BACKGROUND
Glucagon-like-peptide-1 receptor agonists (GLP1as) and sodium-glucose cotransporter-2 inhibitors (SGLT2is) offer advantages over older anti-diabetic agents, including increased survival among patients with comorbid cardiac or renal disease.1, 2 Among privately insured adults, Black individuals are less likely to receive SGLT2is and GLP1as.3, 4 However, about half of Black (and Hispanic) patients have public or no coverage. Moreover, it is unclear if racial inequities exist in the use of other diabetes medications.
OBJECTIVE
To assess racial inequities in the receipt of diabetes medications in a nationally representative sample.
METHODS
We analyzed data on filled prescriptions from the 2010–2019 Medical Expenditure Survey (MEPS).5 We included individuals filling prescriptions for insulin/insulin syringes, metformin, sulfonylureas, DPP4is, GLP1as, and/or SGLT2is. Other diabetes medications were excluded due to insufficient sample sizes (n<10 total unweighted prescriptions). Race/ethnicity is self-reported in the MEPS.
We tabulated the percentage of individuals receiving a medication in each medication class and calculated unadjusted Black:White and Hispanic:White odds ratios (ORs) using logistic regression, as well as ORs adjusted for age, sex, family income (as % of the federal poverty level), educational attainment (for persons ≥25 years old), health insurance, and a modified version of the Charlson Comorbidity Index (CCI) which excluded diabetes, heart disease, and cerebral vascular disease to minimize co-linearity. For years 2014–2019 (the period for which SGLT2is were FDA approved), we repeated these analyses among persons with self-reported or International Classification of Disease (ICD)–coded heart disease or chronic kidney disease, groups known to derive mortality benefit from SGLT2is and GLP1as.
Analyses used Stata version 16.1 (Stata-Corp) procedures that account for the surveys’ complex sampling design and MEPS-provided weights to generate national estimates. The Cambridge Health Alliance institutional review board exempted this study from review.
RESULTS
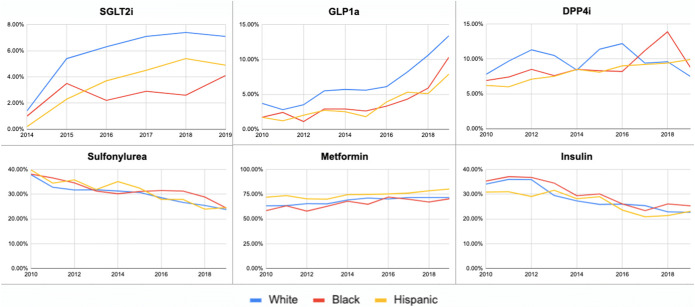
Our sample included 22,894 respondents. In unadjusted analyses, Black individuals had lower odds of receiving SGLT2is (OR, 0.45 [95% CI 0.32 to 0.65]) and GLP1as (OR, 0.58 [95% CI, 0.43 to 0.78]), as did Hispanic individuals (SGLT2i OR, 0.61 [95% CI, 0.43 to 0.86]; GLP1a, OR, 0.52 [95% CI, 0.39 to 0.69]) (Table). Among persons with cardiac/renal disease (n=4,569), Black:White inequities in SGLT2i use were larger than those in the overall sample (unadjusted OR, 0.33 [95% CI, 0.18 to 0.62]). Results were similar among individuals with self-reported or ICD10-diagnosed diabetes (data not shown), and changed little over time (Fig. 1). Compared to White patients, Black and Hispanic patients had slightly greater odds of receiving Sulfonylureas, though results were not statistically significant (Table 1).
Figure 1.
Time trends in the receipt of diabetes medications, 2010–2019. Note: the figure displays the percent of persons receiving a specific medication among all individuals who received any of the medications that year. SGLT2i timeline begins in 2014, the first year of FDA approval.
Table 1.
Black:White and Hispanic:White Differences in the Receipt of Diabetes Medications, 2014–2019
| SGLT2i | GLP1a | DPP4i | |||||||||
| OR | 95% CI | 95%CI | Or | 95% CI | |||||||
| All patients | Unadjusted | Black Hispanic | 0.45 | 0.32 | 0.65 | 0.58 | 0.43 | 0.78 | 1.01 | 0.81 | 1.25 |
| 0.61 | 0.43 | 0.86 | 0.52 | 0.39 | 0.69 | 0.92 | 0.74 | 1.15 | |||
| Adjusted* | Black Hispanic | 0.50 | 0.35 | 0.71 | 0.61 | 0.45 | 0.83 | 1.07 | 0.85 | 1.34 | |
| 0.66 | 0.46 | 0.96 | 0.59 | 0.44 | 0.80 | 0.91 | 0.73 | 1.15 | |||
| Reported cardiac or renal disease | Unadjusted | Black Hispanic | 0.33 | 0.18 | 0.62 | 0.64 | 0.43 | 0.94 | 0.70 | 0.48 | 0.99 |
| 0.78 | 0.39 | 1.57 | 0.62 | 0.35 | 1.11 | 0.79 | 0.54 | 1.15 | |||
| Adjusted* | Black Hispanic | 0.36 | 0.19 | 0.68 | 0.64 | 0.43 | 0.96 | 0.74 | 0.51 | 1.08 | |
| 0.80 | 0.38 | 1.69 | 0.67 | 0.37 | 1.20 | 0.81 | 0.56 | 1.19 | |||
| Sulfonylurea | Metformin | Insulin | |||||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | ||||||
| All patients | Unadjusted | Black Hispanic | 1.09 | 0.94 | 1.27 | 0.90 | 0.78 | 1.04 | 1.09 | 0.95 | 1.25 |
| 1.04 | 0.89 | 1.21 | 1.35 | 1.18 | 154 | 0.96 | 0.83 | 1.11 | |||
| Adjusted* | Black Hispanic | 1.15 | 0.99 | 1.34 | 0.88 | 0.76 | 1.02 | 1.02 | 0.89 | 1.18 | |
| 1.10 | 0.93 | 1.30 | 1.37 | 1.18 | 1.59 | 0.90 | 0.77 | 1.06 | |||
| Reported cardiac or renal disease | Unadjusted | Black Hispanic | 0.87 | 0.67 | 1.14 | 0.74 | 0.59 | 0.91 | 1.31 | 1.06 | 1.62 |
| 0.74 | 0.56 | 0.97 | 1.11 | 0.86 | 1.44 | 1.35 | 1.06 | 1.70 | |||
| Adjusted* | Black Hispanic | 0.99 | 0.75 | 1.31 | 0.72 | 0.58 | 0.90 | 1.17 | 0.95 | 1.45 | |
| 0.82 | 0.61 | 1.11 | 1.15 | 0.87 | 152 | 1.18 | 0.92 | 1.52 | |||
Source: authors’ analysis of data from the Medical Expenditure Panel Survey 2014–2019
OR, Black:White or Hispanic:White odds ratio
*Adjusted for age (continuous), sex (male, female), insurance (private, Medicaid, any Medicare, other public [including VA], other, uninsured), education (less than high school, high school, college +), income (as a percentage of the federal poverty level) and modified Charlson Comorbidity Index (0 conditions, 1 condition, 2+ conditions, excluding diabetes, cerebral vascular disease, heart disease)
All patients = all individuals receiving one or more of the studied medications.
Reported cardiac or renal disease = subgroup of patients with cardiac or renal disease by self-report or ICD9/10 diagnosis
Inequities persisted after adjustment for age, sex, insurance, education, CCI, and income. Black and Hispanic individuals had a lower odds of receiving SGLT2is (Black:White OR, 0.50 [95% CI 0.35 to 0.71]; Hispanic:White OR 0.66 [95% CI 0.46 to 0.96]) and GLP1as (Black:White OR, 0.61 [95% CI 0.45 to 0.83]; Hispanic:White OR, 0.59 [95% CI 0.44 to 0.80]).
DISCUSSION
Black and Hispanic individuals are less likely to receive SGLT2is and GLP1as, newer medications with significant benefits.1, 2 The population-wide racial/ethnic inequities we found are larger than differences previously documented in analyses limited to privately insured persons,3, 4 suggesting that unequal coverage exacerbates racial inequities.
The persistence of inequities in the adjusted models implicates structural racism as a cause of the racial/ethnic inequalities we observed6, 7 Black and Hispanic individuals with diabetes face many obstacles to care, including difficulty accessing physicians,3, 8 high out-of-pocket costs for medications,9 underfunded healthcare institutions,10 interpersonal racism,11 transportation challenges,12 and difficulty taking time off work for healthcare appointments.13 These barriers, and others, reflect racist laws and practices ingrained in the healthcare system and in society at large.
Our study has limitations. Self- or clinician-reported diagnoses understate disease prevalence among people of color.14 While we control for broad categories of insurance, we could not control for differences in cost-sharing (e.g., deductible size). Sample size constraints precluded analyses of other racial/ethnic groups. We were unable to distinguish between type 1 and type 2 diabetes; we lacked clinical metrics (e.g., GFR) that might contraindicate the use of some medications; and some individuals may be receiving the medications for conditions other than diabetes.
Our findings highlight the urgency of antiracist policy reforms that could assure all Americans equitable access to evidence-based treatment for diabetes.
Declarations
Conflicts of Interest
Dr. Christopher Cai was formerly a paid health policy fellow in the office of US Representative Pramila Jayapal and a paid research intern for Physicians for a National Health Program (PNHP), which advocates for single payer national health insurance. Drs. Woolhandler and Himmelstein founded PNHP and served as unpaid advisors to Bernie Sanders’ presidential campaigns. Dr. Jessica Himmelstein receives funding support from an Institutional National Research Service Award from a T32HP32715. No other disclosures were reported.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021;384(2):129–39. doi: 10.1056/NEJMoa2030186. [DOI] [PubMed] [Google Scholar]
- 2.Frías JP, Davies MJ, Rosenstock J, Pérez Manghi FC, Fernández Landó L, Bergman BK, et al. Tirzepatide versus Semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503–15. doi: 10.1056/NEJMoa2107519. [DOI] [PubMed] [Google Scholar]
- 3.Eberly LA, Yang L, Eneanya ND, Essien U, Julien H, Nathan AS, et al. Association of race/ethnicity, gender, and socioeconomic status with Sodium-Glucose Cotransporter 2 Inhibitor use among patients with diabetes in the US. JAMA Netw Open. 2021;4(4):e216139. doi: 10.1001/jamanetworkopen.2021.6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eberly, L. A., Yang, L., Essien, U. R., Eneanya, N. D., Julien, H. M., Luo, J., ... & Adusumalli, S. (2021, December). Racial, ethnic, and socioeconomic inequities in Glucagon-Like Peptide-1 Receptor agonist use among patients with diabetes in the US. In JAMA Health Forum (Vol. 2, No. 12, pp. e214182-e214182). American Medical Association. [DOI] [PMC free article] [PubMed]
- 5.Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: A National information resource to support healthcare cost research and inform policy and practice. Medical Care. 2009;47(Supplement):S44–50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 6.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–63. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 7.Boyd R, Lindo E, Weeks L, McLemore M. On Racism: A new standard for publishing on racial health inequities [Internet]. Health Affairs Blog. 2020. Available from: https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/
- 8.Cai C, Gaffney A, McGregor A, Woolhandler S, Himmelstein DU, McCormick D, Dickman SL. Racial and ethnic disparities in outpatient visit rates across 29 specialties. JAMA Intern Med. 2021;181(11):1525–1527. doi: 10.1001/jamainternmed.2021.3771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kang H, Lobo JM, Kim S, Sohn M-W. Cost-related medication non-adherence among U.S. adults with diabetes. Diabetes Res Clin Pract. 2018;143:24–33. doi: 10.1016/j.diabres.2018.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Himmelstein G, Himmelstein KEW. Inequality set in concrete: physical resources available for care at hospitals serving people of color and other U.S. hospitals. Int J Health Serv. 2020;50(4):363–70. doi: 10.1177/0020731420937632. [DOI] [PubMed] [Google Scholar]
- 11.Powell W, Richmond J, Mohottige D, Yen I, Joslyn A, Corbie-Smith G. Medical mistrust, racism, and delays in preventive health screening among African-American men. Behav Med. 2019;45(2):102–17. doi: 10.1080/08964289.2019.1585327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolfe MK, McDonald NC, Holmes GM. Transportation barriers to health care in the United States: findings from the National Health Interview Survey, 1997–2017. Am J Public Health. 2020;110(6):815–22. doi: 10.2105/AJPH.2020.305579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paid sick days access and usage rates vary by race/ethnicity, occupation, and earnings [Internet]. Institution for Women’s Policy Research; 2016 Feb. Available from: https://iwpr.org/wp-content/uploads/2020/08/B356-paid-sick-days.pdf
- 14.Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, et al. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. 2019;322(24):2389. doi: 10.1001/jama.2019.19365. [DOI] [PMC free article] [PubMed] [Google Scholar]