ABSTRACT
Objective.
To characterize the frequency, causes, and predictors of readmissions of COVID-19 patients after discharge from heath facilities or emergency departments, interventions used to reduce readmissions, and outcomes of COVID-19 patients discharged from such settings.
Methods.
We performed a systematic review for case series and observational studies published between January 2020 and April 2021 in PubMed, Embase, LILACS, and MedRxiv, reporting the frequency, causes, or risk factors for readmission of COVID-19 survivors/patients. We conducted a narrative synthesis and assessed the methodological quality using the JBI critical appraisal checklist.
Results.
We identified 44 studies including data from 10 countries. The overall 30-day median readmission rate was 7.1%. Readmissions varied with the length of follow-up, occurring <10.5%, <14.5%, <21.5%, and <30%, respectively, for 10, 30, 60, and 253 days following discharge. Among those followed up for 30 and 60 days, the median time from discharge to readmission was 3 days and 8–11 days, respectively. The significant risk factor associated with readmission was having shorter length of stay, and the important causes included respiratory or thromboembolic events and chronic illnesses. Emergency department re-presentation was >20% in four studies. Risk factors associated with mortality were male gender, advanced age, and comorbidities.
Conclusions.
Readmission of COVID-19 survivors is frequent, and post-discharge mortality is significant in specific populations. There is an urgent need to further examine underlying reasons for early readmission and to prevent additional readmissions and adverse outcomes in COVID-19 survivors.
Keywords: COVID-19; SARS-CoV-2; systematic review; patient readmission; emergency service, hospital; mortality
RESUMEN
Objetivo.
Caracterizar la frecuencia, las causas y los factores predictores del reingreso de pacientes con COVID–19 tras haber recibido el alta de un centro de salud o un servicio de urgencias, las intervenciones utilizadas para reducir los reingresos y los resultados de los pacientes con COVID-19 dados de alta de dichos entornos.
Métodos.
Se realizó una revisión sistemática de estudios de serie de casos y estudios observacionales publicados entre enero del 2020 y abril del 2021 en PubMed, Embase, LILACS y MedRxiv en los cuales se informó sobre la frecuencia, las causas o los factores de riesgo relativos al reingreso de pacientes y sobrevivientes de COVID-19. Se realizó una síntesis narrativa y se evaluó la calidad metodológica utilizando la lista de verificación de evaluación crítica de JBI.
Resultados.
Se encontraron 44 estudios con datos de 10 países. La tasa media general de reingreso a los 30 días fue de 7,1%. Los reingresos variaron con la duración del seguimiento, y tuvieron lugar en <10,5%, <14,5%, <21,5% y <30%, respectivamente, a los 10, 30, 60 y 253 días después del alta. Entre los que recibieron seguimiento por 30 y 60 días, el tiempo medio entre el alta y la readmisión fue de 3 y de 8 a 11 días, respectivamente. El factor de riesgo significativo asociado al reingreso fue una estancia más corta, y entre las causas importantes se encontraron episodios respiratorios o tromboembólicos y enfermedades crónicas. El reingreso en el servicio de urgencias fue de >20% en cuatro estudios. Los factores de riesgo asociados con la mortalidad fueron sexo masculino, edad avanzada y comorbilidades.
Conclusión.
El reingreso de sobrevivientes de COVID-19 es frecuente, y la mortalidad después del alta es significativa en grupos poblacionales específicos. Existe una necesidad urgente de seguir examinando las razones subyacentes del reingreso temprano, así como de prevenir reingresos adicionales y resultados adversos en los sobrevivientes de COVID–19.
Palabras clave: COVID-19, SARS-CoV-2, revisión sistemática, readmisión del paciente, servicio de urgencia en hospital, mortalidad
RESUMO
Objetivo.
Caracterizar a frequência, as causas e os preditores de reinternação de pacientes com COVID-19 após a alta do estabelecimento de saúde ou do pronto-socorro, intervenções usadas para reduzir reinternações e desfechos de pacientes com COVID-19 que receberam alta de tais instalações.
Métodos.
Revisão sistemática de séries de casos e estudos observacionais publicados entre janeiro de 2020 e abril de 2021, indexados nos bancos de dados PubMed, Embase, LILACS e MedRxiv, que relatassem a frequência, as causas ou os fatores de risco para a reinternação de sobreviventes da COVID-19/pacientes com COVID-19. Realizamos uma síntese narrativa das evidências e avaliamos a qualidade metodológica utilizando a checklist de avaliação crítica do Joanna Briggs Institute (JBI).
Resultados.
Foram identificados 44 estudos, incluindo dados de 10 países. O índice médio geral de reinternação em 30 dias foi de 7,1%. A frequência das reinternações variou com o tempo de acompanhamento, com <10,5%, <14,5%, <21,5% e <30%, respectivamente, ocorrendo nos primeiros 10, 30, 60 e 253 dias após a alta. Dentre aqueles seguidos por 30 e 60 dias, o tempo médio da alta até a reinternação foi de 3 dias e 8 a 11 dias, respectivamente. O único fator de risco significativamente associado à reinternação foi ter um tempo de permanência hospitalar mais curto, e as causas importantes incluíram eventos respiratórios ou tromboembólicos e doenças crônicas. Em quatro estudos, >20% dos pacientes retornaram ao pronto-socorro. Os fatores de risco associados à mortalidade foram sexo masculino, idade avançada e comorbidades.
Conclusões.
A reinternação hospitalar é frequente em sobreviventes da COVID-19 e a mortalidade pós-alta é significativa em populações específicas. Há uma necessidade urgente de examinar melhor as razões que levam à reinternação precoce e de evitar reinternações adicionais e desfechos adversos em sobreviventes da COVID-19.
Palavras-chave: COVID-19, SARS-CoV-2, revisão sistemática, readmissão do paciente, serviço hospitalar de emergência, mortalidade
Hospital readmissions are frequent (1), with 30-day readmission and mortality rates reported as indicators of quality and coordination of care. Studies have also reviewed existing prediction models for readmission based on logistic regression, survival analysis, and machine learning techniques (2). Historically, 30-day and 1-year readmission rates among adults have been 15% to 21% and 20% to 48%, respectively (3, 4). The time interval from discharge to readmission is associated with the cause of readmission and its associated risk factors. Shorter intervals (0–7 days) can be linked to the clinical care and discharge planning during the index admission (5); a medium interval (8–30 days) is likely less related to the index hospitalization but more susceptible to comorbidities, social determinants of health, and geodemographic characteristics (6). Longer intervals (>6 months) could be related to medium- and long-term sequelae, as has been reported in COVID-19 survivors (7).
SARS-CoV-2, the virus that causes COVID-19, has affected more than 500 million people, resulting in more than 6 million deaths worldwide (8). COVID-19 presents with a heterogeneous clinical course, ranging from asymptomatic carrier status to a fatal outcome with multiorgan failure or the presence of persistent post-COVID-19 condition (7). Effective interventions to reduce early hospital readmissions are complex and support patients’ capacity for self-care (9). Although the effectiveness of various interventions for COVID-19 patients is uncertain, a growing body of scientific literature has attempted to describe hospital readmissions, validate hospital discharge/readmission risk prediction tools, and assess interventions to reduce readmissions and mortality for COVID-19 patients (6, 7).
Hospital readmissions have increasingly been used as an indicator of quality of care in a non-pandemic setting (10). Understanding the pathophysiology of COVID-19 and the epidemiology of readmission in patients hospitalized with COVID-19 would allow the health care system to better allocate already limited resources as well as improve clinical outcomes. We reviewed and synthesized the available literature on readmission of COVID-19 patients with the aim to characterize the frequency, follow-up days, causes, predictors, interventions used to reduce early readmissions, and outcomes of inpatient readmission in COVID-19 patients discharged from a health facility and an emergency department (ED).
MATERIALS AND METHODS
Search strategy
We performed a systematic review, and a structured search was conducted in PubMed, Embase, LILACS, and MedRxiv from January 2020 to April 2021 by two authors (SR, LR), with no restriction on type of publication or language. Studies not in English were translated using automatic translation tools. The references of all included studies were searched manually and in Google Scholar to identify other eligible studies. A protocol was developed a priori, and the search strategies are listed in Supplemental Table A1. A PRISMA flow chart was completed to summarize this process (Figure 1). Reassessment took place after publication of a preprint in a peer-reviewed journal.
FIGURE 1. PRISMA flowchart of study inclusions and exclusions.
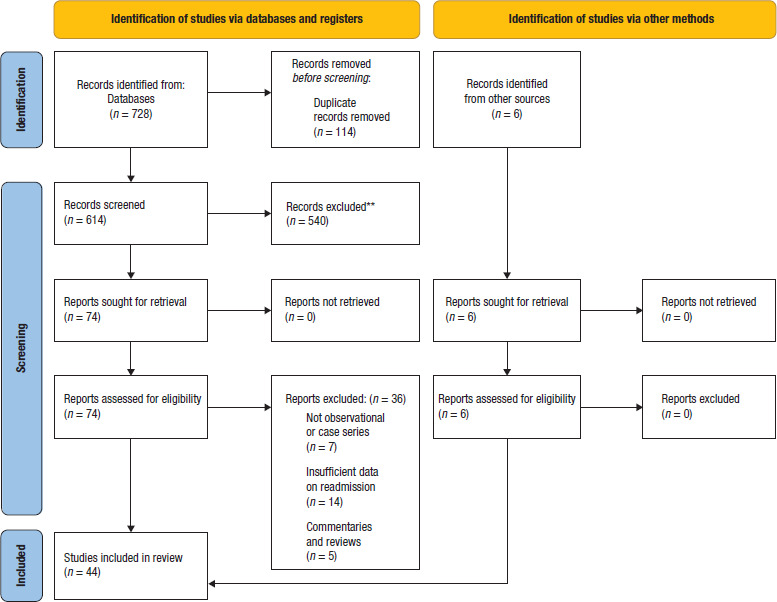
Source: Prepared by the authors from the results of this study, based on published data.
Study selection
For this review, we defined readmission as an unplanned inpatient admission to a health facility, for any cause, within 30, 60, or 90 days from the date of discharge from an index inpatient admission, where the patient was clinically managed for COVID-19. A health facility was defined as a location that provides direct health services by a group of doctors and nurses and includes inpatient and outpatient services. An ED visit was considered an outpatient visit, and a revisit to the ED is referred to as “re-presentation.” Inclusion criteria were (1) studies reporting frequency, causes, or risk factors for readmission of COVID-19 survivors/patients; (2) observational studies and case series with eight or more subjects; and (3) peer-reviewed and non-peer-reviewed studies. Exclusion criteria included (1) case reports and (2) non-original research articles.
The study title and abstract were screened according to the inclusion/exclusion criteria. Full texts of studies that passed the first level screening were critically assessed to determine whether to include them in the review. Disagreements were resolved by discussion, drawing on a third reviewer where required.
Data extraction
Data from the full text were extracted using a predesigned Excel template (Supplemental Table A2) validated by two reviewers (SP, LR). One reviewer (SP) extracted data for all studies, another reviewer (VS) randomly collected data for five (10%) of the studies to compare and confirm the data extracted. Disagreements were resolved by discussion, drawing on a third reviewer where required (LR). Following the a-priori protocol, data were collected for:
Study characteristics: publication year, author, title, country, state/province, number of health facilities, tertiary/academic hospitals, study type, follow-up days, sample size, study sample, and objective.
Readmission: readmission rate, follow-up days, median time from discharge to readmission, hospital mortality, risk factors, reason, type of care, length of hospital stay, ED visits, reason, and risk factors.
Post-discharge interventions, discharge location, post-discharge mortality.
Index hospitalization/discharge: index hospitalization in readmitted patients, index inpatient stay, index ED visit, index length of stay (LOS) in readmitted patients, Charlson comorbidity index, discharge criteria/eligibility, patient symptoms at discharge, and oxygen saturation and requirement at discharge.
Description of strategies to reduce readmission.
Assessment of methodological quality
The methodological quality of the included studies was independently assessed by two reviewers (SP, VS) using the JBI critical appraisal checklist for observational studies and case series (11). Discrepancies were resolved through discussion or the involvement of a third author (LR).
Data synthesis
A narrative synthesis of the evidence was undertaken; the risk factors, interventions, and mortality data were tabulated; and frequency data were presented in graphical form. Readmission incidences were reported in ranges and medians, and the graphs were created using Microsoft® Excel software. Meta-analysis was not appropriate as data synthesis included case series. Ethical approval was not required for this review.
RESULTS
The literature search yielded 734 studies, of which 44 studies met the eligibility criteria. The most common reason for exclusion was the lack of reporting readmission rates and/or risk factors for readmission. The selection strategy of studies is summarized in Figure 1. The list of excluded studies is available upon request.
Critical appraisal of the included studies
We deemed all studies to be eligible to be included in the review (40 “include” and four “seek further info”) (Supplemental Table A3).
Description of studies
The studies’ characteristics are summarized in Supplemental Table A4. Studies varied widely in their size, methodology, and length of follow-up. The review included six prospective studies (12–17) and 38 retrospective studies; 42 of the 44 studies were peer reviewed. Studies were from Australia, Canada, China, Germany, Republic of Korea, the Netherlands, Spain, Turkey, the United Kingdom, and the United States of America, and thus were distributed over four continents. Ten studies had fewer than 100 cases each, 22 studies included 100 to 1 000 cases each, 11 studies reported more than 1 000 COVID-19 patients each, and one study did not report a sample size. The two largest studies were from the United Kingdom and the United States of America, using national data to report 47 780 (7) and 106 543 (18) cases, respectively. Five studies used national data (7, 18–21), of which four detailed long-term outcomes (>30 days), and the fifth was the only study from the Republic of Korea included in our review (20). The mean and median age of patients ranged from 44.5 to 72 years, with a greater proportion of male than female patients in most studies. Studies were published in 2020 and 2021, but the reported index hospitalizations were mostly from the first half of 2020 (n = 36), with only three studies each reporting patients from mid and late 2020, and two studies not reporting the duration. Many were single-center studies (n = 23) and most took place at tertiary level/teaching hospitals (n = 18). All studies included patients diagnosed with COVID-19.
Three groups were analyzed according to the study sample and follow-up days: (1) 30-day readmissions following inpatient discharge of COVID-19 patients (n = 16); (2) >30-day follow-up readmissions following inpatient discharge of COVID-19 patients, including studies that did not report a follow-up duration (n = 23); and (3) inpatient admissions and re-presentations to ED following index presentation to ED for COVID-19 (n = 5).
Readmission of patients within 30 days following index inpatient admission for COVID-19
The readmission rates ranged from 1.9% to 14% in studies that followed patients for 30 days or less, with a median readmission rate of 7.1% (Figure 2). A 10-day follow-up study conducted during the peak of the pandemic in the United Kingdom reported a 10.2% (22) readmission rate. Eight of 11 studies following patients for 30 days reported a 5% or higher readmission rate. The median times from discharge to readmission were reported in eight studies as 3 (22), 4 (23), 5 (24, 25), 6 (26), and 8.1 (17) days.
FIGURE 2. Readmissions within 30 days following index admission for COVID-19.
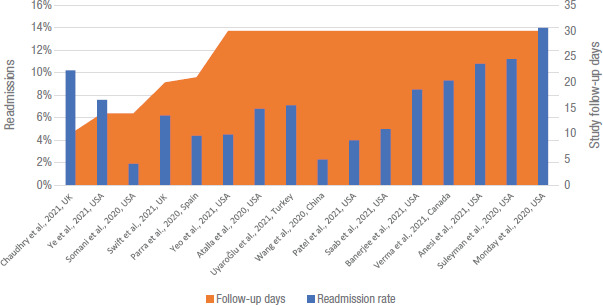
Source: Prepared by the authors from the results of this study, based on published data.
Table 1 presents factors associated with a 30-day or less readmission and reason for readmission in 11 studies. Advanced age, male gender, morbid obesity, and underlying comorbidities were factors for early and late readmissions. Operational factors such as a shorter index LOS, shorter index critical care duration, and early discharge in their illness course were significantly associated with early readmission (22, 26, 27); while Ye et al. reported a decrease in readmissions and ED visits when discharged patients were monitored in a remote care program (23). Patients prescribed a shorter course of steroid (22) and those who did not receive treatment-dose anticoagulation (27) during the index admission were also at an increased risk of readmission.
TABLE 1. Factors and reasons for readmission occurring within 30 days following discharge.
|
Article |
Factors associated with readmissions |
Reason for readmission |
||
|---|---|---|---|---|
|
Clinical |
Operational |
Sociodemographic |
||
|
Chaudhry et al., 2021 (22) |
Shorter courses of steroids (median 2 d vs 5 d, p < 0.001) |
Shorter LOS (median 2 d vs 5 d, p = 0.005), discharged earlier in their illness course (median 8 d vs 13 d, p = 0.005) |
NA |
Oxygen requirement 85%, RF 30% |
|
Ye et al., 2021 (23) |
HTN (67.7% vs 36.8%, p < 0.001), CKD (38.7% vs 12.2%, p < 0.001), CAD (32.3%vs 13.5%, p = 0.01), HF (19.4% vs 8.7%, p = 0.10) |
Remote monitoring had fewer ED visits (OR 0.60, p = 0.12) and readmissions (OR 1.15, p = 0.73) |
Older (66.3 y vs 56.6 y, p = 0.002) |
NA |
|
Somani et al., 2020 (27) |
COPD, HTN, absent index treatment-dose anticoagulation (aP = 0.06). |
Shorter index LOS (aP = 0.006), less index ICU (aP = 0.001). |
NA |
Respiratory distress 50% |
|
Parra et al., 2020 (26) |
Immunocompromised (p = 0.04), HTN (p = 0.07), fever 48 h prior to discharge |
Shorter LOS |
NA |
Pneumonia 55.7%, PTE 13.1%, HF 9.8%, bacterial infection 6.6%, AKF 3.3%, DVT 1.6%, lower arterial thrombosis 1.6% |
|
Saab et al., 2021 (28) |
Absolute lymphocyte count (p = 0.004) |
NA |
NA |
Post-COVID-19 related 100% (5/5) |
|
Atalla et al., 2020 (25) |
HTN (p = 0.038), diabetes (p = 0.021), CLD (e.g., COPD, asthma) (p < 0.001), liver disease (p = 0.001), cancer (p = 0.03) |
NA |
Alcohol (p < 0.001), drug abuse (p = 0.027) |
12 d or <12 d respiratory distress, thrombotic episodes; >12 d psychiatric illness exacerbations and falls |
|
UyaroĞlu et al., 2021 (17) |
Malignancy (p = 0.04), HTN (p = 0.02) |
NA |
NA |
Prolonged fever 45.5%, persistent cough 45.5% |
|
Yeo et al., 2021 (24) |
Obese (20%), HTN (68.6%), diabetes (39.6%), CHF (10.4%), CAD (16.7%), AF (10.4%), CKD (27.1%), COPD/asthma (14.6%), higher index PCT 0.3 ng/mL, troponin 0.04 ng/mL, index peak creatinine ≥1.29 mg/dL (aOR 2.41) |
NA |
Non-Hispanic white (27.8%), discharged to a facility |
Respiratory failure 68.8%, TE 12.5%, sepsis 6.3% |
|
Swift et al., 2021 (12) |
NA |
NA |
NA |
Clotting disorder 100% |
|
Patel et al., 2021 (29) |
NA |
NA |
NA |
New/propagating VTE 22.2% |
|
Wang et al., 2020 (13) |
NA |
NA |
NA |
Fever/positive PCR re-test 2.3% |
Notes: AF, atrial fibrillation; AKF, acute kidney failure; AZT, azithromycin; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; CLD, chronic lung disease; COPD, chronic obstructive pulmonary disease; ED, emergency department; HF, heart failure; HTN, hypertension; ICU, intensive care unit; LOS, length of stay; PCR, polymerase chain reaction; PCT, procalcitonin; PE, pulmonary emboli; PTE, pulmonary thromboembolism; RF, respiratory failure; TE, thromboembolism; VTE, venous thromboembolism.
Source: Prepared by the authors from the results of this study, based on published data.
The common reasons for readmission were respiratory distress/failure and dyspnea or fever (17, 22, 24–28). The diagnoses of thrombosis/emboli were seen in 100% (12), 22.2% (29), 13.1% (26), 12.5% (24), and 10.5% (25) of readmitted cases.
The clinical course during second admission was more severe, with a bigger demand for intensive care compared with the index admission (Supplemental Table A5).
Readmissions in long-term follow-up studies (>30 days) for COVID-19 survivors and studies not reporting a follow-up duration
High readmission rates were seen in studies conducted during the first half of 2020, including 60-day follow-up studies in the United States (19.9%) (21) and the United Kingdom (21.1%) (30). Median times from discharge to readmission of 8 days (18) and 11 days (30) were observed (Figure 3). Studies with a longer follow-up period after discharge, which included a 180-day study in Germany (26.8%) (19) and a 253-day study in the United Kingdom (29.4%) (7), also reported high readmission rates compared with the other studies. Two studies, one from China (31) and the other from Australia (32), had 14% and 16% readmissions, respectively, although there was no study duration reported. Studies that did not report a readmission rate (n = 5) were not included in this analysis.
FIGURE 3. Readmissions in long-term follow-up studies and in studies not reporting the duration of patient follow-up.
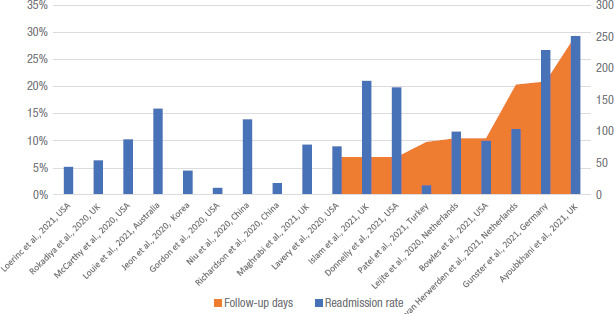
Source: Prepared by the authors from the results of this study, based on published data.
Advanced age, male gender, and underlying comorbidities were factors associated with late readmissions (18, 30, 33, 34). Late readmissions were also dependent on the discharge location and the patients’ mental and functional capacities (18, 33, 34) (Supplemental Table A6). Reasons for readmission were mostly related to COVID-19. A 253-day study in the United Kingdom showed that respiratory causes were the reason for 100% of readmissions (6 085 patients), with 21.5% new-onset respiratory symptoms (7). Diagnoses of thrombosis/emboli were seen in 28.5% (35), 16% (33), 9.1% (36), and 0.3% (37) of readmitted cases. Asymptomatic patients with a positive COVID-19 RT-PCR test were readmitted in three studies presenting data from the early phase of the pandemic in China (38, 39) and Turkey (40).
The need for intensive care, including mechanical ventilation, was reported in COVID-19 survivors who required late readmissions (Supplemental Table A7).
Inpatient admission and emergency department re-presentations following initial discharge from an emergency department
Five studies from Spain (n = 3), the United Kingdom (n = 1), and the United States (n = 1)—four of which were based on data from tertiary care health facilities—detailed the clinical outcomes of COVID-19 patients who were initially seen in an ED and discharged. Three studies were prospective (14–16), and all studies were conducted in different health facilities (Spain: Barcelona [2 of 3] and Madrid [1 of 3]; United Kingdom: London; United States: Pennsylvania and New Jersey) but during the first wave of the pandemic in their respective locations.
The ED re-presentation and inpatient admission frequencies for COVID-19 patients discharged from an index ED visit are presented in Supplemental Table A8. Four of the five studies had 20% or higher ED re-presentation rates. Hernández-Biette et al. reported a 26% rate of re-presentation to ED, with a median time of 3 days, and a 23% rate of inpatient admission (14). The discharge criteria for patients from the ED and telemonitoring of these patients were reported for two of the studies from Spain (Supplemental Table A9). The most common cause of re-presentation to the ED was COVID-19-related (15, 41), and the proportion of patients treated in the ED with corticosteroids was statistically significant (41).
Discharge criteria and post-discharge interventions for all included studies
Twelve studies reported on the criteria applied when discharging patients (Supplemental Table A9), with one study implementing a risk prediction tool to assess high-risk patients at discharge (29). The criteria for discharge were mostly based on the physician’s clinical judgement related to the patient’s clinical improvement. Fever and low oxygen saturation were the most reported symptoms at discharge.
Fifteen studies from the United States, United Kingdom, Spain, China, and the Netherlands detailed the interventions implemented to reduce readmission in COVID-19 survivors (Supplemental Table A10), which were telephone follow-up, virtual/remote app-based monitoring, patient education, home oxygen supplementation, medication interventions, provision of home diagnostics, home visits, scheduled follow-up, and provider continuity. Patel et al. stratified patients according to their risks (29), while others provided post-discharge care according to the patient’s clinical profile at discharge. In four reports, home oxygen supplementation was provided to 621 (100%) (42), 49 (100%) (43), 31 (31.3%) (28), and 75 (24.2%) (37) discharged patients. Patients were also discharged with anticoagulants (26, 37, 43) and corticosteroids (22, 26, 43).
Oxygen requirement
Banerjee et al. reported that discharging 621 patients to an ambulatory setting with low levels of supplementary oxygen was associated with low all-cause mortality and low 30-day return admission rates (42). Van Herwerden et al. reported a median duration of oxygen administration at home of 11 days per patient for 49 patients (43). The potential lying time saving was a total of 616 days. The implementation of the care path “home treatment” resulted in a total cost reduction of €146 736. Dexamethasone for up to 10 days and thromboprophylaxis was continued at home if oxygen was administered (Supplemental Table A11).
Length of hospital stay in index admission and readmission
The median LOS during the index hospitalization ranged from 3.5 days to 17 days (Figure 4) for all studies that reported this statistic. Most of the studies reported a 6-day median LOS during the index hospitalization among the readmitted patients, suggestive of non-severe cases.
FIGURE 4. Median length of hospitalization in index admission, index admission in readmitted patients, and in readmission.
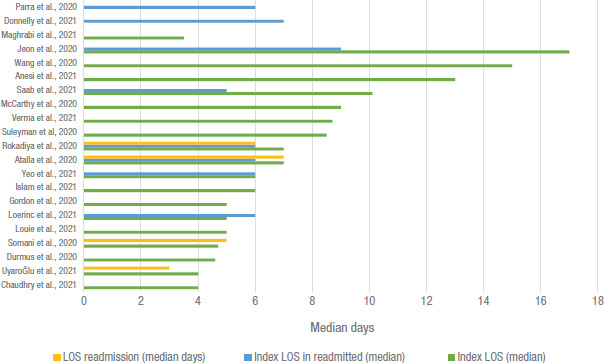
Note: LOS, length of stay.
Source: Prepared by the authors from the results of this study, based on published data.
Mortality
Twenty-four studies reported the percentage of mortality in post-discharged and/or readmitted patients (Table 2). A high post-discharge mortality of 9% was reported in studies analyzing national COVID-19 data: one from the United Kingdom (7) and the other from the United States (21). In a sample of mostly male patients (65%) during the first wave of the pandemic in the United States, Suleyman et al. reported mortalities of 20% in post-discharge patients and 13.7% in readmitted patients (44). Two large studies (n > 1 000 each) reported 14.7% (Spain) (26) and 22.9% (New York, United States) (24) mortality among readmitted patients, wherein the study durations coincided with the initial surge of COVID-19 cases in their respective countries. Increased death rates were seen in studies with a higher percentage of patients who were male or had advanced age, one or more comorbidities (hypertension, obesity, diabetes, cardiovascular disease, chronic lung disease, immunodeficiencies), or national or public health insurance coverage. All these studies were conducted during the first, second, or third wave of the COVID-19 pandemic in their respective countries.
TABLE 2. Mortality in COVID-19 survivors after discharge and after readmission.
|
Article |
Country |
Mortality after discharge |
Characteristics of discharged patients |
Readmission rate |
Mortality after readmission |
Characteristics of readmitted patients |
|---|---|---|---|---|---|---|
|
Louie et al., 2021 (32) |
Australia |
5% |
54 y (mean), 53% male, 79% comorbidity |
16% |
NA |
NA |
|
Leijte et al., 2020 (33) |
Netherlands |
6.4% |
NA |
11.7% |
NA |
NA |
|
van Herwerden et al., 2021 (41) |
Netherlands |
0% |
56 y (mean), 51% male |
12.2% |
NA |
NA |
|
Parra et al., 2020 (26) |
Spain |
NA |
Obesity 9.8%, DM 22.9%, HTN 55.4%, CVD 26.2%, COPD 19.7%, neoplasia 19.7%, immunosuppression 16.4% |
4.4% |
14.7% |
67 y (mean), 73.8% male |
|
Durmus et al., 2020 (40) |
Turkey |
NA |
NA |
NA |
6.6% |
57 y (mean), 43.3% male, 1 or more comorbidities (68.3%) |
|
UyaroĞlu et al., 2021 (17) |
Turkey |
NA |
44.5 y (mean), 50% male |
7.1% |
18.1% |
49 y (mean), 54.5% male |
|
Islam et al., 2021 (30) |
UK |
7.2% |
65 y (median), 52% male, 68% comorbidities |
21.1% |
NA |
NA |
|
Ayoubkhani et al., 2021 (7) |
UK |
9% |
National data, 64.5 y (mean), 55% male |
29.4% |
NA |
NA |
|
Maghrabi et al., 2021 (35) |
UK |
NA |
66.7% male, 71% comorbidity |
9.3% |
7.1% |
NA |
|
Loerinc et al., 2021 (37) |
USA |
0.6% |
58 y (mean), 49% male, HTN 64.5%, BMI ≥ 30 44.5%, DM 36.1%; Insurance: 14.6% private, 36.5% Medicare, 4.2% Medicaid, 6.8% uninsured, 11.9% unknown |
5.2% |
NA |
56% male, HTN 56.3%, CKD 50.0%, BMI ≥ 30 43.8%, DM 43.8%, immunosuppression 18.8% |
|
McCarthy et al., 2020 (36) |
USA |
1.9% |
NA |
10.3% |
NA |
NA |
|
Donnelly et al., 2021 (21) |
USA |
9.1% |
National veterans hospitals data, 71 y (mean) |
19.9% |
NA |
95.5% male, 52.5% Black |
|
Ye et al., 2021 (23) |
USA |
NA |
57.3 y (mean), 60% male, HTN 39.1%, DM 26.2% |
7.6% |
1.7% |
66.3 y (mean), 61% male |
|
Somani et al., 2020 (27) |
USA |
NA |
NA |
1.9% |
5.4% |
66.1 y (mean), 43.9% male |
|
Atalla et al., 2020 (25) |
USA |
NA |
61 y (median), 56.3% male, CHF 9.4%, arrythmias 18.9%, HTN 45.4% |
6.8% |
10.5% |
58 y (median), 63.2% male; commercial insurance 10.5%, Medicaid 31.6%, Medicare 57.9%, self-pay 0%, |
|
Yeo et al., 2021 (24) |
USA |
NA |
56.5 y (mean), 59.50% male |
4.5% |
22.9% |
68.5 y (mean), 52.10% male |
|
Bowles et al., 2021 (34) |
USA |
1% |
67 y (median), 51% male, HTN 69%, diabetes 41%, CLD 16%; Insurance: Medicare 46%, Medicaid 15%, Medicaid + Medicare 12%, other 27.5% |
10% |
2.0% |
NA |
|
Banerjee et al., 2021 (47) |
USA |
1.3% |
51 y (median), 65.1% male; Medicaid 76% |
8.5% |
15.0% |
NA |
|
Anesi et al., 2021 (50) |
USA |
6.8% |
Critical patients 100% |
10.8% |
NA |
NA |
|
Lavery et al., 2020 (18) |
USA |
NA |
National data, 60-day follow-up |
9% |
<0.1% |
51.6% male |
|
Suleyman et al, 2020 (49) |
USA |
20% |
NR |
11.2% |
13.7% |
NA |
|
Spain |
NA |
ED discharged, 54.6 y (mean) |
23% |
4% |
65.5 y (mean), 52% male |
|
|
Spain |
NA |
ED discharged, 57 y (mean), 51% male |
7.1% |
4.5% |
NA |
|
|
Spain |
0% |
ED discharged, 45 y (mean), 47.5% male, 29.9% 1 or more comorbidities |
6.4% |
0% |
46.5 y (mean), 60% male, 40% 1 or more comorbidities |
Notes: All studies occurred during the peak of the pandemic in the respective countries.
Studies reporting COVID-19 patients following index ED discharge.
BMI, body mass index; CHF, congestive heart failure; CKD, chronic kidney disease; CLD, chronic lung disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; DM, diabetes; ED, emergency department; HTN, hypertension; NA, not applicable; NR, not reported.
Source: Prepared by the authors from the results of this study, based on published data.
DISCUSSION
COVID-19 has caused an unprecedented health crisis, resulting in substantial pressure on health care systems to meet the escalating demands. Our study is the most comprehensive review characterizing the frequency, causes, risk factors for readmissions, and outcomes of COVID-19 patients discharged from a health facility or an ED. Our review found that readmission of COVID-19 survivors is frequent, and post-discharge mortality is significant in specific populations.
The overall median 30-day readmission rate of 7.1% was below nationally reported rates for patients 65 years and older in the United Kingdom (15%) (45) and Medicaid patients in the United States (13.7%) (46) but similar to those of privately insured patients in the United States (8.2%). Although the 30-day readmission rates for seasonal influenza (14%) (47, 48), pneumonia (18.3%) (49), and heart failure (23.0%) (50) appear higher than for COVID-19, half of the COVID-19 readmissions occurred within 2 to 8 days after discharge, suggestive of a period of increased risk of clinical deterioration during this time (22–26). A study on 1 853 severe COVID-19 patients aged 18–29 from Texas, United States, reported a 14% (n = 268) return to the hospital following discharge for additional reasons within 30 days (51). Late readmissions were less related to the index hospitalization but were more susceptible to comorbidities, social determinants of health, and geodemographic characteristics (6). High readmission rates in long-term follow-up studies (7, 19) highlight the need for continuous, longer ambulatory monitoring of COVID-19 survivors and an in-depth understanding of COVID-19 sequelae/post-COVID-19 conditions. COVID-19 patients who were readmitted had a lower LOS on index admission (20, 25, 28, 52) compared with the LOS for the total index inpatients; this observation in our review merits further study.
Many studies in which the study durations coincided with the surge of COVID-19 cases in the respective countries, including two large studies (n > 1 000 each), reported high mortality in discharged patients and readmitted patients (17, 24, 30, 44). The risk factors associated with mortality were being male, having advanced age, having one or more comorbidities, and the type of health insurance. COVID-19 survivors had an almost 60% increased risk of death over the six months following their index discharge compared with the general population (53). These later deaths due to long-term complications of SARS-CoV-2 infection are not necessarily recorded as deaths due to COVID-19. The mortality rates we observed in our review suggest that the deaths were due to the immediate viral infection and therefore reported rates are only the tip of the iceberg.
The ED re-presentation rates appear similar in the context of national ED re-presentation average in the United Kingdom (14.0%) (54). Patients presenting to the ED were discharged using observation criteria (16), but studies have indicated that patients with mild symptoms of COVID-19 might worsen days after the onset of symptoms, defying expectations for their prognosis (55). It should also be noted that in the United States the primary portal of entry for hospital admission for uninsured and publicly insured patients that may provide the only readily available care is the ED (56).
Efforts have been made to reduce early readmissions, both at the national and subnational levels. Studies have shown that simple interventions such as a telephone contact, home visits, app-based monitoring, and provision of home diagnostics were effective at reducing readmissions (57–59), but our review did not include randomized controlled trials. The findings of our review are consistent with these studies (23, 32, 60). Risk of venous thromboembolism in patients with COVID-19 has been established previously, in whom venous thromboembolism usually appears progressively during the four weeks after the first hospital presentation (61), which may explain venous thromboembolism as a common cause of readmission; therefore, COVID-19 patients at high risk of venous thromboembolism could benefit from prophylactic heparin (62). To ensure health workers have control of care beyond the immediate post-discharge period, virtual wards have been set up which supported the remote management of respiratory conditions in COVID-19 patients (12).
Implications for health systems and services
Developing and validating clear guidelines and protocols for COVID-19 inpatient and outpatient health facilities should be considered. Establishment of virtual wards, telemonitoring, or app-based monitoring of discharged patients for a short term (critical period of 7 days after discharge) and medium term, provision of home diagnostics and/or home oxygen supplementation for continued respiratory support, with periodic monitoring by the health care team and technicians, could be considered. Further research is needed to evaluate the effectiveness of these interventions alone or in combination. There is a need for local health systems to coordinate and collaborate with external partners for the continued provision of home oxygen therapy. Follow-up clinics are recommended for discharged patients, especially those with continued symptoms and uninsured patients, as well as patients with non-severe symptoms who are referred from primary care services. These clinics should be integrated with a multidisciplinary team with a focus on post-COVID-19 conditions.
Limitations
Our review has some limitations. It should be noted that COVID-19 is a recent disease and the available studies on readmissions are limited; thus, the included studies had heterogenous methodologies, resulting in a risk of bias and low quality of evidence. Most of the studies were retrospective. Most studies were conducted in tertiary level/academic teaching hospitals, which have the capacity to care for severe and critical COVID-19 patients and are therefore likely to have a higher readmission rate. Some studies did not provide the duration of follow-up of the patients following discharge, and there was a lack in detailing the discharge procedure and readmission criteria for these patients. We also had limited data on the cause and risk factors for readmission of these patients.
Conclusion
In this comprehensive systematic review characterizing the readmissions of COVID-19 patients discharged from a health facility or an ED, we found an overall 30-day median readmission rate of 7.1%. Readmissions varied with the length of follow-up. Home oxygen supplementation, telemonitoring, and virtual wards were among the reported strategies to reduce readmissions. The findings from this study are pertinent both to clinical research and health care planning to further examine underlying reasons for readmission of COVID-19 patients.
Data sharing.
The protocol and detailed assessment of each eligible study is available upon request from the corresponding author (LR), and data supporting the findings of this study are available within the article and/or its supplementary material.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH and/or those of the Pan American Health Organization (PAHO).
Acknowledgments.
We would like to thank Dr. Ariel Izcovich for his advice on the presentation of results when drafting the manuscript and Dr. Gisela Alarcón for her comments and suggestions on the results and discussion sections. Editorial support was provided by Bryan Tutt, Scientific Editor, Research Medical Library, MD Anderson Cancer Center.
Footnotes
Author contributions.
LR conceived the study, verified the data, and oversaw the whole process. LR and SP designed the study. SP and LR screened titles. SP and VS extracted data. SP, LR, JN, JT, YLH, and OS analyzed and interpreted the results. SP and VS assessed the studies. SP wrote the first draft, which all authors revised for critical content. All authors had full access to the data in this study and reviewed and approved the final manuscript. LR and SA are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Conflict of interest.
None declared.
REFERENCES
- 1.Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171. doi: 10.1136/bmj.f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]; Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171. [DOI] [PMC free article] [PubMed]
- 2.Artetxe A, Beristain A, Graña M. Predictive models for hospital readmission risk: A systematic review of methods. Comput Methods Programs Biomed. 2018;164:49–64. doi: 10.1016/j.cmpb.2018.06.006. [DOI] [PubMed] [Google Scholar]; Artetxe A, Beristain A, Graña M. Predictive models for hospital readmission risk: A systematic review of methods. Comput Methods Programs Biomed. 2018;164:49-64. [DOI] [PubMed]
- 3.Graham KL, Wilker EH, Howell MD, Davis RB, Marcantonio ER. Differences between early and late readmissions among patients: a cohort study. Ann Intern Med. 2015;162(11):741–749. doi: 10.7326/AITC201506020. [DOI] [PMC free article] [PubMed] [Google Scholar]; Graham KL, Wilker EH, Howell MD, Davis RB, Marcantonio ER. Differences between early and late readmissions among patients: a cohort study. Ann Intern Med. 2015;162(11):741-9. [DOI] [PMC free article] [PubMed]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New Eng J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]; Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New Eng J Med. 2009;360(14):1418-28. [DOI] [PubMed]
- 5.Goldfield N, McCullough E, Hughes J, Tang A, Eastman B, Rawlins L, et al. Identifying Potentially Preventable Readmissions. Health Care Financ Rev. 2008;30:75–91. [PMC free article] [PubMed] [Google Scholar]; Goldfield N, McCullough E, Hughes J, Tang A, Eastman B, Rawlins L, et al. Identifying Potentially Preventable Readmissions. Health Care Financ Rev. 2008;30:75-91. [PMC free article] [PubMed]
- 6.Herrin J, St Andre J, Kenward K, Joshi MS, Audet A-MJ, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20–39. doi: 10.1111/1475-6773.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]; Herrin J, St Andre J, Kenward K, Joshi MS, Audet A-MJ, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20-39. [DOI] [PMC free article] [PubMed]
- 7.Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021;372:n693. doi: 10.1136/bmj.n693. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021;372:n693. [DOI] [PMC free article] [PubMed]
- 8.COVID-19 Dashboard. 2022 Internet. Available from: https://covid19.who.int/ [Google Scholar]; COVID-19 Dashboard [Internet]. 2022 Available from: https://covid19.who.int/.
- 9.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]; Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-107. [DOI] [PMC free article] [PubMed]
- 10.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]; van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391-402. [DOI] [PMC free article] [PubMed]
- 11.JBI . JBI Manual for evidence synthesis. JBI; 2020. Available from: https://wiki.jbi.global/display/MANUAL/7.3.6.3+Assessment+of+methodological+quality. [Google Scholar]; JBI. JBI Manual for evidence synthesis: JBI 2020. Available from: https://wiki.jbi.global/display/MANUAL/7.3.6.3+Assessment+of+methodological+quality.
- 12.Swift J, Harris Z, Woodward A, O’Kelly NI, Barker C, Ghosh S. The implementation of a virtual ward using digital solutions informing community clinicians in early supported discharge of patients with SARS-Cov2 respiratory symptoms from an acute hospital setting. medRxiv. 2021:2021.03.29.21254548. [Google Scholar]; Swift J, Harris Z, Woodward A, O’Kelly NI, Barker C, Ghosh S. The implementation of a virtual ward using digital solutions informing community clinicians in early supported discharge of patients with SARS-Cov2 respiratory symptoms from an acute hospital setting. medRxiv. 2021:2021.03.29.21254548.
- 13.Wang X, Xu H, Jiang H, Wang L, Lu C, Wei X, et al. Clinical features and outcomes of discharged coronavirus disease 2019 patients: a prospective cohort study. QJM. 2020;113(9):657–665. doi: 10.1093/qjmed/hcaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]; Wang X, Xu H, Jiang H, Wang L, Lu C, Wei X, et al. Clinical features and outcomes of discharged coronavirus disease 2019 patients: a prospective cohort study. QJM. 2020;113(9):657-65. [DOI] [PMC free article] [PubMed]
- 14.Hernández-Biette A, Sanz-Santos J, Boix-Palop L, Navarro Rolón A, Martínez-Palau M, de la Sierra Iserte A. Risk factors for later hospitalization of patients discharged from an emergency department with nonsevere COVID-19 symptoms. Emergencias. 2020;32(6):413–415. [PubMed] [Google Scholar]; Hernández-Biette A, Sanz-Santos J, Boix-Palop L, Navarro Rolón A, Martínez-Palau M, de la Sierra Iserte A. Risk factors for later hospitalization of patients discharged from an emergency department with nonsevere COVID-19 symptoms. Emergencias. 2020;32(6):413-5. [PubMed]
- 15.Teigell Muñoz FJ, García-Guijarro E, García-Domingo P, Pérez-Nieto G, Roque Rojas F, García-Peña M, et al. A safe protocol to identify low-risk patients with COVID-19 pneumonia for outpatient management. Intern Emerg Med. 2021:1–9. doi: 10.1007/s11739-021-02660-9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Teigell Muñoz FJ, García-Guijarro E, García-Domingo P, Pérez-Nieto G, Roque Rojas F, García-Peña M, et al. A safe protocol to identify low-risk patients with COVID-19 pneumonia for outpatient management. Intern Emerg Med. 2021:1-9. [DOI] [PMC free article] [PubMed]
- 16.Lanham D, Roe J, Chauhan A, Evans R, Hillman T, Logan S, et al. COVID-19 emergency department discharges: an outcome study. Clin Med (Lond) 2021;21(2):e126–e131. doi: 10.7861/clinmed.2020-0817. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lanham D, Roe J, Chauhan A, Evans R, Hillman T, Logan S, et al. COVID-19 emergency department discharges: an outcome study. Clin Med (Lond). 2021;21(2):e126-e31. [DOI] [PMC free article] [PubMed]
- 17.UyaroĞlu OA, BaŞaran N, ÖziŞik L, Dŀzman GT, EroĞlu ŀ, Şahŀn TK, et al. Thirty-day readmission rate of COVID-19 patients discharged from a tertiary care university hospital in Turkey: an observational, single-center study. Int J Qual Health Care. 2021;33(1) doi: 10.1093/intqhc/mzaa144. [DOI] [PMC free article] [PubMed] [Google Scholar]; UyaroĞlu OA, BaŞaran N, ÖziŞik L, Dŀzman GT, EroĞlu ŀ, Şahŀn TK, et al. Thirty-day readmission rate of COVID-19 patients discharged from a tertiary care university hospital in Turkey: an observational, single-center study. Int J Qual Health Care. 2021;33(1). [DOI] [PMC free article] [PubMed]
- 18.Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, et al. Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695–1699. doi: 10.15585/mmwr.mm6945e2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, et al. Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695-9. [DOI] [PMC free article] [PubMed]
- 19.Günster C, Busse R, Spoden M, Rombey T, Schillinger G, Hoffmann W, et al. 6-Month Follow Up of 8679 Hospitalized COVID-19 Patients in Germany: A Nationwide Cohort Study. doi: 10.1371/journal.pone.0255427. medRxiv. 2021:2021.04.24.21256029. [DOI] [PMC free article] [PubMed] [Google Scholar]; Günster C, Busse R, Spoden M, Rombey T, Schillinger G, Hoffmann W, et al. 6-Month Follow Up of 8679 Hospitalized COVID-19 Patients in Germany: A Nationwide Cohort Study. medRxiv. 2021:2021.04.24.21256029. [DOI] [PMC free article] [PubMed]
- 20.Jeon WH, Seon JY, Park SY, Oh IH. Analysis of Risk Factors on Readmission Cases of COVID-19 in the Republic of Korea: Using Nationwide Health Claims Data. Int J Environ Res Public Health. 2020;17(16) doi: 10.3390/ijerph17165844. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jeon WH, Seon JY, Park SY, Oh IH. Analysis of Risk Factors on Readmission Cases of COVID-19 in the Republic of Korea: Using Nationwide Health Claims Data. Int J Environ Res Public Health. 2020;17(16). [DOI] [PMC free article] [PubMed]
- 21.Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19 in a Large Multihospital System. JAMA. 2021;325(3):304–306. doi: 10.1001/jama.2020.21465. [DOI] [PMC free article] [PubMed] [Google Scholar]; Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19 in a Large Multihospital System. JAMA. 2021;325(3):304-6. [DOI] [PMC free article] [PubMed]
- 22.Chaudhry Z, Shawe-Taylor M, Rampling T, Cutfield T, Bidwell G, Chan XHS, et al. Short durations of corticosteroids for hospitalised COVID-19 patients are associated with a high readmission rate. J Infect. 2021;82(6):276–316. doi: 10.1016/j.jinf.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chaudhry Z, Shawe-Taylor M, Rampling T, Cutfield T, Bidwell G, Chan XHS, et al. Short durations of corticosteroids for hospitalised COVID-19 patients are associated with a high readmission rate. J Infect. 2021;82(6):276-316. [DOI] [PMC free article] [PubMed]
- 23.Ye S, Hiura G, Fleck E, Garcia A, Geleris J, Lee P, et al. Hospital Readmissions After Implementation of a Discharge Care Program for Patients with COVID-19 Illness. J Gen Intern Med. 2021;36(3):722–729. doi: 10.1007/s11606-020-06340-w. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ye S, Hiura G, Fleck E, Garcia A, Geleris J, Lee P, et al. Hospital Readmissions After Implementation of a Discharge Care Program for Patients with COVID-19 Illness. J Gen Intern Med. 2021;36(3):722-9. [DOI] [PMC free article] [PubMed]
- 24.Yeo I, Baek S, Kim J, Elshakh H, Voronina A, Lou MS, et al. Assessment of thirty-day readmission rate, timing, causes and predictors after hospitalization with COVID-19. J Intern Med. 2021;290(1):157–165. doi: 10.1111/joim.13241. [DOI] [PMC free article] [PubMed] [Google Scholar]; Yeo I, Baek S, Kim J, Elshakh H, Voronina A, Lou MS, et al. Assessment of thirty-day readmission rate, timing, causes and predictors after hospitalization with COVID-19. J Intern Med. 2021;290(1):157-165. [DOI] [PMC free article] [PubMed]
- 25.Atalla E, Kalligeros M, Giampaolo G, Mylona EK, Shehadeh F, Mylonakis E. Readmissions among patients with COVID-19. Int J Clin Pract. 2020:e13700. doi: 10.1111/ijcp.13700. [DOI] [PubMed] [Google Scholar]; Atalla E, Kalligeros M, Giampaolo G, Mylona EK, Shehadeh F, Mylonakis E. Readmissions among patients with COVID-19. Int J Clin Pract. 2020:e13700. [DOI] [PubMed]
- 26.Parra LM, Cantero M, Morrás I, Vallejo A, Diego I, Jiménez-Tejero E, et al. Hospital Readmissions of Discharged Patients with COVID-19. Int J Gen Med. 2020;13:1359–1366. doi: 10.2147/IJGM.S275775. [DOI] [PMC free article] [PubMed] [Google Scholar]; Parra LM, Cantero M, Morrás I, Vallejo A, Diego I, Jiménez-Tejero E, et al. Hospital Readmissions of Discharged Patients with COVID-19. Int J Gen Med. 2020;13:1359-66. [DOI] [PMC free article] [PubMed]
- 27.Somani S, Richter F, Fuster V, De Freitas J, Naik N, Sigel K, et al. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization For COVID-19. 2020 doi: 10.1007/s11606-020-06120-6. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]; Somani S, Richter F, Fuster V, De Freitas J, Naik N, Sigel K, et al. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization For COVID-19. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 28.Saab FG, Chiang JN, Brook R, Adamson PC, Fulcher JA, Halperin E, et al. Discharge Clinical Characteristics and Post-Discharge Events in Patients with Severe COVID-19: A Descriptive Case Series. J Gen Intern Med. 2021;36(4):1017–1022. doi: 10.1007/s11606-020-06494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Saab FG, Chiang JN, Brook R, Adamson PC, Fulcher JA, Halperin E, et al. Discharge Clinical Characteristics and Post-Discharge Events in Patients with Severe COVID-19: A Descriptive Case Series. J Gen Intern Med. 2021;36(4):1017-22. [DOI] [PMC free article] [PubMed]
- 29.Patel H, Virapongse A, Baduashvili A, Devitt J, Barr R, Bookman K. Implementing a COVID-19 Discharge Pathway to Improve Patient Safety. Am J Med Qual. 2021;36(2):84–89. doi: 10.1097/01.JMQ.0000735436.50361.79. [DOI] [PMC free article] [PubMed] [Google Scholar]; Patel H, Virapongse A, Baduashvili A, Devitt J, Barr R, Bookman K. Implementing a COVID-19 Discharge Pathway to Improve Patient Safety. Am J Med Qual. 2021;36(2):84-9. [DOI] [PMC free article] [PubMed]
- 30.Islam N, Lewington S, Kharbanda RK, Davies J, Várnai KA, Lacey B. Sixty-day consequences of COVID-19 in patients discharged from hospital: an electronic health records study. Eur J Public Health. 2021;31(2):280–282. doi: 10.1093/eurpub/ckab009. [DOI] [PMC free article] [PubMed] [Google Scholar]; Islam N, Lewington S, Kharbanda RK, Davies J, Várnai KA, Lacey B. Sixty-day consequences of COVID-19 in patients discharged from hospital: an electronic health records study. Eur J Public Health. 2021;31(2):280-282. [DOI] [PMC free article] [PubMed]
- 31.Niu J, Sareli C, Sareli A. 514. Clinical features and outcomes of 112 patients with SARS-CoV-2 infections requiring intensive care in a public healthcare system in South Florida. Open Forum Infect Dis. 2020;7(Supplement_1):S323-S. [Google Scholar]; Niu J, Sareli C, Sareli A. 514. Clinical features and outcomes of 112 patients with SARS-CoV-2 infections requiring intensive care in a public healthcare system in South Florida. Open Forum Infect Dis. 2020;7(Supplement_1):S323-S.
- 32.Louie T, Kwan B, Susanto C, Ng A. Respiratory failure, clinical course and community management of COVID-19 patients in a large Australian cohort. Intern Med J. 2021;51(3):334–340. doi: 10.1111/imj.15206. [DOI] [PMC free article] [PubMed] [Google Scholar]; Louie T, Kwan B, Susanto C, Ng A. Respiratory failure, clinical course and community management of COVID-19 patients in a large Australian cohort. Intern Med J. 2021;51(3):334-40. [DOI] [PMC free article] [PubMed]
- 33.Leijte WT, Wagemaker NMM, van Kraaij TDA, de Kruif MD, Mostard GJM, Leers MPG, et al. Mortality and re-admission after hospitalization with COVID-19. Ned Tijdschr Geneeskd. 2020;164 [PubMed] [Google Scholar]; Leijte WT, Wagemaker NMM, van Kraaij TDA, de Kruif MD, Mostard GJM, Leers MPG, et al. [Mortality and re-admission after hospitalization with COVID-19]. Ned Tijdschr Geneeskd. 2020;164. [PubMed]
- 34.Bowles KH, McDonald M, Barrón Y, Kennedy E, O'Connor M, Mikkelsen M. Surviving COVID-19 After Hospital Discharge: Symptom, Functional, and Adverse Outcomes of Home Health Recipients. Ann Intern Med. 2021;174(3):316–325. doi: 10.7326/M20-5206. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bowles KH, McDonald M, Barrón Y, Kennedy E, O'Connor M, Mikkelsen M. Surviving COVID-19 After Hospital Discharge: Symptom, Functional, and Adverse Outcomes of Home Health Recipients. Ann Intern Med. 2021;174(3):316-25. [DOI] [PMC free article] [PubMed]
- 35.Maghrabi F, Bazaz R, Wilson E, Reilly S, Calisti G, Richardson R, et al. The development and implementation of a virtual discharge ward for patients with covid-19 pneumonia: Data on the first 300 patients. Thorax. 2021;76(SUPPL 1):A35–A6. [Google Scholar]; Maghrabi F, Bazaz R, Wilson E, Reilly S, Calisti G, Richardson R, et al. The development and implementation of a virtual discharge ward for patients with covid-19 pneumonia: Data on the first 300 patients. Thorax. 2021;76(SUPPL 1):A35-A6.
- 36.McCarthy CP, Murphy S, Jones-O'Connor M, Olshan DS, Khambhati JR, Rehman S, et al. Early clinical and sociodemographic experience with patients hospitalized with COVID-19 at a large American healthcare system. EClinicalMedicine. 2020;26:100504. doi: 10.1016/j.eclinm.2020.100504. [DOI] [PMC free article] [PubMed] [Google Scholar]; McCarthy CP, Murphy S, Jones-O'Connor M, Olshan DS, Khambhati JR, Rehman S, et al. Early clinical and sociodemographic experience with patients hospitalized with COVID-19 at a large American healthcare system. EClinicalMedicine. 2020;26:100504. [DOI] [PMC free article] [PubMed]
- 37.Loerinc LB, Scheel AM, Evans ST, Shabto JM, O'Keefe GA, O'Keefe JB. Discharge characteristics and care transitions of hospitalized patients with COVID-19. Healthc (Amst) 2021;9(1):100512. doi: 10.1016/j.hjdsi.2020.100512. [DOI] [PMC free article] [PubMed] [Google Scholar]; Loerinc LB, Scheel AM, Evans ST, Shabto JM, O'Keefe GA, O'Keefe JB. Discharge characteristics and care transitions of hospitalized patients with COVID-19. Healthc (Amst). 2021;9(1):100512. [DOI] [PMC free article] [PubMed]
- 38.Li C, Luo F, Xie L, Gao Y, Zhang N, Wu B. Chest CT study of fifteen COVID-19 patients with positive RT-PCR retest results after discharge. Quantitative Imaging in Medicine and Surgery. 2020 June;Vol 10(No 6):1318–1324. doi: 10.21037/qims-20-530. Quant Imaging Med Surg. 2020;10(6) [DOI] [PMC free article] [PubMed] [Google Scholar]; Li C, Luo F, Xie L, Gao Y, Zhang N, Wu B. Chest CT study of fifteen COVID-19 patients with positive RT-PCR retest results after discharge. Quantitative Imaging in Medicine and Surgery; Vol 10, No 6 (June 2020): Quant Imaging Med Surg. 2020;10(6):1318-1324. [DOI] [PMC free article] [PubMed]
- 39.Cao H, Ruan L, Liu J, Liao W. The clinical characteristic of eight patients of COVID-19 with positive RT-PCR test after discharge. J Med Virol. 2020;92(10):2159–2164. doi: 10.1002/jmv.26017. [DOI] [PMC free article] [PubMed] [Google Scholar]; Cao H, Ruan L, Liu J, Liao W. The clinical characteristic of eight patients of COVID-19 with positive RT-PCR test after discharge. J Med Virol. 2020;92(10):2159-64. [DOI] [PMC free article] [PubMed]
- 40.Durmus E, Guneysu F. Evaluation of re-hospitalized COVID-19 patients in a hospital. Rev Assoc Med Bras (1992) 2020;66(12):1690–1695. doi: 10.1590/1806-9282.66.12.1690. [DOI] [PubMed] [Google Scholar]; Durmus E, Guneysu F. Evaluation of re-hospitalized COVID-19 patients in a hospital. Rev Assoc Med Bras (1992). 2020;66(12):1690-5. [DOI] [PubMed]
- 41.López-Barbeito B, García-Martínez A, Coll-Vinent B, Placer A, Font C, Vargas CR, et al. Factors associated with revisits by patients with SARS-CoV-2 infection discharged from a hospital emergency department. Emergencias. 2020;32(6):386–394. [PubMed] [Google Scholar]; López-Barbeito B, García-Martínez A, Coll-Vinent B, Placer A, Font C, Vargas CR, et al. Factors associated with revisits by patients with SARS-CoV-2 infection discharged from a hospital emergency department. Emergencias. 2020;32(6):386-94. [PubMed]
- 42.Banerjee J, Canamar CP, Voyageur C, Tangpraphaphorn S, Lemus A, Coffey C, Jr., et al. Mortality and Readmission Rates Among Patients With COVID-19 After Discharge From Acute Care Setting With Supplemental Oxygen. JAMA Netw Open. 2021;4(4):e213990. doi: 10.1001/jamanetworkopen.2021.3990. [DOI] [PMC free article] [PubMed] [Google Scholar]; Banerjee J, Canamar CP, Voyageur C, Tangpraphaphorn S, Lemus A, Coffey C, Jr., et al. Mortality and Readmission Rates Among Patients With COVID-19 After Discharge From Acute Care Setting With Supplemental Oxygen. JAMA Netw Open. 2021;4(4):e213990. [DOI] [PMC free article] [PubMed]
- 43.van Herwerden MC, van Steenkiste J, El Moussaoui R, den Hollander JG, Helfrich G, I JAMV Home telemonitoring and oxygen therapy in COVID-19 patients: safety, patient satisfaction, and cost-effectiveness. Ned Tijdschr Geneeskd. 2021;165 [PubMed] [Google Scholar]; van Herwerden MC, van Steenkiste J, El Moussaoui R, den Hollander JG, Helfrich G, I JAMV. [Home telemonitoring and oxygen therapy in COVID-19 patients: safety, patient satisfaction, and cost-effectiveness]. Ned Tijdschr Geneeskd. 2021;165. [PubMed]
- 44.Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open. 2020;3(6):e2012270. doi: 10.1001/jamanetworkopen.2020.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]; Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open. 2020;3(6):e2012270. [DOI] [PMC free article] [PubMed]
- 45.Oliver D. David Oliver: Who is to blame for older people’s readmission? BMJ. 2015;351:h4244. doi: 10.1136/bmj.h4244. [DOI] [PubMed] [Google Scholar]; Oliver D. David Oliver: Who is to blame for older people’s readmission? BMJ. 2015;351:h4244. [DOI] [PubMed]
- 46.Bailey MK WA, Barrett ML, Jiang HJ. Agency for Healthcare Research and Quality. Rockville: 2019. Characteristics of 30-Day Readmissions, 2010-2016. [PubMed] [Google Scholar]; Bailey MK WA, Barrett ML, Jiang HJ. Characteristics of 30-Day Readmissions, 2010-2016. Agency for Healthcare Research and Quality: Rockville; 2019. [PubMed]
- 47.Dobrzynski DM, Ndi DN, Zhu Y, Markus T, Schaffner W, Talbot HK. Hospital Readmissions After Laboratory-Confirmed Influenza Hospitalization. J Infect Dis. 2020;222(4):583–589. doi: 10.1093/infdis/jiaa117. [DOI] [PubMed] [Google Scholar]; Dobrzynski DM, Ndi DN, Zhu Y, Markus T, Schaffner W, Talbot HK. Hospital Readmissions After Laboratory-Confirmed Influenza Hospitalization. J Infect Dis. 2020;222(4):583-9. [DOI] [PubMed]
- 48. [cited 06/17/2021];Unplanned Hospital Visits - National Data. 2021 Internet. Available from: https://data.cms.gov/provider-data/topics/hospitals/unplanned-hospital-visits/ [Google Scholar]; Unplanned Hospital Visits - National Data. [Internet]. 2021 [cited 06/17/2021]. Available from: https://data.cms.gov/provider-data/topics/hospitals/unplanned-hospital-visits/.
- 49.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-63. [DOI] [PMC free article] [PubMed]
- 50.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart Disease and Stroke Statistics—2013 Update. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]; Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart Disease and Stroke Statistics—2013 Update. Circulation. 2013;127(1):e6-e245. [DOI] [PMC free article] [PubMed]
- 51.Sandoval M, Nguyen DT, Vahidy FS, Graviss EA. Risk factors for severity of COVID-19 in hospital patients age 18–29 years. PLOS One. 2021;16(7):e0255544. doi: 10.1371/journal.pone.0255544. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sandoval M, Nguyen DT, Vahidy FS, Graviss EA. Risk factors for severity of COVID-19 in hospital patients age 18–29 years. PLOS One. 2021;16(7):e0255544. [DOI] [PMC free article] [PubMed]
- 52.Rokadiya S, Gil E, Stubbs C, Bell D, Herbert R. COVID-19: Outcomes of patients with confirmed COVID-19 re-admitted to hospital. J Infect. 2020;81(3):e18–e19. doi: 10.1016/j.jinf.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]; Rokadiya S, Gil E, Stubbs C, Bell D, Herbert R. COVID-19: Outcomes of patients with confirmed COVID-19 re-admitted to hospital. J Infect. 2020;81(3):e18-e9. [DOI] [PMC free article] [PubMed]
- 53.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594(7862):259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]; Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594(7862):259-64. [DOI] [PubMed]
- 54.Public Health England Public Health Profiles. 2021 Available from: https://fingertips.phe.org.uk. [Google Scholar]; Public Health England. Public Health Profiles. 2021. Available from: https://fingertips.phe.org.uk.
- 55.Kilaru AS, Lee K, Snider CK, Meisel ZF, Asch DA, Mitra N, et al. Return Hospital Admissions Among 1419 COVID-19 Patients Discharged from Five U.S. Emergency Departments. Acad Emerg Med. 2020;27(10):1039–1042. doi: 10.1111/acem.14117. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kilaru AS, Lee K, Snider CK, Meisel ZF, Asch DA, Mitra N, et al. Return Hospital Admissions Among 1419 COVID-19 Patients Discharged from Five U.S. Emergency Departments. Acad Emerg Med. 2020;27(10):1039-42. [DOI] [PMC free article] [PubMed]
- 56.Weiss AJ, (Truven Health Analytics) WLTHA. Stocks C, AHRQ. Blanchard J, RAND Overview of Emergency Department Visits in the United States, 2011. HCUP Statistical Brief #174. 2014 [PubMed] [Google Scholar]; Weiss AJ (Truven Health Analytics) WLTHA, Stocks C (AHRQ), Blanchard J (RAND). Overview of Emergency Department Visits in the United States, 2011. HCUP Statistical Brief #174, 2014. [PubMed]
- 57.Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. Aust Health Rev. 2010;34(4):445–451. doi: 10.1071/AH09777. [DOI] [PubMed] [Google Scholar]; Scott IA. Preventing the rebound: improving care transition in hospital discharge processes. Aust Health Rev. 2010;34(4):445-51. [DOI] [PubMed]
- 58.Vernon D, Brown JE, Griffiths E, Nevill AM, Pinkney M. Reducing readmission rates through a discharge follow-up service. Future Healthc J. 2019;6(2):114–117. doi: 10.7861/futurehosp.6-2-114. [DOI] [PMC free article] [PubMed] [Google Scholar]; Vernon D, Brown JE, Griffiths E, Nevill AM, Pinkney M. Reducing readmission rates through a discharge follow-up service. Future Healthc J. 2019;6(2):114-7. [DOI] [PMC free article] [PubMed]
- 59.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Dis Mon. 2002;48(4):239–248. doi: 10.1016/s0011-5029(02)90031-3. [DOI] [PubMed] [Google Scholar]; Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Dis Mon. 2002;48(4):239-48. [DOI] [PubMed]
- 60.Gordon WJ, Henderson D, DeSharone A, Fisher HN, Judge J, Levine DM, et al. Remote Patient Monitoring Program for Hospital Discharged COVID-19 Patients. Appl Clin Inform. 2020;11(5):792–801. doi: 10.1055/s-0040-1721039. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gordon WJ, Henderson D, DeSharone A, Fisher HN, Judge J, Levine DM, et al. Remote Patient Monitoring Program for Hospital Discharged COVID-19 Patients. Appl Clin Inform. 2020;11(5):792-801. [DOI] [PMC free article] [PubMed]
- 61.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]; Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. [DOI] [PMC free article] [PubMed]
- 62.Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, Parra-Virto A, Toledano-Macías M, Toledo-Samaniego N, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23–26. doi: 10.1016/j.thromres.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]; Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, Parra-Virto A, Toledano-Macías M, Toledo-Samaniego N, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23-6. [DOI] [PMC free article] [PubMed]


