Abstract
Background
The purpose of the study is to evaluate reoperation rate and its relationship to preoperative mechanical axis of rotating-hinge TKA used as the primary implant in complex knees.
Methods
Patients subjected to primary TKA with a rotating-hinge knee prosthesis due to primary osteoarthritis between 2010 and 2019 were retrospectively reviewed. Preoperative mechanical axis was measured using the last preoperative telemetry x-ray image. Preoperative axis was classified according to the type of deformity (varus or valgus) and its magnitude (0-15°, 16-25° or >25°). Reoperation rate (with or without implant removal) was the primary outcome of the current study. We studied if the preoperative mechanical axis (either varus-valgus, or magnitude of malalignment) was related to implant survival rate.
Results
Forty-two patients were included in the study. Mean follow-up was 51.42 ± 31.88 months. The 83.3% of patients presented a valgus axis while the 16.7% presented a varus axis. Need of reoperation occurred in eight patients (19.0%). However, no patients (0%) required implant removal with revision TKA. No association was seen between the preoperative mechanical axis and risk of reoperation (p = 0.16).
Conclusion
In selected situations that do not permit less constrained implants, primary rotating-hinge arthroplasty could be a good alternative. Risk of reoperation does not seem to depend upon the preoperative mechanical axis when using a rotating-hinge knee prosthesis for primary arthroplasty in non-tumoral complex knees.
Keywords: Mechanical axis, Reoperation, Knee arthroplasty, Constriction, Primary arthroplasty
1. Introduction
The number of primary total knee arthroplasty (TKA) cases is growing exponentially.1 There has been considerable evolution in primary TKA during the last years, with new designs, instruments and materials; allowing treatment of the majority of patients, and yielding an overall success rate of 82% at 25 years.2
Hinge implants were developed to offer constraint in the sagittal and coronal planes, thereby providing stability in primary TKA in complex knees with collateral ligament insufficiency, severe varus or valgus deformity, relevant bone loss or hyperlaxity.3,4 The first generations of hinge implants allowed only flexion and extension, leading to poor results due to high transmission of torsional stresses at the bone-prosthesis interface, and patellar tracking disorders.5 New models of rotating-hinge implants also allow free rotation in the transverse plane, decreasing the rate of prosthesis loosening.6,7
In selected complex primary knee replacements, studies of rotating-hinge systems have reported 10-year survival rates ranging between 51% and 92.5%.4 Generalization of the data can be difficult due to differences in the implant model used, the indication criteria for TKA surgery and the patient's preoperative mechanical axis.
The aim of the current study was to evaluate reoperation rate and its relationship to preoperative mechanical axis when using a single model of rotating-hinge TKA as primary implant in non-tumoral complex knee replacement. Our hypothesis states that in selected patients in whom implantation of an unconstrained prosthetic model is not recommended, use of a rotating-hinge prosthesis for primary arthroplasty may provide satisfactory survivorship regardless of preoperative mechanical axis.
2. Methods
2.1. Study design
A retrospective case series study was performed. Using our institution's database, we selected patients who received primary TKA due to primary osteoarthritis using the Endo-Model Rotational Knee Prosthesis (Endo-Model Rotating-Hinge Knee Prosthesis; Waldemar Link GMBH & Co, Hamburg, Germany) between January 2010 and December 2019. All participants provided informed consent. We studied if the preoperative mechanical axis (either varus-valgus, or magnitude of malalignment) was related to implant survival rate.
The inclusion criteria were: a) adult patients, b) use of primary rotating-hinge TKA, c) primary osteoarthritis as indication criteria for surgery, d) availability of preoperative telemetry x-ray image, and e) minimum follow-up of two years. Patients who did not meet the inclusion criteria were excluded from the study.
2.2. Studied parameters
Patient demographic, clinical and radiological records were collected preoperatively, postoperatively, and during the follow-up period. Reoperation rate was the primary outcome of the current study. Reoperation was defined as the need of further surgery after TKA implantation, with or without implant removal. During follow up, need of reoperation, time to reoperation and its treatment were studied. We also categorized the causes for reoperation: mechanical failures due to periprosthetic fracture, aseptic loosening, patellar complications, instability or rigidity, and non-mechanical failures due to infection or soft tissue problems. Mortality during follow up was recorded too.
Demographic data included patient age at the time of surgery, gender, and ASA (American Society of Anaesthesiologists) classification. The indication criteria for primary TKA using a rotating-hinge model were also recorded. All the patients of the study were operated on due to primary osteoarthritis with coronal deformity or collateral ligament insufficiency. In order to analyse a homogeneous population, patients who presented other indication criteria were excluded.
Preoperative mechanical axis was studied using the last preoperative telemetry x-ray image. Preoperative axis was classified according to the type of deformity (varus or valgus) and its magnitude (0-15°, 16-25° or >25°). These radiological parameters were measured a single time by two general orthopedic surgeons. The digital templating program TraumaCad® version 2.0 (BrainLab, Feldkirchen, Germany) was used for the analysis. The lack of a correct preoperative telemetry x-ray image allowing to measure the mechanical axis was considered an exclusion criterion.
2.3. Statistical analysis
The statistical study was performed using the Stata® statistical program, version 14.1 (StataCorp, College Station, TX). Descriptive statistics were used to present the cohort's characteristics. Categorical variables were described by their absolute values and percentages. Continuous variables were presented by their mean, deviation and range. Normality was tested using the Kolmogorov-Smirnov test. Differences in risk of failure according to patient age, ASA score or mechanical axis were studied using Mann-Whitney, Kruskal-Wallis and Pearson's chi square tests. All p-values were two-sided, and statistical significance was defined as p < 0.05.
3. Results
Of the 373 TKAs operated upon in our institution using the Endo-Model Rotational Knee Prosthesis (Waldemar Link GMBH & Co, Hamburg, Germany) during the studied period, 300 were revisions. These cases were excluded, leaving 73 knees that had undergone primary TKA. Among them, 12 patients were excluded because their preoperative telemetry x-ray image was not available and 19 because their indication criteria for surgery was not primary osteoarthritis (4 fractures, 6 sequels of haemophilia, 6 post-fracture/infection osteoarthritis and 3 avascular necrosis). Finally, 42 patients met our inclusion and exclusion criteria, and were available for analysis. Mean follow-up was 51.42 ± 31.88 months. Patient characteristics are shown in Table 1.
Table 1.
Baseline characteristics of patients.
| Number of patients | 42 |
| Age (years) (mean ± standard deviation, [range]) |
75.02 ± 8.33 [50–86] |
| Gender (Female:Male) | 33:9 (78.6%:21.4%) |
| ASA-score (%) | |
| •ASA-I | •01% |
| •ASA-II | •55% |
| •ASA-III | •43% |
| •ASA-IV | •01% |
ASA (American Society of Anaesthesiologists Physical Status Classification).
Preoperative mechanical axis analysis is shown in Table 2. The 83.3% of patients presented a valgus axis while the 16.7% presented a varus axis.
Table 2.
Preoperative mechanical axis.
| Preoperative mechanical axis | Number of patients, N (%)a | Failure rateb, N (%) |
|---|---|---|
| •Varus axis | •7 (16.7%) | •1 (14.3%) |
| o 0-15° | o 1 | o 0 (0%) |
| o 16-25° | o 5 | o 1 (20%) |
| o >25° | o 1 | o 0 (0%) |
| •Valgus axis | •35 (83.3%) | •7 (20%) |
| o 0-15° | o 10 | o 2 (20%) |
| o 16-25° | o 20 | o 3 (15%) |
| o >25° | o 5 | o 2 (40%) |
Patients were classified according to the type of deformity (varus or valgus) and its magnitude (0-15°, 16-25° or >25°). Failure rate according to the preoperative mechanical axis was analysed.
Percentage over 42 patients (all patients of the study).
P-value = 0.16 (no statistically significant).
Need of reoperation (with or without implant removal) occurred in eight patients (19.0%), (Table 3). Five patients (11.9%) had mechanical failures; all were extensor mechanism complications that were successfully treated through an extensor mechanism realignment. Three patients (7.1%) had non-mechanical failures; all were infection complications, that solved after DAIR surgery (debridement, antibiotics, polyethylene insert exchange and implant retention). However, it highlights that no patient required implant removal with revision TKA. No periprosthetic fracture or aseptic loosening was recorded.
Table 3.
Failures and their treatment.
| Type of Failure | Failure | Number of patients (%)a | Treatment |
|---|---|---|---|
| Mechanical failure | Extensor mechanism complication | 5 (11.9%) | Extensor mechanism realignment |
| Non-mechanical failure | Septic | 3 (7.1%) | DAIR surgery |
DAIR (Debridement Antibiotics and Implant Retention).
%: of total patients of the study (42 patients).
No association was seen between the preoperative mechanical axis (either varus-valgus, or magnitude of malalignment) and risk of reoperation (p = 0.16), (Table 2).
There were no statistically significant differences in risk of reoperation based on patient age (p = 0.4) or ASA score (p = 0.37).
4. Discussion
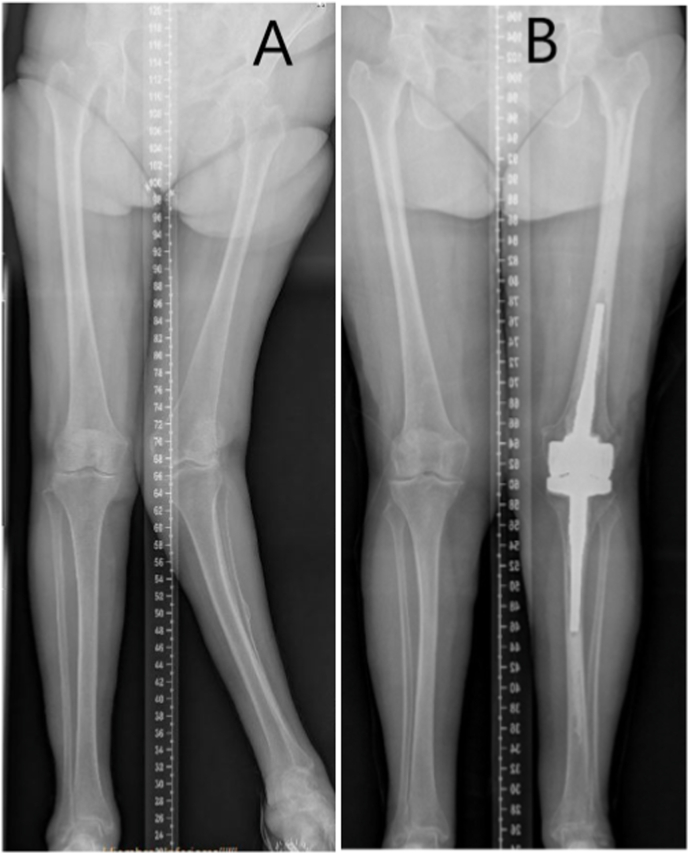
Our most important finding was that, interestingly, preoperative mechanical axis (either varus-valgus, or magnitude of malalignment) was not significantly related to risk of reoperation (p = 0.16). This finding is clinically relevant because it supports the use of primary rotational-hinge prostheses in the most severe cases of malalignment (Fig. 1). To the best of our knowledge, there is little literature studying this association in the rotating-hinge primary TKA scenario.
Fig. 1.
A) Lower limb telemetry showing a 76-year-old patient suffering primary knee osteoarthritis with severe valgus deformity (28°). B) Post-operative lower limb telemetry of the same patient demonstrating coronal malalignment correction. A primary rotating-hinge TKA was correctly implanted.
It has been defended that severe preoperative coronal deformities can result in greater risk of implant failure in unconstrained TKA, and that correction of the malalignment can decrease this risk.8 Regarding preoperative varus deformity, however, some authors have stated that it does not affect survival rates in neutral-aligned TKAs.9 Moreover, Guenoun et al.10 pointed out that a preoperative axial deviation in varus >10° seemed to be a protective factor against failure. On the other hand, results are prone to be worse when correcting knees with preoperative valgus malalignment.11 As higher coronal deformity is linked to more complex TKA surgery and more difficulty to achieve normo-alignment, an increased failure risk could be expected. However, we found no relationship between preoperative mechanical axis and reoperation rate when using primary rotational-hinge prostheses. The results observed in our study could be explained by the capacity of these models to achieve stable and well-aligned primary TKA regardless of preoperative axis. Similar to us, Rodríguez-Merchán4 and Gehrke et al.3 defended that these prosthesis compensated well for deformity and ligamentous insufficiency, being a good therapeutic option for cases with severe preoperative coronal malalignment. Petrou et al.12 and Yang et al. were able to correct coronal malalignment in all the knees of their series, achieving excellent survival rate at 15 years.
Analysing complications among our patients, the 19.0% of them required reoperation. However, it highlights that no patients (0%) required implant removal with revision TKA. With regard to complications, the literature is heterogeneous. While some studies showed promising clinical results and survival rates, others reported high complication rates. In the EFORT review,4 rotating-hinge implants were said to have 10-year survivorship in the range of 51–92.5%, and a complication rate of 9.2–63%. It was proposed that these wide-ranging outcomes result from variations in implant design, indications, and quality of surgical technique. Gehrke et al.3 obtained a complication rate of 10% after a mean follow-up of 13 years in their series of 141 rotating-hinge primary TKA. In a large meta-analysis (1425 prostheses) performed by Abdulkarim et al.,6 short-term and mid-term implant survival rate was 92% and 82% respectively. They maintained that the complexity of complications in this scenario should not be underestimated. In a very large monographic series, Zinck et al.13 reviewed 2682 primary rotating-hinge implants and reported a failure rate of 1.4%, after a mean follow-up of 64 months. Excellent survival rates at 15 years were also reported by Petrou et al.12 and Yang et al.,14 96.1% and 87% respectively. Complication rates similar to ours were found by Bistolfi et al.7 (20.2% at 10 years), Cottino et al.15 (22.5% at 10 years) and Neri et al.5 (25% at 7 years). Most authors consider such complication rates acceptable, in light of the surgery's complexity. Higher failure rates were found by Guenoun et al.10 and Smith et al.,16 30.8% at 36 months and 45.9% at 72 months respectively.
In our series, reoperation due to infection (7.1%) and extensor mechanism complications (11.9%) were noteworthy. We agree with the literature's consensus that infection is the primary cause of failure.5, 6, 7,10,12,14,15,17,18 The high infection rate in this scenario could be explained by the complexity of the surgery, extensive soft-tissue dissection, longer-duration procedures and patient comorbidities. Many articles have also reported high extensor mechanism complication rates.3,10,12,14,18 Some authors prefer non-rotating-hinge implants in case of severe valgus malalignment to improve patellar tracking,3 others prefer to avoid replacing the patella,12 or to perform a lateral release.14
In our case series of primary non-tumoral prostheses, the most common indication for surgery was primary osteoarthritis with coronal deformity (74% of patients, most with severe valgus deformity), followed by sequels of haemophilia (8.2%) and fracture (5.5%). Abdulkarim et al.6 performed a meta-analysis (11 articles, 1425 prostheses) in which they found that among non-tumoral patients the most common indication for primary rotating-hinge TKA was osteoarthritis. Other indications included rheumatoid arthritis, post-traumatic arthritis, fracture malunion, Charcot arthropathy and poliomyelitis. This predominance of osteoarthritis is comparable to our results, and common among the reviewed articles.5,7,10,12,14,18,19 Due to the higher risk of revision, primary constrained prostheses are only recommended for complex situations in which use of unconstrained implants is not allowable,7,19,20 such as knees with collateral ligament insufficiency, severe varus or valgus deformity, relevant bone loss or hyperlaxity.3,4 Martin et al.19 demonstrated an increased reoperation rate, two times higher at 10 years and three times higher at 20 years.
Another point to consider when implanting constrained prostheses is patient age. Gehrke et al.3 recommended that such implants should be reserved for elderly patients (>75 years), as they found lower survival rate in younger patients. Other studies have also observed lower survival rate in younger patients (<60 years), likely due to aseptic loosening.15,20 In our series, the average patient age was 75.02 ± 8.33 years, reserving primary rotating-hinge TKA for older patients. However, in our most severe cases, we chose rotating-hinge TKA regardless of age, due to the impossibility of achieving joint stability with less constricted implants. We did not find statistically significant differences in reoperation risk related to patient age (p = 0.4). It might be explained by the fact that most patients who underwent constrained primary TKA in our institution were older. However, the relationship between survival rate and age is not uniformly reported in the literature; some authors showed that survival was not influenced by age.12
There are some limitations to the current study. The first limitation lies in the study's retrospective nature. Another important limitation is that sample size is relatively small (42 patients), which could underpower our study. Furthermore, follow-up is relatively short (51.42 ± 31.88 months). Larger cohorts and longer follow-ups are necessary for better definition of outcomes. One strength of this study is its homogeneity. All the included patients were operated on by surgeons of the same knee unit, indication criterion for surgery was always primary osteoarthritis and only one model of prosthesis was implanted.
In conclusion, in selected situations that do not permit less constrained implants, primary rotating-hinge arthroplasty could be a good alternative. Risk of reoperation does not seem to depend upon the preoperative mechanical axis when using a rotating-hinge knee prosthesis for primary arthroplasty in non-tumoral complex knees.
Informed consent
Informed consent was obtained from all individual participants included in the study or their relatives.
Institutional ethical committee approval
We consulted our Center's Ethics Committee (CEIC; Vall d’Hebron Institut de Recerca [VHIR]; www.vhir.org). Due to the retrospective and observational nature of our study, it was granted exemption from requiring specific ethics approval.
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Author's contributions
All authors contributed equally to this work. All authors contributed to the study conception and design, material preparation, data collection and analysis. The first draft of the manuscript was written by the first author and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Declaration of competing interest
None.
Acknowledgements
We thank Russell Williams of RoundlyWorded.com for his editorial recommendations.
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Evans J.T., Walker R.W., Evans J.P., Blom A.W., Sayers A., Whitehouse M.R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:655–663. doi: 10.1016/S0140-6736(18)32531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gehrke T., Kendoff D., Haasper C. The role of hinges in primary total knee replacement. Bone Jt J. 2014;96-B doi: 10.1302/0301-620X.96B11.34143. :93–5. [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez-Merchán E.C. Total knee arthroplasty using hinge joints: indications and results. EFORT Open Rev. 2019;4:121–132. doi: 10.1302/2058-5241.4.180056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neri T., Boyer B., Papin P.-E., et al. Contemporary rotating hinge arthroplasty can safely be recommended in complex primary surgery. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05589-x. [DOI] [PubMed] [Google Scholar]
- 6.Abdulkarim A., Keane A., Hu S.Y., Glen L., Murphy D.J. Rotating-hinge knee prosthesis as a viable option in primary surgery: literature review & meta-analysis. Orthop Traumatol Surg Res. 2019;105:1351–1359. doi: 10.1016/j.otsr.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Bistolfi A., Lustig S., Rosso F., Dalmasso P., Crova M., Massazza G. Results with 98 endo-modell rotating hinge prostheses for primary knee arthroplasty. Orthopedics. 2013;36:e746–e752. doi: 10.3928/01477447-20130523-19. [DOI] [PubMed] [Google Scholar]
- 8.Ritter M.A., Davis K.E., Davis P., et al. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Jt Surg-Am. 2013;95:126–131. doi: 10.2106/JBJS.K.00607. [DOI] [PubMed] [Google Scholar]
- 9.Oh S.-M., Bin S.-I., Kim J.-Y., Cho H.-I., Lee B.-S., Kim J.-M. Does the preoperative varus deformity influence the survival of postoperative neutral-aligned TKAs? An analysis with a minimum 5-year follow-up. J Arthroplasty. 2018;33:3181–3185. doi: 10.1016/j.arth.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Guenoun B., Latargez L., Freslon M., Defossez G., Salas N., Gayet L.-E. Complications following rotating hinge Endo-Modell (Link®) knee arthroplasty. Orthop Traumatol Surg Res. 2009;95:529–536. doi: 10.1016/j.otsr.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Apostolopoulos A.P., Nikolopoulos D.D., Polyzois I., et al. Total knee arthroplasty in severe valgus deformity: interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop Traumatol Surg Res. 2010;96:777–784. doi: 10.1016/j.otsr.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Petrou G., Petrou H., Tilkeridis C., et al. Medium-term results with a primary cemented rotating-hinge total knee replacement: a 7 to 15 year follow-up. J Bone Joint Surg Br. 2004;86-B doi: 10.1302/0301-620X.86B6.14708. :813–7. [DOI] [PubMed] [Google Scholar]
- 13.Zinck M., Sellckau R. Rotationsknieprothese ENDO-Modell: geführter Oberflächenersatz mit Sti(e)l. Orthop. 2000;29:S38–S42. doi: 10.1007/PL00003681. [DOI] [PubMed] [Google Scholar]
- 14.Yang J.-H., Yoon J.-R., Oh C.-H., Kim T.-S. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc. 2012;20:517–523. doi: 10.1007/s00167-011-1590-1. [DOI] [PubMed] [Google Scholar]
- 15.Cottino U., Abdel M.P., Perry K.I., Mara K.C., Lewallen D.G., Hanssen A.D. Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Jt Surg. 2017;99:324–330. doi: 10.2106/JBJS.16.00307. [DOI] [PubMed] [Google Scholar]
- 16.Smith T.H., Gad B.V., Klika A.K., Styron J.F., Joyce T.A., Barsoum W.K. Comparison of mechanical and nonmechanical failure rates associated with rotating hinged total knee arthroplasty in nontumor patients. J Arthroplasty. 2013;28:62–67. doi: 10.1016/j.arth.2012.05.008. e1. [DOI] [PubMed] [Google Scholar]
- 17.Baker P., Critchley R., Gray A., et al. Mid-term survival following primary hinged total knee replacement is good irrespective of the indication for surgery. Knee Surg Sports Traumatol Arthrosc. 2014;22:599–608. doi: 10.1007/s00167-012-2305-y. [DOI] [PubMed] [Google Scholar]
- 18.Rouquette L., Batailler C., Muller B., Neyret P., Servien E., Lustig S. Early complications and causes of revision after rotating-hinge TKA. Arch Orthop Trauma Surg. 2020;140:109–119. doi: 10.1007/s00402-019-03290-9. [DOI] [PubMed] [Google Scholar]
- 19.Martin J.R., Beahrs T.R., Stuhlman C.R., Trousdale R.T. Complex primary total knee arthroplasty: long-term outcomes. J Bone Jt Surg. 2016;98:1459–1470. doi: 10.2106/JBJS.15.01173. [DOI] [PubMed] [Google Scholar]
- 20.Badawy M., Fenstad A.M., Furnes O. Primary constrained and hinged total knee arthroplasty: 2- and 5-year revision risk compared with unconstrained total knee arthroplasty: a report on 401 cases from the Norwegian Arthroplasty Register 1994–2017. Acta Orthop. 2019;90:467–472. doi: 10.1080/17453674.2019.1627638. [DOI] [PMC free article] [PubMed] [Google Scholar]