Abstract
Acute myeloid leukemia (AML) is a highly heterogeneous malignancy of the blood and bone marrow, characterized by clonal expansion of myeloid stem and progenitor cells and rapid disease progression. Chemotherapy has been the first-line treatment for AML for more than 30 years. Application of recent high-throughput next-generation sequencing technologies has revealed significant molecular heterogeneity to AML, which in turn has motivated efforts to develop new, targeted therapies. However, due to the high complexity of this disease, including multiple driver mutations and the coexistence of multiple competing tumorigenic clones, the successful incorporation of these new agents into clinical practice remains challenging. These continuing difficulties call for the identification of innovative therapeutic approaches that are effective for a larger cohort of AML patients. Recent studies suggest that chronic immune stimulation and aberrant cytokine signaling act as triggers for AML initiation and progression, facets of the disease which might be exploited as promising targets in AML treatment. However, despite the greater appreciation of cytokine profiles in AML, the exact functions of cytokines in AML pathogenesis are not fully understood. Therefore, unravelling the molecular basis of the complex cytokine networks in AML is a prerequisite to develop new therapeutic alternatives based on targeting cytokines and their receptors.
Keywords: acute myeloid leukemia, cytokine signaling, inflammation, tumor microenvironment, cytokine inhibitors
Introduction
Acute Myeloid Leukemia (AML) is a highly aggressive and heterogenous hematological cancer characterized by the accumulation of molecular and cytogenetic mutations within hematopoietic stem and/or progenitor cells (HSPCs), leading to the establishment of leukemic stem cells (LSCs). LSCs are the source of immature myeloid progenitor cells, so-called myeloblasts or leukemic blasts, which accumulate in the bone marrow (BM), displace normal HSPCs, impair normal hematopoiesis, and eventually spread into the peripheral blood (PB), lymph nodes, liver, spleen, testes, and central nervous system (1–4). Whereas many AML patients follow an aggressive clinical course with an overall 5-year survival rate of only 28%, individual patient survival strongly depends on the underlying tumor-driving genetic alterations and individual risk factors, including age, gender, prior chemotherapy, radiation exposure and genetic predisposition (1, 2, 5–8). However, irrespective of the molecular driver mutations initiating the disease, AML onset and development always go hand in hand with significant remodeling of the BM into a tumor-promoting microenvironment that supports and protects LSCs at the expense of normal HSPCs (9–15). In this review we discuss how cytokine signaling networks contribute to these maladaptations, fuel AML tumorigenesis and progression, and enable chemoresistance and immune evasion. We further shed some light on promising therapeutic approaches targeting cytokine signaling to irradicate the LSC population and prevent relapse after chemotherapy.
Role of cytokines in AML
Within the healthy BM microenvironment, hematopoietic stem cells (HSCs) are normally maintained in a delicate balance between quiescence, self-renewal, and differentiation to ensure life-long steady-state hematopoiesis and replenishment of the blood effector cell population under stress conditions such as infection, acute and chronic inflammation, aging or bleeding (16). During infection and inflammation, an array of cytokines, including Interleukin (IL)-1β (17, 18), IL-3 (19, 20), IL-6 (21–23), Tumor necrosis factor-α (TNF-α) (24–27) and Interferon (IFN) (28, 29) together with hematopoietic growth factors (HGFs) such as M-CSF, G-CSF and GM-CSF (17, 30), orchestrates the switch from steady-state to emergency hematopoiesis (31–33). In patients with preleukemic and leukemic conditions, including AML, the tight regulation of these cytokines is impaired, leading to aberrant cytokine secretion (32–38). Studies evaluating pro- and anti-inflammatory cytokine and growth factor levels in serum revealed that GM-CSF, IL-1β, IL-3, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-27, IL-35, osteopontin and stem cell factor (SCF) are upregulated in all or in distinct AML patient groups compared to age-matched controls (39–43). In contrast to most cytokines, TRAIL and TGF-β levels are decreased in the serum of AML patients (39, 43, 44). To gain insights into the specific functions of individual cytokines and growth factors in AML, numerous studies have characterized the effects of recombinant cytokines and HGFs on proliferation and colony formation of primary AML cells and cell lines in vitro, thereby establishing ex vivo AML cell culture conditions (see Table 1 ).
Table 1.
Cytokines and growth factors supporting or inhibiting AML cells.
| Cytokine | Expression in AML patients compared to healthy individuals | Physiologic function | Function ex vivo in AML cell culture |
|---|---|---|---|
| G-CSF | Not determined | Hematopoietic growth factor | Supports AML cell proliferation and clonogenicity (45–48) |
| GM-CSF | Elevated PB plasma levels and unchanged BM levels (42, 49) | Hematopoietic growth factor | Supports AML cell growth and self-renewal (44, 45, 50) |
| IFN-α | Not determined | Anti-/Pro-inflammatory cytokine | Reduces AML cell proliferation and IL-1, IL-6, GM-CSF expression (51, 52) |
| IFN-γ | Unchanged PB levels and reduced BM levels (39, 53) | Pro-inflammatory cytokine | Reduces AML cell proliferation and survival; increases spontaneous clonogenicity of AML cells (54, 55) |
| IL-1Ra | Elevated PB and reduced BM serum levels (42, 56) | Anti-inflammatory cytokine | Reduces AML cell proliferation (57, 58) |
| IL-1β | Unchanged or elevated PB and unchanged BM levels (39, 41, 42) | Pro-inflammatory cytokine | Supports AML cell proliferation and survival; increases GM-CSF, IL-6 and TNF expression (41, 45, 50, 51, 59, 60) |
| IL-3 | Elevated PB levels (43) | Pro-inflammatory cytokine | Supports AML cell proliferation and self-renewal (45, 47, 61–63) |
| IL-4 | Elevated PB levels in patients > 65 years (39, 53) | Anti-inflammatory cytokine | Inhibits IL-1- and HGF-induced AML cell proliferation (60, 64, 65) |
| IL-6 | Elevated plasma levels (39, 53, 66) | Pro-inflammatory cytokine | Partially supports AML cell proliferation (45, 48, 67–71). |
| IL-8 | Elevated PB and BM levels (39, 44, 66, 72) | Chemoattractant cytokine (chemokine) | Not determined |
| IL-10 | Elevated PB levels (39, 53, 56, 73) | Anti-inflammatory cytokine | Inhibits AML cell proliferation; reduces IL-1α, IL-1β, IL-6, GM-CSF and TNF-α expression (74–76) |
| IL-12p70 | Elevated PB levels in patients > 65 years (39) | Pro-inflammatory cytokine | Inhibits AML cell-induced angiogenesis; supports T cell-mediated cytotoxicity and possibly AML tumor growth (77–79) |
| IL-27 | Elevated PB and BM levels (40) | Anti-inflammatory cytokine | Not determined |
| IL-35 | Elevated PB and BM levels (40, 80, 81) | Anti-inflammatory cytokine | Supports AML cell proliferation and survival; promotes Treg function (80) |
| Osteopontin | Elevated PB and BM levels (44, 82, 83) | Matrix glycoprotein with pro-inflammatory cytokine properties | Supports AML cell self-renewal, proliferation and survival (84) |
| SCF | Elevated PB and BM levels (42) | Hematopoietic growth factor | Supports AML cell proliferation and survival (85–87) |
| TGF-β | Reduced PB and BM levels (39, 53) | Anti-inflammatory cytokine | Inhibits AML cell proliferation and survival (88–90) |
| TNF-α | Elevated PB levels (39, 44, 56, 66) | Pro-inflammatory cytokine | Supports AML cell chemoresistance and maintains proliferating LSCs (91) |
| TRAIL | Reduced PB levels (44) | Pro-inflammatory cytokine | Not determined |
| CXCL12 | Reduced expression in AML blasts (92–94) | Chemoattractant cytokine (chemokine) | Promotes AML cell growth, survival, chemoresistance and adhesion (95–98) |
Importantly, not all patient-derived AML cells or cell lines respond to HGF and cytokine treatment equally well. These observations reflect AML heterogeneity and suggest the presence of leukemic cell subpopulations. PB: peripheral blood; BM: bone marrow.
Suggestive of a supportive feedback loop, some patient-derived LSCs and blasts can produce a variety of cytokines (e.g., IL-1β, IL-1α, IL-6, GM-CSF, and TNF-α) and proliferate in vitro without the addition of exogenous cytokines and HGFs (99–101). In particular, IL-1β was shown to act as an autocrine growth factor for AML blasts by inducing the production of HGFs and cytokines, including GM-CSF and IL-6 (50, 59, 99, 102–105). Moreover, IL-1-stimulated AML blast cells secreted increased levels of TNF-α, which synergized with IL-3- or GM-CSF-induced AML cell proliferation and colony formation (106). Of note, increased autonomous and/or HGF- and cytokine-induced in vitro proliferation of patient-derived leukemic cells correlated with negative clinical outcomes, including lower complete remission rates, higher risk for relapse, and shorter AML patient survival (107–109). In vivo, however, LSC and blast growth, survival, and protection from therapeutic agents do not exclusively rely on endogenous cytokine signaling, but strongly depend on AML cell interactions with the leukemic BM microenvironment and the latter’s provisioning of supporting ligands and soluble factors, including cytokines ( Figure 1 ), some of which are discussed in the following sections (110).
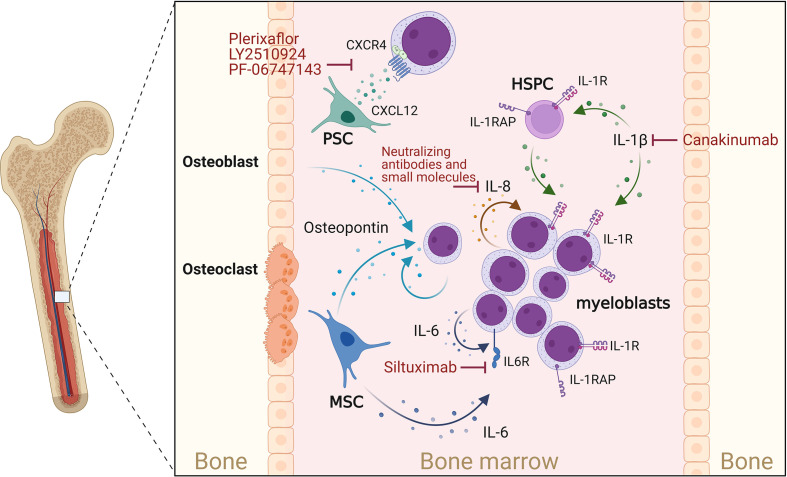
Figure 1.
Cytokines supporting AML progression. Osteoblasts, myeloblasts and mesenchymal stromal cells (MSCs) secrete osteopontin. This in turn promotes AML cell proliferation and disease progression. CXCL12 is mainly secreted by perivascular stromal cells (PSCs), and osteoblasts and promotes growth and survival of AML blasts cell via the chemokine receptor CXCR4. IL-1β acts on myeloblasts and HSPCs, which express the IL-1 receptor (IL-1R) as well as the IL-1 receptor accessor protein (IL-1RAP), thereby enhancing IL-1β production, AML cell proliferation and survival. IL-1 signaling can be blocked by Canakinumab, a human monoclonal antibody targeting IL-1β. IL-8 is constitutively produced by AML myeloblasts and acts in an autocrine way. MSCs and myeloblasts are potent sources of IL-6, which can be blocked by IL-6-blocking antibodies such as Siltuximab. Created with Biorender.com.
AML supporting cytokines
Osteopontin
Osteopontin, a secreted matrix glycoprotein produced by many cell types (e.g., stomal, endothelial, epithelial and immune cells), is crucial for the regulation and/or induction of inflammation, angiogenesis, proliferation, migration, and apoptosis throughout the body. During normal hematopoiesis, osteopontin is predominantly produced by osteoblasts within in the endosteal BM region, to guide and maintain healthy HSCs within supportive niches (111). Interestingly, PB and BM osteopontin levels were significantly increased in AML patients compared to healthy controls, and high osteopontin BM levels were associated with reduced overall and event-free survival (82, 83). Osteopontin was not, however, exclusively expressed by cells of the osteolineage within the leukemic BM, although it was strongly expressed by AML blasts (82). Additionally, it was shown that AML patient-derived mesenchymal stromal cells (MSCs) or healthy MSCs co-cultured with AML cells undergo osteogenic differentiation and produce increased amounts of osteopontin (112). Functionally, osteopontin was shown to upregulate AKT, mTOR, PTEN, and β-catenin mRNA expression in AML cells in vitro (113) and increase AML LSC self-renewal, proliferation, and expression of anti-apoptotic and cell-cycle-associated genes, thereby leading to accelerated disease progression in an MLL-AF9 driven AML mouse model (84). Direct targeting of osteopontin is difficult due to its ubiquitous expression and, so far, has been limited to approaches utilizing RNAi or blocking antibodies and aptamers in breast cancer models. Although delivered without specificity to cell type, these initial treatment studies confirm the antitumoral effect of osteopontin inhibition (114) and call for testing in AML disease models.
Interleukin-1
Due to its pleiotropic effects, IL-1-mediated signaling is recognized as a central hub between inflammation and cancer, including leukemia development and progression (32, 115–119). In AML patients, multiple studies have reported increased levels of IL-1β and IL-1 receptors as well as decreased levels of interleukin-1 receptor antagonist (IL-1RA) in PB and BM (41, 42, 56, 120). In an MLL-AF9-driven leukemic mouse model, chronic exposure to IL-1β accelerated leukemia progression and impaired normal hematopoiesis by modulating stromal niche support. Using both in vitro and in vivo AML models it was shown that depletion or deletion of IL-1RA resulted in reduced expansion of AML progenitor cells and partially restored normal hematopoiesis (121). This was confirmed by targeting IL-1 receptor signaling via inhibition of p38 MAPK, which enabled normal HSPCs to expand in the presence of IL-1β (41). Of note, in vivo AML development was curbed by knockout of IL-1 receptor in the MLL-AF9 mouse model but was increased in FLT3-ITD-driven leukemic mice (122), suggesting different dependencies on IL-1 signaling. Additionally, it was shown that AML HSPCs express high levels of IL-1 receptor accessory protein (IL-1RAP), which contributed to increased IL-1β production, AML cell proliferation and survival, but reduced normal hematopoiesis. This phenotype was further promoted when co-culturing AML CD34+ HSPCs on MSCs (123, 124). Inhibition of IL-1RAP signaling antagonized this effect and enabled HSC proliferation in the presence of AML cell-conditioned media (124). In line with these AML cell-supporting functions, gene expression analysis revealed reduced overall survival (OS) of AML patients who expressed high levels of IL-1RAP (123). These observations suggest an important role for the IL-1β signaling pathway in the pathogenesis of AML and encourage studies to evaluate the therapeutic effects of targeting IL-1 signaling (117, 120). Multiple US Food and Drug Administration (FDA)-approved IL-1 blockers [Anakinra (Kineret); Rilonacept (Arcalyst); Canakinumab (Ilaris)] are already available. In particular, the effect of Canakinumab is being intensely evaluated in the CANTOS trail (NCT01327846), a randomized, double-blind, placebo-controlled phase 3 study involving 10,061 patients with solid tumors as well as hematological malignancies like chronic myelomonocytic leukemia (CMML) and myelodysplastic syndrome (MDS) (125, 126). However, additional studies will be required to fully understand the therapeutic value of targeting IL-1 and in particular IL-1β in hematological malignancies, including AML.
Interleukin-6
IL-6 is a potent pro-inflammatory cytokine which is crucial for a rapid and coordinated immune response during infections and tissue injuries, but also helps to maintain the hematopoietic system (127–129). Deregulated expression of IL-6 is associated with inflammatory and autoimmune diseases as well as skewed hematopoiesis and leukemia (104, 127, 130). In AML patients with reduced OS, blood and BM serum levels of IL-6 are increased (39, 53, 131). Further studies confirm these findings and suggest that IL-6 levels correlate with poor prognosis, rapid disease progression, and resistance to chemotherapy (39, 132–134). The combined assessment of PB IL-6 and FLT3-ligand levels during AML induction therapy revealed that patients with persistent high IL‐6 levels display lower survival rates compared to patients with decreasing IL-6 and increasing FLT3-ligand levels (134). Similarly, low IL-6 levels accompanied by high IL-10 levels have been linked to better prognosis (39). Although AML blasts are clearly exposed to microenvironment-derived (135–137) and self-produced IL-6 (104), it is disputed how IL-6 contributes to AML progression. Curiously, all AML samples express the IL-6 receptor but only a subset responds to IL-6 treatment in vitro (48, 67, 69, 70, 131, 138). However, multiple studies suggest that IL-6-induced STAT3 signaling promotes AML by inducing chemoresistance (132, 135, 139). Hou and colleagues showed that BM MSCs promote chemoresistance against daunorubicin and cytosine arabinoside (Ara-c) by increasing IL-6 secretion and activation of STAT3 signaling and the oxidative phosphorylation metabolic pathway in AML cells (135). Zhang et al. showed that IL-6-induced STAT3 signaling promotes CD36 expression, CD36-mediated uptake of fatty acids, and chemoresistance against Ara-c (139). Several IL-6 or IL-6 receptor-blocking antibodies have demonstrated promising results in (pre-) clinical studies for the treatment of cancers, chronic inflammation, and autoimmune diseases (130). While Siltuximab (CNTO 328; IL-6-blocking antibody) has been proposed as a treatment option for myelodysplastic syndrome (MDS) and multiple myeloma and is FDA-approved for the treatment of idiopathic multicentric Castleman’s disease (140), Siltuximab in the AML setting has so far only been investigated in an AML xenograft mouse model that mimics end-stage BM failure. In that study, Siltuximab treatment antagonized AML-induced anemia and BM failure and prolonged mouse OS (141).
Interleukin-8
IL-8 (CXCL8) belongs to the CXC family of chemokines and is best known for its role as a chemoattractant for neutrophils (142). While production of IL-8 can be induced by various stimuli, including lipopolysaccharide, IL-1, and TNF in healthy cells, many tumor cells express IL-8 constitutively (142) or in a hypoxia-, acidosis-, or chemotherapy-induced manner, leading to anti-apoptotic and growth-supporting MAPK, PI3K, FAK and SRC18 signaling (143). In AML, constitutive production of IL-8 has been observed in both AML cell lines and primary AML samples, together with expression of functional IL-8 receptors [IL-8RA (CXCR1) and IL-8RB (CXCR2)] (144–146). Interestingly, AML cell-derived IL-8 also signals in a paracrine manner and affects neighboring non-leukemic cells in the BM microenvironment. Hypoxia-induced IL-8 secretion by AML cells resulted in increased migration of MSCs into the leukemic BM niche (147). MSCs, in turn, prevent apoptosis and confer drug resistance on leukemic cells by up-regulation of anti-apoptotic proteins and secretion of growth factors, cytokines, and extracellular vesicles (148, 149). Importantly, it has been shown that IL-8 production and secretion by MSCs, fibroblasts, and endothelial cells is induced or increased upon their co-culture with AML cells, thereby contributing to reduced apoptosis and increased proliferation and chemoresistance of the AML cells (150–152). In patients, this bidirectional signaling seems to result in elevated IL-8 levels in PB and BM levels (72), which additionally might contribute to impaired neutrophil migration and hematopoiesis (153). However, further confirmation, especially in the context of AML, is required. Inhibition of the IL-8–IL-8R axis has been proposed as a novel therapeutic intervention targeting the aberrant leukemic BM microenvironment. Blocking the IL-8 pathway with neutralizing antibodies has been shown to restore the sensitivity of malignant cells to chemotherapeutics and reduce AML cell proliferation (150, 151). Using knockdown or pharmacological inhibition approaches, Schinke and colleagues showed that inhibition of IL-8RB-mediated signaling leads to a significant reduction in proliferation and G0/G1 cell cycle arrest in several leukemic cell lines and primary MDS/AML samples (119).
CXC motif chemokine 12
The chemotactic cytokine (chemokine) CXCL12, also referred to as SDF-1, is secreted by a variety of cells including stromal cells, fibroblasts, and epithelial cells (154). CXCL12 initiates signaling by binding to its receptors CXCR4 and CXCR7 and plays a crucial role in regulating hematopoiesis (proliferation, differentiation, survival) and hematopoietic cell trafficking to and within the BM (95, 155), but also contributes to tumor growth, survival, metastasis, vascularization, and chemoresistance of several types of cancer (95, 156–160). In AML, low expression of CXCL12, high expression of CXCR4 and low to intermediate expression of CXCR7 have been measured on AML blasts in comparison to normal HSPCs (92–94). Interestingly, decreased CXCL12 and increased CXCR4 expression by AML blasts was associated with reduced patient relapse-free and overall survival OS (161–164). Within the healthy BM, CXCL12 is mainly secreted by perivascular stromal cells [mesenchymal stem and CXCL12-abundant reticular (CAR) cells], endothelial cells, and osteoblasts, thereby guiding, retaining, and regulating HSPCs to and within supportive BM niches (16). Within the AML BM microenvironment, it has not yet been determined which and to what extent cell populations produce and secrete CXCL12. In vitro, CXCL12 was shown to promote AML cell growth, survival, and chemoresistance (95–98) by activating or inducing the pro-survival proteins PI3K/AKT, MAP3K/ERK1/2, MYC, Bcl-2, and Bcl-XL (93, 96, 165). In vivo, however, while the deletion of CXCR4 in AML MLL-AF9+ HSPCs prolonged leukemic mouse survival, deletion of CXCL12 within the AML microenvironment did not alter the development and progression of the disease (166). This surprising finding suggests that CXCR4 signaling can support AML cells in a CXCL12-independent manner. Nevertheless, blocking the CXCL12/CXCR4 axis represents an attractive therapeutic strategy and several CXCR4 and CXCL12 inhibitors have been developed and used in preclinical and clinical models to induce the mobilization of the AML cells from the BM into the circulation with the aim of increasing their exposure to chemotherapeutic agents (95, 167). Plerixaflor (NCT01319864, NCT01352650, NCT01027923), LY2510924 (NCT02652871), and PF-06747143 (NCT02954653) are among the antagonists that have been under Phase 1 clinical trials to test for safety, tolerability and clinical activity, either alone or in combination with standard chemotherapy in AML patients.
AML inhibiting cytokines
Interferon-γ
Interferon-γ (IFN-γ) is one of the lead cytokines of cellular immunity. It is mainly secreted by activated lymphocytes (168) and orchestrates tumor defense by regulating AML blast survival and apoptosis (118). While T cells obtained from AML patients at primary diagnosis exhibit increased IFN-γ production, strongly reduced levels of IFN-γ were observed in CD8+ T cells from patients who developed relapsed AML after allogeneic HCT (allo-HCT), whereas patients without relapse did not show reduced IFN-γ production (169). This suggests that lower IFN-γ levels may elevate the risk of relapse. An early phase 1 trial was recently started to evaluate the potential of IFN-γ treatment in AML patients with reoccurring disease after allo-HCT (NCT04628338). However, manipulation of IFN-γ levels in AML patients should be carefully assessed, because systemic administration of IFN-γ is limited by rapid IFN-γ clearance and insufficient distribution to tumor sites. Moreover, while IFN-γ can restore T cell-mediated anti-cancer immunity and the surface expression of HLA class II molecules, the loss of which has been shown to impair AML recognition by donor T cells (170), IFN-γ is also capable of promoting PD-L1 and PD-L2 expression in AML (171, 172). Indeed, high expression of PD-L1 and PD-L2 is associated with poor OS in AML patients (173, 174). Binding of PD-L1/PD-L2 to the receptor PD-1 increases T cell exhaustion, promotes effector T cell apoptosis, induces the resistance to effector T cell-mediated killing (175) and increases the conversion and development of Tregs which have strong immune-suppressive abilities (176). Thus, the potential induction of PD-L1 and PD-L2 by IFN-γ may have unfavorable consequences, because the PD-1/PD-L1/PD-L2 axis helps the tumor to maintain an immunosuppressive microenvironment, thereby promoting immune evasion and survival of cancer cells (177). In addition to T cells, innate lymphoid cells type I (ILC1s) are another potent source of IFN-γ in healthy individuals. ILCs are important players of innate immune responses by reacting promptly to signals, or inducer cytokines, expressed by tissue-resident cells. ILC1s function as a first line of defense against intracellular pathogens, such as viruses, and tumors (178). By secreting IFN-γ, healthy ILC1s induce apoptosis and block differentiation by modulating JAK-STAT or PI3K/AKT signaling. However, in AML, ILC1s exhibit reduced IFN-γ secretion and lose their ability to suppress the development of LSCs and antagonize AML progression (179). ILC1s thus seem pivotal as an anti-cancer immune cell, and administration of ex vivo-expanded ILC1s could provide a new immunotherapeutic approach to ensure that IFN-y levels are locally increased within leukemic niches. Importantly, this approach would significantly decrease toxicity for AML patients in comparison to systemic delivery of IFN-y (179).
Interleukin-4
IL-4 is a signature cytokine of type II inflammation and regulates many aspects of Th2-mediated immunity (180). In epithelial cancers, IL-4 is generally considered to have pro-tumorigenic and pro-metastatic functions, suggesting that inhibition of the IL-4/IL-4R axis may be beneficial to limiting diseases (181, 182). Yet, in hematological cancers, a tumor-promoting role of IL-4 is controversial. Already in the early 1990s there were studies reporting that IL-4 might also have tumor-limiting functions, by suppressing IL-1-induced proliferation of AML cells (60, 64, 65). More recent findings substantiate those earlier observations and show that IL-4 has the potential to inhibit survival of AML cell lines as well as patient-derived AML cells, irrespective of their cytogenetic status and French-American-British (FAB) subtype, without affecting normal HSPCs. Anti-leukemic effects of IL-4 are at least partially dependent on STAT6 and Caspase-3, which agrees with the crucial role of STAT6 in mediating IL-4’s effects downstream of the IL-4 receptor (183). In addition, IL-4-induced STAT6, in cooperation with the nuclear receptor protein proliferator-activated receptor gamma (PPARγ), upregulates the expression of prostaglandins. In particular, COX (cyclooxygenase)-dependent prostaglandins, so-called CyPGs, play an important role in apoptosis (184). After stimulation by IL-4, these lipid mediators are increasingly produced via the COX/prostaglandin axis, which leads to activation of p53 and caspase-3 and subsequently stimulates apoptosis of leukemic cells (185). The fact that IL-4 treatment specifically acts on AML blasts, but does not affect HSCs, even upon long-term treatment, makes IL-4 an interesting candidate for therapeutic intervention in AML. Yet, despite its promising role as an anti-leukemic cytokine, IL-4 additionally promotes the differentiation of immune cells, including M2 macrophages, which are regarded as having a leukemia-supporting phenotype. M2 macrophages release various cytokines and growth factors that promote blast survival and proliferation, induce proangiogenic effects and can directly inhibit CD8+ T cell-mediated killing of blast cells (186, 187). Therefore, more detailed studies are required to assess the value of IL-4 as an antileukemic molecule.
Interleukin-10
IL-10, an anti-inflammatory cytokine produced by several immune cells, is crucial for limiting immune responses and damage caused by long-lasting inflammation (188). In AML patients, significantly higher levels of plasma IL-10 are observed (53, 56, 73) which directly correlate with prolonged overall patient survival, event-free survival and higher complete remission rates (39, 189, 190). In vitro, IL-10 treatment of AML blasts inhibited spontaneous AML blast proliferation and colony formation by negatively affecting the production and secretion of pro-leukemic cytokines (IL-1α, IL-1β, TNF-α, GM-CSF, GM-CSF, and IL-6) (74–76, 191). However, contrary to these findings, there is also evidence that IL-10 together with IL-35 — the latter a CD4+ and CD8+ T cell-suppressing and T regulatory cell (Treg)-supporting cytokine upregulated in AML (118) — promotes AML cell proliferation, survival and chemoresistance. So far, ICOS1+ and PD1+ Treg cells as well as BM-MSCs have been suggested as a source for IL-10 in the AML microenvironment (176, 192), contributing to the establishment of an IL-10-induced immunosuppressive and anti-inflammatory niche which ensures LSC survival and stemness (193, 194). Therefore, despite the direct correlation between IL-10 serum level and prolonged patient survival and treatment response (39, 189), antagonizing IL-10 signaling could support current chemotherapeutic approaches to irradicate LSCs and decrease the patient relapse rate (195). However, so far, no combinatory studies have been performed. Interestingly, Chen et al. recently highlighted the IL-10 receptor as a potential candidate for AML immunotherapy as it is significantly upregulated on AML cells in patients and is required for LSC stemness. CAR-T cells harboring an IL-10 peptide structure within their antigen-binding domain were shown to recognize and bind to the IL-10 receptor of multiple AML cell lines (MV4-11, Kasumi-1, U937, THP-1 and MOLM-13) and primary AML cells, thereby inducing the CAR T-cell mediated killing of these cells in vitro and in vivo (196). Although the function of IL-10 may be patient-dependent, immunomodulatory agents that block IL-10 could offer an interesting approach for treatment of AML.
Interleukin-12p70: a new trick for an old cytokine
More than a decade ago, IL-12p70 was shown to inhibit the angiogenic potential but not the survival or proliferation of AML cells (77) and to increase T-cell proliferation and cytotoxicity against leukemic cells in vitro (78, 79). Multiple in vitro co-culture studies overexpressing IL-12p70 in dendritic cells have confirmed these findings (197, 198) and paved the way for initial immunotherapies using genetically modified dendritic cells (phase 1 clinical trial NCT01734304) (199), thereby trying to avoid the toxicity of systemic administration of IL-12. Recently, another elegant therapeutic approach based on transplantation of genetically modified AML blasts constitutively expressing IL-12 in a vaccine-like manner was successfully established in murine and human cells (197) and is currently under investigation in a phase 1 clinical trial (NCT02483312).
Conclusion and future perspectives
Despite intensive research leading to new and targeted therapeutic strategies for AML in recent years, the prognosis for a large proportion of patients remains poor. Due to the highly heterogeneous nature of AML, current therapies often only eliminate specific subclones but cannot permanently halt disease progression. As in many other cancers, chronic inflammation, characterized by the release of pro-inflammatory cytokines and growth factors, which significantly influence the interaction of tumor and immune cells in the tumor microenvironment, can also be observed in AML. On the one hand these cytokines may ensure survival of cancer cells by promoting tumor cell proliferation while inhibiting the antitumor immune responses; on the other hand, some cytokines contribute to cancer cell elimination by supporting the body’s own immunological defense mechanisms. Therapeutic application of cytokines, or therapies that specifically target cytokines and/or their receptors, may provide new avenues for the treatment of AML patients in the coming years. In particular, IL-1β, IL-6 and CXCL12 might be promising new druggable targets. However, due to the pleiotropic effects of most cytokines, which control both tumor growth and anti-tumor immune responses, we are faced with the challenge of establishing new therapies, which on the one hand inhibit tumor growth and at the same time specifically enhance the anti-tumor response. The use of combination therapies, in which potential inhibitors of inflammatory cytokines are combined with other therapeutic molecules and agents, may prove promising for this purpose.
Author contributions
Conceptualization, JH-H, ML, PWK, writing—original draft preparation, ML and PWK, writing—review and editing, JH-H, visualization, ML and funding acquisition, JH-H. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the County of Salzburg, Cancer Cluster Salzburg [grant number 20102-P1601064-FPR01-2017], the Austrian Science Fund (FWF) [grant numbers W1213 and P33969], the Biomed Center Salzburg (project 20102-F1901165-KZP), the European Interreg project EPIC (grant number ITAT1054), and by the Priority program ACBN, University of Salzburg.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Dohner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med (2015) 373(12):1136–52. doi: 10.1056/NEJMra1406184 [DOI] [PubMed] [Google Scholar]
- 2. Estey E, Döhner H. Acute myeloid leukaemia. Lancet (London England) (2006) 368(9550):1894–907. doi: 10.1016/S0140-6736(06)69780-8 [DOI] [PubMed] [Google Scholar]
- 3. Pelcovits A, Niroula R. Acute myeloid leukemia: A review. Rhode Island Med J (2013) (2020) 103(3):38–40. [PubMed] [Google Scholar]
- 4. Papayannidis C, Sartor C, Marconi G, Fontana MC, Nanni J, Cristiano G, et al. Acute myeloid leukemia mutations: Therapeutic implications. Int J Mol Sci (2019) 20(11):2721. doi: 10.3390/ijms20112721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Noone AM HN, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. eds. SEER cancer statistics review, 1975-2015. Bethesda, MD: National Cancer Institute; (2018). Available at: https://seer.cancer.gov/csr/1975_2015/. [Google Scholar]
- 6. Prada-Arismendy J, Arroyave JC, Rothlisberger S. Molecular biomarkers in acute myeloid leukemia. Blood Rev (2017) 31(1):63–76. doi: 10.1016/j.blre.2016.08.005 [DOI] [PubMed] [Google Scholar]
- 7. De Kouchkovsky I, Abdul-Hay M. Acute myeloid leukemia: a comprehensive review and 2016 update Blood Cancer J (2016) 6(7):e441. doi: 10.1038/bcj.2016.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Narayanan D, Weinberg OK. How I investigate acute myeloid leukemia. Int J Lab Hematol (2020) 42(1):3–15. doi: 10.1111/ijlh.13135 [DOI] [PubMed] [Google Scholar]
- 9. Krause DS, Scadden DT. A hostel for the hostile: the bone marrow niche in hematologic neoplasms Haematologica. (2015) 100(11):1376–87. doi: 10.3324/haematol.2014.113852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lane SW, Scadden DT, Gilliland DG. The leukemic stem cell niche: current concepts and therapeutic opportunities. Blood (2009) 114(6):1150–7. doi: 10.1182/blood-2009-01-202606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schepers K, Campbell TB, Passegué E. Normal and leukemic stem cell niches: insights and therapeutic opportunities. Cell Stem Cell (2015) 16(3):254–67. doi: 10.1016/j.stem.2015.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bhatia R, McGlave PB, Dewald GW, Blazar BR, Verfaillie CM. Abnormal function of the bone marrow microenvironment in chronic myelogenous leukemia: role of malignant stromal macrophages. Blood (1995) 85(12):3636–45. doi: 10.1182/blood.V85.12.3636.bloodjournal85123636 [DOI] [PubMed] [Google Scholar]
- 13. Somervaille TC, Cleary ML. Identification and characterization of leukemia stem cells in murine MLL-AF9 acute myeloid leukemia. Cancer Cell (2006) 10(4):257–68. doi: 10.1016/j.ccr.2006.08.020 [DOI] [PubMed] [Google Scholar]
- 14. Reynaud D, Pietras E, Barry-Holson K, Mir A, Binnewies M, Jeanne M, et al. IL-6 controls leukemic multipotent progenitor cell fate and contributes to chronic myelogenous leukemia development. Cancer Cell (2011) 20(5):661–73. doi: 10.1016/j.ccr.2011.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schemionek M, Spieker T, Kerstiens L, Elling C, Essers M, Trumpp A, et al. Leukemic spleen cells are more potent than bone marrow-derived cells in a transgenic mouse model of CML. Leukemia (2012) 26(5):1030–7. doi: 10.1038/leu.2011.366 [DOI] [PubMed] [Google Scholar]
- 16. Krenn PW, Montanez E, Costell M, Fässler R. Integrins, anchors and signal transducers of hematopoietic stem cells during development and in adulthood. Curr Top Dev Biol (2022) 149:203–61. doi: 10.1016/bs.ctdb.2022.02.009 [DOI] [PubMed] [Google Scholar]
- 17. Boettcher S, Manz MG. Regulation of inflammation- and infection-driven hematopoiesis. Trends Immunol (2017) 38(5):345–57. doi: 10.1016/j.it.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 18. Pietras EM, Mirantes-Barbeito C, Fong S, Loeffler D, Kovtonyuk LV, Zhang S, et al. Chronic interleukin-1 exposure drives haematopoietic stem cells towards precocious myeloid differentiation at the expense of self-renewal. Nat Cell Biol (2016) 18(6):607–18. doi: 10.1038/ncb3346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weber GF, Chousterman BG, He S, Fenn AM, Nairz M, Anzai A, et al. Interleukin-3 amplifies acute inflammation and is a potential therapeutic target in sepsis. Science (2015) 347(6227):1260–5. doi: 10.1126/science.aaa4268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ihle JN. Interleukin-3 and hematopoiesis. Chem Immunol (1992) 51:65–106. doi: 10.1159/000420755 [DOI] [PubMed] [Google Scholar]
- 21. Ishihara K, Hirano T. IL-6 in autoimmune disease and chronic inflammatory proliferative disease. Cytokine Growth Factor Rev (2002) 13(4-5):357–68. doi: 10.1016/S1359-6101(02)00027-8 [DOI] [PubMed] [Google Scholar]
- 22. Reynaud D, Pietras E, Barry-Holson K, Mir A, Binnewies M, Jeanne M, et al. IL-6 controls leukemic multipotent progenitor cell fate and contributes to chronic myelogenous leukemia development. Cancer Cell (2011) 20(5):661–73. doi: 10.1016/j.ccr.2011.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maeda K, Baba Y, Nagai Y, Miyazaki K, Malykhin A, Nakamura K, et al. IL-6 blocks a discrete early step in lymphopoiesis. Blood (2005) 106(3):879–85. doi: 10.1182/blood-2005-02-0456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tian T, Wang M, Ma D. TNF-alpha, a good or bad factor in hematological diseases? Stem Cell Investig (2014) 1:12. doi: 10.3978/j.issn.2306-9759.2014.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Selleri C, Maciejewski JP, Sato T, Young NS. Interferon-gamma constitutively expressed in the stromal microenvironment of human marrow cultures mediates potent hematopoietic inhibition. Blood. (1996) 87(10):4149–57. doi: 10.1182/blood.V87.10.4149.bloodjournal87104149 [DOI] [PubMed] [Google Scholar]
- 26. Jacobsen SE, Ruscetti FW, Dubois CM, Keller JR. Tumor necrosis factor alpha directly and indirectly regulates hematopoietic progenitor cell proliferation: role of colony-stimulating factor receptor modulation. J Exp Med (1992) 175(6):1759–72. doi: 10.1084/jem.175.6.1759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rezzoug F, Huang Y, Tanner MK, Wysoczynski M, Schanie CL, Chilton PM, et al. TNF-alpha is critical to facilitate hemopoietic stem cell engraftment and function. J Immunol (2008) 180(1):49–57. doi: 10.4049/jimmunol.180.1.49 [DOI] [PubMed] [Google Scholar]
- 28. Baldridge MT, King KY, Boles NC, Weksberg DC, Goodell MA. Quiescent haematopoietic stem cells are activated by IFN-gamma in response to chronic infection. Nature (2010) 465(7299):793–7. doi: 10.1038/nature09135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Essers MA, Offner S, Blanco-Bose WE, Waibler Z, Kalinke U, Duchosal MA, et al. IFNalpha activates dormant haematopoietic stem cells in vivo . Nature (2009) 458(7240):904–8. doi: 10.1038/nature07815 [DOI] [PubMed] [Google Scholar]
- 30. Ushach I, Zlotnik A. Biological role of granulocyte macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor (M-CSF) on cells of the myeloid lineage. J Leukoc Biol (2016) 100(3):481–9. doi: 10.1189/jlb.3RU0316-144R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mirantes C, Passegue E, Pietras EM. Pro-inflammatory cytokines: emerging players regulating HSC function in normal and diseased hematopoiesis. Exp Cell Res (2014) 329(2):248–54. doi: 10.1016/j.yexcr.2014.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hemmati S, Haque T, Gritsman K. Inflammatory signaling pathways in preleukemic and leukemic stem cells. Front Oncol (2017) 7:265. doi: 10.3389/fonc.2017.00265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. King KY, Goodell MA. Inflammatory modulation of HSCs: viewing the HSC as a foundation for the immune response. Nat Rev Immunol (2011) 11(10):685–92. doi: 10.1038/nri3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Camacho V, McClearn V, Patel S, Welner RS. Regulation of normal and leukemic stem cells through cytokine signaling and the microenvironment. Int J Hematol (2017) 105(5):566–77. doi: 10.1007/s12185-017-2184-6 [DOI] [PubMed] [Google Scholar]
- 35. Vilchis-Ordoñez A, Contreras-Quiroz A, Vadillo E, Dorantes-Acosta E, Reyes-López A, Quintela-Nuñez del Prado HM, et al. Bone marrow cells in acute lymphoblastic leukemia create a proinflammatory microenvironment influencing normal hematopoietic differentiation fates. BioMed Res Int (2015) 2015:386165. doi: 10.1155/2015/386165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hoermann G, Greiner G, Valent P. Cytokine regulation of microenvironmental cells in myeloproliferative neoplasms. Mediators Inflamm (2015) 2015:869242. doi: 10.1155/2015/869242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kiss C, Benko I, Kovács P. Leukemic cells and the cytokine patchwork. Pediatr Blood Cancer (2004) 42(2):113–21. doi: 10.1002/pbc.10436 [DOI] [PubMed] [Google Scholar]
- 38. Pietras EM. Inflammation: a key regulator of hematopoietic stem cell fate in health and disease. Blood (2017) 130(15):1693–8. doi: 10.1182/blood-2017-06-780882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sanchez-Correa B, Bergua JM, Campos C, Gayoso I, Arcos MJ, Banas H, et al. Cytokine profiles in acute myeloid leukemia patients at diagnosis: survival is inversely correlated with IL-6 and directly correlated with IL-10 levels. Cytokine (2013) 61(3):885–91. doi: 10.1016/j.cyto.2012.12.023 [DOI] [PubMed] [Google Scholar]
- 40. Ahmed HA, Maklad AM, Khaled SA, Elyamany A. Interleukin-27 and interleukin-35 in de novo acute myeloid leukemia: expression and significance as biological markers. J Blood Med (2019) 10:341–9. doi: 10.2147/JBM.S221301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Carey A, DKt E, CA E, Newell L, Traer E, BC M, et al. Identification of interleukin-1 by functional screening as a key mediator of cellular expansion and disease progression in acute myeloid leukemia. Cell Rep (2017) 18(13):3204–18. doi: 10.1016/j.celrep.2017.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tao M, Li B, Nayini J, Andrews CB, Huang RW, Devemy E, et al. SCF, IL-1beta, IL-1ra and GM-CSF in the bone marrow and serum of normal individuals and of AML and CML patients. Cytokine (2000) 12(6):699–707. doi: 10.1006/cyto.2000.0666 [DOI] [PubMed] [Google Scholar]
- 43. Elbaz O, Shaltout A. Implication of granulocyte-macrophage colony stimulating factor (GM-CSF) and interleukin-3 (IL-3) in children with acute myeloid leukaemia (AML); malignancy. Hematology (2001) 5(5):383–8. [PubMed] [Google Scholar]
- 44. Islam M, Mohamed EH, Esa E, Kamaluddin NR, Zain SM, Yusoff YM, et al. Circulating cytokines and small molecules follow distinct expression patterns in acute myeloid leukaemia. Br J Cancer (2017) 117(10):1551–6. doi: 10.1038/bjc.2017.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Carlo-Stella C, Mangoni L, Almici C, Frassoni F, Fiers W, Rizzoli V. Growth of CD34+ acute myeloblastic leukemia colony-forming cells in response to recombinant hematopoietic growth factors. Leukemia (1990) 4(8):561–6. [PubMed] [Google Scholar]
- 46. Delwel R, Salem M, Pellens C, Dorssers L, Wagemaker G, Clark S, et al. Growth regulation of human acute myeloid leukemia: effects of five recombinant hematopoietic factors in a serum-free culture system. Blood (1988) 72(6):1944–9. doi: 10.1182/blood.V72.6.1944.1944 [DOI] [PubMed] [Google Scholar]
- 47. Pebusque MJ, Fay C, Lafage M, Sempere C, Saeland S, Caux C, et al. Recombinant human IL-3 and G-CSF act synergistically in stimulating the growth of acute myeloid leukemia cells. Leukemia (1989) 3(3):200–5. [PubMed] [Google Scholar]
- 48. Suzuki T, Morio T, Tohda S, Nagata K, Yamashita Y, Imai Y, et al. Effects of interleukin-6 and granulocyte colony-stimulating factor on the proliferation of leukemic blast progenitors from acute myeloblastic leukemia patients. Jpn J Cancer Res (1990) 81(10):979–86. doi: 10.1111/j.1349-7006.1990.tb03335.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kassem NM, Ayad AM, El Husseiny NM, El-Demerdash DM, Kassem HA, Mattar MM. Role of granulocyte-macrophage colony-stimulating factor in acute myeloid Leukemia/Myelodysplastic syndromes. J Glob Oncol (2018) 4:1–6. doi: 10.1200/JGO.2017.009332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hoang T, Haman A, Goncalves O, Letendre F, Mathieu M, Wong GG, et al. Interleukin 1 enhances growth factor-dependent proliferation of the clonogenic cells in acute myeloblastic leukemia and of normal human primitive hemopoietic precursors. J Exp Med (1988) 168(2):463–74. doi: 10.1084/jem.168.2.463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carter A, Silvian-Draxler I, Tatarsky I. Effect of interleukin-1, tumor necrosis factor-alpha, and interferon-alpha on the blast cells of acute myeloblastic leukemia. Am J Hematol (1992) 40(4):245–51. doi: 10.1002/ajh.2830400402 [DOI] [PubMed] [Google Scholar]
- 52. Sissolak G, Hoffbrand AV, Mehta AB, Ganeshaguru K. Effects of interferon-alpha (IFN) on the expression of interleukin 1-beta (IL-1), interleukin 6 (IL-6), granulocyte-macrophage colony-stimulating factor (GM-CSF) and tumor necrosis factor-alpha (TNF) in acute myeloid leukemia (AML) blasts. Leukemia. (1992) 6(11):1155–60. [PubMed] [Google Scholar]
- 53. Sun YX, Kong HL, Liu CF, Yu S, Tian T, Ma DX, et al. The imbalanced profile and clinical significance of T helper associated cytokines in bone marrow microenvironment of the patients with acute myeloid leukemia. Hum Immunol (2014) 75(2):113–8. doi: 10.1016/j.humimm.2013.11.014 [DOI] [PubMed] [Google Scholar]
- 54. Corradi G, Bassani B, Simonetti G, Sangaletti S, Vadakekolathu J, Fontana MC, et al. Release of IFN-γ by acute myeloid leukemia cells remodels bone marrow immune microenvironment by inducing regulatory T cells. Clin Cancer Res (2022) 28(14):3141–55. doi: 10.1158/1078-0432.CCR-21-3594 [DOI] [PubMed] [Google Scholar]
- 55. Ersvaer E, Skavland J, Ulvestad E, Gjertsen BT, Bruserud Ø. Effects of interferon gamma on native human acute myelogenous leukaemia cells. Cancer Immunol Immunother. (2007) 56(1):13–24. doi: 10.1007/s00262-006-0159-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Tsimberidou AM, Estey E, Wen S, Pierce S, Kantarjian H, Albitar M, et al. The prognostic significance of cytokine levels in newly diagnosed acute myeloid leukemia and high-risk myelodysplastic syndromes. Cancer. (2008) 113(7):1605–13. doi: 10.1002/cncr.23785 [DOI] [PubMed] [Google Scholar]
- 57. Yin M, Gopal V, Banavali S, Gartside P, Preisler H. Effects of an IL-1 receptor antagonist on acute myeloid leukemia cells. Leukemia (1992) 6(9):898–901. [PubMed] [Google Scholar]
- 58. Estrov Z, Kurzrock R, Estey E, Wetzler M, Ferrajoli A, Harris D, et al. Inhibition of acute myelogenous leukemia blast proliferation by interleukin-1 (IL-1) receptor antagonist and soluble IL-1 receptors. Blood (1992) 79(8):1938–45. doi: 10.1182/blood.V79.8.1938.1938 [DOI] [PubMed] [Google Scholar]
- 59. Cozzolino F, Rubartelli A, Aldinucci D, Sitia R, Torcia M, Shaw A, et al. Interleukin 1 as an autocrine growth factor for acute myeloid leukemia cells. Proc Natl Acad Sci USA. (1989) 86(7):2369–73. doi: 10.1073/pnas.86.7.2369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wagteveld AJ, Esselink MT, Limburg P, Halie MR, Vellenga E. The effects of IL-1 beta and IL-4 on the proliferation and endogenous secretion of growth factors by acute myeloblastic leukemic cells. Leukemia (1992) 6(10):1020–4. [PubMed] [Google Scholar]
- 61. Delwel R, Dorssers L, Touw I, Wagemaker G, Lowenberg B. Human recombinant multilineage colony stimulating factor (interleukin-3): stimulator of acute myelocytic leukemia progenitor cells in vitro . Blood (1987) 70(1):333–6. doi: 10.1182/blood.V70.1.333.333 [DOI] [PubMed] [Google Scholar]
- 62. Lemoli RM, Gulati SC, Strife A, Lambek C, Perez A, Clarkson BD. Proliferative response of human acute myeloid leukemia cells and normal marrow enriched progenitor cells to human recombinant growth factors IL-3, GM-CSF and G-CSF alone and in combination. Leukemia (1991) 5(5):386–91. [PubMed] [Google Scholar]
- 63. Santoli D, Yang YC, Clark SC, Kreider BL, Caracciolo D, Rovera G. Synergistic and antagonistic effects of recombinant human interleukin (IL) 3, IL-1 alpha, granulocyte and macrophage colony-stimulating factors (G-CSF and m-CSF) on the growth of GM-CSF-dependent leukemic cell lines. J Immunol (1987) 139(10):3348–54. [PubMed] [Google Scholar]
- 64. Tuyt LM, Dokter WH, Esselink MT, Vellenga E. Divergent effects of IL-10 and IL-4 on the proliferation and growth factor secretion by acute myeloblastic leukemic cells. Eur Cytokine Netw (1995) 6(4):231–5. [PubMed] [Google Scholar]
- 65. Akashi K. The role of interleukin-4 in the negative regulation of leukemia cell growth. Leuk Lymphoma (1993) 9(3):205–9. doi: 10.3109/10428199309147371 [DOI] [PubMed] [Google Scholar]
- 66. Negaard HF, Iversen N, Bowitz-Lothe IM, Sandset PM, Steinsvik B, Ostenstad B, et al. Increased bone marrow microvascular density in haematological malignancies is associated with differential regulation of angiogenic factors. Leukemia (2009) 23(1):162–9. doi: 10.1038/leu.2008.255 [DOI] [PubMed] [Google Scholar]
- 67. Sugiyama H, Inoue K, Ogawa H, Yamagami T, Soma T, Miyake S, et al. The expression of IL-6 and its related genes in acute leukemia. Leuk Lymphoma (1996) 21(1-2):49–52. doi: 10.3109/10428199609067579 [DOI] [PubMed] [Google Scholar]
- 68. Hoang T, Haman A, Goncalves O, Wong GG, Clark SC. Interleukin-6 enhances growth factor-dependent proliferation of the blast cells of acute myeloblastic leukemia. Blood (1988) 72(2):823–6. doi: 10.1182/blood.V72.2.823.823 [DOI] [PubMed] [Google Scholar]
- 69. Säily M, Koistinen P, Zheng A, Savolainen ER. Signaling through interleukin-6 receptor supports blast cell proliferation in acute myeloblastic leukemia Eur J Haematol (1998) 61(3):190–6. doi: 10.1111/j.1600-0609.1998.tb01083.x. [DOI] [PubMed] [Google Scholar]
- 70. Lopez M, Maroc N, Kerangueven F, Bardin F, Courcoul M, Lavezzi C, et al. Coexpression of the genes for interleukin 6 and its receptor without apparent involvement in the proliferation of acute myeloid leukemia cells. Exp Hematol (1991) 19(8):797–803. [PubMed] [Google Scholar]
- 71. Suzuki T, Bessho M, Hirashma K, Tohda S, Nagata K, Imai Y, et al. Interleukin-6 reduces the optimal growth in vitro of leukemic blast progenitors from acute myeloblastic leukemia patients. Acta Haematol (1992) 87(1-2):63–8. doi: 10.1159/000204718 [DOI] [PubMed] [Google Scholar]
- 72. Çelik H, Lindblad KE, Popescu B, Gui G, Goswami M, Valdez J, et al. Highly multiplexed proteomic assessment of human bone marrow in acute myeloid leukemia. Blood Adv (2020) 4(2):367–79. doi: 10.1182/bloodadvances.2019001124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Wu H, Li P, Shao N, Ma J, Ji M, Sun X, et al. Aberrant expression of treg-associated cytokine IL-35 along with IL-10 and TGF-β in acute myeloid leukemia. Oncol Lett (2012) 3(5):1119–23. doi: 10.3892/ol.2012.614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Westermann F, Kube D, Haier B, Bohlen H, Engert A, Zuehlsdorf M, et al. Interleukin 10 inhibits cytokine production of human AML cells. Ann Oncol (1996) 7(4):397–404. doi: 10.1093/oxfordjournals.annonc.a010607 [DOI] [PubMed] [Google Scholar]
- 75. Bruserud O, Tore Gjertsen B, Brustugun OT, Bassøe CF, Nesthus I, Espen Akselsen P, et al. Effects of interleukin 10 on blast cells derived from patients with acute myelogenous leukemia. Leukemia (1995) 9(11):1910–20. [PubMed] [Google Scholar]
- 76. Asano Y, Shibata S, Kobayashi S, Okamura S, Niho Y. Interleukin-10 inhibits the autocrine growth of leukemic blast cells from patients with acute myeloblastic leukemia. Int J Hematol (1997) 66(4):445–50. doi: 10.1016/S0925-5710(97)00070-4 [DOI] [PubMed] [Google Scholar]
- 77. Ferretti E, Di Carlo E, Cocco C, Ribatti D, Sorrentino C, Ognio E, et al. Direct inhibition of human acute myeloid leukemia cell growth by IL-12. Immunol Lett (2010) 133(2):99–105. doi: 10.1016/j.imlet.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 78. Orleans-Lindsay JK, Deru A, Craig JI, Prentice HG, Lowdell MW. In vitro co-stimulation with anti-CD28 synergizes with IL-12 in the generation of T cell immune responses to leukaemic cells; a strategy for ex-vivo generation of CTL for immunotherapy. Clin Exp Immunol (2003) 133(3):467–75. doi: 10.1046/j.1365-2249.2003.02235.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Pan L, Ohnishi K, Zhang WJ, Yoshida H, Maksumova L, Muratkhodjaev F, et al. In vitro IL-12 treatment of peripheral blood mononuclear cells from patients with leukemia or myelodysplastic syndromes: increase in cytotoxicity and reduction in WT1 gene expression. Leukemia (2000) 14(9):1634–41. doi: 10.1038/sj.leu.2401872 [DOI] [PubMed] [Google Scholar]
- 80. Tao Q, Pan Y, Wang Y, Wang H, Xiong S, Li Q, et al. Regulatory T cells-derived IL-35 promotes the growth of adult acute myeloid leukemia blasts. Int J Cancer (2015) 137(10):2384–93. doi: 10.1002/ijc.29563 [DOI] [PubMed] [Google Scholar]
- 81. Wang J, Tao Q, Wang H, Wang Z, Wu F, Pan Y, et al. Elevated IL-35 in bone marrow of the patients with acute myeloid leukemia. Hum Immunol (2015) 76(9):681–6. doi: 10.1016/j.humimm.2015.09.020 [DOI] [PubMed] [Google Scholar]
- 82. Liersch R, Gerss J, Schliemann C, Bayer M, Schwöppe C, Biermann C, et al. Osteopontin is a prognostic factor for survival of acute myeloid leukemia patients. Blood (2012) 119(22):5215–20. doi: 10.1182/blood-2011-11-389692 [DOI] [PubMed] [Google Scholar]
- 83. Lee CY, Tien HF, Hou HA, Chou WC, Lin LI. Marrow osteopontin level as a prognostic factor in acute myeloid leukaemia. Br J Haematol (2008) 141(5):736–9. doi: 10.1111/j.1365-2141.2008.07082.x [DOI] [PubMed] [Google Scholar]
- 84. Zhou J, Chen X, Zhou P, Sun X, Chen Y, Li M, et al. Osteopontin is required for the maintenance of leukemia stem cells in acute myeloid leukemia. Biochem Biophys Res Commun (2022) 600:29–34. doi: 10.1016/j.bbrc.2022.02.022 [DOI] [PubMed] [Google Scholar]
- 85. Carlesso N, Pregno P, Bresso P, Gallo E, Pileri A, Zsebo KM, et al. Human recombinant stem cell factor stimulates in vitro proliferation of acute myeloid leukemia cells and expands the clonogenic cell pool. Leukemia (1992) 6(7):642–8. [PubMed] [Google Scholar]
- 86. Hassan HT, Zander A. Stem cell factor as a survival and growth factor in human normal and malignant hematopoiesis. Acta Haematol (1996) 95(3-4):257–62. doi: 10.1159/000203893 [DOI] [PubMed] [Google Scholar]
- 87. Bendall LJ, Makrynikola V, Hutchinson A, Bianchi AC, Bradstock KF, Gottlieb DJ. Stem cell factor enhances the adhesion of AML cells to fibronectin and augments fibronectin-mediated anti-apoptotic and proliferative signals. Leukemia (1998) 12(9):1375–82. doi: 10.1038/sj.leu.2401136 [DOI] [PubMed] [Google Scholar]
- 88. Wu Y, Chen P, Huang HF, Huang MJ, Chen YZ. Reduction of transforming growth factor-β1 expression in leukemia and its possible role in leukemia development. Leuk Lymphoma (2012) 53(1):145–51. doi: 10.3109/10428194.2011.603446 [DOI] [PubMed] [Google Scholar]
- 89. Nara N, Tohda S, Nagata K, Suzuki T, Yamashita Y. Inhibition of the in vitro growth of blast progenitors from acute myeloblastic leukemia patients by transforming growth factor-beta (TGF-beta). Leukemia (1989) 3(8):572–7. [PubMed] [Google Scholar]
- 90. Tessier N, Hoang T. Transforming growth factor beta inhibits the proliferation of the blast cells of acute myeloblastic leukemia. Blood (1988) 72(1):159–64. doi: 10.1182/blood.V72.1.159.159 [DOI] [PubMed] [Google Scholar]
- 91. Zhou X, Zhou S, Li B, Li Q, Gao L, Li D, et al. Transmembrane TNF-α preferentially expressed by leukemia stem cells and blasts is a potent target for antibody therapy. Blood (2015) 126(12):1433–42. doi: 10.1182/blood-2015-01-624833 [DOI] [PubMed] [Google Scholar]
- 92. Sison EA, Magoon D, Li L, Annesley CE, Rau RE, Small D, et al. Plerixafor as a chemosensitizing agent in pediatric acute lymphoblastic leukemia: efficacy and potential mechanisms of resistance to CXCR4 inhibition. Oncotarget (2014) 5(19):8947–58. doi: 10.18632/oncotarget.2407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Yu X, Munoz-Sagredo L, Streule K, Muschong P, Bayer E, Walter RJ, et al. CD44 loss of function sensitizes AML cells to the BCL-2 inhibitor venetoclax by decreasing CXCL12-driven survival cues. Blood (2021) 138(12):1067–80. doi: 10.1182/blood.2020006343 [DOI] [PubMed] [Google Scholar]
- 94. Wang SS, Xu ZJ, Jin Y, Ma JC, Xia PH, Wen X, et al. Clinical and prognostic relevance of CXCL12 expression in acute myeloid leukemia. PeerJ (2021) 9:e11820. doi: 10.7717/peerj.11820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Mehrpouri M. The contributory roles of the CXCL12/CXCR4/CXCR7 axis in normal and malignant hematopoiesis: A possible therapeutic target in hematologic malignancies. Eur J Pharmacol (2022) 920:174831. doi: 10.1016/j.ejphar.2022.174831 [DOI] [PubMed] [Google Scholar]
- 96. Cho BS, Kim HJ, Konopleva M. Targeting the CXCL12/CXCR4 axis in acute myeloid leukemia: from bench to bedside. Korean J Intern Med (2017) 32(2):248–57. doi: 10.3904/kjim.2016.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Peled A, Klein S, Beider K, Burger JA, Abraham M. Role of CXCL12 and CXCR4 in the pathogenesis of hematological malignancies. Cytokine (2018) 109:11–6. doi: 10.1016/j.cyto.2018.02.020 [DOI] [PubMed] [Google Scholar]
- 98. Ladikou EE, Chevassut T, Pepper CJ, Pepper AG. Dissecting the role of the CXCL12/CXCR4 axis in acute myeloid leukaemia. Br J Haematol (2020) 189(5):815–25. doi: 10.1111/bjh.16456 [DOI] [PubMed] [Google Scholar]
- 99. Rodriguez-Cimadevilla JC, Beauchemin V, Villeneuve L, Letendre F, Shaw A, Hoang T. Coordinate secretion of interleukin-1 beta and granulocyte-macrophage colony-stimulating factor by the blast cells of acute myeloblastic leukemia: role of interleukin-1 as an endogenous inducer. Blood (1990) 76(8):1481–9. doi: 10.1182/blood.V76.8.1481.1481 [DOI] [PubMed] [Google Scholar]
- 100. Russell NH. Autocrine growth factors and leukaemic haemopoiesis. Blood Rev (1992) 6(3):149–56. doi: 10.1016/0268-960X(92)90026-M [DOI] [PubMed] [Google Scholar]
- 101. Murohashi I, Tohda S, Suzuki T, Nagata K, Yamashita Y, Nara N. Autocrine growth mechanisms of the progenitors of blast cells in acute myeloblastic leukemia Blood (1989) 74(1):35–41. doi: 10.1182/blood.V74.1.35.35 [DOI] [PubMed] [Google Scholar]
- 102. Delwel R, Schipper P, van Buitenen C, van Agthoven T, Touw I, Löwenberg B. Comparative analysis of IL-1 regulated and spontaneous growth of acute myeloid leukemia in vitro . Bone marrow Transplant (1990) 6 Suppl 1:22–6. [PubMed] [Google Scholar]
- 103. Bradbury D, Rogers S, Reilly IA, Kozlowski R, Russell NH. Role of autocrine and paracrine production of granulocyte-macrophage colony-stimulating factor and interleukin-1 beta in the autonomous growth of acute myeloblastic leukaemia cells–studies using purified CD34-positive cells. Leukemia (1992) 6(6):562–6. [PubMed] [Google Scholar]
- 104. Oster W, Cicco NA, Klein H, Hirano T, Kishimoto T, Lindemann A, et al. Participation of the cytokines interleukin 6, tumor necrosis factor-alpha, and interleukin 1-beta secreted by acute myelogenous leukemia blasts in autocrine and paracrine leukemia growth control. J Clin Invest (1989) 84(2):451–7. doi: 10.1172/JCI114186 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 105. Beauchemin V, Villeneuve L, Rodriguez-Cimadevilla JC, Rajotte D, Kenney JS, Clark SC, et al. Interleukin-6 production by the blast cells of acute myeloblastic leukemia: regulation by endogenous interleukin-1 and biological implications. J Cell Physiol (1991) 148(3):353–61. doi: 10.1002/jcp.1041480305 [DOI] [PubMed] [Google Scholar]
- 106. Delwel R, van Buitenen C, Salem M, Oosterom R, Touw I, Löwenberg B. Hemopoietin-1 activity of interleukin-1 (IL-1) on acute myeloid leukemia colony-forming cells (AML-CFU) in vitro: IL-1 induces production of tumor necrosis factor-alpha which synergizes with IL-3 or granulocyte-macrophage colony-stimulating factor. Leukemia (1990) 4(8):557–60. [PubMed] [Google Scholar]
- 107. Tsuzuki M, Ezaki K, Maruyama F, Ino T, Kojima H, Okamoto M, et al. Proliferative effects of several hematopoietic growth factors on acute myelogenous leukemia cells and correlation with treatment outcome. Leukemia (1997) 11(12):2125–30. doi: 10.1038/sj.leu.2400870 [DOI] [PubMed] [Google Scholar]
- 108. Russell NH, Hunter AE, Bradbury D, Zhu YM, Keith F. Biological features of leukaemic cells associated with autonomous growth and reduced survival in acute myeloblastic leukaemia. Leuk Lymphoma (1995) 16(3-4):223–9. doi: 10.3109/10428199509049761 [DOI] [PubMed] [Google Scholar]
- 109. Lowenberg B, van Putten WL, Touw IP, Delwel R, Santini V. Autonomous proliferation of leukemic cells in vitro as a determinant of prognosis in adult acute myeloid leukemia N Engl J Med (1993) 328(9):614–9. doi: 10.1056/NEJM199303043280904 [DOI] [PubMed] [Google Scholar]
- 110. Pimenta DB, Varela VA, Datoguia TS, Caraciolo VB, Lopes GH, Pereira WO. The bone marrow microenvironment mechanisms in acute myeloid leukemia. Front Cell Dev Biol (2021) 9:764698. doi: 10.3389/fcell.2021.764698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Nilsson SK, Johnston HM, Whitty GA, Williams B, Webb RJ, Denhardt DT, et al. Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood (2005) 106(4):1232–9. doi: 10.1182/blood-2004-11-4422 [DOI] [PubMed] [Google Scholar]
- 112. Battula VL, Le PM, Sun JC, Nguyen K, Yuan B, Zhou X, et al. AML-induced osteogenic differentiation in mesenchymal stromal cells supports leukemia growth. JCI Insight (2017) 2(13):e90036. doi: 10.1172/jci.insight.90036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Zahed Panah M, Nikbakht M, Sajjadi SM, Rostami S, Norooznezhad AH, Kamranzadeh Fumani H, et al. Anti-apoptotic effects of osteopontin via the up-regulation of AKT/mTOR/β-catenin loop in acute myeloid leukemia cells. Int J Hematol Oncol Stem Cell Res (2017) 11(2):148–57. [PMC free article] [PubMed] [Google Scholar]
- 114. Bandopadhyay M, Bulbule A, Butti R, Chakraborty G, Ghorpade P, Ghosh P, et al. Osteopontin as a therapeutic target for cancer. Expert Opin Ther Targets (2014) 18(8):883–95. doi: 10.1517/14728222.2014.925447 [DOI] [PubMed] [Google Scholar]
- 115. Mantovani A, Dinarello CA, Molgora M, Garlanda C. Interleukin-1 and related cytokines in the regulation of inflammation and immunity. Immunity (2019) 50(4):778–95. doi: 10.1016/j.immuni.2019.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Mantovani A, Ponzetta A, Inforzato A, Jaillon S. Innate immunity, inflammation and tumour progression: double-edged swords. J Intern Med (2019) 285(5):524–32. doi: 10.1111/joim.12886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Arranz L, Arriero MDM, Villatoro A. Interleukin-1beta as emerging therapeutic target in hematological malignancies and potentially in their complications. Blood Rev (2017) 31(5):306–17. doi: 10.1016/j.blre.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 118. Binder S, Luciano M, Horejs-Hoeck J. The cytokine network in acute myeloid leukemia (AML): A focus on pro- and anti-inflammatory mediators. Cytokine Growth Factor Rev (2018) 43:8–15. doi: 10.1016/j.cytogfr.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 119. Zhang W, Borcherding N, Kolb R. IL-1 signaling in tumor microenvironment. Adv Exp Med Biol (2020) 1240:1–23. doi: 10.1007/978-3-030-38315-2_1 [DOI] [PubMed] [Google Scholar]
- 120. de Mooij CEM, Netea MG, van der Velden W, Blijlevens NMA. Targeting the interleukin-1 pathway in patients with hematological disorders. Blood (2017) 129(24):3155–64. doi: 10.1182/blood-2016-12-754994 [DOI] [PubMed] [Google Scholar]
- 121. Wang Y, Sun X, Yuan S, Hou S, Guo T, Chu Y, et al. Interleukin-1β inhibits normal hematopoietic expansion and promotes acute myeloid leukemia progression via the bone marrow niche. Cytotherapy (2020) 22(3):127–34. doi: 10.1016/j.jcyt.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 122. Höckendorf U, Yabal M, Herold T, Munkhbaatar E, Rott S, Jilg S, et al. RIPK3 restricts myeloid leukemogenesis by promoting cell death and differentiation of leukemia initiating cells. Cancer Cell (2016) 30(1):75–91. doi: 10.1016/j.ccell.2016.06.002 [DOI] [PubMed] [Google Scholar]
- 123. Barreyro L, Will B, Bartholdy B, Zhou L, Todorova TI, Stanley RF, et al. Overexpression of IL-1 receptor accessory protein in stem and progenitor cells and outcome correlation in AML and MDS. Blood (2012) 120(6):1290–8. doi: 10.1182/blood-2012-01-404699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. De Boer B, Sheveleva S, Apelt K, Vellenga E, Mulder AB, Huls G, et al. The IL1-IL1RAP axis plays an important role in the inflammatory leukemic niche that favors acute myeloid leukemia proliferation over normal hematopoiesis. Haematologica (2020) 106(12):3067–78. doi: 10.3324/haematol.2020.254987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Svensson EC, Madar A, Campbell CD, He Y, Sultan M, Healey ML, et al. TET2-driven clonal hematopoiesis and response to canakinumab: An exploratory analysis of the CANTOS randomized clinical trial. JAMA Cardiol (2022) 7(5):521–8. doi: 10.1001/jamacardio.2022.0386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Wong CC, Baum J, Silvestro A, Beste MT, Bharani-Dharan B, Xu S, et al. Inhibition of IL1β by canakinumab may be effective against diverse molecular subtypes of lung cancer: An exploratory analysis of the CANTOS trial. Cancer Res (2020) 80(24):5597–605. doi: 10.1158/0008-5472.CAN-19-3176 [DOI] [PubMed] [Google Scholar]
- 127. Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harbor Perspect Biol (2014) 6(10):a016295. doi: 10.1101/cshperspect.a016295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Leary AG, Ikebuchi K, Hirai Y, Wong GG, Yang YC, Clark SC, et al. Synergism between interleukin-6 and interleukin-3 in supporting proliferation of human hematopoietic stem cells: comparison with interleukin-1 alpha. Blood (1988) 71(6):1759–63. doi: 10.1182/blood.V71.6.1759.1759 [DOI] [PubMed] [Google Scholar]
- 129. Ikebuchi K, Wong GG, Clark SC, Ihle JN, Hirai Y, Ogawa M. Interleukin 6 enhancement of interleukin 3-dependent proliferation of multipotential hemopoietic progenitors. Proc Natl Acad Sci USA (1987) 84(24):9035–9. doi: 10.1073/pnas.84.24.9035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Yao X, Huang J, Zhong H, Shen N, Faggioni R, Fung M, et al. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol Ther (2014) 141(2):125–39. doi: 10.1016/j.pharmthera.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 131. Inoue K, Sugiyama H, Ogawa H, Yamagami T, Azuma T, Oka Y, et al. Expression of the interleukin-6 (IL-6), IL-6 receptor, and gp130 genes in acute leukemia. Blood (1994) 84(8):2672–80. doi: 10.1182/blood.V84.8.2672.2672 [DOI] [PubMed] [Google Scholar]
- 132. Stevens AM, Miller JM, Munoz JO, Gaikwad AS, Redell MS. Interleukin-6 levels predict event-free survival in pediatric AML and suggest a mechanism of chemotherapy resistance. Blood Adv (2017) 1(18):1387–97. doi: 10.1182/bloodadvances.2017007856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Saadi MI, Ramzi M, Hosseinzadeh M, Ebrahimi N, Owjfard M, Abdolyousefi EN, et al. Expression levels of il-6 and il-18 in acute myeloid leukemia and its relation with response to therapy and acute GvHD after bone marrow transplantation. Indian J Surg Oncol (2021) 12(3):465–71. doi: 10.1007/s13193-021-01358-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Peterlin P, Gaschet J, Guillaume T, Garnier A, Eveillard M, Le Bourgeois A, et al. A new cytokine-based dynamic stratification during induction is highly predictive of survivals in acute myeloid leukemia. Cancer Med (2021) 10(2):642–8. doi: 10.1002/cam4.3648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Hou D, Wang B, You R, Wang X, Liu J, Zhan W, et al. Stromal cells promote chemoresistance of acute myeloid leukemia cells via activation of the IL-6/STAT3/OXPHOS axis. Ann Transl Med (2020) 8(21):1346. doi: 10.21037/atm-20-3191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Reikvam H, Brenner AK, Hagen KM, Liseth K, Skrede S, Hatfield KJ, et al. The cytokine-mediated crosstalk between primary human acute myeloid cells and mesenchymal stem cells alters the local cytokine network and the global gene expression profile of the mesenchymal cells. Stem Cell Res (2015) 15(3):530–41. doi: 10.1016/j.scr.2015.09.008 [DOI] [PubMed] [Google Scholar]
- 137. O’Hagan-Wong K, Nadeau S, Carrier-Leclerc A, Apablaza F, Hamdy R, Shum-Tim D, et al. Increased IL-6 secretion by aged human mesenchymal stromal cells disrupts hematopoietic stem and progenitor cells’ homeostasis. Oncotarget (2016) 7(12):13285–96. doi: 10.18632/oncotarget.7690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Säily M, Koistinen P, Savolainen M, Rantala M, Savolainen ER. Expression of interleukin-6 (IL-6) receptor gene in acute myeloblastic leukemia and response of leukemic cells to exogenous IL-6. A Comp study between Cell line Cells corresponding native Cells Growth Factors (1998) 15(4):243–57. doi: 10.3109/08977199809017481 [DOI] [PubMed] [Google Scholar]
- 139. Zhang Y, Guo H, Zhang Z, Lu W, Zhu J, Shi J. IL-6 promotes chemoresistance via upregulating CD36 mediated fatty acids uptake in acute myeloid leukemia. Exp Cell Res (2022) 415(1):113112. doi: 10.1016/j.yexcr.2022.113112 [DOI] [PubMed] [Google Scholar]
- 140. Chen R, Chen B. Siltuximab (CNTO 328): a promising option for human malignancies. Drug Des Devel Ther (2015) 9:3455–8. doi: 10.2147/DDDT.S86438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Zhang TY, Dutta R, Benard B, Zhao F, Yin R, Majeti R. IL-6 blockade reverses bone marrow failure induced by human acute myeloid leukemia. Sci Transl Med (2020) 12(538):eaax5104. doi: 10.1126/scitranslmed.aax5104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Xie K. Interleukin-8 and human cancer biology. Cytokine Growth Factor Rev (2001) 12(4):375–91. doi: 10.1016/S1359-6101(01)00016-8 [DOI] [PubMed] [Google Scholar]
- 143. Campbell LM, Maxwell PJ, Waugh DJ. Rationale and means to target pro-inflammatory interleukin-8 (CXCL8) signaling in cancer. Pharm (Basel. (2013) 6(8):929–59. doi: 10.3390/ph6080929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Vinante F, Rigo A, Vincenzi C, Ricetti MM, Marrocchella R, Chilosi M, et al. IL-8 mRNA expression and IL-8 production by acute myeloid leukemia cells. Leukemia (1993) 7(10):1552–6. [PubMed] [Google Scholar]
- 145. Tobler A, Moser B, Dewald B, Geiser T, Studer H, Baggiolini M, et al. Constitutive expression of interleukin-8 and its receptor in human myeloid and lymphoid leukemia. Blood (1993) 82(8):2517–25. doi: 10.1182/blood.V82.8.2517.2517 [DOI] [PubMed] [Google Scholar]
- 146. Schinke C, Giricz O, Li W, Shastri A, Gordon S, Barreyro L, et al. IL8-CXCR2 pathway inhibition as a therapeutic strategy against MDS and AML stem cells. Blood (2015) 125(20):3144–52. doi: 10.1182/blood-2015-01-621631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Kuett A, Rieger C, Perathoner D, Herold T, Wagner M, Sironi S, et al. IL-8 as mediator in the microenvironment-leukaemia network in acute myeloid leukaemia Sci Rep (2015) 5:18411. doi: 10.1038/srep18411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Konopleva M, Konoplev S, Hu W, Zaritskey AY, Afanasiev BV, Andreeff M. Stromal cells prevent apoptosis of AML cells by up-regulation of anti-apoptotic proteins. Leukemia (2002) 16(9):1713–24. doi: 10.1038/sj.leu.2402608 [DOI] [PubMed] [Google Scholar]
- 149. Nefedova Y, Landowski TH, Dalton WS. Bone marrow stromal-derived soluble factors and direct cell contact contribute to de novo drug resistance of myeloma cells by distinct mechanisms. Leukemia (2003) 17(6):1175–82. doi: 10.1038/sj.leu.2402924 [DOI] [PubMed] [Google Scholar]
- 150. Ryningen A, Wergeland L, Glenjen N, Gjertsen BT, Bruserud O. In vitro crosstalk between fibroblasts and native human acute myelogenous leukemia (AML) blasts via local cytokine networks results in increased proliferation and decreased apoptosis of AML cells as well as increased levels of proangiogenic interleukin 8. Leukemia Res (2005) 29(2):185–96. doi: 10.1016/j.leukres.2004.06.008 [DOI] [PubMed] [Google Scholar]
- 151. Vijay V, Miller R, Vue GS, Pezeshkian MB, Maywood M, Ast AM, et al. Interleukin-8 blockade prevents activated endothelial cell mediated proliferation and chemoresistance of acute myeloid leukemia Leukemia Res (2019) 84:106180. doi: 10.1016/j.leukres.2019.106180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Abdul-Aziz AM, Shafat MS, Mehta TK, Di Palma F, Lawes MJ, Rushworth SA, et al. MIF-induced stromal PKCβ/IL8 is essential in human acute myeloid leukemia. Cancer Res (2017) 77(2):303–11. doi: 10.1158/0008-5472.CAN-16-1095 [DOI] [PubMed] [Google Scholar]
- 153. Simonet WS, Hughes TM, Nguyen HQ, Trebasky LD, Danilenko DM, Medlock ES. Long-term impaired neutrophil migration in mice overexpressing human interleukin-8. J Clin Invest (1994) 94(3):1310–9. doi: 10.1172/JCI117450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Shi Y, Riese DJ. 2nd. Role CXCL12/CXCR4/CXCR7 Chemokine Axis Cancer. Front Pharmacol (2020) 11:574667. doi: 10.3389/fphar.2020.574667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Teicher BA, Fricker SP. CXCL12 (SDF-1)/CXCR4 pathway in cancer. Clin Cancer Res (2010) 16(11):2927–31. doi: 10.1158/1078-0432.CCR-09-2329 [DOI] [PubMed] [Google Scholar]
- 156. Khare T, Bissonnette M, Khare S. CXCL12-CXCR4/CXCR7 axis in colorectal cancer: Therapeutic target in preclinical and clinical studies. Int J Mol Sci (2021) 22(14):7371. doi: 10.3390/ijms22147371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Liao YX, Zhou CH, Zeng H, Zuo DQ, Wang ZY, Yin F, et al. The role of the CXCL12-CXCR4/CXCR7 axis in the progression and metastasis of bone sarcomas (Review). Int J Mol Med (2013) 32(6):1239–46. doi: 10.3892/ijmm.2013.1521 [DOI] [PubMed] [Google Scholar]
- 158. Daniel SK, Seo YD, Pillarisetty VG. The CXCL12-CXCR4/CXCR7 axis as a mechanism of immune resistance in gastrointestinal malignancies. Semin Cancer Biol (2020) 65:176–88. doi: 10.1016/j.semcancer.2019.12.007 [DOI] [PubMed] [Google Scholar]
- 159. Nazari A, Khorramdelazad H, Hassanshahi G. Biological/pathological functions of the CXCL12/CXCR4/CXCR7 axes in the pathogenesis of bladder cancer. Int J Clin Oncol (2017) 22(6):991–1000. doi: 10.1007/s10147-017-1187-x [DOI] [PubMed] [Google Scholar]
- 160. Chen N, Jiang X, Wang J, Wu T, Cheng B, Xia J. CXCL12-CXCR4/CXCR7 axis contributes to cell motilities of oral squamous cell carcinoma. Tumour Biol (2016) 37(1):567–75. doi: 10.1007/s13277-015-3803-6 [DOI] [PubMed] [Google Scholar]
- 161. Spoo AC, Lübbert M, Wierda WG, Burger JA. CXCR4 is a prognostic marker in acute myelogenous leukemia. Blood (2007) 109(2):786–91. doi: 10.1182/blood-2006-05-024844 [DOI] [PubMed] [Google Scholar]
- 162. Du W, Lu C, Zhu X, Hu D, Chen X, Li J, et al. Prognostic significance of CXCR4 expression in acute myeloid leukemia. Cancer Med (2019) 8(15):6595–603. doi: 10.1002/cam4.2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Zhao H, Guo L, Zhao H, Zhao J, Weng H, Zhao B. CXCR4 over-expression and survival in cancer: a system review and meta-analysis. Oncotarget (2015) 6(7):5022–40. doi: 10.18632/oncotarget.3217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Ahn JY, Seo K, Weinberg OK, Arber DA. The prognostic value of CXCR4 in acute myeloid leukemia. Appl Immunohistochem Mol Morphol (2013) 21(1):79–84. doi: 10.1097/PAI.0b013e3182606f4d [DOI] [PubMed] [Google Scholar]
- 165. Chen Y, Jacamo R, Konopleva M, Garzon R, Croce C, Andreeff M. CXCR4 downregulation of let-7a drives chemoresistance in acute myeloid leukemia. J Clin Invest (2013) 123(6):2395–407. doi: 10.1172/JCI66553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Ramakrishnan R, Peña-Martínez P, Agarwal P, Rodriguez-Zabala M, Chapellier M, Högberg C, et al. CXCR4 signaling has a CXCL12-independent essential role in murine MLL-AF9-Driven acute myeloid leukemia. Cell Rep (2020) 31(8):107684. doi: 10.1016/j.celrep.2020.107684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Cancilla D, Rettig MP, DiPersio JF. Targeting CXCR4 in AML and ALL. Front Oncol (2020) 10:1672. doi: 10.3389/fonc.2020.01672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Castro F, Cardoso AP, Gonçalves RM, Serre K, Oliveira MJ. Interferon-gamma at the crossroads of tumor immune surveillance or evasion. Front Immunol (2018) 9:847. doi: 10.3389/fimmu.2018.00847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Uhl FM, Chen S, O’Sullivan D, Edwards-Hicks J, Richter G, Haring E, et al. Metabolic reprogramming of donor T cells enhances graft-versus-leukemia effects in mice and humans. Sci Transl Med (2020) 12(567):eabb8969. doi: 10.1126/scitranslmed.abb8969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Toffalori C, Zito L, Gambacorta V, Riba M, Oliveira G, Bucci G, et al. Immune signature drives leukemia escape and relapse after hematopoietic cell transplantation. Nat Med (2019) 25(4):603–11. doi: 10.1038/s41591-019-0400-z [DOI] [PubMed] [Google Scholar]
- 171. Garcia-Diaz A, Shin DS, Moreno BH, Saco J, Escuin-Ordinas H, Rodriguez GA, et al. Interferon receptor signaling pathways regulating PD-L1 and PD-L2 expression. Cell Rep (2017) 19(6):1189–201. doi: 10.1016/j.celrep.2017.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Berthon C, Driss V, Liu J, Kuranda K, Leleu X, Jouy N, et al. In acute myeloid leukemia, B7-H1 (PD-L1) protection of blasts from cytotoxic T cells is induced by TLR ligands and interferon-gamma and can be reversed using MEK inhibitors. Cancer Immunol Immunother (2010) 59(12):1839–49. doi: 10.1007/s00262-010-0909-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Chen C, Liang C, Wang S, Chio CL, Zhang Y, Zeng C, et al. Expression patterns of immune checkpoints in acute myeloid leukemia. J Hematol Oncol (2020) 13(1):28. doi: 10.1186/s13045-020-00853-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Haroun F, Solola SA, Nassereddine S, Tabbara I. PD-1 signaling and inhibition in AML and MDS. Ann Hematol (2017) 96(9):1441–8. doi: 10.1007/s00277-017-3051-5 [DOI] [PubMed] [Google Scholar]
- 175. Xu L, Liu L, Yao D, Zeng X, Zhang Y, Lai J, et al. PD-1 and TIGIT are highly Co-expressed on CD8(+) T cells in AML patient bone marrow. Front Oncol (2021) 11:686156. doi: 10.3389/fonc.2021.686156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Dong Y, Han Y, Huang Y, Jiang S, Huang Z, Chen R, et al. PD-L1 is expressed and promotes the expansion of regulatory T cells in acute myeloid leukemia. Front Immunol (2020) 11:1710. doi: 10.3389/fimmu.2020.01710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Yang X, Ma L, Zhang X, Huang L, Wei J. Targeting PD-1/PD-L1 pathway in myelodysplastic syndromes and acute myeloid leukemia. Exp Hematol Oncol (2022) 11(1):11. doi: 10.1186/s40164-022-00263-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, et al. Innate lymphoid cells: 10 years on. Cell (2018) 174(5):1054–66. doi: 10.1016/j.cell.2018.07.017 [DOI] [PubMed] [Google Scholar]
- 179. Li Z, Ma R, Ma S, Tian L, Lu T, Zhang J, et al. ILC1s control leukemia stem cell fate and limit development of AML. Nat Immunol (2022) 23(5):718–30. doi: 10.1038/s41590-022-01198-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Junttila IS. Tuning the cytokine responses: An update on interleukin (IL)-4 and IL-13 receptor complexes. Front Immunol (2018) 9:888. doi: 10.3389/fimmu.2018.00888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Bankaitis KV, Fingleton B. Targeting IL4/IL4R for the treatment of epithelial cancer metastasis. Clin Exp Metastasis (2015) 32(8):847–56. doi: 10.1007/s10585-015-9747-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Li Z, Jiang J, Wang Z, Zhang J, Xiao M, Wang C, et al. Endogenous interleukin-4 promotes tumor development by increasing tumor cell resistance to apoptosis. Cancer Res (2008) 68(21):8687–94. doi: 10.1158/0008-5472.CAN-08-0449 [DOI] [PubMed] [Google Scholar]
- 183. Peña-Martínez P, Eriksson M, Ramakrishnan R, Chapellier M, Högberg C, Orsmark-Pietras C, et al. Interleukin 4 induces apoptosis of acute myeloid leukemia cells in a Stat6-dependent manner. Leukemia (2018) 32(3):588–96. doi: 10.1038/leu.2017.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Finch ER, Tukaramrao DB, Goodfield LL, Quickel MD, Paulson RF, Prabhu KS. Activation of PPARγ by endogenous prostaglandin J(2) mediates the antileukemic effect of selenium in murine leukemia. Blood (2017) 129(13):1802–10. doi: 10.1182/blood-2016-08-736405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Qian F, Arner BE, Kelly KM, Annageldiyev C, Sharma A, Claxton DF, et al. Interleukin-4 treatment reduces leukemia burden in acute myeloid leukemia FASEB J (2022) 36(5):e22328. doi: 10.1096/fj.202200251R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Miari KE, Guzman ML, Wheadon H, Williams MTS. Macrophages in acute myeloid leukaemia: Significant players in therapy resistance and patient outcomes. Front Cell Dev Biol (2021) 9:692800. doi: 10.3389/fcell.2021.692800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Pan Y, Yu Y, Wang X, Zhang T. Tumor-associated macrophages in tumor immunity. Front Immunol (2020) 11:583084. doi: 10.3389/fimmu.2020.583084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Saraiva M, O’Garra A. The regulation of IL-10 production by immune cells. Nat Rev Immunol (2010) 10(3):170–81. doi: 10.1038/nri2711 [DOI] [PubMed] [Google Scholar]
- 189. Kornblau SM, McCue D, Singh N, Chen W, Estrov Z, Coombes KR. Recurrent expression signatures of cytokines and chemokines are present and are independently prognostic in acute myelogenous leukemia and myelodysplasia. Blood (2010) 116(20):4251–61. doi: 10.1182/blood-2010-01-262071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Dong Q, Li G, Fozza C, Wang S, Yang S, Sang Y, et al. Levels and clinical significance of regulatory b cells and T cells in acute myeloid leukemia. BioMed Res Int (2020) 2020:7023168. doi: 10.1155/2020/7023168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Bruserud O. IL-4, IL-10 and IL-13 in acute myelogenous leukemia. Cytokines Cell Mol Ther (1998) 4(3):187–98. [PubMed] [Google Scholar]
- 192. Han Y, Dong Y, Yang Q, Xu W, Jiang S, Yu Z, et al. Acute myeloid leukemia cells express ICOS ligand to promote the expansion of regulatory T cells. Front Immunol (2018) 9:2227. doi: 10.3389/fimmu.2018.02227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Musuraca G, De Matteis S, Napolitano R, Papayannidis C, Guadagnuolo V, Fabbri F, et al. IL-17/IL-10 double-producing T cells: new link between infections, immunosuppression and acute myeloid leukemia. J Transl Med (2015) 13:229. doi: 10.1186/s12967-015-0590-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Xu Y, Mou J, Wang Y, Zhou W, Rao Q, Xing H, et al. Regulatory T cells promote the stemness of leukemia stem cells through IL10 cytokine-related signaling pathway. Leukemia (2022) 36(2):403–15. doi: 10.1038/s41375-021-01375-2 [DOI] [PubMed] [Google Scholar]
- 195. Jimbu L, Mesaros O, Neaga A, Nanut AM, Tomuleasa C, Dima D, et al. The potential advantage of targeting both PD-L1/PD-L2/PD-1 and IL-10-IL-10R pathways in acute myeloid leukemia. Pharm (Basel) (2021) 14(11):1105. doi: 10.3390/ph14111105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Chen N, Xu Y, Mou J, Rao Q, Xing H, Tian Z, et al. Targeting of IL-10R on acute myeloid leukemia blasts with chimeric antigen receptor-expressing T cells. Blood Cancer J (2021) 11(8):144. doi: 10.1038/s41408-021-00536-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Huang J, Liu Y, Au BC, Barber DL, Arruda A, Schambach A, et al. Preclinical validation: LV/IL-12 transduction of patient leukemia cells for immunotherapy of AML. Mol Ther Methods Clin Dev (2016) 3:16074. doi: 10.1038/mtm.2016.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Curti A, Pandolfi S, Aluigi M, Isidori A, Alessandrini I, Chiodoni C, et al. Interleukin-12 production by leukemia-derived dendritic cells counteracts the inhibitory effect of leukemic microenvironment on T cells. Exp Hematol (2005) 33(12):1521–30. doi: 10.1016/j.exphem.2005.08.005 [DOI] [PubMed] [Google Scholar]
- 199. Schnorfeil F, Lichtenegger F, Geiger C, Köhnke T, Bücklein V, Altmann T, et al. Next-generation dendritic cells for immunotherapy of acute myeloid leukemia. J Immunother Cancer (2014) 2:P84. doi: 10.1186/2051-1426-2-S3-P84 [DOI] [PMC free article] [PubMed] [Google Scholar]