To the Editor: Hidradenitis suppurativa (HS) is a chronic, debilitating inflammatory skin disease characterized by recurrent episodes of inflamed nodules, pustules, and abscesses.1 Physicians often manage patients with HS who have considerable emotional distress from disease burden and reduced quality of life.2 Patients may initially see many physicians who are unfamiliar with HS, resulting in misdiagnosis and diagnostic delays, adding to patients’ frustration and mistrust.3, 4, 5 This study aimed to identify physician perspectives on HS disease management using survey data completed by dermatologists.
This prospective web-based survey study was conducted from December 15, 2020, to January 31, 2021; 30 dermatologists, 6 of whom were HS specialists, were invited, and all completed the survey, for a response rate of 100% (Supplementary Table, available via Mendeley at https://data.mendeley.com/datasets/rnv53crbwg/1). All dermatologists completed a 33-question survey and provided written informed consent prior to participating. Ethics review and data privacy approvals were obtained through a centralized institutional review board.
Data collection was performed using an online platform for dermatologists to complete the survey, which included topics on demographics, treatment and prescribing patterns, and disease awareness. Collected data were analyzed descriptively, and frequency counts and percentages were used to calculate continuous variables. Analyses were conducted by Guidehouse using SAS statistical software or Microsoft Excel.
Dermatologists reported that patients with suspected HS were most often referred to them by primary care providers (50.0%). Hurley staging was identified as the most commonly used (66.7%) measure to assess HS severity (Table I). Most dermatologists (73.3%) felt patients had very low/low understanding of HS at their first visit, and 63.3% identified limited therapeutic options or efficacy of available therapies as top unmet needs for patients with HS. Key factors influencing dermatologists’ treatment decisions included disease severity and insurance coverage. Most dermatologists (96.7%) reported that lack of HS awareness by other physicians was the greatest challenge in diagnosing HS.
Table I.
Dermatologist perspectives on HS patient disease journey
| Characteristic (N = 30)∗ | Patients with HS, n (%) |
|---|---|
| Estimated frequency of referral to dermatologists by physician type, % | n = 19 |
| Primary care | 50.0 |
| Dermatologist | 15.8 |
| General internist | 10.4 |
| Obstetrician/gynecologist | 9.2 |
| Surgeon | 7.4 |
| Pediatrician | 4.7 |
| Urologist | 2.4 |
| Measures used to assess patients for HS† | |
| Hurley staging | 20 (66.7) |
| Pain VAS | 11 (36.7) |
| HS-PGA | 9 (30.0) |
| DLQI | 5 (16.7) |
| None | 5 (16.7) |
| HSSA | 2 (6.7) |
| HiSCR | 2 (6.7) |
| Dermatologist-reported patient understanding of HS at the first visit | |
| Very low | 8 (26.7) |
| Low | 14 (46.7) |
| Average | 7 (23.3) |
| High | – |
| Very high | 1 (3.3) |
| Patient factors affecting dermatologists’ treatment choices† | |
| Disease severity | 29 (96.7) |
| Insurance coverage | 24 (80.0) |
| Comorbidities | 20 (66.7) |
| Age | 18 (60.0) |
| Others‡ | 2 (6.7) |
| Top unmet needs for patients according to dermatologists† | |
| Limited efficacy of available therapies | 19 (63.3) |
| Limited treatment options available | 19 (63.3) |
| High psychological burden of disease | 10 (33.3) |
| Timely diagnosis of HS | 8 (26.7) |
| Dermatologist-identified challenges with diagnosing HS† | |
| Lack of awareness by PCPs/other physicians | 29 (96.7) |
| Inadequate patient access to dermatologists | 18 (60.0) |
| Lack of consensus on diagnostic criteria/tools | 13 (43.3) |
| Difficult to rule out other potential diagnoses | 8 (26.7) |
| Advise patients to discuss their feelings about HS with a trained mental health professional | 13 (43.3) |
DLQI, Dermatology Life Quality Index; HiSCR, HS Clinical Response; HS, hidradenitis suppurativa; HSSA, HS Symptom Assessment; HS-PGA, HS Physician Global Assessment; PCP, primary care provider; VAS, visual analog scale.
N = 30 unless otherwise stated.
Survey participants could select more than one response.
Other factors included the patient’s health literacy, impact on quality of life, and how difficult the patient’s HS is to treat.
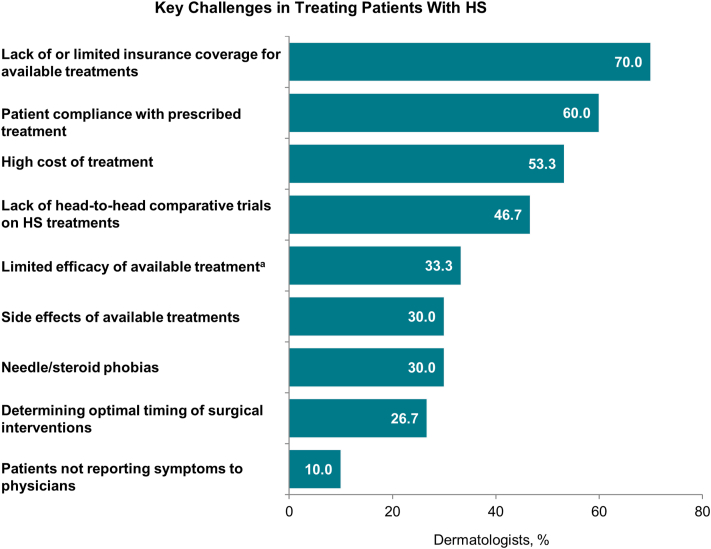
Dermatologists identified limited health insurance coverage of available therapies (70.0%), patient compliance with prescribed treatments (60.0%), and high cost of treatments (53.3%) as key challenges to establishing proper treatment for patients with HS (Fig 1). The most frequently prescribed first-line therapies reported by dermatologists were topical treatments for mild HS and biologics for severe cases (Supplementary Fig 1, available via Mendeley at https://data.mendeley.com/datasets/rnv53crbwg/1). Most dermatologists agreed with being comfortable choosing a second biologic after failure of the first (70%) and with performing or referring a patient for surgical therapy (eg, local excision) while the patient is receiving a biologic (56.7%). One-third of dermatologists (33.3%) reported being comfortable treating HS with dual biologics (Supplementary Fig 2, available via Mendeley at https://data.mendeley.com/datasets/rnv53crbwg/1).
Fig 1.
Dermatologist-reported challenges in treating HS, HS, Hidradenitis suppurativa. aAdalimumab (n = 5), antibiotics (n = 1), biologics (n = 1), doxycycline (n = 1), oral antibiotics (n = 1), and medications may lose efficacy or only give a partial response (n = 1).
Dermatologists reported psychological distress as a major component of the HS patient experience (Supplementary Fig 3, available via Mendeley at https://data.mendeley.com/datasets/rnv53crbwg/1); however, only 43% of dermatologists advised patients to discuss their feelings about HS with a trained professional (Table I). Generalizability of these findings may be limited due to the small sample size and the limited clinical practices represented.
Our study identified key dermatologist-reported challenges in diagnosing and treating HS and substantiated the lack of consistency regarding HS assessment measures. Increased patient and physician awareness and enhanced multidisciplinary care are needed to address unmet needs in HS care.
Conflicts of interest
V.Y. Shi is on the board of directors for the Hidradenitis Suppurativa Foundation (HSF); serves as an advisor for the National Eczema Association; is a stock shareholder of Learn Health; and has served as an advisory board member, investigator, speaker, and/or received research funding from Sanofi Genzyme, Regeneron, AbbVie, Eli Lilly, Novartis, Sun Pharma, LEO Pharma, Pfizer, Incyte, Boehringer Ingelheim, Aristea Therapeutics, Menlo Therapeutics, Dermira, Burt’s Bees, Galderma, Kiniksa, UCB, Target PharmaSolutions, Altus Lab/CQuell, MYOR, Polyfins Techology, GpSkin, and Skin Actives Scientific. J.L. Hsiao is on the board of directors for the HSF and has served as an advisor for Boehringer Ingelheim, Novartis, and UCB and a speaker and advisor for AbbVie. E. Muscianisi and J. Darcy are employees of Novartis Pharmaceuticals Corporation. E. Nguyen is an employee of Novartis Gene Therapies. J.S. Kirby is on the board of directors for the HSF and has served as a speaker for AbbVie; an advisory board member for Novartis and Janssen; an investigator for AbbVie, ChemoCentryx, Incyte, InflaRx, Janssen, Novartis, Pfizer, and UCB; and a consultant for AbbVie, Bayer, ChemoCentryx, CSL Behring, DermTech, InflaRx, Incyte, Novartis, Janssen Pfizer, and UCB.
Acknowledgments
Medical writing support was provided by Charli Dominguez, PhD, CMPP, of Health Interactions, Inc, Chicago, IL, and was funded by Novartis Pharmaceuticals Corporation. This manuscript was developed in accordance with Good Publication Practice (GPP3) guidelines. The authors had full control of the content and made the final decision on all aspects of this publication.
Footnotes
Funding sources: Support for third-party writing assistance for this manuscript was provided by Novartis.
IRB approval status: This study was reviewed and approved by a central institutional review board (WCG IRB; IRB number IRB00000533).
Patient consent: Patients provided written informed consent for use of medical information to be published in print and online prior to participating, and all informed consent forms are on file with the physicians. No patient photographs were collected/used for this study.
References
- 1.Alikhan A., Sayed C., Alavi A., et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81(1):76–90. doi: 10.1016/j.jaad.2019.02.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mac Mahon J., Kirthi S., Byrne N., et al. An update on health-related quality of life and patient-reported outcomes in hidradenitis suppurativa. Patient Relat Outcome Meas. 2020;11:21–26. doi: 10.2147/PROM.S174299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg A., Neuren E., Cha D., et al. Evaluating patients' unmet needs in hidradenitis suppurativa: results from the global survey of impact and healthcare needs (VOICE) project. J Am Acad Dermatol. 2020;82(2):366–376. doi: 10.1016/j.jaad.2019.06.1301. [DOI] [PubMed] [Google Scholar]
- 4.Saunte D.M., Boer J., Stratigos A., et al. Diagnostic delay in hidradenitis suppurativa is a global problem. Br J Dermatol. 2015;173(6):1546–1549. doi: 10.1111/bjd.14038. [DOI] [PubMed] [Google Scholar]
- 5.Kokolakis G., Wolk K., Schneider-Burrus S., et al. Delayed diagnosis of hidradenitis suppurativa and its effect on patients and healthcare system. Dermatology. 2020;236(5):421–430. doi: 10.1159/000508787. [DOI] [PMC free article] [PubMed] [Google Scholar]