19 pandemic for HCPs.[13], [14], [15], [16] The studies included participants from Australia and the UK and used semistructured individual interviews. The focus of these studies was on the experience of HCPs working in critical care14 , 15 with limited emphasis on the impact on the HCPs' life.13 Collective exploration of the impact of the pandemic on HCPs' wellbeing had not been conducted until the time we proposed our study. Therefore, the aim of this study was to undertake an in-depth exploration of the impact of the evolving COVID-19 pandemic on the wellbeing of HCPs working in critical care from the HCPs’ perspectives.
2. Methods
2.1. Design
This was a qualitative study using semistructured focus groups (FGs).17 The underpinning methodological paradigm was pragmatic-constructivist. The Standards for Reporting Qualitative Research18 were used.
2.2. Settings, sampling, and recruitment
In 2021, HCPs working in critical and acute care specialties in Australia and the UK were invited to participate using purposive targeted sampling. There were two separate recruitment processes: UK participants were recruited from a Twitter post, and participants based in Australia were recruited by word of mouth and snowball recruitment. Expressions of interest were received only from nurses and medical doctors. An information and consent form was emailed with a choice of times for the FG to potential participants.
2.3. Data collection
The FG schedule (Supplementary Material 1) was based on previous work by the authors, a large international survey of HCPs’ psychological wellbeing during the COVID-19 pandemic,5 and other research.7 , 19 , 20 FGs were conducted online via Zoom21 in 2021 in April (n = 1), August (n = 1), September (n = 2), and October (n = 1). Participants joined the FG individually in a private location from their homes. An inclusive and active approach to facilitation was used to encourage all participants to contribute. The participants were observed by the facilitator, and memo notes were made to complement the audio-visual recording data. In addition, in-depth contextual notes were made about the pandemic situation in each of the countries and states (for Australia) at the time (Supplementary Material 2). FGs were audio-visual recorded and uploaded to the Australian universities cloud server Cloudstor®. A secure link to the relevant files was provided for the transcription firm, who transcribed the recordings verbatim.
2.4. Number and relevant characteristics of FGs and participants
There were 31 participants in the five FGs (range: 4 to 11 per FG). Most participants were nurses (n = 24), and the other participants were doctors (consultants and trainees). Participants of four FGs were based in Australia (n = 20), and the other FG comprised participants based in the UK (n = 11) (Table 1 ). No participants withdrew from the FGs. The mean duration of recordings was 61 (range: 54 to 80) minutes.
Table 1.
Focus group and participant characteristics.
| Focus group number | Month, location of participants (n = participant numbers) | Role and specialty of participants | Approximate duration in specialty, years (range) |
|---|---|---|---|
| 1 | April, UK; England and Scotland (n = 11) | ICU nurses × 2 | 5–35 |
| ICU/ED nurse × 1 | |||
| Nurse consultant × 1 | |||
| Consultant/medical fellow ICU × 2 | |||
| Consultant/medical fellow paediatric ICU × 2 | |||
| Consultant/medical fellow ED × 2 | |||
| Consultant/medical fellow paediatric ED × 1 | |||
| 2 | August, Australia; NSW and Queensland (n = 6) | ICU/ED casual nurse × 1 | 4–30 |
| ICU nurse × 1 | |||
| CNC ICU/resuscitation × 3 | |||
| Acute care CNE × 1 | |||
| 3 | September, Australia; NSW (n = 4) | ICU nurses × 2 | 15–30 |
| CNC ED × 1 | |||
| Nurse practitioner ICU × 1 | |||
| 4 | October, Australia; NSW (n = 6) | ICU nurses × 3 | 4–30 |
| ICU nurse educator × 1 | |||
| Nurse unit manager × 1 | |||
| ED nurse × 1 | |||
| 5 | October, Australia; NSW n = 4) | ICU nurses × 4 | 1.5 - >30 |
Notes: CNC, clinical nurse consultant; CNE, clinical nurse educator; ED, emergency department; ICU, intensive care unit.
2.5. Data analysis
All potentially identifiable information was removed from the transcribed interview documents. The FG facilitators read transcripts while listening to the FG recordings, and the third researcher (W.P.) read through the transcripts multiple times before performing thematic analysis. The researchers (R.E., W.P., and L.C.) independently performed a detailed exploration of the data for patterns and commonalities as well as outliers and differences. This inductive-deductive iterative analysis was data driven and guided by Gibbs (2007) framework and informed by Braun and Clark (2013). Thus, the researchers immersed and familiarised themselves with the data, coded and performed confirmatory coding, consolidated, and interpreted the results. Codes were categorised before further analysis to synthesise the themes. The themes were then reviewed by the fourth researcher (N.H.), and any discrepancies were resolved by consensus. Slight differences in emphasis existed between the FG performed in the UK and the FGs conducted in Australia, but no new themes were evident for FG 5.
2.6. Ethical considerations
Ethical approval was provided by the Children's Health Queensland, Hospital and Health Service Research Ethics Committee [no. HREC/20/QCHQ/6434]. Informed written consent was obtained before the FGs. Participants were again informed about the aims, procedures, and purpose of the research and that the FG was to be recorded and the researchers had a special interest in HCP wellbeing. Recordings were transcribed by a firm with electronic storage facilities and workers based in the jurisdiction of Australia.
2.7. Reflexivity and other techniques to enhance trustworthiness
All researchers had extensive critical care clinical, education, and research experience. Three researchers were critical care nurses (R.E., N.H., and W.P.), and the other was a social worker with staff wellbeing expertise (L.C.). The UK FG was conducted by L.C. The four FGs in Australia were conducted by a critical care nurse (R.E.) who worked in intensive care during the pandemic. The facilitator of the UK FG knew some participants professionally. The facilitator for the Australia-based FG knew all the participants professionally and worked clinically with many (though not in a supervisory role). To mitigate the potential for implicit bias resulting from the researchers' work and research in critical care, the researchers continuously self-reflected and challenged each other's assumptions.
Thick contextual description was documented for the current pandemic situation in the country in which the respondents practiced (Supplementary Material 2). Three researchers (R.E., L.C., and W.P.) meticulously reread the transcripts independently before sharing their synthesised themes with each other. The fourth researcher checked the themes, and consensus was reached after several iterations. Member checking was performed to enhance credibility. Two participants from two different FGs reviewed the themes and confirmed their agreement with the way in which the data were represented.
3. Findings
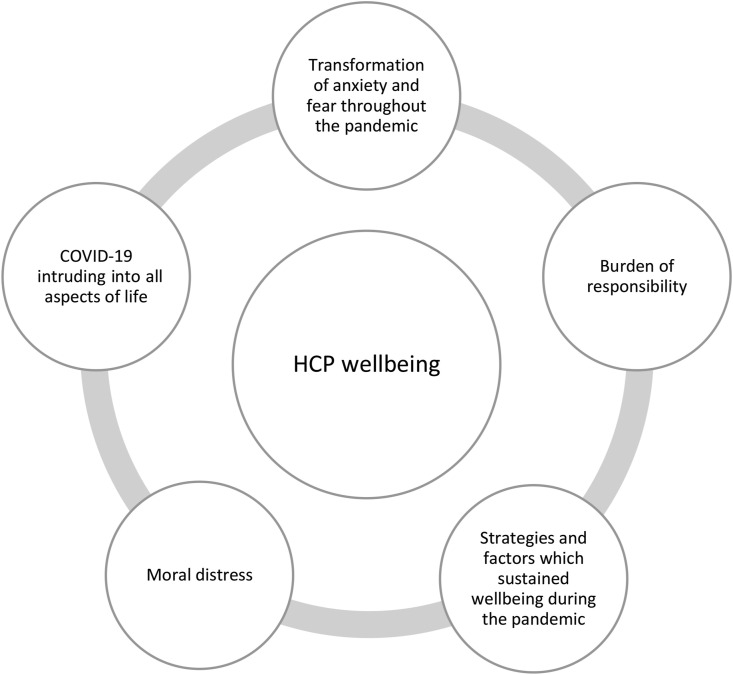
Five themes were synthesised, and all five themes had implications for HCPs' wellbeing (Fig. 1 ).
Fig. 1.
Diagrammatic representation of the five themes. HCP, healthcare professional.
3.1. Transformation of anxiety and fear throughout the pandemic
Fears changed as the pandemic evolved. Changing fears and concerns meant adaptation was difficult. Initially participants were terrified of being infected with COVID-19. As this intensive care medical consultant highlighted,
“ …. I was convinced I was going to die even though the rational part of me knew, well, not knew but didn't think that was going to happen because I was looking after myself …. I was doing all the right things. But actually having seen so many colleagues die that on my turn of having COVID, I was convinced that that would be the end for me, even though I knew clinically that I was okay.” (FG 1)
Participants from the UK described the fear of death and illness for themselves, and their families transformed to a fear of their colleagues being infected. For example,
“I’d written like a little document to my girlfriend about what to do if I died and all this sort of slightly, in hindsight, hysterical stuff [laughing] and then I sort of transitioned from fear for my personal safety to fears of giving it to my partner, then fear of colleagues getting it” (intensive care medical trainee FG 1)
In Australia, there was anticipatory anxiety among participants. As HCPs observed international colleagues struggle, the fear of the unknown and waiting, and threat of the influx of patients with COVID-19 infections in Australia heightened fear and anxiety. This was exemplified by a clinical nurse consultant (CNC) [resuscitation],
“I think the fear initially was the great unknown, like we didn’t really know what we were dealing with. We were getting all these media images from overseas and these horrific scenes, and you didn’t know how it was going to play out.” (FG 2)
This anticipatory anxiety and fear morphed into real concerns about the ability of the healthcare system to cope as case numbers and hospital admissions increased. There were concerns about implications for staff members who were redeployed and the changing guidelines particularly for the supply of personal protection equipment (PPE). For example,
“I think that feeling of being overrun is making me feel more nervous. Can our health system cope? Have we got the right strategic plans in place? Have we got back-up? Have we got enough PPE? … … … There are a lot of variables between last year and this year that I think worry me more” (FG 3 critical care nurse)
The implementation of the COVID-19 vaccination appeared to moderate participants’ anxiety. For example, “I have no shame in saying I burst into tears I was so relieved to be vaccinated” (FG 1 intensive care medical trainee).
3.2. Burden of responsibility
Most participants described the burden of responsibility as their decisions could have catastrophic physical or psychological impacts on others. The absence of evidence and the volume of contradictory information circulating about COVID-19 increased concerns. For example, a critical care nurse described arriving at work,
“I remember the first shift I walked on, and it had my name down as second coordinator,…….and my stomach went into my throat because I knew that I also had four ITU patients to look after as well [laughing] that were responsible to me, as well as overseeing two pods of quite a lot of patients. And I remember thinking, oh my gosh, how can I do this?” (FG 1)
And this CNC (resuscitation) described the burden for her,
“I had to write resuscitation guidelines for staff, for the hospital and obviously for the wider community. And I was terrified, . I don’t mind me going in, I’m a veteran in intensive care ….I was fairly confident for myself, but having to write something and send much younger staff into situations that they could become infected, including the young doctors, was fairly trying.” (FG 2)
The evolving science and progression of the pandemic added to the responsibility of the critical care clinical leaders. Workforce demands that exceeded the number and skillset of staff resulted in staff shortages and redeployment. Many worked in roles with no experience and little support. The guilt, responsibility, and implications for their decisions were burdensome for participants. For example, a critical nurse said,
“I remember feeling worse about it on my days off because I think when I was in work, I was just sort of getting on with it, and then I’d have these days off and I’d just feel atrocious. I felt really horrible and guilty”. (FG 1)
Another nurse in the same FG stated,
“In the very first wave got pulled back to ITU as kind of an additional matron, senior nurse-type role. And one of the things that was really difficult with all of this rapid expansion was I didn't know the team. So I was being put into, or moved from one leadership role to another, to look after an enormous team that was rapidly expanding and had no clue who anybody was.” (FG 1)
3.2.1. Moral distress
Participants suggested that some policies implemented during the pandemic dehumanised patient care. They described sorrow at obeying these policies despite being cognizant of the need for them. Distressing matters included the policy excluding visitors, evidence that COVID-19 infections were predominantly affecting ethnic minority groups, and concerns that patients not infected with COVID-19 were neglected. Excluding visitors from intensive care units (ICUs), including during end-of-life care and critical illness, caused distress. For example,
“But my real problem with it is in the context of end of life where I have been in multiple situations where our facilitation of peaceful end, death with dignity is completely ruined … … and having family members ask me, “Can I take my mask off to kiss my husband goodbye?” You don’t forget those kind of things, so very, very traumatic.” (critical care nurse FG 4)
An intensive care medical consultant based in the UK also highlighted the impact of the visitor restrictions,
“Well, it just put back everything we’ve done about a good death over the last 20-odd years or so ….. if family members wanted to send a family member in to be with somebody who was dying, who are we or who are the government to overrule that? And I think it took away a large amount of our humanity and the patients' humanity but also the relatives' humanity and I think the consequence of that will be felt on a national level” (FG 1)
The absence of visitors had wider implications for patients who had additional vulnerabilities due to age, pre-existing mental health issues, or disability. For example,
“… you’re trying to confine someone to an isolation room who has several layers of anxiety, that really would only be resolved by further contact with their relatives, such as patients with learning difficulties and stuff like that ….” (CNC [emergency] FG 3)
Participants were cognisant that COVID-19 infections were more prevalent in ethnic minorities. This was a source of distress, as an intensive care medical consultant described,
“ ….it hadn’t struck me how much it was affecting the ethnic minorities of East London until we looked at the 20 beds we had and every single patient was a middle-aged Asian man. Every single one. And it was just one of those moments … ….I don’t think will ever leave me …. And yes, it was quite shocking. It’s probably one of the key moments that will always stay with me ….” (FG 1)
Hospital-wide patient care was disrupted. Participants were confronted by the knowledge that patients with other conditions either had no access to acute care or chose not to present for fear of COVID-19 infection. This was highlighted by a CNC (emergency):
“We became really concerned about patients who were leaving it too late, who had no COVID-related issues, but actually were sitting there with congestive heart failure, not coming in until it was drastically too late”. (FG 3)
3.2.2. COVID-19 intruding into all aspects of life
Participants reported that the pandemic intruded into every aspect of their personal and professional lives. They spoke of a deep fatigue using terms such as ‘exhaustion’. Participants described feeling overwhelmed physically and emotionally by the ongoing impacts of the pandemic, for example, “I was exhausted. I don't think I have ever been this exhausted before, and I've got children.” (emergency nurse FG 4)
A point of difference between the COVID-19 pandemic and other modern-day pandemics was the global health policies that closed borders and enforced lockdowns. Many of the ‘COVID-19 restrictions’ prevented participants from engaging in the activities and strategies they previously used to cope with work. This was described by a CNC (resuscitation),
“.. normally when you have a challenging situation at work, …..you have that separation, you finish, ………..you go home, you have a chat with your partner or a friend, you have a glass of wine, ….. You can go to the gym,…………, you can do whatever. You don’t have that ability to turn off, .. You come home, a lot of people are dealing with home schooling, or you can’t do your normal things for your mental health that you would normally want to do. Everything is so COVID-obsessed in this bubble, ………….I think that’s been the hardest thing, is just not having that time away.” (FG 2)
Early in the pandemic, the public demonstrated gratitude and recognition for HCPs. For example, this medical trainee highlighted, “I think that recognition, it's not a local thing, it's a national thing, and I think that has been really a powerful thing to have come out of the pandemic.” (FG 1)
However, as the COVID-19 pandemic progressed, societal attitudes changed. Participants described how confronting they found this. Some described experiencing pariahism because the public considered them potential sources of infection. This was exemplified by a critical care nurse,
“.. I did have a neighbour take her kids by the hand and move them away from me at the dog park … she just grabbed them by the hand [laugh] and almost ran away from me. It was actually quite shocking even though I know it was just protecting herself and all that. … But, yeah, it was a little bit daunting.” (FG 5)
| And a CNC (resuscitation) remarked, |
“… I walked into a [name of supermarket] …………., and people were jumping out of my way, but one woman stood there with an antiseptic bottle and I just looked at her, and I said, “You’re not going to spray me…..I will lose it if you spray me”, and she just stood there and she said, “I’m so sorry, I’m not normally this rude.” And I said, “Well please don’t spray me, because you know, we’re going through enough.”” (FG 2)
Pariahism resulted in a critical care nurse having difficulty finding accommodation and led to secondary homelessness. He reported,
““Blah, blah, blah we think you’re a good candidate, but we’re just not really comfortable with having a nurse move into the house at this time,” which resulted in me crashing on friends'couches for a couple of months, which is stressful, so definitely had some real negatives. That’s probably the biggest negative experience out of COVID for me, was that.” (FG 4)
Being treated differently by friends, family, and the community increased feelings of isolation. Participants spoke about the emotional fatigue resulting from supporting people in their networks and people who were not knowledgeable about COVID-19. For example, this critical care nurse stated,
“I think part of your mental exhaustion is .. you feel like it’s an uphill battle in some ways. I think in health care we’re used to being considered the tellers of truth, and you know, on a pedestal and we’re amazing, and now there’s this information out there that maybe the treatment is worse than the disease and all this sort of thing, and you feel attacked and it’s exhausting!” (FG 2)
Participants spoke about the challenges of juggling the demands of home life and work. Participants in Australia described the pressure associated with homeschooling their children as many schools were closed and offering only online learning, exemplified by this CNC (emergency),
“… you can burn yourself out far too quickly if you’re just coming in and how many cups of coffee, I’m not too sure, but I’ve definitely done at least in my body weight in red bull, just to keep going and support the team. ………………..…the reservoir runs dry and you just become numb. There’s nothing else left to give.” (FG 3)
The extended duration of the pandemic and an inability to predict an end point led to mental and physical fatigue, as this critical care nurse practitioner stated,
“I think particularly this time around [referring to pandemic wave 2], I feel more stressed because it’s been going on so long. There’s not a whole lot left in the reserve and I can imagine, I don’t have children, so I haven't had to do the home-schooling thing and even, just managing the dog at home, has been enough.“. (FG 3)
Participants with long careers in critical care reported the need to make significant changes to preserve their wellbeing. The demands of the COVID-19 pandemic had personally and professionally exceeded their resources. This CNC (resuscitation) described how she sought formal psychological support for the first time,
“I’d never done this before, but I actually talked to a psychologist, because I was so overwhelmed, I didn’t know what was coming, and I was feeling so anxious about it all. And so for the first time in my life, I went on a mental health plan, and I talked to this psychologist, and it was so good.” (FG 2)
3.3. Strategies and factors which sustained wellbeing during a pandemic
Participants were able to describe factors that sustained their wellbeing and so they could continue to work despite many challenges. Having leadership legitimise the need to focus on wellbeing, the solidarity and comradeship among critical care colleagues, the reduction of bureaucracy, and increased effective communication were perceived as positive outcomes. The legitimacy of being ‘allowed’ to focus on their own wellbeing was exemplified by this intensive care medical consultant,
“ …. having wellbeing and the staff put at the kind of top of the priority to enable us to look after patients is the one thing that’s kept me going throughout and being able to get …permission from our very senior leaders at the organisation that I work in, that we can be quite maverick about wellbeing and do some really outlandish things like silent discos, make sure basic needs are met with water and food, have therapy dogs come into the hospital at the height of the pandemic because actually we recognise that the staff needed it, ….“, (FG 1)
And similarly this critical care nurse remarked,
“.. the thing I looked for and appreciated in the leadership was that we felt supported, that we were on the same page, that our health was paramount. In all the training, it was, “Look after yourself first.”” (FG 5)
Participants spoke with enthusiasm about increased collaboration and teamwork and the strong sense of camaraderie with their critical care colleagues in their unique working conditions and how this contributed to their wellbeing. This intensive care medical consultant said, “Everybody just pulled together to do extraordinary things.” (FG 1) And another example,
“..for me, the sustaining factor for wellbeing has been the team dynamic from everyone that I’ve worked with, so from the clinical staff on the floor to the leadership team .., because it really does go to show that, I’m going to sound cliched, but we are all in it together, even though sometimes it doesn’t feel that way. The people that you work with are the only ones that really understand what it’s like to work in this environment, …, definitely has made a difference because at times they are your work family because your family don’t really understand what you do on a given day. That’s been a good thing for me” (critical care nurse FG 4)
The participants spoke about having autonomy and agency to lead. There was a perception that much of the ‘red tape’ had been removed. The participants spoke about the freedom and power inherent in being heard by the leadership and executive of the organisation in which they worked. This intensive care medical consultant explained,
“It was extraordinary what you could get done in five minutes where previously you couldn’t get it done in the previous five years. You know, boxing gloves came off and when certain bureaucracy was removed and it’s also interesting that the people on the front line know where the problems are and know how to sort them out, ….” (FG 1)
Another sustaining feature was innovative ways of communicating directly with their team and contributing ideas through various online platforms. For example,
“ …...our Facebook group has been really, really good …, we had a Zoom meeting with our staff specialist [intensive care medical consultant] that was allocated to us for the COVID period. So, he would give us information on a Monday night from the ICU bosses, what had been discussed in the plans that were being put into place. So, that was really good”. (critical nurse FG 3)
And this innovation instigated by a intensive care medical consultant,
“ …. I started sending a WhatsApp video to 148 members of our department every Monday and Friday. …. . I think that completely revolutionized the way that our staff digest information a bit ….. So we could get information out very fast from a face that you knew and vaguely trusted, hopefully, that wasn’t from the execs or kind of top-down thing….” (FG 1)
Participants remarked that wellbeing for HCPs must be maintained as a permanent feature of health care workforce planning beyond the COVID-19 pandemic, as exemplified by this critical care nurse,
“psychological support …. it’s important now during COVID, but it was just as important before COVID hit us, but it wasn’t discussed. It would be in an incidental case of something quite traumatic in a one-off situation, but it wasn’t there on a regular basis for staff and I think it’s brought to light that we all do need a little bit more psychological support, …” (FG 3)
4. Discussion
Five themes were synthesised from five FGs, conducted with 31 participants based in the UK and Australia: transformation of anxiety and fear throughout the pandemic, the burden of responsibility on HCPs, moral distress, COVID-19 impacting on all aspects of life, and sources of wellbeing sustainment during a pandemic. There was a slight difference between HCPs’ experience in the UK and Australia, and as a result, different impacts were evident. The main difference appeared to stem from the higher levels of community transmission in the UK than in Australia and a higher burden of disease prior to availability of the COVID-19 vaccine, resulting in higher morbidity and mortality among patients (some of whom were colleagues) in the UK.
Research involving HCPs throughout the COVID-19 pandemic has consistently reported anxiety and fear as a consistent negative experience.6 , 22 , 23 The current study findings expand this knowledge to demonstrate that anxiety among HCPs throughout the COVID-19 pandemic has been dynamic rather than static. Fear and anxiety transformed and appeared to vary according to current knowledge, the context, and disease severity. Despite a marked difference in disease burden between the two countries, with the UK experiencing a higher disease burden and higher case numbers and deaths, there was consistency across FGs. Participants based in Australia experienced anticipatory anxiety of the unknown which then transformed to a lived experience over the time in which the FGs were conducted as the hospital admissions for COVID-19 infections and case numbers increased.
The burden of responsibility was driven by a concern that participants could unintentionally cause harm to their patients, themselves, family, and colleagues. The lack of evidence-based (and often improvised) protocols and guidelines and redeployment of teams unfamiliar with critical environments in the early phases of COVID-19 added to the burden experienced by critical care HCPs that may extend beyond the pandemic.24
Moral distress was widely reported among HCPs prior to the COVID-19 pandemic, and the incidence increased significantly during the current pandemic[25], [26], [27] which is consistent with the theme synthesised in the current study. Policy changes that are implemented during a pandemic situation, such as restricted visiting, need to be reviewed and evaluated regularly, with staff involvement, to ensure that the benefits outweigh potential negative impacts for HCPs, patients, and families.28 Finding the balance between the physical protection of critical care HCPs and protecting and maintaining their mental health by ensuring conditions conducive to the provision of humanistic care during a pandemic is challenging.
A significant difference between the COVID-19 pandemic and previous modern-day pandemics was the intrusion on all aspects of HCPs’ lives. The high transmission and infection rate of this coronavirus required extensive public health policy to contain infections through extended lockdowns and concomitant reduced social interaction. The negative impact of this was clearly articulated by participants in the current study. This and the associated fatigue appear to be unique findings; other similar qualitative studies have not revealed this.
The study has several limitations. The FGs were conducted over a 7-month period with variation in the hospital activity and coronavirus variants circulating between the two countries. The UK and Australia have different healthcare systems and had different experiences of the pandemic. FGs in Australia were conducted with HCPs mostly based in New South Wales though participants worked in regional and metropolitan health services and thus had varied experiences of the pandemic. The findings can only speak of the experiences of the participants. Despite these limitations, the themes were consistently evident across FGs. Furthermore, there was no dissent during FG discussions suggesting considerable shared experiences.
Several strategies were used to enhance the trustworthiness of our findings, as outlined in the methods. However, it is possible that our ICU experience and background resulted in us overengaging with the content, and we may have missed something a novice may have identified.29 Conversely, it was a strength that the FGs were conducted by clinicians familiar with ICU, as this may have fostered open and honest discussion, as participants recognised the researchers as peers. While we kept memo and coding notes, no external audit was conducted.
Perhaps the most concerning finding from the current study was the moral distress experienced by participants. There was clear evidence in this study that the wellbeing of HCPs is under threat. This and other findings may in part be a reflection of the failure of society, health organisations, and governments to implement recommendations as a result of past pandemics. Despite decades of evidence from the SARS and Ebola pandemics and studies of the impact of critical care work on HCPs, there continues to be a failure of health organisations and governments to develop and implement resources. In fact many recommendations such as provision of ethical health care, wellbeing programs, and adequate resourcing following the SARS and Ebola outbreaks and other public health emergencies were made to prepare for future health crises, but few have been implemented.[30], [31], [32] The mental health risk for critical care HCPs resulting from daily exposure to trauma has been well reported for several decades.11 , 12 , 33 However, despite a call to action from the Critical Care Societies in 201634 and the National Academy of Medicine in 2019,35 the wellbeing of critical care HCPs has not been prioritised. Many wellbeing programs are not well accessed by HCPs as the concept of formal psychological support is not routine or normalised.36 Most wellbeing programs are discrete initiatives in which there is no long-term sustainability plan.37 Without urgent action to ameliorate the risk to HCPs' physical and mental health such as compulsory provision of multifaceted wellbeing strategies including ‘normalization of mental health support programs’,36 the next epidemic in health may be the absence of skilled critical care HCPs.
5. Conclusion
The COVID-19 pandemic has adversely impacted critical care HCPs and their work experience and wellbeing. Our findings are similar to those of other studies: critical care HCPs have endured exhausting work and exposure to potentially damaging traumatic experiences and often resulting in moral distress. The pandemic intruded into all aspects of HCPs’ lives adding to the heavy psychological burden.
Appropriately funded wellbeing programs and system changes are required to improve the work environment and wellbeing of critical care HCPs. Leaders of healthcare organisations should ensure that interventions to improve and maintain the wellbeing of HCPs are implemented.
Conflict of interest
None.
Funding
This work was supported by the Australian College of Critical Care Nurses Diane Chamberlain Research Seeding Grant 2020.
Credit authorship contribution statement
Rosalind Elliott: conceptualisation, methodology, data acquisition, funding acquisition, investigation, validation, synthesis, formal analysis, writing- original draft preparation, writing-reviewing and editing, visualisation; Wendy Pollock: synthesis, formal analysis, writing-reviewing and editing, visualisation; Liz Crowe: conceptualisation, methodology, data acquisition, funding acquisition, investigation, validation, formal analysis, writing-reviewing and editing, visualisation; Naomi Hammond: conceptualisation, methodology, funding acquisition, writing-reviewing and editing, visualisation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.aucc.2022.10.001.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.-G., Ma W., et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quigley A.L., Stone H., Nguyen P.Y., Chughtai A.A., MacIntyre C.R. Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic. Int J Nurs Stud. 2021;114 doi: 10.1016/j.ijnurstu.2020.103811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mutambudzi M., Niedzwiedz C., Macdonald E.B., Leyland A., Mair F., Anderson J., et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2021;78(5):307–314. doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammond N.E., Crowe L., Abbenbroek B., Elliott R., Tian D.H., Donaldson L.H., et al. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers' depression, anxiety, and stress levels. Aust Crit Care. 2021;34(2):146–154. doi: 10.1016/j.aucc.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abid M., Riaz M., Bano Z., Parveen T., Umar Fayyaz M., Sadia Qureshi H. Association between fear of COVID-19 and emotional distress in nurses with mediating role of socio-demographic features. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.734623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Kock J.H., Latham H.A., Leslie S.J., Grindle M., Munoz S.-A., Ellis L., et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Publ Health. 2021;21(1):104–118. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheraton M., Deo N., Dutt T., Surani S., Hall-Flavin D., Kashyap R. Psychological effects of the COVID 19 pandemic on healthcare workers globally: a systematic review. Psychiatr Res. 2020;292 doi: 10.1016/j.psychres.2020.113360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021 doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent L., Brindley P.G., Highfield J., Innes R., Greig P., Suntharalingam G. Burnout Syndrome in UK Intensive Care Unit staff: data from all three Burnout Syndrome domains and across professional groups, genders and ages. Journal of the Intensive Care Society. 2019;20(4):363–369. doi: 10.1177/1751143719860391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Mol M., Kompanje E., Benoit D., Bakker J., Nijkamp M. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0136955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chuang C.-H., Tseng P.-C., Lin C.-Y., Lin K.-H., Chen Y.-Y. Burnout in the intensive care unit professionals: a systematic review. Medicine (Baltim) 2016;95(50):e5629–e. doi: 10.1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kentish-Barnes N., Morin L., Cohen-Solal Z., Cariou A., Demoule A., Azoulay E. The lived experience of ICU clinicians during the coronavirus disease 2019 outbreak: a qualitative study. Crit Care Med. 2021;49(6):e585–e597. doi: 10.1097/ccm.0000000000004939. PubMed PMID: 00003246-202106000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Parsons Leigh J., Kemp L.G., de Grood C., Brundin-Mather R., Stelfox H.T., Ng-Kamstra J.S., et al. A qualitative study of physician perceptions and experiences of caring for critically ill patients in the context of resource strain during the first wave of the COVID-19 pandemic. BMC Health Serv Res. 2021;21(1):374. doi: 10.1186/s12913-021-06393-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montgomery C.M., Humphreys S., McCulloch C., Docherty A.B., Sturdy S., Pattison N. Critical care work during COVID-19: a qualitative study of staff experiences in the UK. BMJ Open. 2021;11(5) doi: 10.1136/bmjopen-2020-048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perraud F., Ecarnot F., Loiseau M., Laurent A., Fournier A., Lheureux F., et al. A qualitative study of reinforcement workers' perceptions and experiences of working in intensive care during the COVID-19 pandemic: a PsyCOVID-ICU substudy. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0264287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan D.L. SAGE Publications, Inc.; Los Angeles, CA: 2019. Basic and advanced focus groups. [Google Scholar]
- 18.O'Brien B.C., Harris I.B., Beckman T.J., Reed D.A., Cook D.A. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/acm.0000000000000388. PubMed PMID: 00001888-201409000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Chutiyami M., Cheong A.M.Y., Salihu D., Bello U.M., Ndwiga D., Maharaj R., et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: a meta-review of systematic reviews. Front Psychiatr. 2022;12 doi: 10.3389/fpsyt.2021.804525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.da Silva Neto R.M., Benjamim C.J.R., de Medeiros Carvalho P.M., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;104 doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zoom Video Communications Inc . Zoom Video Communications Inc; 2016. Security guide.https://d24cgw3uvb9a9h.cloudfront.net/static/81625/doc/Zoom-Security-White-Paper.pdf [cited 2022 9 June ]. Available from: [Google Scholar]
- 22.Ashley C., James S., Williams A., Calma K., McInnes S., Mursa R., et al. The psychological well-being of primary healthcare nurses during COVID-19: a qualitative study. J Adv Nurs. 2021;77(9):3820–3828. doi: 10.1111/jan.14937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.da Silva F.C.T., Barbosa C.P. The impact of the COVID-19 pandemic in an intensive care unit (ICU): psychiatric symptoms in healthcare professionals. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;110 doi: 10.1016/j.pnpbp.2021.110299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maunder R.G., Leszcz M., Savage D., Adam M.A., Peladeau N., Romano D., et al. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008;99(6):486–488. doi: 10.1007/BF03403782. Epub 2009/01/20. PubMed PMID: 19149392; PubMed Central PMCID: PMC5148615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riedel P.-L., Kreh A., Kulcar V., Lieber A., Juen B. A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. Int J Environ Res Publ Health. 2022;19(3):1666. doi: 10.3390/ijerph19031666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oakley C., Pascoe C., Balthazor D., Bennett D., Gautam N., Isaac J., et al. Assembly Line ICU: what the Long Shops taught us about managing surge capacity for COVID-19. BMJ Open Qual. 2020;9(4) doi: 10.1136/bmjoq-2020-001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bergman L., Falk A.C., Wolf A., Larsson I.M. Registered nurses' experiences of working in the intensive care unit during the COVID-19 pandemic. Nurs Crit Care. 2021;26(6):467–475. doi: 10.1111/nicc.12649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hugelius K., Harada N., Marutani M. Consequences of visiting restrictions during the COVID-19 pandemic: an integrative review. Int J Nurs Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104000. Epub 2021/07/10. doi: 10.1016/j.ijnurstu.2021.104000. PubMed PMID: 34242976; PubMed Central PMCID: PMC8196532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amin M.E.K., Nørgaard L.S., Cavaco A.M., Witry M.J., Hillman L., Cernasev A., et al. Establishing trustworthiness and authenticity in qualitative pharmacy research. Res Soc Adm Pharm. 2020;16(10):1472–1482. doi: 10.1016/j.sapharm.2020.02.005. Epub 2020/02/19. doi: 10.1016/j.sapharm.2020.02.005. PubMed PMID: 32067887. [DOI] [PubMed] [Google Scholar]
- 30.Hsieh K.-Y., Kao W.-T., Li D.-J., Lu W.-C., Tsai K.-Y., Chen W.-J., et al. Mental health in biological disasters: from SARS to COVID-19. Int J Soc Psychiatr. 2021;67(5):576–586. doi: 10.1177/0020764020944200. PubMed PMID: 32722974. [DOI] [PubMed] [Google Scholar]
- 31.Boozary A.S., Farmer P.E., Jha A.K. The Ebola outbreak, fragile health systems, and quality as a cure. JAMA. 2014;312(18):1859–1860. doi: 10.1001/jama.2014.14387. [DOI] [PubMed] [Google Scholar]
- 32.Markwell A., Mitchell R., Wright A.L., Brown A.F. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: can lessons from Ebola Virus Disease be applied to the COVID-19 pandemic? Emerg Med Australasia (EMA) 2020;32(3):520–524. doi: 10.1111/1742-6723.13514. Epub 2020/05/05. doi: 10.1111/1742-6723.13514. PubMed PMID: 32275805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bakker A., Le Blanc P.M., Schaufeli W.B. Burnout contagion among intensive care nurses. J Adv Nurs. 2005;51(3):276–287. doi: 10.1111/j.1365-2648.2005.03494.x. [DOI] [PubMed] [Google Scholar]
- 34.Moss M., Good V.S., Gozal D., Kleinpell R., Sessler C.N. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals a call for action. Am J Respir Crit Care Med. 2016;194(1):106–113. doi: 10.1164/rccm.201604-0708ST. [DOI] [PubMed] [Google Scholar]
- 35.National Academies of Sciences Engineering and Medicine . National Academies Press; Washington DC: 2019. Taking action against clinician Burnout: a systems approach to professional wellbeing; p. 334. [PubMed] [Google Scholar]
- 36.Schwartz R., Sinskey JLA U., Margolis R.D. Addressing postpandemic clinician mental health. Ann Intern Med. 2020;173(12):981–988. doi: 10.7326/m20-4199%m32822206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gray P., Senabe S., Naicker N., Kgalamono S., Yassi A., Spiegel J.M. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: a realist review. Int J Environ Res Publ Health. 2019;16(22):4396. doi: 10.3390/ijerph16224396. PubMed PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.