Abstract
BACKGROUND & AIMS:
Eosinophilic esophagitis (EoE) is a patchy disease of the esophagus with significant variability in intraepithelial eosinophilia. Three biopsies each from distal and proximal esophagus are recommended for identification of active EoE. Recent work suggests 3 biopsy sites are more optimal. We sought to evaluate 2-site vs 3-site esophageal biopsy combinations for utility to identify active EoE.
METHODS:
We prospectively obtained 3-site esophageal biopsies based on rigorous endoscopic measurements of the proximal, mid, and distal esophagus and gastroesophageal junction. Biopsies were reviewed by a pathologist, and those with at least 15 eosinophils per high-power field were considered active EoE. The sensitivity of one or more sites to identify active EoE was determined, and endoscopic measurements were correlated to height and age.
RESULTS:
Five hundred ninety-six endoscopies were performed in 217 patients; of these, 304 endoscopies in 167 patients had active EoE. Among the initial esophagogastroduodenoscopies with active EoE, distal biopsies had greater than 80% sensitivity, whereas mid and proximal biopsies had sensitivity of 65% and 62%, respectively, and distal + proximal biopsies had the highest diagnostic sensitivity for a 2-site combination. Among the 304 endoscopies with active EoE, 9 had focal eosinophilia restricted to the mid esophagus, and 8 were restricted to the proximal esophagus. For patients with multiple endoscopies with active EoE, nearly one fourth had reduced sites with eosinophilia at the second time point. Endoscopic measurements strongly correlated with height and age.
CONCLUSIONS:
This study supports endoscopic measurement–guided 3-site biopsies for optimal disease assessment of active EoE in children.
Keywords: Eosinophilic Esophagitis, Esophagus, Topography, Inflammation, Sites, Eosinophil
Eosinophilic esophagitis (EoE) is a chronic disease characterized by eosinophil-predominant inflammation of the esophagus.1 EoE is a patchy disease, and assessment of biopsies from multiple locations within the esophagus is valuable for accurate diagnosis.2–5 Multiple endoscopies are often necessary for diagnosis, assessment of the response to treatment, and disease surveillance.1 Consensus guidelines recommend obtaining multiple biopsies from distal and proximal esophagus and are based on previous studies that have used only proximal and distal esophageal biopsy locations. A recent study in adults demonstrated that a protocol obtaining and analyzing biopsies from distal, mid, and proximal esophagus may enhance the diagnostic sensitivity for EoE compared with 2-site biopsy.3 However, a study in children by Chernetsova et al,2 which retrospectively assessed 100 EoE patients, was inconclusive regarding the utility of mid-esophageal biopsies. Thus, the question of 3-site biopsies in children remains.
In a retrospective study, Shah et al4 identified histopathologic variability among biopsy specimens and demonstrated that a total of 6 biopsies from 2 locations achieved 100% diagnostic sensitivity. In a prospective adult study Gonsalves et al5 established that multiple locations are necessary for identification of active EoE, with 5 biopsies required to achieve 100% sensitivity. Major limitation of these studies were the study design, small patient cohort, and lack of standardized assessment of multiple esophageal segments to maximize diagnostic sensitivity. Although most studies examined the proximal and distal esophagus, several recent studies have separated the esophagus into proximal, mid, and distal thirds.6–9 Because the practice of obtaining biopsies from multiple areas of the esophagus varies from center to center, we aimed to compare esophageal biopsies from 3 levels with the currently recommended 2-level biopsy protocols for diagnosis of EoE in children.
Most studies pertaining to esophageal length have been performed with the objective of identifying the location of lower esophageal sphincter for impedance/pH studies.10–12 Several methods have been described to estimate esophageal length by using manometry or radiology.10,12,13 There is only one previous study that used height and endoscopy to assess length of the esophagus in a small cohort of adults.14 Moreau et al13 reported a correlation between height and esophageal length; however, the utility of endoscopic measurements to guide esophageal biopsy in children has not been previously studied.
Our primary objective was to prospectively assess the diagnostic utility of biopsies from proximal, mid, and distal esophageal locations and compare their sensitivity with 2-site biopsies. The secondary aim of this study was to correlate endoscopic measurements of topographical esophageal sites (proximal, mid, distal, gastroesophageal junction [GEJ]) to height and age.
Materials and Methods
Study Design
We performed an analysis of a prospective longitudinal cohort of children, ages 2–17 years, undergoing endoscopy at Ann & Robert H. Lurie Children’s Hospital of Chicago for suspected or previously diagnosed EoE from 2012 to 2016. All endoscopies were performed by a single provider (AFK). Indications for endoscopies ranged from symptoms of esophageal dysfunction such as dysphagia and heartburn to evaluation of response to therapy and annual surveillance in previously diagnosed EoE. Diagnosis of EoE was based on 2011 diagnostic criteria, which were defined as the presence of symptoms of esophageal dysfunction and esophageal eosinophilia (at least 15 eosinophils/high-power field [eos/hpf]) after treatment with high dose proton pump inhibitor.15 A waiver of consent was obtained for this study to consecutively register children undergoing endoscopy for suspected EoE or assessment of disease activity in patients with established EoE. Demographic and medication data were obtained by chart review. This study was approved by the Institutional Review Board of Ann & Robert H. Lurie Children’s Hospital of Chicago, IL (IRB #2011–14486).
Biopsy Acquisition and Analysis
Patients had ≥3 biopsies each from the proximal, mid, and distal esophagus. Landmarks including cricopharyngeus and GEJ were recorded in a standardized operative note along with the endoscopic reference score for each site of the esophagus. Measurements were obtained from the lips to the cricopharyngeus and the GEJ. The proximal esophageal biopsy location was located 3 cm below the cricopharyngeus, the mid esophagus was midpoint between the cricopharyngeus and the GEJ, and the distal esophagus location was 2 cm above the GEJ. Routine pathologist review to determine the peak eosinophil count (eos/hpf) at ×400 was performed. Samples with active EoE (defined as ≥15 eos/hpf in any biopsy) were included in the analysis to determine the utility of biopsies from one or multiple sites in the esophagus.
Statistical Analysis
Statistical analysis was performed with SAS v 9.4 (SAS Institute Inc, Cary, NC) and R version 3.4.3. Peak eosinophil counts among the proximal, mid, and distal esophagus were compared with combinations of 1 or 2 sites. We determined the median and interquartile range of peak eos/hpf per site and for the peak values among the 2- and 3-site combinations. The optimal site was assessed on the basis of the number of 2-site and individual sites that identified active EoE relative to a 3-site combination. The sensitivity, predictive value, and accuracy of 1-, 2-, and 3-site combinations to identify active EoE were determined. Pearson correlation coefficient was performed to determine the association between the endoscopic measurement relative to height and esophageal length (GEJ minus proximal measurement) compared with age.
Results
Patient Characteristics
Of the 596 endoscopies in 217 EoE patients who were enrolled, 167 EoE patients with 304 total endoscopies had active EoE (Figure 1). The mean [standard deviation] age of the cohort was 10 [5] years, and the median [standard deviation] number of endoscopies per patient was 2 [1] (Table 1). The cohort was 76% male, 87% white, and 12% Latinx (Table 1). An average of 12 biopsies was obtained per endoscopy (Table 1). Two hundred seventeen patients underwent 1 or more esophagogastroduodenoscopies and had histology consistent with EoE patients. Among the initial endoscopy captured in the study, more than 50% of patients had edema or furrows, 35% demonstrated exudate, and 28% had rings (Supplementary Table 1). At the time of initial study endoscopy, most patients were on a proton pump inhibitor (80%), and only one fourth (24.4%) were on swallowed topical steroids (Supplementary Table 1). Among the 217 EoE patients, 39% had asthma, 42% had eczema and food allergy, and 58% had rhinitis (Supplementary Table 1).
Figure 1.
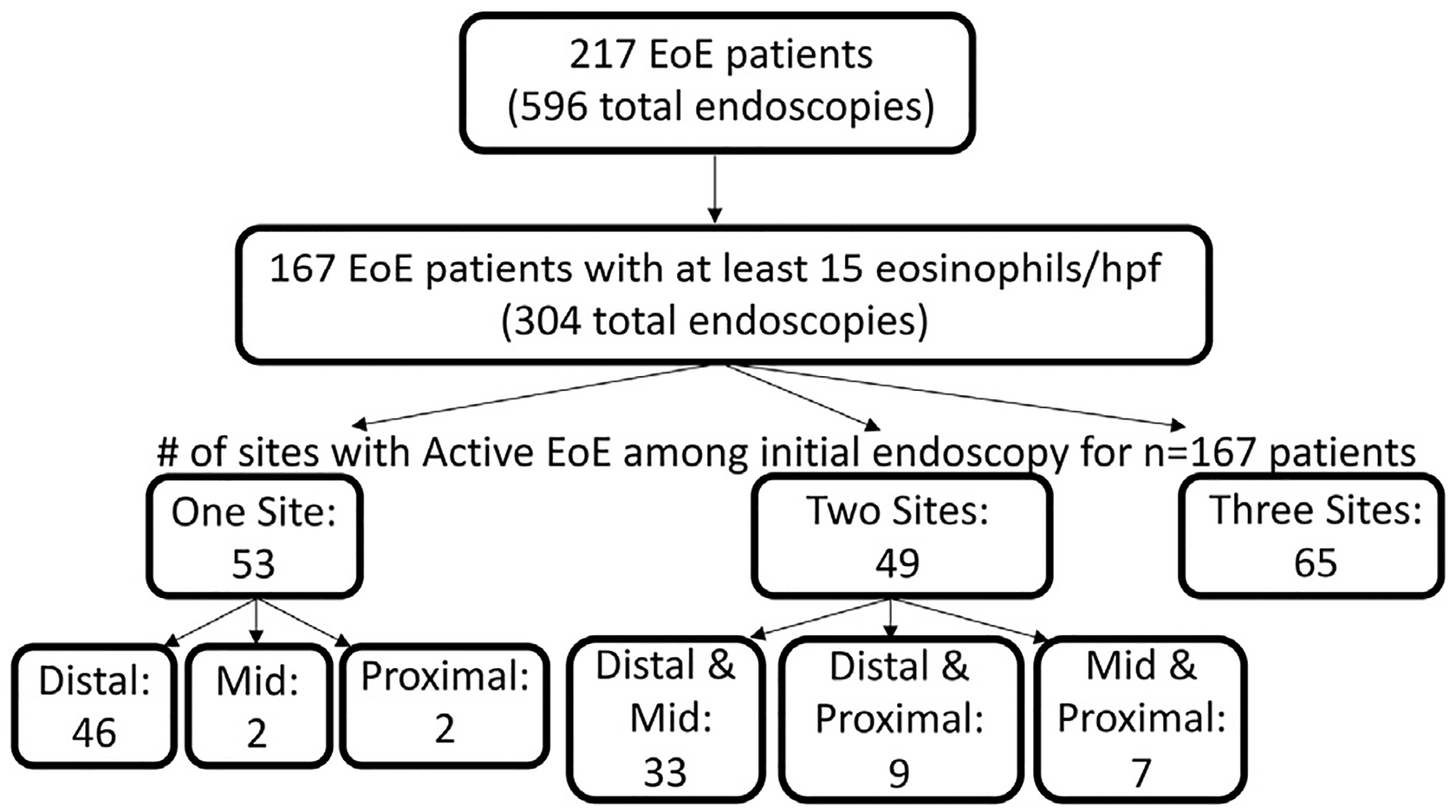
Consort diagram of study subjects. Two hundred seventeen EoE patients had 596 endoscopies between 9/2011 and 1/2017 for which endoscopic measurements of the location of the proximal, mid, and distal esophageal biopsies and gastroesophageal junction were recorded. One hundred sixty-seven of these patients had active EoE during the study period including 304 endoscopies. Among these 167 patients, the number of sites with active EoE (at least 15 eosinophils per high-power field) in the initial endoscopy is noted.
Table 1.
Patient and Endoscopy Characteristics
| Characteristica | |
|---|---|
| Age (y), median ± SD | 10 ± 5 |
| Gender, n (%) | |
| Female | 52 (24) |
| Male | 165 (76) |
| Race/ethnicity, n (%) | |
| White | 188 (87) |
| Black or African American | 12 (6) |
| Asian | 16 (7) |
| Latinx | 26 (12) |
| Endoscopies per patient, median ± SD | 2 ± 1 |
| No. of biopsies, median ± SD | |
| Distal esophagus | 4 ± 1 |
| Mid esophagus | 4 ± 1 |
| Proximal esophagus | 4 ± 1 |
SD, standard deviation.
n = 217 EoE patients/596 endoscopies.
Extent of Eosinophilia in Individual and Combinations of Biopsy Sites
We next examined the extent and distribution of eosinophilia among individual biopsy sites in the cohort (n = 167) of patients whose biopsies met criteria for active EoE. We found significant heterogeneity in the distribution of eosinophils, with many patients with eosinophilia in multiple locations, but many with just distal eosinophilia (Figure 1). Few had isolated mid or proximal eosinophilia.
Relationship of Endoscopy Measurement to Height and Age
The relationship of endoscopic measurement for each topographical esophageal site (proximal, mid, distal, GEJ) to height for each patient was next assessed. We found a very strong relationship with the proximal (r = 0.67, P < .001), mid (r = 0.89, P < .001), and distal (r = 0.94, P < .001) esophagus, and GEJ (r = 0.95, P < .001) (Figure 2). In addition, we assessed the relationship of esophageal length, calculated by subtracting the proximal esophagus and GEJ measurements, with age. We found a strong relationship between esophageal length and age (r = 0.83, P < .001). This validated the rigor to our topographical approach to map the eosinophil density of each third of the esophagus and provides a pediatric guide to esophageal length by age.
Figure 2.
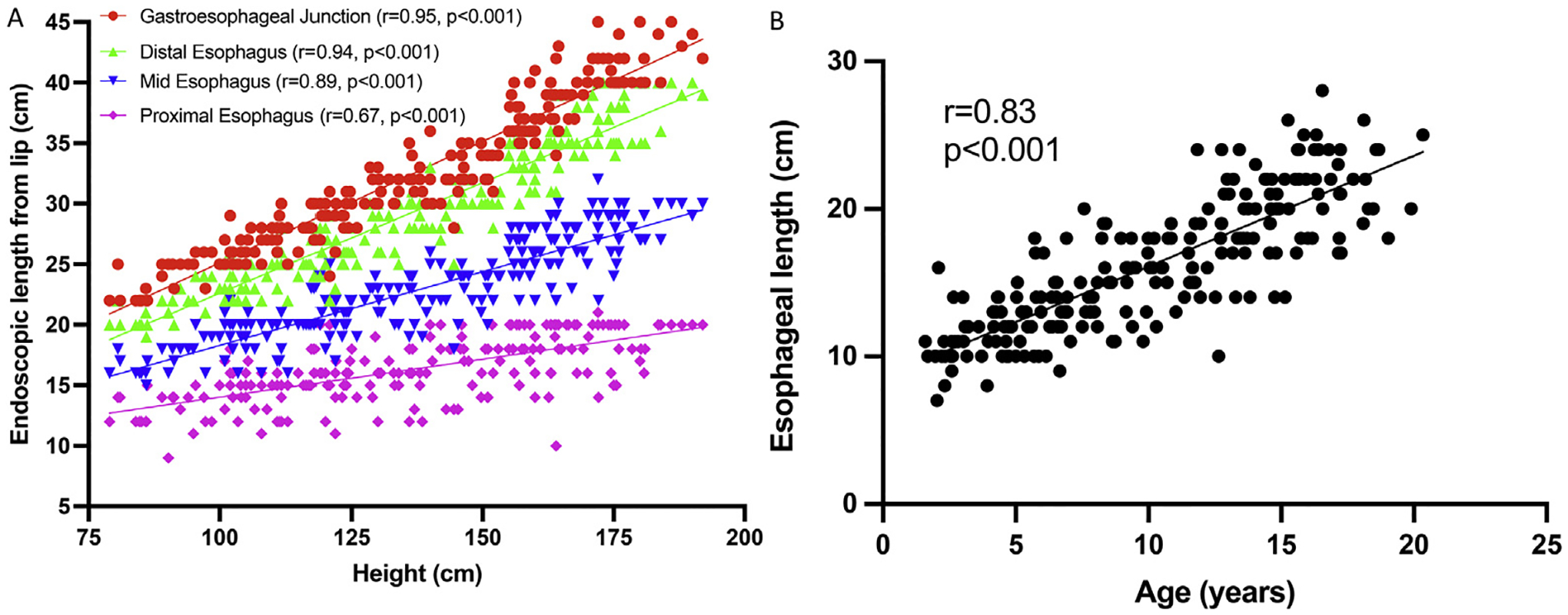
Correlation of endoscopic measurements. (A) Correlation of endoscopic length from lip (cm) with patient height (cm) in N = 217 patients. (B) Correlation of esophagus length (cm, difference between measurement at gastroesophageal junction and proximal esophagus) with age (years). Comparison by Pearson correlation with correlation coefficient (r) and P value is shown.
Utility of One vs Three Sites for Active EoE
The peak eosinophil count (eos/hpf) for each individual site along with comparison with 3 sites was next assessed. We assessed the initial endoscopy with active EoE among unique patients (n = 167). The distal esophagus had the highest eosinophil count, with a median [interquartile range] of 40 [25–72], followed by mid of 30 [9–60] and proximal of 15 [1–40] (Table 2). The sensitivity of distal esophagus biopsies alone to identify active EoE was greater than 80%, whereas the mid esophagus was 65%, and the proximal esophagus was 62% (Table 1). Interestingly, among all 304 endoscopies with active EoE, the distal esophagus identified active EoE in more than 90% of endoscopies (Supplementary Figure 1).
Table 2.
Median Peak Eosinophils per High-Power Field for Combinations of Sites, Sensitivity, Negative Predictive Value, and Accuracy for Identification of Active EoE
| Esophagus site | Eos/hpf, median [interquartile range] | Sensitivity (%)a | Negative predictive value (%)a | Accuracy (%)a | |
|---|---|---|---|---|---|
| Distal/mid/proximal | 50 | 30–82 | 100 | 100 | 100 |
| Distal/mid | 50 | 30–80 | 97.0 | 91.7 | 97.8 |
| Distal/proximal | 40 | 25–75 | 98.8 | 96.3 | 99.1 |
| Mid/proximal | 35 | 11–60 | 73.1 | 67.9 | 82.8 |
| Distal | 40 | 25–72 | 91.6 | 82.1 | 93.9 |
| Mid | 30 | 9–60 | 64.7 | 64.9 | 78.6 |
| Proximal | 15 | 1–40 | 52.7 | 62.3 | 73.6 |
Individual site and 2-site combinations compared with 3-site combination for initial esophagogastroduodenoscopy among 217 EoE patients (167 with active EoE).
Sensitivity of Two vs Three Sites in Active EoE
We next examined the utility of 2- vs 3-site combinations to identify active EoE. Among the initial endoscopy for patients with active EoE (n = 167), the median [interquartile range] eos/hpf in the proximal/distal, mid/distal, and proximal/mid esophagus was 40 [25–75], 50 [30–80], and 35 [11–60], respectively. Notably the median [interquartile] eos/hpf for a 3-site combination was 50 [30–82] (Table 2). The diagnostic sensitivity for proximal/distal (98.8) and mid/distal (97.8) was similar, with lower sensitivity noted in mid/proximal (73.1) biopsies. Similar results were noted among the full 304 active EoE endoscopy group (Supplementary Figure 1) and among unique patients with active EoE stratified by swallowed steroid treatment (Supplementary Table 2 and Supplementary Figure 2). In our cohort a diagnosis of EoE could have been missed in up to 17 endoscopies if biopsies from all 3 sites had not been analyzed. Among these 17 endoscopies, diagnostic eosinophilia (>15 eos/hpf) was isolated to only the mid esophagus in 9 cases, and 8 endoscopies contained isolated proximal inflammation. We further observed that among patients with at least 2 active EoE time points (n = 78), less than half of patients had the same sites involved, and one fourth had fewer sites involved at the second time point. This supports obtaining and analyzing biopsies from 3 sites to achieve optimal diagnosis of EoE.
Sensitivity of Endoscopic Abnormalities for Active EoE
Last, we assessed the utility of obtaining biopsy from visually inflamed areas identified during endoscopy in limiting the number of sites needed to biopsy to identify active EoE. Biopsies obtained from the single most inflamed visual site (defined as highest sum endoscopic reference score between distal, mid, and proximal esophagus) were found to have a diagnostic sensitivity of 89.8%, whereas those obtained from the 2 most inflamed sites achieved 96.7% sensitivity (Supplementary Figure 2), similar to a 2-site location-based approach with distal plus either mid or proximal biopsies. Thus, we have identified a small subset of children with EoE in whom the sole site of active EoE had normal endoscopic appearance, further supporting a 3-site biopsy protocol and a change in paradigm from prior recommendations.
Discussion
EoE is a clinicopathologic condition for which diagnosis relies on the presence of symptoms of esophageal dysfunction and the identification of esophageal mucosal histology demonstrating eosinophilia.1 Prior studies have demonstrated significant variability in eosinophil density between individual biopsies of EoE patients.4,5 Thus, adequate tissue sampling is important to diagnose EoE. In the current study we examined a large prospective cohort of children with EoE and found esophageal eosinophilia is most dense in the distal esophagus, followed by mid and then proximal esophagus. This is consistent with prior adult studies,3,16 thus validating this finding to be consistent in children as well. However, although individual esophageal sites had limited sensitivity to identify active EoE compared with all 3 sites, the distal esophageal biopsies achieved a threshold of 80%–90%. Among 2-site biopsy combinations, distal + proximal and distal + mid esophagus had slightly poorer sensitivity than the 3-site combination but were superior to mid + proximal. Although our study validates the need for biopsies of the distal esophagus, it raises questions regarding whether biopsies of the mid or proximal esophagus or both should be obtained.
Consensus guidelines have established that 2–4 biopsies from 2 different sites distal and proximal are necessary for accurate sampling of tissue.17 The utility of adding biopsies from mid esophagus to distal and proximal has recently been studied.2,3,16 Chernetsova et al2 retrospectively examined 100 pediatric patients with EoE with regard to the question of the utility of mid esophageal biopsies. They found the mid esophagus alone showed histologic abnormalities in up to 8% of biopsies. Radicic et al3 identified increased diagnostic sensitivity in adults with EoE. Fujiwara et al16 found a combination of distal and mid biopsies sufficient to identify active EoE. We found that biopsies from all 3 sites have the highest diagnostic sensitivity, followed by equivalent sensitivity among distal with mid or distal with proximal combinations. Isolated disease in the mid esophagus is rare and occurred in 9 patients, and isolated disease in the proximal esophagus was identified in 8 patients. Thus, in the context of the existing literature, our findings validate the need for biopsies from all 3 sites of the esophagus to optimally assess for active EoE. In addition, we found that biopsies from the 2 locations with the most objectively severe inflammation based on the eosinophilic esophagitis endoscopic reference score18 had similar accuracy as any 2-site combination of biopsies. Although a 3-site protocol is superior, our findings suggest visual findings could guide 2-site biopsy protocols, which is consistent with previous studies that have validated the endoscopic reference score as a marker for active disease.6,9,19
A significant strength of the study was the use of endoscopic measurements to identify the proximal, mid, and distal esophagus and GEJ. This ensured rigor and uniformity of the biopsy protocol, and we also reported a highly significant correlation between these measures, height, and age. Notably, the length of the esophagus has been appreciated to depend on factors such as age and height.20,21 Our findings provide a roadmap to assist gastroenterologists in rigorously assessing the esophagus for EoE. In addition, these measurements may have utility for noninvasive or minimally invasive tests such as esophageal string test, sponge test, or esophageal distensibility/motility studies that may require evaluation of specific sites of the esophagus in children.
Several limitations exist for this study. The cohort was derived from measurements taken by only a single endoscopist, creating a potential observer bias. However, this likely improves the accuracy and precision of the measurements and the standardization among patients. Another limitation was the failure to incorporate the EoE histologic scoring system22 in evaluation of the biopsies. Although our work well represents clinical care, broader examination of the biopsy using the EoE Histological Scoring System in a future study would allow an additional dimension to better delineate the patchy extent of the disease.
In conclusion, we conducted a large, prospective pediatric study to assess the utility of a 3-site biopsy protocol for identification of active EoE using standardized endoscopic measurements which strongly correlated with height. Our study findings suggest that obtaining 3-site distal, mid, and proximal biopsies rather than the current protocol of 2-site distal and proximal location is superior in children. Furthermore, our findings suggest biopsies taken from the 2 most visually abnormal appearing tissue have high diagnostic yield, but that active EoE can occur solely in one site with normal endoscopic appearance in children. This study also demonstrates that visual findings may guide biopsy location.
Supplementary Material
What You Need to Know.
Background
Eosinophilic esophagitis (EoE) is a patchy disease of the esophagus, and 3 biopsies each from distal and proximal esophagus are recommended for identification of active EoE (at least 15 eosinophils per high-power field). We sought to evaluate 2-site vs 3-site esophageal biopsy combinations for utility to identify active EoE.
Findings
Distal + proximal biopsies had the highest diagnostic sensitivity for a 2-site combination. A small subset of patients had focal eosinophilia restricted to the mid or proximal esophagus only, whereas nearly one fourth had reduced sites with eosinophilia at a second time point. Endoscopic measurements strongly correlated with height and age.
Implications for patient care
For optimal identification of active EoE longitudinally in children, a 3-site esophageal biopsy is recommended.
Funding
Supported in part by Buckeye Foundation (to AK), K08DK097721 (to JW), internal funding from Ann & Robert H. Lurie Children’s Hospital of Chicago, and Consortium of Eosinophilic Gastrointestinal Researchers (CEGIR) [to JW]. Dr Wechsler is a trainee in CEGIR (U54 AI117804) part of the Rare Disease Clinical Research Network, an initiative of the Office of Rare Diseases Research, National Center for Advancing Translational Sciences, and is funded through collaboration between National Institute of Allergy and Infectious Disease, National Institute of Diabetes, Digestive, and Kidney Diseases, and Nation Center for Advancing Translational Sciences. CEGIR is also supported by patient advocacy groups including American Partnership for Eosinophilic Disorders, Campaign Urging Research for Eosinophilic Diseases, and Eosinophil Family Coalition.
Abbreviations used in this paper:
- EoE
eosinophilic esophagitis
- eos
eosinophil
- GEJ
gastroesophageal junction
- hpf
high-power field
Footnotes
CRediT Authorship Contributionsr
Joshua B. Wechsler, MD (Data curation: Equal; Formal analysis: Equal; Visualization: Lead; Writing – original draft: Lead; Writing – review & editing: Lead)
Scott M. Bolton (Data curation: Supporting; Formal analysis: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting)
Elizabeth Gray (Formal analysis: Equal; Visualization: Equal)
Kwang-Youn Kim (Formal analysis: Equal; Visualization: Equal; Writing – review & editing: Supporting)
Amir F. Kagalwalla (Conceptualization: Lead; Data curation: Equal; Formal analysis: Equal; Funding acquisition: Lead; Methodology: Lead; Supervision: Lead; Writing – original draft: Equal; Writing – review & editing: Equal)
Conflicts of interest
The authors disclose no conflicts.
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at https://doi.org/10.1016/j.cgh.2021.12.023.
References
- 1.Dellon ES, Liacouras CA, Molina-Infante J, et al. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE Conference. Gastroenterology 2018;155:1022–1033 e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chernetsova E, Agarwal A, Weir A, et al. Diagnostic value of mid-esophageal biopsies in pediatric patients with eosinophilic esophagitis. Pediatr Dev Pathol 2021;24:34–42. [DOI] [PubMed] [Google Scholar]
- 3.Radicic K, Stokes RF. Analysis of midesophageal biopsies increases sensitivity of detection of eosinophilic esophagitis. Clin Gastroenterol Hepatol 2019;17:1408–1409. [DOI] [PubMed] [Google Scholar]
- 4.Shah A, Kagalwalla AF, Gonsalves N, et al. Histopathologic variability in children with eosinophilic esophagitis. Am J Gastroenterol 2009;104:716–721. [DOI] [PubMed] [Google Scholar]
- 5.Gonsalves N, Policarpio-Nicolas M, Zhang Q, et al. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointest Endosc 2006;64:313–319. [DOI] [PubMed] [Google Scholar]
- 6.Wechsler JB, Bolton SM, Amsden K, et al. Eosinophilic esophagitis reference score accurately identifies disease activity and treatment effects in children. Clin Gastroenterol Hepatol 2018; 16:1056–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dellon ES. Approach to diagnosis of eosinophilic esophagitis. Gastroenterol Hepatol (N Y) 2011;7:742–724. [PMC free article] [PubMed] [Google Scholar]
- 8.Carrasco A, Machado RS, Patricio F, et al. Histological features of eosinophilic esophagitis in children and adolescents. Arq Gastroenterol 2017;54:281–285. [DOI] [PubMed] [Google Scholar]
- 9.Dellon ES, Cotton CC, Gebhart JH, et al. Accuracy of the eosinophilic esophagitis endoscopic reference score in diagnosis and determining response to treatment. Clin Gastroenterol Hepatol 2016;14:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strobel CT, Byrne WJ, Ament ME, et al. Correlation of esophageal lengths in children with height: application to the Tuttle test without prior esophageal manometry. J Pediatr 1979;94:81–84. [DOI] [PubMed] [Google Scholar]
- 11.Yang GS, Bishop WP, Smith BJ, et al. Radiographic and endoscopic measurements of esophageal length in pediatric patients. Ann Otol Rhinol Laryngol 2005;114:587–592. [DOI] [PubMed] [Google Scholar]
- 12.Staiano A, Clouse RE. Value of subject height in predicting lower esophageal sphincter location. Am J Dis Child 1991; 145:1424–1427. [DOI] [PubMed] [Google Scholar]
- 13.Moreau B, Kambites S, Levesque D. Esophageal length: esophageal manometry remains superior to mathematical equations. J Pediatr Gastroenterol Nutr 2013;57:236–239. [DOI] [PubMed] [Google Scholar]
- 14.Song TJ, Kim YH, Ryu HS, et al. Correlation of esophageal lengths with measurable external parameters. Korean J Intern Med 1991;6:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol 2011;128:3–20 e6, quiz 21–22. [DOI] [PubMed] [Google Scholar]
- 16.Fujiwara Y, Hashimoto A, Uemura R, et al. Optimal biopsy protocol to evaluate histological effectiveness of proton pump inhibitor therapy in patients with eosinophilic esophagitis. Digestion 2019;100:64–71. [DOI] [PubMed] [Google Scholar]
- 17.Nielsen JA, Lager DJ, Lewin M, et al. The optimal number of biopsy fragments to establish a morphologic diagnosis of eosinophilic esophagitis. Am J Gastroenterol 2014;109: 515–520. [DOI] [PubMed] [Google Scholar]
- 18.Hirano I, Moy N, Heckman MG, et al. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: validation of a novel classification and grading system. Gut 2013; 62:489–495. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez-Sanchez J, Barrio-Andres J, Nantes Castillejo O, et al. The endoscopic reference score shows modest accuracy to predict either clinical or histological activity in adult patients with eosinophilic oesophagitis. Aliment Pharmacol Ther 2017; 45:300–309. [DOI] [PubMed] [Google Scholar]
- 20.Koumanidou C, Manoli E, Anagnostara A, et al. Sonographic features of intestinal and biliary ascariasis in childhood: case report and review of the literature. Ann Trop Paediatr 2004; 24:329–335. [DOI] [PubMed] [Google Scholar]
- 21.Singendonk MMJ, Ferris LF, McCall L, et al. High-resolution esophageal manometry in pediatrics: effect of esophageal length on diagnostic measures. Neurogastroenterol Motil 2020; 32:e13721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins MH, Martin LJ, Alexander ES, et al. Newly developed and validated eosinophilic esophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosis and monitoring. Dis Esophagus 2017;30:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


