Abstract
BACKGROUND
Successful management of a vein of Galen malformation (VoGM) in the newborn patient requires a highly coordinated team approach involving neonatologists, pediatric cardiologists, pediatric neurologists, neurosurgeons, and interventionalists. Indication and timing of catheter intervention are topics of ongoing debate.
OBSERVATIONS
The authors highlighted two key echocardiographic markers believed to be practical indicators regarding the need for urgent catheter embolization in neonates with a VoGM. The first and preferred parameter was the tricuspid valve regurgitation (TR) gradient, an estimate of pulmonary artery hypertension. If the TR gradient exceeds systolic blood pressure (suprasystemic pulmonary hypertension [PH], i.e., >60 mm Hg), urgent intervention should be considered in eligible newborns. The second parameter was the left ventricular end-systolic eccentricity index (EI), a newly emerging echocardiographic marker and indirect correlate of PH. As an alternative to the TR gradient, an increased eccentricity index (>1.6) suggests severe right heart compromise, requiring emergency catheter embolization of the malformation. Postoperatively, the progressive reduction of both the TR gradient and the EI correlated with recovery.
LESSONS
In eligible newborns, urgent embolization of a VoGM is recommended in the presence of suprasystemic TR gradients and/or increased EI >1.6.
Keywords: vein of Galen malformation, embolization, TR gradient, eccentricity index, newborn
ABBREVIATIONS : CHF = congestive heart failure, EI = eccentricity index, LV = left ventricular, PAP = pulmonary artery pressure, PH = pulmonary hypertension, sPAP = systolic PAP, RV = right ventricular, TR = tricuspid valve regurgitation, VoGM = vein of Galen malformation
The indication and timing for emergency endovascular embolization of a vein of Galen malformation (VoGM) in the newborn remain controversial. Generally, the treatment indication follows a clinical score developed by Pierre Lasjaunias at the Bicetre Hospital in Paris.1 However, some of the score’s parameters leave room for subjective interpretation and therefore have limitations. Ultimately, the urgency for treatment is dictated by the degree of heart failure in eligible newborns. In this report, we highlight two basic, objective echocardiographic markers indicating the need for urgent catheter intervention: the tricuspid valve regurgitation (TR) gradient and the left ventricular (LV) end-systolic eccentricity index (EI).
Illustrative Case
A 3.1-kg boy was born via cesarean delivery at 36 weeks’ and 4 days’ gestation. He developed acute right heart failure, requiring intubation and mechanical ventilation shortly after birth. Chest radiography revealed a much-enlarged right heart (Fig. 1). A cranial bruit was observed, and subsequently a VoGM was diagnosed by ultrasound. He was transferred to our institution for definitive care.
FIG. 1.

Images to the left demonstrate the baby’s condition immediately after birth. A: Three-dimensional (3D) brain magnetic resonance angiography (MRA) revealing the complexity of this VoGM with numerous choroidal, pericallosal, and perforating feeding vessels. C: Axial T2-weighted MR imaging (MRI) of the brain at age 1 day demonstrating a giant venous aneurysm standing out with its smaller mural connector anteriorly. E: Chest radiograph obtained at birth demonstrating a massively enlarged right heart, indicative of heart failure causing severe soft tissue edema. Images to the right are during the 6- to 12-month follow-up period. B: One-year 3D MRA showing near resolution of the malformation. D: One-year axial T2-weighted MRI showing glue in the mural connector with substantial size reduction of the venous aneurysm. F: Six-month chest radiograph showing the nearly normal cardiac silhouette.
Clinically, the patient’s Bicetre score was 12. His echocardiogram was consistent with severe, suprasystemic pulmonary hypertension (PH), estimated by significant TR. At the time of the initial echo, his systolic blood pressure was 52 mm Hg versus an estimated pulmonary artery pressure (PAP) (TR gradient) of 68 mm Hg (Fig. 2). His LV end-systolic EI was markedly elevated at 1.69 because his enlarged right ventricle was compressing his left ventricle. The echo further revealed diastolic flow reversal in the aortic arch and descending aorta.
FIG. 2.
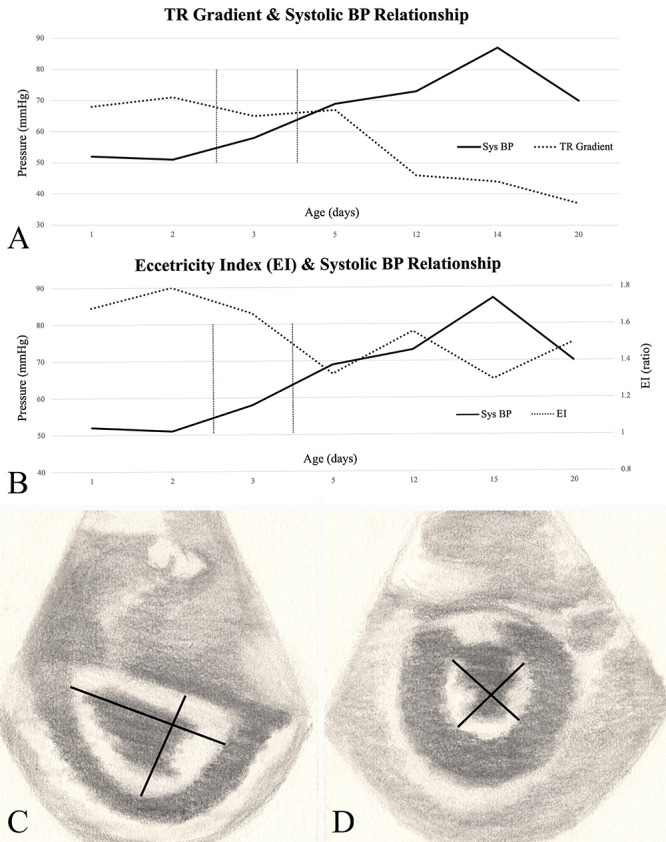
A: Correlation of PAP (estimated as the TR gradient) with systemic arterial pressure for the first 3 weeks of life in baby boy with a VoGM. At baseline, there is notable suprasystemic PH (i.e., the PAP exceeds the systolic pressure). Suprasystemic PH indicates a grave prognosis and the need for emergency intervention. After 2 days of transarterial embolization, the relationship between pulmonary and systemic arterial pressure is reversed. The pulmonary arterial hypertension is no longer suprasystemic, which suggests that further embolization may be postponed until the 5th or 6th month of age. B: Correlation of systemic blood pressure with the EI during the first 3 weeks of life corresponding to the timeline in panel A. An EI > 1.6 was associated with the need for urgent embolization. Note that the EI does not correlate as well as the TR gradient. Thus, if available, the TR gradient is the primary indicator of the need for intervention, and EI is a secondary indicator. An artist’s depiction of the cardiac echo at end-systole demonstrates a normal left ventricle (C) versus a compromised left ventricle secondary to severe PH (D). Note the flattening of the interventricular septum (D) causing an increased EI. The index is calculated as the ratio of the left ventricle anteroposterior to the septolateral dimension (solid black lines).
To improve the patient’s heart failure and provide a potentially life-saving procedure, the patient was emergently treated with two stages of transarterial embolization (90% n-butyl cyanoacrylate at days 3 and 4 via a transfemoral approach. His umbilical arteries were not available for access. Postoperatively, the patient improved substantially. His echo series demonstrated progressive reversal of his suprasystemic PH following the embolization (Fig. 2). The LV EI was reduced to 1.33 postoperatively; after 1 month, the EI was reduced further to 1.13. The progressive reduction of both the TR gradient and EI correlated well with the neonate’s clinical recovery. He was discharged home 2 months postoperatively. He received two additional stages of embolization at age 6 months and 9 months. Although the malformation has not been cured so far, it is substantially reduced in size; the patient is growing and thriving (Fig. 1).
Discussion
Observations
As illustrated in the case above, it is our experience that neonates with VoGM with a suprasystemic TR gradient (i.e., >60 mm Hg) and/or an increased LV EI > 1.6 experience severe right congestive heart failure (CHF) with need for urgent/emergency embolization. Second, reversal of suprasystemic PH postembolization and/or reduction of the EI suggests that further embolization may be deferred to reduce procedural risk.
PH in Newborns With VoGMs
PH in a newborn is the result of a maladaptation to extrauterine life characterized by an elevation in pulmonary vascular resistance, right-to-left shunting and hypoxemia.2,3 In babies with VoGM, PH is mainly triggered by high output right CHF secondary to the high-flow vein of Galen fistula.1,4–6 The increased right ventricular (RV) flow appears to directly cause increased pulmonary vascular resistance. Brinjikji et al. found that newborn age and presence of CHF (secondary to PH) were significant predictors of poor outcome in their review of 578 patients with VoGM.4 Persistent PH in newborns with a VoGM correlates with patient demise.7–9
Several medical interventions may improve the PH. Holden et al.5 showed some improvement in PAPs in response to oxygen inhalation. Hendson et al. report on improvements with nitric oxide.10 McNamara et al. greatly support the use of milrinone, a phosphodiesterase inhibitor, to improve cardiac contractility in babies with PH.11 Nonetheless, despite medical interventions, embolization of the malformation is the key to successful management of severe PH and right CHF in newborns with VoGM.10 In the following sections, we discuss two cardiac markers that indicate the severity of the PH, dictate the urgency or an intervention, and prove useful for monitoring of the cardiac function after intervention, as illustrated in our case study. The two cardiac markers (indicators) are the TR gradient and the EI.
TR Gradient as a Marker of PH in Newborns
Both the TR gradient and the EI are well-characterized markers of PH in the newborn.3,12 However, neither parameter is currently used routinely to determine the need for or monitor the success of a catheter intervention in babies with VoGM. Pulmonary pressure can be estimated by the amount of blood regurgitation at the tricuspid valve. Using echocardiography, the peak tricuspid regurgitation flow velocity (v) is measured and converted into an estimate of the pulmonary pressure via the modified Bernoulli equation Δ pressure = 4v2. “Δ pressure” is the pressure gradient between the pulmonary artery/right ventricle at systole versus the right atrial pressure. This pressure differential is referred to as the TR gradient.
A normal TR jet has a maximal velocity of <2.5 m/sec.13 The normal estimated systolic PAP (sPAP) is ≤35 mm Hg.14 The sPAP can be estimated from a peak TR velocity by continuous-wave Doppler as the most practical noninvasive method to predict sPAP.12,15
If the PAP exceeds the systemic arterial pressure (suprasystemic PH, i.e., >60 mm Hg), the prognosis is poor, in the general neonatal population and particularly in newborns with VoGMs.2,4,9,10,16,17 As an example from the literature, Tiwary et al.2 reported on a newborn with VoGM who developed PH at day 4 of life. An echocardiogram was obtained, demonstrating marked tricuspid regurgitation with a TR valve jet velocity of 4 m/sec, which would correlate with an approximate TR gradient of 67 mm Hg. The baby developed progressive PH that required emergency catheter intervention at day 9 and again day 44. At age 4 months, he was thriving and his cardiac parameters had stabilized.
Without urgent catheter intervention, newborns symptomatic with PH are unlikely to survive. As the PH escalates and surpasses systemic pressures, newborns typically develop severe systemic metabolic acidosis and multiorgan failure. Thus, we believe suprasystemic PH (i.e., TR gradient >60 mm Hg) is a clear indication for immediate or repeat catheter embolization of newborn patients with VoGM without other contraindications.
EI as a Marker of PH in Newborns
Unfortunately, TR may be absent or difficult to quantify by echocardiography in approximately two-thirds of neonates with PH. In this situation, the TR gradient cannot be determined. Thus, the EI has emerged recently as an alternative to estimate the degree of PH (Fig. 2).3,12,18 With a normal RV pressure, the left ventricle is roughly circular in shape during end-systole. With RV pressure overload, the interventricular septum flattens most significantly during end-systole; the LV resumes an eccentric D shape (Fig. 2). The EI is calculated as the ratio between the LV anteroposterior dimension (the long axis of the “D”) divided by the septolateral dimension (the short axis of the “D”; Fig. 2). An EI > 1.0 is abnormal and has been shown to correlate with worse clinical outcomes in adults and children with PH.19–22 Lopez-Candales et al.20 nicely demonstrated the use of EI during the echocardiographic evaluation of PH in 103 patients. In their review, systolic EI was the only multivariate predictor of PH in 103 patients.20 In our experience, an EI > 1.6 in babies with VoGM requires urgent intervention or repeat intervention.
Lessons
Successful management of VoGM in the newborn requires a highly coordinated team approach involving neonatologists, pediatric cardiologists, pediatric neurologists, neurosurgeons, and interventionalists. In our practice, suprasystemic TR gradients and/or increased EI requires consideration of urgent/emergency catheter intervention in the newborn patient with a VoGM. EI and TR gradient appear to supplement the Bicetre score and prove helpful in clinical decision-making.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: EF Hauck, LI Hauck, Athavale, McCrary, Campbell. Acquisition of data: EF Hauck, Yarden, McCrary, Campbell. Analysis and interpretation of data: EF Hauck, Yarden, McCrary, Campbell. Drafting the article: EF Hauck, Yarden, Athavale, Campbell. Critically revising the article: EF Hauck, Yarden, Athavale, McCrary, Campbell. Reviewed submitted version of manuscript: EF Hauck, Athavale, Campbell. Approved the final version of the manuscript on behalf of all authors: EF Hauck. Statistical analysis: EF Hauck, Yarden. Administrative/technical/material support: EF Hauck. Study supervision: EF Hauck.
References
- 1. Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, Garcia-Monaco R. The management of vein of Galen aneurysmal malformations. Neurosurgery. 2006;59(5) suppl 3:S184–S194. doi: 10.1227/01.NEU.0000237445.39514.16. discussion S3–S13. [DOI] [PubMed] [Google Scholar]
- 2. Tiwary S, Geethanath RM, Abu-Harb M. Vein of Galen malformation presenting as persistent pulmonary hypertension of newborn (PPHN) BMJ Case Rep. 2013;2013:bcr2013200425. doi: 10.1136/bcr-2013-200425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCrary AW, Barker PCA, Torok RD, et al. Agreement of an echocardiogram-based diagnosis of pulmonary hypertension in infants at risk for bronchopulmonary dysplasia among masked reviewers. J Perinatol. 2019;39(2):248–255. doi: 10.1038/s41372-018-0277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brinjikji W, Krings T, Murad MH, Rouchaud A, Meila D. Endovascular treatment of vein of Galen malformations: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2017;38(12):2308–2314. doi: 10.3174/ajnr.A5403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holden AM, Fyler DC, Shillito J, Jr, Nadas AS. Congestive heart failure from intracranial arteriovenous fistula in infancy. Clinical and physiologic considerations in eight patients. Pediatrics. 1972;49(1):30–39. [PubMed] [Google Scholar]
- 6. Cumming GR. Circulation in neonates with intracranial arteriovenous fistula and cardiac failure. Am J Cardiol. 1980;45(5):1019–1024. doi: 10.1016/0002-9149(80)90171-x. [DOI] [PubMed] [Google Scholar]
- 7. Huh J, Noh CI, Choi JY, Yun YS. Pulmonary hypertensive crisis as an initial manifestation of intracranial arteriovenous malformation with aneurysm of the vein of Galen. Int J Cardiol. 1998;66(1):107–109. doi: 10.1016/s0167-5273(98)00183-1. [DOI] [PubMed] [Google Scholar]
- 8. Selzer G, Rettwitz-Volk W, Schloesser R, et al. Persistent pulmonary hypertension in the newborn infant caused by aneurysm of the vein of Galen. Article in German. Klin Padiatr. 1993;205(3):190–193. [PubMed] [Google Scholar]
- 9. Yan J, Wen J, Gopaul R, Zhang CY, Xiao SW. Outcome and complications of endovascular embolization for vein of Galen malformations: a systematic review and meta-analysis. J Neurosurg. 2015;123(4):872–890. doi: 10.3171/2014.12.JNS141249. [DOI] [PubMed] [Google Scholar]
- 10. Hendson L, Emery DJ, Phillipos EZ, Bhargava R, Olley PM, Lemke RP. Persistent pulmonary hypertension of the newborn presenting as the primary manifestation of intracranial arteriovenous malformation of the vein of Galen. Am J Perinatol. 2000;17(8):405–410. doi: 10.1055/s-2000-13456. [DOI] [PubMed] [Google Scholar]
- 11. McNamara PJ, Shivananda SP, Sahni M, Freeman D, Taddio A. Pharmacology of milrinone in neonates with persistent pulmonary hypertension of the newborn and suboptimal response to inhaled nitric oxide. Pediatr Crit Care Med. 2013;14(1):74–84. doi: 10.1097/PCC.0b013e31824ea2cd. [DOI] [PubMed] [Google Scholar]
- 12. Jone PN, Ivy DD. Echocardiography in pediatric pulmonary hypertension. Front Pediatr. 2014;2:124. doi: 10.3389/fped.2014.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bossone E, Rubenfire M, Bach DS, Ricciardi M, Armstrong WF. Range of tricuspid regurgitation velocity at rest and during exercise in normal adult men: implications for the diagnosis of pulmonary hypertension. J Am Coll Cardiol. 1999;33(6):1662–1666. doi: 10.1016/s0735-1097(99)00055-8. [DOI] [PubMed] [Google Scholar]
- 14. McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001;104(23):2797–2802. doi: 10.1161/hc4801.100076. [DOI] [PubMed] [Google Scholar]
- 15. Hatle L, Angelsen BA, Tromsdal A. Non-invasive estimation of pulmonary artery systolic pressure with Doppler ultrasound. Br Heart J. 1981;45(2):157–165. doi: 10.1136/hrt.45.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mandell E, Kinsella JP, Abman SH. Persistent pulmonary hypertension of the newborn. Pediatr Pulmonol. 2021;56(3):661–669. doi: 10.1002/ppul.25073. [DOI] [PubMed] [Google Scholar]
- 17. Berenstein A, Fifi JT, Niimi Y, et al. Vein of Galen malformations in neonates: new management paradigms for improving outcomes. Neurosurgery. 2012;70(5):1207–1214. doi: 10.1227/NEU.0b013e3182417be3. [DOI] [PubMed] [Google Scholar]
- 18. Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol. 1985;5(4):918–927. doi: 10.1016/s0735-1097(85)80433-2. [DOI] [PubMed] [Google Scholar]
- 19. Raymond RJ, Hinderliter AL, Willis PW, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol. 2002;39(7):1214–1219. doi: 10.1016/s0735-1097(02)01744-8. [DOI] [PubMed] [Google Scholar]
- 20. López-Candales A, Rajagopalan N, Kochar M, Gulyasy B, Edelman K. Systolic eccentricity index identifies right ventricular dysfunction in pulmonary hypertension. Int J Cardiol. 2008;129(3):424–426. doi: 10.1016/j.ijcard.2007.06.057. [DOI] [PubMed] [Google Scholar]
- 21. Galiè N, Hinderliter AL, Torbicki A, et al. Effects of the oral endothelin-receptor antagonist bosentan on echocardiographic and Doppler measures in patients with pulmonary arterial hypertension. J Am Coll Cardiol. 2003;41(8):1380–1386. doi: 10.1016/s0735-1097(03)00121-9. [DOI] [PubMed] [Google Scholar]
- 22. Kassem E, Humpl T, Friedberg MK. Prognostic significance of 2-dimensional, M-mode, and Doppler echo indices of right ventricular function in children with pulmonary arterial hypertension. Am Heart J. 2013;165(6):1024–1031. doi: 10.1016/j.ahj.2013.02.027. [DOI] [PubMed] [Google Scholar]


