Abstract
Background
Biofilm-related infections are difficult to be treated because of higher resistance to antimicrobial agents. Current study aims to characterize the influence of zinc oxide nanoparticles (ZnO-NPs) on both S. aureus susceptibility to antibiotics and pathogenesis.
Methods
The influence of ZnO-NPs on biofilm formation by S. aureus was characterized by the crystal violet and tube assay. The synergistic effect of ZnO-NPs in combination with antibiotics on S. aureus was characterized using the checkerboard method. The effect of ZnO-NPs on S. aureus cell surface hydrophobicity and blood hemolysis was investigated. RT-qPCR was used to investigate the effect of ZnO-NPs on the expression of biofilm related genes (icaA, icaR and sarA), katA and sigB. The impact of ZnO-NPs on S. aureus pathogenesis was evaluated using mice infection model.
Results
ZnO-NPs exhibited a good antibiofilm activity against S. aureus. The findings indicate a synergistic antibiofilm effect of combination between ZnO-NPs and tested antibiotics. ZnO-NPs were capable of decreasing S. aureus cell surface hydrophobicity which could account for observed decrease in bacterial biofilm forming capacity. Moreover, ZnO-NPs-treated bacteria exhibited a significant decrease in blood hemolysis relative to control untreated S. aureus. The expression of biofilm related genes was significantly repressed in ZnO-NPs treated bacteria as compared to untreated cells. Finally, the effect of ZnO-NPs on S. aureus pathogenesis was investigated using mice infection model where ZnO-NPs accelerated healing of wounds in mice as compared to control untreated mice.
Conclusions
Present data support the efficiency of ZnO-NPs as antibiofilm agent in treatment of S. aureus infections. This study recommends the incorporation of ZnO-NPs as adjuvant with other antibiotics targeting S. aureus based on the promising findings obtained herein in order to control infection with this pathogen.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12866-022-02658-z.
Keywords: Staphylococcus aureus, Zinc oxide nanoparticles (ZnO-NPs), Antibiofilm, Pathogenesis
Introduction
Staphylococcus aureus is a Gram-positive opportunistic pathogen that causes a variety of infections both in nosocomial and community settings. S. aureus is a causative agent of wide range of illnesses due to its higher capability to colonize and survive within different host tissues. For instance, S. aureus causes soft tissue infections, endocarditis, osteomyelitis and urinary tract infections. In addition, S. aureus is responsible for several syndromes caused by secretion of exotoxins and enterotoxins including food poisoning and scalded skin syndromes. S. aureus expresses many potential virulence factors that promote colonization of host tissues including hemolysins and exotoxins [1].
Bacterial biofilm could be defined as ability of bacterial cells to adhere to various surfaces and the formation a matrix-encased community of cells. Bacterial biofilms could be influenced by various environmental factors including nutrient and oxygen availability. Biofilm formation markedly contributes to S. aureus pathogenesis in host. Bacteria within biofilms display a higher resistance to antimicrobial agents including antibiotics. Moreover, bacterial biofilm plays a role in evasion of host immune defenses leading to a difficulty of pathogen removal. The increased biofilm associated staphylococcal infections requires the introducing of effective antibacterial treatment policies [2]. The increased bacterial resistance within biofilms to both antimicrobial agents and host defense is considered the major problem associated with S. aureus biofilms. The biofilm polysaccharide matrix has been shown to play an important role in this bacterial resistance and acts as a barrier that hinders the diffusion of antimicrobial agents. Furthermore, differences in nutrient and oxygen availability within biofilm lead to variations in both bacterial growth rate and metabolic activity. As a result, cell division occurs at much lower rates producing persister cells which are highly tolerant to various antimicrobial agents [3].
Nanotechnology has been previously shown to be a promising approach for treatment of biofilm-related infections. Many advantages have been reported for nanoparticles (NPs) as drug delivery systems that maintain sustained drug release and minimize the side effects of used drugs. Furthermore, various NPs are being widely studied for their potential antimicrobial effects. For example, metallic oxide NPs such as zinc oxide (ZnO-NPs) and copper oxide (CuO-NPs) are characterized by low cytotoxicity and higher capacity to function as drug delivery systems. It has been shown that both the antibacterial and antibiofilm properties of nanomaterials could be largely affected by many factors such as shape and surface charge [4, 5].
Importantly, ZnO-NPs have been reported to exhibit many merits such as higher solubility, bioavailability and biocompatibility. Therefore, ZnO-NPs can mimic the biomolecules activity, localize in many body systems and maintain cellular homoeostasis [6]. Compared with other nanomaterials, ZnO-NPs are relatively less toxic, comparatively inexpensive and therefore could be applied in various applications as anticancer, antibacterial as well as anti-inflammation and diabetes treatment [7]. Furthermore, ZnO-NPs are characterized by chemical stability, strong adsorption ability in addition to their catalytic efficiency [8, 9]. On the other hand, other nanomaterials such as silver NPs and iron oxide NPs have been shown to exhibit serious disadvantages such as cytotoxicity that could limit their use in medicine. In addition, silver NPs induce the release of proinflammatory cytokines and production of reactive oxygen species (ROS) and nitric oxide which affect the central nervous system causing neuroinflammation. Moreover, silver NPs have cytotoxic effects on osteoclasts, osteoblasts, cardiovascular and respiratory systems which could restrict their use in biomedical applications [10]. Despite of the advantageous characteristics of gold NPs such as biocompatibility and low toxicity, it is considered as non-biodegradable which may lead to gold accumulation inside the body and possible interaction with immune cells [11]. Finally, silica NPs have been recently used in the treatment of bacterial infection [12]. However, silica NPs exhibit high density of silanol groups on their surface that could interact with the phospholipids of red blood cells leading to hemolysis which requires surface modification in order to be safely used. In addition, the lower stability and formation of aggregates are another problem that could affect the usage of silica NPs in medicine [13]. Detailed comparison between ZnO-NPs and other nanomaterials based on their advantages and disadvantages is represented in the Supplementary Table S1.
Current study aims to investigate the antibacterial and antibiofilm potential of ZnO-NPs against S. aureus. The influence of ZnO-NPs on both S. aureus susceptibility to antibiotics and host pathogenesis will be investigated herein. Importantly, in addition to S. aureus reference strain, the antibiofilm activity of ZnO-NPs on S. aureus clinical isolates from various sources will be evaluated herein. Investigating the influence of ZnO-NPs on biofilm formation by clinical S. aureus isolates would be important to understand how environment could affect bacterial response to antibiofilm agents. Furthermore, present study is performed in order to characterize the antibacterial and antibiofilm mechanisms of ZnO-NPs. For instance, ZnO-NPs effect on both S. aureus cell surface hydrophobicity and hemolytic activity will be assessed. The findings of this study would expand understanding of S. aureus pathogenesis and consequently help us control infections caused by this opportunistic pathogen.
Materials and methods
Isolation and identification of S. aureus
Clinical S. aureus isolates were provided by the clinical laboratories of Zagazig University Hospitals and El-Ahrar Educational Hospital in Zagazig, Egypt with no direct involvement of patients in the study. S. aureus isolates were further identified biochemically. In addition to S. aureus clinical isolates, S. aureus ATCC 6538 was involved in this study. For long term preservation of S. aureus isolates, glycerol (20%) was added to overnight culture of Mueller Hinton (MH) broth and kept at -80 °C.
Determination of antibiotic susceptibility S. aureus isolates by disc diffusion method
Antimicrobial susceptibility testing was done by Kirby-Bauer standard disc diffusion method against all clinical S. aureus isolates and ATCC 6538 according to CLSI (2018) guidelines. The antibiotic discs used in this study include methicillin, ceftriaxone and cefotaxime, tetracycline, ciprofloxacin, gentamicin, erythromycin, azithromycin, linezolid, vancomycin, clindamycin, chloramphenicol and sulfamethoxazole-trimethoprim. The inhibition zones diameters were measured in millimeter (mm) and S. aureus susceptibility to antibiotic was interpreted as susceptible (S), intermediate (I) and resistant (R) according to interpretative criteria for antimicrobial susceptibility testing recommended by CLSI (2018) [14].
Determination of minimum inhibitory concentration (MIC) of tested antibiotics and ZnO-NPs
ZnO-NPs were purchased from (Sigma-Aldrich, Germany) with particle size of 50 nm and surface area of > 10.8 m2/g. The MICs of both antibiotics and ZnO-NPs against S. aureus ATCC 6538 and clinical isolates were determined by the broth microdilution method according to CLSI (2018). The range of molar concentrations of ZnO-NPs and antibiotics used in MIC assay was as follow; ZnO-NPs (6.29 to 0.01 mM); gentamicin (2.14—0.52 × 10–3 mM); ciprofloxacin (3.09—0.18 × 10–3 mM); clindamycin (2.4—1 × 10–5 mM); chloramphenicol (0.396—0.39 × 10–3 mM); cefotaxime (4.5—0.27 × 10–3 mM) and azithromycin (1.36—1.7 × 10–4 mM). The MIC of selected antibiotics was defined as the lowest concentration of antibiotic that inhibits bacterial growth and no visible growth is observed as compared with both a positive control (culture broth containing bacteria only that should appear turbid) and a negative control (culture broth without bacteria that should remain clear) [14]. In addition, the half maximal inhibitory concentration (IC50) of ZnO-NPs against S. aureus was determined according to Namvar et al. [15]. The experiment was performed in triplicate and the IC50 was calculated by plotting the percentage of growth inhibition to a normal dose–response-inhibition curve.
Quantitative assessment of biofilm formation by spectrophotometry
The ability of S. aureus ATCC 6538 and clinical isolates to form biofilm was tested according to Stepanović et al. [16] with some modifications. A 1:100 dilutions of S. aureus overnight culture were prepared in Trypticase soy (TS) broth supplemented with 1% glucose (TSB1%GLU). Aliquots of 200 µL/well of the prepared suspensions were added to each well of 96 well microtiter plates and incubated for 48 h at 37 °C. Negative control wells that contained 200 µL/well of TSB only were included in each plate. Formed biofilms were fixed using methanol for 20 min. Fixed biofilms were stained with 1% crystal violet for 15 min. The plates were air dried and the bound dye was dissolved by 33% glacial acetic acid. The optical densities were measured spectrophotometrically at 570 nm using Bio-Tek synergy HT microplate reader, USA. Measurements were performed in triplicates and the experiment was repeated three times. The cut-off optical density (ODc) was calculated as three times standard deviations above the mean OD of the negative control. The tested strains were classified into: non-biofilm producer (OD ≤ ODc), weak biofilm producer (OD > ODc, but ≤ 2 × ODc), moderate biofilm producer (OD > 2 × ODc, but ≤ 4 × ODc) and strong biofilm producer (OD > 4 × ODc) [16].
Antibiotic susceptibility testing for bacterial biofilm
The susceptibility of biofilm formed by S. aureus ATCC 6538 and clinical isolates to antibiotics was assayed according to Sabino et al. [17] in 96-wells polystyrene microtiter plates. A 1:100 dilution of S. aureus overnight culture with turbidity matching that of 0.5 McFarland standards were made in TSB1%GLU, then 100 µL aliquots was transferred to wells of microtiter plates. The plates were incubated for 48 h at 37 °C for biofilm formation. Wells were washed thrice with PBS under aseptic conditions to remove unattached bacteria and dried in an inverted position. Two-fold serial dilutions of the respective antibiotic in MH broth were added into the dried wells with established biofilms. The microtiter plates were incubated for 24 h at 37 °C, and minimum biofilm inhibitory concentration (MBIC) was determined. The experiment was performed in triplicate [17].
Assay of antibiofilm ZnO-NPs by microtiter plate method
The antibiofilm potential of ZnO-NPs against both S. aureus ATCC 6538 and clinical isolates was characterized according to Basumatari et al. [18]. Briefly, overnight grown cultures of bacteria were diluted to 1:100 in TSB1%GLU. Then aliquots of about 100 µL were added to wells of sterile microtiter plate and incubated for 48 h to allow biofilm formation. The biofilm eradication activity of ZnO-NPs was determined as follows; aliquots of different concentrations of ZnO-NPs; 256, 128 and 64 µg /mL (3.1, 1.57 and 0.78 mM; respectively) were added to plate. Both negative and positive control wells without bacterial culture and without ZnO-NPs respectively were maintained for each isolate. The plate was incubated at 37 °C for 24 h and the influence of ZnO-NPs on bacterial biofilm eradication was assessed as described above. Each assay was performed in triplicate and percentage of biofilm inhibition was determined as follows [18]:
Characterization of the synergistic effect of ZnO-NPs in combination with antibiotics on inhibition of S. aureus biofilm formation
The effect of combination between ZnO-NPs and tested antibiotics (AB) on inhibition of S. aureus ATCC 6538 biofilm formation was determined by test tube method as described by Ashajyothi et al. [19]. Four separate test tubes were used as follow; tube 1 contained bacterial culture + TSB1%GLU as control, tube 2 contained bacterial culture + TSB1%GLU + corresponding antibiotic, tube 3 contained bacterial culture + TSB1%GLU + ZnO-NPs and tube 4 contained bacterial culture + TSB1%GLU + antibiotic + ZnO-NPs. All tubes were incubated for 48 h at 37 °C. Next, each tube was washed with PBS and biofilm formation was characterized as described above. Percentage of synergistic effect of ZnO-NPs on biofilm inhibition by antibiotics was calculated by following equation [19].
Checkerboard microdilution assay
Checkerboard assay was performed to measure synergy between ZnO-NPs and different antibiotics against S. aureus ATCC 6538 by calculating the fractional inhibitory concentration index (FICI) where FIC index (FICI) = FIC of ZnO-NPs + FIC of antibiotic. Synergy was defined when FICI was ≤ 0.5; while additive in which 0.5 ˂ FICI ≤ 1.0; whereas indifferent when the FICI is between 1 and 4 [19]. The range of molar concentrations used in combination assays was as follow; ZnO-NPs (6.29—6 × 10–3 mM); gentamicin (16 × 10–3—6 × 10–5 mM); ciprofloxacin (12 × 10–3—9 × 10–5 mM); clindamycin (14 × 10–5—1 × 10–5 mM); chloramphenicol (24 × 10–3—5 × 10–5 mM); cefotaxime (0.56—1 × 10–3 mM) and azithromycin (1.3 × 10–3—1.7 × 10–4 mM).
Characterization of S. aureus biofilm inhibition by scanning electron microscopy (SEM) and light microscopy
The antibiofilm activity of ZnO-NPs, gentamicin and their combination against S. aureus ATCC 6538 was characterized using both scanning electron microscope (SEM) and light microscope. Biofilms were developed on polystyrene discs exactly as described above for control untreated, gentamicin-treated, ZnO-NPs-treated and ZnO-NPs + gentamicin-treated bacteria. Following incubation, discs were washed trice with phosphate buffered saline (PBS) and fixed by 2.5% glutaraldehyde for 2 h. Discs were dried and gold coated before imaging and examined using jeol scanning microscope (JSM- T100, Japan) [20].
Determination of hydrophobicity index (HI) of ZnO-NPs treated S. aureus
Hydrophobicity index (HI) of ZnO-NPs treated S. aureus ATCC 6538 cells was done according to Rauf et al. [21]. Briefly, overnight grown bacterial cells were resuspended in MH broth and the optical density was adjusted to 1.0 at a wavelength of 595 nm. A volume of 1 mL toluene was added to cell suspension in a test tube and the tube was vortexed. The biphasic mixture of two phases was allowed to settle for 30 min and the optical density of the aqueous phase was measured. Hydrophobicity index (HI) of microbial cells was determined by using the following equation [21]: , where Ai and Af are the initial and final optical densities of the aqueous phase; respectively.
Haemolysis assay
In vitro erythrocyte lysis test was performed according to Rauf et al. [21]. Briefly, fresh blood isolated from a healthy sheep was collected in anticoagulant solution (EDTA) and spun at 6000 rpm for 10 min at 4 °C. Both buffy coat and plasma were discarded. Washed erythrocytes were diluted with isotonic buffer (20 mM PBS) to prepare 2% hematocrit. The extent of hemolysis was studied by incubating red blood cells (RBCs) suspension with S. aureus ATCC 6538 alone and S. aureus with ZnO-NPs at 37 °C overnight. In addition, erythrocytes were incubated with ZnO-NPs alone as a control to confirm that ZnO-NPs have no hemolytic effect on erythrocytes at used concentration. Next, incubated solutions were centrifuged at 6000 rpm for 10 min and the supernatant was analyzed for released hemoglobin and measured at 490 nm. The percentage hemolysis was determined by the following equation [21]:
where; AbsT is the absorbance of the supernatant from samples incubated with S. aureus, S. aureus with ZnO-NPs respectively, AbsC is the absorbance of the supernatant from control (PBS) and Abs 100% is the absorbance in the presence of 0.1% sodium dodecyl sulfate (SDS).
Total RNA extraction and qRT-PCR
S. aureus ATCC 6538 at cell density of 1 × 106 CFU∕mL was cultured in TSB 1%GLU with or without 0.78 mM ZnO-NPs (64 µg∕mL) for 48 h. Next, bacterial suspensions were centrifuged at 6000 rpm for 10 min at 4 °C and cell pellets were washed with PBS. RNA was extracted from both treated and untreated bacterial pellets using GeneJET RNA Purification Kit (Thermoscientific, USA) following the manufacturer instructions. Obtained RNA was further purified using a Qiagen RNeasy minikit (Qiagen, Valencia, CA). Following purification, 100 μL of nuclease free water was added to elute RNA and stored at -70 °C until use. The expression of S. aureus biofilm-related genes (icaA, icaR, agrA and sarA), oxidative stress response gene; catalase (katA) and the transcription regulator sigma B (sigB) was determined in both ZnO-NPs treated and untreated S. aureus ATCC 6538 using q RT-PCR. The expression level of each gene was normalized to 16S rRNA, a gene for which the expression levels remained unchanged in both control and treated with ZnO-NPs bacteria. Primers used in this study are listed in Table 1. The analysis was conducted following the protocol described in SensiFAST™ SYBR Hi-ROX One-Step Kit (Bioline, UK) using StepOne Real-Time PCR system (Applied Biosystem, USA). Specific PCR amplification was confirmed by both agarose gel electrophoresis and a melting curve analysis of products according to the manufacturer recommendation. Relative gene expression was calculated by the 2−∆∆CT method [22].
Table 1.
Primers used in qRT-PCR
| Gene name | Primer sequence (5‵- 3‵) |
|---|---|
| icaA (F) | CTGGCGCAGTCAATACTATTTCGGGTGTCT |
| icaA (R) | GACCTCCCAATGTTTCTGGAACCAACATCC |
| icaR (F) | TGCTTTCAAATACCAACTTTCAAGA |
| icaR (R) | ACGTTCAATTATCTAATACGCCTG |
| sigB (F) | AAGTGATTCGTAAGGACGTCT |
| sigB (R) | TCGATAACTATAACCAAAGCCT |
| agr (F) | TGATAATCCTTATGAGGTGCTT |
| agr (R) | CACTGTGACTCGTAACGAAAA |
| sarA (F) | CAAACAACCACAAGTTGTTAAAGC |
| sarA (R) | TGTTTGCTTCAGTGATTCGTTT |
| katA (F) | AAAGGTTCTGGTGCATTTGG |
| katA (R) | AACGCAAATCCTCGAATGTC |
| 16s RNA (F) | ACTCCTACGGGAGGCAGCAG |
| 16s RNA (R) | ATTACCGCGGCTGCTGG |
F Forward, R Reverse
Determination of ZnO-NPs effect on staphylococcus biofilm formation on urinary catheter
The inhibitory efficacy of ZnO-NPs on staphylococcal biofilms on catheters was determined in vitro [23]. An overnight culture of S. aureus ATCC 6538 was diluted 1:100 in TSB1%GLU. Sterile 1 cm long segments of Foley catheter were immersed in 5 mL culture tube containing approximately 106 CFU∕mL of S. aureus ATCC 6538 and another tube containing sub-MIC of ZnO-NPs (64 µg∕mL; 0.78 mM). Cultures with catheter pieces were incubated at 37 °C for 48 h. Following incubation, catheter pieces were removed and rinsed twice in PBS to remove the adhering planktonic cells. Next, segments were transferred to another tube containing 5 mL PBS in order to extract biofilm bacterial cell from catheter. Tubes were vortexed for 1 min then sonicated for 15 min and vortexed again for 1 min. Serial dilutions of bacteria were made in sterile PBS, plated onto mannitol salt agar and incubated for 24 h at 37 °C for viable counting.
In vivo mice infection
The influence of ZnO-NPs on S. aureus ATCC 6538 pathogenesis was characterized using mice infection model according to [24]. The animal study was approved by the institutional animal care and used committee, Zagazig University (ZU-IACUC) with approval number ZUIACUC/3/F/159/2019. Thirty-six healthy albino mice were used in this study and randomly divided into 6 groups (6 mice each). In addition to the positive control group (S. aureus-inoculated mice) and negative control groups (PBS-inoculated mice and uninfected mice), other three groups were included; ZnO-NPs treated mice group, gentamicin-treated mice group and ZnO-NPs + gentamicin treated mice group. Mice were anesthetized with thiopental through intraperitonial injection of 100 µL of 40 mg Kg−1. The back of mice was disinfected with 70% alcohol and hair was shaved. Full thickness skin wounds were created by sterile surgical scissor and immediately inoculated intradermally with S. aureus suspension at density (2.5 × 107 CFU∕mL) to each wound site. Wounds were treated intradermally with gentamicin, ZnO-NPs or a combination of gentamicin + ZnO-NPs. The progression of wound healing in different mice groups was assessed every 3 days following bacterial inoculation (day zero). Results were taken by capturing representative images for wound healing in mice in different groups on days 0, 3, 6, 10, and 14 following treatment using a camera (Sony Ciyber Shot, Dsc w80). In addition, the wound contraction percentage (%) was determined by calculating the wound area (mm2) at the analysis day and compared with the initial wound area (mm2) using the following formula [25]: Wound contraction (%) = where; A0 is the initial wound area in mm2 and At is the wound area at the time of image capturing in mm2.
Results
Isolation and identification of S. aureus isolates
A total of 103 S. aureus isolates were involved in current study. S. aureus isolates were from different clinical sources including wound infections, urinary tract infections, respiratory tract infections, burn, eye and ear infections. Bacterial isolates were confirmed as S. aureus based on their biochemical characteristics.
Determination of antibiotic susceptibility of S. aureus isolates by disc diffusion method
S. aureus isolates showed varying resistance patterns to different antibiotics (Supplementary Table S2). All S. aureus clinical isolates were resistant toward methicillin. High bacterial resistance was detected against cefotaxime and ceftriaxone (92.2% each) and tetracycline (63.1%). Intermediate bacterial resistance was observed against gentamicin (47.5%), erythromycin (31.1%) and azithromycin (30.1%). Low bacterial resistance was recorded against chloramphenicol, ciprofloxacin, clindamycin and sulphamethoxazole-trimethoprim (22.3%, 20.4%, 6.7% and 5.8%; respectively). All S. aureus clinical isolates were sensitive to both linezolid and vancomycin. Many S. aureus isolates (64%) were multi-drug resistant (MDR), which could be defined as resistance to at least one member in three or more different categories of antibiotics.
Determination of MIC of tested antibiotics and ZnO-NPs against S. aureus isolates
The MICs of tested antibiotics and ZnO-NPs were determined against both S. aureus ATCC 6538 and twenty clinical isolates recovered from different sources and exhibited variable antibiotic resistance profiles by disc diffusion method. The MICs were determined by the broth microdilution method according to the CLSI (2018) and results are represented in (Supplementary Table S3). In addition, the half maximal inhibitory concentration (IC50) of ZnO-NPs against S. aureus was determined and found to be 0.51 mM (Fig. 1) indicating that ZnO-NPs exhibit a potent antibacterial activity.
Fig. 1.
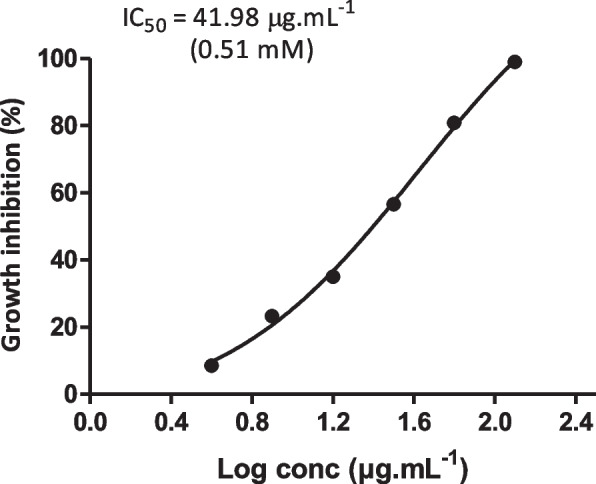
Determination of the half maximal inhibitory concentration (IC50) of ZnO-NPs against S. aureus ATCC 6538. Data shown represent the mean ± standard error from triplicate experiments. IC50 value was calculated from a non-linear regression model
Quantitative assessment of S. aureus biofilm formation
S. aureus ATCC 6538 and clinical isolates were screened for biofilm formation spectrophotometrically at 570 nm. Bacterial isolates were divided into four categories according to their capacity to form biofilm (Fig. 2). These four categories include; non-biofilm forming (OD ≤ 0.163), weak biofilm forming (OD ˃ 0.163, but ≤ 0.326), moderate biofilm forming (OD ˃ 0.326, but ≤ 0.652), strong biofilm forming (OD ˃ 0.652).
Fig. 2.
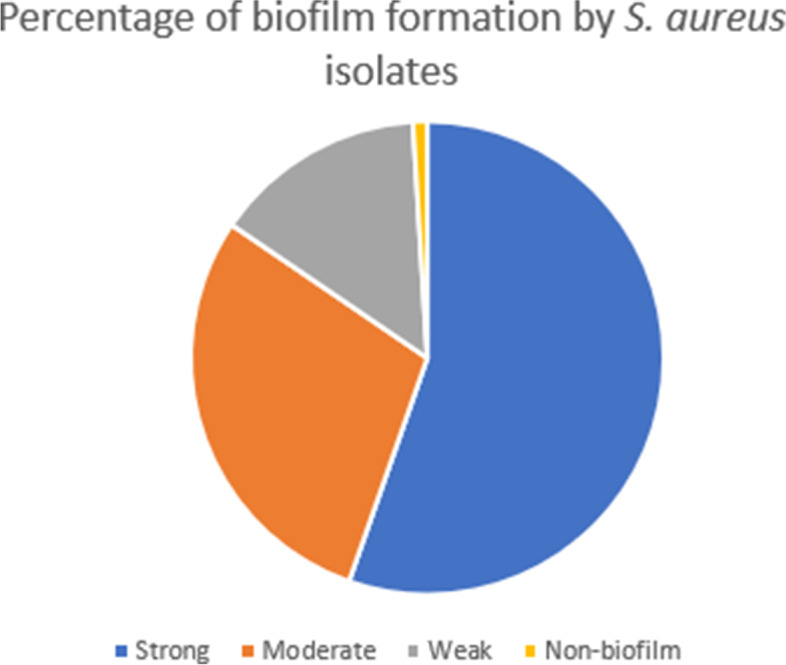
Quantitative assessment of S. aureus isolates biofilm formation. Bacterial biofilms were quantified by crystal violet assay. Optical density (OD) was measured spectrophotometrically at 570 nm. S. aureus isolates were classified according to biofilm forming capacity into strong, moderate, weak and non-biofilm forming
Antibiotic susceptibility testing for bacterial biofilm
The antibiotic susceptibility of biofilm formed by S. aureus ATCC 6538 and clinical isolates against different antibiotics was characterized by determining the MBIC. Results are presented in Table 2. All MBIC values were much higher than respective MIC values for the bacterial isolates tested.
Table 2.
Minimum biofilm inhibitory concentrations (MBICs) of antibiotics against S. aureus
| Isolate NO | Gentamicin (µg/mL) |
Ciprofloxacin (µg/mL) |
Clindamycin (µg/mL) |
Chloramphenicol (µg/mL) |
Cefotaxime (µg/mL) |
Azithromycin (µg/mL) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC | MBIC | MIC | MBIC | MIC | MBIC | MIC | MBIC | MIC | MBIC | MIC | MBIC | |
| S. aureus ATCC 6538 | 4 | 32 | 2 | 64 | 0.03 | 32 | 4 | 8 | 128 | 8192 | 0.5 | 512 |
| 1B | 128 | 512 | 2 | 64 | 0.06 | 2 | 16 | 128 | 16 | 64 | 4 | 256 |
| 2B | 32 | 64 | 0.125 | 64 | < .003 | 16 | 4 | 16 | 0.125 | 4 | 0.25 | 128 |
| 24B | 1024 | ˃4096 | 128 | 2048 | 512 | 2048 | 128 | 1024 | 2048 | 8192 | > 1024 | ˃8192 |
| 38B | 1024 | 4096 | 64 | 256 | 8 | 64 | 64 | 128 | 1024 | 4096 | > 1024 | ˃8192 |
| 41B | 2 | 16 | 1 | 128 | < .003 | 32 | 4 | 16 | 0.125 | 128 | 1 | 256 |
| 42B | 64 | 1024 | 0.25 | 128 | 0.25 | 32 | 0.5 | 256 | 0.125 | 64 | 1 | 128 |
| 44B | 8 | 32 | 1 | 32 | 0.25 | 32 | 4 | 8 | 64 | 512 | 1 | 256 |
| 48U | 4 | 16 | 8 | 64 | 0.03 | 32 | 4 | 8 | 256 | 4096 | 64 | 8192 |
| 55EY | 64 | 256 | 0.25 | 64 | 0.015 | 32 | 4 | 16 | 0.125 | 8 | 0.5 | 256 |
| 62EN | 8 | 16 | 16 | 64 | 0.03 | 2 | 8 | 32 | 32 | 128 | 32 | 8192 |
| 63EN | 8 | 16 | 16 | 256 | 0.5 | 1 | 32 | 128 | 128 | 2048 | 32 | 256 |
| 68EA | 0.5 | 256 | 32 | 128 | < .003 | 64 | 8 | 64 | 0.5 | 2048 | 0.5 | 1024 |
| 82W | 2 | 8 | 0.5 | 128 | 0.015 | 32 | 8 | 16 | 16 | 64 | 0.5 | 256 |
| 83W | 1 | 16 | 0.25 | 64 | 0.06 | 32 | 8 | 32 | 0.5 | 256 | 2 | 256 |
| 91W | 8 | 32 | 1024 | 4096 | 256 | 1024 | 16 | 32 | 1024 | 2048 | 512 | 8192 |
| 97W | 1024 | 4096 | 32 | 1024 | 256 | 1024 | 64 | 128 | 1024 | 4096 | > 1024 | 8192 |
| 99W | 256 | 8192 | 64 | 512 | 4 | 4096 | 128 | 512 | 1024 | 4096 | 32 | ˃8192 |
| 101W | 1024 | ˃4096 | 64 | 1024 | 1024 | 2048 | 64 | 1024 | 1024 | 8192 | > 1024 | 8192 |
B Burn, U Urine, EY Eye, EN Endotracheal aspirate, EA Ear, W Wound
Characterization of antibiofilm activity of ZnO-NPs by microtiter plate method
Antibiofilm activity of ZnO-NPs against both S. aureus ATCC 6538 and four S. aureus clinical isolates from different sources was characterized by microtiter plate method and percentages of biofilm inhibition are presented in Table 3. ZnO-NPs significantly reduced the biofilm biomass of S. aureus in a dose-dependent manner and percentages of biofilm reduction ranges from 29.4% to 50.4%.
Table 3.
Percentage of biofilm inhibition by ZnO-NPs
| Isolate No | ZnO-NPs concentration (µg/mL)/ Percentage reduction of biofilm formation (%) | ||
|---|---|---|---|
| 256 µg/mL | 128 µg/mL | 64 µg/mL | |
| S. aureus ATCC 6538 | 50.4 | 37.8 | 29.4 |
| 42B | 45.2 | 25.4 | 0 |
| 62EN | 10.3 | 8.6 | 0 |
| 68EA | 13.3 | 0 | 0 |
| 99W | 35.7 | 25.9 | 20.2 |
B Burn, EN Endotracheal aspirate, EA Ear, W Wound
Characterization of effect of combination between ZnO-NPs and antibiotics on S. aureus biofilm formation
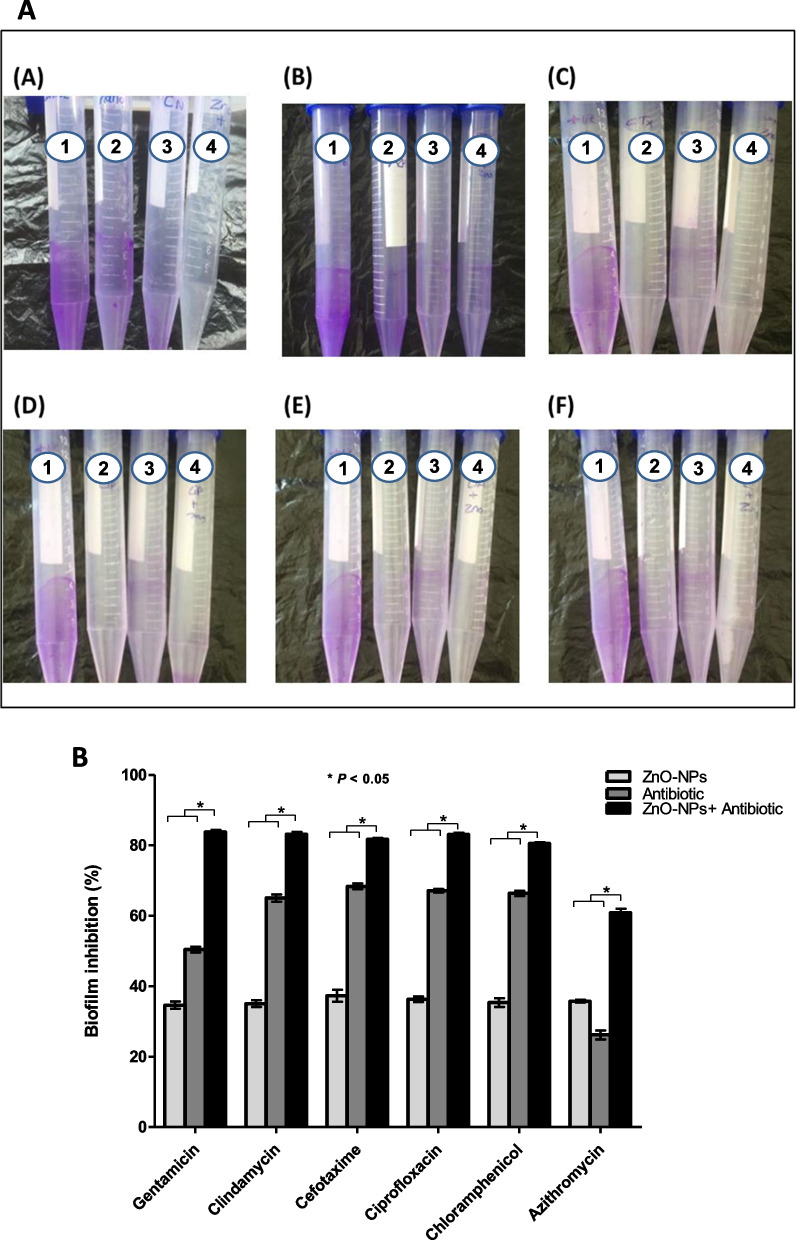
The synergistic effect of combination between ZnO-NPs and tested antibiotics on biofilm inhibition against S. aureus ATCC 6538 was investigated by the test tube method (Fig. 3A). Results show that ZnO-NPs alone were capable of inhibiting biofilm formation by 34–37%. However, combination of ZnO-NPs and various antibiotics inhibited biofilm formation by 65–85% (Fig. 3B).
Fig. 3.
A Antibiofilm assay by test tube method. The first tube in all images represents a positive control. The second and third tubes represent biofilm formed by bacterial cells in presence of antibiotic and ZnO-NPs; respectively. The fourth tube represents the biofilm formed by bacterial cells in presence of a combination of both antibiotic and ZnO-NPs. A; Gentamicin, B; Azithromycin, C; Cefotaxime, D; Ciprofloxacin, E; Clindamycin, and F; Chloramphenicol. B A combination between ZnO-NPs and antibiotics reduces S. aureus biofilm formation. Bacteria biofilms were stained with 1% crystal violet and percentage of biofilm inhibition was analyzed spectrophotometrically. Results are expressed as mean ± SE of three independent experiments. * P < 0.05 was considered significant using 2way ANOVA test
Characterization of synergy between ZnO-NPs and antibiotics by checkerboard microdilution assay
The synergistic potential of ZnO-NPs with commonly used antibiotics; gentamicin, ciprofloxacin, clindamycin, chloramphenicol, cefotaxime and azithromycin to inhibit planktonic S. aureus ATCC 6538 was determined. Synergy was studied by the checkerboard method by determining the FICI (fractional inhibitory concentration index). Importantly, the MICs values for tested antibiotics were reduced when combined with ZnO-NPs giving FIC values ≤ 0.5 indicating a synergistic effect (Table 4). The combination MICs of gentamicin, ciprofloxacin, chloramphenicol, cefotaxime, clindamycin and azithromycin on the S. aureus ATCC 6538 dropped to 0.25, 0.125, 0.125, 4, 0.003 and 0.125 µg/mL in contrast to the individual MICs of 4, 2, 4, 128, 0.03 and 0.05 µg/mL, respectively. All tested antibiotics in combination with ZnO-NPs showed a synergistic effect with FICIs ranging from 0.045 to 0.312.
Table 4.
Fractional inhibitory concentration index (FICI) of ZnO-NPs and tested antibiotics against S. aureus ATCC 6538
| Agent | FIC | FICI | Interpretation |
|---|---|---|---|
| ZnO-NPs | 0.015 | 0.075 | S |
| Gentamicin | 0.06 | ||
| ZnO-NPs | 0.062 | 0.122 | S |
| Ciprofloxacin | 0.06 | ||
| ZnO-NPs | 0.25 | 0.28 | S |
| Chloramphenicol | 0.03 | ||
| ZnO-NPs | 0.015 | 0.045 | S |
| Cefotaxime | 0.03 | ||
| ZnO-NPs | 0.062 | 0.162 | S |
| Clindamycin | 0.1 | ||
| ZnO-NPs | 0.062 | 0.312 | S |
| Azithromycin | 0.25 |
FIC Fractional inhibitory concentration, FICI Fractional inhibitory concentration index, S Synergism
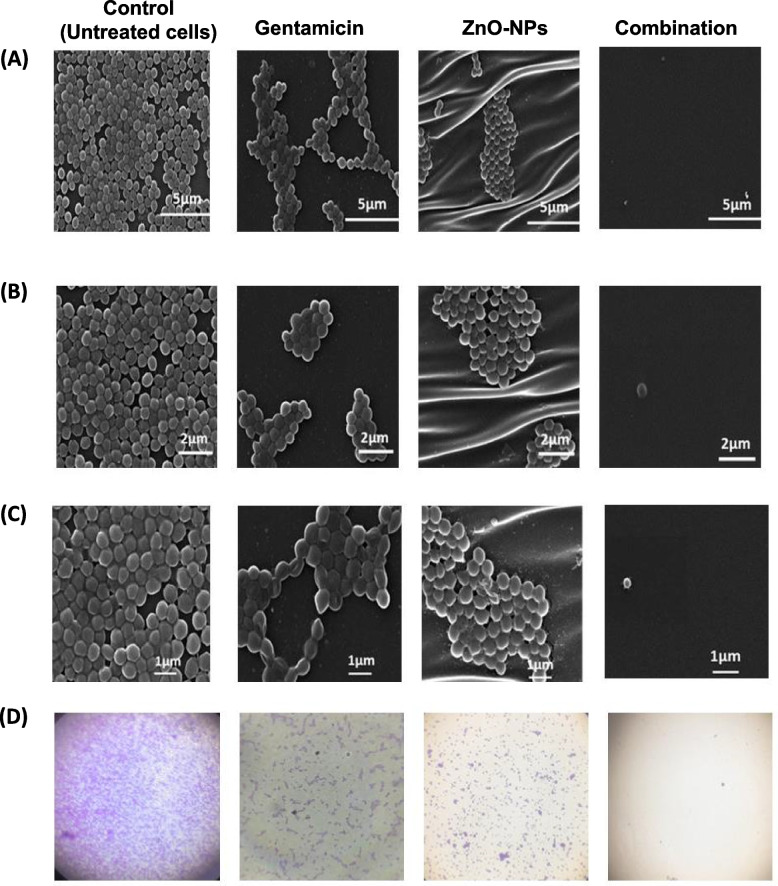
Microscopical characterization of ZnO-NPs-induced inhibition of S. aureus biofilm formation
The effect of ZnO-NPs on S. aureus biofilm was further characterized using both SEM and light microscopy. S. aureus biofilm was allowed to develop on the surface polystyrene discs in the presence of 0.78 mM ZnO-NPs (64 µg/mL), gentamicin (2 µg/mL) as well as their combination and compared to untreated cells. The morphology of S. aureus biofilm architecture formed was visualized microscopically under various magnifications. Under 5000 × and 7500 × magnification, SEM analysis revealed a thick, dense and fully established biofilm consisting of multi-layered bacterial cells for untreated cells (Fig. 4A & B). Upon treatment with ZnO-NPs or gentamicin, biofilm production was highly disrupted and a minimum biofilm mass was detected on polystyrene discs. Bacteria appeared as a monolayer of dispersed cells scattered on the surface. At higher magnification (10000x), untreated S. aureus appeared as large aggregates of cells in overlapped layers (Fig. 4C). In contrast, bacteria treated with ZnO-NPs or gentamicin presented as a uniform layer of cells with minimal clumping. Treatment with a combination of ZnO-NPs and gentamicin significantly lowered bacterial biofilm formation where there was a marked disruption of biofilm production and a negligible biofilm mass was detected (Fig. 4 A, B & C). The results obtained by SEM analysis were in agreement with those revealed by light microscopy (Fig. 4D). Microscopical images validate the data from the crystal-violet biofilm assay indicating a potential role of ZnO-NPs in inhibition of S. aureus biofilm formation.
Fig. 4.
Microscopic visualization of antibiofilm activity of ZnO-NPs, gentamicin and their combination against S. aureus. Scanning electron micrographs at various magnifications; A) 5000X, B) 7500X and C) 10000X. D) Light microscope images (100X magnification)
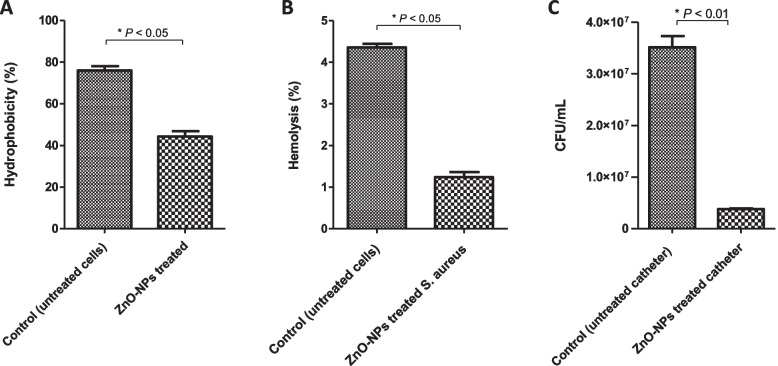
Evaluation of hydrophobicity index
Changes in cell surface hydrophobicity of S. aureus ATCC 6538 cells following exposure to sub-MIC of ZnO-NPs 64 µg/mL (0.78 mM) were investigated. Higher hydrophobicity of bacteria means increased cell adherence to various surfaces that enhances biofilm formation. As shown in Fig. 5A, S. aureus surface hydrophobicity was significantly (P < 0.05) affected upon treatment with sub-MIC of ZnO-NPs. On contrast to untreated bacteria that showed higher surface hydrophobicity (76% ± 1.2) the cell surface hydrophobicity of ZnO-NPs-treated cells was significantly reduced (44.33% ± 1.5). These results clearly indicate that ZnO-NPs were capable of altering S. aureus cell surface hydrophobicity and consequently the bacterial biofilm forming capacity could be decreased.
Fig. 5.
A ZnO-NPs reduced hydrophobicity index of S. aureus. Bacterial cells were grown overnight in presence and absence of ZnO-NPs. Bacterial density adjusted to 1.0 ± 0.01, then 1 ml of toluene was added to bacterial suspension. After that optical density of aqueous phase was measured. B ZnO-NPs inhibited S. aureus-induced haemolysis. RBCs were incubated with S. aureus alone (control) or S. aureus treated with ZnO-NPs. Percentages of haemolysis were measured. C ZnO-NPs decreased S. aureus biofilm formation on urinary catheter. Catheter segments were immersed in S. aureus culture in presence or absence of sub-MIC of ZnO-NPs. Following incubation for 48 h, bacterial counts on the surface of catheter were determined after serial dilution in PBS and plating on mannitol salt agar. The total number of biofilm cells of ZnO-NPs treated catheters was significantly (*P < 0.05) less than untreated catheter. All results are expressed as means ± SE of three independent experiments using Student’s t test
Haemolysis assay
Pre-incubation of S. aureus with sub-MIC of ZnO-NPs decreased the S. aureus-induced RBCs lysis. As shown in Fig. 5B, ZnO-NPs treated bacterial cells exhibited a significant decrease in hemolysis capacity (1.24% ± 0.08) relative to control untreated bacteria (4.35% ± 0.12). Of note that, no hemolysis was observed when RBCs incubated with ZnO-NPs alone at used concentration (0.78 mM). These findings indicate that prior treatment of S. aureus by ZnO-NPs interferes with the hemolytic capability of S. aureus.
In vitro inhibition of S. aureus biofilm formation on urinary catheter by ZnO-NPs
The capacity of ZnO-NPs to inhibit staphylococcal biofilms on the surface of urinary catheter was evaluated. Treatment with ZnO-NPs (0.78 mM) showed a significant reduction in biofilm mass and bacterial count (Fig. 5C). The bacterial cell count on the surface of ZnO-NPs treated catheter (3.50 × 104 ± 2.1 × 106 CFU/mL) was markedly lower than that (3.5 × 107 ± 1.5 × 105 CFU/mL) on the surface of control untreated catheter. These results clearly indicate that ZnO-NPs possess a potent antibiofilm activity on S. aureus biofilms growing on catheters.
Influence of ZnO-NPs on expression of S. aureus biofilm and oxidative stress genes
The expression levels of biofilm genes, catalase; katA and sigB were determined in both ZnO-NPs treated and untreated S. aureus ATCC 6538 by qRT-PCR. The expression of icaA, sarA, katA and sigB was significantly repressed in ZnO-NPs treated bacteria as compared to untreated cells. On the other hand, the expression of icaR and agrA that plays a role in biofilm formation was significantly induced in ZnO-NPs treated S. aureus relative to untreated cells (Fig. 6). These results indicate that exposure of S. aureus to ZnO-NPs negatively affects the expression of genes involved in both biofilm formation and oxidative stress response.
Fig. 6.
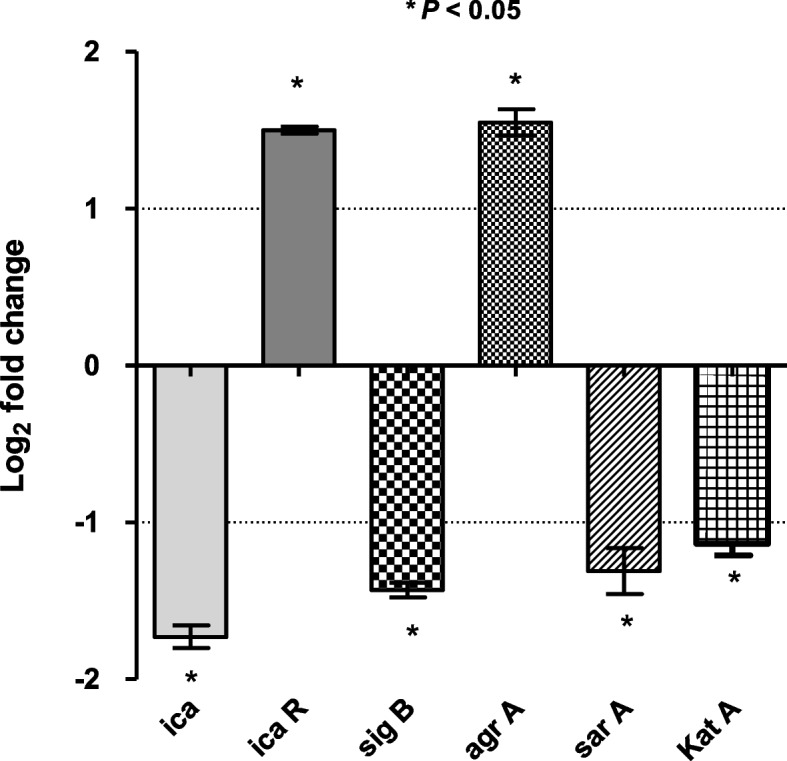
Characterization of influence of ZnO-NPs on the expression of S. aureus biofilm and oxidative stress genes by RT- qPCR. The expression levels of icaA, icaR, agrA, sarA, katA and sigB in both ZnO-NPs treated and untreated S. aureus ATCC 6538 were analyzed by qRT-PCR. The expression level of each gene was normalized to 16S rRNA and expression foldchange was calculated by the 2−∆∆CT method. The data shown are the means ± standard errors from three biological experiments with three technical replicates each. * P < 0.05was considered significant
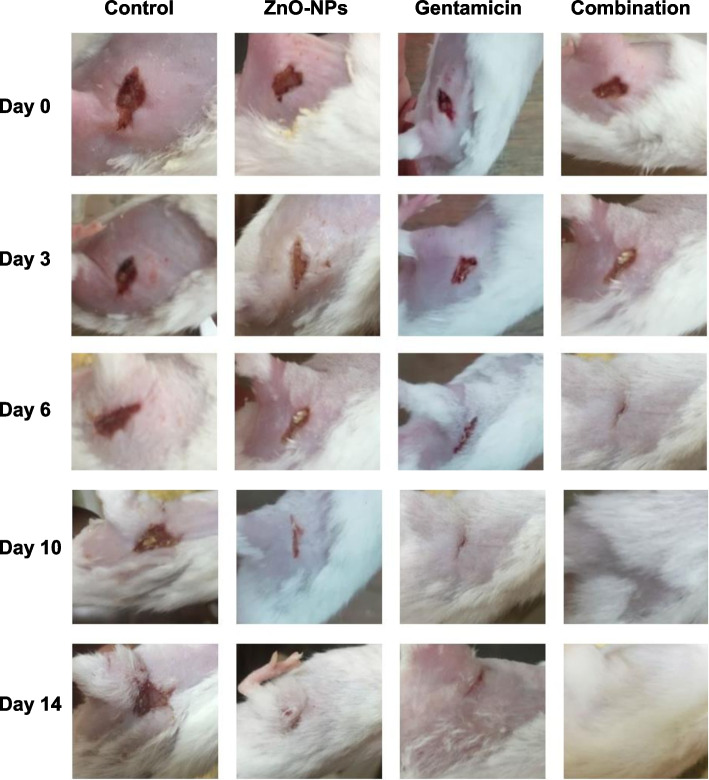
In vivo characterization of the influence of ZnO-NPs on S. aureus pathogenesis using mice infection models
The impact of ZnO-NPs on S. aureus pathogenesis was further characterized in this study. Importantly, wounds on mice in control groups, both untreated and PBS-treated mice, did not heal completely over the experiment course. Skin wounds in mice treated with ZnO-NPs or gentamicin alone needed more time to heal and did not show complete healing until day 14 (Fig. 7). However, topical application of both gentamicin and ZnO-NPs simultaneously increased the progression of wound healing in comparison with mice treated with gentamicin or ZnO-NPs alone. There was a noticeable improvement in wound closure of mice treated with a combination of gentamicin and ZnO-NPs at day 6 with complete wound healing at day 10 (Fig. 7 and Table 5). It is worth mentioning that no adverse effects were observed on mice body weight, general health or behavior during treatment. These results obviously indicate that ZnO-NPs have the potential to accelerate antibiotic action on skin wound promoting rapid closure and healing in wounds of S. aureus-infected mice.
Fig. 7.
ZnO-NPs improved healing of full thickness wounds in mice. Mice were anesthetized and hair on their backs was shaved. Skin wounds were created and inoculated with S. aureus (2.5 × 107 CFU∕mL) at wound site. Wounds were treated with gentamicin, ZnO-NPs or a combination of both. Progression of wound healing was monitored and images of skin wounds on mice from various groups were taken on day 0, 3, 6, 10, and 14 after creation of wound and treatment and represented. Treatment of mice with both ZnO-NPs and gentamicin together accelerates wound healing relative to control untreated mice and those treated with ZnO-NPs or gentamicin alone
Table 5.
Effect of ZnO-NPs, gentamicin and their combination on wound area
| Mice group | Wound area (mm2)/ (% of wound contraction) | ||||
|---|---|---|---|---|---|
| Days post treatment | |||||
| Day zero | Day 3 | Day 6 | Day 10 | Day 14 | |
| Control (Untreated mice) | 72 mm2 | 72 mm2 | 72 mm2 | 70 mm2 | 64 mm2 |
| ZnO-NPs treated mice | 72 mm2 |
48 mm2 (33.3%) |
30 mm2 (58.3%) |
15 mm2 (79.1%) |
0 mm2 (100%)a |
| Gentamicin treated mice | 72 mm2 | 45 mm2 (37.5%) |
25 mm2 (65.3%) |
10 mm2 (86.1%) |
0 mm2 (100%)a |
| ZnO-NPs + gentamicin treated mice | 72 mm2 |
21 mm2 (70.8%) |
5 mm2 (93%) |
0 mm2 (100%)a |
0 mm2 (100%)a |
aComplete healing
Discussion
S. aureus infection has been alarming mainly due to its resistance to multiple antibiotics. Bacterial ability to form biofilm is considered a big challenge that enhances bacterial capacity to resist antimicrobial agents making bacterial eradication is very difficult [26]. In the current study, the ability of S. aureus isolates to form biofilm was quantitatively evaluated. Approximately 99% of S. aureus isolates were capable of forming biofilms with variable degrees. Noticeably, 54.8% of S. aureus isolates were found to be strong biofilm producers. These findings could account for the higher resistance rates developed by S. aureus isolates to various antibiotics tested herein.
Failure to develop new antibiotics, combined with the spread of microbial resistance, may lead to increased morbidity and mortality, especially in health care facilities. Novel strategies for prevention and eradication of bacterial biofilm are urgently required to modify the traditional treatments. In the present study, the approach of using nanoparticles in inhibition of bacterial biofilms was characterized comprehensively. One of the most important used nanoparticles as antibiofilm agent is ZnO-NPs. ZnO-NPs have been previously evaluated for their antibacterial and antibiofilm activity against S. aureus and P. aeruginosa. The antibiofilm and antibacterial activity of ZNO-NPs is thought to be due to the production of reactive oxygen species (ROS) such as superoxide anion, hydroxyl radicals, and hydrogen peroxide that negatively affect bacterial cells [27]. Accumulation of ZnO-NPs in the outer membrane of bacterial cell trigger Zn2+ release, which would cause bacterial cell membrane disintegration, membrane protein damage and genomic instability resulting in the death of bacterial cells. Furthermore, ZnO-NPs suppress amyloid peptide fibrillation essential for bacterial biofilm formation [28]. In addition to the antibacterial potential, it has been shown that ZnO-NPs could possess a potent antiviral activity. The antiviral activity of ZnO-NPs has been shown to be related to prevention of viral entry, viral replication and spreading to organs which can eventually trigger ROS leading to oxidative injury and viral death [29]. Furthermore, zinc containing compounds exhibit antiviral activity through attachment to virus, inhibition of virus infection and uncoating in addition to inhibition of viral polymerases and protease. Finally, the antiviral activity of ZnO-NPs against HSV-1 could be due to trapping the virions and hence block the viral entrance into target cells as well as the selective inhibitory effect of Zn+2 on viral polymerase [30].
The antibiofilm activity of ZnO-NPs against S. aureus ATCC 6538 and four bacterial isolates recovered from different clinical sources; burn, endotracheal aspirate, wound and ear infection, was fully characterized. Importantly, ZnO-NPs exhibited a good antibiofilm activity against S. aureus. This antibiofilm activity was found to be concentration-dependent, which further confirms its efficiency as antibiofilm agents. The antibiofilm activity of ZnO-NPs can be explained by interference with bacterial biofilm integrity. ZnO-NPs affect exopolysaccharide synthesis that plays a crucial role in bacterial initial adhesion to host cells and development of a complex biofilm. Moreover, it was shown that ZnO-NPs could easily penetrate bacterial cell wall and kill the harmful microorganism quickly [31].
Current results indicate a synergistic antibiofilm effect in all combinations between ZnO-NPs and tested antibiotics. This synergistic effect could be due to the interaction between antibiotics and ZnO-NPs. Nanoparticles have large surface area which allows them to closely interact with antibiotics. Antibiotic molecules that contain active groups like hydroxyl and amido groups can easily react with ZnO-NPs by chelation and consequently their diffusion and penetration through biofilm and exhibiting their antimicrobial activity against bacterial cells is largely improved. Ryan et al. (2001) reported that ZnO-NPs could inhibit efflux pump system that mediates bacterial resistance to different antibiotics [32]. In addition, ZnO-NPs induce production of free radicals that significantly attach to thiol-containing proteins in bacterial cell wall and ultimately resulting in higher degradation potency [33].
Targeting cell surface hydrophobicity is a novel way of inhibiting biofilm formation. Cell surface hydrophobicity and exopolysaccharide play an important role in bacterium-host cell interactions and biofilm architectures in microbes. Previous reports confirm that interference with cell surface hydrophobicity would help combat biofilm production in different microorganisms including S. aureus. Furthermore, the increased hydrophobicity of bacterial cell surface could result in improved cell adherence to various surfaces such as mucosal epithelial cells and phagocytes [34]. Current results show that treating S. aureus with ZnO-NPs reduces cell surface hydrophobicity as compared to untreated cells. These finding agreed with Pati et al. (2014) who reported that treatment with ZnO-NPs reduces cell surface hydrophobicity of both S. aureus and P. aeruginosa and leads to inhibition of biofilm formation [35].
The effect of ZnO-NPs on S. aureus virulence was investigated herein. S. aureus produces a plethora of extracellular virulence factors and enzymes to invade and establish infections in the host system. The α-hemolysin is one such kind of exotoxin which is highly potent in lysis of various host cells such as erythrocytes, macrophages, monocytes, endothelial cells and epithelial cells. Importantly, S. aureus-induced lysis of RBCs was greatly reduced upon treatment of bacterial cells with ZnO-NPs. It is possible that ZnO-NPs bind to bacteria and mask the ligands making them less accessible for binding to RBCs [35].
Biofilms represent the major challenging problem for treatment of catheter-associated urinary tract infections (CAUTIs). S. aureus is an opportunistic pathogen that is considered a significant uropathogen in CAUTIs [36]. Importantly, treatment with ZnO-NPs significantly reduced total number of S. aureus biofilm cells on catheter as compared to control untreated catheter. These findings indicate that ZnO-NPs inhibited biofilm formation and thus could be effective in preventing catheter-related urinary tract infections and have the potential to control biofilms in device-associated S. aureus infections.
The gene expression profiles of ZnO-NPs treated S. aureus were studied in order to further investigate the inhibitory mechanism of ZnO-NPs on bacterial biofilm formation. Interestingly, exposure of S. aureus to ZnO-NPs affects the expression of genes involved in both biofilm formation and oxidative stress response. The expression of biofilm-related genes (icaA and sarA) and oxidative stress gene katA as well as the general regulator sigB was significantly repressed in ZnO-NPs treated bacteria as compared to untreated cells. On the other hand, the expression of accessory gene regulator; agrA was significantly induced in S. aureus upon treatment with ZnO-NPs. It has been reported that agr is a dominant regulator of biofilm development and formation. Activation of agr induces dispersion S. aureus cells to transit to planktonic state, so biofilm initiation, adhesion and maturation require low agr transcription. Numerous studies on S. aureus have shown that agrA mutants possessed increased capacity to form biofilm [37, 38] which agreed with current observations that the inhibition of biofilm formation by ZnO-NPs could be due to induced expression of agrA.
The staphylococcal accessory regulator, sarA is a well-known global master regulator of biofilm and virulence genes in S. aureus. Present results revealed the downregulation of sarA in S. aureus upon ZnO-NPs treatment. It is well known that intracellular adhesion genes icaA and icaD are positively regulated by sarA. Both icaA and icaD are involved in slime synthesis and therefore play an important role in S. aureus biofilm formation [39]. Decreased expression of icaA and icaD in S. aureus following treatment with ZnO-NPs could account for the impairment of biofilm formation observed herein. In addition, expression of MSCRAMMs that are involved in the initial stage of biofilm formation including FnbA, FnbB and ClfA are regulated by sarA [40, 41], which further supports that reduced expression of sarA has a negative impact on bacterial biofilm formation by S. aureus.
Reduced biofilm formation in ZnO-NPs treated S. aureus could be further explained by repression of sigB in cells upon treatment with ZnO-NPs. S. aureus mutants in the global regulator sigB are unable to form a biofilm in vitro [42]. It is possible that sigB inhibition will also disperse an established biofilm. Repression of sigB in established S. epidermidis biofilms led to a pronounced dispersal event, suggesting that a similar mechanism may occur in S. aureus. Finally, treatment of S. aureus with ZnO-NPs resulted in the downregulation of catalase, which further account for the antibacterial efficiency of ZnO-NPs. S. aureus expresses a number of proteins that play a critical role in protecting cells against different stresses especially oxidative stress. For instance, KatA enables S. aureus to survive oxidative stress through inactivation of H2O2 and interrupting the formation of toxic ROS [43].
The influence of ZnO-NPs on S. aureus pathogenesis was evaluated herein using mice infection model. Treating S. aureus with ZnO-NPs markedly affects its pathogenesis in host. Current findings indicate that ZnO-NPs could be used as topical anti-infective agent especially in combination with commonly used antibiotics such as gentamicin. Mechanism of ZnO-NPs underlying this effect may be due to production of ROS that damage bacterial cells, interference with biofilm integrity by interrupting exopolysaccharide synthesis that plays a crucial role in development of a complex biofilm [44]. Moreover, interruption of bacterial energy transduction and enzyme activity as well as bacterial DNA synthesis by ZnO-NPs could lead to enhanced bacterial clearance during wound healing and make bacterial cells more susceptible to antibiotic treatment [45].
Conclusion
In this work, the antibacterial and antibiofilm activity of ZnO-NPs against S. aureus have been extensively characterized both in vitro and in vivo. Interestingly, ZnO-NPs exhibited a potent antibiofilm activity against S. aureus. Furthermore, ZnO-NPs significantly enhanced S. aureus susceptibility toward various antibiotics and markedly reduced its pathogenesis in host. Importantly, the present study shed light on the antibacterial and antibiofilm mechanisms of ZnO-NPs. For instance, ZnO-NPs exhibit antibiofilm activity against S. aureus through affecting bacterial cell surface hydrophobicity and genes involved in biofilm formation. The antivirulent potential of ZnO-NPs observed herein could be attributed to the down regulation of S.aureus virulent genes upon exposure to ZnO-NPs. In addition, S. aureus-induced lysis of RBCs was greatly reduced following treatment of bacterial cells with ZnO-NPs. Finally, ZnO-NPs markedly impaired S. aureus pathogenesis in mice infection model. The findings of current study greatly extend our knowledge about ZnO-NPs as a potent antibiofilm and antivirulent agent. In summary, current study in addition to the previously published ones further support the promising role of ZnO-NPs as antibacterial and antibiofilm agent especially against the important pathogen S. aureus. ZnO-NPs could be considered as a valuable adjuvant in combination therapy with traditionally used antibiotics.
Supplementary Information
Additional file 1: Supplementary Table S1. Comparison between different types of nanomaterials based on their advantages and disadvantages.
Additional file 2. Supplementary Table S2. Susceptibility profiles of S. aureus isolates against various antimicrobial agents.
Additional file 3: Supplementary Table S3. MIC values for both antibiotics and ZnO-NPs against S. aureus.
Acknowledgements
The authors would like to acknowledge the medical staff at clinical laboratories of Zagazig University Hospitals and El-Ahrar Educational Hospital in Zagazig, Egypt for providing clinical S. aureus isolates for this study.
Abbreviations
- MH broth
Mueller Hinton
- S
Susceptible
- I
Intermediate
- R
Resistant
- MIC
Minimum inhibitory concentration
- ZnO-NPs
Zinc oxide nanoparticles
- mm
Millimeter
- OD
Optical density
- MBIC
Minimum biofilm inhibitory concentration
- TS
Trypticase soy
- FICI
Fractional inhibitory concentration index
- HI
Hydrophobicity index
- MDR
Multidrug resistant
- RBCs
Red blood cells
- ROS
Reactive oxygen species
Authors’ contributions
Conceptualization, A.A., and M.A; methodology, A.A., and M.A; validation, A.A., and M.A; investigation, A.A., and M.A; data curation, A.A., and M.A; writing-original draft preparation, A.A., and M.A; writing-review and editing, A.A., and M.A; visualization, A.A., N.Y., and M.A; supervision, N.Y and M.A.; All authors have read and agreed to the published version of the manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article.
Declarations
Ethics approval and consent to participate
Ethical approval
The study was carried out according to the Declaration of Helsinki. Informed consent from the subjects was NOT required. All mentioned procedures in the animal study were performed according to Guide for the Care and Use of Laboratory Animals (8th edition, National Academies Press). The animal study was approved by the institutional animal care and used committee, Zagazig University (ZU-IACUC) with approval number ZU-IACUC/3/F/159/2019. The study was performed in compliance with the ARRIVE (Animal Research: Reporting of In Vivo Experiments) guidelines. Clinical S. aureus isolates were kindly provided by the medical stuff at clinical laboratories of Zagazig University Hospitals and El-Ahrar Educational Hospital in Zagazig, Egypt. The patients were NOT directly involved in the current study and therefore the consent to participate from patients was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Aliaa Abdelghafar, Email: dr306aliaa@gmail.com.
Nehal Yousef, Email: dr.nehalyousef@gmail.com.
Momen Askoura, Email: momenaskora@yahoo.com.
References
- 1.Gnanamani A, Hariharan P, Paul-Satyaseela M. Staphylococcus aureus: Overview of Bacteriology, Clinical Diseases, Epidemiology, Antibiotic Resistance and Therapeutic Approach. In: Enany S, Alexander LEC, editors. Frontiers in Staphylococcus aureus. London: IntechOpen; 2017. 10.5772/67338.
- 2.Schulze A, et al. Biofilms by bacterial human pathogens: Clinical relevance-development, composition and regulation-therapeutical strategies. Microbial Cell. 2021;8(2):28. doi: 10.15698/mic2021.02.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedarat Z, Taylor-Robinson AW. Biofilm Formation by Pathogenic Bacteria: Applying a Staphylococcus aureus Model to Appraise Potential Targets for Therapeutic Intervention. Pathogens. 2022;11(4):388. doi: 10.3390/pathogens11040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naskar A, Kim KS. Nanomaterials as delivery vehicles and components of new strategies to combat bacterial infections: advantages and limitations. Microorganisms. 2019;7(9):356. doi: 10.3390/microorganisms7090356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaushik S. Polymeric and ceramic nanoparticles: possible role in biomedical applications. In: Hussain CM, Thomas S, editors. Handbook of polymer and ceramic nanotechnology. Cham: Springer; 2021. p. 1293–308. 10.1007/978-3-030-40513-7_39.
- 6.Elshama SS, Abdallah ME, Abdel-Karim RI. Zinc oxide nanoparticles: therapeutic benefits and toxicological hazards. Open Nanomed J. 2018;5(1):16–22. [Google Scholar]
- 7.Jiang J, Pi J, Cai J. The advancing of zinc oxide nanoparticles for biomedical applications. Bioinorg Chem Appl. 2018. [DOI] [PMC free article] [PubMed]
- 8.Alvi M, Al-Ghamdi A, ShaheerAkhtar M. Synthesis of ZnO nanostructures via low temperature solution process for photocatalytic degradation of rhodamine B dye. Mater Lett. 2017;204:12–15. [Google Scholar]
- 9.Singh S, et al. Cholesterol biosensor based on rf sputtered zinc oxide nanoporous thin film. Appl Phys Lett. 2007;91(6):063901. [Google Scholar]
- 10.Ozdal M, Gurkok S. Recent advances in nanoparticles as antibacterial agent. ADMET DMPK. 2022;10(2):115–129. doi: 10.5599/admet.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinhas R, et al. Gold nanoparticle-based theranostics: disease diagnostics and treatment using a single nanomaterial. Nanobiosensors Dis Diagn. 2015;4:11. [Google Scholar]
- 12.Selvarajan V, Obuobi S, Ee PLR. Silica nanoparticles—a versatile tool for the treatment of bacterial infections. Front Chem. 2020;8:602. doi: 10.3389/fchem.2020.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alavi M, Thomas S, Sreedharan M. Modification of silica nanoparticles for antibacterial activities: mechanism of action. Micro Nano Bio Aspects. 2022;1(1):49–58. [Google Scholar]
- 14.CLSI. Performance standards for antimicrobial susceptibility testing. 29th ed. Wayne, PA, USA: CLSI supplement M100; clinical and laboratory standards institute; 2018.
- 15.Namvar, F., H. S. Rahman, R. Mohamad, S. Azizi, P. M. Tahir, M. S. Chartrand and S. K. Yeap (2015). "Cytotoxic effects of biosynthesized zinc oxide nanoparticles on murine cell lines." Evidence-Based Complementary and Alternative Medicine 2015. [DOI] [PMC free article] [PubMed]
- 16.Stepanović S, Vuković D, Hola V, Bonaventura GD, Djukić S, Ćirković I, Ruzicka F. Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS. 2007;115(8):891–899. doi: 10.1111/j.1600-0463.2007.apm_630.x. [DOI] [PubMed] [Google Scholar]
- 17.Sabino HAC, et al. Biofilm and Planktonic Antibiotic Resistance in Patients With Acute Exacerbation of Chronic Rhinosinusitis. Front Cell Infect Microbiol 2022:1413. [DOI] [PMC free article] [PubMed]
- 18.Basumatari M, et al. Musa balbisiana Colla pseudostem biowaste mediated zinc oxide nanoparticles: Their antibiofilm and antibacterial potentiality. Curr Res Green Sustain Chem. 2021;4:100048. [Google Scholar]
- 19.Ashajyothi C, Manjunath K, Chandrakanth R. Prevention of multiple drug resistant bacterial biofilm by synergistic action of biogenic silver nanoparticle and antimicrobials. J Microbiol Biotech Res. 2015;5(1):7. [Google Scholar]
- 20.Ashajyothi C, Harish KH, Dubey N, Chandrakanth RK. Antibiofilm activity of biogenic copper and zinc oxide nanoparticles-antimicrobials collegiate against multiple drug resistant bacteria: a nanoscale approach. J Nanostructure Chem. 2016;6(4):329–341. [Google Scholar]
- 21.Rauf MA, Owais M, Rajpoot R, Ahmad F, Khan N, Zubair S. Biomimetically synthesized ZnO nanoparticles attain potent antibacterial activity against less susceptible S. aureus skin infection in experimental animals. RSC Advances. 2017;7(58):36361–36373. [Google Scholar]
- 22.Bai J-R, Zhong K, Wu Y-P, Elena G, Gao H. Antibiofilm activity of shikimic acid against Staphylococcus aureus. Food Control. 2019;95:327–333. [Google Scholar]
- 23.Mandakhalikar KD, Rahmat JN, Chiong E, Neoh KG, Shen L, Tambyah PA. Extraction and quantification of biofilm bacteria: method optimized for urinary catheters. Sci Rep. 2018;8(1):8069. doi: 10.1038/s41598-018-26342-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diniz FR, et al. Silver nanoparticles-composing alginate/gelatine hydrogel improves wound healing in vivo. Nanomaterials. 2020;10(2):390. doi: 10.3390/nano10020390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adibhesami M, et al. Effects of silver nanoparticles on Staphylococcus aureus contaminated open wounds healing in mice: an experimental study. in Veterinary Research Forum. 2017. Faculty of Veterinary Medicine, Urmia University, Urmia, Iran. [PMC free article] [PubMed]
- 26.Basanisi M, La Bella G, Nobili G, Franconieri I, La Salandra G. Genotyping of methicillin-resistant Staphylococcus aureus (MRSA) isolated from milk and dairy products in South Italy. Food Microbiol. 2017;62:141–146. doi: 10.1016/j.fm.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Mammari N, et al. Current knowledge on the oxidative-stress-mediated antimicrobial properties of metal-based nanoparticles. Microorganisms. 2022;10(2):437. doi: 10.3390/microorganisms10020437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoo SI, Yang M, Brender JR, Subramanian V, Sun K, Joo NE, Jeong SH, Ramamoorthy A, Kotov NA. Inhibition of amyloid peptide fibrillation by inorganic nanoparticles: functional similarities with proteins. Angew Chem Int Ed. 2011;50(22):5110–5115. doi: 10.1002/anie.201007824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El-Megharbel SM, Alsawat M, Al-Salmi FA, Hamza RZ. Utilizing of (zinc oxide nano-spray) for disinfection against “SARS-CoV-2” and testing its biological effectiveness on some biochemical parameters during (COVID-19 pandemic)—” ZnO nanoparticles have antiviral activity against (SARS-CoV-2)”. Coatings. 2021;11(4):388. [Google Scholar]
- 30.Tavakoli A, Ataei-Pirkooh A, Mm Sadeghi G, Bokharaei-Salim F, Sahrapour P, Kiani SJ, Moghoofei M, Farahmand M, Javanmard D, Monavari SH. Polyethylene glycol-coated zinc oxide nanoparticle: an efficient nanoweapon to fight against herpes simplex virus type 1. Nanomedicine. 2018;13(21):2675–2690. doi: 10.2217/nnm-2018-0089. [DOI] [PubMed] [Google Scholar]
- 31.Mahamuni-Badiger PP, et al. Biofilm formation to inhibition: Role of zinc oxide-based nanoparticles. Mater Sci Eng C. 2020;108:110319. doi: 10.1016/j.msec.2019.110319. [DOI] [PubMed] [Google Scholar]
- 32.Ryan BM, Dougherty TJ, Beaulieu D, Chuang J, Dougherty BA, Barrett JF. Efflux in bacteria: what do we really know about it? Expert Opin Investig Drugs. 2001;10(8):1409–1422. doi: 10.1517/13543784.10.8.1409. [DOI] [PubMed] [Google Scholar]
- 33.Jesline A, John NP, Narayanan P, Vani C, Murugan S. Antimicrobial activity of zinc and titanium dioxide nanoparticles against biofilm-producing methicillin-resistant Staphylococcus aureus. Appl Nanosci. 2015;5(2):157–162. [Google Scholar]
- 34.Kuttinath S, Murugan S, Rammohan R. Inhibition of Methicillin Resistant Staphylococcus aureus Biofilm by Ethanol Extracts of Sauropus androgynus and Solanum torvum. Indian J Pharm Sci. 2021;83(6):1155–1163. [Google Scholar]
- 35.Pati R, Mehta RK, Mohanty S, Padhi A, Sengupta M, Vaseeharan B, Goswami C, Sonawane A. Topical application of zinc oxide nanoparticles reduces bacterial skin infection in mice and exhibits antibacterial activity by inducing oxidative stress response and cell membrane disintegration in macrophages. Nanomedicine. 2014;10(6):1195–1208. doi: 10.1016/j.nano.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Navidinia M, et al. Molecular typing, biofilm formation, and analysis of adhesion factors in Staphylococcus aureus strains isolated from urinary tract infections. Gene Reports. 2021;22:101008. [Google Scholar]
- 37.Mootz JM, Malone CL, Shaw LN, Horswill AR. Staphopains modulate Staphylococcus aureus biofilm integrity. Infect Immun. 2013;81(9):3227–3238. doi: 10.1128/IAI.00377-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boles BR, Horswill AR. Agr-mediated dispersal of Staphylococcus aureus biofilms. PLoS Pathog. 2008;4(4):e1000052. doi: 10.1371/journal.ppat.1000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu M, Wu X, Li J, Liu L, Zhang R, Shao D, Du X. The specific anti-biofilm effect of gallic acid on Staphylococcus aureus by regulating the expression of the ica operon. Food Control. 2017;73:613–618. [Google Scholar]
- 40.Chung PY, Toh YS. Anti-biofilm agents: recent breakthrough against multi-drug resistant Staphylococcus aureus. Pathog Dis. 2014;70(3):231–239. doi: 10.1111/2049-632X.12141. [DOI] [PubMed] [Google Scholar]
- 41.Arya R, Ravikumar R, Santhosh R, Princy S. SarA based novel therapeutic candidate against Staphylococcus aureus associated with vascular graft infections. Front Microbiol. 2015;6:416. doi: 10.3389/fmicb.2015.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang H, et al. Alternative sigma factor B reduces biofilm formation and stress response in milk-derived Staphylococcus aureus. LWT. 2022;162:113515. [Google Scholar]
- 43.Beavers WN, Skaar EP. Neutrophil-generated oxidative stress and protein damage in Staphylococcus aureus. Pathog Dis. 2016;74(6):ftw060. doi: 10.1093/femspd/ftw060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Wrafy FA, et al. Nanoparticles approach to eradicate bacterial biofilm-related infections: a critical review. Chemosphere. 2022;288:132603. doi: 10.1016/j.chemosphere.2021.132603. [DOI] [PubMed] [Google Scholar]
- 45.Mandal AK, et al. Current Research on Zinc Oxide Nanoparticles: Synthesis, Characterization, and Biomedical Applications. Nanomaterials. 2022;12(17):3066. doi: 10.3390/nano12173066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table S1. Comparison between different types of nanomaterials based on their advantages and disadvantages.
Additional file 2. Supplementary Table S2. Susceptibility profiles of S. aureus isolates against various antimicrobial agents.
Additional file 3: Supplementary Table S3. MIC values for both antibiotics and ZnO-NPs against S. aureus.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.