Abstract
Background:
Increased solar and geomagnetic activity (SGA) may alter sympathetic nervous system activity, reduce antioxidant activity, and modulate physiochemical processes that contribute to atmospheric aerosols, all which may reduce pulmonary function.
Objectives:
Investigate associations between forced expiratory volume at 1 s (FEV1) and forced vital capacity (FVC) with SGA, and assess whether SGA enhances adverse effects of particulate pollution, black carbon (BC) and particulate matter ≤2.5 μm in diameter (PM2.5). Methods: We conducted a repeated measures analysis in 726 Normative Aging Study participants (Boston, Massachusetts, USA) between 2000 and 2017, using interplanetary magnetic field (IMF), planetary K index (Kp), and sunspot number (SSN) as SGA measures. Linear mixed effects models were used to assess exposure moving averages up to 28 days for both SGA and pollution.
Results:
Increases in IMF, Kp Index and SSN from the day of the pulmonary function test averaged through day 28 of were associated with a significant decrement in FEV1 and FVC, after adjusting for potential confounders. There were greater effects for longer moving averages and enhanced effects of PM2.5 and BC on FEV1 and FVC with increased SGA. For example, for each inter-quartile increase (4.55 μg/m3) in average PM2.5 28 days before testing, low IMF (10th percentile: 3.2 nT) was associated with a −21.4 ml (95 % CI: −60.8, 18.1) and −7.1 ml (95 % CI: −37.7, 23·4) decrease in FVC and FEV1, respectively; high IMF (90th percentile: 9.0 nT) was associated with a −120.7 ml (95 % CI:-166.5, −74.9) and −78.6 ml (95 % CI: −114.3, −42·8) decrease in FVC and FEV1, respectively.
Discussion:
Increased periods of solar and geomagnetic activity may directly contribute to impaired pulmonary function and also enhance effects of PM2.5 and BC. Since exposure to solar activity is ubiquitous, stricter measures in reducing air pollution exposures are warranted, particularly in elderly populations.
Keywords: Solar radiation, Air pollution, Pulmonary function, Geomagnetic disturbance, Solar activity, Lung outcomes, Particulate matter
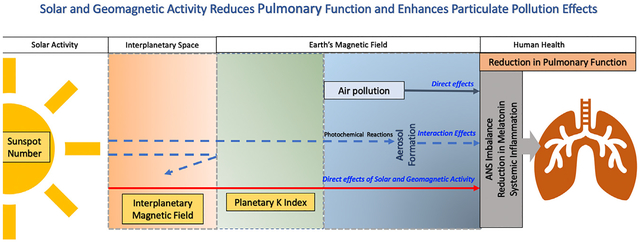
GRAPHICAL ABSTRACT
1. Introduction
The Sun emits electromagnetic radiation that varies over 11-year solar cycles (Hathaway, 2015). Within each solar cycle, periods of high solar activity are characterized by an increased solar flares and corona mass ejections, which release high-energy material into the space, triggering disturbances in the Earth’s magnetic field. Solar activity and geomagnetic disturbances (GMD) have been linked to direct and indirect effects on atmospheric aerosols and human health (J.-L. Chen and Zhao, 2014), including increased risk of cardiovascular mortality (Zilli Vieira et al., 2019), stroke risk (Feigin et al., 2014), higher blood pressure, reduced heart rate variability (Cornélissen et al., 2010; Dimitrova et al., 2009; Wang et al., 2021), lower peripheral white blood cell counts (Tracy et al., 2022), and mental health (Davis and Lowell, 2004). However, to date, no study has investigated the association between solar activity and pulmonary function in observational settings, despite a plausible biological link.
Solar and Geomagnetic Activity (SGA) has been associated with disruption of 24-h circadian rhythm (Riganello et al., 2019), autonomic nervous system imbalance (McCraty et al., 2017), and reduced secretion of melatonin (Burch et al., 1999). Disruption of 24-h circadian rhythm results in higher immune and inflammatory responses, which appears to promote the development and exacerbation of pulmonary diseases (Aquino-Santos et al., 2020; Sundar et al., 2015). Reduced secretion of melatonin, a free-radical scavenger, is associated with greater measures of oxidative stress, which has been implicated as a cause of cell damage and inflammation in the lungs(Bargagli et al., 2009). Similarly, particulate air pollution appears to also promote oxidative stress and inflammation that has the potential to promote lung diseases and reduce lung function (Gangwar et al., 2020; Lodovici and Bigagli, 2011). Moreover, a recent study found a significant association between solar activity and increased ambient ultrafine particle concentrations, suggesting a direct link between solar activity and higher levels of ambient air pollution (Zilli Vieira and Koutrakis, 2021). Therefore, due to joint effects related to inflammation, oxidative stress, and modulation of the physiochemical properties of atmospheric aerosols, we hypothesize interactions between periods of increased solar activity and air pollution is associated with heightened adverse pulmonary effect.
The adverse effects of short- and long-term exposure to particle matter ≤10 and ≤2.5 μm (PM10 and PM2.5, respectively) and black carbon (BC) on pulmonary function has been well documented (C.-H. Chen et al., 2019; Int Panis et al., 2017; Rice et al., 2013). However, there is a paucity of epidemiological evidence on the influence of solar activity and GMD. Our objective was to investigate the association of pulmonary function [forced expiratory volume at 1 s – (FEV1) and forced vital capacity (FVC), and FEV1/FVC] with SGA, and to test whether SGA enhances the adverse effects of particulate air pollution on the outcome of interest.
2. Methodology
2.1. Study population
The study population comprised of elderly male residents of the greater Boston, MA, enrolled in the Normative Aging Study (NAS) cohort established by the U.S. Veterans Administration in 1963 who were free of major illness during enrolment (Bell et al., 1972). We restricted our analysis to visits between 2000 and 2017 for participants due to limitations in availability of exposure data. Participants with C-reactive protein serum levels higher than 10 mg/L (suggesting acute illness) were excluded to arrive at 726 individuals with 2075 observations. Upon every study visit, the participants were administered detailed questionnaires and underwent clinical examinations including pulmonary function tests. Spirometry testing was conducted based on ATS guidelines (Miller et al., 2005). Information on pulmonary disorders, medication use, smoking status, and other personal characteristics were collected at each visit using standardized questionnaires (Sparrow et al., 1987). The study obtained informed consent from the participants and approval from the Institutional Review Boards of Harvard T.H. Chan School of Public Health and VA Boston Healthcare System.
2.2. Exposure assessment
2.2.1. Air pollution
We obtained data on daily PM2.5 in μg/m3 and BC in μg/m3 measured at a Boston Harvard supersite, located at the roof of the Harvard Medical School’s Countway Library of Medicine. Particulate air pollution exposure was assessed using a Harvard Impactor to collect PM2.5 samples and an aethalometer (Magee Scientific Company, model AE-16, Berkeley, CA) to measure hourly BC concentrations averaged to provide daily values.
2.2.2. Solar and geomagnetic activity parameters
Interplanetary Magnetic Field (IMF), sunspot number (SSN), and Planetary K (Kp) Index are indicators of SGA. Intense solar activity causes release of high-energy material entering the interplanetary space by the solar winds. This component of the Sun’s magnetic field entering the interplanetary space is called IMF (Hathaway, 2015). Although the Earth is protected by its own magnetic field, during periods of high solar activity, part of the energy carried by solar wind and solar particles infiltrate the magneto-sphere causing GMD (Yermolaev and Yermolaev, 2010). The Kp Index characterizes the magnitude of fluctuations in the disturbances in the Earth’s magnetic field attributable to solar activity (https://spaceweatherlive.com/en/help/the-kp-index.html). An increase in solar activity is also associated with an increase in sunspot numbers, the dark areas on the sun characterized by a strong magnetic field (Solanki, 2003). Intense solar activity periods are characterized by increases in all parameters included in our study. The data were downloaded from the OMNI data set of the NASA Goddard Space Flight Centre’s Space Physics website (https://omniweb.gsfc.nasa.gov/form/dx1.html).
2.3. Statistical analysis
We used linear mixed effects models with a random intercept for each participant to account for heterogeneity among subjects and correlation between repeated measurements taken on the same subject. The models took the form:
where Yij is the lung function measurement in subject i at visit j, β0 is the intercept, β1 is the effect of the exposure variable on lung function measurement, and Eij is the exposure concentration for the subject i in the day-of and days prior to the visit j. The covariates for subject i at visit j are denoted by C1ij to Cnij, εij was the within-participant error and ui represents a subject-specific random intercept.
Firstly, we estimated the effect of the exposure on the day of testing (day 0) through 28 day moving averages for both air pollutant and solar activity parameters on FEV1 and FVC. Exposure windows/moving averages were calculated as average cumulative exposure (through day 28) starting prior to the day of outcome measurement (day 1). We tested for effect modification with multiplicative interaction terms between air pollution and SGA for each moving average calculated over the same time periods.
We then calculated the effect of these interactions at high (90th percentile) and low (10th percentile) levels of the overall distribution of SGA at each visit for the entire follow up period.
All models were adjusted for a priori determined confounders and covariates based on known associations that included age (yr), height (inches), body mass index (kg/m2), sine and cosine terms based on the pulmonary function test date [sin(2π*(day of year)/365) and cos(2π*(day of year)/365)] adjusting for long-term seasonal trends, day of the week, race category (white or non-white), physician diagnosed asthma (yes/no), chronic bronchitis or emphysema (yes/no), history of chronic heart disease (yes/no), history of stroke (yes/no), smoking status (never, current, former), cumulative smoking in pack-years (number), two or more drinks per day (yes/no), use of corticosteroids (yes/no), use of beta blockers (yes/no) (Lepeule et al., 2014). The FEV1/FVC models were not adjusted for height. We also adjusted for ambient temperature (°C) and relative humidity (%) on the day of pulmonary function testing using data obtained from Boston Logan Airport (https://www.ncei.noaa.gov/). Solar parameters were treated as continuous variables and effect estimates for the above-mentioned period were expressed as the change in FEV1 and FVC (in ml) or change in FEV1/FVC (in %) for interquartile range (IQR) increment for each moving average. All statistical analyses were performed using software R Version 3.6.3.
3. Results
Table 1 shows the baseline and longitudinal characteristics of the study population. There were 726 individuals with 2075 observations between 2000 and 2017. Participants were male, mostly white (98 %) with a mean age of 73 years, and mean BMI of 28.1 kg/m2 at baseline of the present study. In the year 2000, <5 % of subjects were current smokers, but most were former smokers (64·5 %). At study entry the mean FEV1 and FVC were 2.51 L and 3.35 L and respectively and mean percent predicted FEV1, FVC at baseline were 92.7 % and 94.3 % respectively. The FEV1/FVC at baseline was 75 %.
Table 1.
Descriptive characteristics of Normative Aging Study (NAS) cohort for the study period (2000–2017).
| Visit 1 (Baseline) | All visits | |
|---|---|---|
| Total observations (n) | 726 | 2075 |
| Characteristics | n (%) or Mean ± SD | n (%) or Mean ± SD |
| Race (%White) | 706 (98.1) | 2012 (97.9) |
| Current Smoker | 32 (4.4) | 79 (3.8) |
| Former Smoker | 467 (64.5) | 1340 (64.7) |
| Never Smoker | 225 (31.1) | 652 (31.5) |
| Alcohol (>2 drinks daily) | 134 (18.5) | 369 (17.8) |
| Coronary heart disease | 216 (29.8) | 751 (36.2) |
| Stroke | 52 (7.2) | 171 (8.2) |
| Diabetes | 97 (13.4) | 337 (16.2) |
| Corticosteroids | 48 (6.7) | 101 (6.8) |
| Beta blocker | 261 (35.9) | 851 (41.0) |
| Chronic Pulmonary Diseasesa | 132 (18.3) | 346 (18.7) |
| FVC (L) | 3.35 ± 0.67 | 3.42 ± 0.70 |
| %-Predicted FVC | 94.29 ± 16.16 | 95.20 ± 15.80 |
| FEV1 (L) | 2.51 ± 0.58 | 2.53 ± 0.59 |
| %-Predicted FEV1 | 92.65 ± 18.50 | 93.75 ± 17.88 |
| FEV1/FVC (%) | 75.0 ± 8.00 | 73.0 ± 8.00 |
| Age (y) | 73.2 ± 6.90 | 76.7 ± 7.10 |
| Height (in) | 68.5 ± 2.70 | 68.3 ± 2.80 |
| BMI (kg/m2) | 28.1 ± 4.00 | 27.9 ± 4.00 |
| Cumulative smoking (pack-years) | 21.0 ± 25.40 | 28.0 ± 22.80 |
SD (standard deviation); FVC (forced vital capacity); FEV1(forced expiratory volume at 1 s); BMI (body mass index).
Physician diagnosed asthma, emphysema, or chronic bronchitis.
Mean SGA and air pollutant exposures on the day of pulmonary function testing over the study visits (2000–2017) are summarized in Table 2. Across the study period, the mean (±SD) IMF, Kp Index and SSN were 5.80 (±2.6) nT, 18.6 (±11.6), 83.8 (±74.5), respectively. Average PM2.5 and BC were 9.3 (±6.4) and 0.75 (±0.40) μg/m3, respectively, across the study period. The mean values of ambient temperature and relative humidity were 13.3 (±8.7)°C and 68.1 (±17.3) %, respectively.
Table 2.
Solar activity and air pollution exposure on the day of clinical measurement (day zero) across the study period (2000–2017).
| Exposure | Mean (SD) | IQR | 10th, 90th percentile |
|---|---|---|---|
| IMF (nT)a | 5.8 (2.6) | 2.8 | 3.21, 8.97 |
| Kp Indexb | 18.6 (11.6) | 15.6 | 5.3, 35.3 |
| Number of Sunspots (#) | 83.8 (74.5) | 114.6 | 0.0, 190.1 |
| PM2.5 (μg/m3) | 9.3 (6.4) | 6.6 | 3.7, 17.6 |
| Black Carbon (μg/m3) | 0.75 (0.40) | 0.53 | 0.32, 1.31 |
| Ambient Temperature (°C) | 13.3 (8.7) | 13.6 | – |
| Relative Humidity (%) | 68.1 (17.3) | 26.7 | – |
SD (standard deviation); IQR (interquartile range); PM2.5 (particulate matter <2.5μm in aerodynamic diameter); IMF (interplanetary magnetic field); Kp Index (planetary K index); SSN (sunspot number).
Nanotesla (nT) – unit of measurement for magnetic field.
Kp Index is Dimensionless.
The spearman correlation coefficient among the three SGA parameters ranged between 0.31 and 0.69 (Table 3) SGA and the air pollutants were not meaningfully correlated. The correlations between IMF and Kp Index with PM2.5 and BC were between 0.09 and 0.13, and were slightly greater for SSN with PM2.5 and BC (Table 3).The variations in solar and geomagnetic activity over the study period are shown in Fig. 1. The figure illustrates daily variation of the parameters on the day of pulmonary function testing, as well as their magnitude over the solar cycle. The study captured two solar maximum and one solar minimum.
Table 3.
Spearman correlation coefficients of Solar and Geomagnetic Activity and Particulate Air Pollution Parameters on the day of pulmonary function measurement (n = 2075).
| Exposure | PM2.5 | BC | IMF | Kp Index | SSN | Temp | RH |
|---|---|---|---|---|---|---|---|
| PM2.5 | 1 | – | – | – | – | – | – |
| BC | 0.75* | 1 | – | – | – | – | – |
| IMF | 013* | 0.12* | 1 | – | – | – | – |
| Kp Index | 012* | 0.09* | 0.69* | 1 | – | – | – |
| SSN | 0–22* | 0.26* | 0.42* | 0.31* | 1 | – | – |
| Temp | 0.19* | 0.22* | −0.07* | −0.01 | −0.01 | 1 | – |
| RH | −0.04 | 0.13* | 0.2 | 0.01 | 0.11* | −0.06* | 1 |
PM2.5 (particulate matter <2.5 μm in aerodynamic diameter); BC (black carbon); IMF (interplanetary magnetic field); Kp Index (planetary K index); SSN (sunspot number); Temp (temperature); RH (relative humidity).
Indicates p < 0.05.
Fig. 1.
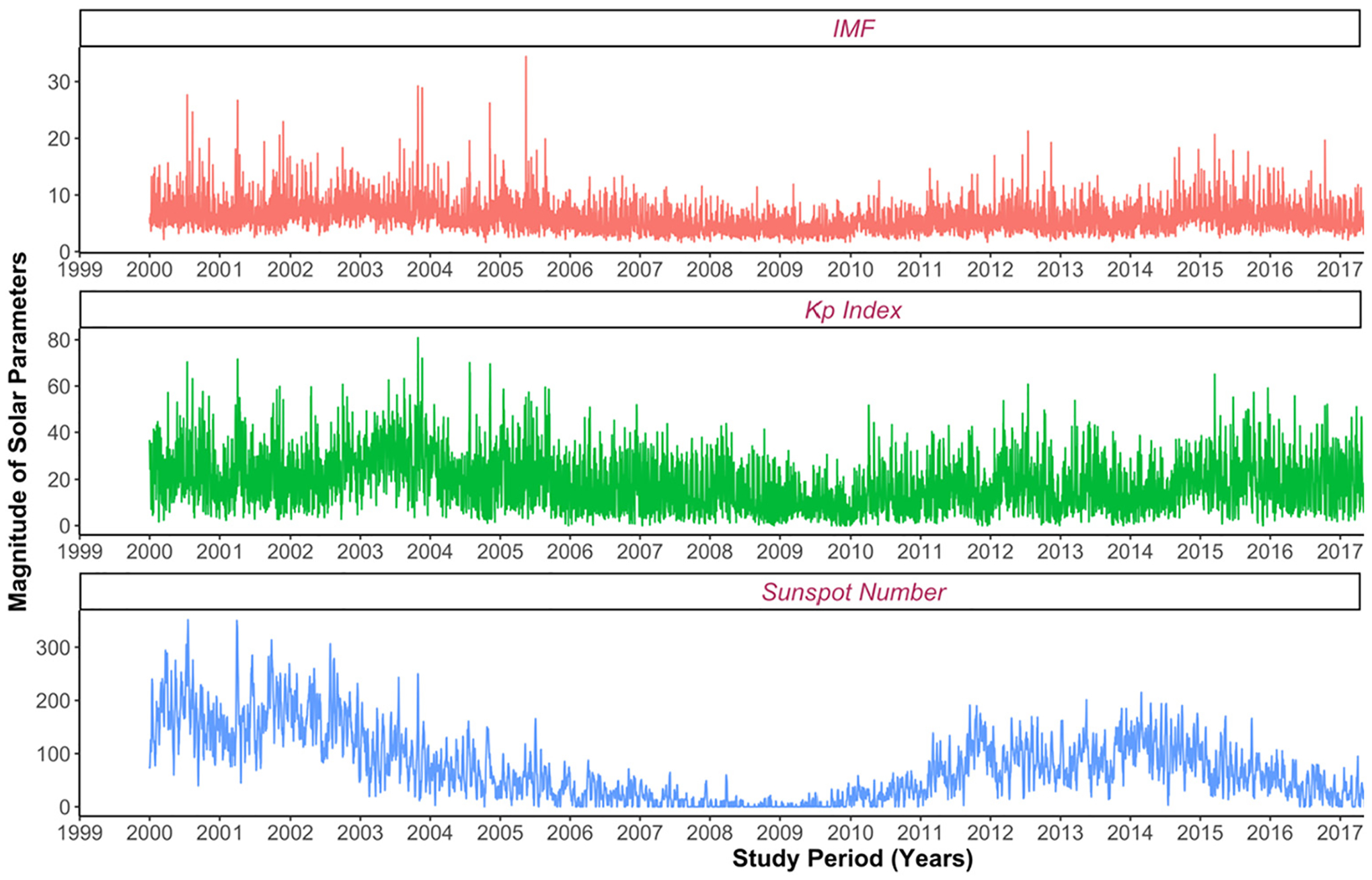
Variations of solar and geomagnetic activity parameters over the study period. Note: IMF is measured in nT (nano tesla), Kp Index is dimensionless and sunspot number is measured in number (#). Footnote: IMF (interplanetary magnetic field); Kp Index (planetary K index).
3.1. Solar and geomagnetic activity and pulmonary function
In our primary models, we found negative associations between 0 to 28 day moving average of all SGA parameters and FVC, FEV1 and positive associations with FEV1/FVC, after adjusting for potential confounders. Other than the association between Kp index and FEV1, the effects were significant, with a greater decrement in FVC (Table S2 and Fig. 2) and FEV1 (Table S1 and Fig. 2) with longer moving averages. For an increase in inter-quartile range of SSN, Kp index, and IMF, for a 28 day moving average (the longest moving average assessed), the decrease in FVC was −173.7 ml (95 % CI: −204.9, −142.6), −26.8 ml (95 % CI: −48, −5.7), and −90.3 ml (95 % CI: −119.5, −61), respectively, and decrease in FEV1 was −116.1 ml (95 % CI: −142.1, −91), −5.2 ml (95 % CI: −21.7, 11.4), and −46.3 ml (95 % CI:−69.8, −22.8). We also observed that an increase in SGA was associated with a slight increase in FEV1/FVC ratio (Table S3, Fig. 3). For an increase in interquartile range of SSN, Kp index, and IMF, for a 28 day moving average, the increase in FEV1/FVC was 0.4 % (95 % CI: −0.1, 0.8), 0.3 % (95 % CI:0,0.6), and 0.4 % (95 % CI: 0,0.8), respectively.
Fig. 2.
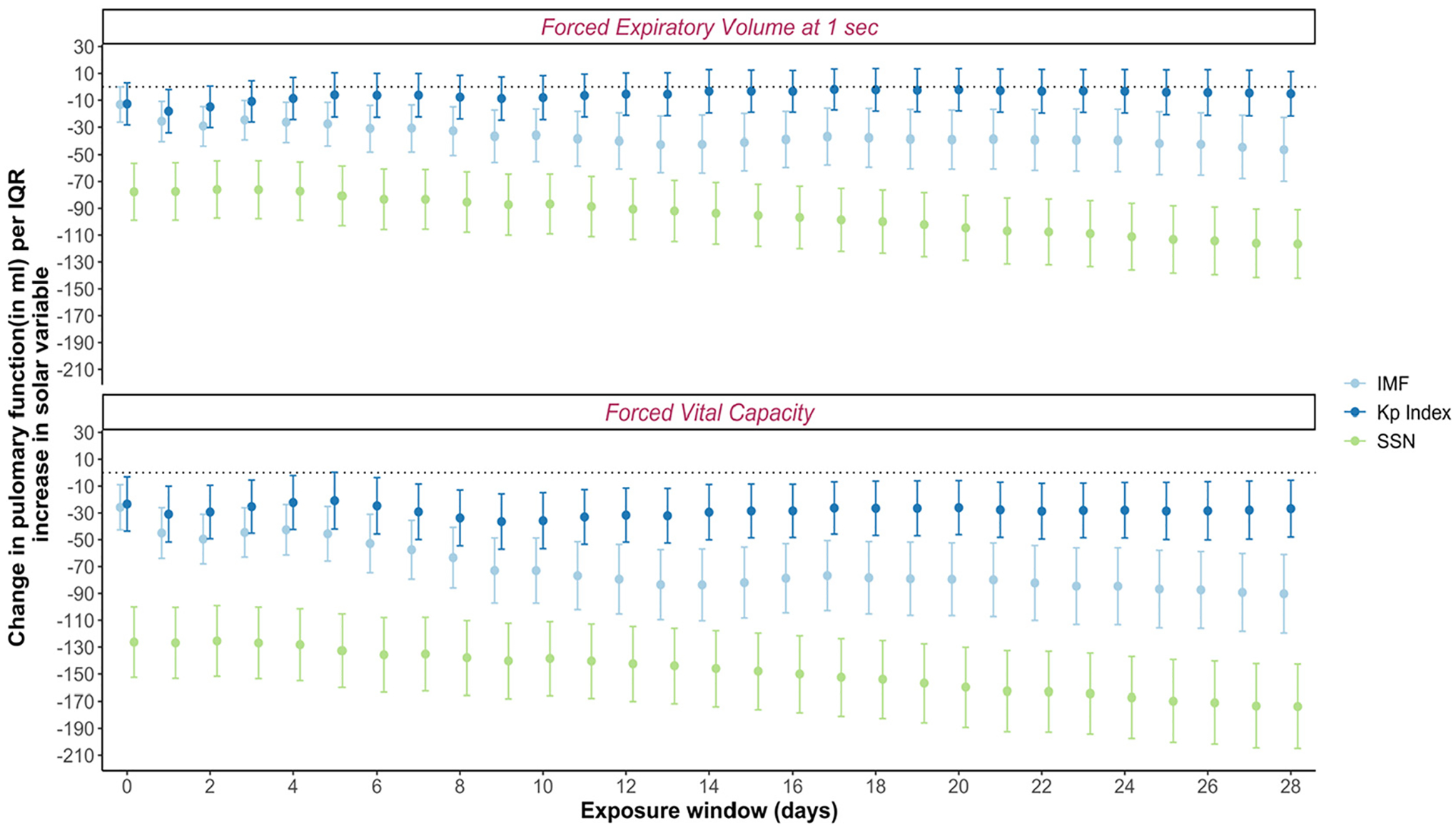
Association of exposure to solar and geomagnetic activity with forced vital capacity (FVC) and forced expiratory volume at 1 s (FEV1). Note: Linear mixed effects models adjusted for age, height, race, selected medication, lifestyle factors (smoking, alcohol), day of the week, seasonality, and medical comorbidities, ambient temperature (°C) and relative humidity (%) on the day of pulmonary function measurement (day 0) were used to estimate the associations (n = 2075). Moving averages calculated starting on day 1 through day 28. Footnote: IMF: Interplanetary Magnetic Field; Kp: Planetary K Index; SSN: Sunspot Number. The IQRs for solar and geomagnetic activity variables are given in Supplementary Material Table S11. The figure is based on the values from Tables S1 and S2 in Supplementary material. Error bars represent the 95 % confidence intervals.
Fig. 3.
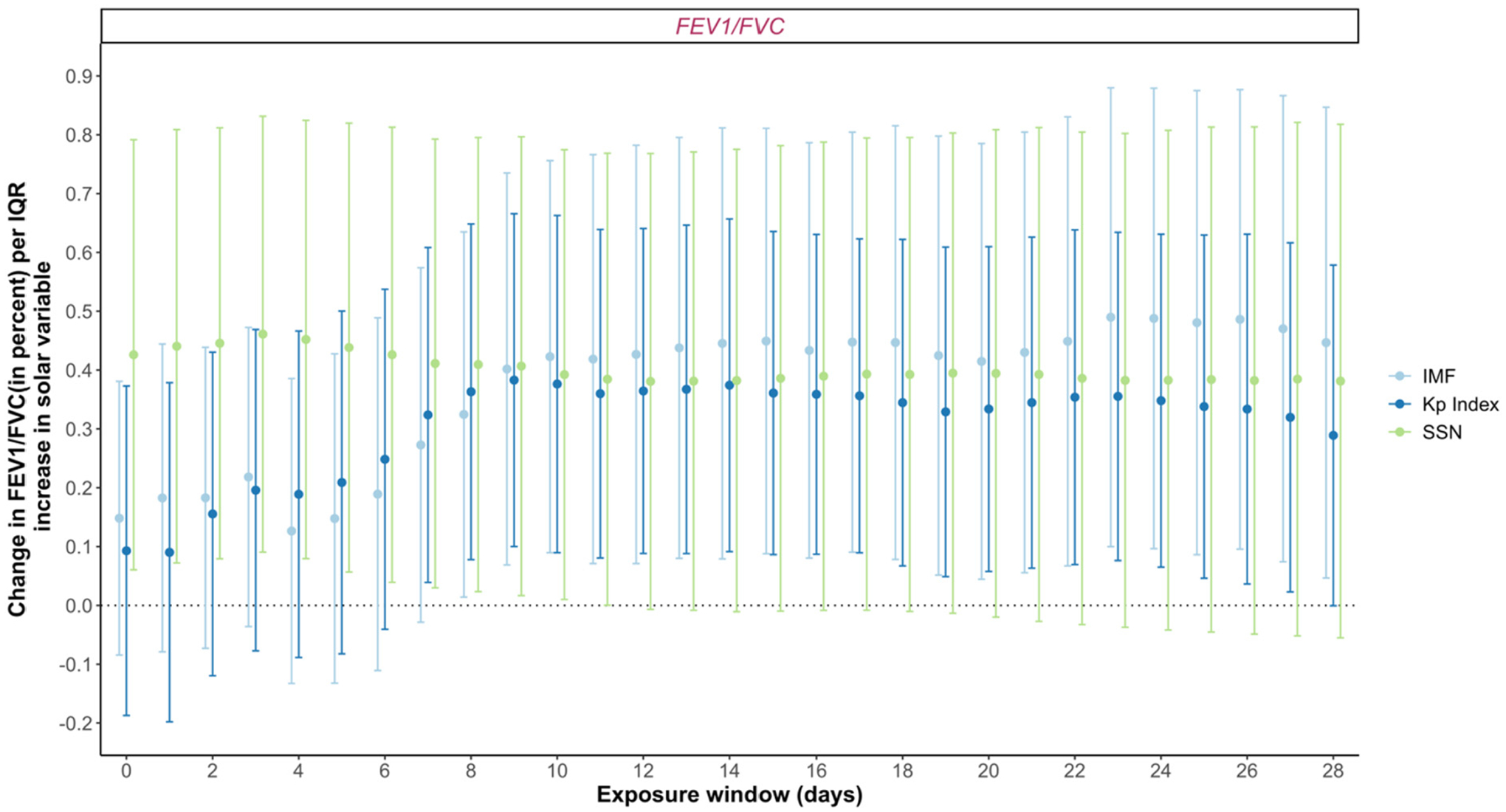
Association of exposure to solar and geomagnetic activity with FEV1/FVC. Note: Linear mixed effects models adjusted for age, race, selected medication, lifestyle factors (smoking, alcohol), day of the week, seasonality, and medical comorbidities, ambient temperature (°C) and relative humidity (%) on the day of pulmonary function measurement (day 0) were used to estimate the associations (n = 2075). Moving averages calculated starting on day 1 through day 28. Footnote: IMF: Interplanetary Magnetic Field; Kp: Planetary K Index; SSN: Sunspot Number; FVC: forced vital capacity;FEV1 forced expiratory volume at 1 s. The IQRs for solar and geomagnetic activity variables are given in Supplementary Material Table S11. The figure is based on the values from Table S3 in Supplementary material. Error bars represent the 95 % confidence intervals.
3.2. Effects of solar and geomagnetic activity on association of particulate air pollution with pulmonary function
As noted by other investigators in other cohorts (Chen et al., 2019; Int Panis et al., 2017; Rice et al., 2013), we found significant negative associations between PM2.5 and BC with of FEV1 and FVC (Supplementary Material Table S4), with a greater effect on FVC. We noted associations with moving averages through day 28 of PM2.5 and BC, with greater adverse effects for longer moving averages. We did not find consistent significant associations between air pollutants and FEV1/FVC (Table S4). We observed significant modification of the effects of particulate pollution on FVC and FEV1 for all SGA parameters across different moving averages, except for the combination of BC and SSN (Supplementary Material Table S5–10). We observed that the interaction between particulate pollution and SGA was associated with a significantly greater decrease in FVC and FEV1 at higher levels of SGA (Figs. 4 and 5).
Fig. 4.
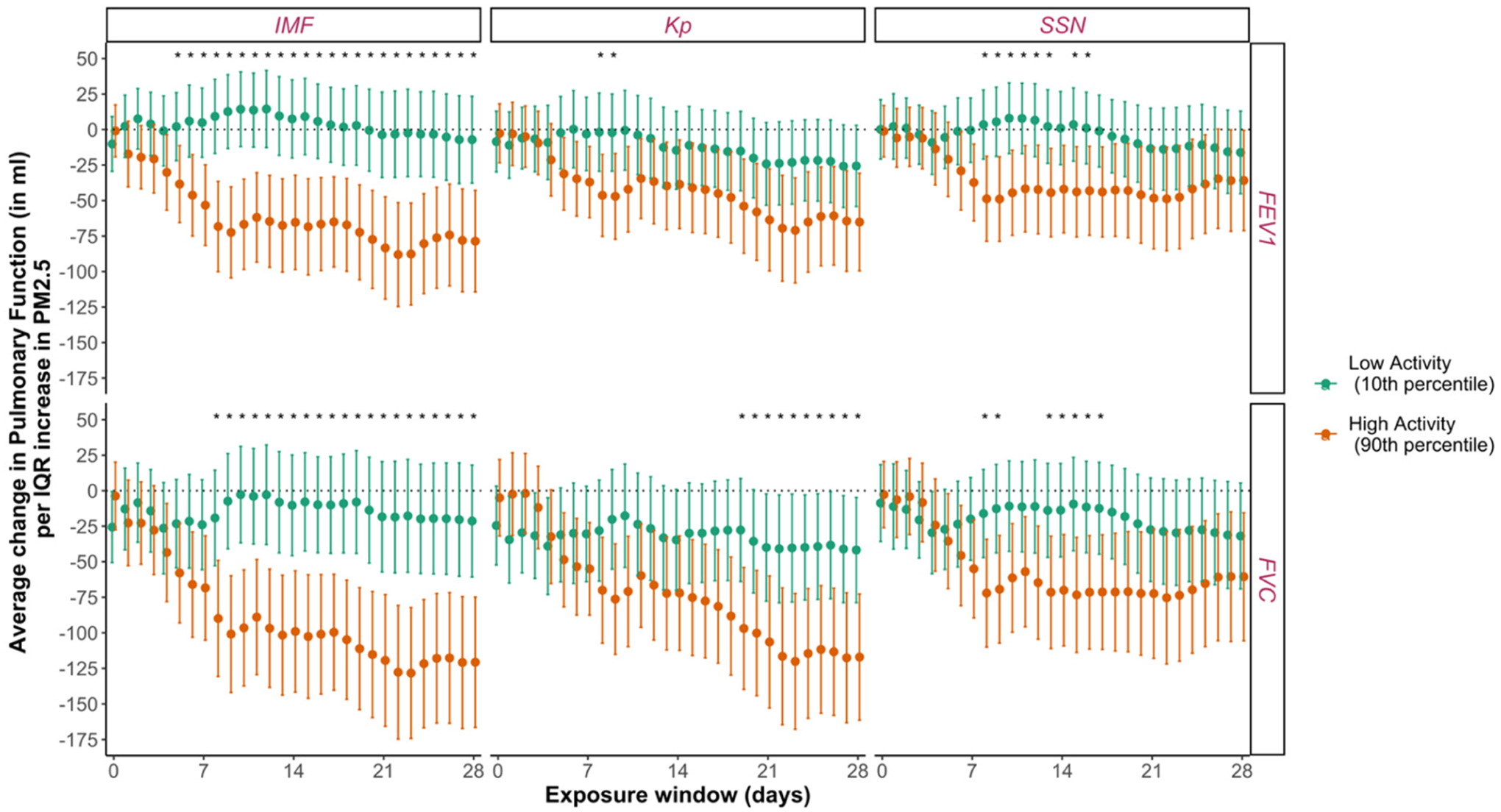
Association of exposure to PM2.5 with forced vital capacity (FVC) and forced expiratory volume at 1 s (FEV1) at high (90th percentile) and low (10th percentile) solar and geomagnetic activity periods. Note: Linear mixed effects models adjusted for age, height, race, selected medication, lifestyle factors (smoking, alcohol), day of the week, seasonality, and medical comorbidities, ambient temperature and relative humidity on the day of pulmonary function measurement (day 0) were used to estimate the association between exposure to PM2.5 and pulmonary function at 10th and 90th percentile of solar and geomagnetic activity parameters (n = 2075). Moving averages calculated starting on day 1 through day 28. Error bars represent the 95 % confidence intervals. Footnote: PM2.5 (particulate matter <2.5μm in aerodynamic diameter); IMF (interplanetary magnetic field); Kp Index (planetary K index); SSN (sunspot number). Asterisks indicate the p-value for interaction term between air pollutant and solar activity parameters with “*” for significant at <0.05 level. 90th percentile and 10th percentile for day zero of all exposure variables are given in Table 2. The IQRs for PM2.5 are given in Supplementary Material Table S11. The figure is based on the values from Table S5, S7, and S9 in Supplementary material.
Fig. 5.
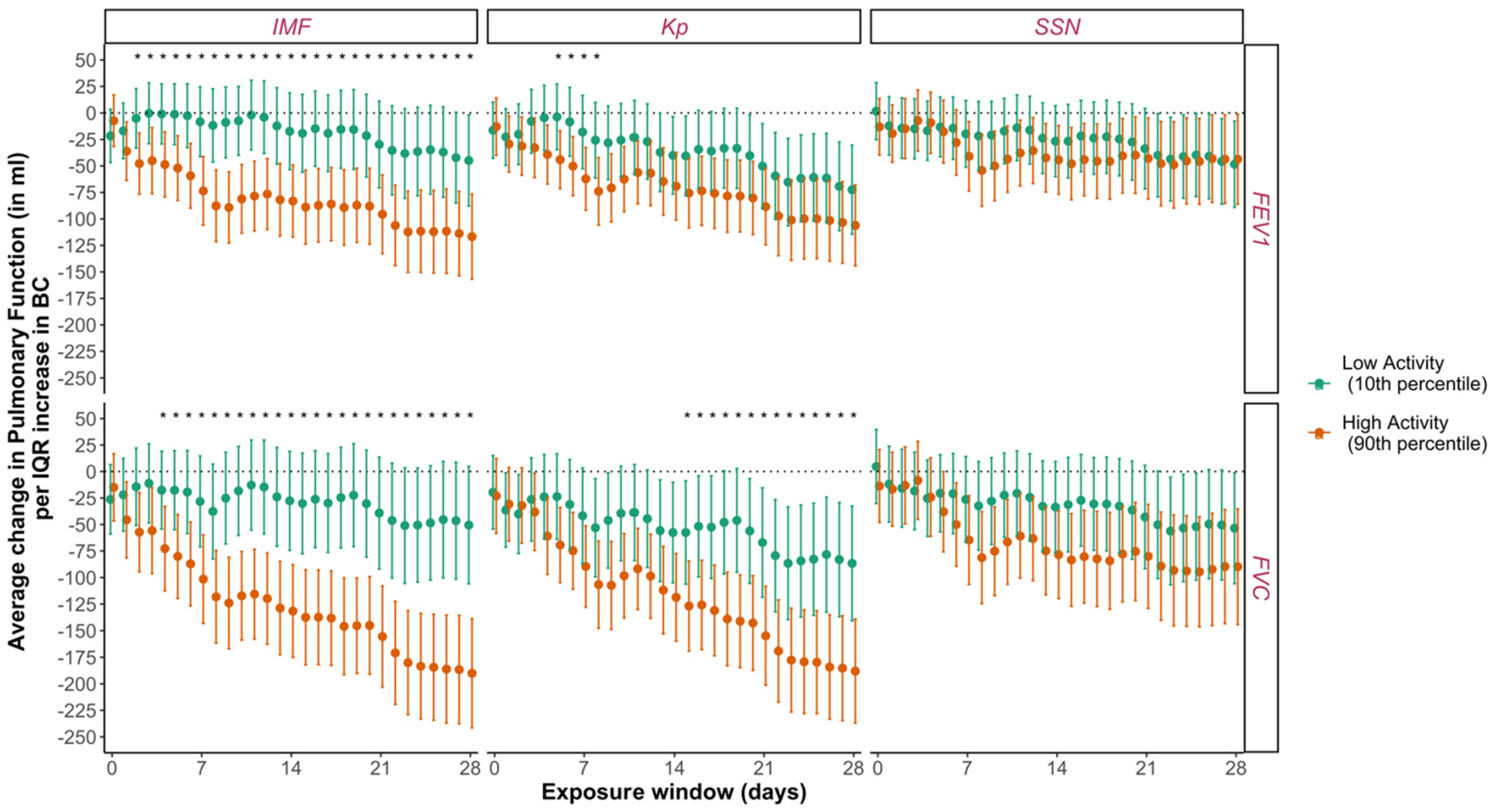
Association of exposure to black carbon (BC) with forced vital capacity (FVC) and forced expiratory volume at 1 s (FEV1) at high (90th percentile) and low (10th percentile) solar and geomagnetic activity periods. Note: Linear mixed effects models adjusted for age, height, race, selected medication, lifestyle factors (smoking, alcohol), day of the week, seasonality, and medical comorbidities, ambient temperature and relative humidity on the day of pulmonary function measurement (day 0) were used to estimate the association between exposure to black carbon and pulmonary function at 10th and 90th percentile of solar and geomagnetic activity parameters (n = 2075). Moving averages calculated starting on day 1 through day 28. Error bars represent the 95 % confidence intervals. Footnote: BC (black carbon); IMF (interplanetary magnetic field); Kp Index (planetary K index); SSN (sunspot number). Asterisks indicate the p-value for interaction term between air pollutant and solar activity parameters with “*” for significant at <0.05 level. 90th percentile and 10th percentile for day zero of all exposure variables are given in Table 2. The IQRs for BC are given in Supplementary Material Table S11. The figure is based on the values from Table S6, S8, and S10 in Supplementary material.
The magnitude of effect modification is shown as the difference in effect estimates between the 10th and 90th percentile values of SGA parameters (green and orange bars in the figure). We noted significantly greater decrements in FVC and FEV1 during periods of increased activity (90th percentile), while smaller decrements that were not statistically significant were observed during periods of decreased activity (10th percentile). The effect estimates tended to be associated with larger decrements in pulmonary function with an increase in cumulative exposure. An IQR (4.55 μg/m3) increase in average exposure 28 days prior to examination to PM2.5 during low IMF (10th percentile: 3.2 nT) over the same time period was associated with a −21.4 ml (95 % CI: −60.8, 18.1) and −7.1 ml (95 % CI:−37.7, 23·4) decrease in FVC and FEV1, respectively, whereas an equivalent increase in PM2.5 during high IMF (90th percentile: 9.0 nT) was significantly (p < 0·001) associated with a −120.7 ml (95 % CI:−166.5, −74.9) and −78.6 ml (95 % CI: −114.3, −42·8) decrease in FVC and FEV1. Kp Index and SSN also appeared to modify effects of air pollution exposure on FVC and FEV1, although with overlapping confidence intervals for effects at the 10th and 90th percentiles of BC and PM2.5. The directions of the interactions between PM2.5 and BC with SGA on FEV1/FVC were inconsistent and nearly all were not significant (Table S12, S13).
4. Discussion
We found a significant decrease in pulmonary function associated with solar and geomagnetic activity with greater decrements for longer moving averages. All the three SGA parameters studied were associated with lower pulmonary function and a greater FEV1/FVC. The greater effect on FVC compared to FEV1 is consistent with a restrictive ventilatory defect attributable to SGA. Our study also explored interactions between SGA parameters and particulate air pollution to assess the concomitant impact of both exposures. We noted a greater impact of PM2.5 and BC on a reduction in FVC and FEV1 (but not FEV1/FVC) during the periods of increased SGA, suggesting that solar and geomagnetic activity modifies the association of PM2.5 and BC on FVC and FEV1. The magnitude of effect modification and of the temporality of interactions with PM2.5 and BC varied based on SGA parameter, but the overall direction of the effect was similar for all interactions. As with other studies of the association between particulate pollution and pulmonary function, we also found an association between exposure and a reduction in FVC and FEV1.. Our findings are consistent with other cohorts (Rice et al., 2015; Rice et al., 2013), where associations between particulate pollution and FEV1/FVC have been weak or inconsistent.
One of the challenges faced by the researchers examining the influence of solar activity on human health has been establishing plausible biological mechanisms to explain the associations. Evidence suggests association of SGA with disruption of 24-h circadian rhythm (Riganello et al., 2019) and autonomic nervous system imbalance (McCraty et al., 2017). Solar radiation regulates the circadian rhythm through suprachiasmatic nucleus (SCN) located in the hypothalamus (central clock) (Reppert and Weaver, 2001). Studies suggest disruption of circadian rhythm and dysregulation of autonomic nervous system could result in higher immune and inflammatory responses, as well as cell damage, which may be finally leading to impairment of lung function and development of lung diseases (Aquino-Santos et al., 2020; Benedusi et al., 2021; Comas et al., 2017; Sundar et al., 2015). Reduced secretion of melatonin, a hormone secreted by pineal gland that regulates the sleep wake cycle and circadian rhythm, has also been linked to solar activity (Burch et al., 1999). Melatonin has shown ability to scavenge free radicals which protects against the effects of harmful radiations (Goswami and Haldar, 2015). Reduced melatonin may increase the oxidative stress increasing pulmonary inflammation and damaged lung cells (Bargagli et al., 2009).
Mechanistic studies explaining the association between particulate air pollution and reduced pulmonary function suggest that exposure can promote small airway remodelling, pulmonary inflammation, cellular changes in immune function, ANS imbalance (Gangwar et al., 2020; Lodovici and Bigagli, 2011; Thurston et al., 2020). These mechanisms suggest that it is biologically plausible that particulate air pollution might be synergistically contributing towards decreased lung function during periods of increased solar activity. Melatonin has been known to mitigate the pathophysiologic responses to air pollution(Carvalho-Sousa et al., 2020; He, 2020; He et al., 2018, 2021); however, it is possible that a reduction in melatonin linked to solar activity can leave individuals more susceptible to the effects of air pollution. Increased ROS generation due to either of the exposures might eventually exacerbates the body’s response to the other. Although the correlation between solar activity with PM2.5 and BC was weak in this study, solar activity also interacts chemically with environmental factors such as air pollution in the atmosphere, which leads to formation of secondary pollutants and aerosols. Discrepancies in the electrical gradient in the atmosphere during periods of intense solar activity can ionize air pollutants and alter the physical and chemical properties (e.g., nature, composition, and toxicity) (Madronich and Flocke, 1999; Mironova et al., 2011; Rycroft et al., 2000). Solar activity has been known to enhance ultrafine particles (Zilli Vieira and Koutrakis, 2021). Therefore, the results corroborate our research hypothesis, which suggests a mechanistic overlap in biology and atmospheric chemistry in the reduction of pulmonary function linked to interactions between solar activity and air pollution.
To the best of our knowledge, this is the first study to investigate the association of pulmonary function with SGA and its interaction with air pollution. We were unable to capture more than one solar cycle due to constraints in availability of data, a more robust association would be possible by considering two solar cycles (22 years). We did not account for exposures other than the measured outdoor exposures (e.g., indoor, and occupational exposures, indoor radiation could not be included). Our study was conducted in a well characterized cohort based in and around Boston with low air pollution levels and relatively high solar radiations (due to high latitude). Association was observed after controlling for a comprehensive list of potential confounders; however, residual confounding remains possible. The NAS population is homogenous composed of healthier elderly white men; therefore, results of the study may not be generalizable to other populations.
These findings suggest that natural phenomena related to solar activity and GMD influence pulmonary function. Our exposure model indicates that these effects may be particularly detrimental during periods of high air pollution. This observation suggests that efforts to mitigate particulate pollution exposures may have more impact when solar disturbances are highest. Our findings also have important public health implications particularly in vulnerable populations such as the elderly since SGA exposures cannot be avoided and exposure to ambient pollution is common (Bentayeb et al., 2012; Simoni et al., 2015).Accounting for SGA in air pollution studies can also help better analyse and understand environmental factors that contribute to impaired lung function.
5. Conclusion
This study demonstrates periods of intense solar activity and geomagnetic disturbances impair lung function. Ambient air pollution and solar radiation might be synergistically contributing towards decreased lung function through biological pathways including increased systemic inflammation, autonomic nervous system imbalance, and reduced melatonin secretion. The chemical pathways of interaction include increased aerosol formation and alteration of the chemical composition of pollutants in the atmosphere. Further studies are required to extend the results across various regions and populations consisting of women, other age groups, race, co-morbidities, varied air pollution levels, geospatial and temporal scales to strengthen the understanding of such interactions in the atmosphere and its underlying biological mechanism. Future research may be able to identify local variations of solar radiation spectra which can have different impacts on human health, including respiratory diseases.
Supplementary Material
HIGHLIGHTS.
First study to analyse the impact of solar and geomagnetic activity (SGA) on lungs.
Intense SGA may contribute to impaired pulmonary function.
Higher SGA promotes adverse effects of particulate pollution on pulmonary function.
Air pollution mitigation may be more impactful when SGA is high.
Acknowledgement
The VA Normative Aging Study is supported by the Cooperative Studies Program/Epidemiology Research and Information Center of the U.S. Department of Veterans Affairs and is a component of the Massachusetts Veterans Epidemiology Research and Information Center (MAVERIC), Boston, Massachusetts. This publication was made possible by U.S. EPA grant RD-835872. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the U.S. EPA. Further, US EPA does not endorse the purchase of any commercial products or services mentioned in the publication. This study was also supported by NIH National Institute of Environmental Health Sciences R21 ES029637 and by resources and the use of facilities at the Veterans Affairs Boston Healthcare System. The views expressed in this article are those of the authors and do not reflect the position or policy of the Department of Veterans Affairs or the United States government.
Abbreviations:
- SD
Standard Deviation
- BMI
Body Mass Index
- PM2.5
Particulate Matter with aerodynamic diameter <2.5 μm
- BC
Black Carbon
- FEV1
Forced Expiratory Volume at 1 s
- FVC
Forced Vital Capacity
- Kp Index
Planetary K Index
- IMF
Interplanetary Magnetic Field
- SSN
Sunspot Number
- SGA
Solar and Geomagnetic Activity
- GMD
Geomagnetic Disturbance
- IQR
Interquartile Range
- CI
Confidence Intervals
- NAS
Normative Aging Study
- ROS
Reactive Oxidative Species
- ANS
Autonomic Nervous System
- CRY
Cryptochrome
Footnotes
CRediT authorship contribution statement
KA was involved in conceptualization, developing methodology and conducted the formal analysis, visualization and wrote the original draft. CLZV, EG and PK were involved in conceptualization, developing methodology and supervision. VW provided data curation and software related assistance. All authors edited and approved the final version of the manuscript.
Ethics committee approval
The study obtained informed consent from the participants and approval from the Institutional Review Boards of Harvard T.H. Chan School of Public Health and VA Boston Healthcare System.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2022.156434.
Data sharing
Individual participant data and data dictionary will not be available for sharing.
References
- Aquino-Santos HC, Tavares-Vasconcelos JS, Brandão-Rangel MAR, Araújo-Rosa AC, Morais-Felix RT, Oliveira-Freitas S, Santa-Rosa FA, Oliveira LVF, Bachi ALL, Alves TGG, Frade-Barros AF, Frison CR, Vieira RP, 2020. Chronic alteration of circadian rhythm is related to impaired lung function and immune response. Int. J. Clin. Pract 74 (10), e13590. 10.1111/ijcp.13590. [DOI] [PubMed] [Google Scholar]
- Bargagli E, Olivieri C, Bennett D, Prasse A, Muller-Quernheim J, Rottoli P, 2009. Oxidative stress in the pathogenesis of diffuse lung diseases: a review. Respir. Med 103 (9), 1245–1256. 10.1016/j.rmed.2009.04.014. [DOI] [PubMed] [Google Scholar]
- Bell B, Rose CL, Damon A, 1972. The normative aging study: an interdisciplinary and longitudinal study of health and aging. Aging Hum. Dev 3 (1), 5–17. 10.2190/GGVP-XLB5-PC3N-EF0G. [DOI] [Google Scholar]
- Benedusi M, Frigato E, Bertolucci C, Valacchi G, 2021. Circadian deregulation as possible new player in pollution-induced tissue damage. Atmosphere 12 (1), 116. 10.3390/atmos12010116. [DOI] [Google Scholar]
- Bentayeb M, Simoni M, Baiz N, Norback D, Baldacci S, Maio S, Viegi G, Annesi-Maesano I, Geriatric Study in Europe on Health Effects of Air Quality in Nursing Homes Group, 2012. Adverse respiratory effects of outdoor air pollution in the elderly. Int. J. Tuberculosis Lung Dis 16 (9), 1149–1161. 10.5588/ijtld.11.0666. [DOI] [PubMed] [Google Scholar]
- Burch JB, Reif JS, Yost MG, 1999. Geomagnetic disturbances are associated with reduced nocturnal excretion of a melatonin metabolite in humans. Neurosci. Lett 266 (3), 209–212. 10.1016/S0304-3940(99)00308-0. [DOI] [PubMed] [Google Scholar]
- Carvalho-Sousa CE, Pereira EP, Kinker GS, Veras M, Ferreira ZS, Barbosa-Nunes FP, Martins JO, Saldiva PHN, Reiter RJ, Fernandes PA, da Silveira Cruz-Machado S, Markus RP, 2020. Immune-pineal axis protects rat lungs exposed to polluted air. J. Pineal Res 68 (3), e12636. 10.1111/jpi.12636. [DOI] [PubMed] [Google Scholar]
- Chen J-L, Zhao J, 2014. A study of short-period variation in solar activity. Res. Astron. Astrophys 14 (8), 1011–1018. 10.1088/1674-4527/14/8/011. [DOI] [Google Scholar]
- Chen C-H, Wu C-D, Chiang H-C, Chu D, Lee K-Y, Lin W-Y, Yeh J-I, Tsai K-W, Guo Y-LL, 2019. The effects of fine and coarse particulate matter on lung function among the elderly. Sci. Rep 9 (1), 14790. 10.1038/s41598-019-51307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas M, Gordon CJ, Oliver BG, Stow NW, King G, Sharma P, Ammit AJ, Grunstein RR, Phillips CL, 2017. A circadian based inflammatory response – implications for respiratory disease and treatment. Sleep Sci. Pract 1 (1), 18. 10.1186/s41606-017-0019-2. [DOI] [Google Scholar]
- Cornélissen G, Halberg F, Sothern RB, Hillman DC, Siegelová J, 2010. Blood pressure, heart rate and melatonin cycles synchronization with the season, earth magnetism and solar flares. Scr. Med 83 (1), 16–32. [PMC free article] [PubMed] [Google Scholar]
- Davis GE, Lowell WE, 2004. Chaotic solar cycles modulate the incidence and severity of mental illness. Med. Hypotheses 62 (2), 207–214. 10.1016/j.mehy.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Dimitrova S, Mustafa FR, Stoilova I, Babayev ES, Kazimov EA, 2009. Possible influence of solar extreme events and related geomagnetic disturbances on human cardiovascular state: results of collaborative Bulgarian-Azerbaijani studies. Adv. Space Res 43 (4), 641–648. 10.1016/j.asr.2008.09.006. [DOI] [Google Scholar]
- OMNIWeb Data Explorer, n.d.OMNIWeb Data Explorer (n.d.). https://omniweb.gsfc.nasa.gov/form/dx1.html. Accessed 4 Apr. 2022.
- Feigin VL, Parmar PG, Barker-Collo S, Bennett DA, Anderson CS, Thrift AG, Stegmayr B, Rothwell PM, Giroud M, Bejot Y, Carvil P, Krishnamurthi R, Kasabov N, 2014. Geomagnetic storms can trigger stroke. Stroke 45 (6), 1639–1645. 10.1161/STROKEAHA.113.004577. [DOI] [PubMed] [Google Scholar]
- Gangwar RS, Bevan GH, Palanivel R, Das L, Rajagopalan S, 2020. Oxidative stress pathways of air pollution mediated toxicity: recent insights. Redox Biol 34, 101545. 10.1016/j.redox.2020.101545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goswami S, Haldar C, 2015. Melatonin as a possible antidote to UV radiation induced cutaneous damages and immune-suppression: an overview. J. Photochem. Photobiol. B Biol 153, 281–288. 10.1016/j.jphotobiol.2015.10.006. [DOI] [PubMed] [Google Scholar]
- Hathaway DH, 2015. The solar cycle. Living Rev. Sol. Phys 12 (1), 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Linchen, 2020. The Role of Melatonin in Pathophysiologic Responses to Air Pollution Exposure. Retrieved fromDuke University. https://hdl.handle.net/10161/22167.
- He L, Cui X, Xia Q, Li F, Xiang J, Fang L, Chung MK, Day D, Mo J, Gong J, Zhang Y, Zhang J.(Jim), 2018. The Effects of Melatonin on the Relationship Between Air Pollution Levels and Biomarkers of Oxidative Stress and Platelet Activation in Healthy Young Adults. ISEE Conference Abstracts. 10.1289/isesisee.2018.P01.0770. [DOI] [Google Scholar]
- He L, Norris C, Cui X, Li Z, Barkjohn KK, Teng Y, Fang L, Lin L, Wang Q, Zhou X, Hong J, Li F, Zhang Y, Schauer JJ, Black M, Bergin MH, Zhang J.(Jim), 2021. Role of endogenous melatonin in pathophysiologic and oxidative stress responses to personal air pollutant exposures in asthmatic children. Science of The Total Environment 773, 145709. 10.1016/j.scitotenv.2021.145709. [DOI] [PubMed] [Google Scholar]
- Int Panis L, Provost EB, Cox B, Louwies T, Laeremans M, Standaert A, Dons E, Holmstock L, Nawrot T, De Boever P, 2017. Short-term air pollution exposure decreases lung function: a repeated measures study in healthy adults. Environ. Health 16 (1), 60. 10.1186/s12940-017-0271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepeule J, Litonjua AA, Coull B, Koutrakis P, Sparrow D, Vokonas PS, Schwartz J, 2014. Long-term effects of traffic particles on lung function decline in the elderly. Am. J. Respir. Crit. Care Med 190 (5), 542–548. 10.1164/rccm.201402-0350OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lodovici M, Bigagli E, 2011. Oxidative stress and air pollution exposure. J. Toxicol 2011, e487074. 10.1155/2011/487074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madronich S, Flocke S, 1999. The role of solar radiation in atmospheric chemistry. In: Boule P (Ed.), Environmental Photochemistry. Springer, pp. 1–26 10.1007/978-3-540-69044-3_1. [DOI] [Google Scholar]
- McCraty R, Atkinson M, Stolc V, Alabdulgader AA, Vainoras A, Ragulskis M, 2017. Synchronization of human autonomic nervous system rhythms with geomagnetic activity in human subjects. Int. J. Environ. Res. Public Health 14 (7), 770. 10.3390/ijerph14070770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CPM, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, ATS/ERS Task Force, 2005. Standardisation of spirometry. Eur. Respir. J 26 (2), 319–338. 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- Mironova IA, Usoskin IG, Kovaltsov GA, Petelina SV, 2011. Possible effect of extreme solar energetic particle event of 20 January 2005 on polar stratospheric aerosols: Direct observational evidence. [Preprint]Aerosols/Remote Sensing/Stratosphere/Physics (Physical Properties and Processes) 10.5194/acpd-11-14003-2011. [DOI]
- National Centers for Environmental Information (NCEI), n.d.National Centers for Environmental Information (NCEI) (n.d.). https://www.ncei.noaa.gov/. Accessed 4 Apr. 2022.
- Reppert SM, Weaver DR, 2001. Molecular analysis of mammalian circadian rhythms. Annu. Rev. Physiol 63 (1), 647–676. 10.1146/annurev.physiol.63.1.647. [DOI] [PubMed] [Google Scholar]
- Rice MB, Ljungman PL, Wilker EH, Gold DR, Schwartz JD, Koutrakis P, Washko GR, O’Connor GT, Mittleman MA, 2013. Short-term exposure to air pollution and lung function in the Framingham heart study. Am. J. Respir. Crit. Care Med 188 (11), 1351–1357. 10.1164/rccm.201308-1414OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice MB, Ljungman PL, Wilker EH, Dorans KS, Gold DR, Schwartz J, Koutrakis P, Washko GR, O’Connor GT, Mittleman MA, 2015. Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am. J. Respir. Crit. Care Med 191 (6), 656–664. 10.1164/rccm.201410-1875OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riganello F, Prada V, Soddu A, di Perri C, Sannita WG, 2019. Circadian rhythms and measures of CNS/autonomic interaction. Int. J. Environ. Res. Public Health 16 (13), 2336. 10.3390/ijerph16132336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rycroft MJ, Israelsson S, Price C, 2000. The global atmospheric electric circuit, solar activity and climate change. J. Atmos. Sol. Terr. Phys 62 (17), 1563–1576. 10.1016/S1364-6826(00)00112-7. [DOI] [Google Scholar]
- Simoni M, Baldacci S, Maio S, Cerrai S, Sarno G, Viegi G, 2015. Adverse effects of outdoor pollution in the elderly. J. Thoracic Dis 7 (1), 34–45. 10.3978/j.issn.2072-1439.2014.12.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solanki SK, 2003. Sunspots: an overview. Astron. Astrophys. Rev 11 (2), 153–286. 10.1007/s00159-003-0018-4. [DOI] [Google Scholar]
- Sparrow D, O’Connor G, Colton T, Barry CL, Weiss ST, 1987. The relationship of nonspecific bronchial responsiveness to the occurrence of respiratory symptoms and decreased levels of pulmonary function. The normative aging study. Am. Rev. Respir. Dis 135 (6), 1255–1260. 10.1164/arrd.1987.135.6.1255. [DOI] [PubMed] [Google Scholar]
- Sundar IK, Yao H, Sellix MT, Rahman I, 2015. Circadian molecular clock in lung path-ophysiology. Am. J. Phys. Lung Cell. Mol. Phys 309 (10), L1056–L1075. 10.1152/ajplung.00152.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- “The Kp-Index|Help”, n.d. “The Kp-Index|Help” (n.d.) SpaceWeatherLive.Com, https://spaceweatherlive.com/en/help/the-kp-index.html. Accessed 4 Apr. 2022.
- Thurston GD, Balmes JR, Garcia E, Gilliland FD, Rice MB, Schikowski T, Van Winkle LS, Annesi-Maesano I, Burchard EG, Carlsten C, Harkema JR, Khreis H, Kleeberger SR, Kodavanti UP, London SJ, McConnell R, Peden DB, Pinkerton KE, Reibman J, White CW, 2020. Outdoor air pollution and new-onset airway disease. An official American Thoracic Society workshop report. Ann. Am. Thoracic Soc 17 (4), 387–398. 10.1513/AnnalsATS.202001-046ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy SM, Vieira CLZ, Garshick E, Wang VA, Alahmad B, Eid R, Schwartz J, Schiff JE, Vokonas P, Koutrakis P, 2022. Associations between solar and geomagnetic activity and peripheral white blood cells in the normative aging study. Environ. Res 204, 112066. 10.1016/j.envres.2021.112066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang VA, Zilli Vieira CL, Garshick E, Schwartz JD, Garshick MS, Vokonas P, Koutrakis P, 2021. Solar activity is associated with diastolic and systolic blood pressure in elderly adults. J. Am. Heart Assoc 10 (21), e021006. 10.1161/JAHA.120.021006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yermolaev Yu.I., Yermolaev M.Yu., 2010. Solar and interplanetary sources of geomagnetic storms: space weather aspects. Izv. Atmos. Oceanic Phys 46 (7), 799–819. 10.1134/S0001433810070017. [DOI] [Google Scholar]
- Zilli Vieira CL, Koutrakis P, 2021. The impact of solar activity on ambient ultrafine particle concentrations: an analysis based on 19-year measurements in Boston, USA. Environ. Res 201, 111532. 10.1016/j.envres.2021.111532. [DOI] [PubMed] [Google Scholar]
- Zilli Vieira CL, Alvares D, Blomberg A, Schwartz J, Coull B, Huang S, Koutrakis P, 2019. Geomagnetic disturbances driven by solar activity enhance total and cardiovascular mortality risk in 263 U.S. Cities. Environ. Health 18 (1), 83. 10.1186/s12940-019-0516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Individual participant data and data dictionary will not be available for sharing.


