Abstract
Introduction
The B.1.1.529 (Omicron) variant of SARS-CoV-2 is the most antigenically unique SARS-CoV-2 variant of concern to date, which is currently widespread across the world. Omicron variant and its sublineages contain a plethora of mutations than other variants of concern, which increases their transmissibility and virulence. Concerns regarding potential immunological evasion have been reignited by emerging subvariants of the Omicron variant. Determining the effectiveness of Omicron-induced immunity and whether it is cross-protective against other variants is a crucial aspect of the research.
Method
A systematic search of relevant articles until September 25, 2022, from databases such as PubMed, Scopus, Google Scholar, and ScienceDirect was done independently by two authors. A total of 11 articles discussing about immunological evasion of different Omicron subvariants were included in the study.
Results
Numerous studies have demonstrated that Omicron variant causes a restricted immune response after infection. Omicron infection boosts preexisting vaccine-induced immunity, but it may not be enough to establish widespread, cross-neutralizing humoral immunity in unvaccinated people.
Conclusion
Due to co-circulation and the emergence of novel SARS-CoV-2 variants, findings highlight the importance of booster vaccinations for immune protection. More studies should focus on the efficacy of Omicron-induced immunity, its cross-protective properties against other variants, and development of a universal vaccine.
Keywords: COVID-19, SARS-CoV-2, Omicron, mutations, cross-neutralizing antibody, vaccine, immunity
Omicron-induced cross-protective immunity
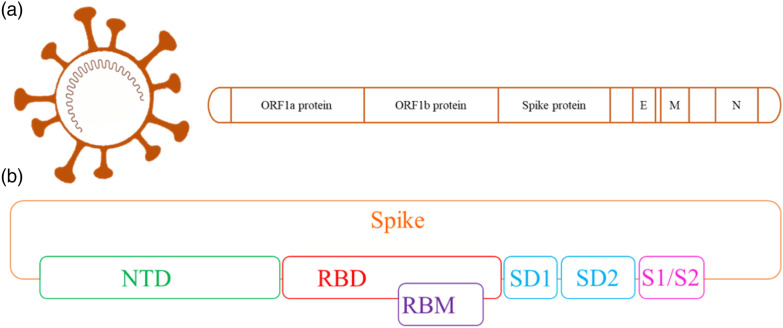
The emergence of the B.1.1.529 (Omicron) severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variant has caused an unprecedented number of cases and fatalities worldwide. By the end of 2021, the Omicron clade, which had more than 30 changes in spike, had emerged, posing a danger to the efficacy of the SARS-CoV-2 vaccination.1 In comparison to other World Health Organization (WHO) recognized variant of concerns (VOC), Omicron and its sublineages have a plethora of genetic and protein level alterations, which contributes to their transmissibility and virulence. New subvariants of the SARS-CoV-2 Omicron variant have rekindled concerns about future immunological evasion. Recently, numerous Omicron sublineages, particularly BA.2.12.1, BA.4, and BA.5, have shown even more immune evasion and are responsible for the recent global outbreaks of infections. In particular, BA.2.12.1, which is becoming more prevalent in the United States, contains two additional mutations than BA.2 (L452Q and S704L).2 Additionally, the prevalent strains in South Africa are BA.4 and BA.5, which both carry identical spike proteins (henceforth referred to as BA.4/5).2 Figure 1 presents a schemetic of SARS-CoV-2 genome and Figure 2 illustrates mutations in the spike protein of different sublineages of Omicron variant.
Figure 1.
Genomic map of SARS-CoV-2 (a and b).3,4 E: Envelope, M: Membrane, N: Nucleocapsid, RBD: Receptor-Binding Domain, RBM: Receptor-Binding Motif, NTD: N-Terminal Domain, SD1 and SD2: Subdomains 1 and 2, S1/S2: Protease Cleavage Site 1 and 2.
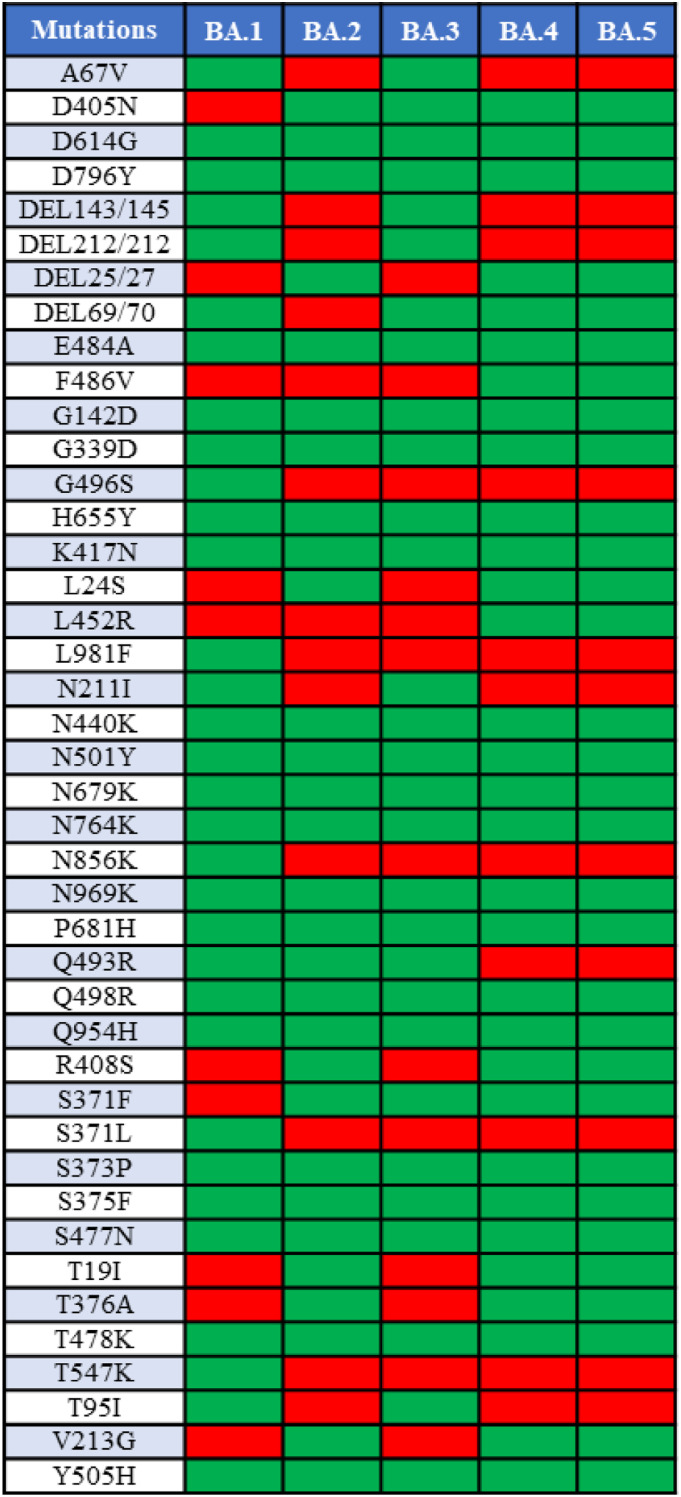
Figure 2.
Mutations in the spike protein of Omicron variants BA.1, BA.2, BA.3, BA.4, and BA.5. Green indicates prevalence of mutation while red indicates little to no mutation.
The effectiveness of neutralizing antibodies generated by vaccines, previous infections, and monoclonal antibody therapy is decreased by the mutations in the Omicron variant.5 After one or two doses of the coronavirus disease 2019 (COVID-19) vaccine, neutralizing antibodies against the Omicron variant stay low and only last a short time, but they are increased in people who have been vaccinated and infected (hybrid immunity) or vaccinated people who have had a booster dose.6,7 Rarely is information available about the neutralization profiles of individuals who have recovered from infection with the Omicron variant.8 A critical component of research is determining the efficacy of Omicron-induced immunity and if it is cross-protective against other variants. Recent research has shown that infection with the Delta variant, but not the Omicron variant, results in the development of widespread immunity.8-10 Suryawanshi et al.8 reported that sera from mice infected with Delta are effective against various VOCs, including Omicron, but sera from mice infected with Omicron are only effective against Omicron. Analyzing human sera from Omicron and Delta breakthrough cases, it has been found that both viruses produce efficient cross-variant neutralization in vaccinated people. Their findings suggest that Omicron infection boosts preexisting vaccine-induced immunity, but that it may not be enough to establish widespread, cross-neutralizing humoral immunity in uninfected people.
Another research study conducted by Stiasny et al.9 agrees with the findings of Suryawanshi et al. This study investigated the nullifying activity of sera following infections with BA.1 and BA.2 in unvaccinated and vaccinated persons since the significantly altered spike protein allows escaping the neutralizing antibodies elicited by prior immunizations or/and infections. The authors reported that initial BA.1 infections resulted in lower neutralizing antibody titers against BA.2, Delta, and wildtype. However, samples of serum from those who had BA.2 infections exhibited no cross-neutralizing activity against the other variants. Up to three months following vaccination, people who were fully vaccinated could still be able to counteract both BA.1 and BA.2. Breakthrough infections due to Omicron exhibited equivalent cross-neutralizing activity against BA.1, BA.2, Delta, and wildtype. Their results indicate that, in pre-immune people, Omicron variants can boost cross-neutralizing antibodies. However, any primary infections with one of the Omicron sublineages resulted in the production of neutralizing antibodies that were only variant-specific. BA.2 infections elicited a response specific to the sublineage, its antigenic distance being indicated. They concluded that primary infections with variants BA.1 and BA.2 will have sublineage-specific neutralization outcomes.9
A neutralization profile study has been conducted by Rössler et al.10 against six variants of SARS-CoV-2 (Delta, Alpha, and Wildtypes). They acquired blood samples from people who recovered from the BA.1 infection; these people may or may not have prior immunity against SARS-CoV-2. This work showed that after BA.1 breakthrough infection, neutralizing antibody titers against all variants increased in vaccinated people, as well as in vaccinated and unvaccinated people with prior infection with some other variant. Against BA.1, the mean neutralizing antibody titers were lesser compared to the similar quantity against the other variants among previously vaccinated people. However, among unvaccinated people with a previous infection with other variants before infection with BA.1, they remained analogous to those against the other variants. On the other hand, if anyone has never been infected with any other variant before being infected with BA.1, samples primarily contained neutralizing antibodies against BA.1. It was rare to find occasions of neutralizing antibodies against the other variants in those samples.10 The findings of this research affirm that the BA.1 variant is very effective to escape immunity and has low cross-responsiveness with previous variants. Therefore, if an unvaccinated person is infected exclusively with BA.1 may not have full protection against infection with other variants. For most defense against any SARS-CoV-2 infection, vaccination is still the best option.10
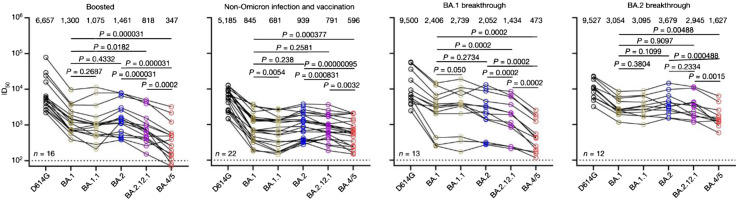
Qu et al. investigated neutralizing antibody titers in serum samples collected from vaccinated individuals who had received one booster dose of the same vaccine used throughout the two-dose series and who had previously been exposed to SARS-CoV-2. The authors reported infection-induced immunity and vaccination-induced immunity against recently discovered omicron subvariants in the study. The BA.4/5 and BA.2.12.1 subvariants were sufficiently neutralized by booster vaccination, but to a lesser extent in comparison to against BA.1 and BA.2. These results emphasize the need for booster shots for defense against novel variants.2 Wang et al.11 assessed the degree of BA.2.12.1 and BA.4/5 resistance to neutralization by sera from four separate clinical cohorts. Figure 3 shows serum neutralization resistance profiles of different Omicron subvariants.
Figure 3.
Neutralization of the wildtype SARS-CoV-2 (D614G) and Omicron subvariants by sera from four different clinical populations.11
Another recent study by Malato et al.12 evaluate the risk of BA.5 infection in those with no recorded previous infections or in those who have had infections in the past at times when certain variants (Wuhan-Hu-1, alpha, delta, and BA.1/BA.2) predominated. They discovered that a history of SARS-CoV-2 infection decreased the likelihood of contracting BA.5. For an initial infection with Wuhan-Hu-1, the protective efficiency was 52.9% compared to the uninfected group, 54.9% for Alpha, 62.3% for Delta, and 80.0% for BA.1/BA.2.11 The results need to be understood in light of new illnesses in a community that has a very high vaccination rate. They concluded that BA.1/BA.2 infection lowers the likelihood of BA.5 breakthrough infections in a highly immunized population. This discovery is crucial for evaluating the existing epidemiological environment and the generation of customized vaccinations.
As of 19 July 2022, the frequency of one newly discovered sublineage, BA.2.75, has been found in at least 16 countries.13 BA.2.75 has nine additional mutations (F157L, G257S, G339H, G446S, I210V, K147E, N460K, W152R) in spike as compared to BA.2 and a reversion to the ancestral variant, R493Q. According to Sheward et al., serum collected before and after the BA.1/BA.2 infection wave, as well as a panel of therapeutically relevant and pre-clinical monoclonal antibodies, can neutralize the BA.2.75 spike. In their collection of serum samples, BA.2.75 displays considerable sensitivity to the monoclonal antibody cocktail made up of tixagevimab and cilgavimab (Evusheld) but no worse immune evasion than the currently dominant BA.5.13
These findings suggest that the Omicron variant elicits less immunity than other variants, which may be caused by its severely altered spike protein or its limited replicative propensity. Despite the immunogenicity of the Omicron variant, infection with this lineage may not cause uninfected individuals to develop efficient cross-neutralizing antibodies against other variants. But in those who have had vaccinations, Omicron infection strengthens defenses against itself and improves protection against other strains. Due to co-circulation and the emergence of novel SARS-CoV-2 variants, findings highlight the importance of booster vaccinations for immune protection.2 This, in conjunction with the finding that Delta infection causes widespread immunogenicity in mice, suggests that Delta- and Omicron-based immunogens should be included in future multivalent vaccination regimens to provide widespread protection against different variants.
Conclusion
The pandemic has not ended yet, and we should expect to see the virus circulating at high levels. It is quite difficult to forecast where the new antigenic variants will appear from here—Delta, Omicron, Deltacron, a new variant or if several lineages may continue circulating similarly to influenza A and B. More studies should focus on the efficacy of Omicron-induced immunity and its cross-protective properties against other variants. We are hopeful that further scientific research will lead to the development of a universal vaccine that can effectively prevent the disease by any existing or emerging mutation of the virus and put an end to this pandemic.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Selia Chowdhury https://orcid.org/0000-0002-4228-9784
References
- 1.Chowdhury S, Bappy MH, Chowdhury S, et al. (2022) Omicron Variant (B. 1.1. 529) of SARS-CoV-2, A Worldwide Public Health Emergency. European Journal of Clinical Medicine 3(1): 5–9. [Google Scholar]
- 2.Qu P, Faraone J, Evans JP, et al. (2022) Neutralization of the SARS-CoV-2 omicron BA. 4/5 and BA. 2.12. 1 subvariants. New England Journal of Medicine 386(26): 2526–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chowdhury S, Bappy MH, Chowdhury S, et al. (2021) Current Review of Delta Variant of SARS-CoV-2. European Journal of Medical and Health Sciences 3(6): 23–29. [Google Scholar]
- 4.Chowdhury S, Bappy MH. (2021) On the Delta Plus Variant of SARS-CoV-2. European Journal of Medical and Health Sciences 3(6): 52–55. DOI: 10.24018/ejmed.2021.3.6.1134. [DOI] [Google Scholar]
- 5.Schmidt F, Muecksch F, Weisblum Y, et al. (2022) Plasma neutralization of the SARS-CoV-2 Omicron variant. New England Journal of Medicine 386(6): 599–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carreño JM, Alshammary H, Tcheou J, et al. (2022) Activity of convalescent and vaccine serum against SARS-CoV-2 Omicron. Nature 602(7898): 682–688. [DOI] [PubMed] [Google Scholar]
- 7.Cele S, Jackson L, Khoury DS, Khan K, et al. (2022) Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature 602(7898): 654–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suryawanshi RK, Chen IP, Ma T, et al. (2022) Limited cross-variant immunity after infection with the SARS-CoV-2 Omicron variant without vaccination. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stiasny K, Medits I, Springer D, et al. Human Primary Omicron BA. 1 and BA. 2. infections result in sub-lineage-specific neutralization, ResearchSquare.
- 10.Rössler A, Knabl L, von Laer D, Kimpel J. (2022) Neutralization Profile after Recovery from SARS-CoV-2 Omicron Infection. New England Journal of Medicine. 386: 1764–1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Q, Guo Y, Iketani S, et al. (2022) Antibody evasion by SARS-CoV-2 Omicron subvariants BA. 2.12. 1, BA. 4 and BA. 5. Nature 608(7923): 603–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malato J, Ribeiro RM, Leite PP, et al. (2022) Risk of BA. 5 Infection in Individuals Exposed to Prior SARS-CoV-2 Variants. medRxiv; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheward DJ, Kim C, Fischbach J, et al. (2022) Evasion of Neutralizing Antibodies by Omicron Sublineage BA. 2.75. bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]