Abstract
Exclusive acral involvement in neonatal pemphigus is unusual. Blisters in neonatal bullous pemphigoid, affecting 2%–3% of newborns of mothers with gestational pemphigoid, can be located in the trunk, limbs and acral areas. Unlike neonatal bullous pemphigoid, which can appear up to 5 days after birth, neonatal pemphigus is often revealed at birth. They are benign diseases in newborns. There is no correlation between the disease severity in babies and mothers. Neonatal risk is dominated by the side effects of corticosteroid therapy.
Keywords: blisters, bullous pemphigoid, neonates, pemphigus
Unlike neonatal bullous pemphigoid, which can appear up to 5 days after birth, neonatal pemphigus is often revealed at birth. They are benign diseases in newborns. Neonatal risk is dominated by the side effects of corticosteroid therapy.
1. INTRODUCTION
Neonatal autoimmune blistering dermatoses (AIBDs) relieve from different etiologies. Neonatal pemphigus (NP) and neonatal bullous pemphigoid (NBP) are rare and transient. 1 They result from the passive transplacental transfer of maternal autoantibodies to fetus through the placenta. 1 , 2 , 3 They can begin or can be exacerbated as the pregnancy progresses and immediately after delivery. Pemphigus becomes active in the second trimester of pregnancy and improves in the third trimester due to endogenous corticosteroid secretion from the placenta. 1 Female patients with AIBDs may experience stillbirth, high proportion of prematurely born neonates and even infertility. The adverse course of the disease during pregnancy is related to poor control as there are high titers of pemphigus or bullous pemphigoid antibodies. In fact, when autoantibodies affect the fetus early in gestation, the clinical sequelae may be more severe, causing a disproportionate effect on the desmosome, hemidesmosome and basement membrane zone adhesion points.
We report 2 cases of NP and a case of NBP with particular clinical presentations.
1.1. Cases 1 and 2
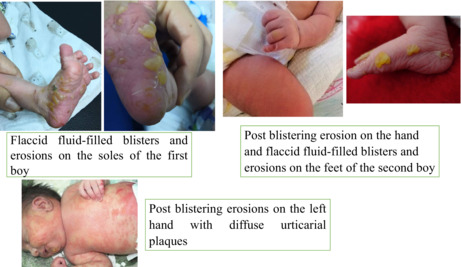
Two newborn boys presented in the first hour of life flaccid fluid‐filled blisters and erosions on the hands and feet (Figures 1, 2, 3) but the skin around blisters was normal while for the rest of their skin, no oral and genital mucosae was observed. The Apgar score was 9 and 10 after 1 and 10 min, respectively. The babies weighed 3200 and 2700 grams, respectively. At the initial dermatological screening, the following diagnoses were suggested: bullous impetigo, hereditary epidermolysis bullosa (HEB) or AIBDs, such as pemphigus or bullous pemphigoid. There was neither family history of HBE nor AIBDs. Other important differential diagnoses were the dermatological manifestation of TORCH and congenital varicella syndrome.
FIGURE 1.

flaccid fluid‐filled blisters and erosions on the soles of the first boy
FIGURE 2.

post blistering erosion on the hand of the second boy
FIGURE 3.

flaccid fluid‐filled blisters and erosions on the feet of the second boy
In the first boy, the diagnosis of bullous impetigo was the most likely to be made. Local care with antibiotic therapy was prescribed with good outcome. Fifteen days later, a follow‐up examination revealed plantar desquamation without new blisters.
His 25‐year‐old mother was very anxious. She confessed that she was being followed up for pemphigus vulgaris. Histology showed supra‐basal clefting with acantholysis in the deep epidermal layer. Direct immunofluorescence (DIF) revealed epidermal intercellular deposition of IgG and C3.
During pregnancy, she was treated with oral corticosteroid therapy (1 mg/kg/day). Her pemphigus was stable throughout the follow‐up with a gradual decline to 0.3 mg/kg/day. At the delivery, she had pigmented macules without active lesions.
For the second baby, his mother was followed up for pemphigus foliaceus in our dermatology department and treated by corticosteroid therapy (10 mg/day). Anti‐desmoglein 1 antibodies were positive over 200 UI/ml while anti‐desmoglein 3 antibodies were negative. Her disease became active again in the second trimester of pregnancy; however, the lesions went into remission after increasing the dose of corticosteroids to 1 mg/kg/day. Her baby was evaluated at the neonatology consultation on his 36th day of life. He was in complete remission of the condition after antiseptic care.
Based on the mother's medical history and the patient's lesions, the diagnosis of NP was retained for the two babies. They did not present new lesions after a 3‐month follow‐up.
1.2. Case 3
A newborn boy presented at birth with diffuse urticarial plaques on the trunk, face and limbs associated with post blistering erosions of the hands and feet (Figure 4) but in good health. His mother was followed up for gestational pemphigoid and an examination showed that she had vesiculo‐bullous lesions of the trunk and upper limbs. The lesions resolved after few weeks under topical corticosteroids without recurrence while the diagnosis was an NPB.
FIGURE 4.

post blistering erosions on the left hand with diffuse urticarial plaques
2. DISCUSSION
NP often affects the trunk and the cephalic region. Exclusive involvement of palms and feet is unusual. Unlike NP vulgaris, which is relatively frequent, NP foliaceus is a very rare disease entity. 4 It may be a result of desmoglein 3 over expression in neonatal epidermis. 5 , 6 Blisters in NBP, affecting 2%–3% of newborns of mothers with gestational pemphigoid, can be located in the trunk, limbs, and acral areas. 4 The clinical aspect could wrongly point to an infectious disease; hence, the importance of the mother examination and medical history screening. 3 According to recommendations for investigation of suspected DBAI, biopsy and DIF are not recommended if the mother has typical lesions. 5 If the diagnosis of AIBD is made before pregnancy, the latter should be scheduled. 5 The disease must be stable under the lowest dose of corticosteroid therapy to avoid its complications (low birth weight, prematurity, etc.). In our cases, the mothers were in clinical remission at delivery while the newborn had an active disease, without having the complications of corticosteroid therapy. NP and NBP have a good prognosis 4 and usually resolve within the first 3–5 weeks of life. 1 , 4 There is no correlation between the severity of the disease on the baby and the mother. 5 However, stabilization of the disease before conception remains essential.
3. CONCLUSION
Unlike neonatal bullous pemphigoid, which can appear up to 5 days after birth and have a male predominant, 4 , 5 neonatal pemphigus is often revealed at birth. They are benign diseases in newborns. Neonatal risk is dominated by the side effects of corticosteroid therapy.
AUTHOR CONTRIBUTIONS
RM, RC, KN, and SK wrote the manuscript. RC and SK revised the manuscript. RM, RC, KH, SK, BM, AM, MA, BTA, GA, and TH contributed to the management of the patient and revised the article. TH critically reviewed the manuscript and gave final approval. All authors have read and approved the final manuscript and agree to take full responsibility for the integrity and accuracy of the work.
CONFLICTS OF INTEREST
None.
DATA AVAILABLITY STATAMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ETHICAL APPROVAL
We have respected ethics of this journal and we have obtained the informed and written consent from the parents of the babies.
CONSENT
We accept the fact that this journal publish our cases.Written informed consent was obtained from the parents of the patients to publish this report in accordance with the journal's patient consent policy.
SOURCES THAT SUPPORTED THE WORK
None.
ACKNOWLEDGMENT
None.
Rekik M, Regaieg C, Sellami K, et al. Acral blisters in neonates: Three rare and benign diseases. Clin Case Rep. 2022;10:e06420. doi: 10.1002/ccr3.6420
This article is protected by copyright. All rights reserved.
REFERENCES
- 1. Carvalho AA, Santos Neto DAD, Carvalho MADR, Eleutério SJP, de Oliveira Xavier ARE. Neonatal pemphigus in an infant born to a mother with pemphigus vulgaris: a case report. Rev Paul Pediatr Orgao of Soc Pediatr Sao Paulo Mars. 2019;37(1):130‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kodagali SS, Subbarao SD, Hiremagaloor R. Pemphigus vulgaris in a neonate and his mother. Indian Pediatr Avr. 2014;51(4):316‐317. [PubMed] [Google Scholar]
- 3. Drerup K, Fölster‐Holst R. Neonatal pemphigus vulgaris. J Dtsch Dermatol Ges J Ger Soc Dermatol JDDG Juill. 2020;18(7):749‐753. [DOI] [PubMed] [Google Scholar]
- 4. Zhao CY, Murrell DF. Blistering diseases in neonates. Curr Opin Pediatr août. 2016;28(4):500‐506. [DOI] [PubMed] [Google Scholar]
- 5. Zhao CY, Chiang YZ, Murrell DF. Neonatal autoimmune blistering disease: a systematic review. Pediatr Dermatol Juill. 2016;33(4):367‐374. [DOI] [PubMed] [Google Scholar]
- 6. Schultz B, Hook K. Bullous diseases in children: a review of clinical features and treatment options. Paediatr Drugs. 2019;21(5):345‐356. [DOI] [PubMed] [Google Scholar]


