Abstract
The coronavirus disease 2019 (COVID-19) pandemic has created a global health crisis, with disproportionate effects on vulnerable sociodemographic groups. Although the pandemic is showing potential to increase suicide ideation (SI), we know little about which sociodemographic characteristics or COVID-19 experiences are associated with SI. Our United States-based sample (n = 837 adults [mean age = 37.1 years]) completed an online survey during August–September 2020. The study utilized an online convenience sample from a prior study, which was enriched for exposure to trauma and experiences of posttraumatic stress symptoms. We assessed SI using the Beck Depression Inventory-II. Traditional (i.e., logistic regression) and machine learning (i.e., LASSO, random forest) methods evaluated associations of 148 self-reported COVID-19 factors and sociodemographic characteristics with current SI. 234 participants (28.0%) reported SI. Twenty items were significantly associated with SI from logistic regression. Of these 20 items, LASSO identified seven sociodemographic characteristics (younger age, lower income, single relationship status, sexual orientation other than heterosexual as well as specifically identifying as bisexual, non-full-time employment, and living in a town) and six COVID-19 factors (not engaging in protective COVID-19 behaviors, receiving mental health treatment (medication and/or psychotherapy) due to the COVID-19 pandemic, socializing during the pandemic, losing one's job due to COVID-19, having a friend with COVID-19, and having an acquaintance with COVID-19) associated with SI. Random forest findings were largely consistent with LASSO. These findings may inform multidisciplinary research and intervention work focused on understanding and preventing adverse mental health outcomes such as SI during and in the aftermath of the pandemic.
Keywords: Machine learning, Suicide, Covid-19, Posttraumatic stress disorder, Depression
Suicide is a major global public health concern, with 800,000 individuals dying by suicide each year (World Health Organization, 2014). In contrast to declining rates of mortality across numerous health conditions, deaths from suicide have remained stable or increased (World Health Organization, 2014). The coronavirus disease 2019 (COVID-19) pandemic has resulted in mental health consequences including increases in depression and posttraumatic stress disorder (PTSD) symptoms, as well as suicide ideation, in certain vulnerable groups (Czeisler et al., 2021; Robinson et al., 2022; Vindegaard and Benros, 2020; Xie et al., 2022). Previous infectious disease epidemics, including the 2003 SARS epidemic and prior influenza epidemics, have been associated with increases in deaths by suicide (Zortea et al., 2020). Social isolation, economic strain, fears of infection, and uncertainty about the future may contribute to suicide risk during the COVID-19 pandemic (Reger et al., 2020; Yao et al., 2020), particularly for groups who have been disproportionately impacted by these stressors.
As a first step towards informing suicide research and prevention efforts during and following the COVID-19 pandemic, we must identify the sociodemographic groups most at risk and the COVID-19-related factors most associated with suicide ideation (SI). SI is characterized by thinking about or planning to kill oneself, and is present in nearly all suicide attempts and deaths by suicide (Klonsky et al., 2016; Nock et al., 2008). A nationally representative survey (n = 5412) in the United States (U.S.) conducted during the COVID-19 pandemic found that 10.7% of adults reported SI in June 2020 (Czeisler et al., 2020), whereas only 4.3% of adults in the U.S. reported SI during the previous 12 months in 2018 in a U.S. population-based survey (n = 67,791) aged 12 and older (SAMHSA, 2019). The COVID-19 Social Study in the United Kingdom (n = 44,775) reported that 17.8% of adults reported SI in March and April 2020 (Iob et al., 2020). However, we know little about the factors associated with SI during the COVID-19 pandemic.
Posttraumatic stress disorder (PTSD) and depression are strong risk factors for and correlates of SI (Cougle et al., 2009; LeBouthillier et al., 2015; Tarrier and Gregg, 2004). PTSD symptoms commonly co-occur with SI (Cougle et al., 2009; Kessler et al., 2005), and each additional trauma exposure increases SI risk by 20.1% based on a nationally representative sample (n = 34,653) of people with PTSD in the U.S. (LeBouthillier et al., 2015). SI is frequently observed in the context of depression (Kessler et al., 2005), and, reflecting this high degree of comorbidity, SI is included in the diagnostic criteria for major depressive disorder (American Psychiatric Association, 2013). Existing studies on SI during the COVID-19 pandemic have been evaluated in non-clinical convenience samples. However, a study of university students in China (n = 2485) reported increases in symptoms of both PTSD and depression during the pandemic (Tang et al., 2020). There is a need to examine SI after adjusting for the presence of well-established predictors of SI like symptoms of PTSD and depression in a sample specifically recruited for these symptoms, which is the focus of the current study.
COVID-19 pandemic experiences may be important for identifying and targeting SI. First, those who have suffered the greatest economic impact of the pandemic appear to be those experiencing the highest levels of distress in a sample (n = 389) from Israel (Achdut and Refaeli, 2020), but it is unclear if they are also at greater risk for SI. Second, shelter-in-place orders and social distancing measures have resulted in unprecedented levels of social disconnection and isolation, which has been linked to greater psychological distress in a nationally-representative sample (n = 6585) from the U.S. (Kämpfen et al., 2020). Third, social distancing policies may decrease access to mental health treatment according to an opinion piece (Reger et al., 2020), which may exacerbate mental health stigma among low income individuals, women, and racial/ethnic minorities (Nadeem et al., 2007; Taylor and Richards, 2019). Fourth, exposure to COVID-19 may increase fear of contracting COVID-19 as well as fear for significant others according to an opinion piece (Schimmenti et al., 2020). Fifth, SI is associated with greater risk-taking in a sample (n = 377) of U.S. adults (Athey et al., 2018). People experiencing SI may engage in risky pandemic behaviors such as not practicing social distancing or not wearing a mask. The extant literature has not identified if such features of the COVID-19 pandemic are associated with SI.
Sociodemographic characteristics are strong predictors of COVID-19 disease and pandemic-related stressors. Sociodemographic factors predict SI in general (Franklin et al., 2017; Walsh et al., 2017), and are emerging as correlates of SI during the pandemic. A survey of adults in the U.S. (n = 10,368) found that identifying as Black, Native American, or Hispanic as well as having children, being unmarried, and being younger were associated with SI during the COVID-19 pandemic after adjusting for physical and psychological health (Fitzpatrick et al., 2020). However, important sociodemographic characteristics were not evaluated including educational attainment, employment status, sexual orientation, or genders beyond male and female. In another general population sample in the U.S. (n = 5412), SI was highest among those who were younger, identified as female, reported economic strain, and experienced physical and mental health problems (Czeisler et al., 2020). We do not know which sociodemographic factors are associated with SI over and above PTSD and depression severity.
Multiple factors across multiple domains are related to SI. Much of the existing research has focused on single domains rather than examining factors across and within domains, which may lead to biased effect sizes (Fanelli and Ioannidis, 2013). Advances in statistical computing and machine learning have made it possible to develop prediction models based on associations between a large number of predictors that otherwise would be too wide-ranging and overlapping to be investigated in observational or experimental designs (Cox et al., 2020; Lewinn et al., 2020; Puterman et al., 2020). Studies focused on suicide risk have made use of these methods to move beyond single-domain hypotheses (Simon et al., 2018; van Mens et al., 2020; Walsh et al., 2017). An environment-wide association approach that evaluates variables across domains has the potential to identify cross-disciplinary correlates of SI and advance our understanding of SI during the COVID-19 pandemic as well as into the future.
In this study, we examined cross-sectional associations of a broad range of COVID-19 pandemic factors and sociodemographic characteristics with SI in a racially and socioeconomically diverse sample of 837 adults living in the U.S. Given the well-established associations between psychiatric conditions and SI, this study utilized an online convenience sample of adults interested in participating in a prior study focused on trauma and posttraumatic stress. First, we examined the contribution of each individual predictor to SI in logistic regression models, adjusting for current depression and PTSD symptoms. Next, our study made use of two data-driven machine-learning techniques, Least Absolute Shrinkage and Selection Operator (LASSO) regression and random forest analysis, to identify which of 148 COVID-19 factors and sociodemographic characteristics were most closely linked with SI. This approach facilitates the examination of associations between multiple variables and SI while minimizing prediction error and overestimation of effects.
1. Method
1.1. Sample
Community-dwelling adults residing in the United States were recruited from a prior PTSD-focused study conducted in 2017–2018 (Niles et al., 2020). This 2017–2018 study recruited participants via Craigslist ads and Reddit discussion forums related to posttraumatic stress or trauma recovery. Craigslist and Reddit are online communities that have been previously utilized to recruit participants for online survey research (Watson et al., 2018). Individuals (n = 3631) interested in the 2017–2018 study, whether or not they participated or met criteria for that study, were contacted via email about participating in a follow-up study regarding the COVID-19 pandemic. Of the 3631 individuals contacted, 1000 started the survey. Among these 1,000, 1 did not consent, 78 did not complete the consent, and 25 did not provide demographic information, which provided an eligible sample of 896 participants. We refer to this sample as “enriched” for trauma exposure and posttraumatic stress symptoms given that 96.9% of participants had a history of trauma, the average PCL score was 40.33 (SD = 19.5), and 32.8% of participants reported symptoms consistent with a probable diagnosis of PTSD (PCL ≥ 33). The analytic sample for this study included participants with a response on the SI measure. There were 59 (6.6%) participants with missing SI data, which resulted in a sample of 837. Supplemental Table 2 compares the 2017–2018 screening data among all potential survey respondents (n = 3361) and by non-participants (n = 2794) versus the analytic sample (n = 837). The participants in the analytic sample were older and had lower PTSD severity than non-participants. Participants received a $5 gift card upon completing the survey. Data were collected between August 4, 2020 and September 19, 2020. This study was approved and conducted in compliance with the Institutional Review Board at the University of California, San Francisco.
1.2. Measures
1.2.1. Primary outcome
Suicide ideation (SI). Current SI was assessed with the Beck Depression Inventory-II (BDI-II) and included the following options: “I don't have any thoughts of killing myself”, “I have thoughts of killing myself, but I would not carry them out.“, “I would like to kill myself.“, and “I would kill myself if I had the chance.” (Beck et al., 1996). A response greater than 0 was used to categorize SI (0 = SI-, 1 = SI+), which is consistent with prior research demonstrating high predictive validity for death by suicide and repeated suicide attempts (Green et al., 2015).
1.2.2. Predictors
A total of 148 self-reported variables were identified as potential predictors of SI. Descriptions of study variables are reported in Supplemental Table 1.
Sociodemographic characteristics. Variables included age, education, employment status, gender, type of residence, income, living with other people, number of people in the household, people living in the house, race/ethnicity, relationship status, sexual orientation, type of area of residence, and United States Census Region.
COVID-19 pandemic factors. Self-reported experiences specific to COVID-19 were assessed.
COVID-19 risk and protective behaviors. A sum score of protective behaviors included the average frequency of viewing news, washing/sanitizing hands, mask wearing, sanitizing packages, stockpiling supplies, changing clothes, social distancing, isolating, and taking health supplements. A sum score of risk behaviors included going to the grocery store, using public transportation, taking a flight, attending an indoor or outdoor gathering, attending a large event, and eating at indoor or outdoor restaurants.
COVID-19 status and exposure. Participants self-reported confirmed, probable, and potential exposure to COVID-19 regarding oneself, one's household, acquaintances, close family, extended family, friends, neighbors, and/or anyone else. Quarantine status and symptom severity of COVID was assessed.
Social interaction during COVID-19. Items included in-person social interaction for dining/drinking, exercise, medical/dental, religious reasons, shopping/chores, socializing, work/education, and other.
Vulnerability to COVID-19. Participants reported a history of medical conditions and weight (5-point scale from “normal weight” to “obese”). Participants estimated their likelihood of contracting COVID-19 (5-point scale from “very unlikely” to “very likely”), as well as expected severity of COVID-19 symptoms if contracted (5-point scale from “mild” to “extreme”).
COVID-19 employment. Items included employment-related changes due to COVID-19 including difficulty working due to caregiving, gaining a job, experiencing an increased workload, laying off or furloughing employees, losing hours/income, losing a job, or working in unsafe conditions. We asked if participants’ work involved direct COVID-19 care, supportive COVID-19 care, or no COVID-19 care.
Mental and physical health changes. Items included mental health treatment (medication and/or psychotherapy) due to psychological distress experienced because of the COVID-19 pandemic (yes/no), positive life changes resulting from COVID-19 pandemic (5-point scale from “a great deal” to “none at all”), as well as COVID-19-related changes in sleep (5-point scale from “much worse than normal” to “much better than normal”), alcohol and/or cannabis use (5-point scale from “decreased a lot” to “increased a lot”), and experiences of discrimination (5-point scale from “no experience of discrimination prior to COVID” to “very large increase”).
Perceived Threat of Pandemic Scale. Items examined perceived current and future threat of COVID-19 to work life, education and training, financial security, housing, social relationships (inside and outside the home), emotional health, and physical health (5-point scale from “no threat” to “extreme threat”) based on Niles and O’Donovan (2018).
1.2.3. Covariates
Past month depression symptoms assessed by the Depression Anxiety Stress Scales (Lovibond and Lovibond, 1995) and past month posttraumatic symptoms measured by the PTSD Checklist for the DSM-5 (PCL-5; Weathers et al., 2013) were included as covariates because SI frequently occurs among individuals with depression and PTSD symptoms (Cougle et al., 2009; LeBouthillier et al., 2015; Tarrier and Gregg, 2004).
1.3. Data analysis
Data analysis occurred in multiple steps. In Step 1, 148 separate binomial logistic regression models were specified for each of the variables with SI as the outcome while adjusting for depression and PTSD symptoms. Associations were considered statistically significant with a nominal p < 0.05. Continuous variables were mean-centered. Categorical variables with two response options were coded as 0 or 1. Categorical variables with multiple response options were converted to an indicator variable with a value of 1 with all other levels as −1.
In Step 2, a LASSO model was estimated with all variables significantly associated with SI from Step 1. Thus, variables included in Step 2 were associated with SI independent of depression and PTSD symptoms. LASSO is a type of regularized linear regression that shrinks the effect of variables weakly associated with the outcome toward 0 and assists with variable selection. Analyses were implemented with the “glmnet” package in R (Friedman et al., 2010).
In Step 3, random forest analysis was used to assess the robustness of our findings when using different methods of data analysis. Variables significantly associated with SI from Step 1 were entered into the random forest model. Random forest is a nonparametric machine learning algorithm that is an extension of classification and regression trees (Breiman, 2001). Random forest is an ensemble learning technique that creates multiple classification models and aggregates the results. In contrast to other methods such as decision trees that create a single classification tree, random forest uses a bootstrapping method to take a predetermined number of random samples (n = 500 in the current study) of the data with replacement and produces classification trees with each random sample of data. In each random sample, some of the data is left out of the algorithm to create an out of bag (OOB) sample. Once each classification tree is created, these trees are tested on the OOB sample to determine the accuracy of the models and the prediction “importance” of each variable. Compared with other classification methods, random forest reduces the variance and risk of overfitting, which improves the prediction accuracy of the model. Analyses were implemented with the “randomForest” package in R (Liaw and Wiener, 2002).
LASSO regression and random forest require complete data. Missing data were imputed using “missForest,” which produced a single dataset (Stekhoven and Bühlmann, 2012). Thirty variables had missing data (mean = 0.05%, range = 0.00%–0.48%). Number of observations prior to imputation are reported in Supplemental Table 1.
2. Results
2.1. Sample characteristics
Participants primarily identified as cisgender women (73.6%), 20.1% identified as cisgender men, and 2.5% identified as a gender other than cisgender men or women. Sample demographics reflected those of the U.S. in terms of race and ethnicity with 14.1% identifying as Black/African American, 11.0% as Asian, 10.9% as Latinx, 63.1% as non-Hispanic white, and 8.7% as other or more than one race. The average age was 37.1 years (SD = 11.1 years). 63.4% had a 4-year college degree or more. The median income range was $50,001 to $60,000 per year and 55.8% were employed full-time.
Of the 837 participants included in the analytic sample, 234 (28.0%) reported current SI (SI+) and 603 (72.0%) reported no current SI (SI-). As predicted, higher odds of reporting SI were observed for participants with higher depression symptoms (OR = 3.21, 95% CI = 2.67, 3.86) and higher PTSD symptoms (OR = 2.48, 95% CI = 2.09, 2.94). Complete descriptive statistics and unadjusted ORs and 95% CIs for study variables are provided in Supplemental Table 1.
2.2. Correlates of suicide ideation in the COVID-19 pandemic
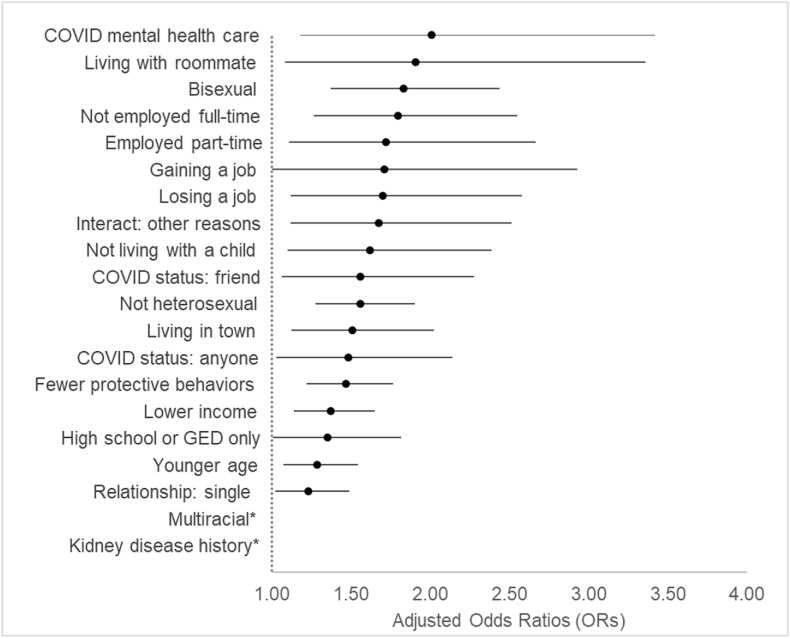
In Step 1, 20 of the 148 variables evaluated in logistic regressions were significantly associated with SI after adjusting for depression and PTSD symptoms (Fig. 1 ). In Step 2, LASSO regression retained 13 of the 20 variables associated with SI from Step 1. Statistics from Steps 1 and 2 are reported in Table 1 .
Fig. 1.
Odds ratios from logistic regression models of variables associated with suicide ideation. Note. Points on figure are odds ratios (OR) derived from logistic regression models adjusting for depression and PTSD symptoms. ORs for variables with negative coefficients were calculated as 1/exp(coefficient). Error bars represent 95% confidence intervals (95% CI).* The OR and 95% CI for kidney disease history (OR = 9.91, 95% CI = 1.07, 91.29) and multiracial (OR = 3.50, 95% CI = 1.32, 9.33) are not depicted in order to enhance the legibility of the figure and because the estimates may be unstable given the small number of individuals endorsing these items (kidney disease history: n = 10, 1.2%; multiracial: n = 23, 2.7%).
Table 1.
Model coefficients, odds ratios, and R-squared values for variables associated with suicide ideation.
|
B |
OR |
B |
OR |
95% CI |
p |
|
|---|---|---|---|---|---|---|
| (lasso) | (lasso) | (log. reg.) | (log. reg.) | (log. reg.) | (log. reg.) | |
| COVID-19 Pandemic Experiences | ||||||
| COVID-19 mental health care | 0.303 | 1.35 | 0.698 | 2.01 | [1.18, 3.42] | 0.010 |
| Lost a job | 0.234 | 2.00 | 0.530 | 1.70 | [1.12, 2.58] | 0.013 |
| Interact: other reasons | 0.114 | 1.12 | 0.516 | 1.68 | [1.12, 2.51] | 0.013 |
| COVID status: friend | 0.114 | 1.12 | 0.443 | 1.56 | [1.06, 2.28] | 0.023 |
| COVID status: anyone | 0.035 | 1.04 | 0.394 | 1.48 | [1.03, 2.14] | 0.035 |
| Protective COVID-19 behaviors | −0.192 | 1.21 | −0.384 | 1.47 | [1.22, 1.77] | <0.001 |
| Gained a joba | 0.000 | 1.00 | −0.538 | 1.71 | [1.00, 2.93] | 0.049 |
| Sociodemographic Characteristics | ||||||
| Age | −0.089 | 1.09 | −0.252 | 1.29 | [1.07, 1.54] | 0.007 |
| Area type: Live in town | 0.092 | 1.10 | 0.410 | 1.51 | [1.12, 2.02] | 0.007 |
| Sexual orientation: Bisexual | 0.107 | 1.11 | 0.604 | 1.83 | [1.37, 2.44] | <0.001 |
| Sexual orientation: Heterosexual | −0.309 | 1.36 | −0.442 | 1.56 | [1.27, 1.90] | <0.001 |
| Income | −0.174 | 1.19 | −0.316 | 1.37 | [1.14, 1.65] | 0.001 |
| Employed full-time | −0.150 | 1.16 | −0.586 | 1.80 | [1.26, 2.55] | 0.001 |
| Relationship status: Single | 0.029 | 1.03 | 0.208 | 1.23 | [1.02, 1.49] | 0.030 |
| Multiraciala | 0.000 | 1.00 | 1.254 | 3.50 | [1.32, 9.33] | 0.012 |
| High school or GED onlya | 0.000 | 1.00 | 0.303 | 1.35 | [1.01, 1.82] | 0.044 |
| Employed part-timea | 0.000 | 1.00 | 0.543 | 1.72 | [1.11, 2.67] | 0.015 |
| Living with a childa | 0.000 | 1.00 | −0.483 | 1.62 | [1.10, 2.39] | 0.015 |
| Living with roommatea | 0.000 | 1.00 | 0.645 | 1.91 | [1.08, 3.36] | 0.026 |
| Kidney disease historya | 0.000 | 1.00 | −2.293 | 9.91 | [1.07, 91.79] | 0.043 |
Note. OR: odds ratio. 95% CI: 95% confidence interval. Log. reg.: logistic regression statistical estimate adjusting for depression symptoms and posttraumatic stress symptoms. ORs for variables with negative coefficients were calculated as 1/exp(coefficient).
Variable was not retained by LASSO regression model.
Six COVID-19 pandemic experience variables were retained by LASSO regression (Table 1). Compared with SI- participants, SI+ was associated with: engaging in mental health treatment (medication and/or psychotherapy) due to psychological distress experienced because of the COVID-19 pandemic (SI+: 17.5%, SI-: 6.5%); knowing a friend (SI+: 34.2%, SI-: 21.9%) or an acquaintance (SI+: 67.9%, SI-: 58.2%) who had been diagnosed with COVID-19; and losing a job due to the COVID-19 pandemic (SI+: 28.6%, SI-: 14.4%). A higher percentage of SI + participants socially interacted for “other” reasons (SI+: 28.2%, SI-: 18.2%) and engaged in fewer protective COVID-19 behaviors (SI + average: 2.6, SI- average: 2.8).
Seven sociodemographic variables were selected by LASSO regression (Table 1). SI + participants, compared with SI-, were younger (SI + mean age: 34.8 years, SI-: 38.0 years). A higher percentage of SI + participants were not employed full-time (SI+: 56.4%, SI-: 39.5%). SI + participants had lower income (SI+: $50,001 to $60,000 per year, SI-: $70,001 to $80,000 per year). SI was more common among individuals who did not identify as heterosexual (SI+: 34.6%, SI-: 16.6%) compared with all other sexual orientations, and specifically people who identified as bisexual (SI+: 16.3%, SI-: 5.1%). SI + participants were more often single and not in a relationship (SI+: 34.8%, SI-: 25.2%) and tended to live in a town compared with living in a city, suburb, or rural area (SI+: 12.4%, SI-: 6.1%).
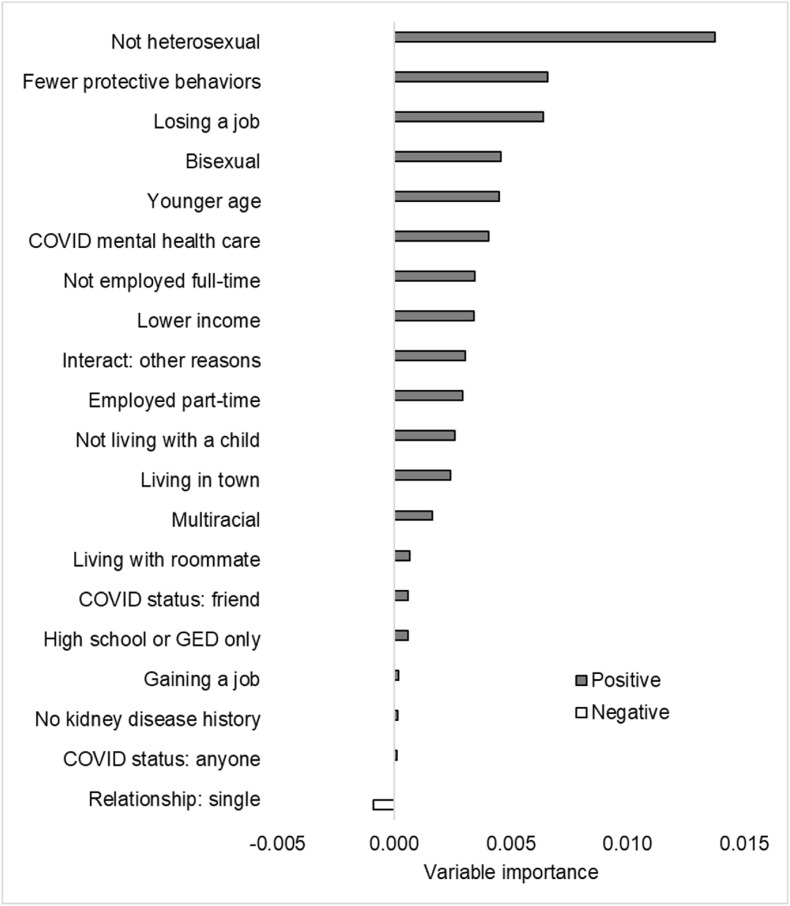
Random forest analysis (Step 3) was used to examine the 20 variables associated with SI from Step 1. Random forest assigns an importance score to all variables rather than dropping less important variables like LASSO. Importance scores are depicted in Fig. 2 . Positive importance scores indicate that the variable increases the accuracy of the random forest model whereas negative scores decrease the accuracy. Nine of the top 10 most important correlates of SI ranked by random forest were variables retained by LASSO. Only one variable—single relationship status—had a negative importance score, which indicated that this variable reduced the predictive accuracy of the random forest model and is thus less useful for classifying SI.
Fig. 2.
Random forest to classify suicide ideation (absence/presence). Note. Variables included in random forest analysis included 20 variables significantly (p < 0.05) associated with SI from logistic regression (Step 1). Variables with positive importance values increased the accuracy of the random forest algorithm; negative values decrease accuracy. Negative values are likely due to random error.
3. Discussion
The goal of our study was to identify the most salient COVID-19 factors and sociodemographic characteristics associated with SI in a racially and socioeconomically diverse sample of 837 adults enriched for trauma exposure and posttraumatic stress symptoms. In this sample, 28.0% of participants reported current SI. SI prevalence estimates during the COVID-19 pandemic have ranged from 10.7 to 17.8% in the general population and 22.1–44.8% among adults with clinically significant psychiatric symptoms (Czeisler et al., 2020; Iob et al., 2020). After adjustment for depression and PTSD symptoms, machine learning analyses identified six COVID-19 pandemic factors and seven sociodemographic characteristics associated with SI from among 148 variables. These data highlight that pre-pandemic vulnerabilities and specific pandemic stressors could be useful for identifying individuals at risk for SI, both now and in the aftermath of the pandemic.
Some of the most compelling findings from our models were that job loss because of COVID-19 as well as having lower income and non-full-time employment were important correlates of SI. The COVID-19 pandemic has had devastating economic consequences. A survey of adults in the U.S. (n = 13,200) found that 15% of adults reported losing their jobs due to the pandemic between March and August 2020 (Pew Research Center, 2020), the period of time covered by our survey. Economic losses have been especially severe for those who were more socioeconomically vulnerable prior to the pandemic. Indeed, lower income adults, relative to middle- and upper income adults, who lost their jobs due to the COVID-19 pandemic were 29.7% less likely to have returned to work by August 2020 (Pew Research Center, 2020). Experts have hypothesized in opinion pieces that unemployment and economic strain may be especially strong contributors to suicide in the aftermath of the COVID-19 pandemic (Bastiampillai et al., 2020). The current findings provide initial empirical evidence that the economic consequences of the COVID-19 pandemic may be key contributors to SI.
Social disconnection has been a defining experience of the COVID-19 pandemic. Having a friend or acquaintance with COVID-19 was associated with SI, which may increase concerns for the health of others and signal the need to socially isolate. SI was more common in towns, which are more densely populated than rural areas but less populated than cities or suburban areas (Geverdt, 2015). Pre-pandemic social connection experienced in towns may paradoxically foster greater psychological vulnerability given the relatively larger increase in social isolation experienced by those with higher pre-pandemic social integration (Henning-Smith et al., 2018). This study was conducted between August and September 2020, a period in which COVID case rates were increasing in the Midwest and South, particularly in small metropolitan counties and nonmetropolitan U.S. counties, and decreasing in other regions (Frey, 2021). Our statistical models included U.S. region as well as degree of urbanicity, and the present findings indicate that assessing urbanicity may be more relevant to SI than region of the U.S. However, larger samples are needed to test this hypothesis.
Single relationship status was associated with SI. Marriage may be a deterrent to suicide (Yip and Thorburn, 2004), in part due to the availability of social and emotional support from one's partner (Qin et al., 2003), however, these studies were conducted before the pandemic. In the context of the pandemic, people were instructed to socialize only with those in their households, and individuals with a single relationship status may have experienced greater decreases in social support than those in romantic relationships. Social interaction for reasons other than dining/drinking, exercise, medical/dental, religious reasons, shopping/chores, socializing, and work/education was also associated with SI. Although interpretation of this finding is challenging, people experiencing more distress may engage in more social interaction overall during the pandemic, perhaps as a means of interpersonal emotion regulation (Zaki and Williams, 2013). Similarly, people with probable PTSD engaged in more social interaction during the pandemic (Nishimi et al., 2022b). These experiences highlight the deleterious effect the pandemic has had on social connection, and the potential consequences for SI.
The COVID-19 pandemic has included the uptake of multiple new behaviors to slow the spread of the virus. Individuals with SI engaged less frequently in COVID-19 protective behaviors. This finding may reflect an increase in risk taking and a decrease in self-care, which are associated with SI (Athey et al., 2018). Fewer COVID-19 protective behaviors could also signify ambivalence regarding one's health and well-being, which may be a potential warning sign for SI. In an online study of 907 adults, 7.4% of participants reported intentional COVID-19 exposure with suicide intent (Ammerman et al., 2021). Additional research is needed to evaluate whether these higher-risk COVID-19 factors may function as suicide-related behaviors.
Our findings highlight the role of pre-pandemic sociodemographic characteristics and SI in our trauma-enriched sample. Sexual orientation was among the most robust correlates of SI, including having a sexual orientation other than heterosexual, as well as specifically identifying as bisexual. LGBTQ + individuals were at markedly elevated risk for suicide before the pandemic (Pompili et al., 2014). Moreover, as a result of the pandemic, LGBTQ + individuals have experienced greater psychological stress, depression, and identity-based discrimination based on evidence from a survey (n = 398) of LGBTQ + individuals from April to July 2020 (Kneale and Bécares, 2020). Younger age was also associated with SI, which is consistent with pre-pandemic epidemiological and machine learning studies (Nock et al., 2008; Walsh et al., 2017). Moreover, accumulating evidence indicates that younger adults may be more susceptible to psychological stress resulting from the pandemic (Carstensen et al., 2020; Nwachukwu et al., 2020). The pandemic may be perceived as threatening to current and future opportunities for personal and career progression, which may affect younger individuals to a greater extent than older individuals. Mental health interventions during and after the pandemic should be targeted at and tailored to the particular needs of these vulnerable individuals.
Rising rates of SI highlight the critical need for mental healthcare in the context of the COVID-19 pandemic (Czeisler et al., 2020; Iob et al., 2020). There was an increase in emergency department (ED) visits related to mental health from mid-March 2020 to October 2020 based on data that included 70% of U.S. ED visits (Holland et al., 2021), approximately the period of time covered by our study. In our study, 17.5% of participants with SI, compared with 6.5% without SI, sought out mental healthcare such as medication and/or psychotherapy due to the pandemic. This finding is encouraging given that individuals with SI sought out this mental health treatment despite restrictions on in-person treatment. Nonetheless, most individuals with SI did not seek out additional mental healthcare, highlighting the need for reducing barriers and expanding access to treatment.
Our study points to pre-pandemic vulnerabilities and stressors that may confer risk for adverse mental health outcomes like SI. Although the focus of the current study was on SI, the present findings may also inform policy decisions aimed at reducing death by suicide. For example, we found that economic strain was an important contributor to SI during the COVID-19 pandemic. If replicated, these findings may suggest that government policies aimed at reducing economic strain may play an important role in suicide prevention. During the 2008 economic recession, findings from Japan and Denmark demonstrated that increased government spending resulted in lower rates of suicide (Matsubayashi et al., 2020; Steeg et al., 2020). Additionally, the present findings may inform public health efforts to help alleviate the COVID-19 pandemic. The CDC includes mood disorders such as depression and schizophrenia spectrum disorders among the conditions with greater susceptibility to severe COVID-19 illness (CDC, 2021). In this study, we found evidence that engaging in activities that may increase risk for COVID-19 such as socializing were associated with higher risk for SI, which is in line with findings indicating that PTSD, depression, and anxiety are associated with more risky behaviors for contracting COVID-19 (Nishimi et al., 2022a, 2022b). Taken together, these findings suggest that targeted behavioral interventions could be helpful for individuals experiencing distress during the pandemic. COVID-19 continues to contribute to significant morbidity and mortality across the world, and there is a need to identify novel risk factors that may help to mitigate the spread of COVID-19 and reduce adverse mental health consequences of the pandemic.
This study has several limitations. First, this study was cross-sectional and as with other machine-learning suicide-focused studies (Gradus et al., 2020; Walsh et al., 2017), it is not possible to determine the directionality or causality of the observed effects. Prospective studies will be needed to evaluate how COVID-19 factors and sociodemographic characteristics relate to future SI. Second, LASSO regression identifies the most salient predictors from a large set of variables while minimizing prediction error; however, models have high specificity but low sensitivity. Similarly, random forest determines variable importance based on predictive accuracy of variables aggregated over multiple classification trees. Thus, the LASSO and random forest models may have selected variables slightly more predictive overall but missed other variables still important for predicting SI. It is encouraging that among the 13 variables selected by LASSO, nine were highly ranked variables by the random forest analysis. Third, although SI is on the continuum of suicide risk, most individuals with SI do not attempt suicide (Nock et al., 2008). Additional research is needed to examine sociodemographic and COVID-19-specific predictors of suicide-related behaviors and deaths by suicide during and following the pandemic. Fourth, the current sample utilized the same recruitment pool as a prior PTSD-focused treatment study conducted in 2017–2018 (see also Niles et al., 2020). In addition to being recruited from an unknown population of Craigslist and Reddit users, the participants in this study had higher rates of trauma exposure and PTSD symptoms than the general population. Thus, these findings may not generalize beyond Craigslist and Reddit users with a history of trauma exposure. Additionally, the majority of participants in this sample identified as women. Women are twice as likely as men to experience trauma and posttraumatic sequelae (Tolin and Foa, 2006). Nevertheless, overrepresentation of women is common in survey research (Dickinson et al., 2012), and future studies would benefit from samples that more closely reflect the gender distribution of the population of interest.
As the COVID-19 pandemic continues to unfold, there is serious concern regarding the impact of the pandemic on mental health and an escalating need to identify those at greatest risk for poor mental health outcomes such as SI. In a sample enriched for trauma exposure and posttraumatic stress symptoms, we identified a range of COVID-19 pandemic factors and sociodemographic characteristics associated with SI. Taken together with other emerging data on SI and suicide during the COVID-19 pandemic, these findings can inform suicide prevention efforts during and following these challenging times. The current study provides evidence that specific individual characteristics and exposures may warrant further investigation for COVID-19 prevention efforts, with implications for researchers and interventionists across a variety of disciplines.
Author statement
Conceptualization: EAD, KN, KZL, PT, EW, AJK, BPM, BB, AJ, TCN, AOD; Methodology: EAD, KN, KZL, ALB, AOD; Writing – Original Draft: EAD, AOD; Writing – Reviewing and Editing: EAD, KN, KZL, ALB, PT, EW, AJK, BPM, BB, AJ, TCN, AOD; Statistical analysis: EAD; Resources: TCN, AOD; Data curation: EAD, KN, PT; Funding Acquisition: AOD. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding statement
This work was supported by the UCSF Department of Psychiatry Rapid Award (AOD), the National Institutes of Mental Health (AOD; K01MH109871), and a Mental Illness Research and Education Clinical Center fellowship of the U.S. Veterans Health Administration at the San Francisco VA Healthcare System (EAD).
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.10.009.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Achdut N., Refaeli T. Unemployment and psychological distress among young people during the COVID-19 pandemic: psychological Resources and risk factors. Int. J. Environ. Res. Publ. Health. 2020;17:7163. doi: 10.3390/ijerph17197163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. fifth ed. American Psychiatric Publishing, Inc; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders. 5th ed. [Google Scholar]
- Ammerman B.A., Burke T.A., Jacobucci R., McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J. Psychiatr. Res. 2021;134:32–38. doi: 10.1016/j.jpsychires.2020.12.037. [DOI] [PubMed] [Google Scholar]
- Athey A., Overholser J., Bagge C., Dieter L., Vallender E., Stockmeier C.A. Risk-taking behaviors and stressors differentially predict suicidal preparation, non-fatal suicide attempts, and suicide deaths. Psychiatr. Res. 2018;270:160–167. doi: 10.1016/j.psychres.2018.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastiampillai T., Allison S., Looi J.C.L., Licinio J., Wong M.L., Perry S.W. The COVID-19 pandemic and epidemiologic insights from recession-related suicide mortality. Mol. Psychiatr. 2020:3445–3447. doi: 10.1038/s41380-020-00875-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A., Steer R., Brown G. 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- Breiman L. Random forests. Mach. Learn. 2001;45:5–32. doi: 10.1023/A:1010933404324. [DOI] [Google Scholar]
- Carstensen L.L., Shavit Y.Z., Barnes J.T. Age advantages in emotional experience persist even under threat from the COVID-19 pandemic. Psychol. Sci. 2020;31:1374–1385. doi: 10.1177/0956797620967261. [DOI] [PubMed] [Google Scholar]
- CDC . 2021. COVID-19: People with Certain Medical Conditions.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html [WWW Document]. URL. [Google Scholar]
- Cougle J.R., Resnick H., Kilpatrick D.G. PTSD, depression, and their comorbidity in relation to suicidality: cross-sectional and prospective analyses of a national probability sample of women. Depress. Anxiety. 2009;26:1151–1157. doi: 10.1002/da.20621. [DOI] [PubMed] [Google Scholar]
- Cox C.R., Moscardini E.H., Cohen A.S., Tucker R.P. Machine learning for suicidology: a practical review of exploratory and hypothesis-driven approaches. Clin. Psychol. Rev. 2020;82 doi: 10.1016/j.cpr.2020.101940. [DOI] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Wiley J.F., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, september 2020. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.37665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson E.R., Adelson J.L., Owen J. Gender balance, representativeness, and statistical power in sexuality research using undergraduate student samples. Arch. Sex. Behav. 2012:325–327. doi: 10.1007/S10508-011-9887-1. 2012 412 41. [DOI] [PubMed] [Google Scholar]
- Fanelli D., Ioannidis J.P.A. US studies may overestimate effect sizes in softer research. Proc. Natl. Acad. Sci. U.S.A. 2013;110:15031–15036. doi: 10.1073/pnas.1302997110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. How bad is it? Suicidality in the middle of the COVID-19 pandemic. Suicide Life-Threatening Behav. 2020:1–9. doi: 10.1111/sltb.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin J.C., Ribeiro J.D., Fox K.R., Bentley K.H., Kleiman E.M., Huang X., Musacchio K.M., Jaroszewski A.C., Chang B.P., Nock M.K. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol. Bull. 2017;143:187–232. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- Frey W.H. Brookings; 2021. One Year In, COVID-19’s Uneven Spread Across the US Continues.https://www.brookings.edu/research/one-year-in-covid-19s-uneven-spread-across-the-us-continues/ [Google Scholar]
- Friedman J., Hastie T., Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Software. 2010;33:1–22. doi: 10.18637/jss.v033.i01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geverdt D. U.S. Department of Education. Washington, DC: National Center for Education Statistics; 2015. Education Demographic and Geographic Estimates Program (EDGE): Locale Boundaries User’s Manual (NCES 2016-012)http://nces.ed.gov/pubsearch Retrieved [date] from. [Google Scholar]
- Gradus J.L., Rosellini A.J., Horváth-Puhó E., Street A.E., Galatzer-Levy I., Jiang T., Lash T.L., Sørensen H.T. Prediction of sex-specific suicide risk using machine learning and single-payer health care registry data from Denmark. JAMA Psychiatr. 2020;77:25–34. doi: 10.1001/jamapsychiatry.2019.2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green K.L., Brown G.K., Jager-Hyman S., Cha J., Steer R.A., Beck A.T. The predictive validity of the Beck Depression Inventory suicide item. J. Clin. Psychiatr. 2015;76:1683–1686. doi: 10.4088/JCP.14m09391. [DOI] [PubMed] [Google Scholar]
- Henning-Smith C., Ecklund A., Kozhimannil K. Rural-urban differences in social isolation and its relationship to health. Innov. Aging. 2018;2 doi: 10.1093/geroni/igy023.2851. 770–770. [DOI] [PubMed] [Google Scholar]
- Holland K.M., Jones C., Vivolo-Kantor A.M., Idaikkadar N., Zwald M., Hoots B., Yard E., D'Inverno A., Swedo E., Chen M.S., Petrosky E., Board A., Martinez P., Stone D.M., Law R., Coletta M.A., Adjemian J., Thomas C., Puddy R.W., Peacock G., Dowling N.F., Houry D. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatr. 2021 doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iob E., Steptoe A., Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry. 2020;217:543–546. doi: 10.1192/bjp.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kämpfen F., Kohler I.V., Ciancio A., de Bruin W.B., Maurer J., Kohler H.P. Predictors of mental health during the Covid-19 pandemic in the US: role of economic concerns, health worries and social distancing. PLoS One. 2020;15:1–13. doi: 10.1371/journal.pone.0241895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Borges G., Nock M., Wang P.S. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. J. Am. Med. Assoc. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Klonsky E.D., May A.M., Saffer B.Y. Suicide, suicide attempts, and suicidal ideation. Annu. Rev. Clin. Psychol. 2016;12:307–330. doi: 10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- Kneale D., Bécares L. The mental health and experiences of discrimination of LGBTQ+ people during the COVID-19 pandemic: initial findings from the Queerantine Study. medRxiv. 2020 doi: 10.1101/2020.08.03.20167403. 2020.08.03.20167403. [DOI] [Google Scholar]
- LeBouthillier D.M., McMillan K.A., Thibodeau M.A., Asmundson G.J.G. Types and number of traumas associated with suicidal ideation and suicide attempts in PTSD: findings from a U.S. Nationally representative sample. J. Trauma Stress. 2015;28:183–190. doi: 10.1002/jts.22010. [DOI] [PubMed] [Google Scholar]
- Lewinn K.Z., Bush N.R., Batra A., Tylavsky F., Rehkopf D. Identification of modifiable social and behavioral factors associated with childhood cognitive performance. JAMA Pediatr. 2020;174:1063–1072. doi: 10.1001/jamapediatrics.2020.2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaw A., Wiener M. Classification and regression by randomForest. R. News. 2002;2:18–22. [Google Scholar]
- Lovibond S.H., Lovibond P.F. Psychology Foundation of Australia; 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- Matsubayashi T., Sekijima K., Ueda M. Government spending, recession, and suicide: evidence from Japan. BMC Publ. Health. 2020;20 doi: 10.1186/s12889-020-8264-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeem E., Lange J.M., Edge D., Fongwa M., Belin T., Miranda J. Does stigma keep poor young immigrant and U.S.-born black and Latina women from seeking mental health care? Psychiatr. Serv. 2007;58:1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
- Niles A.N., O'Donovan A. Personalizing affective stimuli using a recommender algorithm: an example with threatening words for trauma exposed populations. Cognit. Ther. Res. 2018;42:747–757. doi: 10.1007/s10608-018-9923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles A.N., Woolley J.D., Tripp P., Pesquita A., Vinogradov S., Neylan T.C., O'Donovan A. Randomized controlled trial testing mobile-based attention-bias modification for posttraumatic stress using personalized word stimuli. Clin. Psychol. Sci. 2020;8:756–772. doi: 10.1177/2167702620902119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimi K., Borsari B., Marx B.P., Rosen R.C., Cohen B.E., Woodward E., Maven D., Tripp P., Jiha A., Woolley J.D., Neylan T.C., O'Donovan A. Clusters of COVID-19 protective and risky behaviors and their associations with pandemic, socio-demographic, and mental health factors in the United States. Prev. Med. Reports. 2022;25 doi: 10.1016/J.PMEDR.2021.101671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimi K., Borsari B., Marx B.P., Tripp P., Woodward E., Rosen R.C., Cohen B.E., Maven D., Jiha A., Woolley J.D., Neylan T.C., O'Donovan A. Posttraumatic stress disorder symptoms associated with protective and risky behaviors for coronavirus disease 2019. Health Psychol. 2022;41:104–114. doi: 10.1037/hea0001157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M.K., Borges G., Bromet E.J., Alonso J., Angermeyer M., Beautrais A., Bruffaerts R., Wai T.C., De Girolamo G., Gluzman S., De Graaf R., Gureje O., Haro J.M., Huang Y., Karam E., Kessler R.C., Lepine J.P., Levinson D., Medina-Mora M.E., Ono Y., Posada-Villa J., Williams D. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwachukwu I., Nkire N., Shalaby R., Hrabok M., Vuong W., Gusnowski A., Surood S., Urichuk L., Greenshaw A.J., Agyapong V.I.O. Covid-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int. J. Environ. Res. Publ. Health. 2020;17:1–10. doi: 10.3390/ijerph17176366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center . 2020. Economic Fallout from COVID-19 Continues to Hit Lower-Income Americans the Hardest. [Google Scholar]
- Pompili M., Lester D., Forte A., Seretti M.E., Erbuto D., Lamis D.A., Amore M., Girardi P. Bisexuality and suicide: a systematic review of the current literature. J. Sex. Med. 2014 doi: 10.1111/jsm.12581. [DOI] [PubMed] [Google Scholar]
- Puterman E., Weiss J., Hives B.A., Gemmill A., Karasek D., Mendes W.B., Rehkopf D.H. Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proc. Natl. Acad. Sci. U.S.A. 2020;117:16273–16282. doi: 10.1073/pnas.1918455117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin P., Agerbo E., Mortensen P.B. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981-1997. Am. J. Psychiatr. 2003;160:765–772. doi: 10.1176/appi.ajp.160.4.765. [DOI] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019-A perfect storm? JAMA Psychiatr. 2020;77:1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA . HHS Publ; 2019. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. No. PEP19-5068, NSDUH Ser. H-54. [Google Scholar]
- Schimmenti A., Billieux J., Starcevic V. The four horsemen of fear: an integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry. 2020;17:41–45. doi: 10.36131/CN20200202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon G.E., Johnson E., Lawrence J.M., Rossom R.C., Ahmedani B., Lynch F.L., Beck A., Waitzfelder B., Ziebell R., Penfold R.B., Shortreed S.M. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am. J. Psychiatr. 2018;175:951–960. doi: 10.1176/appi.ajp.2018.17101167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steeg S., Carr M.J., Mok P.L.H., Pedersen C.B., Antonsen S., Ashcroft D.M., Kapur N., Erlangsen A., Nordentoft M., Webb R.T. Temporal trends in incidence of hospital-treated self-harm among adolescents in Denmark: national register-based study. Soc. Psychiatr. Psychiatr. Epidemiol. 2020;55:415–421. doi: 10.1007/s00127-019-01794-8. [DOI] [PubMed] [Google Scholar]
- Stekhoven D.J., Bühlmann P. Missforest-Non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28:112–118. doi: 10.1093/bioinformatics/btr597. [DOI] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrier N., Gregg L. Suicide risk in civilian PTSD patients - predictors of suicidal ideation, planning and attempts. Soc. Psychiatr. Psychiatr. Epidemiol. 2004;39:655–661. doi: 10.1007/s00127-004-0799-4. [DOI] [PubMed] [Google Scholar]
- Taylor D., Richards D. Triple jeopardy: complexities of racism, sexism, and ageism on the experiences of mental health stigma among young Canadian black women of caribbean descent. Front. Sociol. 2019;4:43. doi: 10.3389/fsoc.2019.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin D.F., Foa E.B. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol. Bull. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- van Mens K., de Schepper C.W.M., Wijnen B., Koldijk S.J., Schnack H., de Looff P., Lokkerbol J., Wetherall K., Cleare S., C O'Connor R., de Beurs D. Predicting future suicidal behaviour in young adults, with different machine learning techniques: a population-based longitudinal study. J. Affect. Disord. 2020;271:169–177. doi: 10.1016/j.jad.2020.03.081. [DOI] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh C.G., Ribeiro J.D., Franklin J.C. Predicting risk of suicide attempts over time through machine learning. Clin. Psychol. Sci. 2017;5:457–469. doi: 10.1177/2167702617691560. [DOI] [Google Scholar]
- Watson N.L., Mull K.E., Heffner J.L., McClure J.B., Bricker J.B. Participant recruitment and retention in remote eHealth intervention trials: methods and lessons learned from a large randomized controlled trial of two web-based smoking interventions. J. Med. Internet Res. 2018;20 doi: 10.2196/10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. The PTSD Checklist for DSM-5 (PCL-5) 2013. www.ptsd.va.gov Scale available from the National Center for PTSD at.
- World Health Organization . WHO Press. World Health Organization; Geneva: 2014. Preventing Suicide: A Global Imperative. Geneva. [Google Scholar]
- Xie Y., Xu E., Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ. 2022 doi: 10.1136/bmj-2021-068993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatr. 2020;7 doi: 10.1016/S2215-0366(20)30090-0. e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip P.S.F., Thorburn J. Marital status and the risk of suicide: experience from england and wales, 1982-1996. Psychol. Rep. 2004;94:401–407. doi: 10.2466/pr0.94.2.401-407. [DOI] [PubMed] [Google Scholar]
- Zaki J., Williams W.C. Interpersonal emotion regulation. Emotion. 2013;13:803–810. doi: 10.1037/a0033839. [DOI] [PubMed] [Google Scholar]
- Zortea T.C., Brenna C.T.A., Joyce M., McClelland H., Tippett M., Tran M.M., Arensman E., Corcoran P., Hatcher S., Heisel M.J., Links P., O'Connor R.C., Edgar N.E., Cha Y., Guaiana G., Williamson E., Sinyor M., Platt S. Crisis; 2020. The Impact of Infectious Disease-Related Public Health Emergencies on Suicide, Suicidal Behavior, and Suicidal Thoughts: A Systematic Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.