Abstract
Background
Prior research indicates that female physicians spend more time working in the electronic health record (EHR) than do male physicians.
Objective
To examine gender differences in EHR usage among primary care physicians and identify potential causes for those differences.
Design
Retrospective study of EHR usage by primary care physicians (PCPs) in an academic hospital system.
Participants
One hundred twenty-five primary care physicians
Interventions
N/A
Main Measures
EHR usage including time spent working and volume of staff messages and patient messages.
Key Results
After adjusting for panel size and appointment volume, female PCPs spend 20% more time (1.9 h/month) in the EHR inbasket and 22% more time (3.7 h/month) on notes than do their male colleagues (p values 0.02 and 0.04, respectively). Female PCPs receive 24% more staff messages (9.6 messages/month), and 26% more patient messages (51.5 messages/month) (p values 0.03 and 0.004, respectively). The differences in EHR time are not explained by the percentage of female patients in a PCP’s panel.
Conclusions
Female physicians spend more time working in their EHR inbaskets because both staff and patients make more requests of female PCPs. These differential EHR burdens may contribute to higher burnout rates in female PCPs.
KEY WORDS: Gender, Electronic health record, Burnout
INTRODUCTION
Recent data suggest that female physicians spend more time working in the electronic health record (EHR) than do male physicians.1–3 This increased EHR time may contribute to the documented higher rates of burnout among female physicians nationwide compared with their male colleagues.4 In particular, time spent in the EHR inbasket, within which physicians respond to messages from patients, staff, and colleagues, has been linked to burnout.5, 6
Prior research also has shown that female physicians spend more time with patients per in-person visit than do male physicians.7–10 Studies have shown that patients communicate differently toward female versus male physicians, for example disclosing more information to female physicians, and also expect different communication styles based on physician gender, for example expecting more empathic listening from female physicians.11–17 Additionally, the composition of patient panels varies between male and female physicians, with female physicians having substantially more female patients.18
With the rise of electronic health records, work outside of in-person visits has become an increasingly large share of time spent by primary care physicians (PCPs). One recent study found that PCPs now spend more time working in the electronic health record than they spend face-to-face with patients.19 PCPs have disproportionately more total and after-hours EHR time than do medical specialty or surgical specialty clinicians.20
The existing literature has not explored the causes of the additional time that female PCPs spend working in the EHR. Based on our clinical experience, we hypothesized that female PCPs receive more inbox communication than do their male colleagues. We therefore examine three reasons that female PCPs might spend more time working their inbasket: an increased workload composed of a higher volume of messages from staff and patients; an equivalent workload with lower efficiency in EHR usage; or a higher percentage of female patients, combined with more inbasket time per female patient than male patient.
In this paper, we use the terms “female” and “male” to describe physician and patient gender because those are the terms that have been used in the relevant literature.
METHODS
We performed a retrospective study of EHR usage by primary care physicians in the Brigham and Women’s Hospital system. We obtained 6 months of data, from June 2019 through November 2019. We excluded physicians who were not active in the EHR during at least two of the months of the study period. Only attending physicians were included. This produced an analysis sample of 125 physicians (76 female MDs and 49 male MDs).
The BWH Institutional Review Board judged this paper to meet criteria for quality improvement/quality assessment project and thus did not require IRB approval.
The primary data come from Epic Systems records of EHR use. Specific measures include total time spent by physicians in Epic, defined as the number of minutes the provider was logged into the system; time spent in the inbasket; time spent in notes; time spent in clinical review; time spent in orders; turnaround time, defined as number of days a provider took to mark a message as done, and the physicians’ number of appointments each month.21 Within the inbasket category, we separately analyze patient messages (composed of patient calls, in which a patient telephones the office and an Epic message is then routed, and patient advice requests, in which a patient sends a message through the electronic portal) and staff messages, in which a staff member initiates a message to the physician. Epic stops measuring time working after 5 s of inactivity.22 To the extent that a physician pauses for longer than 5 s, this portion of potential working time would not be captured in our data.
We matched the Epic data to Brigham and Women’s primary care administrative data containing physician demographics: gender, panel size, clinical workload (clinical FTE), and panel gender composition. We determined physician gender through the BWH physician database; only male and female gender responses appear in this database. A few primary care physicians had panel sizes and number of appointments per month that were extremely different from the typical numbers for their FTE. Therefore, to reduce the impact of outliers, we Winsorized (top coded) the number of monthly appointments per FTE and the panel size per FTE at 800 and 4000, respectively. Similarly, to reduce the impact of outliers, we Winsorized the turnaround time to staff and patient messages at 14 days.
Statistical Methods
We compared male and female physicians with respect to their EHR usage using both simple comparisons of means as well as multivariate linear regression models. The regression models adjust for panel size and appointments per month so as to allow us to distinguish between gender differences in EHR workload that result from differences in patient volume and ones that result from other factors. By separately including panel size and appointments per month in our model, we are also capturing a portion of patient complexity (i.e., more complex patients will need to be seen more frequently). We estimated the regression models and tested for differences in means using the xtreg command in Stata/MP Version 17.0. To account for within-physician correlation, all tests used robust standard errors clustered by MD. Statistical significance was assessed at the 0.05 level.
Role of the Funding Source
The study received funding from the Brigham Care Redesign Incubator and Startup Program (BCRISP), Brigham and Women’s Hospital. The funders had no role in study design; data collection, analysis, and interpretation; writing of the report; or in the decision to submit for publication.
RESULTS
Our study population included 125 Brigham Health primary care physicians. Of the 125 physicians, 76 (61%) were women (see Table 1). Physicians in our sample worked an average of 0.55 clinical FTEs (female MDs 0.57, male MDs 0.52, p=0.34 on male-female difference); thus, volume measures in this paper can be converted to clinical FTE equivalents by multiplying by approximately 1.8. Female and male physicians had similar workload characteristics including average clinical FTE, panel size, and panel size per FTE, and both appointments per month and appointments per FTE (p>0.05 on male-female differences).
Table 1.
Workload and Panel Characteristics of Brigham Health Primary Care Physicians
| Female MDs (n=76) | Male MDs (n=49) | p value of female-male difference | |
|---|---|---|---|
| Clinical FTE (mean) | 0.57 | 0.52 | p=0.34 |
| Patient panel size (mean) | 953 | 940 | p=0.89 |
| Appointments per month (mean) | 114 | 112 | p=0.79 |
| Appointments per month per FTE (mean)1 | 215 | 233 | p=0.31 |
| Patient panel size per clinical FTE (mean)2 | 1778 | 1876 | p=0.39 |
| Patient panel percent female | 78.1 | 38.7 | p=0.00 |
1Winsorized above 800
2Winsorized above 4000
We examined time spent in EHR activities by physician gender (Table 2). Total EHR usage by female PCPs was 13% higher than by male PCPs, but this difference was not statistically significant (58.9 h per month vs. 52.1 h, p-value on regression-adjusted difference =0.08).
Table 2.
Differences in Time in Epic Activities per Month (in Hours) by Physician Gender
| Activity | Mean (SD) Monthly hours Female MDs |
Mean (SD) Monthly hours Male MDs |
Difference1 | Percent difference | Regression adjusted difference1, 2 | ||
|---|---|---|---|---|---|---|---|
| Value (95% CI) | p-value | Value (95% CI) | p-value | ||||
| Total Epic | 58.9 (31.1) | 52.1 (31.7) | 6.8 (−3.6 to 17.1) | 0.20 | 13% | 6.7 (−0.8 to 14.1) | 0.08 |
| In-basket | 10.7 (5.9) | 8.9 (6.1) | 1.9 (−0.2 to 3.9 ) | 0.07 | 20% | 1.9 (0.3 to 3.4) | 0.02 |
| Notes | 20.3 (13.5) | 16.6 (11.5) | 3.7 (−0.3 to 7.8) | 0.07 | 22% | 3.6 (0.1 to 7.1) | 0.04 |
| Clinical review | 9.8 (6.6) | 8.8 (6.2) | 1.0 (−1.1 to 3.2) | 0.35 | 11% | 1.1 (−0.7 to 2.9) | 0.25 |
| Orders | 8.0 (5.0) | 8.5 (6.1) | −0.5 (−2.4 to 1.5) | 0.64 | −6% | −0.5 (−2.0 to 1.0) | 0.50 |
1Robust standard errors clustered by MD
2Adjusted for appointments per month and panel size
Total EHR time was disaggregated into its components to determine which activities might show gender differences (Table 2). Female PCPs in our sample spent 20% more time performing work in their inbaskets (10.7 h vs. 8.9 h, p-value on regression-adjusted difference =0.02) and 22% more time working on notes (20.3 h vs. 16.6 h, p-value on regression-adjusted difference =0.04) than the male PCPs. We also examined time in clinical review and orders, two components of EHR usage that are less likely to be affected by gender differences in practice style or by staff and patient expectations. In contrast to inbasket and notes, there were no statistically significant differences by gender in time spent on clinical review or orders (p=0.25 and p=0.50, respectively).
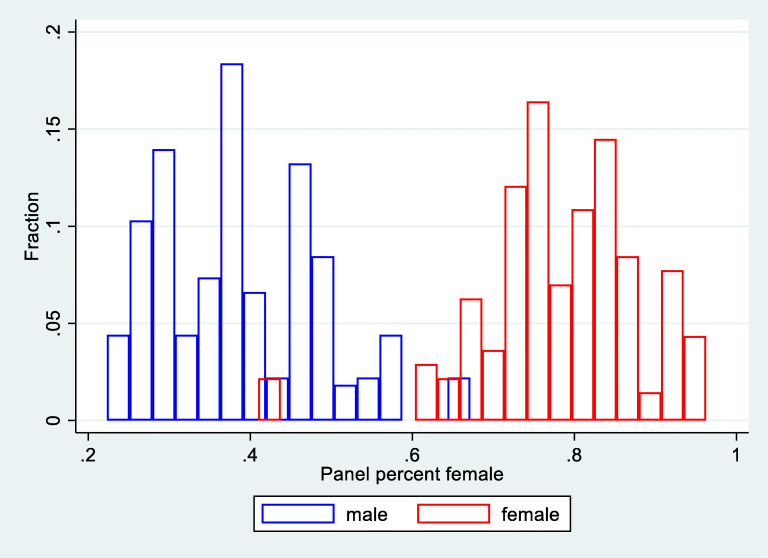
In our sample, female PCPs have much higher percentages of female patients than do male PCPs: the mean percentage of female patients was 78% for female PCPs and 39% for male PCPs (Table 1). There is minimal overlap between the patient panel gender percentages of female and male physicians (Fig. 1).
Figure 1.
Fraction of patient panel that is female by physician gender.
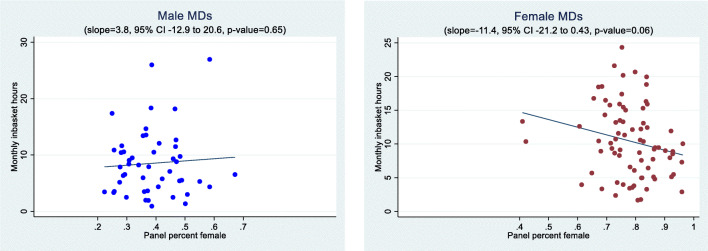
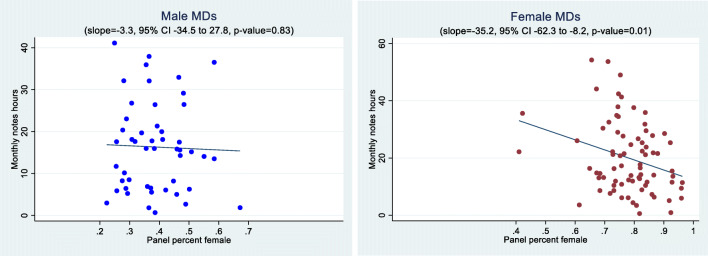
Figures 2 and 3, along with the associated regression results presented in the figure notes, show the relationship between the proportion of female patients in the physician’s case mix and time spent in the inbasket and notes. For male PCPs, there is essentially no relationship between time in the two activity categories and female percentage of panel (slope=3.5, 95% CI −15.2 to 22.2, p-value=.72 for inbasket; slope=−3.4, 95% CI −37.6 to 30.8, p-value=.85 for notes). For female PCPs, there is a decrease in time for both categories as the female patient percentage increases (slope=−12.4, 95% CI −21.5 to −3.3, p-value=.01 for inbasket; slope=−32.6, 95% CI −57.9 to −7.3, p-value=.01 for notes).
Figure 2.
Time spent in inbasket by physician gender and the percentage of female patients in the panel. Note: Figure shows one data point per physician where the monthly observations have been collapsed to the physician level by taking the mean of the monthly observations. The regression lines are estimated on the collapsed data. The comparable slopes and p-values for a regression of inbasket time on panel percent female using the individual monthly observations are 3.5 (95% CI −15.2 to 22.2, p-value=.72) for male MDs and −12.4 (95% CI −21.5 to −3.3, p-value =0.01) for female MDs.
Figure 3.
Time spent in notes per month by patient gender. Note: Figure shows one data point per physician where the monthly observations have been collapsed to the physician level by taking the mean of the monthly observations. The regression lines are estimated on the collapsed data. The comparable slopes and p-values for a linear regression of monthly notes hours on panel percent female using the individual monthly observations are −3.4 (95% CI −37.6 to 30.8, p-value=.85) for male MDs and −32.6 (95% CI −57.9 to −7.3, p-value =0.01) for female MDs.
To evaluate inbasket workload, we measured the numbers of staff messages and patient messages received by PCPs. Table 3 shows that female physicians received 24% more staff messages per month than did male physicians (51.0 messages vs 41.2 messages, p-value on regression-adjusted difference =0.03), and 26% more patient messages per month (259.9 messages vs. 206.5 messages, p-value on regression-adjusted difference =0.004).
Table 3.
Differences in Staff and Patient Messages Received per Month by Physician Gender
| Activity | Mean (SD) Monthly count Female MDs |
Mean (SD) Monthly count Male MDs |
Difference1 | Percent difference | Regression adjusted difference1, 2 | ||
|---|---|---|---|---|---|---|---|
| Value (95% CI) | p-value | Value (95% CI) | p-value | ||||
| Staff messages | 51.0 (33.2) | 41.2 (26.5) | 9.9 (0.4 to 19.3) | 0.04 | 24% | 9.6 (1.1 to 18.2) | 0.03 |
| Patient messages | 259.9 (142.7) | 206.5 (161.9) | 53.4 (0.0 to 106.8 ) | 0.05 | 26% | 51.5 (16.3 to 86.6) | 0.004 |
1Robust standard errors clustered by MD
2Adjusted for appointments per month and panel size
To explore whether the additional inbasket workload for female PCPs had a negative impact on patient care, we analyzed the time between the physician’s receipt of staff and patient messages and the physician’s response (turnaround time). We found no significant differences in turnaround time between female and male physicians for staff messages or patient messages (3.8 days vs 4.3 days, p=0.40, and 4.0 vs 4.9 days, p=.27, Table 4).
Table 4.
Differences in Turnaround Time to Respond, in Days, by Physician Gender
| Activity | Mean (SD) Turnaround time Female MDs |
Mean (SD) Turnaround time Male MDs |
Difference1 | Percent difference | Regression adjusted difference1, 2 | ||
|---|---|---|---|---|---|---|---|
| Value (95% CI) | p-value | Value (95% CI) | p-value | ||||
| Staff messages* | 3.8 (4.1) | 4.3 (5.0) | −0.5 (−1.8 to 0.7) | 0.40 | −12% | −0.5 (−1.8 to 0.7) | 0.40 |
| Patient messages* | 4.0 (4.2) | 4.9 (6.2) | −1.0 (−2.7 to 0.7) | 0.27 | −19% | −1.0 (−2.7 to 0.7) | 0.26 |
*Winsorized above 14
1Robust standard errors clustered by MD
2Adjusted for appointments per month and panel size
We also explored the impact of EHR on work-life balance, examining time spent working in the EHR outside of typical work hours. There was a trend for female PCPs to spend more EHR time outside of scheduled hours than male PCPs but these differences were not statistically significant (Table 5).
Table 5.
Epic Time Outside Schedule per Month, in Hours, by Physician Gender
| Activity | Mean (SD) Hours Female MDs |
Mean (SD) Hours Male MDs |
Difference1 | Percent difference | Regression adjusted difference1, 2 | ||
|---|---|---|---|---|---|---|---|
| Value (95% CI) | p-value | Value (95% CI) | p-value | ||||
| Outside scheduled hours | 17.9 (14.1) | 14.2 (13.2) | 3.6 (−0.9 to 8.2) | 0.12 | 26% | 3.6 (−0.5 to 7.7) | 0.09 |
| Outside scheduled days | 11.0 (10.5) | 10.0 (9.9) | 1.0 (−2.5 to 4.4) | 0.58 | 10% | 1.0 (−2.4 to 4.5) | 0.56 |
| Outside 7am–7pm | 5.2 (6.4) | 4.2 (6.1) | 1.0 (−1.2 to 3.2) | 0.39 | 24% | 1.0 (−1.1 to 3.1) | 0.34 |
1Robust standard errors clustered by MD
2Adjusted for appointments per month and panel size
DISCUSSION
We found that female primary care physicians spend substantially more time in the EHR inbasket and notes than do their male colleagues, accounting for panel size and appointment volume. In their inbasket, they receive significantly more staff messages and patient messages. The gender difference in overall time spent in the EHR is consistent with the pattern for inbasket and notes, but does not reach statistical significance.
We undertook to distinguish among three possible explanations for increased female inbasket time: a higher workload for female PCPs in which staff and patients of all genders contact female physicians more frequently; female PCPs spend more time because they are less efficient; or a higher workload for female PCPs because their patient panels are disproportionately female, and female patients require more time.
Our data show that female PCPs receive significantly more messages both from their patients and their staff than do male PCPs (Table 3). This finding suggests gendered expectations of physician accessibility, leading to a lower threshold to contact a female physician than male physician. Such expectations are consistent with previous research showing that patients communicate differently towards female physicians than towards males: patients speak more, make more partnership statements, and disclose more medical information to female physicians than to male physicians.11–14 Previous literature also has demonstrated differences in patient expectations of physician communication style based on the physician gender, drawing on stereotypical gender norms.11, 15–17 Gendered expectations and practice styles may contribute to time pressure during visits and excess work hours, that in turn affect burnout rates.23 Our study demonstrates that these gendered patterns of communication with physicians appear within the EHR, in the volume of messages from both patients and staff. Despite increased message volume, we found that there were no significant differences in the time female physicians took to respond to patient or staff messages (Table 4).
Our data do not support the hypothesis that female physicians simply are slower at doing the equivalent work as their male colleagues. We found strong gender differences in Epic activities that would be most affected by patient and staff expectations, such as messages and phone calls. In contrast, Epic activities related to work tasks, such as orders and clinical review, showed no significant gender differences (Table 2). These findings agree with evidence from Gupta and colleagues who found that female physicians used more Epic documentation efficiency tools than did male physicians.1 Although we did not examine use of documentation efficiency tools in our population, if a similar pattern held it would suggest that if female physicians did not have this added efficiency, the time difference between male and female physicians would be even greater.
Finally, our data do not support the hypothesis that the increased EHR time for female PCPs is explained by the higher percentage of female patients in their panels. Previous research has found that female patients ask more questions and make more emotional statements than do male patients.24 Female patients might also have different psychosocial or medical complexity than male patients. Because panel patient gender composition tracks so closely with PCP gender (Table 1, Fig. 1), it is challenging to separate out the effects of patient and PCP gender. In order to explore whether differences in EHR time by physician gender could be explained by differences in the percentage of female patients in physician panels, we examined patterns of inbasket and notes time within female PCPs and within male PCPs. If each female patient required more physician time, then within male or female PCPs, one would expect to see higher inbasket and notes time as the percent of female patients increased. However, higher percentages of female patients in PCP panels did not correlate with increasing time in the inbasket or in notes for either female or male physicians. In fact, for female PCPs, there was a decrease in time spent as the female patient percentage increased (Figs. 2 and 3). This finding raises the possibility that the small group of male patients of female physicians have particularly time-consuming communication patterns.
In addition to increased inbasket time, we found that female physicians spent significantly more time in notes than did male physicians (Table 2). This finding is consistent with previous research showing a difference in note length by physician gender.1
Primary care physicians spend a large portion of their time engaged in work outside of the in-person office visit.25, 26 A 2017 study found that full-time PCPs spent 5.9 h of an 11.4-h workday in the EHR; of this EHR work, inbasket management accounted for 85 min.27 Inbasket time is particularly high for adult PCPs, who spend approximately twice as long on inbasket messages as do pediatricians.28
The clerical burden and time pressure associated with use of the EHR have been shown to contribute to physician burnout and intention to leave clinical practice.29, 30 In particular, one study found that receiving an above-average number of EHR system-generated inbasket messages was associated with increased probability of burnout and intent to reduce clinical work hours; interestingly, spending more time on EHR notes was not associated with these outcomes.31
The increased time that female primary care physicians spend working in the EHR inbasket and notes may contribute to their higher burnout rate. Studies have consistently found that the prevalence of burnout is higher among female physicians than male physicians by 20 to 60%. 4, 32 In a 2018 nationwide survey by Medscape of 15,543 physicians across 29 specialties, 48% of female physicians versus 38% of males reported burnout; likewise, burnout rates in primary care physicians are high, with 46% and 47% burnout rates among internists and family medicine physicians, respectively.33 At the Brigham and Women’s Hospital, female primary care physicians have a burnout rate of 57% versus 42% of male PCPs (unpublished communication, 2019). Understanding the causes of an increased EHR workload is therefore important in order to develop successful mitigation strategies for burnout in female physicians.
This study has implications for potential practical solutions to reducing gender differences in electronic health record time among PCPs. EHR usage data not only can contribute to predicting physician risk for distress, burnout, and intent to cut back or leave practice, but can also be used to inform potential solutions including expectations for patient-scheduled hours and appropriate support systems.34
Claytor and Grant propose that the solution lies in “training new physicians on optimal time management to empower them to balance manifold time constraints with minimal necessary documentation.”3 However, our study suggests that the increased time that female PCPs spend in the EHR is not due to over-documentation or lack of computer proficiency, but rather stems from the increased requests that patients and staff make of female PCPs. Additionally, this study suggests that providing compensation to physicians based on their percentage of female patients is likely an imperfect solution to the increased workload faced by female PCPs. Instead, developing support systems and team-based care to respond to inbox messages offers a potential avenue to mitigate burnout in female physicians.
This study has several limitations. First, it was conducted in a single academic medical center and may not reflect patterns among other types of primary care practices. Second, it included only EHR data without individual time/motion observation. EHR record logged actions may not exactly capture physician clinical activities.35 Third, it included only physician-level data and not patient-level data. In previous research, while female physicians reported similar numbers of medically complex patients, they reported greater numbers of psychosocially complex and frustrating patients.3 Patient-level data would enable further evaluation of whether patient complexity explains the gender differences in EHR care, and whether adjusting panel-size expectations for patient complexity would reduce gender differences in workload. Fourth, we used the hospital physician database to identify physician gender, which at the time of this study required respondents to categorize themselves as either male or female; therefore, we could not capture information on physicians who were transgender or nonbinary; similar limitations at the time applied to available patient gender (legal gender as listed in Epic).
In sum, we found that the increased time that female primary care physicians spend working in the EHR inbasket is due to the higher volume of staff messages and patient advice requests they receive. Our study did not directly measure burnout, which may be affected by the differences in EHR workload that we found. Future studies could directly test the relationship between patterns of inbasket use and physician burnout, as well as the impact of interventions to decrease inbasket message volume. Development of strategies to provide equitable support for female PCPs is needed in order to provide patient-centered care while decreasing the high rate of burnout among female PCPs.
FUNDING
Funded by a grant from the Brigham Care Redesign Incubator and Startup Program (BCRISP), Brigham and Women’s Hospital.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations: BCRISP Cohort 7 Final Presentations, November 5, 2020, Brigham and Women’s Hospital
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gupta K, Murray SF, Sarkar U, Mourad M, Adler-Milstein J. Differences in Ambulatory EHR Use Patterns for Male vs. Female Physicians. NEJM Catalyst. November 13, 2019. Available at: https://catalyst.nejm.org/ambulatory-ehrpatterns-physician-gender/. Accessed 30 Nov 2019.
- 2.Tait SD, Oshima SM, Ren Y, Fenn AE, Boazak M, Hinz E, Hwang ES. Sex-Based Differences Entangling with Electronic Health Record Documentation. JAMA Intern Med Published online 2020; 5036.
- 3.Claytor J, Grant RW. Sex-Based Differences Entangling with Electronic Health Record Documentation. JAMA Intern Med. Published online 2020. 10.1001/jamainternmed.2020.5008 [DOI] [PubMed]
- 4.McMurray JE, Linzer M, Shugerman R, Nelson K. The Work Lives of Women Physicians Results from the Physician Work Life Study; The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15(6):372–380. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akbar F, Mark G, Prausnitz S, et al. Physician Stress During Electronic Health Record Inbox Work: In Situ Measurement With Wearable Sensors. JMIR Med Inform. 2021;9(4):e24014. doi: 10.2196/24014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hilliard RW, Haskell J, Gardner RL. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc. 2020 Jul 1;27(9):1401-1410. 10.1093/jamia/ocaa092. PMID: 32719859; PMCID: PMC7647296. [DOI] [PMC free article] [PubMed]
- 7.Jefferson L, Bloor K, Birks Y, Hewitt C, Bland M. Effect of physicians’ gender on communication and consultation length: a systematic review and meta-analysis. J Health Serv Res Policy. 2013;13:242–248. doi: 10.1177/1355819613486465. [DOI] [PubMed] [Google Scholar]
- 8.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 9.Ganguli I, Sheridan B, Gray J, Chernew M, Rosenthal MB, Neprash H. Physician Work Hours and the Gender Pay Gap – Evidence from Primary Care. NEJM. 2020;383(14):1349–1357. doi: 10.1056/NEJMsa2013804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women Physicians: Gender and the Medical Workplace. J Womens Health. 2020;29(3):297–309. doi: 10.1089/jwh.2018.7290. [DOI] [PubMed] [Google Scholar]
- 11.Hall JA, Roter DL. Physician-patient communication. In Friedman HS, ed. The Oxford Handbook of Health Psychology. New York: Oxford University Press; 2011: 317-346.
- 12.Hall JA, Roter DL. Physician-patient communication. In: Friedman HS, editor. The Oxford handbook of health psychology. 2011. pp. 317–346. [Google Scholar]
- 13.Schmid Mast M, Hall JA, Roter DL. Disentangling physician sex and physician communication style: their effects on patient satisfaction in a virtual medical visit. Patient Educ Couns. 2007;68:16–22. doi: 10.1016/j.pec.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 14.Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Gender in medical encounters: An analysis of physician and patient communication in primary care setting. Health Psychol. 1994;13:384–392. doi: 10.1037/0278-6133.13.5.384. [DOI] [PubMed] [Google Scholar]
- 15.Kilminster S, Downes J, Gough B, Murdoch-Eaton D, Roberts T. Women in medicine—is there a problem? A literature review of the changing gender composition, structures and occupational cultures in medicine. Med Educ. 2007;41:39–49. doi: 10.1111/j.1365-2929.2006.02645.x. [DOI] [PubMed] [Google Scholar]
- 16.Mast MS, Kadji KK. How female and male physicians' communication is perceived differently. Patient Educ Couns. 2018 Sep;101(9):1697-1701. 10.1016/j.pec.2018.06.003. Epub 2018 Jun 7.PMID: 29903628 [DOI] [PubMed]
- 17.Hall JA, Gulbrandsen P, Dahl FA. Physician gender, physician patient-centered behavior, and patient satisfaction: a study in three practice settings within a hospital. Patient Educ Couns. 2014;95(3):313–8. doi: 10.1016/j.pec.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 18.Franks P, Bertakis KD. Physician gender, patient gender, and primary care. J Womens Health (Larchmt). 2003;12(1):73–80. doi: 10.1089/154099903321154167. [DOI] [PubMed] [Google Scholar]
- 19.Young RA, MD, Burge SK, Kumar KA, Wilson JM, Ortiz DF. A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era. Fam Med. 2018;50(2):91–99. doi: 10.22454/FamMed.2018.184803. [DOI] [PubMed] [Google Scholar]
- 20.Rotenstein LS, Holmgren AJ, Downing NL, Bates DW. Differences in Total and After-hours Electronic Health Record Time Across Ambulatory Specialties. JAMA Intern Med. 2021 Jun 1;181(6):863-865. 10.1001/jamainternmed.2021.0256. PMID: 33749732; PMCID: PMC7985815. [DOI] [PMC free article] [PubMed]
- 21.Epic Signal Metric Reference Guide. Epic Systems Corporation 2021. Available at: https://signal.epic.com/Documentation/MetricReference. Accessed 19 Aug 2021.
- 22.Epic Signal Frequently Asked Questions (FAQs). Epic Signal Corporation 2021. Available at: https://galaxy.epic.com/?#Browse/page=1!68!483!3933199,100067954&. Accessed 19 Aug 2021.
- 23.Linzer M, Harwood E. Gendered expectations: Do they contribute to high burnout among female physicians? J Gen Intern Med. 2018;33(6):963–965. doi: 10.1007/s11606-018-4330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hall JA, Roter DL. Patient gender and communication with physicians: results of a community-based study. Womens Health. 1995;1(1):77–95. [PubMed] [Google Scholar]
- 25.Doerr E, Galpin K, Jones-Taylor C, Anander S, Demosthenes C, Platt S, Ponkshe S. Between-visit workload in primary care. J Gen Intern Med. 2010;25(12):1289–1292. doi: 10.1007/s11606-010-1470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dyrbye LN, West CP, Burriss TC, Shanafelt TD. Providing Primary Care in the United States: The Work No One Sees. Arch Intern Med. 2012;172(18):1420–1421. doi: 10.1001/archinternmed.2012.3166. [DOI] [PubMed] [Google Scholar]
- 27.Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W, Sinsky CA, Gilchrist VJ. Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Ann Fam Med. 2017;15(5):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rotenstein LS, Holmgren AJ, Downing NL, Longhurst CA, Bates DW. Differences in Clinician Electronic Health Record Use Across Adult and Pediatric Primary Care Specialties. JAMA Netw Open. 2021;4(7):e2116375. doi: 10.1001/jamanetworkopen.2021.16375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shanafelt TD, Dyrbye LN, Sinsky C, Hasan O, Satele D, Sloan J, West CP. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91(7):836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100–6. doi: 10.1136/amiajnl-2013-001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ Well-Being Linked to In-Basket Messages Generated By Algorithms in Electronic Health Records. Health Affairs 2019; 38(7): 10.1377/hlthaff.2018.05509 [DOI] [PubMed]
- 32.Templeton KC, Bernstein C, Sukhera J, et al. Gender-based differences in burnout: Issues faced by women physicians. 2019. NAM Perspectives. Discussion Paper, Nat Acad Med, Washington DC. 10.31478/201905a
- 33.Peckah C. Medscape national physician burnout and depression report. January 17, 2018. Available at https://www.medscape.com/slideshow/2018-lifestyle-burnoutdepression-6009235. Accessed 3 Apr 2020.
- 34.Sinsky CA, Rule A, Cohen G, et al. Metrics for assessing physician activity using electronic health record log data. J Am Med Inform Assoc. 2020;27(4):639–643. doi: 10.1093/jamia/ocz223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rule A, Chiang MF, Hribar MR. Using electronic health record audit logs to study clinical activity: a systematic review of aims, measures, and methods. J Am Med Inform Assoc. 2020;27(3):480–490. doi: 10.1093/jamia/ocz196. [DOI] [PMC free article] [PubMed] [Google Scholar]