ABSTRACT
Objective
Sexual minority men (e.g., gay, bisexual, and other men who have sex with men) experience stigma and sexual minority stress, which are theorized to drive negative health outcomes. Sexual minority men with treated HIV display persistent immune dysregulation, which could be amplified by sexual minority stress responses to potentiate cellular aging.
Methods
This cross-sectional study included 52 sexual minority men living with HIV who had undetectable viral load (<40 copies/mL) and biologically confirmed recent methamphetamine use. Participants completed measures assessing sexual minority stress and openness about sexual minority status (i.e., outness). DNA methylation–derived outcomes included the following: the extrinsic epigenetic age acceleration clock, telomere length, naive CD4+ T-helper cells, and naive CD8+ T-cytotoxic/suppressor cells.
Results
After adjusting for negative affect and recent stimulant use, higher sexual minority stress was associated with a faster extrinsic epigenetic age acceleration clock (β = 0.29, p = .030), shorter telomere length (β = −0.43, p = .002), and fewer naive CD4+ (β = −0.57, p < .001) and naive CD8+ T cells (β = −0.57, p < .001). Greater outness was associated with higher naive CD4+ (β = 0.32, p = .030) and naive CD8+ T cells (β = 0.38, p = .008) as well as lower plasma interleukin 6 (β = −0.33, p = .027).
Conclusions
Sexual minority stress processes are associated with markers of cellular aging and inflammation in methamphetamine-using sexual minority men living with HIV. Longitudinal research should elucidate biobehavioral mechanisms linking sexual minority stress processes with accelerated cellular aging in those with and without HIV.
Key words/Abbreviations: aging, epigenetic clock, HIV, methamphetamine, sexual minority stress, ANS = autonomic nervous system, ART = antiretroviral therapy, ASI = Addiction Severity Index, CTRA = conserved transcriptional response to adversity, EEAA = extrinsic epigenetic age acceleration, HIV = human immunodeficiency virus, HPA axis = hypothalamic-pituitary-adrenal axis, IL-6 = interleukin-6, mRNA = messenger RNA, sCD14 = soluble CD14, sCD163 = soluble CD163, TNF-α = tumor necrosis factor - alpha
INTRODUCTION
People with human immunodeficiency virus (HIV) receiving effective antiretroviral therapy (ART) experience accelerated biological aging (1), which is likely due to interacting pathophysiologic alterations driven in part by translocation of microbial products from the intestinal lumen into the systemic circulation (2–4). The resulting persistent immune activation and inflammation could partially account for evidence that people with HIV display accelerated cellular aging equivalent to 5.2 years, which is particularly associated with exhaustion of CD8+ cytotoxic/suppressor T cells (5). Ultimately, cellular and biological alterations may account for the disproportionate burden of HIV-associated non-AIDS comorbidities including greater risk for cardiovascular disease (6–12), diabetes (13–15), osteoporosis (16), frailty (17), renal disease (18,19), and neurocognitive disorders (20,21).
People with HIV are also more likely to have a faster epigenetic clock (5,22,23). Epigenetic clocks are biological age estimators with validated composite measures reflecting epigenetic alterations in genome-wide DNA methylation patterns (23). Derived from DNA methylation arrays, the extrinsic epigenetic age acceleration (EEAA) clock indexes alterations in methylation of select DNA cytosine-phosphate-guanosine dinucleotides (23,24). Interestingly, the faster EEAA clock persists among people with treated HIV for up to 24 months (22). This is consistent with findings that people with HIV receiving ART display shorter leukocyte telomere length, another validated measure of cellular aging (24,25).
Commonly used among persons with HIV (26), stimulants such as methamphetamine have been consistently linked to faster clinical HIV progression, even after adjusting for viral load and ART adherence (27,28). The deleterious consequences of stimulant use for HIV pathogenesis are supported partially by mechanistic studies documenting its direct and indirect effects on immune function (29,30). Several recent cross-sectional studies in those with treated HIV highlight that stimulant use could potentiate immune activation, inflammation, HIV persistence, and immunosenescence (31–35). Methamphetamine-induced alterations in these pathophysiologic processes could accelerate cellular aging. This is partially supported by one recent cross-sectional study where methamphetamine dependence and HIV were independently associated with shorter leukocyte telomere length (36).
Before the modern ART era (i.e., before 2007), cohort studies identified trauma and depression as risk factors for clinical HIV progression (37–40). These effects are theorized to be mediated in part by concomitant dysregulation of the autonomic nervous system (ANS) and hypothalamic-pituitary-adrenal (HPA) axis (41,42). Greater ANS activation at rest predicted poorer CD4+ T-helper cell recovery and higher HIV viral load in the year after highly active ART initiation (43). Interestingly, elevations in urinary levels of norepinephrine predict decrements in CD4+ T-cell count and increases in viral load for 4 years among highly active ART-treated people with HIV (44). An important gap is that few similar studies have been conducted in the modern ART era (i.e., 2007 to present) where life expectancy of individuals living with HIV in high-income countries is approaching that of the general population (45). Further research is especially warranted in high-priority populations that experience profound HIV-related health disparities, including racial and ethnic minorities, sexual minority men, and people who use stimulants (46,47).
The minority stress model (48,49) proposes that sexual minority populations experience unique forms of social stigma such as prejudice, anticipating prejudice, internalized stigma about being a sexual minority (i.e., internalized heterosexism), and concealment of sexual identity that have consequences for mental and physical health. These sexual minority stress processes are over and above stressors experienced by the general population, which is why sexual minority stress is theorized as a primary driver of health disparities. Thus, sexual minority stress could not only directly influence physical health but also indirectly via psychological (e.g., negative affect) and behavioral (e.g., stimulant use) pathways (Figure 1). Prior research observed that elevated sexual minority stress was associated with perturbations in leukocyte messenger RNA (mRNA) gene expression patterns relevant to inflammation and immune dysregulation in methamphetamine-using sexual minority men with treated HIV (50). This is consistent with other cross-sectional studies indicating that experiences of social adversity such as discrimination and homophobic victimization alter the conserved transcriptional response to adversity (CTRA) mRNA gene expression profile (51,52). The CTRA is often characterized by upregulated expression of genes involved in inflammation as well as downregulated expression of genes involved with type I interferon and antibody synthesis (53). An important gap is that few studies have examined the associations of sexual minority stress processes with alterations in DNA methylation patterns that could be mechanistically linked with mRNA gene expression and yield validated estimates of cellular aging such as the EEAA clock.
FIGURE 1.
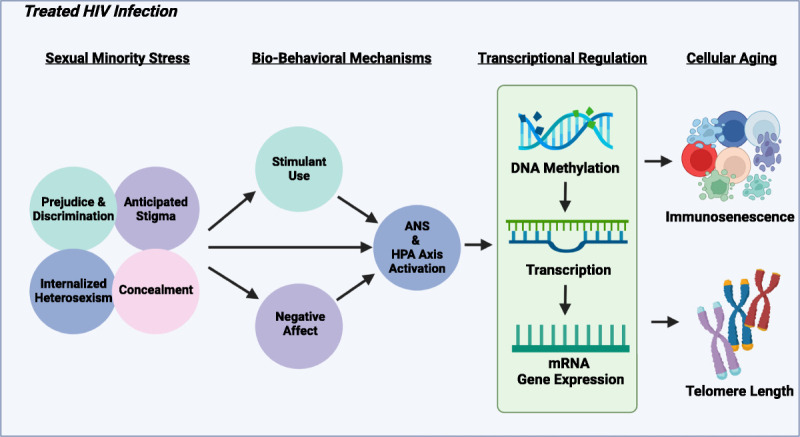
Conceptual model of the biobehavioral mechanism linking sexual minority stress processes with cellular aging in the context of treated HIV infection. ANS = autonomic nervous system; HIV = human immunodeficiency virus; HPA = hypothalamic-pituitary-adrenal; mRNA = messenger RNA.
This cross-sectional study leveraged measures of leukocyte DNA methylation and soluble plasma markers of immune dysregulation (i.e., immune activation and inflammation) from 52 sexual minority men with treated HIV who use methamphetamine. As shown in Figure 1, the conceptual model illustrates the hypothesized pathways whereby sexual minority stress processes (i.e., anticipated stigma, prejudice and discrimination, internalized heterosexism, and concealment) may influence cellular senescence in the context of treated HIV infection. Prior research states that the experience of minority stress could potentiate activation of the ANS and HPA axis via increased negative affect and more frequent stimulant use (54–56). Alterations in the ANS and HPA axis could, in turn, influence transcriptional regulation in leukocytes such as alterations in DNA methylation patterns and downstream profiles of mRNA gene expression such as that observed in mechanisms related to the CTRA. Alterations in DNA methylation and mRNA gene expression could further alter processes relevant to cellular aging, including greater immunosenescence and shorter leukocyte telomere length. Drawing upon the proposed conceptual model, we hypothesized that sexual minority stress processes would be directly associated with DNA methylation–derived measures of cellular aging such as a faster EEAA clock, fewer naive CD4+ and CD8+ T cells, and shorter leukocyte telomere length. Similarly, we proposed that sexual minority stress processes would be directly associated with soluble measures of immune activation and inflammation. Because the correlates of outness (i.e., degree of openness about sexual minority status) have been previously shown to vary by race and ethnicity (57), we also explored whether the beneficial associations of outness with these outcomes were more pronounced among non-Hispanic White sexual minority men when compared with sexual minority men of color.
METHODS
Participants were 52 sexual minority men living with HIV who had undetectable viral load and biologically confirmed recent methamphetamine use based on urine or hair toxicology screening. Participants were recruited as part of a randomized controlled trial conducted from 2013 to 2017 in the San Francisco Bay Area. Additional details regarding the methods and outcomes of the randomized controlled trial are reported elsewhere (58,59). The institutional review board of the University of California at San Francisco approved all procedures, and reliance agreements were made with the University of Miami and Northwestern University. The present cross-sectional study focused on the baseline visit, which included self-report measures, a urine sample for onsite toxicology testing, and a peripheral venous blood sample to measure immune and HIV disease markers. From those who provided consent to bank biospecimens for future studies, we selected baseline leukocyte DNA samples for 52 participants who had an undetectable HIV viral load (i.e., <40 copies/mL) for measurement of genome-wide DNA methylation patterns and markers of immune activation.
Measures
Demographics and Health Status
Participants reported their age, race, ethnicity, education level, income, and time since HIV diagnosis in a demographic questionnaire. HIV viral load testing was performed to detect plasma HIV RNA using the Abbott Real Time HIV-1 assay (Abbott Molecular, Inc., Des Plaines, Illinois). The lower limit of detection was 40 copies/mL. CD4+ and CD8+ T-cell counts were measured with whole blood using flow cytometry by Quest Diagnostics.
Recent Stimulant Use
Urine samples were collected for onsite toxicology screenings for methamphetamine and cocaine using the iCup (Redwood Biotech, Inc., Santa Rosa, California). The iCup can detect any stimulant use (i.e., methamphetamine or cocaine) within the past 72 hours (coded as 1) versus no stimulant use (coded as 0).
Severity of Substance Use
The Addiction Severity Index (ASI) was administered to assess the severity of substance use (60). The ASI Drug Score includes the self-reported number of days using multiple illicit substances during the past 30 days, perceived impairment related to substance use, and perceived need for substance use disorder treatment.
Negative Affect
The modified Differential Emotions Scale was administered to assess positive and negative affect (61,62). Participants rated how frequently they felt a particular emotion in the past week from 0 (never) to 4 (most of the time). The eight negative affect items demonstrated adequate internal consistency in our sample (Cronbach α = .88).
Sexual Minority Stress
The degree to which participants experienced sexual minority stress in theory-based domains—that is, concealment, isolation, internalized stigma, and social rejection—was measured using the five-item sexual minority stress subscale of the Cultural Assessment of Risk for Suicide scale (63). Sample items include, “The decision to hide or reveal my sexual orientation to others causes me significant distress,” and “I was rejected by a family member or friend after telling him/her my sexual orientation.” Likert-type response options ranged from 1 (strongly disagree) to 6 (strongly agree). Higher scores represent more sexual minority stress (Cronbach α = .70).
Internalized Heterosexism
The revised Internalized Homophobia Scale (64), a measure that was previously validated among sexual minority people, was used to assess internalized stigma (Cronbach α = .85). Sample items include, “I wish I weren’t gay/bisexual” and “I have tried to stop being attracted to men in general.” Participants rated five items from 1 (disagree strongly) to 5 (agree strongly) such that higher composite scores were indicative of greater internalized heterosexism.
Outness
The extent to which participants were out as sexual minority persons to other people was measured using the eight-item composite score of the Outness Inventory (65). Sample items included, “To which degree does your father know about your sexual orientation?” and “To which degree do your work peers know about your sexual orientation?” Likert-type response options ranged from 1 (person definitely does not know about your sexual orientation status) to 7 (person definitely knows about your sexual orientation status), with higher scores indicating more outness as a sexual minority person (Cronbach α = .91).
DNA Methylation–Derived Estimates of Accelerated Cellular Aging
The EEAA measure and leukocyte telomere length were estimated with methylation of selected cytosine-phosphate-guanosine groups from genome-wide methylation of DNA extracted from leukocytes using the Infinium Methylation EPIC array (Illumina, San Diego, California). Samples were preprocessed using standard procedures as described previously (66) to yield validated estimates of the EEAA, leukocyte telomere length, and naive CD4+ and CD8+ T-cell levels (5,67–70).
Soluble Markers of Immune Activation and Inflammation
Plasma levels of soluble CD14 and soluble CD163 (sCD163) were determined using Human Quantikine Immunoassay (R&D Systems, Minneapolis, Minnesota) following the manufacturer’s instructions. For soluble CD14 measurement, samples were diluted 400-fold, and results were expressed in nanograms per milliliter. For sCD163 measurement, samples were diluted 30-fold, and results were expressed in nanograms per milliliter. Plasma levels of tumor necrosis factor α and interleukin 6 (IL-6) were obtained via twofold undiluted plasma samples using the Human Quantikine Immunoassay (R&D Systems) following the manufacturer’s instructions.
Statistical Analyses
We began by conducting zero-order correlations to examine bivariate associations among DNA methylation–derived estimates of accelerated cellular aging, sexual minority stress, and soluble markers of inflammation and immune activation. All measures were normally distributed except for sCD163 and tumor necrosis factor α, which were log10 transformed. Guided by zero-order correlations, we conducted 15 multiple linear regression analyses examining the associations of sexual minority stress processes with methylation-derived estimates of accelerated cellular aging and plasma IL-6 after adjusting for negative affect and recent stimulant use. A sensitivity analysis examined the robustness of these associations after replacing recent stimulant use with the ASI Drug Score. Each sexual minority stress measure was further tested in a separate linear regression because of collinearity among these conceptually related independent variables (71). Finally, we examined interaction effects to determine whether the beneficial associations of outness with these outcomes were moderated by race and ethnicity (i.e., more pronounced among non-Hispanic White men versus men of color).
RESULTS
Among the 52 participants, ages ranged from 24 to 59 years with a mean (standard deviation [SD]) of 43.3 (9.5) years. Half of the participants were White (52%), 25% were Hispanic/Latino, 12% were African American, 4% were Asian American, and 7% were other ethnic minorities or multiracial. Most participants completed at least some college (76%), and 67% had an income of less than US $16,000 per year. The median baseline CD4+ T-cell count was 670 (interquartile range = 468–9569) cells/mm3. Participants had been living with HIV for an average (SD) of 14.1 (8.7) years. In addition, participants had been prescribed ART for a mean (SD) of 11.1 (7.1) years.
As shown in Table 1, we examined bivariate associations among sexual minority stress processes, DNA methylation–derived estimates relevant to cellular aging, and soluble markers of immune activation and dysregulation. Greater sexual minority stress scores were significantly associated with a faster EEAA clock (r = 0.35; p = .011), shorter leukocyte telomere length (r = −0.049; p = .0003), and fewer naive CD4+ (r = −0.54; p < .0001) and naive CD8+ (r = −0.57; p < .0001) T cells. Scatterplots of the associations of sexual minority stress with these outcomes are provided in Figure 2. Greater internalized heterosexism was significantly associated with shorter leukocyte telomere length (r = −0.32; p = .020) as well as fewer naive CD4+ (r = −0.37; p = .008) and naive CD8+ (r = −0.34; p < .010) T cells. Finally, higher outness scores were significantly associated with greater naive CD4+ (r = 0.30; p = .030) and naive CD8+ (r = 0.40; p = .004) T cells as well as lower plasma IL-6 (r = −0.32; p = .020). None of the soluble markers of immune activation or inflammation were significantly associated with DNA methylation–derived measures relevant to cellular aging.
TABLE 1.
Associations Among DNA Methylation–Derived Markers of Cellular Aging, Soluble Markers of Immune Dysregulation, and Sexual Minority Stress (N = 52)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. EEAA clock | − | ||||||||||
| 2. Telomere length | −0.71*** | — | |||||||||
| 3. Naive CD4+ | −0.19 | 0.42** | — | ||||||||
| 4. Naive CD8+ | −0.45*** | 0.60*** | 0.70*** | — | |||||||
| 5. sCD14 | 0.25 | −0.27 | −0.09 | −0.18 | — | ||||||
| 6. sCD163 (1og10) | −0.18 | 0.05 | −0.14 | −0.10 | −0.06 | — | |||||
| 7. IL-6 | −0.16 | 0.02 | 0.01 | 0.05 | 0.16 | 0.17 | — | ||||
| 8. TNF-α (log10) | −0.08 | −0.02 | −0.15 | −0.08 | 0.17 | −0.01 | −0.27 | — | |||
| 9. Sexual minority stress | 0.35* | −0.49*** | −0.54*** | −0.57*** | 0.14 | −0.05 | 0.16 | 0.15 | — | ||
| 10. Internalized heterosexism | 0.20 | −0.32* | −0.37*** | −0.34* | 0.03 | −0.24 | 0.17 | 0.17 | 0.39** | — | |
| 11. Outness | −0.14 | 0.24 | 0.30* | 0.40** | −0.11 | −0.07 | −0.32* | −0.07 | −0.60** | −0.31* | — |
| Mean | 0.96 | 6.89 | 618.32 | 211.71 | 1888.86 | 661.72 | 2.26 | 2.02 | 11.97 | 1.80 | 4.80 |
| SD | 12.58 | 0.34 | 85.03 | 37.32 | 496.23 | 379.32 | 1.88 | 0.09 | 5.71 | 0.93 | 1.75 |
| Skewness | −0.87 | 0.22 | 0.34 | 0.17 | 0.49 | 4.91 | 2.03 | −0.03 | 0.56 | 1.02 | −0.73 |
EEAA = extrinsic epigenetic age acceleration; CD4+ = T-helper cells; CD8+ = T-cytotoxic/suppression cells; sCD14 = soluble CD14; sCD163 = soluble CD163; IL-6 = interleukin 6; TNF-α = tumor necrosis factor α; SD = standard deviation.
Analyses were zero-order Pearson correlations.
* p < .05.
** p < .01.
*** p < .001.
FIGURE 2.

Scatterplots of the bivariate associations of greater sexual minority stress with DNA methylation–derived makers of cellular aging (N = 52). CD4+ = T-helper cells.
Multiple linear regression analyses examined the direct associations of sexual minority stress with DNA methylation–derived measures of cellular aging and IL-6 (Table 2). After adjusting for negative affect and recent stimulant use, greater sexual minority stress was directly associated with a faster EEAA clock (β = 0.29; p = .030), shorter leukocyte telomere length (β = −0.43; p = .002), fewer naive CD4+ T cells (β = −0.57; p < .001), and fewer naive CD8+ T cells (β = −0.57; p < .001). These models accounted for 21.9% of the variance (R2 = 0.219) in the EEAA clock, 30.4% of the variance (R2 = 0.304) in leukocyte telomere length, 30.7% of the variance (R2 = 0.307) in naive CD4+ T cells, and 33.0% of the variance (R2 = 0.330) in naive CD8+ T cells. Higher internalized heterosexism was directly associated with lower counts of naive CD4+ (β = −0.35; p = .012) and CD8+ (β = −0.31; p = .026) T cells, with the models accounting for 14.6% (R2 = 0.146) and 14.2% (R2 = 0.142) of the variance in these outcomes. Finally, greater outness was directly associated with more naive CD4+ (β = 0.32; p = .030) naive CD8+ (β = 0.38; p = .008) T cells and lower plasma IL-6 (β = −0.33; p = .027), with models accounting for 11.1% (R2 = 0.111), 17.8% (R2 = 0.178), and 12.0% (R2 = 0.120) of the variance in these outcomes. This pattern of findings was unchanged in models controlling for the ASI Drug Score instead of recent stimulant use. There was no evidence from moderation analyses that the beneficial associations of outness with these outcomes were more pronounced among non-Hispanic White men.
TABLE 2.
Direct Associations of Sexual Minority Stress Processes With DNA Methylation–Derived Markers of Cellular Aging and Inflammation (N = 52)
| EEAA Clock | Telomere Length | Naive CD4+ | Naive CD8+ | IL-6 | |
|---|---|---|---|---|---|
| β | β | β | β | β | |
| Sexual minority stress | 0.29* | −0.43** | −0.57*** | −0.57*** | 0.19 |
| Internalized heterosexism | 0.14 | −0.26 | −0.35* | −0.31* | 0.19 |
| Outness | −0.14 | 0.23 | 0.32* | 0.38** | −0.33* |
EEAA = extrinsic epigenetic age acceleration; CD4+ = T-helper cells; CD8+ = T-cytotoxic/suppressor cells; IL-6 = interleukin 6.
Sexual minority stress processes were entered into separate linear regression models that included negative affect and recent stimulant use as covariates.
* p < .05.
** p < .01.
*** p < .001.
DISCUSSION
Findings from this cross-sectional study indicated that sexual minority stress is directly associated with DNA methylation–derived measures relevant to cellular aging after adjusting for prevailing negative affect and recent stimulant use. Most notably, the model examining a composite measure of sexual minority stress accounted for a medium-large proportion of the variance in the EEAA clock, which has been shown to be elevated in people with HIV up to 2 years after ART initiation (22). We also observed that sexual minority stress was directly associated with DNA methylation–derived estimates of shorter leukocyte telomere length as well as fewer naive CD4+ and CD8+ T cells. The fact that these associations remained even after adjusting for negative affect provides direct support for the minority stress model (48,49), which emphasizes the centrality of sexual minority stress processes in negative health outcomes and related disparities. Associations of sexual minority stress with measures of cellular aging also remained after adjusting for recent stimulant use and severity of substance use that have been previously linked to immune dysregulation in those with treated HIV (31–35). Based on the proposed conceptual model (Figure 1), these results will guide future longitudinal studies to examine the biobehavioral mechanisms for the indirect effects of sexual minority stress such as increased negative affect and stimulant use that alter ANS and HPA axis functioning to influence measures of cellular aging and immune dysregulation among people with and without HIV.
There was also some evidence that specific dimensions of sexual minority stress were directly associated with cellular aging and inflammation. Greater internalized heterosexism was associated with fewer naive CD4+ and CD8+ T cells after adjusting for negative affect and recent stimulant use. This is consistent with prior studies documenting the negative consequences of internalized heterosexism (72,73). Furthermore, greater outness was associated with more naive CD4+ and naive CD8+ T cells as well as lower plasma IL-6 levels. These findings are consistent with previously documented benefits of outness in sexual minority men with HIV before the modern ART era (74). Further research is needed to better characterize the potential benefits of outness in the context of important sources of social adversity affecting sexual minority men in different regions and among racially diverse populations (75,76). Although we did not observe that beneficial associations of outness were more pronounced among non-Hispanic White sexual minority men, the potential moderating effects of social adversity as well as race and ethnicity should be carefully examined in future longitudinal studies examining markers of cellular aging and inflammation. Taken together, findings highlight that there may be important health benefits of cognitive-behavioral treatments to provide coping skills for managing sexual minority stress, challenging cognitions linked to internalized heterosexism, and examining the potential benefits of disclosing one’s sexual identity in contexts where there is likely to be a supportive outcome (77,78). Further clinical research is needed to determine whether and how interventions to modify sexual minority stress processes could alter epigenetic markers relevant to cellular aging and inflammation.
This study should be interpreted in the context of some limitations. First, the cross-sectional design and modest sample size limited our ability to determine if sexual minority stress predicted increases in cellular aging and inflammation over time. Longitudinal research is needed to replicate and extend these findings as well as examine multilevel determinants and biobehavioral mechanisms relevant to the effects of sexual minority stress. As shown in Figure 1, advancing our basic understanding of the mediating mechanisms (e.g., negative affect and stimulant use) for the associations of sexual minority stress processes would guide more comprehensive approaches to reduce cellular aging and inflammation in sexual minority men.
Randomized controlled trials should also test the efficacy of cognitive-behavioral interventions targeting sexual minority stress processes for improving epigenetic aging, which would provide more direct, causal evidence for the role of sexual minority stress processes on cellular aging and inflammation. Second, although prior studies have observed associations of shorter telomere length with inflammation (36), there were no significant associations of soluble markers of immune activation or inflammation with DNA methylation–derived measures of cellular aging. Future studies should include more comprehensive panels of soluble markers of immune activation and dysregulation to determine if measures of epigenetic aging can yield more precise estimates of risk for negative health outcomes. Third, the present study enrolled sexual minority men with treated HIV who use methamphetamine residing in San Francisco. The fact that sexual minority stress processes were associated with these outcomes in a progressive community underscores their potentially enduring consequences. Further research in more representative samples of sexual minority men with and without HIV is needed to examine the generalizability of these findings. Fourth, although we leveraged a composite measure of the EEAA clock to minimize the false discovery rate, future studies should plan for adequate statistical power with the appropriate statistical corrections for multiple tests as well as examining theory-based moderators (e.g., race and ethnicity) and mediators (e.g., negative affect).
Despite these limitations, this study is among the first to observe that sexual minority stress is associated with accelerated cellular aging in methamphetamine-using men with treated HIV. These results provide direct support for the scientific premise of longitudinal research to elucidate biobehavioral mechanisms whereby sexual minority stress processes accelerate biological aging in men with and without HIV. Furthermore, findings highlight the need for clinical research examining the efficacy of interventions targeting different aspects of sexual minority stress with respect to measures of accelerated cellular aging and immune dysregulation.
Acknowledgments
This project was supported by the National Institute on Drug Abuse (R01-DA033854: Carrico, Woods, and Moskowitz, principal investigators [PIs]; K23-DA039800 and R01-DA052016: Flentje, PI). Additional support for this project was provided by the University of California, San Francisco Center for AIDS Research’s Virology Core (P30-AI027763: Volberding, PI) and the Miami Center for AIDS Research (P30-AI073961: Pahwa, PI).
D.G. and A.W.C. share co-primary first authorship.
Source of Funding and Conflicts of Interest: The authors have no conflicts of interest to report.
Open Access publication for this article, which is part of a special themed issue of Psychosomatic Medicine, was funded by the National Institute of Mental Health.
Footnotes
D.G. and A.W.C. are co-primary first authors.
Contributor Information
Delaram Ghanooni, Email: dghanooni@med.miami.edu.
Renessa Williams, Email: rsw95@med.miami.edu.
Tiffany R. Glynn, Email: trglynn@mgh.harvard.edu.
Judith T. Moskowitz, Email: judith.moskowitz@northwestern.edu.
Savita Pahwa, Email: spahwa@med.miami.edu.
Suresh Pallikkuth, Email: spallikkuth@med.miami.edu.
Margaret E. Roach, Email: mroach@med.miami.edu.
Samantha Dilworth, Email: Samantha.Dilworth@ucsf.edu.
Bradley E. Aouizerat, Email: bea4@nyu.edu.
Annesa Flentje, Email: annesa.flentje@ucsf.edu.
REFERENCES
- 1.Justice AC. HIV and aging: time for a new paradigm. Curr HIV/AIDS Rep 2010;7:69–76. [DOI] [PubMed] [Google Scholar]
- 2.Brenchley JM Price DA Schacker TW Asher TE Silvestri G Rao S, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 2006;12:1365–71. [DOI] [PubMed] [Google Scholar]
- 3.Lederman MM, Funderburg NT, Sekaly RP, Klatt NR, Hunt PW. Residual immune dysregulation syndrome in treated HIV infection. Adv Immunol 2013;119:51–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babu H Ambikan AT Gabriel EE Svensson Akusjarvi S Palaniappan AN Sundaraj V, et al. Systemic inflammation and the increased risk of Inflamm-aging and age-associated diseases in people living with HIV on long term suppressive antiretroviral therapy. Front Immunol 2019;10:1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horvath S, Levine AJ. HIV-1 infection accelerates age according to the epigenetic clock. J Infect Dis 2015;212:1563–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernal E Martinez M Torres A Guillamon CF Alcaraz A Alcaraz MJ, et al. T cell senescence predicts subclinical atherosclerosis in HIV-infected patients similarly to traditional cardiovascular risk factors. Antiviral Res 2019;162:163–70. [DOI] [PubMed] [Google Scholar]
- 7.Brites-Alves C Luz E Netto EM Ferreira T Diaz RS Pedroso C, et al. Immune activation, proinflammatory cytokines, and conventional risks for cardiovascular disease in HIV patients: a case-control study in Bahia, Brazil. Front Immunol 2018;9:1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fontela C Castilla J Juanbeltz R Martinez-Baz I Rivero M O’Leary A, et al. Comorbidities and cardiovascular risk factors in an aged cohort of HIV-infected patients on antiretroviral treatment in a Spanish hospital in 2016. Postgrad Med 2018;130:317–24. [DOI] [PubMed] [Google Scholar]
- 9.Ataro Z, Ashenafi W, Fayera J, Abdosh T. Magnitude and associated factors of diabetes mellitus and hypertension among adult HIV-positive individuals receiving highly active antiretroviral therapy at Jugal Hospital, Harar, Ethiopia. HIV AIDS (Auckl) 2018;10:181–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fahme SA, Bloomfield GS, Peck R. Hypertension in HIV-infected adults: novel pathophysiologic mechanisms. Hypertension 2018;72:44–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar S, Dhanwal DK. Central obesity & dyslipidemia in HIV patients on antiretroviral therapy. Indian J Med Res 2018;148:366–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiwanitkit S, Wiwanitkit V. Dyslipidemia among HIV-infected patients. Ann Afr Med 2014;13:142. [DOI] [PubMed] [Google Scholar]
- 13.Todowede OO, Sartorius B. Prevalence of metabolic syndrome, discrete or comorbid diabetes and hypertension in sub-Saharan Africa among people living with HIV versus HIV-negative populations: a systematic review and meta-analysis protocol. BMJ Open 2017;7:e016602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Putcharoen O Wattanachanya L Sophonphan J Siwamogsatham S Sapsirisavat V Gatechompol S, et al. New-onset diabetes in HIV-treated adults: predictors, long-term renal and cardiovascular outcomes. AIDS 2017;31:1535–43. [DOI] [PubMed] [Google Scholar]
- 15.Prioreschi A Munthali RJ Soepnel L Goldstein JA Micklesfield LK Aronoff DM, et al. Incidence and prevalence of type 2 diabetes mellitus with HIV infection in Africa: a systematic review and meta-analysis. BMJ Open 2017;7:e013953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Compston J. HIV infection and osteoporosis. Bonekey Rep 2015;4:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leng SX, Margolick JB. Understanding frailty, aging, and inflammation in HIV infection. Curr HIV/AIDS Rep 2015;12:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Althoff KN McGinnis KA Wyatt CM Freiberg MS Gilbert C Oursler KK, et al. Comparison of risk and age at diagnosis of myocardial infarction, end-stage renal disease, and non–AIDS-defining cancer in HIV-infected versus uninfected adults. Clin Infect Dis 2015;60:627–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doshi S Ucanda M Hart R Hou Q Terzian AS, DC Cohort Executive Committee . Incidence and risk factors for renal disease in an outpatient cohort of HIV-infected patients on antiretroviral therapy. Kidney Int Rep 2019;4:1075–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eggers C Arendt G Hahn K Husstedt IW Maschke M Neuen-Jacob E, et al. HIV-1–associated neurocognitive disorder: epidemiology, pathogenesis, diagnosis, and treatment. J Neurol 2017;264:1715–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zayyad Z, Spudich S. Neuropathogenesis of HIV: from initial neuroinvasion to HIV-associated neurocognitive disorder (HAND). Curr HIV/AIDS Rep 2015;12:16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sehl ME Rickabaugh TM Shih R Martinez-Maza O Horvath S Ramirez CM, et al. The effects of anti-retroviral therapy on epigenetic age acceleration observed in HIV-1–infected adults. Pathog Immun 2020;5:291–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oblak L, van der Zaag J, Higgins-Chen AT, Levine ME, Boks MP. A systematic review of biological, social and environmental factors associated with epigenetic clock acceleration. Ageing Res Rev 2021;69:101348. [DOI] [PubMed] [Google Scholar]
- 24.Esch T, Kream RM, Stefano GB. Chromosomal processes in mind-body medicine: chronic stress, cell aging, and telomere length. Med Sci Monit Basic Res 2018;24:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zanet DL Thorne A Singer J Maan EJ Sattha B Le Campion A, et al. Association between short leukocyte telomere length and HIV infection in a cohort study: no evidence of a relationship with antiretroviral therapy. Clin Infect Dis 2014;58:1322–32. [DOI] [PubMed] [Google Scholar]
- 26.Carrico AW Hunt PW Neilands TB Dilworth SE Martin JN Deeks SG, et al. Stimulant use and viral suppression in the era of universal antiretroviral therapy. J Acquir Immune Defic Syndr 2019;80:89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carrico AW Shoptaw S Cox C Stall R Li X Ostrow DG, et al. Stimulant use and progression to AIDS or mortality after the initiation of highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2014;67:508–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cook JA Burke-Miller JK Cohen MH Cook RL Vlahov D Wilson TE, et al. Crack cocaine, disease progression, and mortality in a multicenter cohort of HIV-1 positive women. AIDS 2008;22:1355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saloner R Fields JA Marcondes MCG Iudicello JE von Kanel S Cherner M, et al. Methamphetamine and cannabis: a tale of two drugs and their effects on HIV, brain, and behavior. J Neuroimmune Pharmacol 2020;15:743–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prasad A, Kulkarni R, Shrivastava A, Jiang S, Lawson K, Groopman JE. Methamphetamine functions as a novel CD4(+) T-cell activator via the sigma-1 receptor to enhance HIV-1 infection. Sci Rep 2019;9:958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carrico AW Cherenack EM Roach ME Riley ED Oni O Dilworth SE, et al. Substance-associated elevations in monocyte activation among methamphetamine users with treated HIV infection. AIDS 2018;32:767–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carrico AW Flentje A Kober K Lee S Hunt P Riley ED, et al. Recent stimulant use and leukocyte gene expression in methamphetamine users with treated HIV infection. Brain Behav Immun 2018;71:108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grosgebauer K Salinas J Sharkey M Roach M Pallikkuth S Dilworth SE, et al. Psychosocial correlates of monocyte activation and HIV persistence in methamphetamine users. J Neuroimmune Pharmacol 2018;14:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Massanella M Gianella S Schrier R Dan JM Perez-Santiago J Oliveira MF, et al. Methamphetamine use in HIV-infected individuals affects T-cell function and viral outcome during suppressive antiretroviral therapy. Sci Rep 2015;5:13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller M Lee JY Fulcher JA Roach ME Dilworth SE Chahine A, et al. Getting to the point: methamphetamine injection is associated with biomarkers relevant to HIV pathogenesis. Drug Alcohol Depend 2020;213:108133. [DOI] [PubMed] [Google Scholar]
- 36.Mehta SR Iudicello JE Lin J Ellis RJ Morgan E Okwuegbuna O, et al. Telomere length is associated with HIV infection, methamphetamine use, inflammation, and comorbid disease risk. Drug Alcohol Depend 2021;221:108639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med 2008;70:539–45. [DOI] [PubMed] [Google Scholar]
- 38.Ironson G, Fitch C, Stuetzle R. Depression and survival in a 17-year longitudinal study of people with HIV: moderating effects of race and education. Psychosom Med 2017;79:749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ironson G O’Cleirigh C Fletcher MA Laurenceau JP Balbin E Klimas N, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med 2005;67:1013–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leserman J Pence BW Whetten K Mugavero MJ Thielman NM Swartz MS, et al. Relation of lifetime trauma and depressive symptoms to mortality in HIV. Am J Psychiatry 2007;164:1707–13. [DOI] [PubMed] [Google Scholar]
- 41.Pariante CM, Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci 2008;31:464–8. [DOI] [PubMed] [Google Scholar]
- 42.Cole SW. Psychosocial influences on HIV-1 disease progression: neural, endocrine, and virologic mechanisms. Psychosom Med 2008;70:562–8. [DOI] [PubMed] [Google Scholar]
- 43.Cole SW, Naliboff BD, Kemeny ME, Griswold MP, Fahey JL, Zack JA. Impaired response to HAART in HIV-infected individuals with high autonomic nervous system activity. Proc Natl Acad Sci U S A 2001;98:12695–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ironson G O’Cleirigh C Kumar M Kaplan L Balbin E Kelsch CB, et al. Psychosocial and Neurohormonal predictors of HIV disease progression (CD4 cells and viral load): a 4 year prospective study. AIDS Behav 2015;19:1388–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Samji H Cescon A Hogg RS Modur SP Althoff KN Buchacz K, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One 2013;8:e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Katz IT, Maughan-Brown B. Improved life expectancy of people living with HIV: who is left behind? Lancet HIV 2017;4:e324–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Palella FJ Hart R Armon C Tedaldi E Yangco B Novak R, et al. Non-AIDS comorbidity burden differs by sex, race, and insurance type in aging adults in HIV care. AIDS 2019;33:2327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129:674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Meyer IH. Prejudice as stress: conceptual and measurement problems. Am J Public Health 2003;93:262–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Flentje A Kober KM Carrico AW Neilands TB Flowers E Heck NC, et al. Minority stress and leukocyte gene expression in sexual minority men living with treated HIV infection. Brain Behav Immun 2018;70:335–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li MJ, Takada S, Okafor CN, Gorbach PM, Shoptaw SJ, Cole SW. Experienced homophobia and gene expression alterations in Black and Latino men who have sex with men in Los Angeles County. Brain Behav Immun 2020;83:120–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thames AD, Irwin MR, Breen EC, Cole SW. Experienced discrimination and racial differences in leukocyte gene expression. Psychoneuroendocrinology 2019;106:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cole SW. The conserved transcriptional response to adversity. Curr Opin Behav Sci 2019;28:31–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goldbach JT, Tanner-Smith EE, Bagwell M, Dunlap S. Minority stress and substance use in sexual minority adolescents: a meta-analysis. Prev Sci 2014;15:350–63. [DOI] [PubMed] [Google Scholar]
- 55.Li MJ, Okafor CN, Gorbach PM, Shoptaw S. Intersecting burdens: homophobic victimization, unstable housing, and methamphetamine use in a cohort of men of color who have sex with men. Drug Alcohol Depend 2018;192:179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Birkett M, Espelage DL, Koenig B. LGB and questioning students in schools: the moderating effects of homophobic bullying and school climate on negative outcomes. J Youth Adolesc 2009;38:989–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vincent W Carrico AW Dilworth SE Fuchs D Neilands TB Moskowitz JT, et al. Intersecting minority statuses and tryptophan degradation among stimulant-using, sexual minority men living with HIV. J Consult Clin Psychol 2021;89:156–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carrico AW Gόmez W Jain J Shoptaw S Discepola MV Olem D, et al. Randomized controlled trial of a positive affect intervention for methamphetamine users. Drug Alcohol Depend 2018;192:8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carrico AW Neilands TB Dilworth SE Evans JL Gomez W Jain JP, et al. Randomized controlled trial of a positive affect intervention to reduce HIV viral load among sexual minority men who use methamphetamine. J Int AIDS Soc 2019;22:e25436. [DOI] [PMC free article] [PubMed]
- 60.Cacciola JS, Alterman AI, McLellan AT, Lin Y-T, Lynch KG. Initial evidence for the reliability and validity of a “Lite” version of the Addiction Severity Index. Drug Alcohol Depend 2007;87:297–302. [DOI] [PubMed] [Google Scholar]
- 61.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol 2003;84:365–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carrico AW Woods WJ Siever MD Discepola MV Dilworth SE Neilands TB, et al. Positive affect and processes of recovery among treatment-seeking methamphetamine users. Drug Alcohol Depend 2013;132:624–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chu J, Floyd R, Diep H, Pardo S, Goldblum P, Bongar B. A tool for the culturally competent assessment of suicide: the Cultural Assessment of Risk for Suicide (CARS) measure. Psychol Assess 2013;25:424–34. [DOI] [PubMed] [Google Scholar]
- 64.Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: insights froma social psychological perspective. J Couns Psychol 2019;56:32. [Google Scholar]
- 65.Mohr J, Fassinger R. Measuring dimensions of lesbian and gay male experience. Meas Eval Counsel Dev 2000;33:66. [Google Scholar]
- 66.Zhang X Hu Y Justice AC Li B Wang Z Zhao H, et al. DNA methylation signatures of illicit drug injection and hepatitis C are associated with HIV frailty. Nat Commun 2017;8:2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen BH Marioni RE Colicino E Peters MJ Ward-Caviness CK Tsai P-C, et al. DNA methylation–based measures of biological age: meta-analysis predicting time to death. Aging (Albany NY). 2016;8:1844–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Horvath S. DNA methylation age of human tissues and cell types. Genome Biol 2013;14:R115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Horvath S Gurven M Levine ME Trumble BC Kaplan H Allayee H, et al. An epigenetic clock analysis of race/ethnicity, sex, and coronary heart disease. Genome Biol 2016;17:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lu AT Seeboth A Tsai P-C Sun D Quach A Reiner AP, et al. DNA methylation–based estimator of telomere length. Aging (Albany NY) 2019;11:5895–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Flentje A Clark KD Cicero E Capriotti MR Lubensky ME Sauceda J, et al. Minority stress, structural stigma, and physical health among sexual and gender minority individuals: examining the relative strength of the relationships. Ann Behav Med 2021;56:573–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clin Psychol Rev 2010;30:1019–29. [DOI] [PubMed] [Google Scholar]
- 73.Flentje A, Heck NC, Brennan JM, Meyer IH. The relationship between minority stress and biological outcomes: a systematic review. J Behav Med 2020;43:673–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cole SW, Kemeny ME, Taylor SE, Visscher BR, Fahey JL. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosom Med 1996;58:219–31. [DOI] [PubMed] [Google Scholar]
- 75.Anderson-Carpenter KD. Do spirituality, rurality, and LGBTQ support increase outness and quality of health in gay and bisexual men? J Homosex 2022;69:1081–96. [DOI] [PubMed] [Google Scholar]
- 76.Kauth MR, Barrera TL, Denton FN, Latini DM. Health differences among lesbian, gay, and transgender veterans by rural/small town and suburban/urban setting. LGBT Health 2017;4:194–201. [DOI] [PubMed] [Google Scholar]
- 77.Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol 2015;83:875–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Flentje A. AWARENESS: development of a cognitive-behavioral intervention to address intersectional minority stress for sexual minority men living with HIV who use substances. Psychotherapy (Chic) 2020;57:35–49. [DOI] [PMC free article] [PubMed] [Google Scholar]


