Purpose of review
Gambiense human African trypanosomiasis (gHAT), a disease that has killed hundreds of thousands as recently as the 1990s, could be on the verge of elimination or even eradication. This review describes recent developments that give us reasons for optimism as well as some caveats.
Recent findings
New developments in diagnostic and vector control tools, and especially in treatment, make it possible to strive for elimination of transmission of gHAT by 2030, perhaps even eradication.
Summary
Gambiense human African trypanosomiasis is a deadly infectious disease affecting West and Central Africa, South Sudan and Uganda, and transmitted between humans by tsetse flies. The disease has caused several major epidemics, the latest one in the 1990s. Thanks to recent innovations such as rapid diagnostic tests for population screening, a single-dose oral treatment and a highly efficient vector control strategy, interruption of transmission of the causative parasite is now within reach. If indeed gHAT has an exclusively human reservoir, this could even result in eradication of the disease. Even if there were an animal reservoir, on the basis of epidemiological data, it plays a limited role. Maintaining adequate postelimination surveillance in known historic foci, using the newly developed tools, should be sufficient to prevent any future resurgence.
Keywords: African trypanosomiasis, elimination of transmission, epidemiology, treatment, vector control
INTRODUCTION
Human African trypanosomiasis (HAT) is a parasitic disease affecting rural areas of sub-Saharan Africa. There are two forms of the disease, the West-African form caused by the protozoan Trypanosoma brucei gambiense (Gambiense human African trypanosomiasis) and the East-African form caused by T. brucei rhodesiense (rhodesiense HAT or rHAT), both being transmitted by tsetse flies (Glossina) [1–3]. Whereas rHAT, is in principle, a zoonosis in which humans are accidental hosts, gHAT is an anthroponosis with transmission occurring in a human–fly–human cycle, exclusively in sub-Saharan Africa. Of the two forms, gHAT is by far the most common, accounting for over 95% of all cases reported since 2010 and is the focus of this review [4]. The fact that gHAT is an anthroponosis, dependent on a vector, makes it theoretically feasible to strive for elimination. WHO has set a target of interruption of transmission of T. brucei gambiense by 2030 [5].
Box 1.
no caption available
THE HISTORY OF GAMBIENSE HUMAN AFRICAN TRYPANOSOMIASIS IN SUB-SAHARAN AFRICA
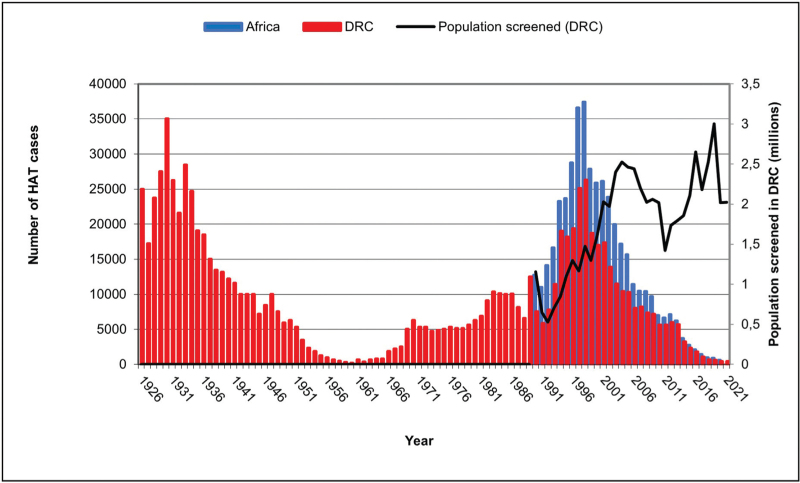
Since the 19th century, gHAT is known to have caused several devastating epidemics. It is estimated that at the turn of the 20th century, 300 000–500 000 people died of gHAT, with another epidemic occurring in the 1920s–1930s [6]. By 1960, intensive efforts had brought the disease under control in most endemic countries but when measures were neglected, it reemerged. The most recent flare-up in the 1990s in all probability again killed hundreds of thousands [7]. Figure 1 shows case notification numbers in the Democratic Republic of the Congo (DRC) since 1926 based on data from the national HAT control program (PNLTHA) and overall figures for gHAT case notification across Sub-Saharan Africa since 1990 as reported to WHO. Also shown are the numbers screened each year in DRC since 1990.
FIGURE 1.
Gambiense human African trypanosomiasis case notification in the Democratic Republic of Congo (DRC) (1926–2021) and all of sub-Saharan Africa (1990–2020), as well as population screened in DRC (1990–2021).
Continent-wide trends are clearly driven by the DRC caseload. At the height of the most recent outbreak, in 1998, DRC reported 26 318 cases but only 12% of the population at risk was covered by active screening [8]. Given the weak health systems in the areas affected, WHO estimates that the true incidence may have been up to 10 times higher [9].
CLINICAL ASPECTS
The clinical course of HAT is classically divided into two stages, the hemolymphatic stage (first or early stage), corresponding to the dissemination of the trypanosomes in the blood and reticuloendothelial system, followed by the meningoencephalitic stage (second or late stage), when the causative parasite has crossed the blood–brain barrier. Second stage can only be diagnosed by lumbar puncture and examination of cerebrospinal fluid (CSF) [10]. The two forms of HAT have very different clinical presentations. rHAT mainly presents as an acute systemic febrile illness sometimes complicated by multiple organ failure and is mostly diagnosed during the first stage [10]. In contrast, gHAT more often presents as a chronic neurological disease. Neurological manifestations include disturbances of sleep pattern (daytime sleeping and/or insomnia), motor weakness, sensorimotor deficit, and behavior change [11]. In the absence of appropriate treatment, all HAT infections are assumed to eventually be fatal [1].
DIAGNOSIS AND TREATMENT
Although the treatment of first-stage gHAT has for a long time relied on fairly well tolerated 7-day intramuscular administration of pentamidine, therapy for second-stage gHAT was until recently limited to a very toxic drug, melarsoprol, an arsenical derivative combined with an antidote to world war I era battle gases [12,13]. An estimated 3–6% of patients treated with melarsoprol died from an encephalopathic syndrome, during or shortly after treatment, and many patients developed other toxicities [14]. To avoid overtreatment, complex diagnostic procedures were introduced. These include screening of HAT suspects with an antibody-detecting serological test, followed by the cumbersome search for parasites in those found seropositive, by microscopic examination of blood or lymph node aspirate. Whenever parasites are found in blood or lymph, CSF must be examined to determine the disease stage. (Supplementary Materials: Video 1, Trypanosomes in blood, Video 2, Trypanosomes in CSF).
Since 2010, eflornithine was introduced as an alternative drug, and it was effective and much less toxic [15]. However, its complex mode of administration, requiring intravenous infusions every 6 h for 2 weeks, was problematic in HAT-endemic areas. Two new treatments have since emerged that made a real difference for first-line health practitioners. First the nifurtimox–eflornithine combination therapy (NECT) reduced the need for intravenous infusions to twice daily for 1 week [16–19]. More recently, fexinidazole, an all-oral 10-day treatment, has been positively evaluated in clinical trials [20▪,21]. Fexinidazole is active against both stages of the disease, thus obviating the need for lumbar puncture and is now the first choice treatment for gHAT [22]. Only for cases with clinical symptoms suggestive of severe meningoencephalitic stage (>100 white blood cells/μl in CSF), is NECT still recommended.
STRATEGIES FOR CONTROL OF GAMBIENSE HUMAN AFRICAN TRYPANOSOMIASIS
The backbone of gHAT control has always been active case-finding, followed by treatment [23]. This is likely to remain the case for the foreseeable future. In the strategy defined by WHO, villages from which gHAT cases have been reported are to be screened annually until no further cases are found for 3 years in a row [24]. They are to be screened once more 5 years after the last case was reported and if no new cases are found, surveillance is shifted to passive mode. Finding a new case means the village returns to the list of villages to be screened annually.
Passive case-finding relies on symptomatic patients presenting at fixed health facilities for diagnosis and treatment of HAT. Simarro et al.[25] in 2014 identified 632 fixed health facilities that had been providing such services across all endemic countries from 2000 till 2012. At the time of writing, 41, 71 and 83%, respectively of the population at-risk for gHAT were assumed to be living within 1, 3 and 5 h travel of a facility that can provide diagnosis. Unfortunately, such facilities in gHAT-endemic areas are typically poorly equipped and poorly attended [26,27]. As was explained earlier, current diagnostic procedures are complex. They require visualization of T. brucei gambiense through microscopy, preferably making use of concentration methods that enhance sensitivity [28]. Apart from the fact that such methods require electricity and equipment, such as a centrifuge and a microscope, they also require skills that are hard to maintain whenever lab technicians only rarely come across actual gHAT cases.
Vector control for gHAT has historically been considered too expensive and logistically challenging [29]. The breakthrough came when researchers discovered the effectiveness of using small (∼0.13m2) targets for gHAT vectors [30]. This discovery led to the development of Tiny Targets [31,32]. Tiny Targets are small, 25 cm × 50 cm, used in Central Africa and the Nile catchment of East Africa where Glossina fuscipes are the predominant vectors, or 75 cm × 50 cm, used in West Africa where Glossina palpalis predominate, insecticide-treated visual baits constituting a blue panel, which attracts the flies. The blue panel is flanked by a black mesh, which is invisible to tsetse; tsetse collide with the mesh and take up a lethal dose of insecticide. This novel technology was found to be more cost-effective than previous control operations for gHAT vectors, and it is now widely used in Uganda, Chad, Côte d’Ivoire, Guinea, and DRC [33–35]. (supplementary material picture 1,Tiny Target DRC, picture 2, Tiny Target Uganda). Entomological surveys demonstrate that Tiny Targets can achieve reductions to more than 80% in tsetse densities [36–39]. Analyses have shown that Tiny Target operations can significantly reduce the incidence of gHAT, thus demonstrating the value of adding vector control to screening and treatment efforts [37,38,40▪].
ENABLING FACTORS AND INNOVATIONS
Currently there are several factors that make it possible to consider interruption of gHAT transmission, despite all the obstacles mentioned. Even at times of high prevalence, gHAT has always been known for its very focal distribution. Approximately 300 gHAT foci have been described, distributed across 24 countries in sub-Saharan Africa [41]. This opens up perspectives for permanent disease elimination as interrupting transmission from these foci and keeping them under postelimination surveillance is at least theoretically feasible. In 2012, WHO formulated a strategy for elimination of gHAT as a public health problem, defined as the detection of less than 1 new case per 10 000 population in at least 90% of these endemic foci and fewer than 2000 cases reported annually by 2020 [41]. These targets have by and large been achieved [42]. The new target set for 2030 is interruption of transmission of T. brucei gambiense[5].
We are now at an all-time low with less than 1000 cases reported across the African continent in 2019, before the start of the COVID-19 pandemic. Importantly, the current low is a different low from that of 1960. As shown in Fig. 1, screening coverage for HAT in DRC has consistently been very high for the past 20 years; even during the pandemic years, approximately two million people were screened each year. Despite such intensive screening, numbers of cases detected have continued to drop. Moreover, recent innovations in diagnostics and treatment now make it possible to consider alternative strategies that could lead to interruption of transmission.
In the field of diagnostics, there have been some important innovations. Since the mid-1990s, the card agglutination test for trypanosomiasis (CATT), an antibody detection test requiring a cold chain and a battery operated rotator, has been used extensively as serological screening tool [43]. More recently, two rapid diagnostic tests (RDTs) based on native antigen (HAT Sero-K-SeT and SD Bioline HAT) have been developed and validated [44,45]. These RDTs are thermostable and do not require any equipment or source of electricity. A phase 2 study on stored plasma samples comparing two RDTs showed a sensitivity of 99.6% for SD Bioline HAT and 99.1% for HAT Sero-K-Set [46]. A case–control study that prospectively enrolled 134 gHAT cases showed a sensitivity of 98.5% for HAT Sero-K-SeT [44]. However, in two recent phase 3 studies, sensitivity estimates were much lower: 69.1% for CATT versus 92.0% for SD Bioline HAT and 62.5% for CATT versus 59.0% for SD Bioline HAT [45,47]. RDTs based on recombinant antigens have now also been developed, a prototype of one has already been evaluated under field conditions [47]. Importantly, these are all screening tests. Out of 1 621 170 people actively screened in DRC in 2021, 9794 (0.6%) tested positive to either RDT or CATT, among them 303 were confirmed gHAT cases (Data PNLTHA of DRC). Thus, despite excellent specificity, their positive-predictive value in population screening was only in the order of 3%.
Until recently in DRC, there were so many villages to be screened that the available screening capacity was largely surpassed. With only 421 cases reported in 2021 (active and passive case detection combined), this is no longer the case. At this stage, quality rather than quantity becomes of crucial importance. Diagnostic confirmation tests are not only highly specific but also complex, and errors do occur [48] Quality-assured diagnosis remains of crucial importance [49]. With the drugs currently available, overtreatment is less of an issue, but it is important not to waste scarce resources on screening villages that are nonendemic.
A shift from active to passive screening may seem a logical next step once no more cases are found. Yet, because of the constraints described earlier, this will not be sufficient to achieve permanent elimination of gHAT. Some form of active screening will always be required to reach and sustain interruption of transmission. In a postelimination phase, such active surveillance can focus on historic foci, villages that have been endemic in the past. They will need to be screened actively once every 5–10 years to ensure that there is no resurgence. There may also be blind spots, villages that are suspected to be endemic but from which no data is available. Such villages should be screened at least once to rule out gHAT endemicity.
In all probability, the greatest breakthrough in recent years is a nontoxic single-dose oral drug acoziborole that has recently passed phase 3 clinical evaluation [50,51▪]. Publication of the final results is eagerly awaited (ClinicalTrials.gov Identifier: NCT03087955), because this novel treatment would make it possible to consider entirely different approaches to achieve interruption of transmission. As acoziborole can be used to treat HAT irrespective of disease stage, stage determination would become redundant.
The combination of highly specific screening tests (>99% specificity in DRC in 2021) and a single-dose oral treatment, now makes it possible to consider a screen-and-treat approach, skipping the on-the-spot diagnostic confirmation step. A phase 3A study exploring safety of acoziborole in serological suspects is currently ongoing (ClinicalTrials.gov Identifier: NCT05256017). If one were to screen HAT endemic villages with an RDT and presumptively treat all those testing positive, there would probably be a major reduction in numbers of dropouts during the diagnostic procedures [23]. The fact that treatment is provided on the spot and that the dreaded lumbar puncture is no longer required would almost certainly result in increased participation in screening [52]. Such a screen-and-treat strategy could also be applied in passive screening.
With fewer than 10 000 serological suspects identified in DRC last year, treating all presumptively is far from impossible. There would still be a need for post hoc diagnostic confirmation to decide whether a village should be kept under active surveillance and eventually to confirm whether or not T. brucei gambiense is still circulating. For a posteriori diagnostic confirmation too, there have been some promising innovations. A highly specific inhibition ELISA, as well as a molecular test, are currently being validated for use in regional hospitals [53,54▪].
The combination of a screen-and-treat strategy with well targeted vector control using Tiny Targets is already showing great promise [33]. There is no need to permanently eliminate tsetse flies, reducing their density by more than 70%, as achieved in various settings, is sufficient to interrupt transmission [35–39]. Rather than aiming to control tsetse everywhere, efforts can be targeted to foci with active transmission. Combining tsetse control with the treatment of all potential sources of infection, including humans testing positive to serological tests would accelerate the interruption of transmission and ultimately eradicate the disease.
There is plenty of reason for optimism, but some word of caution is also required. Even though gHAT is assumed to be anthroponotic, there have been reports of pigs and other livestock being infected with T. brucei gambiense, and potentially playing a role in transmission [55]. At this stage, the existence of cryptic reservoirs in animals cannot be excluded with certainty. If they do exist, Tiny Targets could offer a solution to this threat. There have also been reports of humans carrying parasites in the skin but not in the blood and remaining asymptomatic [56]. So far, such asymptomatic carriers were identified among serological gHAT suspects, and thus would only strengthen the case for presumptive treatment based on serology. But we need to know more about this group, in particular whether the serological tests used in gHAT screening are sufficiently sensitive to pick them up or not, and whether current drugs are able to reach those parasites residing in the skin or not.
In a screen-and-treat strategy, sensitivity of serological tests becomes of crucial importance, and results from most studies seem to be reassuring [44,46]. However, there were also two phase 3 studies showing poor sensitivity of CATT and three RDTs [45,47]. Unfortunately, further research into sensitivity of screening tests is hampered by low numbers of new gHAT cases being identified and by the fact that existing specimen banks have very much been preselected on CATT.
CONCLUSION
Over the past 20 years, the combination of improved control tools and their implementation in screening of gHAT-endemic villages, followed by treating all diagnosed patients, has greatly reduced gHAT transmission. The targets of elimination of gHAT as a public health problem by 2020 have been achieved. Thanks to further innovations in diagnostics, vector control, and treatment in particular, the new target of interruption of transmission by 2030 is well within reach. Even if there was an animal or a cryptic human reservoir, based on the current epidemiological developments, it does not appear to play a major role. If transmission from the known human reservoir can be interrupted and historic foci kept under surveillance, a full-scale resurgence of gHAT as we have repeatedly witnessed in the past becomes highly unlikely. This will require sustained commitment from all stakeholders as well as adaptation of gHAT control strategies, making optimal use of available innovations.
Acknowledgements
We greatly acknowledge the support of Dr Erick Mwamba Miaka (director PNLTHA, DRC), Professor Philippe Büscher (ITM), Professor Steve Torr (LSTM), and Dr Paul Verlé (ITM).
Disclosure of funding: The DRC data was obtained with financial support of the Bill & Melinda Gates Foundation and the Government of Belgium.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Supplementary Material
Footnotes
Supplemental digital content is available for this article.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Buscher P, Cecchi G, Jamonneau V, Priotto G. Human African trypanosomiasis. Lancet 2017; 390:2397–2409. [DOI] [PubMed] [Google Scholar]
- 2.Checchi F, Funk S, Chandramohan D, et al. Updated estimate of the duration of the meningo-encephalitic stage in gambiense human African trypanosomiasis. BMC Res Notes 2015; 8:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malvy D, Chappuis F. Sleeping sickness. Clin Microbiol Infect 2011; 17:986–995. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Human African trypanosomiasis (sleeping sickness) 2022. Available at: https://www.who.int/health-topics/human-african-trypanosomiasis#tab=tab_1. [Accessed 16 July 2022]. [Google Scholar]
- 5.WHO. Ending the neglect to attain the sustainable development goals. A road map for neglected tropical diseases 2021-2030. Geneva: WHO; 2020. [Google Scholar]
- 6.Barrett MP. The rise and fall of sleeping sickness. Lancet 2006; 367:1377–1378. [DOI] [PubMed] [Google Scholar]
- 7.Pepin J, Meda HA. The epidemiology and control of human African trypanosomiasis. Adv Parasitol 2001; 49:71–132. [DOI] [PubMed] [Google Scholar]
- 8.Van Nieuwenhove S, Betu-Ku-Mesu VK, Diabakana PM, et al. Sleeping sickness resurgence in the DRC: the past decade. Trop Med Int Health 2001; 6:335–341. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Factsheet: trypanosomiasis, human African (sleeping sickness) Geneva, 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness). [Accessed 16 July 2022]. [Google Scholar]
- 10.Bottieau E, Clerinx J. Human African trypanosomiasis: progress and stagnation. Infect Dis Clin North Am 2019; 33:61–77. [DOI] [PubMed] [Google Scholar]
- 11.Blum J, Schmid C, Burri C. Clinical aspects of 2541 patients with second stage human African trypanosomiasis. Acta Trop 2006; 97:55–64. [DOI] [PubMed] [Google Scholar]
- 12.Jennings FW, Atouguia JM, Murray M. The importance of 2,3-dimercaptopropinol (British antilewisite, BAL) in the trypanocidal activity of topical melarsoprol. Acta Trop 1996; 62:83–89. [DOI] [PubMed] [Google Scholar]
- 13.Pepin J, Milord F. The treatment of human African trypanosomiasis. Adv Parasitol 1994; 33:1–47. [DOI] [PubMed] [Google Scholar]
- 14.Chappuis F. Melarsoprol-free drug combinations for second-stage Gambian sleeping sickness: the way to go. Clin Infect Dis 2007; 45:1443–1445. [DOI] [PubMed] [Google Scholar]
- 15.Chappuis F, Udayraj N, Stietenroth K, et al. Eflornithine is safer than melarsoprol for the treatment of second-stage Trypanosoma brucei gambiense human African trypanosomiasis. Clin Infect Dis 2005; 41:748–751. [DOI] [PubMed] [Google Scholar]
- 16.Lindner AK, Lejon V, Chappuis F, et al. New WHO guidelines for treatment of gambiense human African trypanosomiasis including fexinidazole: substantial changes for clinical practice. Lancet Infect Dis 2020; 20:e38–e46. [DOI] [PubMed] [Google Scholar]
- 17.Neau P, Hanel H, Lameyre V, et al. Innovative partnerships for the elimination of human African trypanosomiasis and the development of fexinidazole. Trop Med Infect Dis 2020; 5:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Priotto G, Kasparian S, Mutombo W, et al. Nifurtimox-eflornithine combination therapy for second-stage African Trypanosoma brucei gambiense trypanosomiasis: a multicentre, randomised, phase III, noninferiority trial. Lancet 2009; 374:56–64. [DOI] [PubMed] [Google Scholar]
- 19.Alirol E, Schrumpf D, Amici Heradi J, et al. Nifurtimox-eflornithine combination therapy for second-stage gambiense human African trypanosomiasis: Medecins Sans Frontieres experience in the Democratic Republic of the Congo. Clin Infect Dis 2013; 56:195–203. [DOI] [PubMed] [Google Scholar]
- 20▪.Kande Betu Ku Mesu V, Mutombo Kalonji W, Bardonneau C, et al. Oral fexinidazole for stage 1 or early stage 2 African Trypanosoma brucei gambiense trypanosomiasis: a prospective, multicentre, open-label, cohort study. Lancet Glob Health 2021; 9:e999–e1008. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article describes a pivotal trial on the effectiveness of oral fexinidazole for stage 1 and early stage 2 gHAT. It confirms effectiveness of fexinidazole across disease stages, making lumbar puncture no longer necessary, except in cases of severe stage 2 disease.
- 21.Mesu V, Kalonji WM, Bardonneau C, et al. Oral fexinidazole for late-stage African Trypanosoma brucei gambiense trypanosomiasis: a pivotal multicentre, randomised, noninferiority trial. Lancet 2018; 391:144–154. [DOI] [PubMed] [Google Scholar]
- 22.WHO. WHO interim guidelines for the treatment of gambiense human African trypanosomiasis 2019. Available at: https://apps.who.int/iris/bitstream/handle/10665/326178/9789241550567-eng.pdf. [Accessed 16 July 2022]. [Google Scholar]
- 23.Robays J, Bilengue MM, Van der Stuyft P, Boelaert M. The effectiveness of active population screening and treatment for sleeping sickness control in the Democratic Republic of Congo. Trop Med Int Health 2004; 9:542–550. [DOI] [PubMed] [Google Scholar]
- 24.WHO. Control and surveillance of human African trypanosomiasis: WHO TRS N°984. Available at: https://www.who.int/publications/i/item/WHO-TRS-984. [Accessed 16 July 2022]. [Google Scholar]
- 25.Simarro PP, Cecchi G, Franco JR, et al. Mapping the capacities of fixed health facilities to cover people at risk of gambiense human African trypanosomiasis. Int J Health Geogr 2014; 13:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitashi P, Hasker E, Mbo F, et al. Integration of diagnosis and treatment of sleeping sickness in primary healthcare facilities in the Democratic Republic of the Congo. Trop Med Int Health 2015; 20:98–105. [DOI] [PubMed] [Google Scholar]
- 27.Wembonyama S, Mpaka S, Tshilolo L. Medicine and health in the Democratic Republic of Congo: from Independence to the Third Republic. Med Trop (Mars) 2007; 67:447–457. [PubMed] [Google Scholar]
- 28.Buscher P, Mumba Ngoyi D, Kabore J, et al. Improved Models of Mini Anion Exchange Centrifugation Technique (mAECT) and Modified Single Centrifugation (MSC) for sleeping sickness diagnosis and staging. PLoS Negl Trop Dis 2009; 3:e471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shaw AP, Torr SJ, Waiswa C, et al. Estimating the costs of tsetse control options: an example for Uganda. Prev Vet Med 2013; 110:290–303. [DOI] [PubMed] [Google Scholar]
- 30.Lindh JM, Torr SJ, Vale GA, Lehane MJ. Improving the cost-effectiveness of artificial visual baits for controlling the tsetse fly Glossina fuscipes fuscipes. PLoS Negl Trop Dis 2009; 3:e474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Esterhuizen J, Rayaisse JB, Tirados I, et al. Improving the cost-effectiveness of visual devices for the control of riverine tsetse flies, the major vectors of human African trypanosomiasis. PLoS Negl Trop Dis 2011; 5:e1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rayaisse JB, Esterhuizen J, Tirados I, et al. Towards an optimal design of target for tsetse control: comparisons of novel targets for the control of Palpalis group tsetse in West Africa. PLoS Negl Trop Dis 2011; 5:e1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ndung’u JM, Boulange A, Picado A, et al. Trypa-NO! contributes to the elimination of gambiense human African trypanosomiasis by combining tsetse control with “screen, diagnose and treat” using innovative tools and strategies. PLoS Negl Trop Dis 2020; 14:e0008738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shaw AP, Tirados I, Mangwiro CT, et al. Costs of using “tiny targets” to control Glossina fuscipes fuscipes, a vector of gambiense sleeping sickness in Arua District of Uganda. PLoS Negl Trop Dis 2015; 9:e0003624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tirados I, Hope A, Selby R, et al. Impact of tiny targets on Glossina fuscipes quanzensis, the primary vector of human African trypanosomiasis in the Democratic Republic of the Congo. PLoS Negl Trop Dis 2020; 14:e0008270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berte D, De Meeus T, Kaba D, et al. Population genetics of Glossina palpalis palpalis in sleeping sickness foci of Cote d’Ivoire before and after vector control. Infect Genet Evol 2019; 75:103963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Courtin F, Camara M, Rayaisse JB, et al. Reducing human-tsetse contact significantly enhances the efficacy of sleeping sickness active screening campaigns: a promising result in the context of elimination. PLoS Negl Trop Dis 2015; 9:e0003727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahamat MH, Peka M, Rayaisse JB, et al. Adding tsetse control to medical activities contributes to decreasing transmission of sleeping sickness in the Mandoul focus (Chad). PLoS Negl Trop Dis 2017; 11:e0005792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tirados I, Esterhuizen J, Kovacic V, et al. Tsetse control and Gambian sleeping sickness; implications for control strategy. PLoS Negl Trop Dis 2015; 9:e0003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪.Bessell PR, Esterhuizen J, Lehane MJ, et al. Estimating the impact of Tiny Targets in reducing the incidence of Gambian sleeping sickness in the North-west Uganda focus. Parasit Vectors 2021; 14:410. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study described in this article demonstrates an impact of Tiny Targets not only just on tsetse abundance but also on gHAT incidence.
- 41.WHO. Report of a WHO meeting on elimination of African trypanosomiasis (Trypanosoma brucei gambiense). 2013. Available at: http://apps.who.int/iris/bitstream/10665/79689/1/WHO_HTM_NTD_IDM_2013.4_eng.pdf. [Accessed 16 July 2022]. [Google Scholar]
- 42.Franco JR, Cecchi G, Paone M, et al. The elimination of human African trypanosomiasis: achievements in relation to WHO road map targets for 2020. PLoS Negl Trop Dis 2022; 16:e0010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Magnus E, Vervoort T, Van Meirvenne N. A card-agglutination test with stained trypanosomes (C.A.T.T.) for the serological diagnosis of T. B. gambiense trypanosomiasis. Ann Soc Belg Med Trop 1978; 58:169–176. [PubMed] [Google Scholar]
- 44.Buscher P, Mertens P, Leclipteux T, et al. Sensitivity and specificity of HAT Sero-K-SeT, a rapid diagnostic test for serodiagnosis of sleeping sickness caused by Trypanosoma brucei gambiense: a case-control study. Lancet Glob Health 2014; 2:e359–e363. [DOI] [PubMed] [Google Scholar]
- 45.Lumbala C, Bessell PR, Lutumba P, et al. Performance of the SD BIOLINE(R) HAT rapid test in various diagnostic algorithms for gambiense human African trypanosomiasis in the Democratic Republic of the Congo. PLoS One 2017; 12:e0180555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jamonneau V, Camara O, Ilboudo H, et al. Accuracy of individual rapid tests for serodiagnosis of gambiense sleeping sickness in West Africa. PLoS Negl Trop Dis 2015; 9:e0003480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lumbala C, Bieler S, Kayembe S, et al. Prospective evaluation of a rapid diagnostic test for Trypanosoma brucei gambiense infection developed using recombinant antigens. PLoS Negl Trop Dis 2018; 12:e0006386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Nieuwenhove S. Challenges in diagnosing Human African trypanosomiasis: evaluation of MSD OCG's HAT project in Dingila, DRC. 2015. Available at: https://evaluation.msf.org/evaluation-report/challenges-in-diagnosing-human-african-trypanosomiasis-evaluation-of-msf-ocgs-hat. [Accessed 16 July 2022]. [Google Scholar]
- 49.Hasker E, Kwete J, Inocencio da Luz R, et al. Innovative digital technologies for quality assurance of diagnosis of human African trypanosomiasis. PLoS Negl Trop Dis 2018; 12:e0006664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dickie EA, Giordani F, Gould MK, et al. New drugs for human African trypanosomiasis: a twenty first century success story. Trop Med Infect Dis 2020; 5:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51▪.Lutje V, Probyn K, Seixas J, et al. Chemotherapy for second-stage human African trypanosomiasis: drugs in use. Cochrane Database Syst Rev 2021; 12:CD015374. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article presents a Cochrane review, largely based on ref. [21] by Mesu et al. (Lancet, 2018), comparing effectiveness of NECT and fexinidazole in stage 2 gHAT patients. It concludes that though slightly less effective than NECT, in particular, in late-stage disease, oral drugs such as fexinidazole and possibly also acoziborole (still in the pipeline) are true game changers, given the challenging circumstances in which most gHAT patients are treated.
- 52.Mpanya A, Hendrickx D, Vuna M, et al. Should I get screened for sleeping sickness? A qualitative study in Kasai province, Democratic Republic of Congo. PLoS Negl Trop Dis 2012; 6:e1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Geerts M, Van Reet N, Leyten S, et al. Trypanosoma brucei gambiense-iELISA: a promising new test for the postelimination monitoring of human African trypanosomiasis. Clin Infect Dis 2020; 73:e2477–e2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54▪.Ngay Lukusa I, Van Reet N, Mumba Ngoyi D, et al. Trypanosome SL-RNA detection in blood and cerebrospinal fluid to demonstrate active gambiense human African trypanosomiasis infection. PLoS Negl Trop Dis 2021; 15:e0009739. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article confirms the high sensitivity of trypanosome SL-RNA detection in blood and is the first to demonstrate its diagnostic performance in CSF. Molecular tests will be of key importance in a possible future test-and-treat strategy.
- 55.Buscher P, Bart JM, Boelaert M, et al. Do cryptic reservoirs threaten Gambiense-sleeping sickness elimination? Trends Parasitol 2018; 34:197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Capewell P, Cren-Travaille C, Marchesi F, et al. The skin is a significant but overlooked anatomical reservoir for vector-borne African trypanosomes. Elife 2016; 5:e17716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.