Abstract
Background
Multimorbidity and polypharmacy are common among individuals hospitalized for heart failure (HF). Initiating high-risk medications such as antipsychotics may increase the risk of poor clinical outcomes, especially if these medications are continued unnecessarily into skilled nursing facilities (SNFs) after hospital discharge.
Objective
Examine how often older adults hospitalized with HF were initiated on antipsychotics and characteristics associated with antipsychotic continuation into SNFs after hospital discharge.
Design
Retrospective cohort.
Participants
Veterans without prior outpatient antipsychotic use, who were hospitalized with HF between October 1, 2010, and September 30, 2015, and were subsequently discharged to a SNF.
Main Measures
Demographics, clinical conditions, prior healthcare utilization, and antipsychotic use data were ascertained from Veterans Administration records, Minimum Data Set assessments, and Medicare claims. The outcome of interest was continuation of antipsychotics into SNFs after hospital discharge.
Key Results
Among 18,008 Veterans, antipsychotics were newly prescribed for 1931 (10.7%) Veterans during the index hospitalization. Among new antipsychotic users, 415 (21.5%) continued antipsychotics in skilled nursing facilities after discharge. Dementia (adjusted OR (aOR) 1.48, 95% CI 1.11–1.98), psychosis (aOR 1.62, 95% CI 1.11–2.38), proportion of inpatient days with antipsychotic use (aOR 1.08, 95% CI 1.07–1.09, per 10% increase), inpatient use of only typical (aOR 0.47, 95% CI 0.30–0.72) or parenteral antipsychotics (aOR 0.39, 95% CI 0.20–0.78), and the day of hospital admission that antipsychotics were started (day 0–4 aOR 0.36, 95% CI 0.23–0.56; day 5–7 aOR 0.54, 95% CI 0.35–0.84 (reference: day > 7 of hospital admission)) were significant predictors of continuing antipsychotics into SNFs after hospital discharge.
Conclusions
Antipsychotics are initiated fairly often during HF admissions and are commonly continued into SNFs after discharge. Hospital providers should review antipsychotic indications and doses throughout admission and communicate a clear plan to SNFs if antipsychotics are continued after discharge.
KEY WORDS: antipsychotic agents, heart failure, hospitalization, nursing homes, older adults
INTRODUCTION
Heart failure (HF) is highly prevalent among older adults, affecting 6.9% of males and 4.8% of females 60–79 years old and 12.8% of males and 12.0% of females ≥ 80 years old, and is associated with significant healthcare utilization and costs.1 Older adults hospitalized for HF who cannot return home due to medical, functional, or social vulnerabilities are frequently transferred to skilled nursing facilities (SNFs) and are particularly susceptible to poor clinical outcomes.2–5 Given that new medications are often added to older adults’ medication regimens following a hospitalization,6–9 and multimorbidity and polypharmacy are common in older adults hospitalized for HF,10 increases in polypharmacy resulting from the hospitalization may further augment the risk of adverse drug events, drug interactions, or poor clinical outcomes. Of particular concern are medications started in the hospital and continued after discharge even when they are non-essential or are no longer indicated. Such medications are unlikely to provide additional benefits, but could potentially increase the risk for harms. Examining inpatient initiation of high-risk medications and predictors of medication continuation into SNFs post-hospital discharge may inform future strategies to reduce potentially harmful medication effects and improve outcomes for vulnerable older adults with HF.
Antipsychotics are commonly initiated during non-psychiatric hospital admissions.11–13 Due to the risk of severe medication adverse effects,14–21 limited evidence supporting antipsychotic use for several off-label indications,22–25 and concern that most new antipsychotic prescribing continued after hospital discharge is potentially inappropriate,26 multiple studies have examined inpatient antipsychotic initiation and factors associated with continuing antipsychotics after hospital discharge.11–13,27–30 However, antipsychotic use across transitions of care has rarely been studied specifically among individuals discharged to SNFs, although this group may be particularly susceptible to medication-related harms. Additionally, several challenges have precluded prior studies from reliably and accurately ascertaining antipsychotic use prior to, during, and after a hospital admission. Many studies do not link data from multiple care settings because clinicians and researchers are often limited in their ability to access and obtain the resources necessary to conduct such sophisticated analyses appropriately. Using administrative claims-based datasets alone would not provide information on both inpatient and outpatient medication use, while hospital electronic medical records often rely on error-prone admission or discharge medication lists for medication use prior to hospital admission or after hospital discharge.31,32
Using a data linkage that overcomes the aforementioned challenges, we aimed to describe patterns of new antipsychotic use in a national cohort of older adults hospitalized with HF and predictors of continuing antipsychotics into SNFs post-hospital discharge. Based on prior literature,11–13,27–30 we hypothesized that certain conditions (e.g., dementia, delirium), longer hospital length of stay, and inpatient drug characteristics such as antipsychotic type, route of administration, and duration of therapy would be important predictors of continuing antipsychotics into SNFs.
METHODS
Study Design and Data Sources
In this retrospective cohort study, we linked Veterans Health Administration (VHA) electronic medical records to VA outpatient pharmacy claims, Minimum Data Set (MDS) version 3.0 assessments, and Medicare claims using unique VA identifiers. VHA records include demographics, comorbidities, prior healthcare utilization, test results, outpatient medication dispensings, and inpatient barcode medication administration records. The MDS is a federally mandated, standardized resident assessment administered at scheduled intervals in Medicare- and Medicaid-certified SNFs.33 Assessments include information on clinical conditions, functional and cognitive status, and medications received in the facility. This study was approved by the Institutional Review Board at the Providence VA Medical Center.
Study Population
Our nationally representative study population included Veterans who were hospitalized for HF at a U.S. VA hospital between October 1, 2010, and September 30, 2015, and were subsequently discharged to a non-VA SNF. We examined non-VA SNFs as data restrictions prevented us from reliably ascertaining MDS records from VA-affiliated SNFs. Veterans were identified through hospitalization claims if an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for HF was documented in the primary position, regardless of HF type (Appendix Table 4). Discharges to SNF were included if an admission MDS assessment was documented up to 14 days after the date of discharge from the index HF hospitalization since MDS admission assessments must be completed by day 14 of the SNF-stay.33 Veterans were excluded if they resided in a nursing home prior to the index hospital admission, were dispensed antipsychotics in the 12 months before the index HF admission, were missing an admission or follow-up MDS assessment, or were missing variables derived from the MDS that were used during statistical modeling. For Veterans with multiple eligible HF hospitalizations with subsequent discharges to SNF, only the first hospital admission was included.
Table 4.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Codes Used to Identify Index Heart Failure Hospitalizations
| International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Codes | 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.0, 428.1, 428.20, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43, 428.9 |
Index heart failure admissions were identified if one of the above International Classification of Diseases, Ninth Revision, Clinical Modification codes was listed in the primary position on the inpatient claim
Antipsychotic Initiation During HF Hospitalization
Antipsychotic exposure was derived from three sources: (1) VA outpatient pharmacy dispensing claims (to identify and exclude individuals dispensed antipsychotics in the 12 months before the index admission), (2) VA barcode medication administration records for inpatient antipsychotic use, and (3) MDS assessments for antipsychotic use during the post-hospitalization SNF stay. Participants with antipsychotic initiation during hospitalization received at least one dose of an antipsychotic during the index HF admission.
Continuation of Hospital Antipsychotics into SNFs
Among participants with antipsychotic initiation during hospitalization, we classified individuals as those who discontinued antipsychotics at or prior to hospital discharge and those who continued antipsychotics into the SNF. Veterans were classified as continuing antipsychotics in the SNF if their admission MDS assessment reported receipt of an antipsychotic for at least one day out of the previous seven days in the SNF (or since SNF admission if the MDS assessment was completed prior to day 7 of SNF admission). For patients who continued antipsychotics into the SNF, we also examined the next available MDS follow-up assessment (nearest to the 30-day scheduled assessment, but no later than 90 days after SNF admission) to better understand how frequently antipsychotics are continued long-term. Participants with no documentation of antipsychotic administration on their admission MDS assessment were classified as having discontinued antipsychotics at or prior to hospital discharge.
Patient Characteristics
Demographics (e.g., age, sex, race/ethnicity) were measured using VHA records. Comorbidities were ascertained from VHA records using ICD-9-CM code documentation on inpatient and outpatient encounters from the year prior to SNF admission. Medicare claims were also used to identify patients with dementia (Appendix). We measured multimorbidity by summing the number of conditions in the set of comorbidity measures developed by Elixhauser et al.34 MDS assessments at SNF admission reported the cognitive function scale,35 functional status using a 28-point scale of independence in activities of daily living (ADLs),36 and presence of delirium using the Confusion Assessment Method.33 We ascertained data from the index HF admission using VHA records, including length of hospital stay, admission type, critical care requirement, use of mechanical ventilation, and palliative care prior to or during the index hospital admission. Ejection fraction, measured nearest to the time of index HF admission, was obtained from electronic medical record notes using an automated information extraction application validated for the VA. Finally, healthcare utilization costs were extracted from VA administrative records, which totaled inpatient, outpatient (including emergency department), and pharmacy costs in the year prior to the index hospitalization.
Inpatient Antipsychotic Characteristics
Medication name, dose, and route of administration were available for antipsychotics administered inpatient through VA barcode medication administration records. We also ascertained the day of hospital admission that antipsychotics were started, the number and proportion of days that antipsychotics were administered, the type of antipsychotic (typical or atypical), and route of administration. Antipsychotic type was based on the Food and Drug Administration classification framework (Appendix Table 5).37,38 Similar to prior literature,13 we constructed a measure for potentially excessive antipsychotic dosing by summing the doses for a specific antipsychotic for a given day and comparing it to the daily dose thresholds set forth in the Centers for Medicare and Medicaid Services guidelines for antipsychotic use in nursing homes.39 Any daily dose that exceeded this threshold was considered potentially excessive.
Table 5.
Antipsychotics Included in the Study, by Antipsychotic Type
| Typical antipsychotics | Atypical antipsychotics |
|---|---|
| Haloperidol | Quetiapine |
| Chlorpromazine | Lurasidone |
| Perphenazine | Olanzapine |
| Fluphenazine | Risperidone |
| Thiothixene | Aripiprazole |
| Trifluoperazine | Clozapine |
| Loxapine | Paliperidone |
| Thioridazine | Asenapine |
| Pimozide | Ziprasidone |
| Molindone | Amisulpride |
| Iloperidone |
Statistical Analysis
We compared patient characteristics between participants with and without antipsychotic initiation during hospitalization. Among participants with antipsychotic initiation during hospitalization, we compared patient and inpatient antipsychotic characteristics between those who discontinued antipsychotics at or prior to hospital discharge and those who continued antipsychotics into the SNF. Characteristics were summarized in proportions, means and standard deviations, or medians with the first and third quartiles. Cohen’s standardized mean differences were also reported.40 Additionally, we constructed univariable and multivariable random effects regression models with random intercepts for hospitals and SNFs to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for predictors of continuing antipsychotics into SNFs (versus discontinuing antipsychotics at or prior to hospital discharge). We checked variables for collinearity before entering them into the multivariable model based on variance inflation factors, all of which were less than 5. All analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Study Cohort
Our study cohort consisted of 18,008 older adults who were hospitalized for HF and were subsequently discharged to a SNF (Fig. 1). The mean (standard deviation) age of the overall cohort was 78.0 (10.1) years, 546 (3.0%) were female patients, and 14,269 (79.2%) were non-Hispanic White patients (Appendix Table 6). Antipsychotics were newly prescribed for 1931 (10.7%) individuals during their index hospitalization. Among participants with inpatient antipsychotic initiation, 415 (21.5%) received an antipsychotic in the SNF after hospital discharge, and of these, 328 (79.0%) also had antipsychotics documented at the next MDS follow-up assessment. Several patient characteristics differed between participants with and without antipsychotic initiation during hospitalization (Appendix Table 6).
Figure 1.
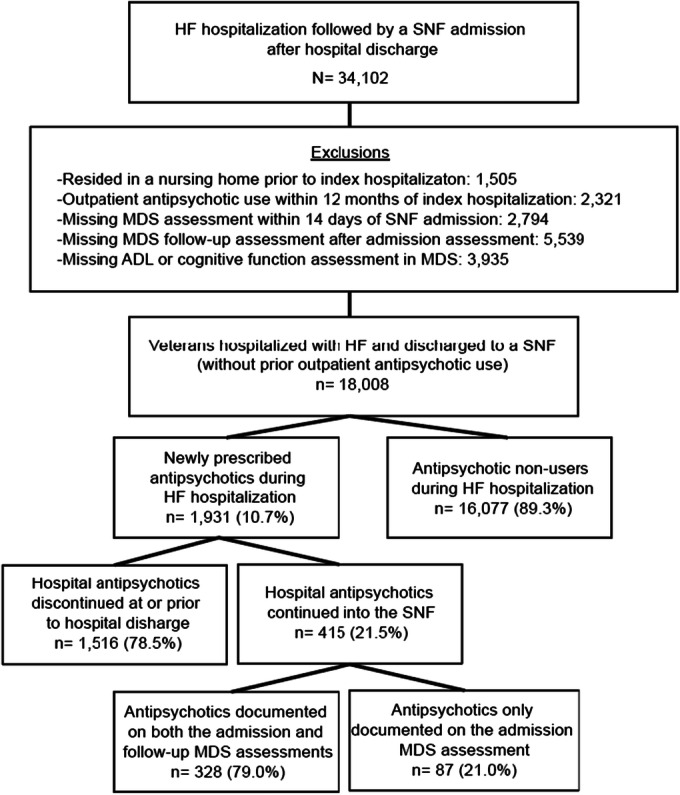
Flow diagram of Veterans hospitalized for heart failure and discharged to a skilled nursing facility by antipsychotic exposure, 2010–2015. Abbreviations: HF, heart failure; SNF, skilled nursing facility; MDS, minimum data set; ADL, activities of daily living.
Table 6.
Characteristics of Veterans Hospitalized for Heart Failure and Discharged to a Skilled Nursing Facility Overall and by Antipsychotic Exposure During Hospitalization, 2010–2015
| Characteristics |
Total (n = 18,008) |
No inpatient antipsychotic exposure (n = 16,077) |
Inpatient antipsychotic initiation (n = 1931) |
Standardized mean difference |
|---|---|---|---|---|
| Age, years, mean (SD) | 78.0 (10.1) | 77.9 (10.2) | 79.1 (9.6) | 0.12 |
| Female | 546 (3.0) | 491 (3.1) | 55 (2.9) | 0.01 |
| Race/ethnicity | 0.00 | |||
| Non-Hispanic White | 14,269 (79.2) | 12,747 (79.3) | 1522 (78.8) | |
| Non-Hispanic Black | 2848 (15.8) | 2542 (15.8) | 306 (15.9) | |
| Hispanic | 506 (2.8) | 442 (2.8) | 64 (3.3) | |
| Other | 385 (2.1) | 346 (2.2) | 39 (2.0) | |
| Heart failure type | 0.20 | |||
| EF 0–40%, reduced | 4599 (25.5) | 4167 (25.9) | 432 (22.4) | |
| EF 40–50%, borderline | 2572 (14.3) | 2349 (14.6) | 223 (11.6) | |
| EF > 50%, preserved | 4715 (26.2) | 4240 (26.4) | 475 (24.6) | |
| EF missing | 6122 (34.0) | 5321 (33.1) | 801 (41.5) | |
| Conditions | ||||
| Comorbidity index, mean (SD)* | 4.6 (2.7) | 4.7 (2.7) | 4.0 (2.6) | − 0.29 |
| Dementia | 5254 (29.2) | 4378 (27.2) | 876 (45.4) | 0.38 |
| Delirium | 691 (3.8) | 543 (3.4) | 148 (7.8) | 0.19 |
| Chronic lung disease | 7597 (42.2) | 6874 (42.8) | 723 (37.4) | − 0.10 |
| Diabetes | 9151 (50.8) | 8279 (51.5) | 872 (45.2) | − 0.13 |
| Hypothyroidism | 2576 (14.3) | 2356 (14.7) | 220 (11.4) | − 0.09 |
| Chronic kidney disease | 1689 (9.4) | 1558 (9.7) | 131 (6.8) | − 0.11 |
| Tumor history | 3141 (17.4) | 2849 (17.7) | 294 (15.2) | − 0.07 |
| Obesity | 3689 (20.5) | 3401 (21.2) | 288 (14.9) | − 0.16 |
| Weight loss | 1652 (9.2) | 1487 (9.3) | 165 (8.5) | − 0.02 |
| Anemia | 6745 (37.5) | 6157 (38.3) | 588 (30.5) | − 0.17 |
| Alcohol use disorder | 1257 (7.0) | 1114 (6.9) | 143 (7.4) | 0.02 |
| Substance use disorder | 557 (3.1) | 509 (3.2) | 48 (2.5) | − 0.04 |
| Psychosis | 2040 (11.3) | 1783 (11.1) | 257 (13.3) | 0.07 |
| Depression | 3934 (21.9) | 3551 (22.1) | 383 (19.8) | − 0.06 |
| Healthcare utilization in previous year, $, mean (SD)† | 29,160 (37,147) | 29,897 (37,691) | 23,024 (31,612) | − 0.20 |
| Index hospitalization | ||||
| Admission LOS, days, mean (SD) | 10.5 (8.8) | 9.9 (8.1) | 15.8 (11.6) | 0.60 |
| Type of admission | 0.17 | |||
| Medicine | 15,591 (86.6) | 13,937 (86.7) | 1654 (85.7) | |
| Surgery | 1774 (9.8) | 1529 (9.5) | 245 (12.7) | |
| Psychiatry | 643 (3.6) | 611 (3.8) | 32 (1.7) | |
| ICU stay during admission | 2585 (14.4) | 2110 (13.1) | 475 (24.6) | 0.30 |
| Mechanical ventilation | 794 (4.4) | 508 (3.2) | 286 (14.8) | 0.42 |
| Palliative care | 2244 (12.5) | 1880 (11.7) | 364 (18.9) | 0.20 |
| SNF admission assessment | ||||
| Cognitive function‡ | 0.53 | |||
| Intact | 9466 (52.7) | 8834 (55.2) | 632 (32.9) | |
| Mild impairment | 5212 (29.0) | 4624 (28.8) | 588 (30.6) | |
| Moderate impairment | 2776 (15.5) | 2184 (13.6) | 592 (30.8) | |
| Severe impairment | 495 (2.8) | 386 (2.4) | 109 (5.7) | |
| ADL dependency score, mean (SD)§ | 16.2 (5.1) | 16.1 (5.1) | 16.8 (5.2) | 0.14 |
Characteristics reported as number (percent (%)) unless otherwise indicated
ADL activities of daily living, EF ejection fraction, ICU intensive care unit, LOS length of stay, SNF skilled nursing facility
*Sum of the number of conditions listed in the set of comorbidity measures developed by Elixhauser et al.
†Sum of inpatient, outpatient (including emergency department), and pharmacy costs in the year prior to index hospitalization. Presents costs in terms of US dollars (not inflation adjusted)
‡Derived from the Minimum Data Set Cognitive Function Scale, where higher scores indicate greater impairment in cognition
§Derived from the Minimum Data Set 28-point scale of independence in activities of daily living, where higher scores indicate greater dependency in activities of daily living
Age was similar between participants who continued antipsychotics into SNFs versus discontinued antipsychotics at or prior to hospital discharge (Table 1). Individuals who continued antipsychotics into SNFs after hospital discharge generally had fewer comorbidities and lower prior healthcare utilization costs, but a greater proportion had diagnoses of dementia, delirium, and psychosis. During the index HF admission, hospital length of stay and the proportion of patients with a flag for palliative care were similar between groups. A smaller proportion of those who continued antipsychotics into SNFs had an admission to the ICU or required mechanical ventilation. Once discharged to the SNF, admission MDS assessments for participants who continued antipsychotics reported greater cognitive impairment, but dependency in ADLs was similar to participants who discontinued antipsychotics at or prior to hospital discharge.
Table 1.
Characteristics of Veterans Hospitalized for Heart Failure and Discharged to a Skilled Nursing Facility among Participants with Inpatient Antipsychotic Initiation, 2010–2015
| Characteristics |
Total (N = 1931) |
Antipsychotics D/C’d prior to discharge (n = 1516) |
Antipsychotics continued into SNFs (n = 415) |
Standardized mean difference |
|---|---|---|---|---|
| Age, years, mean (SD) | 79.1 (9.6) | 79.0 (9.5) | 79.4 (9.8) | 0.04 |
| Female | 55 (2.9) | 41 (2.7) | 14 (3.4) | − 0.04 |
| Race/ethnicity | 0.25 | |||
| Non-Hispanic White | 1522 (78.8) | 1201 (79.2) | 321 (77.4) | |
| Non-Hispanic Black | 306 (15.9) | 231 (15.2) | 75 (18.1) | |
| Hispanic | 64 (3.3) | |||
| Other | 39 (2.0) | 26 (1.7) | 13 (3.1) | |
| Heart failure type | 0.10 | |||
| EF 0–40%, reduced | 432 (22.4) | 339 (22.4) | 93 (22.4) | |
| EF 40–50%, borderline | 223 (11.6) | 184 (12.1) | 39 (9.4) | |
| EF > 50%, preserved | 475 (24.6) | 370 (24.4) | 105 (25.3) | |
| EF missing | 801 (41.5) | 623 (41.1) | 178 (42.9) | |
| Conditions | ||||
| Comorbidity index, mean (SD)* | 4.0 (2.6) | 4.0 (2.7) | 3.7 (2.6) | − 0.14 |
| Dementia | 876 (45.4) | 624 (41.2) | 252 (60.7) | 0.40 |
| Delirium | 148 (7.7) | 103 (6.8) | 45 (10.8) | 0.14 |
| Chronic lung disease | 723 (37.4) | 592 (39.1) | 131 (31.6) | − 0.16 |
| Diabetes | 872 (45.2) | 702 (46.3) | 170 (41.0) | − 0.11 |
| Hypothyroidism | 220 (11.4) | 169 (11.2) | 51 (12.3) | 0.04 |
| Chronic kidney disease | 131 (6.8) | 109 (7.2) | 22 (5.3) | − 0.08 |
| Tumor history | 294 (15.2) | 238 (15.7) | 56 (13.5) | − 0.06 |
| Obesity | 288 (14.9) | 242 (16.1) | 44 (10.6) | − 0.16 |
| Weight loss | 165 (8.5) | 129 (8.5) | 36 (8.7) | 0.01 |
| Anemia | 588 (30.5) | 478 (31.5) | 110 (26.5) | − 0.11 |
| Alcohol use disorder | 143 (7.4) | 119 (7.9) | 24 (5.8) | − 0.08 |
| Substance use disorder | 48 (2.5) | 33 (2.2) | 15 (3.6) | 0.09 |
| Psychosis | 257 (13.3) | 180 (11.9) | 77 (18.6) | 0.19 |
| Depression | 383 (19.8) | 307 (20.3) | 76 (18.3) | − 0.05 |
| Healthcare utilization in previous year, $, mean (SD)† | 23,024 (31,611) | 24,024 (33,319) | 19,373 (24,061) | − 0.16 |
| Index hospitalization | ||||
| Admission LOS, days, mean (SD) | 15.8 (11.6) | 15.9 (11.6) | 15.3 (11.6) | − 0.05 |
| Type of admission | 0.21 | |||
| Medicine | 1654 (85.7) | 1298 (85.6) | 356 (85.8) | |
| Surgery | 245 (12.7) | 202 (13.3) | 43 (10.4) | |
| Psychiatry | 32 (1.7) | 16 (1.1) | 16 (3.8) | |
| ICU stay during admission | 475 (24.6) | 395 (26.1) | 80 (19.3) | − 0.16 |
| Mechanical ventilation | 286 (14.8) | 244 (16.1) | 42 (10.1) | − 0.18 |
| Palliative care | 364 (18.9) | 284 (18.7) | 80 (19.3) | 0.01 |
| SNF admission assessment | ||||
| Cognitive function‡ | 0.29 | |||
| Intact | 632 (32.9) | 519 (34.4) | 113 (27.4) | |
| Mild impairment | 588 (30.6) | 486 (32.2) | 102 (24.7) | |
| Moderate impairment | 592 (30.8) | 426 (28.3) | 166 (40.2) | |
| Severe impairment | 109 (5.7) | 77 (5.1) | 32 (7.8) | |
| ADL dependency score, mean (SD)§ | 16.8 (5.2) | 16.7 (5.2) | 17.1 (5.1) | 0.07 |
Characteristics reported as number (percent (%)) unless otherwise indicated. Some cells were left blank due to data use agreements that require the suppression of small cells (< 11 individuals)
D/C’d discontinued, SNF skilled nursing facility, SD standard deviation, EF ejection fraction, LOS length of stay, ICU intensive care unit, ADL activities of daily living
*Sum of the number of conditions listed in the set of comorbidity measures developed by Elixhauser et al.
†Sum of inpatient, outpatient (including emergency department), and pharmacy costs in the year prior to index hospitalization. Presents costs in terms of US dollars (not inflation adjusted)
‡Derived from the Minimum Data Set Cognitive Function Scale, where higher scores indicate greater impairment in cognition
§Derived from the Minimum Data Set 28-point scale of independence in activities of daily living, where higher scores indicate greater dependency in activities of daily living
Inpatient Antipsychotic Characteristics
Among participants with antipsychotic initiation during hospitalization, antipsychotics were typically started around day four of hospital admission and 44.4% of admissions included at least one potentially excessive daily dose of antipsychotics (Table 2). Antipsychotics were administered for a greater number of inpatient days and a greater proportion of inpatient days for individuals who continued antipsychotics into the SNF versus those who discontinued antipsychotics at or prior to hospital discharge. Individuals who continued antipsychotics into the SNF also had a greater proportion of inpatient days with potentially excessive antipsychotic dosing. Participants who continued antipsychotics into the SNF were less likely to have been treated with only typical antipsychotics or only parenteral antipsychotics during their index HF admission.
Table 2.
Inpatient Antipsychotic Use Characteristics Among Veterans Hospitalized for Heart Failure and Discharged to a Skilled Nursing Facility, 2010–2015
| Antipsychotic characteristics during index HF admission |
Overall (n = 1931) |
Antipsychotics D/C’d prior to discharge (n = 1516) |
Antipsychotics continued into SNFs (n = 415) |
Standardized mean difference |
|---|---|---|---|---|
| Day of hospital admission antipsychotic started, median (Q1, Q3) | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 3.0 (2.0, 6.0) | − 0.14 |
| Number of days antipsychotic administered, median (Q1, Q3) | 3.0 (1.0, 7.0) | 2.0 (1.0, 6.0) | 8.0 (4.0, 13.0) | 0.71 |
| Proportion (%) of days antipsychotics administered, median (Q1, Q3) | 26.7 (11.6, 57.1) | 20.0 (10.0, 42.9) | 62.9 (40.0, 82.4) | 1.21 |
| Type of antipsychotic, n (%) | 0.78 | |||
| Typical only | 808 (41.8) | 741 (48.9) | 67 (16.1) | |
| Atypical only | 657 (34.0) | 479 (31.6) | 178 (42.9) | |
| Both typical and atypical | 466 (24.1) | 296 (19.5) | 170 (41.0) | |
| Antipsychotic route of administration, n (%) | 0.08 | |||
| Oral only | 891 (46.1) | 666 (43.9) | 226 (54.5) | |
| Parenteral only | 482 (25.0) | 473 (31.2) | 14 (3.4) | |
| Both oral and parenteral | 528 (27.3) | 377 (24.9) | 175 (42.2) | |
| Admissions with at least one day of potentially excessive antipsychotic dosing, n (%)* | ||||
| Any antipsychotic exposure | 858 (44.4) | 677 (44.7) | 181 (43.6) | − 0.41 |
| Exposure to typical antipsychotics only | 447 (55.3) | 418 (56.4) | 29 (43.2) | − 0.49 |
| Exposure to atypical antipsychotics only | 68 (10.4) | 36 (7.5) | 32 (18.0) | 0.20 |
| Exposure to both typical and atypical antipsychotics | 343 (73.6) | 223 (75.3) | 120 (70.6) | − 0.37 |
| Number of days with potentially excessive antipsychotic dosing, mean (SD)* | ||||
| Any antipsychotic exposure | 1.5 (3.5) | 1.3 (3.2) | 2.1 (4.4) | 0.20 |
| Exposure to typical antipsychotics only | 1.4 (2.7) | 1.3 (2.5) | 2.1 (4.2) | 0.23 |
| Exposure to atypical antipsychotics only | 0.6 (2.4) | 0.3 (1.7) | 1.2 (3.6) | 0.30 |
| Exposure to both typical and atypical antipsychotics | 3.0 (5.2) | 2.9 (5.3) | 3.1 (5.1) | 0.03 |
| Proportion (%) of days with potentially excessive antipsychotic dosing, mean (SD)* | ||||
| Any antipsychotic exposure | 9.7 (17.8) | 8.6 (15.9) | 13.4 (23.3) | 0.24 |
| Exposure to typical antipsychotics only | 10.5 (16.9) | 10.2 (15.9) | 14.4 (25.1) | 0.20 |
| Exposure to atypical antipsychotics only | 4.2 (16.3) | 2.5 (11.9) | 8.6 (24.1) | 0.32 |
| Exposure to both typical and atypical antipsychotics | 15.9 (19.1) | 14.7 (18.1) | 17.9 (20.7) | 0.16 |
HF heart failure, D/C’d discontinued, SNF skilled nursing facility, Q1 quartile 1, Q3 quartile 3, SD standard deviation
*Denominators are the corresponding cells from the “Type of antipsychotic” variable
Predictors of Continuing Hospital Antipsychotics into SNFs
In the univariable model, multiple characteristics were associated with continuing antipsychotics into SNFs after hospital discharge (Appendix Table 7). However, in the multivariable model, only dementia (adjusted OR (aOR) 1.48, 95% CI 1.11–1.98), psychosis (aOR 1.62, 95% CI 1.11–2.38), proportion of inpatient days with antipsychotic use (aOR 1.08, 95% CI 1.07–1.09, per 10% increase), inpatient use of only typical (aOR 0.47, 95% CI 0.30–0.72) or parenteral antipsychotics (aOR 0.39, 95% CI 0.20–0.78), and the day of hospital admission that antipsychotics were started (day 0–4 aOR 0.36, 95% CI 0.23–0.56; day 5–7 aOR 0.54, 95% CI 0.35–0.84 (reference: day > 7 of hospital admission)) remained significant predictors of continuing antipsychotics into SNFs after hospital discharge (Table 3).
Table 7.
Univariable Model Estimating Odds of Continuing an Antipsychotic into a Skilled Nursing Facility After Hospital Discharge, Among Participants with Inpatient Antipsychotic Initiation
| Characteristic | Odds ratio | 95% confidence interval | P value | |
|---|---|---|---|---|
| Age, per 5 years | 1.02 | 0.96 | 1.08 | 0.50 |
| Female | 1.29 | 0.70 | 2.40 | 0.42 |
| Race/ethnicity | ||||
| Non-Hispanic White | Reference | |||
| Non-Hispanic Black | 1.17 | 0.88 | 1.57 | 0.28 |
| Hispanic | 0.38 | 0.16 | 0.90 | 0.03 |
| Other | 1.83 | 0.93 | 3.60 | 0.08 |
| Heart failure type | ||||
| EF 0–40%, reduced | Reference | |||
| EF 40–50%, borderline | 0.77 | 0.51 | 1.17 | 0.23 |
| EF > 50%, preserved | 1.03 | 0.75 | 1.42 | 0.84 |
| EF missing | 1.04 | 0.78 | 1.38 | 0.81 |
| Conditions | ||||
| Comorbidity index* | ||||
| Comorbidity index ≥ 6 | Reference | |||
| Comorbidity index 3–5 | 1.27 | 0.96 | 1.68 | 0.10 |
| Comorbidity index 0–2 | 1.39 | 1.04 | 1.86 | 0.03 |
| Dementia | 2.21 | 1.77 | 2.76 | < 0.001 |
| Delirium | 1.67 | 1.15 | 2.42 | 0.007 |
| Chronic lung disease | 0.72 | 0.57 | 0.91 | 0.006 |
| Diabetes | 0.79 | 0.64 | 0.99 | 0.04 |
| Hypothyroidism | 1.12 | 0.80 | 1.57 | 0.50 |
| Chronic kidney disease | 0.73 | 0.46 | 1.18 | 0.20 |
| Tumor history | 0.85 | 0.62 | 1.16 | 0.30 |
| Obesity | 0.62 | 0.44 | 0.87 | 0.006 |
| Weight loss | 1.03 | 0.70 | 1.51 | 0.90 |
| Anemia | 0.78 | 0.61 | 1.00 | 0.05 |
| Alcohol use disorder | 0.73 | 0.46 | 1.15 | 0.17 |
| Substance use disorder | 1.71 | 0.92 | 3.18 | 0.09 |
| Psychosis | 1.69 | 1.26 | 2.27 | < 0.001 |
| Depression | 0.89 | 0.67 | 1.18 | 0.42 |
| Healthcare utilization in previous year, per $5000† | 0.97 | 0.95 | 0.99 | 0.009 |
| Index hospitalization LOS | ||||
| ≥ 15 days | Reference | . | ||
| 8–14 days | 1.04 | 0.81 | 1.35 | 0.74 |
| 1–7 days | 1.19 | 0.91 | 1.56 | 0.21 |
| Type of admission | ||||
| Medicine | Reference | |||
| Surgery | 0.79 | 0.55 | 1.12 | 0.18 |
| Psychiatry | 3.57 | 1.77 | 7.22 | < 0.001 |
| ICU stay during index hospitalization | 0.68 | 0.52 | 0.89 | 0.005 |
| Mechanical ventilation during index hospitalization | 0.59 | 0.42 | 0.84 | 0.003 |
| Cognitive function‡ | ||||
| Intact | Reference | |||
| Mild impairment | 0.96 | 0.72 | 1.29 | 0.79 |
| Moderate impairment | 1.78 | 1.36 | 2.34 | < 0.001 |
| Severe impairment | 1.91 | 1.21 | 3.02 | 0.006 |
| ADL dependency score§ | ||||
| ≥ 20 | Reference | |||
| 15–19 | 0.85 | 0.66 | 1.10 | 0.21 |
| 0–14 | 0.81 | 0.61 | 1.09 | 0.17 |
| Day of index hospital admission antipsychotic started | ||||
| Day > 7 of hospital admission | Reference | |||
| Day 5–7 of hospital admission | 1.03 | 0.72 | 1.47 | 0.87 |
| Day 0–4 of hospital admission | 1.54 | 1.16 | 2.04 | 0.003 |
| Proportion of days antipsychotics administered, per 10% increase | 1.09 | 1.08 | 1.10 | < 0.001 |
| Type of antipsychotic during index hospitalization | ||||
| Both typical and atypical | Reference | |||
| Typical only | 0.16 | 0.11 | 0.21 | < 0.001 |
| Atypical only | 0.65 | 0.50 | 0.83 | < 0.001 |
| Antipsychotic route of administration during index hospitalization | ||||
| Both oral and parenteral | Reference | |||
| Oral only | 0.73 | 0.58 | 0.93 | 0.01 |
| Parenteral only | 0.06 | 0.04 | 0.11 | < 0.001 |
| Potentially excessive antipsychotic dosing during admission | 0.34 | 0.25 | 0.47 | < 0.001 |
Model adjusted for random effects of hospitals and skilled nursing facilities
EF ejection fraction, LOS length of stay, ICU intensive care unit, ADL activities of daily living
*Sum of the number of conditions listed in the set of comorbidity measures developed by Elixhauser et al.
†Sum of inpatient, outpatient (including emergency department), and pharmacy costs in the year prior to index hospitalization. Presents costs in terms of US dollars (not inflation adjusted)
‡Derived from the Minimum Data Set Cognitive Function Scale, where higher scores indicate greater impairment in cognition
§Derived from the Minimum Data Set 28-point scale of independence in activities of daily living, where higher scores indicate greater dependency in activities of daily living
Table 3.
Multivariable Model Estimating Odds of Continuing an Antipsychotic into a Skilled Nursing Facility After Hospital Discharge, Among Participants with Inpatient Antipsychotic Initiation
| Characteristic | Odds ratio | 95% confidence interval | p value | |
|---|---|---|---|---|
| Age, per 5 years | 1.01 | 0.93 | 1.10 | 0.78 |
| Female | 1.53 | 0.73 | 3.18 | 0.26 |
| Race/ethnicity | ||||
| Non-Hispanic White | Reference | |||
| Non-Hispanic Black | 1.03 | 0.72 | 1.48 | 0.86 |
| Hispanic | 0.40 | 0.15 | 1.03 | 0.06 |
| Other | 1.78 | 0.77 | 4.13 | 0.18 |
| Heart failure type | ||||
| EF 0–40%, reduced | Reference | |||
| EF 40–50%, borderline | 0.76 | 0.46 | 1.25 | 0.28 |
| EF > 50%, preserved | 1.07 | 0.73 | 1.56 | 0.74 |
| EF missing | 0.70 | 0.49 | 1.01 | 0.06 |
| Conditions | ||||
| Comorbidity index* | ||||
| Comorbidity index ≥ 6 | Reference | |||
| Comorbidity index 3–5 | 0.88 | 0.58 | 1.35 | 0.57 |
| Comorbidity index 0–2 | 0.80 | 0.44 | 1.46 | 0.48 |
| Dementia | 1.48 | 1.11 | 1.98 | 0.008 |
| Delirium | 1.14 | 0.73 | 1.81 | 0.56 |
| Chronic lung disease | 0.86 | 0.63 | 1.17 | 0.32 |
| Diabetes | 0.97 | 0.72 | 1.30 | 0.82 |
| Hypothyroidism | 0.96 | 0.64 | 1.46 | 0.86 |
| Chronic kidney disease | 0.89 | 0.49 | 1.61 | 0.70 |
| Tumor history | 0.98 | 0.67 | 1.44 | 0.93 |
| Obesity | 0.85 | 0.55 | 1.30 | 0.45 |
| Weight loss | 1.15 | 0.71 | 1.88 | 0.57 |
| Anemia | 0.82 | 0.58 | 1.14 | 0.24 |
| Alcohol use disorder | 0.69 | 0.38 | 1.22 | 0.21 |
| Substance use disorder | 1.77 | 0.76 | 4.09 | 0.19 |
| Psychosis | 1.62 | 1.11 | 2.38 | 0.01 |
| Depression | 0.80 | 0.55 | 1.15 | 0.23 |
| Healthcare utilization in previous year, per $5000† | 0.98 | 0.95 | 1.01 | 0.18 |
| Index hospitalization LOS | ||||
| ≥ 15 days | Reference | |||
| 8–14 days | 1.02 | 0.72 | 1.44 | 0.92 |
| 1–7 days | 1.25 | 0.83 | 1.88 | 0.30 |
| Type of admission | ||||
| Medicine | Reference | |||
| Surgery | 0.93 | 0.62 | 1.40 | 0.73 |
| Psychiatry | 1.46 | 0.61 | 3.48 | 0.40 |
| ICU stay during index hospitalization | 1.02 | 0.73 | 1.42 | 0.92 |
| Mechanical ventilation during index hospitalization | 0.82 | 0.52 | 1.30 | 0.41 |
| Cognitive function‡ | ||||
| Intact | Reference | |||
| Mild impairment | 0.72 | 0.50 | 1.02 | 0.07 |
| Moderate impairment | 1.12 | 0.77 | 1.63 | 0.57 |
| Severe impairment | 0.97 | 0.53 | 1.79 | 0.93 |
| ADL dependency score§ | ||||
| ≥ 20 | Reference | |||
| 15–19 | 0.95 | 0.70 | 1.30 | 0.76 |
| 0–14 | 0.82 | 0.56 | 1.18 | 0.29 |
| Day of index hospital admission antipsychotic started | ||||
| Day > 7 of hospital admission | Reference | |||
| Day 5–7 of hospital admission | 0.54 | 0.35 | 0.84 | 0.007 |
| Day 0–4 of hospital admission | 0.36 | 0.23 | 0.56 | < 0.001 |
| Proportion of days antipsychotics administered, per 10% increase | 1.08 | 1.07 | 1.09 | < 0.001 |
| Type of antipsychotic during index hospitalization | ||||
| Both typical and atypical | Reference | |||
| Typical only | 0.47 | 0.30 | 0.72 | < 0.001 |
| Atypical only | 0.73 | 0.46 | 1.15 | 0.18 |
| Antipsychotic route of administration during index hospitalization | ||||
| Both oral and parenteral | Reference | |||
| Oral only | 1.08 | 0.70 | 1.65 | 0.74 |
| Parenteral only | 0.39 | 0.20 | 0.78 | 0.009 |
| Potentially excessive antipsychotic dosing during admission | 0.75 | 0.49 | 1.16 | 0.20 |
Model adjusted for random effects of hospitals and skilled nursing facilities
EF ejection fraction, LOS length of stay, ICU intensive care unit, ADL activities of daily living
*Sum of the number of conditions listed in the set of comorbidity measures developed by Elixhauser et al.
†Sum of inpatient, outpatient (including emergency department), and pharmacy costs in the year prior to index hospitalization. Presents costs in terms of US dollars (not inflation adjusted)
‡Derived from the Minimum Data Set Cognitive Function Scale, where higher scores indicate greater impairment in cognition
§Derived from the Minimum Data Set 28-point scale of independence in activities of daily living, where higher scores indicate greater dependency in activities of daily living
DISCUSSION
In this national retrospective cohort study, several important findings emerged. First, one in ten older adults hospitalized for HF and eventually discharged to a SNF were newly prescribed an antipsychotic medication during their hospitalization. Second, one in five patients who were newly prescribed an antipsychotic continued the medication upon discharge to a SNF, and of these individuals, nearly 80% remained on antipsychotics at the time of their MDS follow-up assessment. Third, several patient and medication characteristics were associated with continuing antipsychotics after hospital discharge, which could guide future interventions to reduce the potentially harmful continuation of antipsychotics during transitions from hospitals to SNFs. Taken together, these findings highlight important opportunities to evaluate and improve the clinical care provided to older adults hospitalized for HF as they transition across care settings.
Prior studies reported that antipsychotics were initiated in 5–9% of non-psychiatric hospital admissions,11–13 although these studies did not focus specifically on individuals discharged to SNFs or those with a diagnosis of HF. Examining patients with HF separately may be beneficial since HF is a chronic, progressive disease associated with tremendous healthcare utilization and costs, with the potential for worse clinical outcomes due to antipsychotic-related adverse effects. It may be especially important to study the post-acute care period for older adults discharged to SNFs since the risk for some antipsychotic-related adverse outcomes is greater for new or short-term antipsychotic users.16,19,41–44 A more thorough understanding of the risks of new inpatient antipsychotic use on outcomes during the post-acute care period is necessary to guide safe prescribing practices, including when and for whom to initiate this medication class, as well as the appropriate duration of therapy. Such information would be particularly useful for deprescribing efforts.
The finding that 21.5% of participants with inpatient antipsychotic initiation continued antipsychotics into SNFs is similar to previous studies examining antipsychotic continuation after hospital discharge.11,12,27–30 Although antipsychotics may be intended for short-term therapy, patients discharged on antipsychotics often remain on the medications long-term.45 In our study, nearly 80% of participants who continued antipsychotics from the hospital into the SNF also received the medications at their next follow-up assessment. Since a majority of antipsychotic use in nursing homes may be inappropriate,46,47 there is a need to improve medication review processes across transitions of care. The hospital is an important setting where antipsychotics are started for nursing home residents,48 and continuing the medication after hospital discharge may have unintended consequences such as long-term continuation. If discharge documentation provided to SNFs by the hospitals is inaccurate or incomplete, SNF staff may not recognize the indication for antipsychotic use, and may perceive the medication as chronic rather than short-term therapy.
Documenting the indication for antipsychotics, the intended duration of therapy, and a written plan if antipsychotics are intended for use after hospital discharge may help to reduce the inappropriate long-term continuation of antipsychotics. Clear communication is especially important since little evidence supports off-label antipsychotic prescribing for indications such as delirium and behavioral and psychological symptoms of dementia,22–25 and if needed, the lowest effective dose should be administered for a short duration.25,49–52 Guidelines recommend discontinuing inpatient antipsychotics when the severe or distressing symptoms of delirium resolve, ideally before hospital discharge.51,52 The treatment duration for behavioral and psychological symptoms of dementia is less clear, although a trial of antipsychotic therapy may last several weeks to months.50 Regardless of the treatment response, an attempt should be made to taper and withdraw (i.e., deprescribe) antipsychotics due to the risk of severe medication adverse effects. If antipsychotics are intended for use after hospital discharge, hospital providers should provide a written plan to the SNF for tapering and withdrawing therapy so the medications are not continued long-term unnecessarily. Future research should examine if the factors driving antipsychotic continuation after hospital discharge differ by indication to guide future interventions that reduce potentially inappropriate antipsychotic continuation into SNFs.
Describing characteristics associated with continuing antipsychotics into SNFs after hospital discharge is an essential step toward guiding future quality improvement interventions. Based on our results, patients with a diagnosis of dementia or psychosis and a higher proportion of inpatient days with antipsychotic use, and those who start antipsychotics after day 7 of the hospital stay, are more likely to continue antipsychotics into SNFs after hospital discharge. Developing and validating formal risk stratification tools may be highly useful to identify such patients who may benefit most from antipsychotic medication review and/or deprescribing interventions. These interventions may include “timeouts,” which have been previously described in relation to antibiotic stewardship,53 where clinicians would reassess antipsychotic doses and the continued need for antipsychotics over the course of the hospitalization. Implementing structured antipsychotic tapering and discontinuation protocols may also be beneficial.54 Integrating these reminders, protocols, and risk stratification tools into the electronic medical record systems of both the hospital and the SNF involved in a patient’s care may be a potential approach to improve an intervention’s efficiency and uptake into routine workflow.
Our results should be interpreted in light of several limitations. First, our results may not generalize to female patients, individuals hospitalized outside of the VA health system, or those discharged to VA-affiliated SNFs. Second, we did not have information on some variables that may influence the decision to start antipsychotics inpatient or continue them after hospital discharge, including the indication for antipsychotics, behavioral problems during hospitalization (e.g., physically abusive to staff), inpatient consultative services (e.g., psychiatry), or facility-level characteristics.13, 55 Third, our study was not designed to examine antipsychotic polypharmacy for individuals receiving more than one antipsychotic in a given day. Finally, a large proportion of admissions were missing a recent ejection fraction, which limits the interpretation of HF type in our study population. Despite these limitations, to our knowledge, this is the first study describing antipsychotic use patterns and predictors of antipsychotic continuation for patients hospitalized with HF and discharged to SNFs.
In conclusion, we found that antipsychotics were initiated fairly often during HF admissions and were commonly continued into SNFs after discharge. A majority of participants who continued antipsychotics into SNFs remained on the medications at their next SNF follow-up assessment. To reduce the potentially inappropriate and harmful continuation of antipsychotics into SNFs after hospital discharge, future interventions should focus on improving processes to review and communicate antipsychotic indications, doses, and plans to continue therapy throughout the hospital admission and at transitions of care.
Appendix
Enhanced definition of dementia diagnosis using Medicare claims data
Based on prior experience working with these data, we hypothesized that dementia diagnoses would be underreported in Veterans Health Administration electronic medical records. Therefore, we used an enhanced definition that ascertained dementia diagnoses from International Classification of Diseases, Ninth Revision, Clinical Modification code documentation on inpatient and outpatient encounters in the year prior to the index skilled nursing facility admission using both Veterans Health Administration electronic medical records and Medicare claims data. Among 18,008 participants without previous outpatient antipsychotic use, 17,165 (95.3%) were Medicare eligible during the year of the index heart failure admission/skilled nursing facility stay. Of the 1931 participants with inpatient antipsychotic initiation in the study population, 1861 (96.4%) were Medicare eligible. Medicare eligibility during the year of the index heart failure admission/skilled nursing facility stay was evenly distributed among participants who continued antipsychotics into skilled nursing facilities versus discontinued antipsychotics at or prior to hospital discharge (96.14% vs. 96.44%).
Funding
VA Health Services Research and Development (CIN 13-419).
Role of the Funding Source
The funding organization was not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Financial Support
Some authors are VA employees (L.J., S.E., J.L.R., J.E.M., N.M.R-P., C.M., L.Q., W-C.W., and A.R.Z.). The content and views expressed in this article are those of the authors and do not necessarily reflect the position or official policies of the United States Government or the US Department of Veterans Affairs. This work was also partially supported by the William S. Middleton Veteran Affairs Hospital, Madison, WI (Dr. Rogus-Pulia, GRECC Manuscript 010-2021); Center of Innovation in Long-term Services and Supports at the Providence VA Medical Center via the Office of Academic Affiliation’s Advanced Fellowship in Health Services Research (Dr. Madrigal); and National Institute on Aging (R21AG061632, R01AG065722, RF1AG061221, R24AG064025, and R01AG062492 to Dr. Zullo).
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4(3):293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orr NM, Boxer RS, Dolansky MA, et al. Skilled Nursing Facility Care for Patients With Heart Failure: Can We Make It "Heart Failure Ready?". J Card Fail. 2016;22(12):1004–14. doi: 10.1016/j.cardfail.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orr NM, Forman DE, De Matteis G, et al. Heart Failure Among Older Adults in Skilled Nursing Facilities: More of a Dilemma Than Many Now Realize. Curr Geriatr Rep. 2015;4(4):318–26. doi: 10.1007/s13670-015-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orr NM, Jones CD, Daddato AE, et al. Post-acute Care for Patients with Heart Failure. Curr Cardiovasc Risk Rep. 2018;12(18).
- 6.Mansur N, Weiss A, Beloosesky Y. Relationship of in-hospital medication modifications of elderly patients to postdischarge medications, adherence, and mortality. Ann Pharmacother. 2008;42(6):783–9. doi: 10.1345/aph.1L070. [DOI] [PubMed] [Google Scholar]
- 7.Harris CM, Sridharan A, Landis R, et al. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150–3. doi: 10.1097/PTS.0b013e318286f87d. [DOI] [PubMed] [Google Scholar]
- 8.Weir DL, Lee TC, McDonald EG, et al. Both New and Chronic Potentially Inappropriate Medications Continued at Hospital Discharge Are Associated With Increased Risk of Adverse Events. J Am Geriatr Soc. 2020;68(6):1184–92. doi: 10.1111/jgs.16413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goyal P, Kneifati-Hayek J, Archambault A, et al. Prescribing Patterns of Heart Failure-Exacerbating Medications Following a Heart Failure Hospitalization. JACC Heart Fail. 2020;8(1):25–34. doi: 10.1016/j.jchf.2019.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Unlu O, Levitan EB, Reshetnyak E, et al. Polypharmacy in Older Adults Hospitalized for Heart Failure. Circ Heart Fail. 2020;13(11):e006977. doi: 10.1161/CIRCHEARTFAILURE.120.006977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herzig SJ, Rothberg MB, Guess JR, et al. Antipsychotic Use in Hospitalized Adults: Rates, Indications, and Predictors. J Am Geriatr Soc. 2016;64(2):299–305. doi: 10.1111/jgs.13943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loh KP, Ramdass S, Garb JL, et al. From hospital to community: use of antipsychotics in hospitalized elders. J Hosp Med. 2014;9(12):802–4. doi: 10.1002/jhm.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herzig SJ, Rothberg MB, Guess JR, et al. Antipsychotic medication utilization in nonpsychiatric hospitalizations. J Hosp Med. 2016;11(8):543–9. doi: 10.1002/jhm.2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician. 2010;81(5):617–22. [PubMed] [Google Scholar]
- 15.Salvo F, Pariente A, Shakir S, et al. Sudden cardiac and sudden unexpected death related to antipsychotics: A meta-analysis of observational studies. Clin Pharmacol Ther. 2016;99(3):306–14. doi: 10.1002/cpt.250. [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Xu J, Fang K, et al. Current antipsychotic agent use and risk of venous thromboembolism and pulmonary embolism: a systematic review and meta-analysis of observational studies. Ther Adv Psychopharmacol. 2021;11:2045125320982720. doi: 10.1177/2045125320982720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zivkovic S, Koh CH, Kaza N, et al. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):189. doi: 10.1186/s12888-019-2177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gareri P, De Fazio P, Manfredi VG, et al. Use and safety of antipsychotics in behavioral disorders in elderly people with dementia. J Clin Psychopharmacol. 2014;34(1):109–23. doi: 10.1097/JCP.0b013e3182a6096e. [DOI] [PubMed] [Google Scholar]
- 19.Basciotta M, Zhou W, Ngo L, et al. Antipsychotics and the Risk of Mortality or Cardiopulmonary Arrest in Hospitalized Adults. J Am Geriatr Soc. 2020;68(3):544–50. doi: 10.1111/jgs.16246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Food and Drug Administration. FDA Issues Public Health Advisory for Antipsychotic Drugs used for Treatment of Behavioral Disorders in Elderly Patients. Available at: http://psychrights.org/drugs/ANS01350.html. Accessed March 2, 2021.
- 21.FDANews. FDA Expands Mortality Warnings on Antipsychotic Drugs. Available at: https://www.fdanews.com/articles/107752-fda-expands-mortality-warnings-on-antipsychotic-drugs. Accessed March 2, 2021.
- 22.Flaherty JH, Gonzales JP, Dong B. Antipsychotics in the treatment of delirium in older hospitalized adults: a systematic review. J Am Geriatr Soc. 2011;59(Suppl 2):S269–76. doi: 10.1111/j.1532-5415.2011.03675.x. [DOI] [PubMed] [Google Scholar]
- 23.Nikooie R, Neufeld KJ, Oh ES, et al. Antipsychotics for Treating Delirium in Hospitalized Adults: A Systematic Review. Ann Intern Med. 2019;171(7):485–95. doi: 10.7326/M19-1860. [DOI] [PubMed] [Google Scholar]
- 24.Oh ES, Needham DM, Nikooie R, et al. Antipsychotics for Preventing Delirium in Hospitalized Adults: A Systematic Review. Ann Intern Med. 2019;171(7):474–84. doi: 10.7326/M19-1859. [DOI] [PubMed] [Google Scholar]
- 25.Tampi RR, Tampi DJ, Balachandran S, et al. Antipsychotic use in dementia: a systematic review of benefits and risks from meta-analyses. Ther Adv Chronic Dis. 2016;7(5):229–45. doi: 10.1177/2040622316658463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morandi A, Vasilevskis E, Pandharipande PP, et al. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61(7):1128–34. doi: 10.1111/jgs.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marshall J, Herzig SJ, Howell MD, et al. Antipsychotic utilization in the intensive care unit and in transitions of care. J Crit Care. 2016;33:119–24. doi: 10.1016/j.jcrc.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tomichek JE, Stollings JL, Pandharipande PP, et al. Antipsychotic prescribing patterns during and after critical illness: a prospective cohort study. Crit Care. 2016;20(1):378. doi: 10.1186/s13054-016-1557-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson KG, Fashoyin A, Madden-Fuentes R, et al. Discharge Plans for Geriatric Inpatients with Delirium: A Plan to Stop Antipsychotics? J Am Geriatr Soc. 2017;65(10):2278–81. doi: 10.1111/jgs.15026. [DOI] [PubMed] [Google Scholar]
- 30.Flurie RW, Gonzales JP, Tata AL, et al. Hospital delirium treatment: Continuation of antipsychotic therapy from the intensive care unit to discharge. Am J Health Syst Pharm. 2015;72(23 Suppl 3):S133–9. doi: 10.2146/ajhp150474. [DOI] [PubMed] [Google Scholar]
- 31.Corbett CF, Setter SM, Daratha KB, et al. Nurse identified hospital to home medication discrepancies: implications for improving transitional care. Geriatr Nurs. 2010;31(3):188–96. doi: 10.1016/j.gerinurse.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 32.King BJ, Gilmore-Bykovskyi AL, Roiland RA, et al. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc. 2013;61(7):1095–102. doi: 10.1111/jgs.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Medicare and Medicaid Services. Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual. Accessed March 2, 2021.
- 34.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Thomas KS, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function Scale. Med Care. 2017;55(9):e68–e72. doi: 10.1097/MLR.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54(11):M546–53. doi: 10.1093/gerona/54.11.M546. [DOI] [PubMed] [Google Scholar]
- 37.U.S. Food and Drug Administration. Information on Conventional Antipsychotics. Available at: https://wayback.archive-it.org/7993/20170722033234/https:/www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm107211.htm. Accessed March 2, 2021.
- 38.U.S. Food and Drug Administration. Atypical Antipsychotic Drugs Information. Available at: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/atypical-antipsychotic-drugs-information. Accessed March 2, 2021.
- 39.Centers for Medicare and Medicaid Services. National Partnership to Improve Dementia Care in Nursing Homes; Interim Changes to Appendix P State Operations Manual (SOM). Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/SC-Letter-13-35-Advanced-Copy.pdf. Accessed March 2, 2021.
- 40.Sullivan GM, Feinn R. Using Effect Size-or Why the P Value Is Not Enough. J Grad Med Educ. 2012;4(3):279–82. doi: 10.4300/JGME-D-12-00156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pariente A., Fourrier-Réglat A., Ducruet T., et al. Antipsychotic use and myocardial infarction in older patients with treated dementia. Arch Intern Med. 2012;172(8):648-53; discussion 54-5. [DOI] [PubMed]
- 42.Brauer R, Smeeth L, Anaya-Izquierdo K, et al. Antipsychotic drugs and risks of myocardial infarction: a self-controlled case series study. Eur Heart J. 2015;36(16):984–92. doi: 10.1093/eurheartj/ehu263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu C. S., Tsai Y. T., Tsai H. J. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Assoc. 2015;4(2). [DOI] [PMC free article] [PubMed]
- 44.Straus SM, Bleumink GS, Dieleman JP, et al. Antipsychotics and the risk of sudden cardiac death. Arch Intern Med. 2004;164(12):1293–7. doi: 10.1001/archinte.164.12.1293. [DOI] [PubMed] [Google Scholar]
- 45.Loh KP, Ramdass S, Garb JL, et al. Long-term outcomes of elders discharged on antipsychotics. J Hosp Med. 2016;11(8):550–5. doi: 10.1002/jhm.2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stock KJ, Amuah JE, Lapane KL, et al. Prevalence of, and Resident and Facility Characteristics Associated With Antipsychotic Use in Assisted Living vs. Long-Term Care Facilities: A Cross-Sectional Analysis from Alberta, Canada. Drugs Aging. 2017;34(1):39–53. doi: 10.1007/s40266-016-0411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Levinson D. Medicare atypical antipsychotic drug claims for elderly nursing home residents. Department of Health and Human Services Office of Inspector General; 2011.
- 48.Zhang Y, Letuchy EM, Carnahan RM. Where Are Antipsychotics Prescribed in Nursing Homes Initiated? J Am Geriatr Soc. 2018;66(6):1082–8. doi: 10.1111/jgs.15223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Targum S. D. Treating Psychotic Symptoms in Elderly Patients. Prim Care Companion. J Clin Psychiatry. 2001;3(4):156-63. [DOI] [PMC free article] [PubMed]
- 50.Reus VI, Fochtmann LJ, Eyler AE, et al. The American Psychiatric Association Practice Guideline on the Use of Antipsychotics to Treat Agitation or Psychosis in Patients With Dementia. Am J Psychiatry. 2016;173(5):543–6. doi: 10.1176/appi.ajp.2015.173501. [DOI] [PubMed] [Google Scholar]
- 51.Thom RP, Levy-Carrick NC, Bui M, et al. Delirium. Am J Psychiatry. 2019;176(10):785–93. doi: 10.1176/appi.ajp.2018.18070893. [DOI] [PubMed] [Google Scholar]
- 52.Devlin JW, Skrobik Y, Gélinas C, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. 2018;46(9):e825–e73. doi: 10.1097/CCM.0000000000003299. [DOI] [PubMed] [Google Scholar]
- 53.CDC. Core Elements of Hospital Antibiotic Stewardship Programs. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. Available at: https://www.cdc.gov/antibiotic-use/core-elements/hospital.html.
- 54.D'Angelo RG, Rincavage M, Tata AL, et al. Impact of an Antipsychotic Discontinuation Bundle During Transitions of Care in Critically Ill Patients. J Intensive Care Med. 2019;34(1):40–7. doi: 10.1177/0885066616686741. [DOI] [PubMed] [Google Scholar]


